Abstract
Purpose
This study aimed to systematically evaluate the clinical, functional, and radiological outcomes, complications, and rate of return to sports among patients with RAMP lesion of the medial meniscus encountered during anterior cruciate ligament (ACL) reconstruction.
Methods
A systematic review was conducted based on the PRISMA guidelines. Two independent reviewers searched the PubMed, Scopus, Embase, and Cochrane Library databases using the terms “ACL” or “anterior cruciate ligament,” and “RAMP lesion.” The outcome measures extracted from the studies were the Short Form-12 (SF-12) in its mental and physical component (MCS and PCS), Lysholm score, Subjective IKDC, Marx Score, WOMAC Score, Tegner, Radiological changes, complications, failures and/or revision surgery, and rate of return to sports.
Results
The cohort of patients consisted of 1,243 participants with a mean age of 28.6 ± 2.6. The mean postoperative follow-up was 40.9 ± 6.3 months. A total of 1145 (92.1%) RAMP lesions were repaired with concomitant ACL reconstruction, while only 98 (7.9%) lesions were left untreated (or treated with abrasion only). The Lysholm score was used in 6 studies (in one only at final follow-up), with a significant improvement in all the studies (Lysholmpre 60.03 ± 6.12; Lysholmpost 89.9 ± 5.0). Eight studies out of nine reported Subjective IKDC score, and a significant improvement was noted in all cases (IKDCpre 56.2 ± 5.8. IKDCpost 84.9 ± 3.7). Of 18 (1.4%) complications reported, 15 (1.2%) were related to RAMP/ACL surgery, and of the remaining three (0.2%) two (0.2%) were hematomas and one (0.1%) a contralateral ACL lesion. Of the 106 (8.5%) revision surgeries required, 5 (0.4%) were in non-treated lesions [two (0.2%) ACL re-ruptures and three (0.2%) medial meniscus re-injury]. In treated patients, the revision occurred for the following reasons: 75 (6.0%) meniscectomy, 14 (1.1%) meniscal suture revisions, 11 (0.9%) ACL failures and one (0.1%) arthrolysis.
Conclusions
It is not yet clear if, in all cases of ACL reconstruction in which a medial meniscal RAMP lesion is encountered, the lesion needs to undergo surgical repair. Accordingly, it is recommended that in the repair of all unstable medial meniscal RAMP lesions during an ACL reconstruction in cases associated with a stable RAMP lesion, the surgeon may decide on repair based on the patient profile.
Level of evidence
Level IV.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00167-022-07067-3.
Keywords: RAMP lesion, Medial meniscus injury, ACL reconstruction, Meniscal repair, Meniscectomy, Posterior horn
Introduction
RAMP lesions are identified as a specific type of injury involving the peripheral attachment of the posterior horn of the medial meniscus, and more precisely they are caused by a peripheral vertical longitudinal detachment of the posterior horn of the medial meniscus due to tears of the meniscocapsular ligament, leading to meniscocapsular or meniscotibial separation [4, 7, 14, 27].
RAMP lesions are increasingly gaining attention in the orthopaedic field, especially due to their association with an anterior cruciate ligament (ACL) injury [7], with a significantly variable prevalence in concomitant ACL injury [5]. Their importance also lies in the fact that this injury is associated with increased anterior translation of the tibia, dynamic rotational laxity, and excessive rotational mobility of the knee [19, 20]. For these reasons, despite being found in a vascularized area, currently the recommended treatment appears to suggest surgical repair [2, 6, 8], even if a possible spontaneous healing has also been reported [17].
To clarify the treatment of RAMP lesions, several classifications have been proposed that divide them into subtypes [12, 21, 25]. It is also important to pay attention to possible risk factors, recently identified, such as bone contusion on the posterior medial tibial plateau, chronic injury, steeper tibial and medial meniscal slope, gradual lateral tibial slope, and varus knee alignment > 3° [16].
Despite the recent increased awareness, RAMP injuries remain significantly underdiagnosed, for instance due to the use of the classic anterior arthroscopic portal, which limits the complete visualization of the posterior horn of the medial meniscus and its meniscocapsular junction, and therefore the visualization of RAMP lesions or the presence of a membrane-like tissue that might hide the aforementioned lesions, their being made visible only after a certain degree of debridement through a posteromedial portal [23].
Moreover, there is low RAMP injury detection on preoperative magnetic resonance imaging (MRI). It may be useful to look for indirect signs such as a bruise of the posteromedial tibial bone that has been found to be a secondary sign of a RAMP injury [6, 9].
Undoubtedly, this topic deserves greater attention to clarify the diagnostic–therapeutic algorithm in the face of these complexly managed lesions.
This study aimed to systematically evaluate the clinical, functional, and radiological outcomes, complications, and rate of return to sports among patients with RAMP lesion of the medial meniscus encountered during anterior cruciate ligament (ACL) reconstruction.
Materials and methods
The current systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and is registered in the PROSPERO Registry (CRD42022335486) [18].
Eligibility criteria
The literature selected for this study was based on the following criteria.
Study design
Randomized controlled trials (RCTs), controlled (non-randomized) clinical trials (CCTs), prospective and retrospective comparative cohort studies, case–control studies, and case series were included. Case reports and case series that did not report data on clinical and functional results were excluded.
