Abstract
Left distal transradial artery (dTRA) access in the anatomical snuffbox is a relatively novel technique and is considered beneficial when left TRA access is required. This technique offers essential advantages, including improved patient comfort and lower vascular complications. dTRA may provide an entry site for retrograde recanalization of the radial artery. We presented a case of a 65-year-old man with 5-stage chronic kidney disease (CKD) and had left a radio-cephalic arteriovenous fistula (AVF) for routine hemodialysis. There was obstruction of AVF a month after creation. The vascular intervention has been performed using left dTRA access for retrograde recanalization. Angiogram showed cephalic vein obstruction and non-significant stenosis of the proximal radial artery. Percutaneous transluminal angioplasty was successful in improving cephalic vein flow. Hemostatic performed without a hemostatic device. This case report highlights the dTRA access approach in the anatomical snuffbox to recanalize AVF occlusion in the wrist in a patient with CKD.
Keywords: Distal radial artery, Snuffbox, Arteriovenous fistula, Dialysis
Introduction
The radial artery has been accepted as vascular access for both diagnostic and interventional angiographic purposes. The use of transradial access in interventional procedures was initiated by Lucian Canpeau, who performed coronary angiography through the left radial artery. By 1992, Ferdinand Kiemeneiji began using transradial artery for percutaneous coronary intervention (PCI) [1]. Transradial access is favored over transfemoral access in various countries, and 20% of intervention procedures are estimated to use transradial access. Countries with the highest proportion of transradial access procedures (70%-80%) are Norway, Malaysia, and Bulgaria [2].
Anatomical snuffbox is the newest method that has been developed for intervention through distal radial artery access [3]. This small triangular area is often used to perform clinical procedures, such as cephalic vein cannulation and surgical procedures as arteriovenous fistula [4]. Iatrogenic occlusion is better tolerated with distal transradial access [5]. We report a case of intervention of an arteriovenous fistula occlusion in the left wrist via the left distal transradial access to the anatomical snuffbox.
Case report
A 65-year-old man came to the cardiovascular center at Dr. Soetomo Surabaya with a chief complaint of clogged dialysis access. The patient's first dialysis was performed about 3 months ago. The current dialysis routine was scheduled twice a week, every Tuesday and Friday. The patient underwent dialysis access (AV shunt) placement on the left wrist about 1 month ago. Dialysis was performed 3 times through the installed access, but it stopped working correctly due to clogged access. The patient had a history of hypertension and diabetes mellitus for more than 10 years and kidney disease in 3 months.
From the physical examination, the patient was fully conscious of the moderate general condition. The patient was found to have a blood pressure of 170/80 mmHg, a pulse rate of 84 bpm, a respiratory rate of 18 breaths/min, and 98% room air oxygen saturation. Head and neck examination revealed pale conjunctiva. The chest and heart are within normal limits. In the extremities, there was pitting edema of both hands and feet (Fig. 1).
Fig. 1.
Clinical picture of the patient. The arrows indicate where the AV shunt is attached for hemodialysis access.
Laboratory results showed hemoglobin 7.5 g/dL, leukocytes 8.860/mm3, platelets 272,000/mm3, sodium 139 mmol/L, potassium 4.1 mmol/L, chloride 98 mmol/L, random blood sugar as 161 mg/dL, SGOT 27 U/L, SGPT 29 U/L, albumin 3.4 g/dL, BUN 34 mg/dL, and serum creatinine as 8.46 mg/dL. ECG showed a sinus rhythm of 75 bpm with first-degree AV block, normal axis, low voltage QRS in the limb leads, poor R-wave progression in leads V1-V4. Chest X-ray showed less inspiration and cardiomegaly impression. The upper limb artery's ultrasound results showed obstruction in the AV fistula in the left forearm, interstitial edema in the forearm, and the size of the left forearm's and arm's cephalic vein was 2.9 mm and 1.6 mm, respectively.
Our patient was diagnosed with ESRD on regular HD + AV fistula obstruction + Hypertension grade II ESC 2018. For medical treatment, we prescribed Candesartan 1 × 8 mg and Amlodipine 1 × 10 mg. For AV fistula obstruction, transradial access through the left hand's anatomical snuffbox was performed (Fig. 2). After determining the location of the puncture, local anesthesia was done using lidocaine 2% subcutaneously. Puncture is performed. The sheath is gently inserted into the radial artery. A cocktail injection of 3000 IU UFH, 300 µg nitroglycerin, and 20 mg lidocaine 2% is slowly injected through the access sheath. During the procedure, the administration of antispasms and anticoagulants did not differ from the standard transradial access.
