Abstract
Importance:
To explore potential differences in pathophysiologies of OAB-wet and OAB-dry.
Objectives:
To define fundamental and unique presenting features of patients exhibiting storage lower urinary tract symptoms (LUTS) with urgency incontinence (OAB-wet) and patients without urgency incontinence (OAB-dry).
Study Design:
This was a secondary analysis of cross-sectional data from the NIH/NIDDK-sponsored Symptoms of Lower Urinary Tract Dysfunction Research Network. Demographic, physical exam, and questionnaire responses were analyzed for women seeking care for LUTS at 6 U.S centers. Differences between OAB-wet and OAB-dry subjects were compared using Fisher’s exact test and Mann-Whitney U test. Differences in questionnaire data were assessed using a Benjamini-Hochberg false discovery rate correction.
Results:
56, 84, and 67 women were included in the OAB-dry, wet, and control cohorts, respectively. There was no difference in demographic and physical exam characteristics of the two groups. OAB-wet patients reported more urgency incontinence symptoms (LUTS 16a, p<0.001). OAB-dry reported more bladder pain, feeling of incomplete bladder emptying (LUTS 4, p<0.001) and a need to strain to urinate (AUA-SI 7, p=0.003). Sensation of incomplete emptying and straining with urination did not correlate with elevated post-void residual volumes. While degrees of symptomatic bother were similar, bother in OAB-dry was most closely related to pelvic floor tenderness severity while bother in OAB-wet was most related to urgency severity.
Conclusion:
Women with OAB-dry have distinct presenting features of straining with urination, bladder pain, and a feeling of incomplete emptying. These suggest a unique pathophysiology driving OAB-dry symptoms, which we hypothesize is pelvic floor myofascial dysfunction.
Keywords: Overactive bladder, urgency incontinence, phenotype, high tone pelvic floor dysfunction
Introduction
Overactive bladder (OAB) is defined by the International Continence Society (ICS) as a storage symptom syndrome characterized by “urgency, with or without urgency urinary incontinence (UUI), usually with increased daytime frequency and nocturia”1. Patients with OAB are heterogeneous in nature, with some exhibiting urgency and frequency only (OAB-dry) and others displaying urgency and frequency with urgency incontinence (OAB-wet).
Cross-sectional studies such as NOBLE (National Overactive Bladder Evaluation) and EpiLUTS (Epidemiology of Lower Urinary Tract Symptoms) have estimated the prevalence of OAB in the US from 16.5% to 35.6%.2,3. Within the OAB population, frequency and urgency are the most common complaint occurring in 85% and 54% of individuals respectively, while only 36% of patients experience urge incontinence.4
Conventional thinking has been that OAB-dry and OAB-wet fall within a single spectrum of disease, with OAB-wet perhaps constituting a more severe form of OAB-dry. As such, current guidelines apply the same treatment algorithm to both, following a linear pathway based on treatment invasiveness. However, the high rate of discontinuation of OAB medications, lack of an option that provides total or permanent resolution of symptoms, and similar effectiveness of all options5 highlight the limitation of this “one size fits all” approach. Of note, most large-scale registration trials for medications and treatment like onabotulinumtoxinA include exclusively or predominately OAB-wet patients.6 As such, the efficacies of most these therapies have been are judged primarily by reductions in incontinence episodes.7 Few studies have tested these therapies in OAB-dry patients (mostly in post hoc analyses)8, leaving unknown their true efficacy for isolated urgency or frequency symptoms. Without an understanding of whether OAB reflects single or multiple etiologies, we will face substantial challenges to improving management and design new targeted therapies.
While prior research has examined the different urodynamic findings in patients with and without urgency incontinence9,10, little information compares specific presenting urinary symptoms, physical exam findings, and demographics for these two populations.
Thus, we sought to explore the unique features of OAB-dry and OAB-wet through a comparison of self-reported symptoms, physical exam findings, and demographic data in women seeking care for lower urinary tract symptoms (LUTS). With better understanding of the definitive features of OAB-wet vs. -dry, we can start to understand the potential difference in the pathophysiology of the two groups, which allows therapies to be tailored to achieving efficacious treatment sooner.
Materials and Methods
The Lower Urinary Tract Dysfunction Research Network (LURN) is a multi-center National Institute of Diabetes and Digestive and Kidney Diseases sponsored research network, whose development, objectives, and conceptual framework has been described previously.11 Deidentified data from the LURN was obtained from the NIDDK repository. This included demographic, physical exam, and questionnaire data for women with LUTS seeking care at six US centers. Questionnaire data contained responses to LUTS Tool, Functional Comorbidity Index (FCI), female Genitourinary Pain Index (fGUPI), Pelvic-Floor Distress Inventory (PFDI-20), and American Urologic Association Symptom Index (AUA-SI).