Participants
Studies conducted on skeletally mature patients treated for RAMP lesion of the medial meniscus in association with anterior cruciate ligament (ACL) reconstruction. and were evaluated through a minimum follow-up of 1 year were considered eligible.
Interventions
Studies that reported data on clinical, functional, and radiological outcomes following the ACL reconstruction associated with RAMP lesion of the medial meniscus, independently if treated surgically or conservatively.
For ACL reconstruction the surgical technique (type of graft used, numbers of bundles, fixation technique, and tensioning protocol), and rehabilitation protocol were collected as well as approach and surgical technique for meniscal RAMP repair.
Types of outcome measures
The outcome measures extracted from the studies were the Short Form-12 (SF-12) in its mental and physical component (MCS and PCS), Lysholm score, Subjective IKDC, Marx Score, WOMAC Score, Tegner, radiological changes, complications, failures and/or revision surgery, and rate of return to sports.
RAMP lesions were classified according to the current literature as follows:
Thaunat et al. [25] approached the tear pattern, direction, thickness (partial vs. full), and associated meniscocapsular disruption, peripheral zone, or meniscotibial ligament lesion and instability (Type 1: meniscocapsular tear; Type 2: partial superior tear; Type 3: partial inferior tear; Type 4: complete tear; Type 5: double tear)
Greif et al. [12] in an extended Thaunat classification version integrate the recent knowledge from cadaveric studies showing that meniscocapsular and meniscotibial ligaments merge in their posterior horn meniscal attachment (Type 1: meniscocapsular ligament tear; Type 2: partial superior peripheral posterior meniscal horn tear; Type 3A: partial inferior peripheral posterior horn meniscal tear; Type 3B: meniscotibial ligament tear; Type 4A: complete peripheral posterior horn meniscal tear; Type 4B: complete meniscocapsular junction tear; Type 5: peripheral posterior horn meniscal double tear)
Seil et al. [21] approached the mediolateral extent of tears, degree of capsular attachment injury, and adherent (self-heal) vs. dehiscent (repair).
Information sources and search
A systematic search for relevant literature was performed on the PubMed (MEDLINE), Scopus, EMBASE, and Cochrane Library databases. The publication date was not considered an inclusion criterion. The search was carried out in April 2022. Two independent reviewers (RD and AM) assisted in conducting and validating the search. The following search terms were entered in the title, abstract, and keywords fields: “ACL” or “anterior cruciate ligament,” and “RAMP lesion.” Lastly, only papers published in English were included.
Data collection and analysis
Study selection
The retrieved articles were first screened by title and, if found relevant, screened further by reading the abstract. After excluding studies not meeting the eligibility criteria, the entire content of the remaining articles was evaluated for eligibility. To minimize the risk of bias, the authors reviewed and discussed all the selected articles, references, as well as the articles excluded from the study. In case of any disagreement between the reviewers, the senior investigator made the final decision. At the end of the process, further studies that might have been missed were manually searched by going through the reference lists of the included studies and relevant systematic reviews.
Data collection process
The data was extracted from the selected articles by the first two authors using a computerized tool created with Microsoft Access (Version 2010, Microsoft Corp, Redmond Washington). Every article was validated again by the first author before analysis. For each study, data regarding the patients was extracted (age, gender, duration between injury and surgery, and follow-up evaluation), their injuries (type, aetiology, and associated injuries), the surgical technique (type of graft used, numbers of bundles, fixation technique, and tensioning protocol), rehabilitation protocol, post-operative outcomes, rate of complications, and the rate of return to sports.
Level of evidence
The Oxford Levels of Evidence set by the Oxford Centre for Evidence-Based Medicine was used to categorize the level of evidence [11].
Evaluation of the quality of studies
The quality of the selected studies was evaluated using the Methodological Index for Nonrandomized Studies (MINORS) score [22]. The checklist includes 12 items, of which the last four are specific to comparative studies. Each item was given a score of 0–2 points. The ideal score was set at 16 points for non-comparative studies and 24 for comparative studies.
