Abstract
Venovenous (VV) extracorporeal membrane oxygenation (ECMO) is a form of mechanical life support that provides full respiratory bypass in patients with severe respiratory failure as a bridge to recovery or lung transplantation. The use of ECMO for respiratory failure and capable centers offering ECMO has expanded over the years, increasing its availability. As VV-ECMO provides an artificial mechanism for oxygenation and decarboxylation of native blood, it allows for an environment in which safer mechanical ventilatory care may be provided, allowing for treatment and resolution of underlying respiratory pathologies. Landmark clinical trials have provided a framework for better understanding patient selection criteria, resource utilization, and outcomes associated with ECMO when applied in settings of refractory respiratory failure. Maintaining close vigilance and management of complications during ECMO as well as identifying strategies post-ECMO (e.g., recovery, transplantation, etc.), are critical to successful ECMO support. In this review, we examine considerations for candidate selection for VV-ECMO, review the evidence of utilizing VV-ECMO in respiratory failure, and provide practical considerations for managing respiratory ECMO patients, including complication identification and management, as well as assessing for the ability to separate from ECMO support and the procedures for decannulation.
Keywords: ECMO, ECLS, Respiratory failure, Extracorporeal support, ARDS
Key Summary Points
| The use of VV-ECMO in patients with severe acute respiratory failure has dramatically increased in recent years. |
| VV-ECMO enables a respiratory support environment in which safer, less injurious mechanical ventilator care can be provided, thereby placing an emphasis on minimizing ventilator-induced lung injury. |
| VV-ECMO provides an artificial mechanism of gas exchange while underlying pulmonary pathologies resolve or lung transplantation is pursued. |
| Successful ECMO support requires individualization of cannulation and management strategies. |
Introduction
Extracorporeal membrane oxygenation (ECMO) is a form of modified cardiopulmonary bypass that provides temporary respiratory and/or cardiac support. In a venovenous (VV) configuration, ECMO provides a means of artificial oxygenation and decarboxylation in patients suffering hypoxemic and/or hypercapnic respiratory failure with preserved cardiac function thereby allowing for recovery of underlying pulmonary pathologies or facilitating support pending lung transplantation when medically indicated [1]. Importantly, ECMO enables a respiratory support environment in which safer, less injurious mechanical ventilator care can be provided, thereby placing an emphasis on minimizing ventilator-induced lung injury [2].
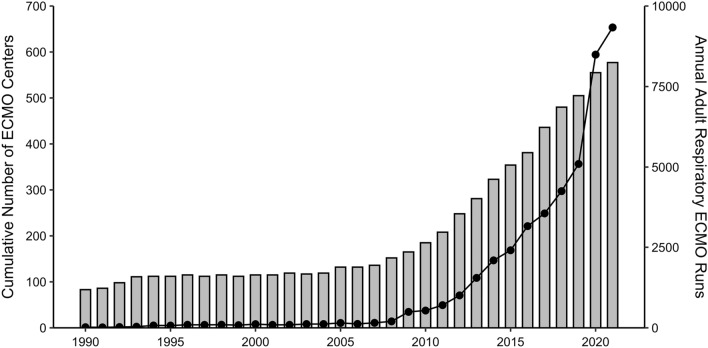
The number of centers worldwide providing ECMO continues to rise and the use of ECMO for respiratory failure has dramatically increased over the years, and now available in over 50 countries (Fig. 1) [3]. Over the past decade, there has been a greater than tenfold increase the global annual number of adult respiratory ECMO runs having approached 10,000 runs in 2021. Superimposed upon the general trend towards increased ECMO volumes, outbreaks of H1N1 influenza in 2009 [4, 5], Middle East Respiratory Syndrome in 2012–2015 [6], and SARS-CoV-2 (COVID-19) in 2020 [7, 8] were temporal periods that saw particularly elevated utilization of VV-ECMO (Fig. 1). Additionally, interhospital [9], regional [10], and remote retrievals [11] to referral ECMO centers with utilization of regional experts to establish new programs during crisis [12] has further expanded global accessibility to this complex resource. In this review, we examine considerations for candidate selection for ECMO, review the evidence of utilizing ECMO in respiratory failure, and provide practical considerations for managing respiratory ECMO patients.
Fig. 1.
International trends of cumulative number of ECMO centers worldwide (bars) and annual number of adult respiratory ECMO runs (line) over time (data sourced from the Extracorporeal Life Source Organization Registry [3])
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Clinical Trial Evidence
CESAR 2009
The Conventional ventilation or ECMO for Severe Acute Respiratory failure (CESAR) trial was a United Kingdom-based trial in which adults with severe respiratory failure and a Murray score of ≥ 3 or uncompensated hypercapnia were eligible [13]. One-hundred eighty patients were randomized to transfer to a referral center for continued conventional mechanical ventilatory management or transfer to an ECMO center for consideration of cannulation. Included patients had primarily hypoxemic respiratory failure due to pneumonia or acute respiratory distress syndrome (ARDS), with a PaO2/FiO2 (P/F) ratio of 75 and a mean Murray score of 3.5 at entry. Patients in the ECMO arm had greater steroid use and spent longer durations under low-pressure/low-volume ventilation. The use of pulmonary vasodilators was minimal in both arms. In the intention-to-treat analysis, those in the ECMO arm were less likely to die or have severe disability at 6 months (37 vs. 53%, RR 0.69, 95% CI 0.05–0.97, p = 0.03). Due to the trial design, it is challenging to distinguish the true benefits of ECMO from optimal conventional management at a specialized center. Indeed, 22 patients (24%) randomized to the ECMO arm never received ECMO with the majority manifesting clinical improvement following conventional management.
EOLIA 2018
The ECMO to Rescue Lung Injury in Severe ARDS (EOLIA) trial was a multicontinental trial that included 249 patients with severe ARDS defined by P/F < 50 for > 3 h, P/F < 80 for > 6 h, or PCO2 ≥ 60 mmHg with pH < 7.25 for > 6 h [14]. Patients were randomized to ECMO or conventional management that encouraged the use of pharmacologic neuromuscular blockade and prone ventilation. At study entry, the mean P/F ratio was approximately 73 with fully half of the patients having received inhaled pulmonary vasodilators. Importantly, the median duration from endotracheal intubation to randomization was 34 h. The trial was terminated early due to futility (planned enrollment, n = 331). In the intention-to-treat analysis at 60 days, mortality was lower in the ECMO group (35 vs. 46%, RR 0.76, 95% CI 0.55–1.04, p = 0.09), albeit non-statistically significant. Of note, 35 patients in the conventional arm (28%) crossed over and were cannulated for ECMO at a median of 4 days following randomization with these patients manifesting elevated plateau and driving pressure, increased vasoactive use, and exacerbated acidosis as compared to those not requiring crossing over. It is important to recognize that the 60-day mortality in these crossover patients (57%) was significantly greater than the remainder of the conventional arm (41%).
A Bayesian post hoc analysis of the EOLIA trial data found a 96% posterior probability of a RR < 1 for 60-day mortality [15]. An individual patient data meta-analysis of the CESAR and EOLIA trials found a reduced risk of 90-day mortality in ECMO recipients compared to conventional management (RR 0.75, 95% CI 0.6–0.94, p = 0.013) [16]. Additionally, a meta-analysis of these two trials pooled with three observational studies found reduced risk of 60-day mortality with use of ECMO (RR 0.73, 95% CI 0.58–0.92, p = 0.008) [17]. In a network meta-analysis evaluating the effect of protective ventilation strategies on hospital mortality, ECMO was amongst the most promising performers (RR 0.78, 95% CI 0.58–1.05, p = 0.10) [18]. However, this was limited to the those with severe respiratory failure and the settings of CESAR and EOLIA, as these were the only trials included in the analysis. Lastly, data from CESAR and subsequent analyses have demonstrated cost-effectiveness and increased quality-adjusted life years with ECMO compared to conventional mechanical ventilator managed severe ARDS [13, 19].