At enrollment, patients were categorized into urinary incontinence (UI) subtypes. UI subtype was determined by LURN clinical staff from responses to the LUTS Tool12. Participants were classified as having urgency incontinence (OAB-wet) if they responded “sometimes” or more to leakage due to a sudden feeling of needing to rush to urinate. Participants without incontinence who responded “sometimes” or more to sudden rush to urinate or “sometimes” or more to bothersome frequency were defined as OAB-dry. Those classified as having stress or mixed incontinence were excluded from data analysis for the purpose of this study. Patients with a major component of pelvic or bladder pain were ineligible for the LURN study. A control population within the LURN dataset without LUTS was also assessed with the same questionnaires and exam.12
RStudio (Version 1.4.1106) was used for data management and statistical analysis. Demographic and clinical characteristics of the LURN cohort were described using means and standard deviations for continuous variables and frequencies and percentages for categorical variables, and differences were assessed using chi-square or a Mann-Whitney U test, as appropriate. Questionnaire differences were compared between OAB-dry and control as well as OAB-wet and OAB-dry using a Mann-Whitney U test. For questionnaire data, a Benjamini-Hochberg false discovery rate (FDR) correction was conducted to account for the multiple related hypothesis testing. Additionally, within dry and wet groups the association of symptom severity with symptomatic bother was assessed using linear regression.
Results
In this multicenter dataset, 545 women presented with LUTS. Using the LURN classifications of incontinence type, 84 patients were defined as OAB-wet, 56 patients were defined as OAB-dry, and 67 patients were in the control population. Control group was used to define baseline population characteristics.
Overall, mean age of the cohort was 58.8± 14.1 years. Participants were predominantly white (83%). There were no significant differences in the demographics of the OAB-dry and OAB-wet population (Table 1), specifically with no differences in the mean age, postmenopausal status, or hormone use. There were more current or former smokers in the OAB-dry population compared to OAB-wet (41% vs 26%) although this did not meet statistical significance. There were no differences in pelvic surgery history between the two groups. Both groups had 10–12% of patients with a prior history of pelvic pain.
Table 1:
Demographic and medical history of LURN participants by OAB subgroup
| Control (n=67) n(%) |
OAB-dry (n=56) n(%) |
OAB-wet (n=84) n(%) |
Wet vs Dry p value |
|
|---|---|---|---|---|
|
| ||||
| Age (mean[SD]) | - | 58.4[16.1] | 56.8[15.8] | 0.95 |
|
| ||||
| Race | ||||
| American Indian/Alaskan Native | 0(0%) | 3(5%) | 1(1%) | 0.22 |
| Asian | 1(2%) | 3(5%) | 4(5%) | 0.99 |
| African-American | 9(13%) | 4(7%) | 16(19%) | 0.08 |
| Native Hawaiian/Pacific Islander | 0(0%) | 0(0%) | 1(1%) | 0.49 |
| White | 58(85%) | 46(83%) | 63(75%) | 0.31 |
| Multi-racial/Other | 0(0%) | 1(2%) | 0(0%) | NS |
|
| ||||
| BMI (kg/m2) (mean[SD]) | 28[7.1] | 30[6.7] | 31[7.9] | 0.31 |
|
| ||||
| Number of vaginal births (median [IQR]) | 0[0–2] | 1[0–2] | 2[0–2] | 0.25 |
|
| ||||
| Post-menopausal | 35(51%) | 34(61%) | 58(69%) | 0.35 |
|
| ||||
| Hormone use | 21(31%) | 10(17%) | 12(14%) | 0.72 |
|
| ||||
| Current or former smoker | 22(33%) | 23(41%) | 22(26%) | 0.09 |
|
| ||||
| Diabetes type I or II | 6(9%) | 8(15%) | 12(14%) | 0.93 |
|
| ||||
| COPD | 0(0%) | 10(18%) | 18(22%) | 0.44 |
|
| ||||
| Previous surgery | ||||
| Prior hysterectomy | 7(11%) | 18(32%) | 27(32%) | 0.96 |
| Prior surgery for LUTS | 0(0%) | 14(25%) | 14(17%) | 0.42 |
| Prior c-section | 14(21%) | 8(15%) | 11(13%) | 0.82 |
|
| ||||
| History of Pelvic pain | 1(2%) | 7(12%) | 9(11%) | 0.09 |
|
| ||||
| PVR (ml) (mean[SD]) | 29[42] | 43[48] | 47[64] | 0.73 |
|
| ||||
| Prolapse stage | - | 0.98 | ||
| Stage 0 | - | 28(50%) | 26(31%) | |
| Stage 1 | - | 13(23%) | 28(33%) | |
| Stage 2 | - | 9(16%) | 21(25%) | |
| Stage 3 | - | 2(3%) | 2(2%) | |
| Stage 4 | - | 0(0%) | 0(0%) | |
|
| ||||
| Finding of atrophy on exam | - | 12(22%) | 17(20%) | 0.85 |
|
| ||||
| Pelvic Floor Contraction Strength (Oxford Strength) (median [IQR]) | - | 2[2–4] | 2[1–3] | 0.24 |
There was no difference in prolapse stage between the two groups. Most participants had stage 0 or 1 prolapse (72.6% of OAB-dry and 63.8% of OAB-wet). There was no difference in finding of vaginal atrophy on exam, oxford pelvic floor contraction strength, or post-void residual (PVR).
