Abstract
Myofibroblasts escape apoptosis and proliferate abnormally under pathological conditions, especially fibrosis; they synthesize and secrete a large amount of extracellular matrix (ECM), such as α-SMA and collagen, which leads to the distortion of organ parenchyma structure, an imbalance in collagen deposition and degradation, and the replacement of parenchymal cells by fibrous connective tissues. Fibroblast to myofibroblast transition (FMT) is considered to be the main source of myofibroblasts. Therefore, it is crucial to explore the influencing factors regulating the process of FMT for the prevention, treatment, and diagnosis of FMT-related diseases. In recent years, non-coding RNAs, including microRNA, long non-coding RNAs, and circular RNAs, have attracted extensive attention from scientists due to their powerful regulatory functions, and they have been found to play a vital role in regulating FMT. In this review, we summarized ncRNAs which regulate FMT during fibrosis and found that they mainly regulated signaling pathways, including TGF-β/Smad, MAPK/P38/ERK/JNK, PI3K/AKT, and WNT/β-catenin. Furthermore, the expression of downstream transcription factors can be promoted or inhibited, indicating that ncRNAs have the potential to be a new therapeutic target for FMT-related diseases.
Keywords: fibroblast, myofibroblast, FMT, ncRNA, signaling pathways, fibrosis
1. Introduction
Fibroblasts are the major cellular components of connective tissues derived from mesodermal cells. They can secrete extracellular matrix proteins (collagen; non-collagenous glycoproteins such as fibronectin and laminin; proteoglycans) and matrix-degrading enzymes to maintain the homeostasis of the extracellular matrix, proliferating and migrating to wounds to deposit granulation tissue during tissue repair. Generally, cells that secrete the ECM protein, MMPS, TIMPs, and vimentin, but do not express α-SMA, are regarded as fibroblasts (vimentin+α-SMA−) [1].
Myofibroblasts do not generally exist in normal tissues but are distributed in injured, fibrotic, and cancer tissues. They can exert their functions by ① expressing α-SMA, ② secreting extracellular matrix/collagen, and ③ secreting integrin/cytokine (VEGF/PDGF/TGF-β). The sources of myofibroblasts are complex, involving resident fibroblasts, epithelial cells, endothelial cells, fibrocytes, pericytes, and macrophages [2]. Among these cell types, the differentiation from fibroblast to myofibroblast is considered to be the most important source of myofibroblasts. Myofibroblasts are generally regarded as fibronectin ED-A+α-SMA+ cells that secrete large amounts of type I collagen and produce matrix cross-linking enzymes. Under normal circumstances, myofibroblasts face three outcomes after completing their function: (1) inactivation and changing into low-activity fibroblasts, (2) becoming scar or aging cells, or (3) apoptosis, through which they are largely eliminated; however, in fibrosis and cancer, myofibroblasts escape apoptosis, continue to multiply, and ultimately cause irreversible damage [1].
FMT is a phenomenon that mainly occurs under pathological conditions and is considered to be the main pathological mechanism of fibrosis. This process goes through two steps: fibroblasts are first differentiated into proto-myofibroblasts containing stress fibers, and the latter turn into mature myofibroblasts containing stress fibers and α-SMA [3]. The causes of FMT can be broadly divided into two categories: physical factors and humoral factors. Physical factors include hypoxia [4], high glucose [5], tension [6], mechanical damage [7], etc. Humoral factors include the stimulation of cytokines, chemokines, growth factors, etc. After receiving these stimuli, the corresponding receptors on the surface of fibroblasts phosphorylate and transmit these signals into the cells through signaling pathways such as TGF-β/Smad, MAPK/P38/ERK/JNK, PI3K/AKT, and JAK/STAT [2], which initiate the expression of related genes and form the myofibroblast phenotype. ncRNAs have been reported to play an important role in the process of FMT. In this review, we summarize the ncRNAs regulating FMT (as shown in Supplementary Materials) and find that ncRNAs mainly affect TGF-β/Smad, MAPK/P38/ERK/JNK, PI3K/AKT, JAK/STAT, WNT/β-catenin, and other signaling pathways, and then promote or inhibit the expression of downstream transcription factors (as shown in Figure 1).