COVID-19
Randomized controlled trial data assessing the efficacy of ECMO for COVID-19-associated respiratory failure are lacking. Several emulated trials have attempted to provide estimates, all with seemingly encouraging results [20–22]. While such studies are utilized to estimate causal effect, they do so through observational data, and are therefore by nature prone to confounding and selection biases. A recent meta-analysis of 42 observational studies sought to examine prognostic factors associated with mortality of 17,449 ECMO treated COVID-19 patients [23]. Amongst those factors with high certainty of evidence included older age and higher driving pressures, and with moderate certainty included male sex, chronic lung disease, longer symptom duration and mechanical ventilation, lower P/F ratio, bacterial co-infection, and lower volume ECMO centers.
Patient Selection
Indications
VV-ECMO is utilized in patients with refractory hypoxemia, acidosis due to hypercarbia, or for procedural support when more conventional means of oxygenation and ventilation have failed. Prior to initiation of VV-ECMO, patients are typically undergoing some or all of the combination of ARDSnet or other optimized modes of ventilation, pharmacologic neuromuscular blockade, prone positioning, and inhaled pulmonary vasodilators [1, 24–27]. VV-ECMO, as with all temporary methods of support, should only be used for patients with a pathway to recovery or lung transplant. Indications for VV-ECMO initiation include ARDS due to infectious or inflammatory causes, aspiration pneumonitis, blunt chest injury, refractory status asthmaticus, or lung transplant [1, 4, 22, 28–33].
Contraindications
The purpose of VV-ECMO is to support a patient either to lung recovery or transplantation, or occasionally through a procedure. As such, if a patient is unrecoverable and is not a candidate for lung transplantation, VV-ECMO should not be deployed. Though rare, a complete lack of vascular access options also precludes the use of VV-ECMO.
Other conditions that should prompt serious consideration as to the benefits of VV-ECMO include severe neurologic injury such as large stroke or significant intracranial hemorrhage with inability to recover. Additionally, VV-ECMO is less likely to be beneficial in circumstances of active hemorrhage, end-stage cancer with life expectancy less than 1 year, and baseline multiorgan dysfunction that cannot be progressed to transplantation (e.g., cirrhosis, end-stage heart failure, or bone marrow suppression to the point of need for chronic transfusion). Extreme age is typically viewed as a relative contraindication to VV-ECMO and many institutions consider age above 70 as the threshold, though in the COVID-19 population a reduced age of 65 may be reasonable based on the available published data [1, 22]. A threshold for mechanical ventilation duration is a contested topic, with the Extracorporeal Life Support Organization (ELSO) stating that 7 days or more of mechanical ventilation at an FiO2 above 90% is a relative contraindication to VV-ECMO support [1].
Selection Considerations
Physiologic selection criteria (hypoxemia and respiratory acidosis) for VV-ECMO are typically based on two clinical trials [13, 14]. The EOLIA trial used several inclusion criteria based on the ratio of partial pressure of oxygen (PaO2) to fraction of inspired oxygen (FiO2), also known as the P/F ratio < 80 for > 6 h or < 50 for > 3 h [14]. Additionally, pH criteria of < 7.25 with a PaCO2 of 60 mmHg or greater for over 6 h despite a respiratory rate of 35 and a plateau pressure as high as 32 was also used. The most recent ELSO guidelines utilize these criteria (with the notable difference of a plateau pressure of 30 cm H2O or less), in addition to the need for support to receive lung transplantation, as indications for VV-ECMO initiation [1].
Scoring Systems and Prognostication
The most well-known scoring systems are the Murray score and the RESP score [34, 35]. The Murray score was first described in 1988 and combines chest radiograph consolidations, P/F ratio, positive end expiratory pressure (PEEP), and respiratory compliance assess ARDS survival in a non-VV-ECMO cohort [34]. The RESP score estimates survival in patients already undergoing VV-ECMO support by the parameters of age, PaCO2 of 75 mmHg or above, peak inspiratory pressure of 42 cm H2O and above, immune status, mechanical ventilation duration, diagnosis, central nervous dysfunction, non-pulmonary infection status, and pre-VV-ECMO parameters of neuromuscular blockade, nitric oxide, sodium bicarbonate, and cardiac arrest [35]. Notably, a high Murray score implies lower survival while a high RESP score implies improved survival. Other prediction scores also exist such as the PRESET score [36], the ECMOnet score [37], and the PRESERVE score [38].
Duration and Requirement of Mechanical Ventilation
The duration of mechanical ventilation prior to VV-ECMO initiation is used by many centers as part of the decision-making process for cannulation. In the CESAR trial, greater than 7 days of either peak pressures above 30 cm H2O or FiO2 greater than 0.8 excluded patients from the study [13]. In the trial by the EOLIA group, a mechanical ventilation duration of greater than 7 days excluded patients from randomization. More recently, a registry analysis of 7345 patients with COVID-19 (844 of which were supported by VV-ECMO) found that increasing ventilator duration prior to cannulation was statistically significantly associated with lower survival [22]. Additionally, this study also found that ECMO was most effective in patients with driving pressures above 15 mm H2O [22]. Increasing driving pressures have also been associated with increased mortality during VV-ECMO support [39].
Cannulation and General Management
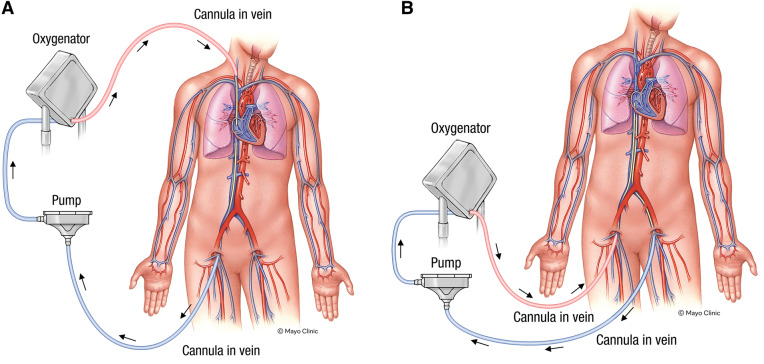
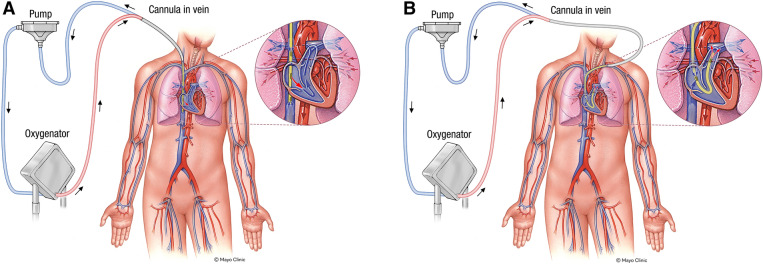
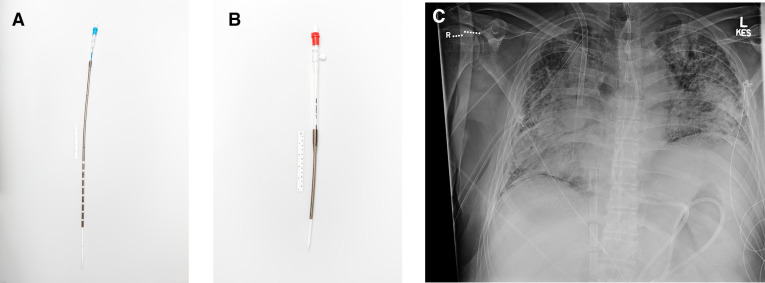
The basic ECMO circuit consists of inflow (drainage) and outflow (return) lumens, tubing, a centrifugal pump, a membrane oxygenator, and a heat exchanger (Figs. 2, 3). The general approach to ECMO management necessitates delivery of appropriate gas exchange, augmentation of mechanical ventilatory settings, and close attention to possible complications including circuit-related mechanical issues, renal impairment, cardiovascular compromise, and hemorrhage (Table 1).