Results
Search results
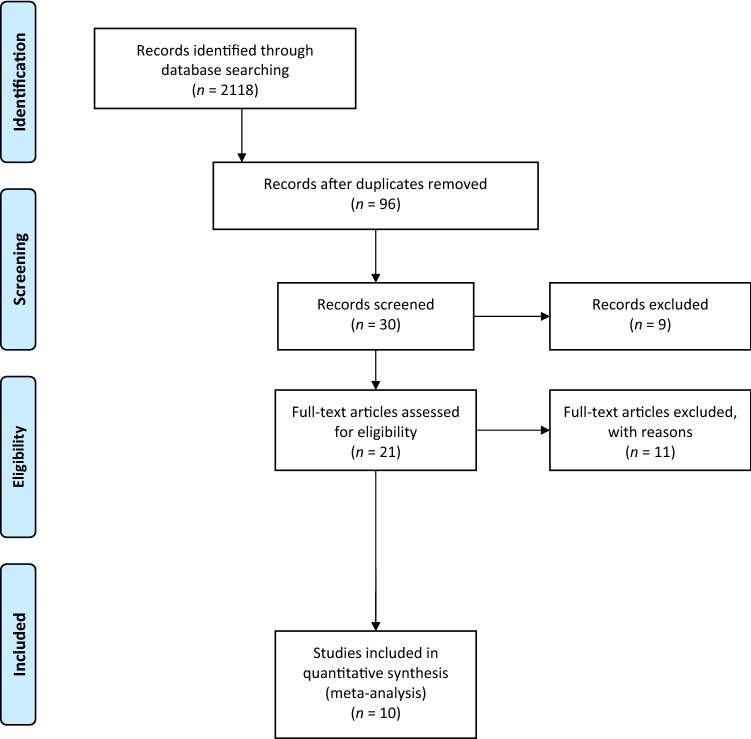
The electronic search yielded 2118 studies. After 2022 duplicates were removed, 96 studies remained, of which 66 were excluded after reviewing the abstracts, bringing the number down to 30. An additional 20 articles were excluded based on the aforementioned inclusion and exclusion criteria. No additional studies were found by manually searching the reference lists of the selected articles. This left 10 studies for analysis [1, 3, 8, 10, 13, 15, 17, 24, 26, 28]. Figure 1 shows the flowchart depicting the selection process for studies. The analyzed studies had a mean MINORS score of 12.9 (range, 9–18), which confirmed the methodological quality of the available literature (Table 1).
Fig. 1.
A flowchart of the literature screening performed in this study
Table 1.
Characteristics of the selected studies
| Authors, Year | MINORS | Level of Evidence | Patients (n) | M: F (n) | Age Mean ± SD (range) | Time between injury and surgery | FU | Ramp lesion classification | Aetiology/ mechanism of injury (n) | Associated injuries (n) |
|---|---|---|---|---|---|---|---|---|---|---|
| Albayrak 2020 [1] | 9 | III | 33 | 32:1 | 28.3 ± 7.8 | 15.8 weeks | 47.3 ± 9.4 months | Type 1 | 25 contact injury 8 non-contact | n.a |
| Balzas 2020 [3] | 11 | III | 67 | 36:31 | 28.4 | n.a | 1–5 years | 36 Stable 31 unstable | 23 contact 44 non-contact | n.a |
| Chen 2017 [8] | 12 | IV | 46 | 34:12 | 26 (18–41) | n.a | 32 (14–36) months | 18 Meniscotibial ligament tear (MLT) 13 meniscocapsular tear (MCT), 15 combined MLT/MCT | n.a | n.a |
| DePhilippo 2020 [10] | 18 | III | 50 | 22:28 | 30.5 ± 11.4 |
31 acute 19 chronic |
2.8 (2–8) years | n.a | n.a | n.a |
| Hatayama 2020 [13] | 18 | III |
50 25 non repaired 25 repaired |
Non repaired: 13:12 Repaired: 17:8 |
Non repaired: 29.5 Repaired: 26.6 |
Non repaired: 680 days Repaired: 494 |
24 months |
25 Stable 25 Unstable |
n.a | n.a |
| Liu 2017 [17] | 18 | II |
73 40 repaired 33 abraded and trephined |
n.a |
Repaired: 35.6 ± 8.5 Abraded and trephined: 34.8 ± 9.1 |
Repaired: 9.4 ± 12.1 Abraded and trephined: 8.3 ± 10.5 |
Repaired: 37.9. ± 15.9 Abraded and trephined: 40.3 ± 16.5 |
n.a | n.a | n.a |
| Sonnery-Cottet 2018 [24] | 9 | IV | 416 | n.a | n.a | n.a | 45.6 (24–2 – 66.2) months | n.a | n.a | n.a |
| Thaunat 2022 [26] | 11 | III | 248 | 174:74 | 29.5 ± 9.5 |
107 < 3 months 141 > 3 months |
46.4 ± 9.6 months (31–72) |
Type 1 129 Type 2 13 Type 3 27 Type 4 64 Type 5 15 |
n.a | n.a |
| Thaunat 2016 [28] | 11 | IV | 132 | 110:22 | 26.4 (12–57) | n.a | 27 (24–29) | n.a | n.a | 45 lateral meniscal tear |
| Keyhani 2016 [15] | 12 | IV | 128 | 107:21 | 24 (18–48) | n.a | 24 (24–47) | n.a | n.a | n.a |
n.a. not available; FU follow-up; MINORS Methodological Index for Non-Randomized Studies
Patient and study characteristics
Table 1 shows the characteristics of the cohorts involved in the 10 selected studies and a summary of their data. The cohort of patients consisted of 1,243 participants (545 (43.8%) men and 209 (16.8%) women – 2 studies did not report ratio M:F [17, 24]) with a mean age of 28.6 ± 2.6 (range 12–57). The mean postoperative follow-up was 40.9 ± 6.2 months (range, 14–72 months). Five studies [1, 3, 8, 13, 26] reported RAMP classification and were divided as follows: 162 (13.0%) type 1, 13 (1.0%) type 2, 27 (2.2%) type 3, 64 (5.1%) type 4, 15 (1.2%) type 5, 61 (4.9%) stable, 56 (4.5%) unstable, 18 (1.44%) meniscotibial ligament tear (MLT), 13 (1.0%) meniscocapsular tear (MCT), 15 (1.2%) combined MLT/MCT.