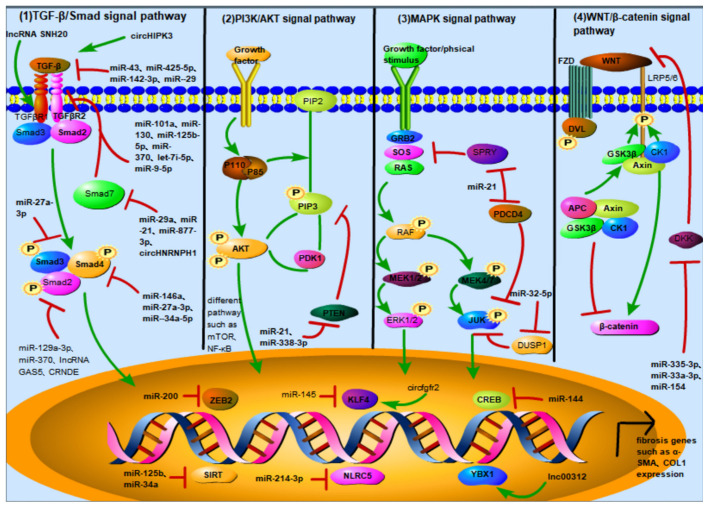
Figure 1.
Noncoding RNAs and their targets in different signaling pathways and nuclear transcription factors can affect FMT. (1) TGF-β/Smad signaling pathway: ncRNA can target TGF-β, TGF-βR family, and Smad family to regulate TGF-β/Smad and affect FMT progression. circHIPK3, miR-43, miR-425-5p, miR-142-3p, and miR-29b target TGF-β; miR-101a, miR-130, miR-let-7i-5p, miR-133a, and miR-125b-5p, and lncRNA SNHG20 target TGFβR Ⅰ; miR-30c, and miR-370 and miR-9-5p regulate TGFβR Ⅱ to affect TGF-β/Smad signal transduction; miR-23b-3p and miR-21 target TGFβR Ⅲ; miR-27a-3p targets Smad2; miR-370, lncRNA GAS5, and lncRNA CRNDE target Smad3; miR-146a and miR-27-3p target Smad4; miR-92a, miR-21, and miR-877-3p and circHNRNPH1 target Smad7. (2) PI3K/AKT signaling pathway: PTEN (phosphatase and tension homology deleted on chromosome ten) is an important protein regulating PI3K/AKT signaling pathway. It has lipid phosphatase activity and can dephosphorylate PIP3, the downstream target molecule of PI3K; miR-718, and miR-21 and miR-338-3p can directly target PTEN to regulate PI3K/AKT signaling pathway. (3) MAPK signaling pathway: ncRNA targets some proteins of the MAPK signaling pathway, such as PDCD4, DUSP1, and SPRY1, to regulate the FMT process; miR-32-5p can directly target DUSP1, and miR-21 can simultaneously target PDCD4 and SPRY1. (4) Wnt/β-catenin signaling pathway: Dickkopf-associated protein (DKK) is a secreted protein that can form a ternary complex with the transmembrane proteins KREMEN and LRP5/6 to promote the internalization of LRP5/6 and inhibit the binding of LRP5/6 to wnt, thereby inhibiting the Wnt/β-catenin signaling pathway; miR-33a-3p and miR-154 regulate Wnt/β-catenin signaling pathway by targeting DKK. (5) ncRNA regulates nuclear transcription factors and affects the expression of fibrotic genes: miR-200 targets the ZEB family; miR-125b and miR-34a targeted SIRT; miR-145 targets KLF4; miR-214-3p targets NLRC5; miR-144 targets CREB; and lncRNA 00312 targets YBX1.
2. Overview of Non-Coding RNA (ncRNA)
Among the numerous human genes, non-coding genes account for more than 90%, and a large amount of ncRNA is transcribed. More and more studies have shown that the expression dysregulation of ncRNA is related to a variety of diseases, and ncRNA is expected to become a diagnostic marker and prognostic indicator. There are many kinds of ncRNA, including small nuclear RNA (snRNA), small nucleolar RNA (snoRNA), piwi-interacting RNA (piRNA), small interfering RNA (siRNA), and others. MicroRNA (miRNA), long non-coding RNA (lncRNA), and circular RNA (circRNA) have become the focus of research due to their formidable regulatory capacity.
