Abstract
Hong Kong has implemented stringent public health and social measures (PHSMs) to curb each of the four COVID-19 epidemic waves since January 2020. The third wave between July and September 2020 was brought under control within 2 m, while the fourth wave starting from the end of October 2020 has taken longer to bring under control and lasted at least 5 mo. Here, we report the pandemic fatigue as one of the potential reasons for the reduced impact of PHSMs on transmission in the fourth wave. We contacted either 500 or 1,000 local residents through weekly random-digit dialing of landlines and mobile telephones from May 2020 to February 2021. We analyze the epidemiological impact of pandemic fatigue by using the large and detailed cross-sectional telephone surveys to quantify risk perception and self-reported protective behaviors and mathematical models to incorporate population protective behaviors. Our retrospective prediction suggests that an increase of 100 daily new reported cases would lead to 6.60% (95% CI: 4.03, 9.17) more people worrying about being infected, increase 3.77% (95% CI: 2.46, 5.09) more people to avoid social gatherings, and reduce the weekly mean reproduction number by 0.32 (95% CI: 0.20, 0.44). Accordingly, the fourth wave would have been 14% (95% CI%: −53%, 81%) smaller if not for pandemic fatigue. This indicates the important role of mitigating pandemic fatigue in maintaining population protective behaviors for controlling COVID-19.
Keywords: pandemic fatigue, COVID-19, mathematical model
The COVID-19 pandemic has caused significant health, social, and economic burdens globally. In response, many countries enacted public health and social measures (PHSMs), which has led to the loss of employment, education, and exercise opportunities and the disruption of other important social and cultural activities (1). Pandemic fatigue is a natural response to a prolonged public health crisis due to the complex interplay of cultural and social factors (e.g., the risk perception of threats) (2). Although its precise meaning and scope remain up for controversy, pandemic fatigue usually refers to psychological fatigue as involving feelings of tiredness and physical and mental exhaustion (3, 4). The outcome of pandemic fatigue of COVID-19 would be a reduced motivation or ability to comply with protective behaviors (3).
Hong Kong has implemented stringent PHSMs to curb four COVID-19 epidemic waves from January 2020 to April 2021. Although the third wave between July and September was brought under control within 2 mo, the fourth wave starting from the end of October 2020 took more than 5 mo to be contained. Emergence of pandemic fatigue is one of the potential reasons for the reduced effectiveness of PHSMs on controlling COVID-19 transmission in Hong Kong’s fourth wave (5).
To understand the changing patterns of Hong Kong residents’ risk perception and compliance with protective policies and the impact on local COVID-19 transmission, we conducted 40 rounds of weekly cross-sectional telephone surveys from May 2020 to February 2021. More than 31,000 local adult residents were interviewed by these surveys. These large-scale data provide an opportunity to quantify the changing patterns in risk perception and its impact on population protective behaviors. We used the coupled disease–behavior framework to analyze the chain reactions from Risk perceptions to Protective behaviors to COVID-19 Transmission and to Public reports, abbreviated as the RPT-P framework.