A comparison of responses to the LUTS tool by OAB subtype demonstrated that the OAB-wet and OAB-dry groups had similar reporting of frequency, urgency, and nocturia. All the OAB-dry group had both bothersome urgency and frequency, apart from two participants who only had bothersome urgency. Both groups had significantly more urinary symptoms and symptomatic bother compared to the control population. As expected, OAB-wet group reported more urgency with fear of incontinence (LUTS 12, p<0.001) and more leakage while sleeping (LUTS 16e, p=0.001).
Interestingly, a greater number of OAB-dry women experienced a feeling of incomplete emptying after urination (LUTS 4, p<0.001 and fGUPI 5, p<0.001) and needing to “push or strain to begin urination” (AUA-SI 7, p=0.003). There was no relation of either the subjective sensation of incomplete voiding or the need to strain to empty with PVR volumes for either group. We therefore investigated the relationship between sensation of straining and incomplete emptying by simple linear regression (Figure 1). In OAB-dry subjects, there was a strong positive relationship between straining and incomplete emptying (slope 0.62, p=0.004). In contrast, OAB-wet subjects infrequently expressed the need to strain to empty, with little relation of this value to the sensation of incomplete emptying (slope 0.16, p=0.005).
Figure 1. OAB-dry subjects exhibit more subjective obstructive urinary symptom without objective obstructive findings.
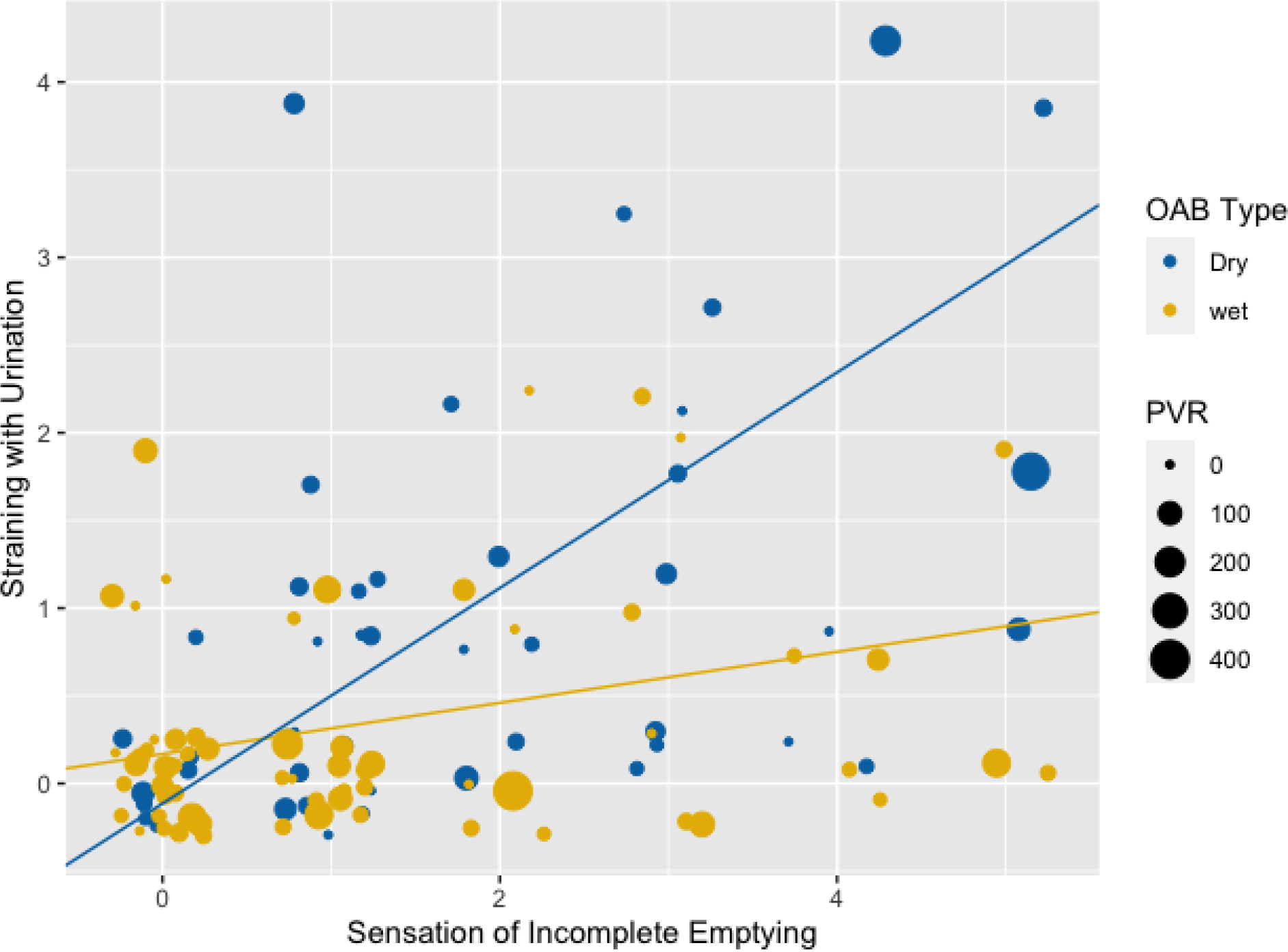
Plot of sensation of incomplete emptying vs. sensation of straining of urination. Lines represent linear regression with slope of OAB-wet line being 0.146, with intercept 0.169 and slope of OAB-dry line is 0.615 with intercept −0.115.
OAB-dry women also reported more “pain or discomfort in the bladder area” (LUTS 13, p<0.001). There was no difference between the two groups in reported pain of the vagina, urethra, or pelvic area as measured by fGUPI 1.
Both groups had similar rates of defecatory complaints on the CRADI-8 with all patients reporting low bother from bowel and defecatory symptoms. Despite the OAB-dry group having few incontinence symptoms, they had a similar dissatisfaction with their current symptoms as the OAB-wet group (fGUPI9). The full distribution of participant responses on the LUTS Tool, AUA-SI, fGUPI, and PFDI can be found in Table 2.
Table 2:
Questionnaire Responses by OAB sub group
| p-value * = significant with FDR correction | |||||||
|---|---|---|---|---|---|---|---|
| Questionnaire | Question | Scale | Control (Mean) |
Dry (Mean) |
Wet (Mean) |
dry vs. control | dry vs. wet |
| LUTS 1 | How often during the past week did you urinate too frequently? | 0–4 | 0.23 | 2.57 | 2.52 | <0.001* | 0.942 |
| LUTS 2 | During a typical day in the past week, how many times did you urinate during waking hours? | 0–4 | 0.80 | 2.00 | 1.64 | <0.001* | 0.030 |