Origin
Only 2 studies [1, 3] reported type of injuries, and in 48 (3.9%) cases there was a sports contact injury while 52 (4.2%) cases had a non-sports contact injury.
Surgical protocol
ACL
All data in terms of the surgical technique followed in each of the examined studies are displayed in “Appendix”. All studies reported the type of graft used, except two [3, 15]. Only in one study was the use of a double bundle technique reported [13].
RAMP
Repaired
All studies except one [1] reported RAMP lesion repair with different techniques as reported in “Appendix”, for a total of 1145 (92.1%) lesions.
Unrepaired
In one study [1] only were all RAMP lesions not treated, while in the study of Balzas et al. [3] 32 (2.6%) stable RAMP lesions were not treated and in the study of Liu et al. [17] 33 (2.6%) RAMP lesions were treated with abrasion and trephination for a total of 98 (7.9%) lesions.
Rehabilitation protocol
Only three studies reported the use of postoperative brace [1, 8, 17]; partial weight bearing was granted from day 0 in 2 studies [10, 24], while in remaining studies it ranged from 2nd to 4th week post the operation. For range of motion all studies reported different protocol ranging from early range of motion after discharge to complete full extension for 4 weeks post-operative.
Clinical and functional outcomes
Two studies reported clinical evaluation using SF-12, and Balzas et al. [3] found no difference among different treatments. Alabaryak et al. [1] noted significant improvement between pre- and post-operative PCS and MCS SF-12 (MCSpre 53.0 ± 1.35; MCSpost: 55.8 ± 2.9; PCSpre 43.8 ± 3.3 PCSpost 54.2 ± 0.6) [1, 3].
Lysholm score was used in 6 studies (in one only at final follow-up), with a significant improvement reported in all the papers (Lysholmpre 60.0 ± 6.1; Lysholmpost 89.9 ± 5.0) [1, 8, 10, 13, 15, 17].
Eight studies out of ten reported Subjective IKDC score, and in all cases a significant improvement was noted (IKDCpre 56.2 ± 5.8. IKDCpost 84.9 ± 3.7) [1, 3, 8, 10, 15, 17, 26, 28].
Marx score was used only by Balzas et al., with no differences between the different treatment groups (p > 0.05) [3]; WOMAC score was reported only by DePhilippo, with a significant improvement (p < 0.05) [10], whereas Tegner was reported in three studies (of which one only was post-operative), with contrasting results (Tegnerpre 5.8 ± 2.3; Tegnerpost: 7.0 ± 0.5) [10, 13, 28].
Post-operative changing
At second look arthroscopy, Chen et al. noted complete healing in 40 (3.2%) cases, incomplete healing in 5 (0.4%), and in 1 (0.08%) failure after repair using the FastFix System [8].
Hatayama et al. reported complete healing in 10 (0.8%) cases, partial healing in five (0.4%), and 10 (0.8%) unhealed non-repaired lesions, while in repaired lesions 20 (1.6%) healed and 5 (0.4%) partially healed were noted on MRI [13].
In his randomized clinical trial, Liu et al. observed 38 (3.1%) healed, one (0.1%) partially healed, and one (0.1%) non-healed in sutured lesions, while the abrasion group reported 29 (2.3%) healed, two (0.2%) partially healed, and two (0.2%) non-healed [17].
Thaunat et al. reported 12 (1.0%) non-healed on post-operative MRI [28].
Detailed results are reported in Table 2.
Table 2.
Clinical and functional outcomes, complications, and return to sports and activity
| Lead Author | SF-12 MCS | SF-12 PCS | Lysholm | Subjective IKDC | Marx | Womac total | Tegner | Changing | Complications | Failures/Revisions | Return to sport | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |||||
| Albayrak 2020 [1] | 53.6 ± 2.6 | 58.5 ± 2.4* | 41.7 ± 2.7 | 54.8 ± 2.6* | 54.1 ± 6.5 | 86.0 ± 6.4* | 44.4 ± 7.8 | 77.4 ± 9.2* |
4: 1 Movement limitations 1 acl tear in opposite knee 2 pain related to the implants |
0 |
28 Patients returned to sports: 3 lower level 25 same level |
|||||||
| Balzas 2020 [3] |
Stable untreated: 51.3 (9.4) Unstable ramp— partial meniscectomy: 52.8 (6.7) Unstable ramp— Repaired: 53.6 (9.2) |
Stable untreated: 51.7 (8.6) Unstable ramp— partial meniscectomy: 57.8 (3.4) Unstable ramp— Repaired: 55.9 (3.2) |
Stable untreated: 41.8 (7.3) Unstable ramp— partial meniscectomy: 49.8 (8.3) Unstable ramp— Repaired: 43.9 (9.5) |
Stable untreated: 54.3 (4.5) Unstable ramp— partial meniscectomy: 53.1 (7.2) Unstable ramp— Repaired: 54.2 (6.1) |
