Significance
During the COVID-19 pandemic, the world has experienced significant social and political unrest. Here, we show that individual-level discontent with the political system was related to feelings of “pandemic fatigue.” This “fatigue” varied with level of restrictions and severity of the epidemic but also grew as the pandemic prolonged. It fueled distrust in the government, conspiracy beliefs, and support for protests. Prior to the pandemic, several Western countries already faced increasing political destabilization. Our findings raise concerns that the pandemic will further undermine the political stability of Western countries. Furthermore, they highlight the importance of integrating the social sciences into pandemic management in order to buffer fatigue and counteract further increase in political discontent.
Keywords: fatigue, discontent, COVID-19, populism, politics
Abstract
Health authorities have highlighted “pandemic fatigue” as a psychological consequence of the COVID-19 pandemic and warned that “fatigue” could demotivate compliance with health-related policies and mandates. Yet, fatigue from following the policies of authorities may have consequences far beyond the health domain. Theories from the social sciences have raised that real and perceived costs of policies can also drive sentiments of discontent with the entire political establishment. Integrating theories from the health and social sciences, we ask how pandemic fatigue (i.e., perceived inability to “keep up” with restrictions) developed over the pandemic and whether it fueled political discontent. Utilizing longitudinal and panel surveys collected from September 2020 to July 2021 in eight Western countries (N = 49,116), we analyze: 1) fatigue over time at the country level, 2) associations between pandemic fatigue and discontent, and 3) the effect of pandemic fatigue on political discontent using panel data. Pandemic fatigue significantly increased with time and the severity of interventions but also decreased with COVID-19 deaths. When triggered, fatigue elicited a broad range of discontent, including protest support and conspiratorial thinking. The results demonstrate the significant societal impact of the pandemic beyond the domain of health and raise concerns about the stability of democratic societies, which were already strained by strife prior to the pandemic.
When the COVID-19 pandemic hit Western democracies in March 2020, it hit societies already strained by tension and strife. Longitudinal analyses suggest that political instability has been increasing in some Western democracies across multiple decades (1) and was fueled further by the global financial crisis in 2008, the immigrant crisis in Europe in 2015, the 2016 Brexit referendum, and the results of the 2016 US elections. These events have been analyzed as being associated—as causes or effects—with increasing antisystemic sentiments in Western democracies, which have motivated public protests against the establishments, support for authoritarian leaders and policies, and the circulation of and belief in conspiracy theories (2). The COVID-19 pandemic also caused a sharp rise in public protests, and even political violence (3), and the World Health Organization (WHO) warned of an “infodemic” of misinformation during the pandemic (4).
In this article, we examine whether and how the COVID-19 pandemic contributed to political discontent in Western democracies. Prior research has consistently argued that political discontent is fueled by feelings of loss of control (5). The COVID-19 pandemic also gave rise to such feelings, often discussed by authorities and researchers under the label of “pandemic fatigue” (6, 7). As argued by some researchers, the costs of prolonged compliance with behavioral policies could elicit “fatigue” and fuel anger toward the political system (3, 8).
Theoretically, we review and clarify the concept of pandemic fatigue, which has been the object of considerable debate. We argue that pandemic fatigue should be conceptualized as exhaustion from the costs of continued compliance and can reveal itself as the perceived inability to “keep up” with restrictions. Integrating arguments from social science and health psychology, we contend that such feelings of pandemic fatigue can fuel political discontent. Empirically, we present an analysis of the development of perceived inability to keep up with restrictions across eight Western countries (Denmark, France, Germany, Hungary, Italy, the United Kingdom, the United States, and Sweden) from September 2020 to July 2021. This analysis shows that these feelings reflected the social and mental costs of compliance (i.e., social isolation); that they were triggered when pandemic restrictions were put in place; and that these feelings strengthened as time went by. Consistent with our main theoretical claim, we subsequently show that the feeling of being unable to keep up with restrictions was correlated with multiple indicators of political discontent across the observed countries. In line with theoretical distinctions between authoritarian aggression and submission as distinct bases of discontent (9), the results show that this inability to keep up with restrictions specifically fueled more active forms of discontent and not passive submission to strong authorities. Furthermore, we are able to strengthen the causal interpretation of these findings using panel data, suggesting that pandemic fatigue exerted a causal effect on political discontent and populist sentiments.
These findings provide at least three contributions. First, they provide a test of a key psychological argument within the literature on political discontent, showing that feelings of exhaustion due to external demands can lead to antiestablishment backlash. Second, the findings provide an important message for authorities during a large-scale health crisis such as a pandemic. The emergence and effects of pandemic fatigue show that a pandemic has consequences far beyond the domain of health. Pandemic management should, therefore, draw not only on health expertise but also on the full expertise of the social sciences to ease feelings of exhaustion. Fatigue—if ignored—may have immediate effects on compliance with restrictions but may also undermine trust in authorities over time. Finally, while some studies suggest that the pandemic on average increased the public’s trust in science and elites (10, 11), our findings raise more worrisome prospects for the future. Prior to the pandemic, several Western democracies already faced dynamics of political destabilization. The present findings suggest that the pandemic will worsen those dynamics among individuals and groups strongly affected by the costs of compliance.
The Concept of Pandemic Fatigue
Since the outbreak of the COVID-19 pandemic, multiple different notions have been used to capture the potential exhaustion, tiredness, and fatigue induced by the pandemic. Currently, there is a convergence toward using pandemic fatigue as “the most appropriate concept” to denote such feelings (12). At the same time, however, this and related concepts have been the objects of significant debate. For example, the British government delayed their lockdown during the first wave of the pandemic with an argument that, within weeks, compliance with restrictions would generate “behavioral fatigue.” This decision and its justification were met with significant criticism due to the lack of evidence for behavioral fatigue (13). Later, in the early phases of the second wave of infections, the WHO warned about pandemic fatigue and defined it as a “demotivation to follow recommended protective behaviors, emerging gradually over time and affected by a number of emotions, experiences, and perceptions” (6). This warning was also met with criticism due to the disjunction between the WHO’s motivation-oriented definition and more traditional definitions of fatigue within health psychology, which are oriented toward how exhaustion can emerge, even if motivation is high (8, 14).
The concept of fatigue has a long history within health psychology and has often been the object of disagreement. A conceptual review concluded that “the term ‘fatigue’ has defied efforts to provide a single, broadly acceptable definition.” (15) Overall, however, two general approaches to assessments of fatigue exist: An indirect method of assessing fatigue as time-dependent decreases in objective performance and a direct method of assessing the subjective sense of exhaustion (15). Importantly, however, both methods converge on the argument that fatigue is caused by prior engagement in a costly action. This is particularly clear in more psychological applications of the concept of fatigue such as in literatures on compassion fatigue (i.e., fatigue among care workers, ref. 16) or harassment fatigue (i.e., fatigue in victims following continued rejection of harassers, ref. 17). Compassion fatigue is, for example, directly conceptualized as a response to the “costs of caring” (16). While these costs may reduce subsequent motivation and engagement in care, demotivation is an effect of fatigue but not fatigue per se.