| LUTS 3 | During a typical night in the past week, how many times did you wake up because you needed to urinate? | 0–4 | 0.55 | 1.83 | 1.74 | <0.001* | 0.008* |
| LUTS 4 | During the past week, how often have you had the feeling your bladder was not empty after urinating? | 0–4 | 0.06 | 1.50 | 1.24 | <0.001* | <0.001* |
| LUTS 6 | During the past week, how often have you had a sudden need to rush to urinate? | 0–4 | 0.35 | 2.34 | 2.56 | <0.001* | 0.022 |
| LUTS 7 | During the past week, how often have you had a delay before you start to urinate? | 0–4 | 0.08 | 0.71 | 0.57 | <0.001* | 0.684 |
| LUTS 9 | During the past week, how often did you strain to urinate or strain while you were urinating? | 0–4 | 0.03 | 0.71 | 0.33 | <0.001* | 0.025 |
| LUTS 12 | During the past week, how often have you had a sudden need to rush to urinate for fear of leaking urine? | 0–4 | 0.24 | 1.55 | 2.52 | <0.001* | <0.001* |
| LUTS 13 | During the past week, how often have you had pain or discomfort in your bladder area? | 0–4 | 0.03 | 0.88 | 0.55 | <0.001* | <0.001* |
| LUTS 14 | During the past week, how often have you had a burning feeling when you urinate? | 0–4 | 0.02 | 0.27 | 0.12 | 0.005* | 0.154 |
| LUTS 15 | During the past week, how often did you leak urine? | 0–4 | 0.24 | 0.66 | 2.05 | 0.001* | <0.001* |
| LUTS16a | Leaked urine in connection with a sudden need to rush to urinate? | 0–4 | 0.15 | 0.40 | 2.59 | 0.003* | <0.001* |
| LUTS 16e | Leaked urine when you are sleeping? | 0–4 | 0.00 | 0.12 | 0.64 | 0.035* | 0.001* |
| AUA-SI 5 | Over the past month or so, how often have you found it difficult to postpone urination? | 0–5 | 0.14 | 2.70 | 3.37 | <0.001* | 0.031 |
| AUA-SI 6 | Over the past month or so, how often have you had a weak urine stream? | 0–5 | 0.06 | 1.27 | 0.94 | <0.001* | 0.310 |
| AUA-SI 7 | Over the last month or so, how often have you had to push or strain to begin urination? | 0–5 | 0.00 | 0.85 | 0.30 | <0.001* | 0.003* |
| AUA-SI 8 | If you were to spend the rest of your life with your urinary condition just the way it is now, how would you feel about that? | 0–6 | 0.56 | 4.05 | 4.33 | <0.001* | 0.197 |
| fGUPI1a | Pain/discomfort at the entrance to the vagina | 0–1 | 0.00 | 0.22 | 0.14 | 0.699 | 0.911 |
| fGUPI1b | Pain/discomfort in the vagina | 0–1 | 0.00 | 0.20 | 0.09 | 0.713 | 0.862 |
| fGUPI1c | Pain/discomfort in the urethra | 0–1 | 0.00 | 0.13 | 0.06 | 0.767 | 0.891 |
| fGUPI1d | Pain/discomfort below the waist, in pubic or bladder area | 0–1 | 0.00 | 0.34 | 0.21 | 0.631 | 0.883 |
| fGUPI2a | Pain or burning during urination | 0–1 | 0.00 | 0.08 | 0.05 | 0.816 | 0.945 |
| fGUPI2b | Pain or discomfort during or after sexual intercourse | 0–1 | 0.00 | 0.11 | 0.11 | 0.785 | 1.000 |
| fGUPI2c | Pain or discomfort as your bladder fills | 0–1 | 0.00 | 0.34 | 0.22 | 0.632 | 0.893 |
| fGUPI2d | Pain or discomfort relieved by voiding | 0–1 | 0.00 | 0.45 | 0.21 | 0.580 | 0.801 |
| fGUPI3 | Frequency of pain or discomfort over the last week | 0–5 | 0.03 | 1.12 | 0.93 | <0.001* | 0.072 |