Fig. 2.
Example VV-ECMO circuit configurations utilizing a two-cannula approach. a Right femoral vein to right internal jugular vein. b Left femoral vein to right femoral vein. Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved
Fig. 3.
Example VV-ECMO circuit configurations utilizing a single dual-lumen cannula approach. a Dual-lumen cannula via right internal jugular vein access. b Dual-lumen cannula pseudo-right ventricular assist device configuration via left subclavian vein access. Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved
Table 1.
Most common VV-ECMO complications
| Complication | Total (N = 30,717) |
|---|---|
| Mechanical | |
| Oxygenator failure | 5534 (18.0%) |
| Circuit exchange | 3581 (11.7%) |
| Cannula problems | 2015 (6.6%) |
| Hemorrhagic | |
| Surgical site hemorrhage | 2001 (6.5%) |
| Gastrointestinal hemorrhage | 1824 (5.9%) |
| Renal | |
| Required renal replacement therapy | 7772 (25.3%) |
| Serum creatinine 1.5–3.0 | 3296 (10.7%) |
| Cardiovascular | |
| Arrhythmia | 2908 (9.5%) |
| Required CPR | 1706 (5.6%) |
| Pulmonary | |
| Pneumothorax | 3282 (10.7%) |
Data sourced from Extracorporeal Life Support Organization Registry and includes 30,717 adult respiratory ECMO runs from 2017 to 2021 [3]. Complications summarized are those reported with > 5% frequency
Gas Exchange Dynamics
In general, a VV-ECMO circuit consists of venous drainage to a centrifugal pump in series with a membrane oxygenator followed by the return of oxygenated and decarboxylated blood back to the venous circulation whereby the native heart then serves to propel the necessary blood volume from the left ventricle to maintain end-organ perfusion. Contemporary oxygenators are constructed of polymethylpentene hollow gas fibers to maintain physical separation of the blood and gas compartments, while efficiency is provided through parallelization of pathways and the associated massive surface area where passive diffusion of gas down its concentration gradient with the blood components. Oxygen contained in the gas passing through the hollow tubules, known as sweep gas, migrates down its concentration gradient to the blood components (bound to hemoglobin and solubilized) while carbon dioxide moves in a reverse direction from dissolved plus bound sites within blood into the sweep gas. Manipulation of the concentration of oxygen contained within the sweep gas adjusts the imparting of oxygen into the blood passing through the artificial lung while maintaining of the concentration gradient for carbon dioxide through adjustments of the flow rate of the sweep gas enables achievement of the desired patient PaCO2.
Cannula Configuration
When considering cannulation strategy for VV-ECMO, the primary goals are to maximize flow and minimize recirculation of blood (i.e., back to the ECMO circuit). Standard cannula designs utilize wire-reinforced polyurethane that is resistant to kinking or collapse that are inserted percutaneously over a guidewire via the Seldinger technique. The most commonly employed drainage cannulation strategy involves the insertion of a multiport venous drainage cannula into the femoral vein with the tip advanced to approximately 5–10 cm below the inferior vena cava-right atrial junction (Fig. 4). A second dedicated long (> 50 cm) outflow cannula is then inserted either through the contralateral femoral vein and advanced until the tip lies in the right atria (Fig. 2b) or, alternatively, a shorter (20 cm) venous cannula may be placed through the right internal jugular vein with the tip advanced to the superior vena cava-right atrial junction (Fig. 2a). While it is possible to reverse the path of blood flow by utilizing the cephalad cannula (insertion via the right internal jugular) as the drainage cannula with the return then being the caudad cannula (insertion into the femoral vein), this technique is more prone to recirculation and is generally not recommended [40].
Fig. 4.
Multistage femoral venous drainage cannula (a), jugular vein return cannula (b), and corresponding chest film of VV-ECMO configuration with a right femoral multistage venous drainage cannula and a right internal jugular vein return cannula (c). Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved
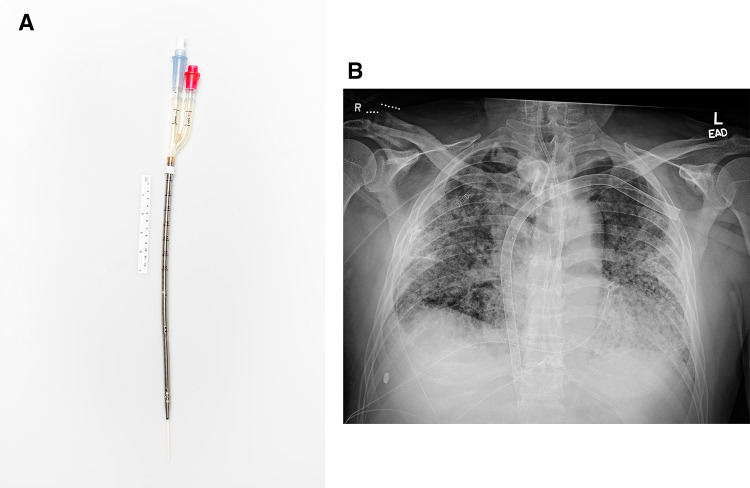
The development of dual-lumen cannulae (e.g., Avalon Elite, Bi-caval Dual-Lumen Catheters, Avalon Laboratories; Crescent, Bi-caval Dual-Lumen Catheters, Medtronic) facilitated the delivery of VV-ECMO through a single insertion site; most typically the right internal jugular vein although the subclavian vein may also be utilized (Fig. 5). The self-reinforcing lumens enable dual drainage from the SVC and IVC while the return lumen carefully positioned with the ejection port directed towards the tricuspid valve thereby permitting the return of oxygenated blood back to the right atrium while encouraging forward flow across the tricuspid valve to mitigate recirculation (Fig. 3a). Image guidance with transesophageal echocardiography and fluoroscopy is used at most centers [41]. Numerous advantages for this technique include simplification of the circuit using a single cannula, low rates of recirculation if adequate positioning is maintained, ease of prone positioning and medical transportation, and augmented ability to ambulate patients with extended duration support. Disadvantages include the limited range of cannula diameter, the increased requirement for image guidance during insertion and cannula repositioning, challenges associated with securement at the insertion site, potential for cerebral venous congestion, and limited flow rates as compared to dual-cannula strategies [42].
Fig. 5.
Dual-lumen cannula (a) with corresponding chest film with cannula placed via left subclavian access (b). Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved
Cardiovascular Compromise During VV-ECMO
Acute right ventricular dysfunction is both common and potentially lethal in acute respiratory failure while frequently manifesting secondary to alterations in one or more of the determinants of right ventricular performance (preload, afterload, and contractility). The most frequent etiologies in the context of respiratory failure include acute pulmonary embolism that yields cardiogenic shock in approximately 5% of cases while carrying a greater than 50% 90-day mortality rate [43] and ARDS associated acute RV dysfunction occurring in 30–56% of cases due to elevated pulmonary vascular resistance and/or impairment in RV contractile function [44]. A percutaneous right ventricular assist device (RVAD) offers the capability of augmenting blood flow through the native pulmonary system while the incorporation of a membrane oxygenator into the RVAD facilitates the oxygenation and decarboxylation of blood representative of VV-ECMO. Percutaneous RVAD support in the setting of acute respiratory failure is most frequently accomplished through the use of a dual-lumen cannula inserted through the right internal jugular or left subclavian vein where it is advanced across the tricuspid and pulmonic valves with the tip placed into the common pulmonary artery (Fig. 3b). The Protek Duo cannula (LivoNova, London, UK) represents one example of a dedicated dual-lumen cannula designed for percutaneous RVAD support that offers up to 4.5 L per minute of flow [45].