Results
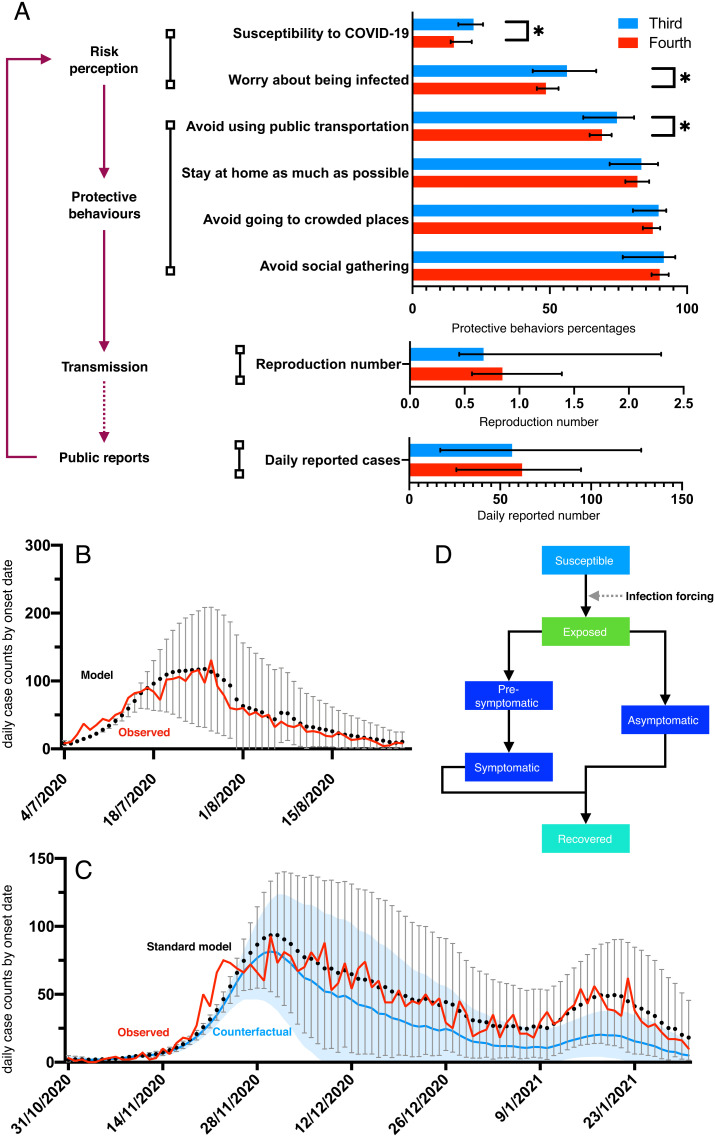
We first summarized the changing patterns in risk perceptions and self-reported behaviors using the RPT-P framework (Fig. 1). By checking survey results in the fourth wave and in the third wave, on average, 7.2% (the decrease of susceptibility to COVID-19) to 7.7% (the decrease of worry about being infected) fewer surveyed participants perceived the risk of infection (according to the two indicators of “risk perception” in Fig. 1A), and on average, 1.5% (the decrease of avoid social gathering) to 5.5% (the decrease of avoid using public transportation) fewer participants followed physical distancing policies (according to the four indicators of “protective behaviors” in Fig. 1A) during the fourth wave. These indicators of increasing pandemic fatigue in the fourth wave were associated with a 25% increment in the weekly mean reproduction number for the fourth wave with respect to the third wave (Fig. 1).
Fig. 1.
Coupled disease–behavior analysis of the risk perceptions, protective behaviors, COVID-19 transmission, and public case reports suggests the emergence of pandemic fatigue in Hong Kong’s fourth COVID-19 wave (end of October 2020 to January 2021). (A) Coupled disease–behavior framework. The Left panel indicates the interactions among risk perceptions, protective behaviors, transmission, and public case reports. The Right panel shows the percentages of participants who perceived a higher level of infection risk and who followed the guidance to take protective behaviors as estimated from our cross-sectional survey, the weekly mean reproduction numbers of SARS-CoV-2, and the number of daily reported cases for the third and fourth waves in Hong Kong. Colored horizontal bars and black error bars indicate the median and 95% credible interval (CrI), respectively. The asterisk indicates the rejection of equal medians for the third wave versus the fourth wave at the 5% significance level using the two-sided Wilcoxon rank sum test (6). (B–D) Reconstruction of the third and fourth waves of COVID-19 in Hong Kong. Using an epidemic model that incorporates the weekly survey data and Google’s real-time population mobility data, we projected the daily time series of the observed data by tracking the new symptomatic cases (SI Appendix, Epidemic Model). Red curves indicate the observed daily counts of new symptomatic cases, according to the data from the Centre for Health Protection in Hong Kong. Black dots and gray error bars indicate the median and 95% CrI of our reconstructed daily time series of new cases who developed symptoms. (B) Results for the third wave from early July to the end of August 2020. (C) Results for the fourth wave. Our standard model incorporating the transmission forcing adjusted by data of population protective behaviors (black dots and gray bars) is well fitted to the observed data (red curves) in (B) and (C), informed by the respective data in the third and fourth waves. In (C), using the fitted relationship between the transmission forcing and protective behaviors for the fourth wave, our counterfactual scenario assuming a 5% increase in the proportion of population avoiding social gathering per day (blue curve and shaded region) suggests that mitigating pandemic fatigue can substantially reduce the number of new cases after the peak of the fourth wave at around the end of November 2020. (D) Structure of the epidemic model (details in SI Appendix).
