Abstract
Omalizumab, a recombinant anti-immunoglobulin E (IgE) monoclonal antibody, is indicated for moderate to severe allergic asthma, chronic spontaneous urticaria, and nasal polyps, and is approved for self-administration. However, specific guidance on identifying candidates with characteristics suitable for this type of administration is lacking. To help address this issue, this article provides practical considerations for the health care provider treating patients with omalizumab. We encourage health care providers to consider self-administration of omalizumab as an option for all appropriate, but not all, patients, and we recommend an individualized approach when considering self-administration of omalizumab.
Keywords: Allergic asthma, Chronic spontaneous urticaria, Nasal polyps, Omalizumab, Self-administration
Key Summary Points
| Omalizumab is approved for self-administration; however, guidance to identify suitable patients is lacking. |
| We provide practical considerations for the health care provider treating patients with omalizumab. |
| Considerations include ability of patient/caregiver to identity and treat anaphylaxis, patient empowerment, personal attributes, comorbid conditions, and potential impact of quality of life. |
| Shared decision-making between the health care provider and the patient is essential. |
Omalizumab, a recombinant anti-immunoglobulin E (IgE) monoclonal antibody, is indicated for moderate to severe allergic asthma, chronic spontaneous urticaria, and nasal polyps [1]. Self-administration of omalizumab by appropriate patients was approved by the European Medicines Agency in 2018 and by the US Food and Drug Administration in 2021. Although the omalizumab prescribing information includes criteria for selection of patients for self-administration using prefilled syringes, these criteria lack specific guidance on identifying candidates with characteristics suitable for this type of administration. For reference, the prescribing information for omalizumab in the USA includes the following criteria for selection of patients for self-administration using pre-filled syringes [1]: consider known risk factors for anaphylaxis (a black box warning highlights that selection of patients for self-administration should be based on criteria to mitigate risk from anaphylaxis) and consider patient-specific factors including (i) no prior history of anaphylaxis to Xolair or other agents, such as foods, drugs, biologics etc., (ii) patient should receive at least three doses of Xolair under the guidance of a health care provider with no hypersensitivity reactions, (iii) patient or caregiver is able to recognize symptoms of anaphylaxis, (iv) patient or caregiver is able to treat anaphylaxis appropriately, (v) patient or caregiver is able to perform subcutaneous injections with Xolair pre-filled syringes with proper technique according to the prescribed dosing regimen and instructions for use.
This lack of guidance for identifying candidates is an important note because self-administration of omalizumab will not be suitable for all patients. Further, health care providers treating patients with omalizumab, particularly in the USA, lack experience with self-administration. To help address this issue, this article provides practical considerations for the health care provider treating patients with omalizumab. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. Although we advocate for shared decision-making, the health care provider is responsible for evaluating treatment options that will ensure the highest likelihood of successful disease management. This decision at the point of care is individualized for each patient and this article aims to support the providers and encourage due diligence for consideration of self-administration.
Self-administration of biologics is an established therapeutic option for various chronic dermatologic, rheumatologic, immunologic, neurologic, gastrointestinal, and endocrine condition, and this experience provides a wealth of information that is relevant to omalizumab. Examples include rheumatoid arthritis [2], primary immunodeficiency [2], multiple sclerosis [2], diabetes [3], ulcerative colitis [4], Crohn’s disease [5], psoriasis [6], atopic dermatitis [7], fertility treatment [8], and growth hormone deficiency [9]. Self-administration of biologics was recently reviewed by Lombardi et al. [10] for patients with severe asthma; on the basis of their extensive experience in Europe, the authors suggested that for correct use of self-administration procedures it would be essential to identify the appropriate patient. In addition, a literature review and expert opinion of the self-administration of omalizumab was recently published by Menzella et al. [11]; although this paper included considerations for selection of suitable patients, we provide the additional perspective of in-clinic and advocate experience.
Self-administration of omalizumab is preferred by most patients and physicians because of the beneficial impact on daily life [12]. Self-administration could have psychological quality of life benefits, such as patient empowerment, and this is an important aspect that warrants further consideration by health care providers. A systematic review discussed the association between patient empowerment and positive health behaviors and clinical outcomes, including disease management, use of health services, health status, and medication adherence [13]. The authors suggested that the association was based on the theory that patient autonomy, or sense of freedom, is beneficial for health [13]. However, because self-administration of omalizumab will not be suitable for all patients, additional factors are pertinent.
For patients being treated with omalizumab, there are many patient characteristics that could be considered by the health care provider to identify candidates for self-administration.