From the perspective of this broader fatigue literature, pandemic fatigue is best conceptualized as feelings of exhaustion or tiredness caused by the costs of compliance such as the mental costs of social isolation (18–20). These feelings of exhaustion can make it difficult to keep up with restrictions, even if motivation is high. Against the WHO definition, a demotivation may thus be an effect of fatigue, but it is not integral to the sense of pandemic fatigue (8, 13). Put differently, a demotivated person is not necessarily a fatigued person. As evidenced by multiple studies, decreased compliance may thus have multiple other causes including lack of fear of the virus (21), a lack of a clear sense of how to act (22), and the existence of practical barriers against complying (23).
Prior empirical studies of pandemic fatigue have used overtime decreases in compliance as their indicator, i.e., the indirect method measuring objective performance. In relation to early epidemics, Cowling and colleagues (24) studied the H1N1 epidemic in Hong Kong and found that social distancing significantly declined over an 8-mo period. During the COVID-19 pandemic, Goldstein and colleagues (25) estimated the effects of restrictions on mobility and found that the effect of interventions on mobility decreases over time, which they attribute to fatigue. Similarly, Petheric et al. (26) noted crossnational decreases in adherence to costly policies such as physical distancing as the COVID-19 pandemic prolonged. Importantly, this was not observed for mask wearing, a less costly protective behavior. While the distinct dynamics for more and less costly behavior is consistent with the role of pandemic fatigue, these associations are potentially confounded by other drivers of decreased compliance.
Importantly, however, some studies have used measures of subjective feelings of exhaustion to more directly establish the existence of pandemic fatigue. Lilleholt and colleagues (7) developed a measure of feelings of pandemic fatigue and found it to relate negatively to people’s self-reported tendency to follow each of the following four health-protective behaviors: physical distancing, hygienic behavior, mask wearing, and information seeking. Using a survey experiment in which pandemic fatigue was induced via a self-reflection task, this research also provides evidence that the feelings of pandemic fatigue have a negative causal effect on motivations to adhere to pandemic restrictions. Similarly, refs. 12 and 27 measure pandemic fatigue by a scale of feelings of pandemic-specific “burnout.” Consistent with the notion that pandemic fatigue reflects the costs of compliance and not merely a lack of motivation, these studies found that people who are higher in pandemic fatigue are also more (rather than less) afraid of the coronavirus and feel greater stress because of the pandemic. As further evidence, Ford and colleagues (28) used another scale of pandemic fatigue (modeled after a scale of harassment fatigue by Ford and Ivancic (17)) to demonstrate that people who are higher in pandemic fatigue are motivated to avoid COVID-19-related information but nonetheless continue to seek it out. Finally, Taylor and colleagues (29) used another scale of pandemic burnout and found it to be related to pandemic-specific feelings of stress, anxiety, and depression as well as elevated fear of public shaming if they did not comply with pandemic policies. By more directly assessing pandemic fatigue, these studies provide prima facie evidence in favor of the existence of feelings of exhaustion and highlight the importance of conceptualizing pandemic fatigue as a reflection of the perceived costs of compliance rather than a change in objective behavior. At the same time, this set of studies also demonstrates that there is not yet an established, widely used measure of pandemic fatigue.
How Pandemic Fatigue May Fuel Political Discontent.
Beyond the conceptual and methodological challenges, prior studies have mainly focused on the association between pandemic fatigue and adherence to behavioral guidelines during health emergencies. Here, we investigate the possibility that feelings of pandemic fatigue have long-term consequences beyond compliance with interventions during the COVID-19 pandemic. In fact, the researchers most critical of the concept of pandemic fatigue argue that the most likely effect of fatigue—if it exists—is anger directed at those deemed responsible during the pandemic (8). It is difficult to direct anger toward a faceless virus, and thus, the immediate targets of anger in this regard are the political elites and the COVID-19 interventions that cause the distress.
Antiestablishment sentiments can reveal themselves in multiple different and more specific opinions and behaviors including rejection of the policies of mainstream parties and governments on specific issues (e.g., on COVID-19) (30), sharing of misinformation (31), support for protests including extreme protests involving the use of violence for a political purpose (32), and support for dominant and tough-minded leaders (33).
Pandemic fatigue can facilitate antiestablishment views through two processes. First, compliance with some public health measures is a source of stress in terms of physical health, well-being, social relationships, and finances (3, 34). Second, in the beginning of the COVID-19 pandemic, new social norms and demands emerged overnight (35, 36). Not only were face masks suddenly used in public and handshakes replaced by elbow bumps, but much costlier norms and demands such as self-isolation and homeschooling were also introduced. These rapid norm changes during the COVID-19 pandemic are likely to cause mentally taxing feelings of control loss and uncertainty that may increase levels of pandemic fatigue (12, 37). In tandem, the material losses and demands placed on citizens due to health interventions may trigger an “aversive sense of low power or control,” which has been highlighted in populism research as a key psychological cause of political discontent (5).
Specifically, as with other issues often discussed in research on discontent (e.g., immigration and globalization), the pandemic and associated interventions may lead to both actual socioeconomic change (e.g., unemployment due to decreasing economic activity or isolation following infection) and subjective feelings of loss (5). Members of a dominant group who feel threatened are particularly attracted to discourses that explicitly highlight routes toward greater control, and this may help them regain a sense of dominance and well-being (2, 5, 38). Political discontent aimed toward the established political elites can be seen as one way to regain control.
Some evidence suggests that fatigue does indeed facilitate political discontent. Using a two-wave panel design, a prior study compares the existence of extreme antisystemic sentiments in four countries in April and June 2020 and correlates this development with a measure of the psychological burden of the COVID-19 pandemic (3). This measure of the psychological burden is an additive measure of experiences of losses, both material (e.g., financial) and immaterial (e.g., well-being), over the pandemic, and predicts the emergence of radicalized behaviors and sentiments.
Moving beyond this finding, here, we track feelings of pandemic fatigue, measured as the perceived inability to keep up with restrictions, over 13 rounds of data collected over 11 mo of the COVID-19 pandemic in eight countries. This allows us to both understand the causes of feelings of pandemic fatigue and provide analyses with higher causal leverage using a panel component of this study. Furthermore, we utilize a wide range of outcome measures, which capture several forms of discontent, including governmental distrust, opposition to mainstream policies, belief in conspiracy theories, support for public protests, and support for authoritarian leaders. This allows us to move beyond outcomes that are indicative of radicalized behavior and focus on less extreme forms of discontent (for a discussion of this distinction, see also ref. 2). At present, we do not know whether pandemic fatigue and discontent are limited to a few radicalized groups of conspiracy theorists or whether pandemic fatigue has elicited discontent in broader segments of citizens.
Methods and Materials
All data and command files are available in the online repository at Open Science Framework: https://osf.io/ax6zv/. The data collection fully complies with the Aarhus University’s Code of Conduct and was approved by the Technology Transfer Office at Aarhus University. The study did not undergo further ethics review, as per section 14(2) of the Act on Research Ethics Review of Health Research Projects, “notification of questionnaire surveys... to the system of research ethics committee system is only required if the project involves human biological material.” All participants provided informed consent and were reimbursed according to their standing agreements with the data provider.