We next explored the interactive relationships among the four key factors of the RPT-P framework that may drive the community transmission of the COVID-19, including risk perceptions, self-reported protective behaviors, epidemic transmission, and public reports. We used the structural equation modeling approach to unravel the relationship path among these factors, including risk perception, self-reported protective behaviors, transmission, and public reports (Fig. 1). Furthermore, our linear regression using each indicator of four factors in RPT-P to predict the weekly mean reproduction number suggests that on average an increase of 100 daily new reported cases (0.0133‰ of population, 2.82% increase in the epidemic size of the fourth wave) will lead to 6.60% (95% CI: 4.03, 9.17) more people worrying about being infected, 3.77% (95% CI: 2.46, 5.09) more people avoiding social gatherings, and the weekly mean reproduction number reduced by 0.32 (95% CI: 0.20, 0.44). Our main analysis assumes a linear relationship between the number of daily new reported cases and risk perceptions. We also conducted a sensitivity analysis using the natural logarithm for the number of daily new reported cases. This sensitivity analysis suggests a lower degree of determination (adjusted R2). For example, the adjusted R2 is 0.40 (and 0.34) for the linear (and logistic) regression between the number of daily new reported cases and the risk perception of worry about being infected, respectively.
Based on the changing proportions of protective behaviors, the “avoidance of social gathering” has the highest adjusted R2 to explain the real-time reproduction number in Hong Kong (0.43). Therefore, the avoidance of social gathering is expected to be an essential element for modeling COVID-19 transmission in Hong Kong. Our epidemic model with transmission forcing adjusted by the daily change in the avoidance of social gathering can now cast the local incidence curve of symptomatic cases (Fig. 1). Furthermore, 1.7% (i.e., the ratio of the median value between the third and fourth waves) and 6.3% (i.e., the ratio between the upper limit value of 95% credible interval in the third wave and the median value in the fourth wave) increases in the percentage of people avoiding social gathering per day would reduce the final size of the fourth wave from October, 31 2020 to January, 15 2021 by 14% (95% CI%: −53%, 81%) and 39% (95% CI: −11%, 90%), respectively.
Discussion
Informed by weekly cross-sectional telephone surveys, our results indicate signs of pandemic fatigue in Hong Kong by measuring public responses to pandemic interventions. The observed problem of pandemic fatigue suggests that the population compliance with public health advice can decline when multiple waves repeatedly emerge within a short time period and pandemic fatigue might be contagious and spreading without detection in countries without capacities to rapidly detect new outbreaks.
Our results are consistent with the reports of pandemic fatigue in other regions during 2020. Based on a large-scale survey of 238,797 adults in 2020, the emergence of pandemic fatigue has been observed in 14 countries (7). Many factors other than those analyzed in this study may also contribute to the emergence of pandemic fatigue, and it is crucial to identify efficient measures that can mitigate pandemic fatigue. To maintain a high level of population risk perception to the COVID-19 and reduce the pandemic fatigue, concise and respectful communication with the general public together with a feasible execution plan would be helpful (1). The general public may have higher incentives to follow governmental policies if they can receive financial support or monetary incentives instead of penalties (8, 9), suggesting that the pandemic fatigue can be mitigated if policymakers can invest more to understand the difficulties and needs of the general public (1, 10).
Our study has several limitations. First, although we analyzed the self-reported behaviors and did not validate this against actual behaviors, self-reported surveys have been widely used to study human behaviors such as contact patterns (11) and hospital attendance (12). Second, other social activities may affect the risk perception and protective behaviors. Prolonged financial stress due to job loss and mask costs and distrust of the government’s policies such as the slow rollout of vaccination schemes may also contribute to the emergence of pandemic fatigue in the fourth wave. Our specific findings on pandemic fatigue were based on the surveys for adults, which may not be applicable to children. Further research and surveys can be carried out by considering the unit of pandemic fatigue as a family unit, including both adults and children within the same household.