| fGUPI4 | Number that best describes average pain/discomfort | 0–10 | 0.10 | 2.08 | 1.56 | <0.001* | 0.059 |
| fGUPI5 | Frequency of sensation of incomplete emptying | 0–5 | 0.02 | 1.41 | 1.18 | <0.001* | <0.001* |
| fGUPI6 | Need to urinate <2 hours after last urinating | 0–5 | 0.32 | 2.93 | 2.63 | <0.001* | 0.368 |
| fGUPI7 | Have your symptoms kept you from doing the kinds of things you would usually do | 0–3 | 0.00 | 0.98 | 0.70 | <0.001* | 0.181 |
| fGUPI8 | How much did you think about your symptoms | 0–3 | 0.03 | 1.80 | 1.98 | <0.001* | 0.392 |
| fGUPI9 | Satisfaction with current symptoms | 0–6 | 0.40 | 3.95 | 4.02 | <0.001* | 0.641 |
| POPDI-1 | Pressure in the lower abdomen | 0–4 | 0.02 | 0.33 | 0.18 | <0.001* | 0.036 |
| POPDI-2 | Heaviness or dullness in the lower abdomen | 0–4 | 0.03 | 0.22 | 0.17 | 0.003* | 0.244 |
| POPDI-3 | A bulge or something falling out that can see or feel in the vaginal area | 0–4 | 0.02 | 0.12 | 0.10 | 0.025* | 0.690 |
| POPDI-4 | A need to push on the vagina or around the rectum to have a complete bowel movement | 0–4 | 0.00 | 0.07 | 0.07 | 0.032* | 0.252 |
| POPDI-5 | A feeling of incomplete bladder emptying | 0–4 | 0.00 | 0.40 | 0.36 | <0.001* | 0.796 |
| POPDI-6 | A need to push up in the vagina area to start or complete urination | 0–4 | 0.00 | 0.02 | 0.02 | 0.268 | 0.432 |
| CRADI-8–1 | A need to strain too hard to have a bowel movement | 0–4 | 1.63 | 2.23 | 2.26 | 0.011* | 0.718 |
| CRADI-8–2 | A feeling that you have not completely emptied your bowels after a bowel movement | 0–4 | 0.16 | 0.40 | 0.36 | 0.007* | 0.862 |
| CRADI-8–3 | Losing stool without control when stools are well formed | 0–4 | 0.00 | 0.12 | 0.06 | 0.005* | 0.595 |
| CRADI-8–4 | Losing stool without control when stool is loose or liquid | 0–4 | 0.08 | 0.28 | 0.24 | 0.012* | 0.531 |
| CRADI-8–5 | Losing gas from the rectum without control | 0–4 | 0.15 | 0.39 | 0.45 | 0.005* | 0.789 |
| CRADI-8–6 | Pain with passing stools | 0–4 | 0.02 | 0.12 | 0.11 | 0.011* | 0.788 |
| CRADI-8–7 | A strong sense of urgency and have to rush to the bathroom to have a bowel movement | 0–4 | 0.15 | 0.39 | 0.35 | 0.005* | 0.805 |
| CRADI-8–8 | Stool passes through the rectum and bulges outside during or after a bowel movement | 0–4 | 0.00 | 0.08 | 0.02 | 0.030* | 0.356 |
| UDI-6–1 | Bothered by frequent urination | 0–4 | 0.02 | 2.03 | 2.06 | <0.001* | 0.929 |
| UDI-6–2 | Bothered by leakage related to feeling of urgency | 0–4 | 0.06 | 0.20 | 0.81 | 0.003* | <0.001* |
| UDI-6–3 | Bothered by leakage related to physical activity, coughing, or sneezing | 0–4 | 0.07 | 0.17 | 0.20 | 0.096 | 0.923 |
| UDI-6–4 | Bothered by small amounts of leakage (drops) | 0–4 | 0.05 | 0.37 | 0.56 | <0.001* | 0.042 |
| UDI-6–5 | Bothered by difficulty emptying bladder | 0–4 | 0.00 | 1.93 | 2.22 | <0.001* | 0.213 |
| UDI-6–6 | Bothered by pain or discomfort in the lower abdominal or genital area | 0–4 | 0.00 | 0.21 | 0.13 | <0.001* | 0.321 |