Myocardial dysfunction due to hypoxemia, elevated pulmonary vascular resistance, pulmonary embolism, myocardial infarction, or myocarditis can occur in COVID-19. Any one or a combination of the aforementioned pathologies may occur in patients supported by VV-ECMO, and hemodynamic collapse has occurred in this patient population necessitating either pulmonary artery or systemic arterial support [46]. One early report of approximately 50 COVID-19 patients supported by ECMO found that seven required arterial support: four with cardiac arrest due to hypoxia, two with pulmonary embolism, and one with myocarditis [46]. A report from the ELSO registry found that of 4792 patients undergoing ECMO support for COVID-19, 234 (4.9%) underwent venoarterial (VA)-ECMO support [47]. Furthermore, of this 4792 patient cohort, 88 carried a diagnosis of myocarditis (though approximately only half of these 88 underwent VA-ECMO support) [47]. Mortality in the myocarditis group was 51%, in line with the average mortality of the general population undergoing VA-ECMO as well as the COVID-19 VV-ECMO population [47]. We believe that patients with COVID-19 supported by VV-ECMO should be monitored very closely for signs of hemodynamic decompensation due to multiple etiologies, and that mechanical hemodynamic support should be added by pulmonary arterial or systemic arterial support devices if indicated. In fact, in select patients with COVID-19, hemodynamic support with either VA-ECMO or veno-pulmonary arterial-ECMO (i.e., RVAD configuration) may be the most prudent initial support strategy to achieve hemodynamic stability and rescue the most decompensated patients. If peripheral VA-ECMO is utilized in patients with COVID-19 ARDS, north–south syndrome (also known as Harlequin syndrome or differential hypoxemia) must be closely monitored for [48].
ECMO Management
Following cannulation performed with heparinization, ECMO is commenced by unclamping the circuit and gradually increasing flows towards the intended range. Important parameters utilized to determine pump flows include the oxygen saturation of blood (SaO2) and the oxygen saturation of the blood in the ECMO drainage cannula (SdO2) [49]. In the absence of native lung function, VV-ECMO blood flows must be maintained > 60% of the native cardiac output to consistently achieve a systemic arterial saturation of at least 90% [50] while targeting a DO2/VO2 (oxygen delivery to oxygen consumption ratio) of ≥ 3 as recommended by ELSO [51]. It is important to recognize that although no direct hemodynamic support is provided by VV-ECMO, normalization of PaCO2 and PaO2 may improve pulmonary vascular resistance and myocardial performance with attendant improvements in hemodynamics.
Ventilator settings while supported on VV-ECMO can vary based upon the underlying pathophysiology with ideal settings yet to be definitively defined. Typical rest settings consist of pressure-controlled ventilation with low respiratory rates (< 12 bpm), low tidal volumes (< 4–6 ml/kg), low FiO2 (< 50%), peak inspiratory pressure (< 25 cm H2O), and positive end expiratory pressure (< 12 cm H2O) [1]. Centers offering ECMO leverage internally developed protocols for the management of bleeding, transfusion, blood volume, temperature, nutrition, patient positioning, and infection prevention. Drug disposition is altered by increased volumes of distribution, reduced drug elimination, and drug sequestration to ECMO circuit components thereby necessitating dose adjustments and close partnership with clinical pharmacists for the optimal management of VV-ECMO patients [52]. These considerations are exacerbated by the frequent occurrence of multisystem organ dysfunction, systemic inflammatory response, hemodilution, acute renal and hepatic failure associated with critically ill patients portending significant difficulties in pharmacologic management [53].
An important consideration with regard to ECMO is the careful weighing of the requirement for anticoagulation to mitigate thrombus deposition against the necessity to avoid hemorrhage as both are associated with adverse outcomes [54]. Despite advances in material and circuit design, including biocompatible surface coatings and improved flow metrics, thromboembolic and hemorrhagic complications still complicate 10–30% of ECMO runs [55]. The ECMO circuit serves as a classic model of contact-phase activation whereby prolonged contact between the blood with the non-endothelial surfaces of the artificial components activates primary and secondary hemostatic cascades cumulating in the genesis of fibrin deposition and clot deposition [56]. Consequently, the prolonged maintenance of an ECMO circuit typically necessitates systemic anticoagulants to prevent thrombus formation. The most frequently utilized agent is unfractionated heparin due to its ubiquitous availability, rapid onset of action, titratability, and availability of an antidote with protamine. Important limitations include the requirement for the cofactor antithrombin that is essential for its clinical action but predisposes to fluctuations in dose sensitivity and its proclivity to trigger immune (type 2) and non-immune (type 1) thrombocytopenia [57]. In contrast, direct thrombin inhibitors (e.g., bivalirudin) down regulate the cleavage of fibrinogen into its active form without the need of a cofactor through the transient inhibition of thrombin [58]. Potential advantages include the ability to act on soluble (circulating) and clot-bound thrombin yielding abatement of propagation of existing thrombus [59], ease of titratability, and short half-life (approximately 25 min for bivalirudin) while the chief downside is the lack of a reversable agent. Recently, an expanding body of evidence has been published demonstrating the potential superiority of bivalirudin as compared to unfractionated heparin for maintenance systemic anticoagulation in adult and pediatric ECMO [60–64].
Considerable controversy remains with regard to optimal anticoagulant intensity, titration strategy (e.g., frequency of laboratory assessment and assay utilized), antithrombin replacement in patients receiving unfractionated heparin [65, 66], and the biocompatible surface coating employed advances in durable biocompatible coatings (covalently or ionically bonded heparinoids, phosphorylcholine, poly acrylates) [67] have facilitated surface coating of most components, including polymethylpentene membrane oxygenators, and allow patients to be maintained on low, or even absent, levels of anticoagulation for prolonged periods with acceptably low rats of complication [68]. Bleeding complications for ECMO patients are frequent and include cannulation and/or surgical site bleeding, gastrointestinal hemorrhage, cardiac tamponade, pulmonary hemorrhage, and central nervous system bleeds (Table 1) [56, 69].
Separation and Decannulation
ECMO therapy mirrors that of mechanical ventilation in that neither cures a disease process, but rather both stabilize/improve physiological derangements to allow for resolution of a disease process. When the patient’s clinical course while on VV-ECMO has progressed to the point that continued extracorporeal support may not be needed, weaning of ECMO should be pursued. Fairly widely accepted criteria (e.g., Murray Score, RESP Score, or EOLIA criteria) for VV-ECMO initiation/cannulation exist, but there is a comparative paucity of literature to guide VV-ECMO weaning. There are varied methods for VV-ECMO weaning, although not guided by robust trials.