Materials and Methods
In this study, we contacted more than 31,000 local residents in Hong Kong through these 40 cross-sectional telephone surveys from May 2020 to February 2021 (SI Appendix). We analyze the epidemiological impact of pandemic fatigue to quantify risk perception and self-reported protective behaviors and mathematical models.
This study involves human participants who gave informed consent to participate. This study has been approved by the Institutional Review Board (IRB) of The University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB) (UW 20-095).
Supplementary Material
Appendix 01 (PDF)
Acknowledgments
We acknowledge the financial support from the AIR@InnoHK administered by the Innovation and Technology Commission of the Research Grants Council of the Hong Kong SAR Government, and the Collaborative Research Scheme of the Research Grants Council of the Hong Kong SAR Government (Project No. C7123-20G). We thank Dr. Qi Tan for technical support. Codes are available in a GitHub repository (github.com/ZhanweiDU/Fatigue).
Author contributions
Z.D., S.S., and B.J.C. designed research; Z.D., and L.W. performed research; Z.D., and L.W. contributed new reagents/analytic tools; Z.D., L.W., S.S., D.L., T.K.T., J.X., H.G., B.Y., S.T.A., S.P., I.C.-H.F., E.H.Y.L., Q.L., P.W., L.A.M., G.M.L., and B.J.C. analyzed data; and Z.D., L.W., L.A.M., and B.J.C. wrote the paper.
Competing interests
G.M.L., and B.J.C., were supported by the AIR@innoHK program of the Innovation and Technology Commission of the Hong Kong SAR Government. B.J.C. reports honoraria from AstraZeneca, Fosun Pharma, Sanofi Pasteur, GSK, Moderna, and Roche. The authors declare no other potential conflicts of interest.
Data, Materials, and Software Availability
All study data are included in the article and/or SI Appendix.
Change History
November 30, 2022: Due to a production error, the SI Appendix appeared incorrectly. The SI Appendix has been updated.
Supporting Information
References
- 1.“Pandemic fatigue - Reinvigorating the public to prevent COVID-19” (WHO/EURO Tech. Rep. Series No. 2020-1160-40906-55390, 2021). [Google Scholar]
- 2.Masten A. S., Motti-Stefanidi F., Multisystem resilience for children and youth in disaster: Reflections in the context of COVID-19. Advers. Resil. Sci. 1, 95–106 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michie S., West R., Harvey N., The concept of "fatigue" in tackling covid-19. BMJ 371, m4171 (2020). [DOI] [PubMed] [Google Scholar]
- 4.Lee K. A., Hicks G., Nino-Murcia G., Validity and reliability of a scale to assess fatigue. Psychiatry Res. 36, 291–298 (1991). [DOI] [PubMed] [Google Scholar]
- 5.Government of the Hong Kong Special Administrative Region, HK determined to beat COVID-19. (2020). news.gov.hk (Accessed 28 April 2021).
- 6.Gibbons J. D., Chakraborti S., Nonparametric Statistical Inference (CRC Press, 2020). [Google Scholar]
- 7.Petherick A., et al. , A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat. Hum. Behav. 5, 1145–1160 (2021). [DOI] [PubMed] [Google Scholar]
- 8.Campos-Mercade P., et al. , Monetary incentives increase COVID-19 vaccinations. Science 374, 879–882 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmelz K., Enforcement may crowd out voluntary support for COVID-19 policies, especially where trust in government is weak and in a liberal society. Proc. Natl. Acad. Sci. U.S.A. 118, e2016385118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao C., Liu J., Network-based modeling for characterizing human collective behaviors during extreme events. IEEE Trans. Syst. Man Cybern. 47, 171–183 (2017). [Google Scholar]
- 11.Mossong J., et al. , Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 5, e74 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hegde S. T., et al. , Using healthcare-seeking behaviour to estimate the number of Nipah outbreaks missed by hospital-based surveillance in Bangladesh. Int. J. Epidemiol. 48, 1219–1227 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 01 (PDF)
Data Availability Statement
All study data are included in the article and/or SI Appendix.