Uncorrected p-values from Mann Whitney U test presented.
= p-value was statistically significant after applying Benjamini-Hochberg false discovery rate (FDR) correction
As the OAB-dry group exhibited similar symptomatic bother to OAB-wet, despite having significantly less severe urgency incontinence, we sought to determine the predominant symptoms driving these elevations in bother using linear regression analysis. For both OAB-dry and wet groups, overall symptom severity, as measured by the composite AUA SI, had a significant association with patient bother as measured by how frequently respondents thought about their symptoms in the last week. However, bother was impacted by different symptoms depending on OAB subgroup. Bother in the OAB-wet group had a positive association with the complaint of leaking urine in connection to a sudden need to urinate (slope 0.44, p=<.001). There was no association between urgency incontinence and bother in the OAB-dry group. In the OAB-dry group bother was most strongly associated with the finding of pelvic floor tenderness on exam (slope 0.85, p=0.036), but also associated with post-void dribbling (0.28, p=0.011) (Table 3).
Table 3:
Multiple Linear Regression comparing bother to specific symptom severity
| OAB-dry | OAB-wet | |||
|---|---|---|---|---|
| Slope [SE] | p-value | Slope[SE] | p-value | |
|
| ||||
| Composite AUA Symptom Score Index | 0.06 [0.02] | 0.008* | 0.06 [0.02] | 0.004* |
|
| ||||
| Average pain over last week | 0.12 [0.06] | 0.044* | 0.05 [0.05] | 0.352 |
|
| ||||
| Sudden rush to urinate for fear of leak | 0.25 [0.14] | 0.0835 | 0.44 [0.11] | 6.98E-05* |
|
| ||||
| Sudden need to rush to urinate | 0.54 [0.24] | 0.028* | 0.53 [0.11] | 1.05E-05* |
|
| ||||
| Pain or discomfort in bladder | 0.09 [0.12] | 0.453 | 0.05 [0.11] | 0.612 |
|
| ||||
| Pelvic floor tenderness | 0.86 [0.40] | 0.036* | 0.36 [0.30] | 0.24 |
|
| ||||
| Trickle or dribble at end of urine flow | 0.28 [0.11] | 0.011* | 0.09 [0.08] | 0.292 |
= p-value which is statistically significant
Discussion
Our results show while the demographics of women with OAB-dry and OAB-wet are similar, there are distinct differences in their presenting symptoms. Despite the OAB-dry group not having any incontinence, they have the same level of reported urgency, frequency, nocturia and bother from their symptoms compared with the wet group. One condition was not milder than the other and both were significantly more bothered than controls. OAB-dry patients more commonly experience a feeling of incomplete bladder emptying, straining to begin urination, and bladder pain; these symptoms, in conjunction with urinary urgency, were significantly associated with the elevated symptomatic bother. In agreement with previously published work, the perceived symptom of incomplete emptying did not correlate with actual urinary retention as there was no relation between subjective obstructive complaints and objective findings13.