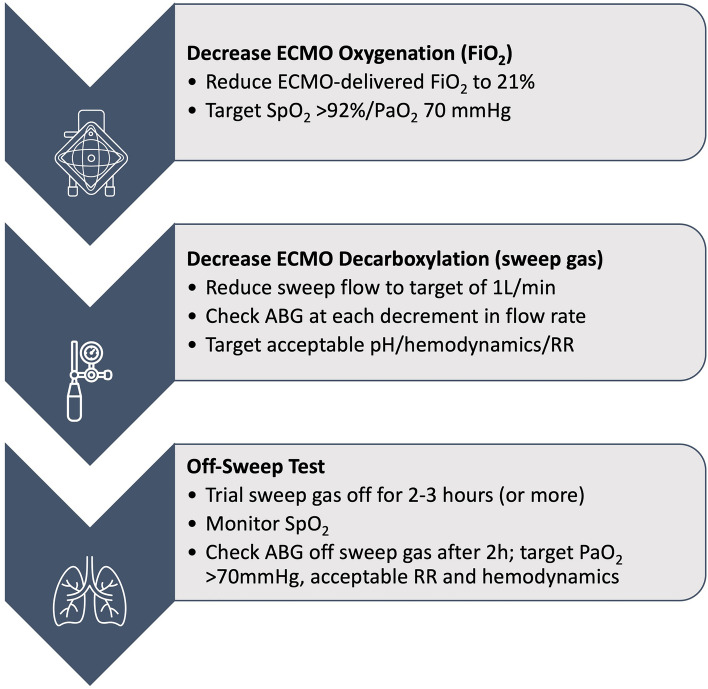
Weaning and Assessment for Separation
Broman et al. describe the weaning strategies among three large VV-ECMO referral centers in Europe; although the particulars of weaning conduct are extremely varied among the three centers, the fundamental concepts are the same, and they serve as a sensible framework for liberation from ECMO support [70]. The ELSO Guideline document from 2021 offers a set of clinical parameters for consideration for weaning intubated patients on VV-ECMO [1]. Weaning is initiated when there is physiologic improvement in respiratory status/reserve, evidence of improvement in the appearance of chest radiographs, and some degree of resolution of the underlying condition. Specifically improved oxygenation such that FiO2 support is ≤ 60%, PEEP ≤ 10 cm H2O, and PaO2 ≥ 70 mmHg, and improved ventilation such that tidal volume ≤ 6 ml/kg predicted body weight, plateau pressure ≤ 28 cm H2O, respiratory rate ≤ 28 bpm, and the pH and PaCO2 are acceptable [1]. Once the patient is deemed ready for VV-ECMO liberation, the ELSO Guidelines again offer a conceptual roadmap to fulfill this effort; our iteration of this treatment algorithm is illustrated in Fig. 6 [1]. Some ECMO centers seek to extubate patients (once able to do so) while on full VV-ECMO support; although portions of their liberation routines differ, the aforementioned fundamental principles remain.
Fig. 6.
A roadmap for weaning from VV-ECMO. ABG arterial blood gas, RR respiratory rate
Technical Aspects of Decannulation
After assurance of the patient’s physiological tolerance for discontinuation of ECMO support, removal of the intravascular cannulae should be pursued. Decannulation of central veins can cause undesirable complications including hemorrhage, air embolism, and insertion site hematoma. Monitoring for complications and clinical decompensation is mandatory. At our institutions, VV-ECMO decannulation is usually performed at bedside. Decannulation typically does not require sedation or analgesic administration, but liberal use of subcutaneous local anesthetic (e.g., lidocaine) prior to placement of purse-string sutures is important. Following an organized routine for decannulation may help prevent errors and set the stage for prompt recognition of potential issues (Table 2).
Table 2.
Recommended ECMO decannulation checklist
| Preparation for decannulation | Decannulation procedure |
Post-decannulation care |
|---|---|---|
|
□ Verify patient’s physiological stability, allowing for ECMO discontinuation □ Hold patient as nil by mouth □ Verify blood products are available (i.e., valid crossmatch, known antibody history, etc.) □ Consider holding systemic anticoagulation & confirmed acceptable coagulation profile □ Have IV sedatives, analgesics, and subcutaneous local anesthetics available □ Have sterile skin prep and drapes, gauze packs, sutures/suture items, and dressings available □ Ensure two providers are available for entirety of procedure (including PPE) □ Verify support team (bedside nurse, perfusionist/ ECMO specialist) is available at bedside for entirety of procedure |
1. Perform time-out and verify planned decannulation procedure 2. Verify patient comfort and clinical stability with position for the procedure (i.e., Trendelenburg for IJ cannula removal) 3. Draping of cannula site is recommended to support cleanliness 4. Local anesthetic should be placed prior to purse-string suture around cannula insertion site 5. One provider should remove cannula quickly while other cinches closed the purse-string, and pressure is applied to the site. If able, positive pressure should be applied via mechanical ventilation, or the patient instructed to perform Valsalva at the time of cannula removal 6. Check removed cannula for any evidence of thrombus burden or soft tissue adherence 7. Site should be dressed with clean dressing after inspection of site for hematoma collection |
□ Verify physiological stability and continue monitoring as per routine ICU care □ Check decannulation sites for hematoma or bleeding at 15 min, 30 min, and then every 1 h for 2 h post-decannulation □ Consider prophylactic pharmacologic anticoagulation, at a minimum □ Venous doppler ultrasound of decannulated vessels on post-decannulation days 1 and 3 |
PPE personal protective equipment
Post-decannulation Surveillance
Deep vein thrombosis and thromboembolism and pulmonary embolism are unfortunately well described in patients who have been decannulated from VV-ECMO support. A recent systematic review of 18 studies reported deep venous thrombosis (DVT) incidence of 53.5% (95% CI 50.0–57.0%) in VV-ECMO patients who underwent surveillance imaging for the period of ECMO therapy initiation to 7 days after decannulation [71]. A separate single-center study of 105 patients who underwent computerized tomography scanning within 4 days of VV-ECMO decannulation found evidence of venous thrombosis in 75 of the 105 patients (71.4%), and pulmonary embolism was diagnosed in 16.2% of studied patients [72]. These data make a compelling case for mandatory imaging surveillance for all decannulated patients; no clear evidence exists that favors a particular imaging modality for thrombus evaluation in this cohort of patients, nor is an optimal imaging interval implied. A high level of suspicion for DVT must be maintained alongside a low threshold for seeking imaging evaluation for DVT or PE in the post-decannulation patient. Creation of an institutional policy for DVT imaging evaluation in the post-decannulation period is recommended.
Anticoagulation after decannulation, akin to anticoagulation during VV-ECMO therapy, requires an individualized approach, considering each patient’s particular clinical profile [73]. At present, there is equipoise regarding which type of anticoagulant is best in patients undergoing ECMO therapy; likewise, there is no clear choice for the optimal anticoagulant in the post-ECMO phase of care. Given the striking incidence of venous thrombosis described above, a bare minimum of prophylactic pharmacological anticoagulation should be employed unless absolute contraindications for such therapy exist.
Bridge to Transplantation
VV-ECMO serves an important role bridging patients with respiratory failure to lung transplantation. Patients with end-stage lung disease who suffer an acute respiratory decompensation face extremely high mortality rates that can be stabilized with ECMO. Note that in the United States’ lung transplant allocation scoring system (the Lung Allocation Score), ECMO therapy is not considered specifically and does not independently increase the likelihood of receiving a lung transplant [74].
A crucial consideration for patients who undergo ECMO cannulation in the pre-lung transplantation period is to move those patients to “awake ECMO”, as there are data describing improved likelihood in surviving to receive a lung transplant and post-transplant patient outcomes in “awake” patients when compared to those who are heavily sedated, bed-bound, and mechanically ventilated prior to transplantation [75]. “Awake ECMO” mandates bare minimum amounts of sedation and maximal participation with physical therapy as able, and the ideal form of “awake ECMO” allows for ambulatory ECMO [76]. Meticulous planning prior to ECMO cannulation of the bridge-to-transplant patient is essential, as the cannulation strategy chosen should consider the patient’s awake ECMO potential.