Stable untreated: 49.5 (15.5) Unstable ramp— partial meniscectomy 64.0 (10.4) Unstable ramp— Repaired: 50.7 (12.8) |
Stable untreated: 85.6 (10.8) Unstable ramp— partial meniscectomy: 87.7 (13.1) Unstable ramp— Repaired: 80.6 (17.2) |
Stable untreated: 12.8 (4.2) Unstable ramp— partial meniscectomy: 9.0 (5.2) Unstable ramp— Repaired: 11.9 (5.8) |
Stable untreated: 9.3 (5.0) Unstable ramp— partial meniscectomy: 8.3 (4.2) Unstable ramp— Repaired: 9.3 (5.7) |
Stable untreated: 2 ACL re-rupture 1 medial meniscus re-injury Unstable ramp— partial meniscectomy: 1 medial meniscus re-injury Unstable ramp— Repaired: 2 ACL re-rupture 5 medial meniscus re-injury |
|||||||||
| Chen 2017 [8] | 56.81 (37–70) | 94.44 (90–99)* | 52.74 (28–66) | 90.59 (80–98)* |
Second Look Arthroscopy: 40 complete healing 5 incomplete healing 1 failed |
2 mild articular cartilage of MFC 1 implant displaced |
5 partial meniscectomy revision 1 repeated repair revision 3 rasp refresh revision 1 ACL revsion |
|||||||||||
| DePhilippo 2020 [10] | 53 [31, 69] | 86 [80, 95]* | 66 [62, 72] | 78 [72, 80]* | 28 [17, 52] | 0 [0, 8]* | 2 [1, 3] | 8 [6, 9]* |
1 cyclops lesion 1 ORIF patellar fracture 2 arthrofibrosis 1 MCL injury |
1 medial meniscus revision repair 1 partial meniscectomy revision |
84% returned to their preinjury activity | |||||||
| Hatayama 2020 [13] |
Non repaired: 98.5 Repaired: 98.7 |
Non repaired: 6.0 Repaired: 6.8 |
MRI: non repaired 10 completely healed 5 partially healed 10 unhealed Repaired 20 completely healed 5 partially healed |
Non repaired: 2 subsequent meniscecomy |
||||||||||||||
| Liu 2017 [17] |
Sutured: 68.6 ± 6.1 abrasion: 64.3 ± 7.5 |
Sutured: 88.7 ± 4.8* Abrasion: 90.4 ± 5.8* |
Sutured: 51.1 ± 5.5 Abrasion: 53.6 ± 6.7 |
Sutured: 83.6 ± 3.7* Abrasion: 82.2 ± 4.5* |
MRI: Sutured: Completely healed 38 Partially healed 1 Nonhealed 1 Abrasion: Completely healed 29 Partially healed 2 Nonhealed 2 |
|||||||||||||
| Sonnery-Cottet 2018 [24] | 45 partial meniscectomy | |||||||||||||||||
| Thaunat 2022 [26] | 56 ± 12 | 88 ± 10* |
15 meniscectomy 3 sutures 8 acl failures 4 cyclops syndrome 1 arthrolysis |
|||||||||||||||
| Thaunat 2016 [28] | 63.8 ± 13.5 | 85.7 ± 12* | 7.2 ± 1.92 | 6.9 ± 1.72 | MRI. 12 unhealed | 2 hematoma | 9 meniscal revision | 82% of patients returned to their premorbidity activity | ||||||||||
| Keyhani 2016 [15] | 61.7 ± 3.2 | 87.8 ± 3.9* | 53.6 ± 2.1 | 82.1 ± 3.5* | 3 meniscectomy | |||||||||||||
SF-12 Short Form-12; MCS Mental component; PCS Physical component; IKDC The international knee documentation committee; WOMAC Western Ontario and McMaster university; MRI Magnetic resonance imaging
Statistically significant versus pre-operative score (p < 0.05)
Return to sports
Only three studies analyzed return to sports, and in all these studies more than 80% of the patients returned to their pre-injury activity [1, 10, 28].
Complications and revisions surgery
Of 18 (1.4%) complications reported, 15 (1.2%) were related to RAMP/ACL surgery (one (0.1%) had movement limitations and two (0.2%) were due to arthrofibrosis, in two (0.2%) pain related to the implants, one (0.1%) had implant displacement, five (0.4%) had cyclops lesion, one (0.1%) a patellar fracture, one (0.1%) MCL injury, two (0.2%) MFC cartilage lesion), and of the remaining three (0.2%) two (0.2%) were hematomas and one (0.1%) a contralateral ACL lesion.
Of the 106 (8.5%) revision surgeries required, 5 (0.4%) were in non-treated lesions (two (0.2%) ACL re-ruptures and three (0.2%) medial meniscus re-injury). In treated patients the revision occurred for the following reasons: 75 (6.0%) meniscectomy, 14 (1.1%) meniscal suture revisions, 11 (0.9%) ACL failures, one (0.1%) arthrolysis. Detailed results are reported in Table 2.
Discussion
The most important findings of this analysis were that the most commonly reported outcome score in the studies included in the study, the subjective IKDC score, showed significant functional improvement for all the treatment methods used for RAMP lesion repair along with ACL reconstruction, while the second most commonly reported outcome score in the included studies, the Lysholm score, also showed significant functional improvement in all the studies it was reported in.