Data.
We fielded quota-sampled surveys in eight countries from September 13, 2020, until July 20, 2021: Denmark, Sweden, the United Kingdom, the United States of America, Italy, France, Germany, and Hungary (see SI Appendix, Table S1 for an overview of the data collection) (39). These countries represent a diverse set of Western countries in terms of the severity of and the national responses to the COVID-19 pandemic as well as the degree of political polarization and the strength of democratic institutions. Data were collected one or two times per month in rounds of about 500 respondents per country. In total, we collected 13 rounds of data in Denmark and 12 rounds in the remaining countries within this time period (total N = 49,116).
In each of the eight countries, the survey company Epinion sampled adult respondents using online panels. Among the panelists invited to take our survey, the response rate across the countries in our sample was between 15% (Hungary) and 60% (the United States). Survey respondents were quota sampled to match the population margins on age, gender, and geographic location for each of the eight countries. We address imbalances by poststratifying our sample data to match the demographic margins from the population (see SI Appendix, Tables S4–S11 for an overview of sample versus population characteristics). All statistical analyses except panel analyses employ these poststratification weights.
In each round, some participants are recontacted, which provides a panel component to the data. Most participants in the panel component have only participated twice, while some of the participants have participated up to five times. Furthermore, the distribution of the participants in the panel component is not equal across countries. Specifically, about half of the participants in the panel component are from Denmark, while the rest are more equally distributed across the rest of the countries in the sample (SI Appendix, Table S2). In SI Appendix, Table S3, we show that participants in the panel component are demographically similarly to single-wave participants.
Measurements
Pandemic fatigue.
We measure pandemic fatigue using respondents’ degree of agreement with the following statement: “I do not think I can keep up with the restrictions against the coronavirus for much longer.” Respondents provided responses on a 5-point scale ranging from “completely disagree” to “completely agree.” We rescale responses to vary between 0 and 1 with higher values indicating higher levels of pandemic fatigue. SI Appendix, Fig. S1 shows the distribution of responses across the countries in the sample. The wording of the item is designed to capture expressions of a sense of exhaustion using everyday, face-valid terms similar to the sense of being unable to keep up with the pace of a runner or the incoming tasks at work. Importantly, to the extent this measure does capture pandemic fatigue, it should reflect the perceived costs of compliance with pandemic policies rather than mere demotivation to follow them. For example, a person not concerned about getting sick with COVID-19 may be demotivated to comply with restrictions, yet this would not constitute fatigue.
To assess the construct validity of the measure, SI Appendix, Fig. S2 displays the associations between the measure of pandemic fatigue and a key measure of the mental costs of pandemic compliance, loneliness (18–20), as well as the most important factors associated with the potential confounder, motivation. Specifically, beyond loneliness, the model includes feelings of personal and social fear, self-efficacy, self-reported behavioral compliance, and sociodemographic variables (see below for further discussion). The analyses demonstrate that there is a unique and substantively strong association between the reported loneliness and the measure of pandemic fatigue: A two standard deviation increase in loneliness is associated with a 23.4%-points increase in fatigue (95% CI: 19.9, 26.8). This association is 3.3 times larger than the second strongest association. Finally, to assess the convergent validity of the present measure with other measures of pandemic fatigue, a separate study was conducted in Germany in March 2022 (40). In this study, we assessed pandemic fatigue using the present measure as well as a validated pandemic fatigue scale (7) and a validated scale for “COVID-19 burnout” (29). In support of the measure’s convergent validity, we found large correlations between our item and the pandemic fatigue scale (r = 0.48), and particularly with its behavioral fatigue subcomponent (r = 0.52), and a lower, albeit still sizable correlation with the COVID-19 burnout scale (r = 0.30) (SI Appendix, section S1.5).
Country-level predictors of pandemic fatigue.
We focus on three potentially important country-level predictors to assess the development of pandemic fatigue. First, we measured the stringency of national COVID-19 policies using the Oxford COVID-19 Government Response Tracker (OxCGRT) (41). The index tracks public and social measures implemented against the pandemic taken in a specific country at a given point in time (e.g., school and workplace closings, curfews, and restrictions on international travel). Second, we used the registered count of daily deaths per capita (as reported by the OxCGRT dataset) to measure the severity of the epidemic in the given country. Third, we included a simple measure of time since the start of the pandemic (26). We standardized each of these predictors with a mean 0 and a unit of 2 standard deviations to make their estimated coefficients comparable with each other (42). Two standard deviations correspond to about half a year, 10.4 new deaths per million people, and a 25.5 points change on the 100-point stringency index.
Individual-level consequences of pandemic fatigue.
To assess whether pandemic fatigue fuels political discontent, we analyze how pandemic fatigue correlates with six individual-level indicators of discontent: 1) opposition to COVID-19 restrictions, 2) protesting over restrictions, 3) belief in COVID-19 conspiracies, 4) concern about democratic rights, 5) government distrust, and 6) support for strong leaders. This multitude of indicators is chosen to reflect the many potential faces of political discontent including policy opposition, mistrust, protest behavior, and the promotion of dominant, populist leaders (2).
We measure five of these discontent indicators with a battery, where respondents are asked to report how much they agree or disagree with five statements each tapping into one of the discontent indicators. On opposition to COVID-19 restrictions: “The government’s response to the coronavirus has been too extreme.” On support for antilockdown protests: “I support the public protests against the government’s policies during the COVID-19 pandemic.” On conspiratorial thinking: “I believe the government is hiding important information from the public about the coronavirus and its cures.” On concern over democratic rights: “I am concerned about my democratic rights in the current circumstances.” On preferences for strong leaders: “Our country needs a strong leader right now.” For each statement, the respondents reported their level of agreement on a 5-point scale ranging from completely disagree to completely agree. We rescale each measure to vary from 0 to 1 with higher values indicating higher levels of discontent. We measure the sixth and final discontent indicator, distrust in the government, by asking respondents the following: “Give your assessment on a scale from 0 to 10, where 0 indicates that you have no confidence in the government at all, and 10 indicates that you have full confidence in the government.” Again, we rescale this measure to range from 0 to 1 with higher values indicating higher levels of distrust in the government. In SI Appendix, Fig. S5, we provide an overview of the developments across time and countries in these indicators.
Individual-level controls.
We measure the following demographic control variables: sex, age, education, and income. Sex is an indicator variable (0 for females; 1 for males). Age is a continuous variable that we rescale with mean 0 and a unit of 2 standard deviations. Education is an indicator variable based on the International Standard Classification of Education typology (0 for nontertiary education; 1 for tertiary education). Income is measured in country-specific deciles. We recode the income information into three categories, including below the median, above the median, and not reported.