Personal attributes: Health care providers should try to understand the patient and be aware of the patient’s home situation so that they can take into consideration different personal aspects that are unique for each individual. Attributes may include historical adherence to visits and treatment; patient medical history; patient preference, expectations, beliefs, and attitudes; patient medical literacy; patient relationship with health care provider; patient and caregiver comfort with needles; demographic, socioeconomic, and social support factors; language barriers; and self-care behaviors. Many of these attributes have been identified from studies of patients with chronic conditions who routinely self-administer their medication and some pertinent examples are presented here. For patients using home self-administration of intravenous antibiotics, a patient interview study found that key to success was to ensure that the patients felt knowledgeable, skillful, and competent, and the main reason that patients chose not to self-administer was anxiety [14]. For patients who self-administered methotrexate for inflammatory arthritis, one of the key reasons patients felt empowered was the support they received from health care providers [15]. For patients who self-administered medication for multiple sclerosis, there was a higher likelihood of adherence for patients were older or male [16]. Although these studies provide some guidance, the holistic personal attributes of each individual patient should be considered by the health care provider, as some factors may not be as relevant to all patients.
Comorbid conditions: Comorbidities may be a limiting factor in determining whether the patient is suitable for self-administration of omalizumab; for example, cognitive function may affect the ability to understand and follow instructions; conditions that affect dexterity and vision may impact the ability to inject; and complex medication regimens may impact adherence. In addition, psychiatric conditions may not only increase the likelihood of self-administration anxiety but also decrease adherence to self-administration treatment because patients may lack motivation or become overwhelmed. For example, Munsell et al. [16] found that the presence of depression was associated with lower likelihood of adherence to self-injected medication in patients with multiple sclerosis.
Potential impact on quality of life: We recommend that health care providers consider whether self-administration of omalizumab would benefit the individual patient and their quality of life. Examples of factors, identified from studies that investigated patient-reported outcomes, that are important to patients include reduced travel time (particularly for those with a long distance to travel to specialty clinics, or who are reliant on public transport), increased flexibility (especially with regard to employment), and impact on daily life including convenience [12, 17–19]. Further, self-administration of omalizumab reduced both direct and indirect costs to the patient compared with in-clinic administration [20].
The final decision regarding self-administration of omalizumab rests with the clinical judgment of the health care provider; however, shared decision-making between the health care provider and the patient is essential. Shared decision-making for asthma and allergy treatment has been reviewed extensively, including by Bukstein et al. [21], and is supported by decision-making aids and education information, particularly from societies (e.g., https://acaai.org/resources/interactive-tools/http://severeasthmatreatments.chestnet.org/). Factors such as using decision aids together, ensuring the patient feels confident, and the health care provider presenting themselves as reliable, balanced, and empathetic can lead to optimal care decisions that have long-term consequences for the patient, including the development of self-efficacy [21]. For omalizumab self-administration, discussion of risks may highlight the possibility of anaphylaxis, the decreased interaction with the health care provider, and the burden on the patient to be (i) adherent to administration technique and timing, (ii) have the ability to recognize signs of anaphylaxis and other adverse events, and (iii) treat an anaphylaxis event if needed.
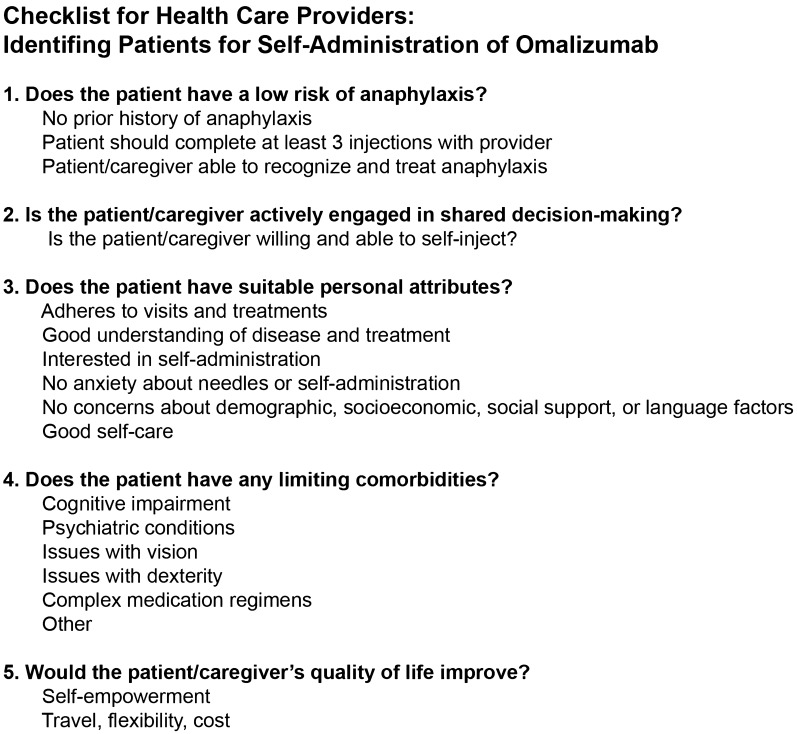
In summary, we encourage health care providers to consider self-administration of omalizumab as an option for all appropriate, but not all, patients. Although our guidance may serve only as a timely reminder to health care providers, highlighting the considerations for identifying candidates for self-administration of omalizumab may assist providers who are unfamiliar with self-administration (especially as patient self-advocacy is on the increase), and we have provided a practical checklist (Fig. 1). If self-administration is selected, a follow-up plan for consistent assessment of disease status and evaluation of patient experience with self-administration is essential. We recommend an individualized approach when considering self-administration of omalizumab, an approach that considers the unique characteristics of each patient and ultimately results in shared decision-making between the patient and the health care provider, regardless of whether the patient has allergic asthma, chronic spontaneous urticaria, or nasal polyps.