The Tegner activity score, which was reported in three of the included studies, showed improvement, although this was not statistically significant. Therefore, there is clinically significant functional improvement in knees where ACL reconstruction was performed along with RAMP lesion repair.
In the study by Albayrak et al., non-treatment of stable unrepaired RAMP lesions with ACL reconstruction did not show lower functional knee scores than isolated ACL reconstructions [1],
whereas the study by Balzas et al. showed no significant difference in outcomes between non-repaired medial meniscal root lesions and those repaired with ACL reconstruction surgery [3].
Three studies had analyzed return to sports activity at a preinjury level, namely the studies by Dephilippo et al., Albayrak et al., and Thaunat et al. [1, 10, 28]. The study by Thaunat et al. [28] found an 82% rate of return to preinjury level of activity. Moreover, the study by Albayrak et al. [1] reported no significant differences in return to sports rates between isolated ACL reconstruction and ACL reconstruction with a non-repaired stable RAMP lesion, while that of Dephilippo et al. [10] found no significant differences between patients who underwent ACL reconstruction with a meniscal RAMP repair and patients of isolated ACL reconstruction, in return to sports activity. Further, the study by Balzas et al. [3] found no significant differences between ACL reconstructions with concomitant non-repaired stable RAMP lesions and those with a repaired unstable RAMP lesion. Therefore, one may suggest that despite the presence of a RAMP lesion, repairing these lesions may not be necessary while undertaking a concomitant ACL reconstruction, if the RAMP lesion is found to be stable intraoperatively, at least in most patients. However, returning to sports at the same activity level took a significantly longer period for the group with RAMP lesions than for those with isolated ACL reconstructions, in the study by Albayrak et al. [1]. As such, it may be worthwhile, in high demand populations such as professional sportspersons, to repair a stable RAMP lesion, which may ensure earlier return to preinjury levels of sports activity participation. The unstable meniscal RAMP lesion needs to be repaired for healing of the lesion and subsequent good knee function.
Healing of RAMP lesions was not significantly different with respect to repair and abrasion-trephination, as reported by Liu et al. [17]. The healing rate of RAMP lesions was significantly higher in the repaired group compared with unrepaired lesions on postoperative MRI in the study by Hatayama et al. [13], who reported good healing rates (87%). Hence, surgical repair of RAMP lesions appears to ensure good rates of healing. A low rate of complications was found upon review of all the studies. The rate of failure and overall rate of revision repair was also low in the articles reviewed. The included studies showed a low rate of conversion to partial meniscectomy due to failure and reinjury.
To the best of our knowledge, this is the first systematic review in terms of ACL reconstruction with concomitant RAMP lesions of the posterior horn of the medial meniscus. However, by the very nature of a systematic review, the collection of data is limited to the studies available in the literature and what those studies report. Limitations of the current systematic review are a lack of studies with higher level of evidence in the literature, with only a few studies having been done on ACL reconstruction with a concomitant RAMP lesion, the fact that there is only one prospective randomized controlled study, the heterogenous nature of the techniques used to treat the RAMP lesion, and non-uniform reporting of outcome scores across the studies.
Conclusion
With the currently available data, it is not yet clear if all cases of ACL reconstruction in which a medial meniscal RAMP lesion is encountered should undergo repair of the lesion. With that said, repair of RAMP lesion appears to hasten the return to sporting activity, without much impact on the overall rate of return to sports. Accordingly, we recommend the repair of all unstable medial meniscal RAMP lesions during an ACL reconstruction, while in cases associated with a stable RAMP lesion the surgeon may decide on repair based on the patient profile. Randomized prospective studies with greater size of study populations will need to be undertaken in order to make more concrete recommendations regarding the management of ACL injury with associated RAMP lesions.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
This study was supported and funded by the Italian Ministry of Health - “Ricerca Corrente”.
Appendix
See Table 3 below.
Table 3.