As noted in the theoretical discussion, a methodological concern is whether the associations of measures of pandemic fatigue are confounded by factors related to motivation or opportunity. As additional individual-level controls, we therefore include two motivational factors highlighted by prior research: personal and social fear and feelings of self-efficacy (see refs. 22 and 36). Opportunities for compliance will be related to socioeconomic factors and the statistical control for income and education will reduce confounding from this source. In addition, to control away confounding factors not tapped by the other controls, we also include a direct measure of the degree of self-reported change in behavior to avoid spreading infection (i.e., behavioral compliance, ref. 22). Finally, as noted above, there is a strong association between loneliness and pandemic fatigue. As loneliness may also be related to political discontent, we also include loneliness as a control variable to reduce spuriosity in the association between fatigue and discontent. The coding of all control variables is detailed in SI Appendix, section S1.7. As with age, we rescale these measures with mean 0 and a unit of 2 SD.
Statistical analysis.
First, we want to assess how the country-level factors shape pandemic fatigue at the individual level. Our baseline model regresses pandemic fatigue on policy stringency, deaths per capita, and time since the start of the pandemic. It also includes random intercepts by country to account for the clustering in the data. To test whether associations between country-level trends in the pandemic and our measure of fatigue reflect shifts in motivation, we report an additional model, which includes our attitudinal individual-level controls. To the extent that the coefficient estimates for stringency, deaths, and time remain substantively similar across the two models, we can be confident that stringency, deaths, and time do not shape pandemic fatigue through motivation.
Second, we want to assess the individual-level associations between pandemic fatigue and forms of political discontent. To do this, we rely on two complementary strategies. As a first strategy, we use the same multilevel regression modeling approach as above, but now with fatigue as a predictor rather than the outcome. In our baseline models, we regress each of the six political discontent outcomes one by one on pandemic fatigue and the demographic controls while including random intercepts for countries and survey wave. Again, the random intercepts account for clustering in our data and improve the precision of our estimates. Next, we add to the models the additional individual-level controls to assess whether the associations revealed in our baseline model are confounded by motivational factors. Again, if coefficient estimates for pandemic fatigue do not change much, it increases our confidence that the relationships are not an artifact of differences in motivations shaping both feelings of fatigue and discontent.*
As a second strategy, we use our panel data component in two-way fixed-effects models to increase the causal leverage of our estimates of the impact of fatigue on political discontent. More specifically, the two-way fixed-effects estimators regress each of the political discontent outcomes on pandemic fatigue while including fixed effects for individuals and survey waves. The individual-level fixed effects control for stable individual differences by only using within-individual variation in political discontent and fatigue while the survey wave fixed effects account for potential common time trends in the variables. Whereas the multilevel estimators compare political discontent between individuals with high versus low levels of fatigue, the two-way fixed-effects estimators compare how political discontent changes when fatigue changes compared to an earlier interview. This means that the estimator eliminates all time-invariant confounding. However, time-variant confounding might still bias estimates. Only on the assumption that individuals’ discontent would have followed parallel trends in the absence of changes in fatigue (43) does the two-way fixed-effects estimators yield unbiased estimates for the causal impacts of fatigue on political discontent. Importantly, we provide tests that support the parallel trends assumption in this application (see SI Appendix, section S2.5 for details).
Results
Pandemic Fatigue is Predicted by Time, Higher Stringency, and Fewer Deaths.
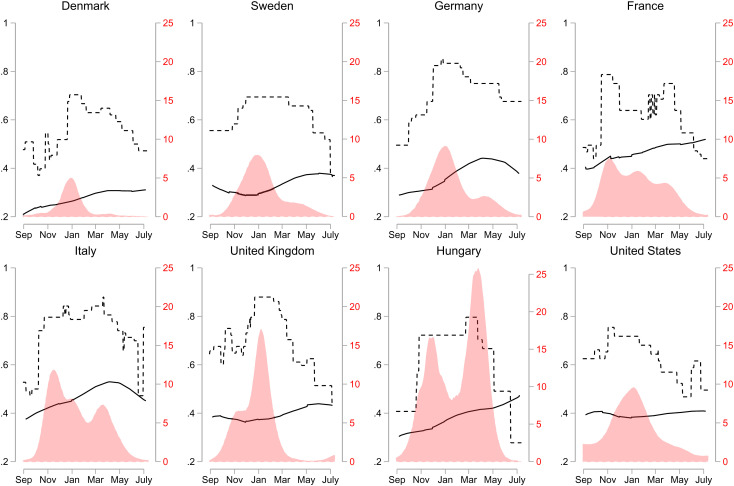
Focusing first on country-level predictors of pandemic fatigue, Fig. 1 illustrates the developments of fatigue, policy stringency, and severity of the pandemic in each country over the survey period (September 2020–July 2021). Fig. 1 shows that pandemic fatigue (the solid line) gradually increased in all countries throughout these 11 mo in seven out of the eight countries. However, it is also clear that these increases leveled off in most countries in the spring of 2021 (around April 2021). This pattern is most notable in Germany and Italy, but can also be found in Denmark, Sweden, the UK, and, to some extent, France.
Fig. 1.
Developments in fatigue, policy stringency, and daily COVID-19 deaths (September 2020–July 2021). Solid lines are developments in fatigue based on our survey data using a lowess smoother. Dashed lines are developments in stringency of government responses to COVID-19 (based on the Oxford Stringency Index). Red areas are developments in daily COVID-19 deaths per million using a kernel smoother.
The overall pattern reveals some parallel development with respect to policy stringency (the dashed line) and pandemic fatigue in most countries. Thus, we observe an increase in stringency across all countries in the first half of the study period until January 2021 that fits the general increase in pandemic fatigue. Similarly, we observe that stringency levels overall remained high in the first months of 2021 and thereafter began to drop by April 2021. At least in Italy and Germany, this led to decreased pandemic fatigue in the same period.
Finally, Fig. 1 suggests that pandemic fatigue was negatively related to the severity of the pandemic (the red area). Across the eight countries, the figure shows that when daily death counts (per capita) decrease, fatigue tended to increase. In sum, Fig. 1 provides some evidence that pandemic fatigue increased with time, when stringency went up and when the severity of the pandemic decreased. However, the figure also suggests that these macrolevel predictors are intercorrelated.
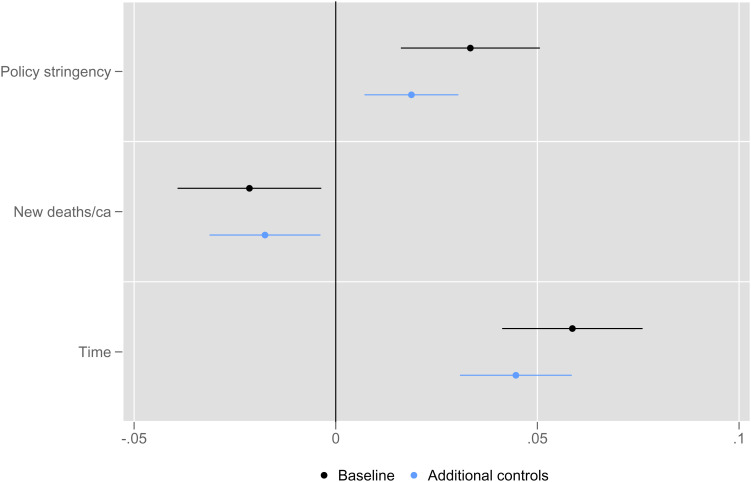
In Fig. 2, we seek to disentangle the associations of each country-level correlate with pandemic fatigue. The black points are estimates from the baseline multilevel regression model, while the blue points are estimates from the model with additional individual-level controls. Fig. 2 indicates that fatigue increased with time even controlling for the severity of the pandemic and the stringency of policies. Specifically, across the eight countries, pandemic fatigue increased with about 5.8%-points (95% CI: 4.1, 7.6) every 6 mo during the study period. Correspondingly, consistent with the method of using time as an indicator of fatigue, we find support that the phenomenon emerges over time but slowly so.