It has been hypothesized across the literature14 that OAB-wet is a more severe form of OAB-dry, with OAB-wet having more detrusor overactivity on urodynamic testing. The presence of distinct patterns of symptoms in OAB-dry patients, some of which are significantly more severe than in OAB-wet, speaks against this assumption.
These results support while there is convergent symptomatology between the OAB-wet and OAB-dry groups, there are enough distinct differences between them to suggest divergent etiologies of the two conditions. OAB-wet symptomatology is dominated by the classic symptoms of urgency and UUI, which are the symptoms most closely associated with their level of bother. In contrast, OAB-dry patients have distinct symptoms not found in OAB-wet, and these symptoms, common features of pelvic floor myofascial dysfunction, are most closely associated with their similar high levels of symptomatic bother.
Future work is needed to determine why the OAB-dry patients have a feeling of incomplete emptying, straining to urinate, and bladder pain. We hypothesize these symptoms may represent a pelvic floor muscle dysfunction as opposed to a true bladder pathology. There is significant overlap between the bladder symptoms of OAB-dry and those in patients with high-tone pelvic floor dysfunction (HTPFD) or myofascial pelvic pain.15,16,17 Commonly reported urinary symptoms of HTPFD include urinary frequency, a sensation of incomplete bladder emptying, urinary hesitancy, varied force of urinary stream and discomfort with bladder filling.18, 12 There are several possible mechanisms by which overactive pelvic muscles may contribute to OAB symptoms. One mechanism is that changes in muscle function may lead to a change in the resting angle of the urethrovesical junction, which could cause irritation of the urethra or bladder neck.19 Alternatively, neuromuscular dysfunction may lead to HTPFD and OAB symptoms. Evaluation of pelvic floor myofascial fitness with standardized myofascial assessment20 and electromyography (EMG) in the OAB-dry population deserves further investigation.
This report has several strengths and limitations. Data was from a large national multi-center study involving all comers seeking care for LUTS. Most women were white, limiting the generalizability to a more diverse population of patients. The definition of incontinence and incontinence type was based solely on patient-reported questionnaires and are not corroborated with any objective testing. Furthermore, patients with significant pelvic pain were excluded from this cohort, resulting in mostly negative pelvic floor exam findings. As similar bladder symptoms are often seen in subjects with pelvic floor myalgia21, this exclusion criterion may have obscured additional features of OAB-dry patients, particularly pelvic floor myalgia or hypertonicity.
While much effort has been spent comparing the urodynamic and bladder diary findings of OAB patients with and without urgency incontinence, this comparison of presenting symptoms between the two groups provides valuable distinctions between OAB-dry and -wet to guide future mechanistic research.
Conclusions
OAB-wet and OAB-dry have been traditionally grouped under the larger OAB diagnosis and the same treatment pathway has been applied to both. By examining presenting symptoms of the two conditions, we see there are enough unique symptomatic features of each to suggest divergent etiologies. OAB-dry subjects present with the unique findings of straining with urination, feeling of incomplete emptying and pain, all which suggest a pelvic floor myofascial dysfunction. Further work is needed to examine the distinct pathophysiologies of these two LUTS groups.
Acknowledgements:
The LURN was conducted by the LURN Investigators and supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The data from the LURN reported here were supplied by the NIDDK Central Repositories. This manuscript was not prepared in collaboration with Investigators of the LURN study and does not necessarily reflect the opinions or views of the LURN study, the NIDDK Central Repositories, or the NIDDK. This work was also supported in part by the AUGS/Duke UrogynCREST Program (Urogynecology Clinical Research Educational Scientist Training) Program (R25HD094667 (NICHD)).