Future Outlooks
The use of VV-ECMO in patients with severe acute respiratory failure has dramatically increased in recent years. Appropriate candidate selection is critical to successful ECMO utilization ensuring ultimate goals of underlying respiratory pathology recovery or receipt of lung transplantation. Ongoing areas of uncertainty and need for further investigation include earlier application in less severe respiratory failure, ideal anticoagulation management strategies, and post-decannulation surveillance and care.
Acknowledgements
Funding
No funding or sponsorship was received for writing or publication of this article.
Author Contributions
All authors contributed to the article conception and design, drafting, revising, and editing of the manuscript, and read and approved the final manuscript.
Disclosures
PMW has previously served as a consultant for La Jolla Pharmaceutical Company. JPO serves as a consultant for Third Pole Therapeutics and has previously received honoraria from La Jolla Pharmaceutical Company. All other authors have no declarations.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
References
- 1.Tonna JE, Abrams D, Brodie D, Greenwood JC, RUBIO Mateo-Sidron JA, Usman A, et al. Management of Adult Patients Supported with Venovenous Extracorporeal Membrane Oxygenation (VV ECMO): Guideline from the Extracorporeal Life Support Organization (ELSO). ASAIO J. 2021;67:601–10. [DOI] [PMC free article] [PubMed]
- 2.Marhong JD, Munshi L, Detsky M, Telesnicki T, Fan E. Mechanical ventilation during extracorporeal life support (ECLS): a systematic review. Intensive Care Med. 2015;41:994–1003. doi: 10.1007/s00134-015-3716-2. [DOI] [PubMed] [Google Scholar]
- 3.ECMO Registry of the Extracorporeal Life Support Organization (ELSO), Ann Arbor, Michigan 2022.
- 4.Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators, Davies A, Jones D, Bailey M, Beca J, Bellomo R, et al. Extracorporeal Membrane Oxygenation for 2009 Influenza A(H1N1) Acute Respiratory Distress Syndrome. JAMA. 2009;302:1888–95 [DOI] [PubMed]
- 5.Noah MA, Peek GJ, Finney SJ, Griffiths MJ, Harrison DA, Grieve R, et al. Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A(H1N1) JAMA. 2011;306:1659–1668. doi: 10.1001/jama.2011.1471. [DOI] [PubMed] [Google Scholar]
- 6.Alshahrani MS, Sindi A, Alshamsi F, Al-Omari A, El Tahan M, Alahmadi B, et al. Extracorporeal membrane oxygenation for severe Middle East respiratory syndrome coronavirus. Ann Intensive Care. 2018;8:3. doi: 10.1186/s13613-017-0350-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barbaro RP, MacLaren G, Boonstra PS, Iwashyna TJ, Slutsky AS, Fan E, et al. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the extracorporeal life support organization registry. Lancet. 2020;396:1071–1078. doi: 10.1016/S0140-6736(20)32008-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barbaro RP, MacLaren G, Boonstra PS, Combes A, Agerstrand C, Annich G, et al. Extracorporeal membrane oxygenation for COVID-19: evolving outcomes from the international extracorporeal life support organization registry. Lancet. 2021;398:1230–1238. doi: 10.1016/S0140-6736(21)01960-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Broman LM, Holzgraefe B, Palmér K, Frenckner B. The Stockholm experience: interhospital transports on extracorporeal membrane oxygenation. Crit Care. 2015;19:278. doi: 10.1186/s13054-015-0994-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonadonna D, Barac YD, Ranney DN, Rackley CR, Mumma K, Schroder JN, et al. Interhospital ECMO transport: regional focus. Semin Thorac Cardiovasc Surg. 2019;31:327–334. doi: 10.1053/j.semtcvs.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Creel-Bulos C, Miller C, Hassani B, Farthing H, Caridi-Schieble M, Connor MJ, et al. “Pushing Geographic Boundaries: Interfacility transport and remote extracorporeal membrane oxygenation cannulation of patients during COVID-19 pandemic.” Perfusion. 2022; Ahead of print. [DOI] [PMC free article] [PubMed]
- 12.Rabie AA, Azzam MH, Al-Fares AA, Abdelbary A, Mufti HN, Hassan IF, et al. Implementation of new ECMO centers during the COVID-19 pandemic: experience and results from the Middle East and India. Intensive Care Med. 2021;47:887–895. doi: 10.1007/s00134-021-06451-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. The Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 14.Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 15.Goligher EC, Tomlinson G, Hajage D, Wijeysundera DN, Fan E, Jüni P, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc Bayesian analysis of a randomized clinical trial. JAMA. 2018;320:2251. doi: 10.1001/jama.2018.14276. [DOI] [PubMed] [Google Scholar]
- 16.Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, et al. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46:2048–2057. doi: 10.1007/s00134-020-06248-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Munshi L, Walkey A, Goligher E, Pham T, Uleryk EM, Fan E. Venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: a systematic review and meta-analysis. Lancet Respir Med. 2019;7:163–172. doi: 10.1016/S2213-2600(18)30452-1. [DOI] [PubMed] [Google Scholar]
- 18.Sud S, Friedrich JO, Adhikari NKJ, Fan E, Ferguson ND, Guyatt G, et al. Comparative effectiveness of protective ventilation strategies for moderate and severe acute respiratory distress syndrome. A network meta-analysis. Am J Respir Crit Care Med. 2021;203:1366–77. doi: 10.1164/rccm.202008-3039OC. [DOI] [PubMed] [Google Scholar]
- 19.Barrett KA, Hawkins N, Fan E. Economic evaluation of venovenous extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Critical Care Med. 2019;47:186–93. doi: 10.1097/CCM.0000000000003465. [DOI] [PubMed] [Google Scholar]
- 20.The STOP-COVID Investigators, Shaefi S, Brenner SK, Gupta S, O’Gara BP, Krajewski ML, et al. Extracorporeal membrane oxygenation in patients with severe respiratory failure from COVID-19. Intensive Care Med. 2021;47:208–21. [DOI] [PMC free article] [PubMed]
- 21.Hajage D, Combes A, Guervilly C, Lebreton G, Mercat A, Pavot A, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: an emulated target trial analysis. Am J Respir Crit Care Med. 2022;206:281–294. doi: 10.1164/rccm.202111-2495OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Urner M, Barnett AG, Bassi GL, Brodie D, Dalton HJ, Ferguson ND, et al. Venovenous extracorporeal membrane oxygenation in patients with acute COVID-19 associated respiratory failure: comparative effectiveness study. BMJ. 2022;377:e068723. doi: 10.1136/bmj-2021-068723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tran A, Fernando SM, Rochwerg B, Barbaro RP, Hodgson CL, Munshi L, et al. Prognostic factors associated with mortality among patients receiving venovenous extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis. The Lancet Respiratory Medicine. 2022;S221326002200296X. [DOI] [PMC free article] [PubMed]