Fig. 2.
Country-level correlates of pandemic fatigue. Point estimates along with 95% confidence intervals from weighted multilevel regression models (n = 49,116). Baseline multilevel regression models (black) represent estimates from specifications that regress fatigue on policy stringency, new deaths, and time while also including random intercepts. Models with additional controls (blue) represent estimates from models that include for social and personal fear, efficacy, behavioral change, and feelings of loneliness as additional controls.
Turning to policy stringency, Fig. 2 corroborates that people felt less fatigued when restrictions in a given country were more stringent, i.e., when the costs of compliance were higher. Thus, we observe that fatigue increased with about 3.3%-points (95% CI: 1.6, 5.1) when policy stringency was tightened by 2 SD. Finally, citizens seemed to experience less pandemic fatigue when pandemic severity increased. Specifically, when COVID-19 deaths increased by 2 SD, we observe an average decrease in pandemic fatigue of about −2.2%-points (95% CI: −3.9, −0.3). This suggests that people felt less exhaustion from complying with a constant set of restrictions when the pandemic was increasingly severe. In SI Appendix, Fig. S7, we also examine whether stringency and COVID-19 deaths interact in their associations with pandemic fatigue. This interaction is, however, insignificant, providing little evidence against the claim that the severity of the response and the severity of deaths do not mainly operate independently in their associations with fatigue.
Reassuringly, across all the three country-level predictors, we find that the model with additional controls yield substantively similar estimates. This implies that our estimates track how time, stringency, and deaths correlated with a feeling of exhaustion and does not simply reflect changes in, for example, motivational factors such as fear of the coronavirus.
In the above analyses, we examine the accumulation of costs of pandemic policies by assessing associations between, on the one hand, fatigue and, on the other hand, time and policy stringency. In SI Appendix, Fig. S6, we provide additional evidence by combining the latter two factors and assessing whether time is more strongly associated with fatigue when stringency is above a certain level. These analyses demonstrate that the number of consecutive days where stringency is above the median stringency (specifically, the country-specific median for the period of March 2020–July 2021) has an independent association with fatigue, over and beyond the simple associations of stringency and time. Hence, a prolonged period with significant interventions is particularly exhausting to the public.
Pandemic Fatigue Predicts Individual-Level Political Discontent.
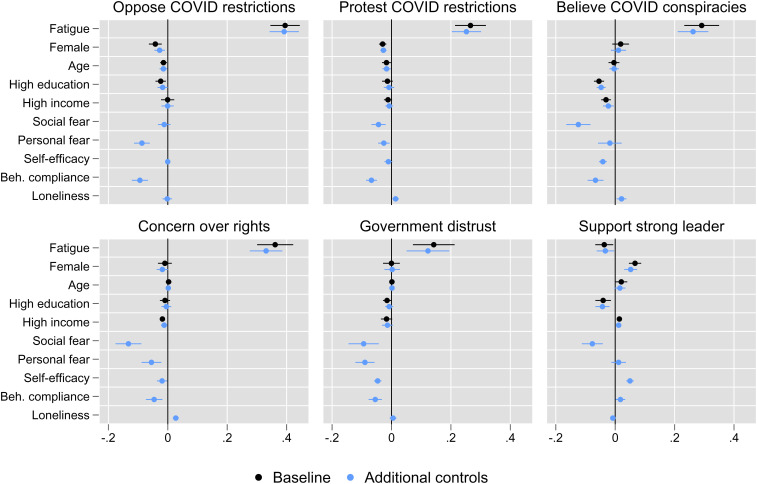
On this basis, we turn toward understanding whether pandemic fatigue predicted political discontent. Fig. 3 reports coefficient estimates from our multilevel models regressing discontent on fatigue and controls. Focusing on the baseline models (in black), we find that feelings of pandemic fatigue overall were associated with political discontent. More specifically, when comparing respondents with the highest level of fatigue to respondents with the lowest level of fatigue, the baseline models show an increase in opposition to COVID restrictions of 39.5% -points (95% CI: 34.6, 44.4), in support for protests against COVID restrictions of 27.6%-points (95% CI: 21.4, 31.8), in beliefs in COVID conspiracies of 29.1%-points (95% CI: 23.3, 35.0), in concerns over democratic rights of 36.2%-points (95% CI: 30.1, 42.2), and in government distrust of 14.2%-points (95% CI: 7.2, 21.2). At the same time, people who suffered from higher fatigue support strong leaders less by −3.7%-points (95% CI: −6.7, −0.7).
Fig. 3.
The figure shows that fatigue correlates with political discontent. Point estimates along with 95% confidence intervals from weighted multilevel regressions (n = 46,222–48,714). Baseline models (filled black circles) represent estimates from specifications that along with fatigue also include demographic controls (sex, age, education, and income). Models with additional controls (filled blue circles) represent estimates from models that along the demographics variables additionally control for social and personal fear, efficacy, behavioral compliance, and feelings of loneliness. All models include random country and survey wave intercepts.
As is clear from the covariates in the baseline models, we overall observe little demographic heterogeneity in political discontent. The models with additional controls (in blue) corroborate the findings above and suggest that motivational and opportunity factors do not strongly confound the observed relationship between pandemic fatigue and political discontent.
The presented models assume that the correlation between fatigue and each of the discontent indicators is the same across all countries. In SI Appendix, Fig. S8, we relax this assumption by adding varying slopes for fatigue into our multilevel regression models to extract the country-specific correlations between pandemic fatigue and each of the six political discontent outcome measures. The analyses show that the country-specific results are highly consistent with the overall findings presented here.
An important limitation to the individual-level findings above is that they may suffer from selection bias. One source of bias emerges from the possibility of confounding due to omitted variables (i.e., alternative explanations). Many of the relevant omitted variables are stable individual-level characteristics such as chronic mental challenges, general health concerns, general political trust, or a lack of socioeconomic opportunities (7, 29). If such factors simultaneously exert independent impacts on pandemic fatigue and political discontent, then they create omitted variable bias in the estimates. Another equally important source of bias is reversed causality. For example, it might be that an increased concern about democratic rights leads to increased feelings of pandemic fatigue. In traditional observational data, it is difficult to measure and control for all potential sources of selection bias. However, by exploiting the panel component of our data, we are able to limit these sources of bias and thereby gauge causality. Specifically, we rely on the two-way (i.e., individuals and survey waves) fixed-effects estimator described in the Statistical analyses section to increase causal leverage regarding the influence of pandemic fatigue on the six political discontent outcome measures. Fig. 4 reports the results from the two-way fixed-effects analyses.