Surgical and rehabilitation protocols
| Lead Author | Graft type | Fixation technique | Surgical technique | Ramp lesion treatment | Bundle | Tension protocol | Rehabilitation protocol | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Femur | Tibia | Brace/Splint | Full weight-bearing | ROM time | ||||||
| Albayrak 2020 [1] | Four-strand hamstring | n.a | n.a | n.a | Untreated | Single bundle | n.a | Hinged knee brace for 4 weeks | 4 weeks | 90º was not allowed until the end of the third week |
| Balzas 2020 [3] | n.a | n.a | n.a | n.a | 32 stable—untreated 23 unstable ramp repaired with all inside technique 12 unstable ramp—meniscectomy | n.a | n.a | n.a | n.a | n.a |
| Chen 2017 [8] | Hamstring | Bioresorbable IS + staples | Endobutton | n.a | Repaired using FastFix System | Single Bundle | n.a | Hinged brace | 6 weeks | 0 to 90 degrees at 4 weeks |
| DePhilippo 2020 [10] | BTPB | Cannulated titanium IS | Cannulated titanium IS | Anatomic | Inside-out suture | Single Bundle | Full extension | No | Weight as tolerated upon discharge | 24 h after surgery initiate early range of motion |
| Hatayama 2020 [13] | Semitendinosus tendon | Endobutton | 2 staples | Anatomic | All-inside by posteromedial portal | Double bundle | 15° | No | 3 weeks | 1 week after surgery |
| Liu 2017 [17] | Four-strand hamstring | n.a | n.a | n.a | 40: From posteromedial portal with suture hook 33: abrasion and trephination without surgical repair | Single bundle | n.a | Hinged Brace | Partial weightbearing at 2 weeks; full weightbearing at 4 weeks | Full extension for 4 weeks |
| Sonnery-Cottet 2018 [24] | Quadrupled semitendinosus tendons, bone–patellar tendon–bone,1quadrupled hamstring tendons, or in the case of combined ACL–anterolateral ligament grafts, a tripled semitendinosus with a single strand of gracilis | n.a | n.a | n.a | From posteromedial portal with suture hook | n.a | n.a | no | Weightbearing as tolerated from day 0 | 0–90° for the first 4 weeks |
| Thaunat 2022 [26] | 16 BPTB 232 Hamstring + ALLR | n.a | n.a | n.a | 38 All-inside device 184 suture hook repair 16 all-inside + suture hook 10 missing data | n.a | n.a | n.a | n.a | n.a |
| Thaunat 2016 [28] | 89 hamstring 41 BPTB 2 quadriceps | n.a | n.a | n.a | All-inside posterior Lasso sutures; all-inside fast-fix; out-in | n.a | n.a | no | From week 3 | 0–90° for 6 weeks |
| Keyhani 2016 [15] | n.a | n.a | n.a | Anatomic | Posteromedial portal with suture hook | n.a | n.a | no | Toe-touch weight for 2 weeks, partial weight-bearing 2–4 weeks |
Passive 0–45° for 2 weeks 0–90° 2–4 weeks |
BPTPB Bone-patellar tendon-bone; ALLR Anterolateral ligament reconstruction; IFS Interference screw; ROM Range of motion
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. There is no funding source.
Declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Not needed.
Consent to publish
All authors consent to the publication of the manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Riccardo D’Ambrosi, Email: riccardo.dambrosi@hotmail.it.
Amit Meena, Email: dr.meenaamit1624@gmail.com.
Akshya Raj, Email: raj.ackshai@gmail.com.
Riccardo Giorgino, Email: riccardo.giorgino@unimi.it.
Nicola Ursino, Email: nicolaursino@libero.it.
Laura Mangiavini, Email: laura.mangiavini@unimi.it.
Jon Karlsson, Email: jon.kssta@gmail.com.
References
- 1.Albayrak K, Buyukkuscu MO, Kurk MB, Kaya O, Kulduk A, Misir A. Leaving the stable ramp lesion unrepaired does not negatively affect clinical and functional outcomes as well as return to sports rates after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2021;29:3773–3781. doi: 10.1007/s00167-020-06402-w. [DOI] [PubMed] [Google Scholar]
- 2.Alessio-Mazzola M, Lovisolo S, Capello AG, Zanirato A, Chiarlone F, Formica M, Felli L. Management of ramp lesions of the knee: a systematic review of the literature. Musculoskelet Surg. 2020;104:125–133. doi: 10.1007/s12306-019-00624-z. [DOI] [PubMed] [Google Scholar]
- 3.Balazs GC, Greditzer HG, 4th, Wang D, Marom N, Potter HG, Marx RG, Rodeo SA, Williams RJ., 3rd Ramp lesions of the medial meniscus in patients undergoing primary and revision ACL reconstruction: prevalence and risk factors. Orthop J Sports Med. 2019;7:2325967119843509. doi: 10.1177/2325967119843509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balazs GC, Greditzer HG, 4th, Wang D, Marom N, Potter HG, Rodeo SA, Marx RG, Williams RJ., 3rd Non-treatment of s ramp lesions does not degrade clinical outcomes in the setting of primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28:3576–3586. doi: 10.1007/s00167-020-06017-1. [DOI] [PubMed] [Google Scholar]
- 5.Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med. 2013;41:1801–1807. doi: 10.1177/0363546513490649. [DOI] [PubMed] [Google Scholar]