Fig. 1.
A practical checklist highlighting the considerations for identifying candidates for self-administration of omalizumab
Acknowledgements
Funding
The journal Rapid Service and Open Access Fees were funded by Genentech, Inc., a member of the Roche Group. Medical writing assistance was funded by Genentech, Inc., a member of the Roche Group.
Medical Writing and/or Editorial Assistance
Medical writing assistance was provided by Janelle Keys, PhD, CMPP, of Envision Pharma Group.
Author Contributions
Kevin Murphy, Tonya Winders, Brandy Smith, Lauren Millette, and Bradley E. Chipps contributed to the manuscript concept and drafting, review, and approval of the manuscript.
List of Investigators
Not applicable to this commentary article.
Prior Presentation
Not applicable to this commentary article.
Disclosures
Dr Murphy is a consultant for AstraZeneca, Genentech, GlaxoSmithKline, Novartis, Regeneron, and Sanofi Genzyme, and part of a speaker’s bureau for Amgen, AstraZeneca, Genentech, Novartis, Regeneron, and Sanofi Genzyme. Ms Winders is a consultant for AstraZeneca, GlaxoSmithKline, Novartis, Regeneron, Sanofi Genzyme, and Teva, and part of a speaker’s bureau for AstraZeneca, Novartis, Regeneron, Sanofi Genzyme, and Teva. B Smith and Dr Millette are employees of Genentech, Inc. and stockholders in Roche. Dr Chipps serves as a consultant for AstraZeneca, Boehringer Ingelheim, Genentech, GlaxoSmithKline, Novartis, Regeneron, and Sanofi Genzyme, and serves as part of a speaker’s bureau for AstraZeneca, Genentech, Novartis, Regeneron, and Sanofi Genzyme.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors
Footnotes
The original online version of this article was revised due to update in text.
Change history
11/18/2022
A Correction to this paper has been published: 10.1007/s12325-022-02373-1
Contributor Information
Kevin R. Murphy, Email: Kevin.Murphy@boystown.org
Tonya Winders, Email: twinders@allergyasthmanetwork.org.
Brandy Smith, Email: smithb62@gene.com.
Lauren Millette, Email: millette.lauren@gene.com.
Bradley E. Chipps, Email: bchipps@capitalallergy.com
References
- 1.Xolair Prescribing Information. South San Francisco, California: Genentech, Inc. 2021.