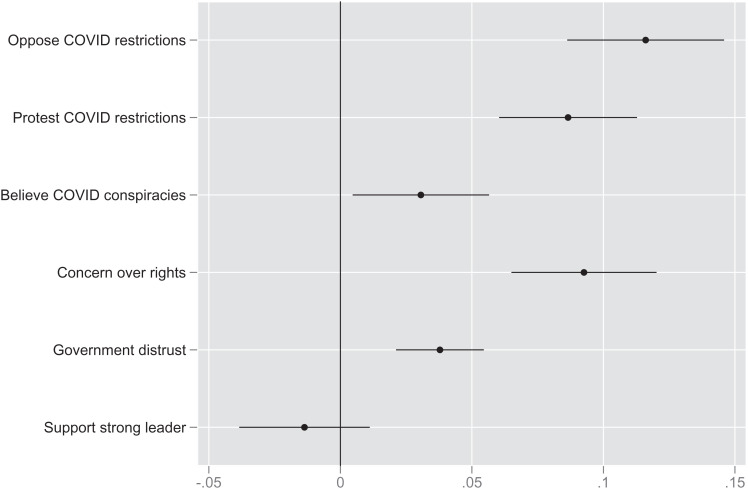
Fig. 4.
Two-way fixed-effects estimates of fatigue on political discontent. Point estimates along with 95% confidence intervals (standard errors are clustered on individuals) from two-way fixed-effects models (n = 9,815–10,792).
Overall, the effect estimates displayed in Fig. 4 support the correlational results from Fig. 3. An individual change from the lowest to the highest level of pandemic fatigue spurred an increase in opposition to COVID restrictions of 11.6%-points (95% CI: 8.6, 14.6), in support for protests against COVID restrictions of 8.7%-points (95% CI: 6.0, 11.3), in beliefs in COVID conspiracies of 3.1%-points (95% CI: 0.5, 5.6), in concerns over democratic rights of 9.3%-points (95% CI: 6.5, 12.0), in government distrust of 3.8%-points (95% CI: 2.1, 5.5), and a decrease in support for strong leaders of −1.4%-points (95% CI: −3.8, 1.1). Despite high consistency with the previous correlational results, it is important to note that the estimated effects of pandemic fatigue on political discontent are substantially lower when using the two-way fixed-effects estimator. However, we still observe substantial effects of pandemic fatigue—except for preferences for a strong leader—which suggest that feelings of fatigue fueled political discontent across the countries.
SI Appendix, section S2.5 reports robustness checks probing the parallel trends assumption on which the causal interpretation of these results hinges. The robustness checks show that reverse causality is unlikely to bias our results. An increase in political discontent does not appear to feed back to increased feelings of pandemic fatigue. The robustness checks also show that the effect of fatigue on political discontent remains similar if we do not assume that all respondents follow similar trends, but allow each respondent to follow their own linear trend.
To further probe the robustness of the effect estimates, SI Appendix, Fig. S10 shows the two-way fixed effects for each country separately. SI Appendix, Fig. S10 suggests that the estimated effects are relatively homogeneous in terms of coefficient sign across the eight countries, especially regarding opposition to COVID restrictions, support for protests against COVID restrictions, and concerns over democratic rights (although the precision varies crossnationally due to variation in the number of observations). Similarly, the estimated effect for support for strong is nonsignificant and close to zero in all countries. Coefficients for beliefs in government-related COVID conspiracies as well as government distrust are less consistent, potentially because of crossnational heterogeneity in the exact actions taken by the individual governments.
Taken together, the individual-level longitudinal results overall mirror the correlational evidence relatively closely. In other words, this means that pandemic fatigue should be regarded not only as a key predictor of political discontent, but as a causal factor that fueled discontent across the eight countries. This conclusion, however, only applies to indicators of political discontent beyond submission to strong leaders.
Discussion and Conclusion
In this study, we investigated 1) the levels and developments of feelings of pandemic fatigue (measured as the perceived inability to keep up with restrictions) across eight Western countries during the COVID-19 pandemic, 2) the contextual determinants of pandemic fatigue, and 3) whether pandemic fatigue correlates with and causes populist sentiments and political discontent. The results show that pandemic fatigue increased when stringency went up, when death numbers went down, and as time went by. Additional analyses demonstrated that a prolonged period with stringent interventions had an accumulating impact and were particularly exhausting to the public (SI Appendix, Fig. S6). Both the cross-sectional and panel data provide evidence that pandemic fatigue elicited a broad range of antiestablishment sentiments, including opposition to COVID-19 policies, government distrust, protest support, and conspiratorial thinking. Moving beyond extant research’s findings that the COVID-19 pandemic radicalized some groups (3), we show how pandemic fatigue fueled a broader range of political discontent, including lowered support for COVID-19 policies, increased support for antilockdown protests, and generated distrust in the government. Fatigue-induced discontent is not limited to radicalized sentiments among the few.
Interestingly, pandemic fatigue does not, however, elicit support for strong leaders, suggesting that pandemic fatigue elicits active forms of discontent rather than passive submission to authority figures (for a further discussion of this distinction, see ref. 2). Essentially, when fatigued is caused by the costs of complying with state-mandated restrictions, people do not become further motivated to submit to authority but rather to protest against authority. While the results thus demonstrate the importance of exhaustion for the activation of political discontent, it highlights a distinction between active and passive forms of discontent (9).
The present findings stand in contrast to some prior research, which found that, overall, the pandemic increased trust in establishment authorities and reduced the appeal of populism (10, 11). There are two complementary explanations for this divergence in findings. First, the present findings zoom in on how feelings of pandemic fatigue fueled political discontent. Such feelings are most likely prominent among a smaller segment of the public. While people on average may have experienced increasing trust, some groups—those who felt fatigued—decreased in their levels of trust. Analyses in SI Appendix, Fig. S2 suggest that those groups reacted to the perceived costs—in terms of loneliness—of prolonged restrictions. Groups more severely affected mentally by the pandemic are thus those more likely to have reacted with decreasing trust.
Second, the effects of the pandemic may differ for different time periods. While the initial response of the public may have been to rally around the authorities, trust may have begun to decrease in the later phases of the pandemic as fatigue emerged. Consistent with this, SI Appendix, Fig. S5 tracks developments in the indicators of discontent over time, and it is visually clear that many of the indicators trend toward greater discontent toward the end of the study period.