Fig. 2.
Transradial access to the anatomy of the snuffbox.
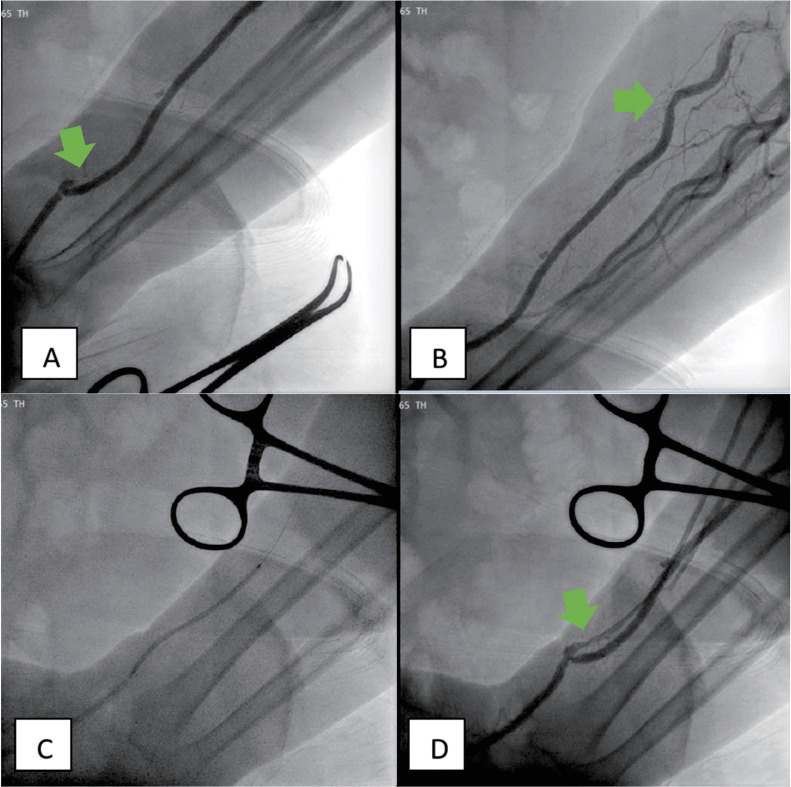
Angiography showed total occlusion in the left cephalic vein and 40% nonsignificant stenosis proximal to the left radial artery (Fig. 3A). Angioplasty was performed using a Coyote Balloon of 2.5 × 60 mm, dilated at 8 atm/3 minutes 3 times. Postballooning evaluations revealed flow in the cephalic vein (Fig. 3B).
Fig. 3.
Diagnostic angiography results show total occlusion in the left cephalic vein (arrow, panel A) and 40% nonsignificant stenosis in the proximal left radial artery (arrow, panel B). The Coyote Balloon size 2.5 × 60 mm was dilated 8 atm for 3 minutes (panel C). Postballooning result obtained flow in the cephalic vein (arrows, panel D).
After the procedure, hemostasis was performed by pressing the puncture area with 2 fingers for 30 minutes, ensuring no active bleeding. Later on, we performed a direct pressure using elastic tape onto the palm and dorsal side of the hand, allowing the fingers to move freely. The dressing was removed the next day. The evaluation showed no hematoma in the puncture site, and good saturation of the fingers was obtained. The patient was given an enoxaparin injection of 2.5 mg once daily for 3 days for postintervention advice.
Discussion
The anatomical snuffbox is a triangular deepening on the radial side of the wrist. Its border formed between the tendons of the extensor pollicis brevis and abductor pollicis longus laterally and the tendon of the extensor pollicis longus medially. The styloid process of the radius forms the proximal border, and the base consists of the scaphoid bone. The distal radial artery lies deep to the snuffbox across the scaphoid bone from the ventral to the dorsal hand. The distal radial artery is approximately 80% of the artery's size in the forearm, about 2.5 mm. The snuffbox's identification is made by positioning the patient's thumb in abduction and extension to activate the tendon extensor pollicis longus and abductor pollicis longus [4,6]. The radial artery bifurcates before entering the snuffbox, anastomose with ulnar artery to form the superficial palmar branch. The distal portion of the radial artery continues through the snuffbox dorsally to supply the deep palmar arch. The main feature of the radial artery's distal segment is its location distal to the superficial palmar branch of the radial artery [7].
Several considerations might indicate the choice of vascular access to the distal radial artery, both from the patient's and the physician's side. Access to the distal radial artery can provide;
-
1.