- 2.Bittner B, Richter W, Schmidt J. Subcutaneous administration of biotherapeutics: an overview of current challenges and opportunities. BioDrugs. 2018;32:425–440. doi: 10.1007/s40259-018-0295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thurman JE. Analysis of insulin pen devices for the treatment of diabetes mellitus. J Diabetes Sci Technol. 2008;2:482–483. doi: 10.1177/193229680800200319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sparrow MP. Adalimumab in ulcerative colitis-efficacy, safety and optimization in the era of treat-to target. Expert Opin Biol Ther. 2017;17:613–621. doi: 10.1080/14712598.2017.1309390. [DOI] [PubMed] [Google Scholar]
- 5.Schiff M, Saunderson S, Mountian I, Hartley P. Chronic disease and self-injection: ethnographic investigations into the patient experience during treatment. Rheumatol Ther. 2017;4:445–463. doi: 10.1007/s40744-017-0080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Callis Duffin K, Bagel J, Bukhalo M, et al. Phase 3, open-label, randomized study of the pharmacokinetics, efficacy and safety of ixekizumab following subcutaneous administration using a prefilled syringe or an autoinjector in patients with moderate-to-severe plaque psoriasis (UNCOVER-A) J Eur Acad Dermatol Venereol. 2017;31:107–113. doi: 10.1111/jdv.13768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ito M, Kamata M, Uchida H, et al. Introduction of self-injection increases compliance with dupilumab administration in adult patients with atopic dermatitis: a single-center retrospective study. JAAD Int. 2020;1:91–92. doi: 10.1016/j.jdin.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Platteau P, Laurent E, Albano C, et al. An open, randomized single-centre study to compare the efficacy and convenience of follitropin beta administered by a pen device with follitropin alpha administered by a conventional syringe in women undergoing ovarian stimulation for IVF/ICSI. Hum Reprod. 2003;18:1200–1204. doi: 10.1093/humrep/deg234. [DOI] [PubMed] [Google Scholar]
- 9.Rohrer TR, Horikawa R, Kappelgaard AM. Growth hormone delivery devices: current features and potential for enhanced treatment adherence. Expert Opin Drug Deliv. 2017;14:1253–1264. doi: 10.1080/17425247.2017.1243526. [DOI] [PubMed] [Google Scholar]
- 10.Lombardi C, Bagnasco D, Passalacqua G. Biological agents for severe asthma: the evolution of the at-home self-injection approach. Curr Opin Allergy Clin Immunol. 2020;20:421–427. doi: 10.1097/ACI.0000000000000656. [DOI] [PubMed] [Google Scholar]
- 11.Menzella F, Ferrari E, Ferrucci SM, et al. Self-administration of omalizumab: why not? A literature review and expert opinion. Expert Opin Biol Ther. 2021;21:499–507. doi: 10.1080/14712598.2021.1882990. [DOI] [PubMed] [Google Scholar]
- 12.Timmermann H, Mailänder C. Home self-administration of biologics: a German survey among omalizumab-treated oatients with severe asthma and their treating physicians. Pneumologie. 2020;74:103–111. doi: 10.1055/a-1069-0900. [DOI] [PubMed] [Google Scholar]
- 13.Náfrádi L, Nakamoto K, Schulz PJ. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS ONE. 2017;12:e0186458. doi: 10.1371/journal.pone.0186458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tonna A, Anthony G, Tonna I, et al. Home self-administration of intravenous antibiotics as part of an outpatient parenteral antibiotic therapy service: a qualitative study of the perspectives of patients who do not self-administer. BMJ Open. 2019;9:e027475. doi: 10.1136/bmjopen-2018-027475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hiley J, Homer D, Clifford C. Patient self-injection of methotrexate for inflammatory arthritis: a study evaluating the introduction of a new type of syringe and exploring patients' sense of empowerment. Musculoskelet Care. 2008;6:15–30. doi: 10.1002/msc.114. [DOI] [PubMed] [Google Scholar]
- 16.Munsell M, Frean M, Menzin J, Phillips AL. An evaluation of adherence in patients with multiple sclerosis newly initiating treatment with a self-injectable or an oral disease-modifying drug. Patient Prefer Adher. 2017;11:55–62. doi: 10.2147/PPA.S118107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Denman S, Ford K, Toolan J, et al. Home self-administration of omalizumab for chronic spontaneous urticaria. Br J Dermatol. 2016;175:1405–1407. doi: 10.1111/bjd.15074. [DOI] [PubMed] [Google Scholar]
- 18.Ghazanfar M, Holm J, Thomsen SF. Effectiveness of omalizumab in chronic spontaneous urticaria assessed with patient-reported outcomes: a prospective study. J Eur Acad Dermatol Venereol. 2018;32:1761–1767. doi: 10.1111/jdv.15045. [DOI] [PubMed] [Google Scholar]
- 19.Greenhawt M, Shaker M. Keeping risk in context while rethinking the setting of asthma biologics in patient-centered care. Ann Allergy Asthma Immunol. 2020;125:124–125. doi: 10.1016/j.anai.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shaker M, Briggs A, Dbouk A, Dutille E, Oppenheimer J, Greenhawt M. Estimation of health and economic benefits of clinic versus home administration of omalizumab and mepolizumab. J Allergy Clin Immunol. 2020;8:565–572. doi: 10.1016/j.jaip.2019.09.037. [DOI] [PubMed] [Google Scholar]
- 21.Bukstein DA, Guerra DG, Jr, Huwe T, Davis RA. A review of shared decision-making: a call to arms for health care professionals. Ann Allergy Asthma Immunol. 2020;125:273–279. doi: 10.1016/j.anai.2020.06.030. [DOI] [PubMed] [Google Scholar]