- 6.Bumberger A, Koller U, Hofbauer M, Tiefenboeck TM, Hajdu S, Windhager R, Waldstein W. Ramp lesions are frequently missed in ACL-deficient knees and should be repaired in case of instability. Knee Surg Sports Traumatol Arthrosc. 2020;28:840–854. doi: 10.1007/s00167-019-05521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chahla J, Dean CS, Moatshe G, Mitchell JJ, Cram TR, Yacuzzi C, LaPrade RF. Meniscal ramp lesions: anatomy, incidence, diagnosis, and treatment. Orthop J Sports. 2016;4:2325967116657815. doi: 10.1177/2325967116657815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Z, Li WP, Yang R, Song B, Jiang C, Hou JY, Luo H, Zhou YF. Meniscal ramp lesion repair using the fast-fix technique: evaluating healing and patient outcomes with second-look arthroscopy. J Knee Surg. 2018;31:710–715. doi: 10.1055/s-0037-1606378. [DOI] [PubMed] [Google Scholar]
- 9.DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:2233–2237. doi: 10.1177/0363546517704426. [DOI] [PubMed] [Google Scholar]
- 10.DePhillipo NN, Dornan GJ, Dekker TJ, Aman ZS, Engebretsen L, LaPrade RF. Clinical characteristics and outcomes after primary ACL reconstruction and meniscus ramp repair. Orthop J Sports Med. 2020;8:2325967120912427. doi: 10.1177/2325967120912427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DiSilvestro KJ, Tjoumakaris FP, Maltenfort MG, Spindler KP, Freedman KB. Systematic reviews in sports medicine. Am J Sports Med. 2016;44:533–538. doi: 10.1177/0363546515580290. [DOI] [PubMed] [Google Scholar]
- 12.Greif DN, Baraga MG, Rizzo MG, Mohile NV, Silva FD, Fox T, Jose J. MRI appearance of the different meniscal ramp lesion types, with clinical and arthroscopic correlation. Skeletal Radiol. 2020;49:677–689. doi: 10.1007/s00256-020-03381-4. [DOI] [PubMed] [Google Scholar]
- 13.Hatayama K, Terauchi M, Saito K, Takase R, Higuchi H. Healing status of meniscal ramp lesion affects anterior knee stability after ACL reconstruction. Orthop J Sports. 2020;8:2325967120917674. doi: 10.1177/2325967120917674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang J, Ni L, Chen J. Isolated meniscal ramp lesion without obvious anterior cruciate ligament rupture. Orthop Surg. 2021;13:402–407. doi: 10.1111/os.12860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keyhani S, Ahn JH, Verdonk R, Soleymanha M, Abbasian M. Arthroscopic all-inside ramp lesion repair using the posterolateral transseptal portal view. Knee Surg Sports Traumatol Arthrosc. 2017;25:454–458. doi: 10.1007/s00167-016-4410-9. [DOI] [PubMed] [Google Scholar]
- 16.Kim SH, Seo HJ, Seo DW, Kim KI, Lee SH. Analysis of risk factors for ramp lesions associated with anterior cruciate ligament injury. Am J Sports Med. 2020;48:1673–1681. doi: 10.1177/0363546520918207. [DOI] [PubMed] [Google Scholar]
- 17.Liu X, Zhang H, Feng H, Hong L, Wang XS, Song GY. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? a prospective randomized controlled trial. Am J Sports Med. 2017;45:1004–1011. doi: 10.1177/0363546516682493. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA; PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mouton C, Magosch A, Pape D, Hoffmann A, Nührenbörger C, Seil R. Ramp lesions of the medial meniscus are associated with a higher grade of dynamic rotatory laxity in ACL-injured patients in comparison to patients with an isolated injury. Knee Surg Sports Traumatol Arthrosc. 2020;28:1023–1028. doi: 10.1007/s00167-019-05579-z. [DOI] [PubMed] [Google Scholar]
- 20.Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23:2967–2973. doi: 10.1007/s00167-015-3751-0. [DOI] [PubMed] [Google Scholar]
- 21.Seil R, Hoffmann A, Scheffler S, Theisen D, Mouton C, Pape D. Rampenläsionen : tipps und tricks in diagnostik und therapie [ramp lesions : tips and tricks in diagnostics and therapy] Orthopade. 2017;46:846–854. doi: 10.1007/s00132-017-3461-z. [DOI] [PubMed] [Google Scholar]
- 22.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 23.Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921–926. doi: 10.1177/0363546514522394. [DOI] [PubMed] [Google Scholar]
- 24.Sonnery-Cottet B, Praz C, Rosenstiel N, Blakeney WG, Ouanezar H, Kandhari V, Vieira TD, Saithna A. Epidemiological evaluation of meniscal ramp lesions in 3214 anterior cruciate ligament-injured knees from the SANTI Study Group database: a risk factor analysis and study of secondary meniscectomy rates following 769 ramp repairs. Am J Sports Med. 2018;46:3189–3197. doi: 10.1177/0363546518800717. [DOI] [PubMed] [Google Scholar]
- 25.Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5:e871–e875. doi: 10.1016/j.eats.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thaunat M, Foissey C, Ingale P, Haidar I, Bauwens PH, Penet A, Kacem S, Fayard JM. Survival and risk factor analysis of arthroscopic ramp lesion repair during anterior cruciate ligament reconstruction. Am J Sports Med. 2022;50:637–644. doi: 10.1177/03635465211068524. [DOI] [PubMed] [Google Scholar]
- 27.Thaunat M, Ingale P, Penet A, Kacem S, Haidar I, Bauwens PH, Fayard JM. Ramp lesion subtypes: prevalence, imaging, and arthroscopic findings in 2156 anterior cruciate ligament reconstructions. Am J Sports Med. 2021;49:1813–1821. doi: 10.1177/03635465211006103. [DOI] [PubMed] [Google Scholar]
- 28.Thaunat M, Jan N, Fayard JM, Kajetanek C, Murphy CG, Pupim B, Gardon R, Sonnery-Cottet B. Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: outcome study with a minimum 2-year follow-up. Arthroscopy. 2016;32:2269–2277. doi: 10.1016/j.arthro.2016.02.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.