- 24.Acute Respiratory Distress Syndrome Network. Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 25.Papazian L, Forel J-M, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 26.National Heart, Lung, and Blood Institute PETAL Clinical Trials Network, Moss M, Huang DT, Brower RG, Ferguson ND, Ginde AA, et al. Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome. N Engl J Med. 2019;380:1997–2008. [DOI] [PMC free article] [PubMed]
- 27.Garfield B, McFadyen C, Briar C, Bleakley C, Vlachou A, Baldwin M, et al. Potential for personalised application of inhaled nitric oxide in COVID-19 pneumonia. Br J Anaesth. 2021;126:e72–e75. doi: 10.1016/j.bja.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Menaker J, Tesoriero RB, Tabatabai A, Rabinowitz RP, Cornachione C, Lonergan T, et al. Veno-venous extracorporeal membrane oxygenation (VV ECMO) for acute respiratory failure following injury: outcomes in a high-volume adult trauma center with a dedicated unit for VV ECMO. World J Surg. 2018;42:2398–2403. doi: 10.1007/s00268-018-4480-6. [DOI] [PubMed] [Google Scholar]
- 29.Jacobs JV, Hooft NM, Robinson BR, Todd E, Bremner RM, Petersen SR, et al. The use of extracorporeal membrane oxygenation in blunt thoracic trauma: a study of the Extracorporeal Life Support Organization database. J Trauma Acute Care Surg. 2015;79:1049–53. doi: 10.1097/TA.0000000000000790. [DOI] [PubMed] [Google Scholar]
- 30.Dellgren G, Riise GC, Swärd K, Gilljam M, Rexius H, Liden H, et al. Extracorporeal membrane oxygenation as a bridge to lung transplantation: a long-term study. Eur J Cardiothorac Surg. 2015;47:95–100. doi: 10.1093/ejcts/ezu112. [DOI] [PubMed] [Google Scholar]
- 31.Hakim AH, Ahmad U, McCurry KR, Johnston DR, Pettersson GB, Budev M, et al. Contemporary outcomes of extracorporeal membrane oxygenation used as bridge to lung transplantation. Ann Thorac Surg. 2018;106:192–198. doi: 10.1016/j.athoracsur.2018.02.036. [DOI] [PubMed] [Google Scholar]
- 32.Makdisi G, Wang I-W. Extra corporeal membrane oxygenation (ECMO) review of a lifesaving technology. J Thorac Dis. 2015;7:E166–176. doi: 10.3978/j.issn.2072-1439.2015.07.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yeo HJ, Kim D, Jeon D, Kim YS, Rycus P, Cho WH. Extracorporeal membrane oxygenation for life-threatening asthma refractory to mechanical ventilation: analysis of the extracorporeal life support organization registry. Crit Care. 2017;21:297. doi: 10.1186/s13054-017-1886-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988;138:720–723. doi: 10.1164/ajrccm/138.3.720. [DOI] [PubMed] [Google Scholar]
- 35.Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The respiratory extracorporeal membrane oxygenation survival prediction (RESP) score. Am J Respir Crit Care Med. 2014;189:1374–82. doi: 10.1164/rccm.201311-2023OC. [DOI] [PubMed] [Google Scholar]
- 36.Hilder M, Herbstreit F, Adamzik M, Beiderlinden M, Bürschen M, Peters J, et al. Comparison of mortality prediction models in acute respiratory distress syndrome undergoing extracorporeal membrane oxygenation and development of a novel prediction score: the PREdiction of Survival on ECMO Therapy-Score (PRESET-Score) Crit Care. 2017;21:301. doi: 10.1186/s13054-017-1888-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pappalardo F, Pieri M, Greco T, Patroniti N, Pesenti A, Arcadipane A, et al. Predicting mortality risk in patients undergoing venovenous ECMO for ARDS due to influenza A (H1N1) pneumonia: the ECMOnet score. Intensive Care Med. 2013;39:275–281. doi: 10.1007/s00134-012-2747-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmidt M, Zogheib E, Rozé H, Repesse X, Lebreton G, Luyt C-E, et al. The PRESERVE mortality risk score and analysis of long-term outcomes after extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensive Care Med. 2013;39:1704–1713. doi: 10.1007/s00134-013-3037-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Serpa Neto A, Schmidt M, Azevedo LCP, Bein T, Brochard L, Beutel G, et al. Associations between ventilator settings during extracorporeal membrane oxygenation for refractory hypoxemia and outcome in patients with acute respiratory distress syndrome: a pooled individual patient data analysis: mechanical ventilation during ECMO. Intensive Care Med. 2016;42:1672–1684. doi: 10.1007/s00134-016-4507-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sidebotham D, Allen SJ, McGeorge A, Ibbott N, Willcox T. Venovenous extracorporeal membrane oxygenation in adults: practical aspects of circuits, cannulae, and procedures. J Cardiothorac Vasc Anesth. 2012;26:893–909. doi: 10.1053/j.jvca.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 41.Javidfar J, Wang D, Zwischenberger JB, Costa J, Mongero L, Sonett J, et al. Insertion of bicaval dual lumen extracorporeal membrane oxygenation catheter with image guidance. ASAIO J. 2011;57:203–205. doi: 10.1097/MAT.0b013e3182155fee. [DOI] [PubMed] [Google Scholar]
- 42.Tulman DB, Stawicki SPA, Whitson BA, Gupta SC, Tripathi RS, Firstenberg MS, et al. Veno-venous ECMO: a synopsis of nine key potential challenges, considerations, and controversies. BMC Anesthesiol. 2014;14:65. doi: 10.1186/1471-2253-14-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kucher N, Rossi E, De Rosa M, Goldhaber SZ. Massive pulmonary embolism. Circulation. 2006;113:577–582. doi: 10.1161/CIRCULATIONAHA.105.592592. [DOI] [PubMed] [Google Scholar]
- 44.Grignola JC, Domingo E. Acute right ventricular dysfunction in intensive care unit. Biomed Res Int. 2017;2017:1–15. doi: 10.1155/2017/8217105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ravichandran AK, Baran DA, Stelling K, Cowger JA, Salerno CT. Outcomes with the Tandem Protek Duo Dual-Lumen Percutaneous right ventricular assist device. ASAIO J. 2018;64:570–572. doi: 10.1097/MAT.0000000000000709. [DOI] [PubMed] [Google Scholar]
- 46.Fiore A, de Roux Q, Daami N, Clariot S, Folliguet T, Taccone FS, et al. Clinical feedback from experience with COVID-19: Specific considerations for extracorporeal membrane oxygenation. J Infect. 2020;81:e59–60. doi: 10.1016/j.jinf.2020.06.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tonna JE, Tan CS, Hryniewicz K, Barbaro RP, Brodie D, MacLaren G. Outcomes after extracorporeal life support for COVID-19 myocarditis: an analysis of the extracorporeal life support organization registry. Crit Care. 2022;26:235. doi: 10.1186/s13054-022-04111-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Falk L, Sallisalmi M, Lindholm JA, Lindfors M, Frenckner B, Broomé M, et al. Differential hypoxemia during venoarterial extracorporeal membrane oxygenation. Perfusion. 2019;34:22–29. doi: 10.1177/0267659119830513. [DOI] [PubMed] [Google Scholar]
- 49.Messai E, Bouguerra A, Harmelin G, Di Lascio G, Bonizzoli M, Bonacchi M. A numerical model of blood oxygenation during veno-venous ECMO: analysis of the interplay between blood oxygenation and its delivery parameters. J Clin Monit Comput. 2016;30:327–332. doi: 10.1007/s10877-015-9721-8. [DOI] [PubMed] [Google Scholar]