It is also important to highlight limitations in current discussions about pandemic fatigue. As we have argued, it is important to move beyond the WHO’s initial equation of pandemic fatigue with demotivation and instead conceptualize, and empirically assess, pandemic fatigue as a reflection of the perceived costs of compliance. While pandemic fatigue may lead to reduced motivation as a coping mechanism (see ref. 7 for evidence), motivation is best viewed as a distinct concept that may be high or low as exhaustion emerges due to the costs of compliance. This conceptual confusion in prior discussions is paralleled by the lack of convergence on a single widely used instrument for assessing subjective feelings of pandemic fatigue. Such convergence would benefit future research through more conceptual clarity and more precise measurement and, in this regard, we acknowledge a need to move beyond our one-item measure (see e.g., ref. 7). It is also important to acknowledge that while the present study suggests that feelings of pandemic fatigue emerge in response to the use of public and social measures against infection spread, the findings need to be interpreted with care. For example, against initial concerns that fatigue would emerge rapidly (13), our results suggest that pandemic fatigue emerges slowly. Holding stringency and restrictions constant, half a year of the pandemic only increased fatigue with around 5% points. Furthermore, our measure of the stringency of interventions is oriented toward the most costly interventions such as stay-at-home orders. Other evidence suggests that less costly measures, such as mask wearing, are less likely to induce fatigue (26). Similarly, it is possible that voluntary compliance with well-communicated health advice may be less exhausting than compliance with strict mandates. Finally, in drawing policy responses from the present findings, it is important to be aware that the analyses of the real-world associations between fatigue and policies are likely to be more complex than modeled here. For example, stringency will exert both direct and indirect effects on fatigue, as a stringent response in the presence may decrease the epidemic severity and therefore, potentially, the stringency of the policy response in future. In this way, future fatigue may at times be best reduced by a swift response in the present. Given this, the main policy implication is to be mindful of the costs of policies, especially as these costs accumulate over time.
These caveats notwithstanding, the results suggest that pandemic fatigue has negative consequences even beyond undermining adherence to restrictions, which has been health authorities’ primary focus until now. Because pandemic fatigue spurs antiestablishment views, fatigue may also erode the long-term possibility of efficient crisis management. For example, prior research finds trust in authorities and the political system to be the most important factors behind the acceptance of COVID-19 vaccines (44, 45). Pandemic fatigue could make it more difficult to mobilize support for vaccinations, triggering a vicious cycle, wherein slow vaccination uptake prolongs restrictions, which in turn increase fatigue and thus further slow down vaccination uptake. Importantly, however, the results also show that fatigue decreases when the severity of the national epidemic increases. When the need for interventions is most obvious, the interventions feel least burdening. This shows that restrictions imposed for perceived legitimate reasons will have less negative impact on well-being. Furthermore, it suggests that pandemic fatigue can be buffered if the public understands and accepts the meaningfulness of strict epidemic control, for example, by emphasizing the importance of such control for the vulnerable (46). By extension, pandemic fatigue can also be viewed as an indicator of inadequate and ineffective risk communication and management from the side of authorities and politicians.
Finally, these findings add to increasing concerns about the future stability of many Western democracies (1). When the COVID-19 pandemic hit the Western world in March 2020, stability was already strained by increasing inequality, cultural wars, and the financial crisis. The effect of pandemic fatigue on antiestablishment views suggests that the pandemic is likely to deepen such cleavages and erode stability further, adding to the challenges of the coming years. These challenges may be particularly pertinent as other crises—such as the climate crisis—will also require interventions that significantly impact people’s private lives and, therefore, may potentially elicit similar adverse reactions as those observed during the COVID-19 pandemic. For these reasons, it is of crucial importance to establish further evidence-based insights on how to use communication and support programs to most effectively buffer against feelings of fatigue caused by public interventions.
Supplementary Material
Appendix 01 (PDF)
Acknowledgments
This research has been supported by the Carlsberg Foundation’s grant CF20-0044 awarded to M.B.P.
Author contributions
F.J., A.B., and M.B.P. designed research; F.J., A.B., M.F.L., and M.B.P. performed research; F.J., A.B., M.S.R., M.F.L., and M.B.P. analyzed data; and F.J., A.B., M.S.R., M.F.L., and M.B.P. wrote the paper.
Competing interests
The authors declare no competing interest.
Footnotes
This article is a PNAS Direct Submission.
*In the main text, we analyze the association of country-level factors and pandemic fatigue and the association of fatigue and political discontent. Given statistical concerns about mediation models (47), we refrain from employing those in the main text. However, in SI Appendix, Table S13, we report models of the full path from country-level factors over pandemic fatigue to discontent. In SI Appendix, Table S14, we provide alternative models as well as sensitivity analyses. Overall, the analyses reveal small mediation effects that are likely to be sensitive to violations of key assumptions of causality. However, it should be noted that the panel analyses suggest that the relationship between fatigue and discontent is indeed causal.
Data, Materials, and Software Availability
Survey data have been deposited in Open Science Framework (https://osf.io/ax6zv/).
Supporting Information
References
- 1.Turchin P., Ages of discord: A Structural-Demographic Analysis of American History (Beresta Books, Chaplin Connecticut, 2016). [Google Scholar]
- 2.Petersen M. B., Osmundsen M., Bor A. “Beyond populism: the psychology of status-seeking and extreme political discontent” in The Psychology of Populism: The Tribal Challenge to Liberal Democracy, Forgas J. P., Crano W. D., Fiedler K., Eds. (Routledge, 2021), pp. 62–80. [Google Scholar]
- 3.Bartusevičius H., Bor A., Jørgensen F., Petersen M. B., The Psychological burden of the COVID-19 pandemic is associated with antisystemic attitudes and political violence. Psycholog. Sci. 32, 1391–1403 (2021). [DOI] [PubMed] [Google Scholar]
- 4.Zarocostas J., How to fight an infodemic. Lancet 395, 676 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Obradović S., Power S. A., Sheehy-Skeffington J., Understanding the psychological appeal of populism. Curr. Opin. Psychol. 35, 125–131 (2020). [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization, Pandemic fatigue: reinvigorating the public to prevent COVID-19: Policy framework for supporting pandemic prevention and management: Revised version November 2020 (Technical report, World Health Organization, Regional Office for Europe, 2020). [Google Scholar]
- 7.Lilleholt L., Zettler I., Betsch C., Böhm R., Pandemic fatigue: measurement, correlates, and consequences. PsyArxiv [Preprint] (2020). https://psyarxiv.com/10.31234/osf.io/2xvbr (Accessed 2 November 2022).