Improve left arm access for patient and physician.
-
2.
Permit access to prevent rotated arm motion in patients with orthopedic limitations.
-
3.
A more natural position for the patient to be treated during a long procedure.
-
4.
Provide alternative access besides radial access.
-
5.
Provide alternative access if other intravenous access preclude radial use.
-
6.
Provide an entry site for retrograde recanalization of the radial artery.
-
7.
Provide more minor risk radial artery injury [8].
In this case, we chose vascular access via the ipsilateral hand's anatomical snuffbox because it is easier to perform retrograde cannulation of radio-cephalic AV shunt. Snuffbox access is the closest access to intervention in the radio-cephalic area with retrograde cannulation. Identification of the snuffbox area is made by positioning the left hand's thumb in abduction and extension [9].
Patient preparation
Patient selection is essential before initiating radial access. A Barbeau test or modified Allen's test (MAT) can be performed before starting transradial access. The Barbeau test is a simple examination to ensure patency of the ulnoradial pathway and adequate perfusion. The ulna-palmar patency includes the following 4 types:
-
1.
There is no damping of the pulse immediately after compression.
-
2.
There is a damping of the pulsation.
-
3.
Loss of pulse followed by recovery within 2 minutes, and
-
4.
Loss of pulse without recovery within 2 minutes [10].
Palpation of the radial pulse can be very weak in patients with systemic shock or underlying vascular disease. The pulse may be erroneous in a patient with proximal radial artery occlusion due to a strong palmar flow.
An ultrasound examination was performed to evaluate the occluded AV shunt and the cephalic vein's size in this patient. The ultrasound examination helps the operator determine the accurate puncture location, vessel size, potential tortuosity, and vascular patency. It also helps the operator identify vasospasm and puncture-related complications such as hematoma or dissection. The incidence of arterial spasm is lower on access assisted by ultrasound. The ultrasound examination of the radial artery starts from the space between the thumb and index finger, which consists of the first dorsal interosseous muscle. The examination continues from the forearm's radial artery until it appears to join the brachial artery at the elbow level. The size of the vessels must be evaluated to determine the compatibility of the equipment to be used—subcutaneous injection of nitroglycerin results in vasodilation, assessing artery-catheter compatibility to be more accurate. The sheath's outer diameter should be equal to or less than the inner diameter of the artery lumen. The artery/sheath ratio (A/S) should be >1 to reduce radial artery occlusion risk. The sheath and the catheter size commonly used are 5 French (Fr) [11,12]. A sheath size larger than the arterial diameter results in vascular damage and results a pro-thrombotic area around it [13].
Equipment preparation and operating procedure
Equipment preparation for snuffbox access does not differ from the standard radial artery access procedures once the sheath is in place. An ultrasound can localize blood vessels and help measure the appropriate diameter of the sheath. The catheter can be used as in the routine access preceded by a wire insertion into the vessel. The size of the vascular access sheath must be appropriately fitted to reduce spasms. The possibility of “kinking” should be considered because of the initial distal radial artery branch's tortuosity. The thinner the sheath walls, the more likely the “kinking” can occur [8].
Hand positioning determines successful access of the distal radial artery. The wrist should be positioned 90° from the standard radial access position to stabilize the wrist's lateral surface. The wrist should be slightly bent toward the ulnar side to align the distal radial artery into the radial artery. Place a small towel/grip so that the corner between the base of the thumb and first finger is naturally exposed. This position helps keep the tendons and underlying soft tissue away from the distal radial artery to stabilize the surface [8].
There are 2 sites where the radial pulse can be palpated: in the anatomical snuffbox and the first intermetacarpal space [14]. The distal radial artery can be accessed in either the right or the left hand. The left-hand snuffbox approach is preferred because it uses the patient's nondominant hand (in most cases), and the operator can use the right hand to perform fine movements, such as in the femoral access. Besides, the operator's distance from the fluoroscope is safer [15]. If left-handed access is selected, the patient's arm can be placed over the body with the operator on the right side. The radial artery access in this snuffbox approach facilitates better arm position for the patient and improves ergonomics for the operator. Left-hand access is mainly considered for coronary artery procedures due to a better catheter position across the aortic arch [8]. If right-hand access is, the patient's arm remains on the right side with the hand resting (neutral position) on the prepared action board [12].
The left hand (ipsilateral to the AV shunt) was selected on the anatomical snuffbox to perform retrograde cannulation in this patient. The patient's hand was positioned on top of the patient's body in a neutral hand position. The operator worked from the patient's right side, allowing the operator to use the right hand for catheter manipulation and be at a fluoroscopy-safe distance.