- 50.Schmidt M, Tachon G, Devilliers C, Muller G, Hekimian G, Bréchot N, et al. Blood oxygenation and decarboxylation determinants during venovenous ECMO for respiratory failure in adults. Intensive Care Med. 2013;39:838–846. doi: 10.1007/s00134-012-2785-8. [DOI] [PubMed] [Google Scholar]
- 51.Schmidt M, Pham T, Arcadipane A, Agerstrand C, Ohshimo S, Pellegrino V, et al. Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome an international multicenter prospective cohort. Am J Respir Crit Care Med. 2019;200:1002–12. doi: 10.1164/rccm.201806-1094OC. [DOI] [PubMed] [Google Scholar]
- 52.Ha MA, Sieg AC. Evaluation of altered drug pharmacokinetics in critically Ill adults receiving extracorporeal membrane oxygenation. Pharmacotherapy. 2017;37:221–235. doi: 10.1002/phar.1882. [DOI] [PubMed] [Google Scholar]
- 53.Shekar K, Fraser JF, Smith MT, Roberts JA. Pharmacokinetic changes in patients receiving extracorporeal membrane oxygenation. J Crit Care. 2012;27:741.e9–741.e18. doi: 10.1016/j.jcrc.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 54.Dalton HJ, Garcia-Filion P, Holubkov R, Moler FW, Shanley T, Heidemann S, et al. Association of bleeding and thrombosis with outcome in extracorporeal life support. Pediatric Critical Care Med. 2015;16:167–74. doi: 10.1097/PCC.0000000000000317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thomas J, Kostousov V, Teruya J. Bleeding and thrombotic complications in the use of extracorporeal membrane oxygenation. Semin Thromb Hemost. 2018;44:020–29. doi: 10.1055/s-0037-1606179. [DOI] [PubMed] [Google Scholar]
- 56.Brokmeier HM, Wieruszewski ED, Nei SD, Loftsgard TO, Wieruszewski PM. Hemostatic management in extracorporeal membrane oxygenation. Crit Care Nurs Q. 2022;45:132–143. doi: 10.1097/CNQ.0000000000000396. [DOI] [PubMed] [Google Scholar]
- 57.Pollak U, Yacobobich J, Tamary H, Dagan O, Manor-Shulman O. Heparin-induced thrombocytopenia and extracorporeal membrane oxygenation: a case report and review of the literature. J Extra Corpor Technol. 2011;43:5–12. [PMC free article] [PubMed] [Google Scholar]
- 58.Burstein B, Wieruszewski PM, Zhao Y-J, Smischney N. Anticoagulation with direct thrombin inhibitors during extracorporeal membrane oxygenation. WJCCM. 2019;8:87–98. doi: 10.5492/wjccm.v8.i6.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bates SM, Weitz JI. The mechanism of action of thrombin inhibitors. J Invasive Cardiol. 2000;12:27F–32. [PubMed]
- 60.Hamzah M, Jarden AM, Ezetendu C, Stewart R. Evaluation of bivalirudin as an alternative to heparin for systemic anticoagulation in pediatric extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2020;21:827–834. doi: 10.1097/PCC.0000000000002384. [DOI] [PubMed] [Google Scholar]
- 61.Ranucci M, Ballotta A, Kandil H, Isgrò G, Carlucci C, Baryshnikova E, et al. Bivalirudin-based versus conventional heparin anticoagulation for postcardiotomy extracorporeal membrane oxygenation. Crit Care. 2011;15:R275. doi: 10.1186/cc10556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sanfilippo F, Asmussen S, Maybauer DM, Santonocito C, Fraser JF, Erdoes G, et al. Bivalirudin for alternative anticoagulation in extracorporeal membrane oxygenation: a systematic review. J Intensive Care Med. 2017;32:312–319. doi: 10.1177/0885066616656333. [DOI] [PubMed] [Google Scholar]
- 63.Seelhammer TG, Bohman JK, Schulte PJ, Hanson AC, Aganga DO. Comparison of bivalirudin versus heparin for maintenance systemic anticoagulation during adult and pediatric extracorporeal membrane oxygenation. Crit Care Med. 2021;49:1481–1492. doi: 10.1097/CCM.0000000000005033. [DOI] [PubMed] [Google Scholar]
- 64.Wieruszewski PM, Macielak SA, Nei SD, Moman RN, Seelhammer TG, Nabzdyk CGS, et al. Heparin versus bivalirudin for anticoagulation in adult extracorporeal membrane oxygenation: a systematic review and meta-analysis. ASAIO J. 2022; Publish Online Ahead of Print. [DOI] [PubMed]
- 65.Nei SD, Wieruszewski PM, Wittwer ED. Aggressive antithrombin supplementation often not necessary during extracorporeal membrane oxygenation. Anesthesia Analgesia. 2020;130:e153–4 [DOI] [PubMed]
- 66.Seelhammer TG, Hamzah M, Wieruszewski P. Antithrombin replacement and extracorporeal membrane oxygenation: the time is ripe for a simpler solution. ASAIO J. 2022;68:e166–e167. doi: 10.1097/MAT.0000000000001704. [DOI] [PubMed] [Google Scholar]
- 67.Zhang M, Pauls JP, Bartnikowski N, Haymet AB, Chan CHH, Suen JY, et al. Anti-thrombogenic surface coatings for extracorporeal membrane oxygenation: a narrative review. ACS Biomater Sci Eng. 2021;7:4402–4419. doi: 10.1021/acsbiomaterials.1c00758. [DOI] [PubMed] [Google Scholar]
- 68.Olson SR, Murphree CR, Zonies D, Meyer AD, Mccarty OJT, Deloughery TG, et al. Thrombosis and bleeding in extracorporeal membrane oxygenation (ECMO) without anticoagulation: a systematic review. ASAIO J. 2021;67:290–296. doi: 10.1097/MAT.0000000000001230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Murphy DA, Hockings LE, Andrews RK, Aubron C, Gardiner EE, Pellegrino VA, et al. Extracorporeal membrane oxygenation—hemostatic complications. Transfus Med Rev. 2015;29:90–101. doi: 10.1016/j.tmrv.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 70.Broman LM, Malfertheiner MV, Montisci A, Pappalardo F. Weaning from veno-venous extracorporeal membrane oxygenation: how I do it. J Thorac Dis. 2018;10:S692–S697. doi: 10.21037/jtd.2017.09.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Iannattone PA, Yang SS, Koolian M, Wong EG, Lipes J. Incidence of venous thromboembolism in adults receiving extracorporeal membrane oxygenation: a systematic review. ASAIO J. [Internet]. 2022 [cited 2022 Nov 20]; Publish Ahead of Print. Available from: https://journals.lww.com/10.1097/MAT.0000000000001694 [DOI] [PubMed]
- 72.Parzy G, Daviet F, Persico N, Rambaud R, Scemama U, Adda M, et al. Prevalence and risk factors for thrombotic complications following venovenous extracorporeal membrane oxygenation: a CT scan study. Crit Care Med. 2020;48:192–199. doi: 10.1097/CCM.0000000000004129. [DOI] [PubMed] [Google Scholar]
- 73.McMichael ABV, Ryerson LM, Ratano D, Fan E, Faraoni D, Annich GM. 2021 ELSO adult and pediatric anticoagulation guidelines. ASAIO J. 2022;68:303–310. doi: 10.1097/MAT.0000000000001652. [DOI] [PubMed] [Google Scholar]
- 74.Furfaro D, Rosenzweig EB, Shah L, Robbins H, Anderson M, Kim H, et al. Lung transplantation disparities based on diagnosis for patients bridging to transplant on extracorporeal membrane oxygenation. J Heart Lung Transplant. 2021;40:1641–1648. doi: 10.1016/j.healun.2021.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tipograf Y, Salna M, Minko E, Grogan EL, Agerstrand C, Sonett J, et al. Outcomes of extracorporeal membrane oxygenation as a bridge to lung transplantation. Ann Thorac Surg. 2019;107:1456–1463. doi: 10.1016/j.athoracsur.2019.01.032. [DOI] [PubMed] [Google Scholar]
- 76.Loor G, Chatterjee S, Shafii A. Extracorporeal membrane oxygenation support before lung transplant: a bridge over troubled water. JTCVS Open. 2021;8:147–154. doi: 10.1016/j.xjon.2021.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]