- 8.Michie S., West R., Harvey N., The concept of “fatigue” in tackling covid-19. BMJ 371, m4171 (2020). [DOI] [PubMed] [Google Scholar]
- 9.Passini S., Different ways of being authoritarian: The distinct effects of authoritarian dimensions on values and prejudice. Political Psychol. 38, 73–86 (2017). [Google Scholar]
- 10.Bromme R., Mede N. G., Thomm E., Kremer B., Ziegler R., An anchor in troubled times: Trust in science before and within the COVID-19 pandemic. PloS One 17, e0262823 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Foa R. S., et al. , The Great Reset: Public Opinion, Populism, and the Pandemic (Centre for the Future of Democracy, Cambridge, United Kingdom, 2022). [Google Scholar]
- 12.Haktanir A., Can N., Seki T., Kurnaz M. F., Dilmaç B., Do we experience pandemic fatigue? Current state, predictors, and prevention. Curr. Psychol. 41, 7314–7325 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harvey N., Behavioral fatigue: Real phenomenon, naïve construct, or policy contrivance? Frontiers in Psychol. 11, 2960 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reicher S., Drury J., Pandemic fatigue? How adherence to covid-19 regulations has been misrepresented and why it matters. BMJ 372, n137 (2021). [DOI] [PubMed] [Google Scholar]
- 15.Christodoulou C., “The assessment and measurement of fatigue” in Fatigue as a Window to the Brain, DeLuca J., Ed. (MIT Press, 2005), pp. 19–35. [Google Scholar]
- 16.Figley C. R., “Compassion fatigue: Toward a new understanding of the costs of caring” in Secondary Traumatic Stress: Self-Care Issues for Clinicians, Researchers, and Educators, Stamm B. H., Ed. (The Sidran Press, 1995), pp. 3–28. [Google Scholar]
- 17.Ford J. L., Ivancic S. R., Surviving organizational tolerance of sexual harassment: An exploration of resilience, vulnerability, and harassment fatigue. J. Appl. Commun. Res. 48, 186–206 (2020). [Google Scholar]
- 18.Hwang T. J., Rabheru K., Peisah C., Reichman W., Ikeda M., Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatrics 32, 1217–1220 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palgi Y., et al. , The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affective Disord. 275, 109–111 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Groarke J. M., et al. , Loneliness in the uk during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. PloS One 15, e0239698 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harper C. A., Satchell L. P., Fido D., Latzman R. D., Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Mental Health Addict. 19, 1875–1888 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jørgensen F., Bor A., Petersen M. B., Compliance without fear: Individual-level protective behaviour during the first wave of the COVID-19 pandemic. British J. Health Psychol. 26, 679–696 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Betsch C., Böhm R., Chapman G. B., Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav. Brain Sci. 2, 61–73 (2015). [Google Scholar]
- 24.Cowling B. J., et al. , Community psychological and behavioral responses through the first wave of the 2009 influenza A (H1N1) pandemic in Hong Kong. J. Infect. Dis. 202, 867–876 (2010). [DOI] [PubMed] [Google Scholar]
- 25.Goldstein P., Yeyati E. L., Sartorio L., Lockdown fatigue: The diminishing effects of quarantines on the spread of COVID-19. (CID Working Paper Series, Harvard University Cambridge, MA, 2021). [Google Scholar]
- 26.Petherick A., et al. , A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat. Human Behav. 5, 1145–1160 (2021). [DOI] [PubMed] [Google Scholar]
- 27.Yıldırım M., Solmaz F., COVID-19 burnout, COVID-19 stress and resilience: Initial psychometric properties of COVID-19 burnout scale. Death Stud. 46, 524–532 (2022). [DOI] [PubMed] [Google Scholar]
- 28.Ford J. L., Douglas M., Barrett A. K., The role of pandemic fatigue in seeking and avoiding information on COVID-19 among young adults. Health Commun., 10.1080/10410236.2022.2069211 (2022). [DOI] [PubMed]
- 29.Taylor S., Rachor G. S., Asmundson G. J., Who develops pandemic fatigue? medRxiv [Preprint] (2022). https://www.medrxiv.org/https://doi.org/10.1101/2022.01.24.22269786 (Accessed 2 November 2022).
- 30.Capelos T., Katsanidou A., Reactionary politics: Explaining the psychological roots of anti preferences in european integration and immigration debates. Polit. Psychol. 39, 1271–1288 (2018). [Google Scholar]
- 31.Osmundsen M., Bor A., Vahlstrup P. B., Bechmann A., Petersen M. B., Partisan polarization is the primary psychological motivation behind political fake news sharing on Twitter. Am. Polit. Sci. Rev. 115, 999–1015 (2021). [Google Scholar]
- 32.Berggren E., Neergaard A., “Populism: Protest, democratic challenge and right-wing extremism” in International Migration and Ethnic Relations, (Routledge, 2015), pp. 187–217. [Google Scholar]
- 33.Selçuk O., Strong presidents and weak institutions: populism in Turkey, Venezuela and Ecuador. Southeast Eur. Black Sea Stud. 16, 571–589 (2016). [Google Scholar]
- 34.Clemmensen C., Petersen M. B., Sørensen T. I., Will the COVID-19 pandemic worsen the Obesity epidemic? Nat. Rev. Endocrinol. 16, 469–470 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laskowski-Jones L., COVID-19 and changing social norms. Nursing 50, 6 (2020). [DOI] [PubMed] [Google Scholar]
- 36.Bor A., Jørgensen F., Lindholt M. F., Petersen M. B., Moralizing the COVID-19 Pandemic: Self-interest Predicts Moral Condemnation of Other’s Compliance, Distancing, and Vaccination (Political Psychology Early View, 2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nitschke J. P., et al. , Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. British J. Health Psychol. 26, 553–569 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mutz D. C., Status threat, not economic hardship, explains the 2016 presidential vote. Proc. Nat. Acad. Sci. U.S.A. 115, E4330–E4339 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jørgensen F., Bor A., Lindholt M. F., and Petersen M. B., Study 1. Open Science Framework. https://osf.io/ax6zv/. Deposited 24 June 2022.
- 40.Bor A., Jørgensen F., and Petersen M. B., Study 2. Open Science Framework. https://osf.io/ax6zv/. Deposited 13 June 2022.
- 41.Hale T. , et al. , A global panel database of pandemic policies (Oxford COVID-19 government response tracker). Nat. Human Behav. 5, 529–538 (2021). [DOI] [PubMed] [Google Scholar]
- 42.Gelman A., Scaling regression inputs by dividing by two standard deviations. Stat. Med. 27, 2865–2873 (2008). [DOI] [PubMed] [Google Scholar]
- 43.Angrist J. D., Pischke J. S., Mostly Harmless Econometrics (Princeton University Press, 2008). [Google Scholar]
- 44.Lindholt M. F., Jørgensen F., Bor A., Petersen M. B., Public acceptance of COVID-19 vaccines: Cross-national evidence on levels and individual-level predictors using observational data. BMJ Open 11, e048172 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Petersen M. B., Bor A., Jørgensen F., Lindholt M. F., Transparent communication about negative features of COVID-19 vaccines decreases acceptance but increases trust. Proc. Nat. Acad. Sci. U.S.A. 118, e2024597118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pfattheicher S., Nockur L., Böhm R., Sassenrath C., Petersen M. B., The emotional path to action: Empathy promotes physical distancing and wearing of face masks during the COVID-19 pandemic. Psychol. Sci. 31, 1363–1373 (2020). [DOI] [PubMed] [Google Scholar]
- 47.J. G- Bullock, Green D. P., Ha S. E., Yes, But what’s the mechanism? (Don’t expect an easy answer). J. Pers. Soc. Psychol. 98, 550–558 (2010). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 01 (PDF)
Data Availability Statement
Survey data have been deposited in Open Science Framework (https://osf.io/ax6zv/).