Patent hemostasis in distal radial artery access
The term “patent hemostasis” is commonly used to describe the radial artery patency during hemostasis at the puncture site. The principle of patent hemostasis in distal radial artery access is to apply sufficient pressure to stop bleeding while maintaining antegrade blood flow to the radial artery [16]. Patent hemostasis without special devices can be achieved by pressing the puncture site with 2 fingers or a thumb to expand the compression area for 15 minutes. Once hemostasis is achieved, with no bleeding from antegrade or retrograde blood flow nor fluid in the surrounding tissue around the puncture site, the operator can complete the 15-minute compression with 1 finger [12]. When using standard hemostasis devices for regular radial access, various hemostasis methods involving elastic tape and bandages have been suggested for fixation [16].
There is another hemostasis procedure in the study of Cardarelli et al. using modified rapid hemostasis [17]. This procedure uses a special hemostatic disk (Statseal, Biolife, FL) and a hemostatic band (Safeguard radial, Merit Medical, S Jordan, UT). The balloon is inflated with 3-4 mL of air, and all air is expelled after 10 minutes. The device is removed 15 minutes later if no bleeding is observed, and arterial patency is evaluated using Doppler ultrasound. Of the 43 study subjects, 2 patients had hematoma, and no arterial occlusion was found. Patients can go home 90 minutes after the procedure. Based on this study, modified rapid hemostasis is also a safe procedure if appropriate equipment is available [17].
Another factor associated with endothelial injury is arterial spasms. Commonly used vasodilator agents include nitrates, calcium channel blockers, lidocaine, magnesium sulfate, and alpha-blockers. A systematic review by Kwok et al. [18] concluded that verapamil 5 mg or verapamil administration with nitroglycerin could prevent arterial spasms. However, Izgi et al. [19] showed that none of 15 patients treated without vasodilator administration developed radial artery occlusion.
Complications
A relatively few studies had been reported regarding complications associated with the distal radial artery access procedure. The most common complication is a hand hematoma of several degrees. The incidence of distal and proximal radial artery occlusion, neuropathy, and pain is low. Rarely, complications include arteriovenous fistulas, distal artery dissection, and pseudoaneurysms. Several factors that increase the risk of complications include recurrent arterial puncture, old age, nonsterile surgical procedures, long duration of treatment, coagulation disorders or anticoagulant/antiplatelet use, the larger diameter of sheath compared to the artery (A/S ratio <1), and imperfect hemostasis [3,20].
Conclusion
Access to the left distal radial artery in the anatomical snuffbox for intervention or coronary angiogram is a relatively new and safe technique. There are several considerations for the operator to choose vascular access to the anatomy of the snuffbox. Patient preparation and access tools and procedures are not much different from conventional radial access. This access benefits both the patient and the operator and has fewer bleeding complications and radial artery occlusion than conventional radial techniques. Ultrasound examination can help the operator determine the location of the puncture, the size, and the arteries' patency to minimize complications that may arise. Hemostasis at the distal radial artery access should use an appropriate hemostasis device.
Authors’ contributions
MP, IPD, and LFKW contributed to the concept and design of the article, patient data acquisition, and writing the article. JN was involved in revising the article critically for important intellectual content.
Ethics approval
Not applicable.
Availability of data and material
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Patient consent
Written informed consent was obtained from the patient for the anonymized information published in this article.
Footnotes
Funding: None.
Presentation at a Meeting: The article never been presented previously in a scientific meeting orally or as a poster.
Competing Interests: None declared.