References
- 1.Abrams P, Cardozo L, Fall M et al. The standardization of terminology of lower urinary tract function: Report from the standardization sub-committee of the international continence society. Neurourol Urodyn, 2002;21:167–178. [DOI] [PubMed] [Google Scholar]
- 2.Stewart WF, Van Rooyen JB, Cundiff GW. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327–336. [DOI] [PubMed] [Google Scholar]
- 3.Sexton CC, Coyne KS, Thompson C, et al. Prevalence and effect on health-related quality of life of overactive bladder in older Americans: results from the epidemiology of lower urinary tract symptoms study. J Am Geriatrsoc. 2011;59:1465–1470. [DOI] [PubMed] [Google Scholar]
- 4.Milsom I, Abrams P, Cardozo L, et al. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001. Jun;87(9):760–6. [DOI] [PubMed] [Google Scholar]
- 5.Amundsen CL, Richter HE, Menefee SA, et al. Onabotulinumtoxin A vs Sacral Neuromodulation on Refractory Urgency Urinary Incontinence in Women: A Randomized Clinical Trial. JAMA. 2016;316(13):1366–1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chapple C, Sievert KD, MacDiarmid S, et al. OnabotulinumtoxinA 100 U significantly improves all idiopathic overactive bladder symptoms and quality of life in patients with overactive bladder and urinary incontinence: a randomised, double-blind, placebo-controlled trial. Eur Urol. 2013. Aug;64(2):249–56. [DOI] [PubMed] [Google Scholar]
- 7.Visco AG, Brubaker L, Richter HE, et al. Pelvic Floor Disorders Network. Anticholinergic therapy vs. onabotulinumtoxina for urgency urinary incontinence. N Engl J Med. 2012;367(19):1803–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rai BP, Cody JD, Alhasso A, et al. Anticholinergic drugs versus non-drug active therapies for non-neurogenic overactive bladder syndrome in adults. Cochrane Database Syst Rev. 2012. Dec 12;12(12) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anger JT, Le TX, Nissim HA, et al. How dry is “OAB-dry”? Perspectives from patients and physician experts. J Urol. 2012;188:1811–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsia S, Wu P, Chang T, et al. Urodynamic and Bladder diary Factors Predict Overactive Bladder-wet in Women: A comparison with Overactive Bladder-dry. Int Neurourol J. 2019;23(1):69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang CC, Weinfurt KP, Merion RM, et al. Symptoms of lower urinary tract dysfunction research network. J Urol. 2016;196:146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cameron AP, Lewicky-Gaupp C, Smith AR, et al. Symptoms of Lower Urinary Tract Dysfunction Research Network Study Group. Baseline Lower Urinary Tract Symptoms in Patients Enrolled in LURN: A Prospective, Observational Cohort Study. J Urol. 2018;199(4):1023–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Kuiken M, Volkin D, Zaila Ardines K, et al. Sensation of incomplete bladder emptying in women: Lack of correlation to an elevated post-void residual. Neurourol Urodyn. 2022;41(1):490–497. [DOI] [PubMed] [Google Scholar]
- 14.Hsia S, Wu P, Chang T, et al. Urodynamic and Bladder diary Factors Predict Overactive Bladder-wet in Women: A comparison with Overactive Bladder-dry. Int Neurourol J. 2019;23(1):69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faubion S, Shuster LT, Bharucha AE Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clinic proceedings, 2012;87(2):187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pastore EA, Katzman WB. Recognizing myofascial pelvic pain in the female patient with chronic pelvic pain. J Obstet Gynecol Neonatal Nurs. 2012;41(5):680–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meister MR, Sutcliffe S, Badu A, et al. Pelvic floor myofascial pain severity and pelvic floor disorder symptom bother: is there a correlation?. Am J Obstet Gynecol. 2019;221(3):235.e1–235.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finamore P, Goldstein H, Whitmore K Pelvic Floor Muscle Dysfunction, Journal of Pelvic Medicine and Surgery. 2008;14(6):417–422. [DOI] [PubMed] [Google Scholar]
- 19.Knight S, Luft J, Nakagawa S, et al. Comparisons of pelvic floor muscle performance, anxiety, quality of life and life stress in women with dry overactive bladder compared with asymptomatic women. BJU Int. 2012;109(11):1695–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meister MR, Sutcliffe S, Ghetti C, et al. Development of a standardized, reproducible screening examination for assessment of pelvic floor myofascial pain. Am J Obstet Gynecol. 2019;220(3):255.e1–255.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolff BJ, Joyce CJ, Brincat CA, Mueller ER, Fitzgerald CM. Pelvic floor myofascial pain in patients with symptoms of urinary tract infection. Int J Gynaecol Obstet. 2019;145(2):205–211 [DOI] [PubMed] [Google Scholar]