References
- 1.Rigatelli G, Zuin M, Daggubati R, Vassilev D, Zuliani G, Nguyen T, et al. Distal snuffbox versus conventional radial artery access: an updated systematic review and meta-analysis. J Vasc Access. 2021;23(4):653–659. doi: 10.1177/11297298211005256. [DOI] [PubMed] [Google Scholar]
- 2.Caputo RP, Ttremmel JA, Rao S, Gilchrist IC, Pyne C, Pancholy S, et al. Transradial arterial access for coronary and peripheral procedures: executive summary by the transradial committee of the SCAI. Catheter Cardiovasc Interv. 2011;78(6):823–839. doi: 10.1002/ccd.23052. [DOI] [PubMed] [Google Scholar]
- 3.Boumezrag M, Ummat B, Reiner J, Venbrux A, Sarin S. Pseudoaneurysm: a rare complication of distal transradial access in the anatomical snuffbox. CVIR Endovasc. 2019;2:21. doi: 10.1186/s42155-019-0064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cerda A, Sol MD. Anatomical snuffbox and it clinical significance: a literature review. Int J Morphol. 2015;33(4):1355–1360. doi: 10.4067/S0717-95022015000400027. [DOI] [Google Scholar]
- 5.Watanabe S, Usui M. Distal transradial artery access for vascular access intervention. J Vasc Access. 2020;23(1):157–161. doi: 10.1177/1129729820974235. [DOI] [PubMed] [Google Scholar]
- 6.Rajah G, Garling R, Hudson M, Luqman A. Snuff box radial access: a technical note on distal radial access for neuroendovascular procedures. Brain Circ. 2019;5(1):36–40. doi: 10.4103/bc.bc_2_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brunet MC, Chen SH, Sur S, Mccarthy DJ, Snelling B, Yavagal DR, et al. Distal transradial access in the anatomical snuffbox for diagnostic cerebral angiography. J Neurointerv Surg. 2019;11(7):710–713. doi: 10.1136/neurintsurg-2019-014718. [DOI] [PubMed] [Google Scholar]
- 8.Shroff A, Pinto D. Abiomed; Danvers: 2019. Vascular access, management and closure. Society for cardiovascular angiography and interventions. [Google Scholar]
- 9.Al-Azizi KM, Lotfi AS. Beyond radial: ulnar, snuffbox, and palmar branch access. Cardiac Interv Today. 2019;1(13):40–43. [Google Scholar]
- 10.Ronald J, Durocher N, Martin JG, Smith TP, Kim CY, Sag AA. Evaluation of repeat distal transradial access in the anatomic snuffbox. Diagn Interv Radiol. 2021;27(5):639–643. doi: 10.5152/dir.2021.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hadjivassiliou A, Kiemeneij F, Nathan S, Klass D. Ultrasound-guided access of the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: a technical guide. EuroIntervention. 2019;16(16):1342–1348. doi: 10.4244/EIJ-D-19-00555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flores EA. Making the right move: use of the distal radial artery access in the hand for coronary angiography and percutaneous coronary interventions. Cathlab Digest. 2018;26(12):16–25. [Google Scholar]
- 13.Avdikos G, Karatasakis A, Tsoumeleas A, Lazaris E, Ziakas A, Koutouzis M. Radial artery occlusion after transradial coronary catheterization. Cardiovasc Diagn Ther. 2017;7(3):305–316. doi: 10.21037/cdt.2017.03.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sgueglia GA, Giorgio AD, Gaspardone A, Babunashvili A. Anatomic basis and physiological rationale of distal radial artery access for percutaneous coronary and endovascular procedures. JACC Cardiovasc Interv. 2018;11(20):2113–2119. doi: 10.1016/j.jcin.2018.04.045. [DOI] [PubMed] [Google Scholar]
- 15.Li F, Shi GW, Zhang BF, Yu XL, Huang HM, Xiao JQ, et al. Recanalization of the occluded radial artery via distal transradial access in the anatomic snuffbox. BMC Cardiovasc Disord. 2021;21(1):67. doi: 10.1186/s12872-021-01890-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koutouzis M, Maniotis C, Avdikos G. Prevention of radial artery occlusion after transradial catheterization. JACC Cardiovasc Interv. 2017;10(1):103. doi: 10.1016/j.jcin.2016.10.030. [DOI] [PubMed] [Google Scholar]
- 17.Cardarelli LL, Kiemeneij F, Chung J, Liu DM, Ho S, Legiehn G, et al. Safety and efficacy of a modified rapid hemostasis protocol for left distal radial artery access (ldPROTEA) CIRSE. 2018 [Google Scholar]
- 18.Kwok CS, Rashid M, Fraser D, Nolan J, Mamas M. Intra-arterial vasodilators to prevent radial artery spasm: a systematic review and pooled analysis of clinical studies. Cardiovasc Revasc Med. 2015;16(8):484–490. doi: 10.1016/j.carrev.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Izgi C, Feray H. Is radial access and transradial cardiac catheterization feasible without the use of any vasodilator? Int J Angiol. 2014;23(1):41–46. doi: 10.1055/s-0033-1358384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee J, Park S, Son J, Ahn S, Lee S. Real-world experience of the left distal transradial approach for coronary angiography and percutaneous coronary intervention: a prospective observational study (LeDRA) EuroIntervention. 2018;14(9):e995–e1003. doi: 10.4244/EIJ-D-18-00635. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.