miRNAs, first identified in the 1990s, originate from genomic introns or exons and are transcribed into the primary transcription of miRNA (pri-miRNAs) under the action of RNA polymerase. In the nucleus, pri-miRNAs are cleaved into pre-miRNAs under the control of Drosha and DGCR8. Pre-miRNAs are subsequently exported to the cytosol by exportin and cleaved into small double-stranded RNAs (dsRNAs) by the Dicer. Finally, dsRNAs bind to Ago2, forming an RNA-induced silencing complex (RISC), and they finally become mature endogenous non-coding single-stranded RNA (18–24 nucleotides in length). miRNAs directly degrade or inhibit target mRNA by complete or incomplete pairing with the 3′ untranslated region (3′UTR) of target mRNA so as to regulate the expression of transcribed genes. Approximately 30% of genes in the human genome are regulated by them [8,9].
lncRNA is a class of endogenous RNA that is more than 200 nucleotides in length but cannot encode proteins due to the lack of a long enough open reading frame [10]. lncRNA contains a 5′-terminal 7-methylguanosine cap (m7G) and a 3′-terminal polyadenylate (poly) tail, so it is easily degraded. lncRNA is transcribed from genomes and is divided into intronic lncRNA, intergenic lncRNA, and antisense lncRNA. It can function in the following ways: ① by remodeling chromatin state, ② by stabilizing proteins or protein complexes, or ③ by acting as competing endogenous RNAs (ceRNA) to regulate gene expression [11]. Due to the development of proteomics and ribosome mapping technology, a small number of lncRNAs have been found to be translated into small molecule peptides through ① CAP-dependent, ② IRES-dependent, ③ M6A-dependent, and ④ SORF-dependent methods, and they play a role in various disease through different mechanisms [12].
circRNA, first identified in plants in 1976 [13], is an endogenous single-stranded circular non-coding RNA with a length from several hundred to several thousand nucleotides derived from pre-mRNA or lncRNA [14,15]. Different from the classical alternative splicing of linear RNA, pre-mRNA undergo reverse splicing during the process of maturation. The 5′ and 3′ ends of pre-mRNA are connected in covalently closed loops to form circRNAs. Circular RNA can resist the degradation of exonuclease precisely because it lacks the free ends of 5′ methyl guanosine and a 3′ poly A tail, which also results in a longer half-life and higher stability than linear RNA [16]. Approximately 30% of circRNAs are conserved among various species, with specific expression in different tissues and pathological stages [17]. circRNAs can be divided into three types according to their components: exonic circRNAs (ecRNA), intronic circRNAs (ciRNA), and exon-intronic circRNAs (eliRNA), among which ecRNA is mostly localized in the cytosol, while ciRNA and eliRNA are localized in the nucleus [18]. circRNA can function in the following ways: ① as an miRNA sponge, ② as an RBP sponge, ③ as a protein scaffold to recruit protein regulation gene transcription and splicing, ④ by being translated into a protein and ⑤ by being secreted into the peripheral blood by exosomes as potential biomarkers [19].
It is worth noting that the mode of action for lncRNA and circRNA is limited by their location. Generally speaking, they are located in the nucleus to act as protein sponges or protein scaffolds directly, while they are located in the cytoplasm by binding to miRNAs, which in turn promotes downstream gene expression. Therefore, when discovering new lncRNA and circRNA, it is important to first focus on their localization in the cell.
3. ncRNA Activates or Inhibits Different Signaling Pathways to Regulate FMT
3.1. TGF-β/Smad Signaling Pathway
The TGF-β/Smad signaling pathway is recognized as a signal pathway of fibrosis. It has been found that TGF-β1 is upregulated in the fibrosis of the liver, myocardium, lungs, and other organs and induces fibroblasts to differentiate into myofibroblasts through the TGF-β/Smad pathway. Its mechanism of action is as follows: TGF-β binds to TGFβR Ⅱ on fibroblasts, and TGFβR Ⅱ is activated and phosphorylates TGFβR Ⅰ. Phosphorylated TGFβR Ⅰ then phosphorylates downstream Smad2/3, and p-Smad2/3 bind to Smad4 and enter the nucleus as heterotrimers to regulate the transcription of fibrotic genes. This promotes phenotypic change in fibroblasts [20,21].
ncRNA in the TGF-β/Smad Pathway
TGF-β/Smad is the most well-known fibrosis signaling pathway by researchers. Multiple studies have shown that ncRNA can target TGF-β, TGFβR Ⅰ/Ⅱ/Ⅲ, and smad2/3/4/7 to regulate TGF-β/Smad and then affect the FMT process.
TGF-β as the downstream target of ncRNA
As the initiator protein of TGF-β/Smad signal transduction, the inhibition of TGF-β can regulate the activation of TGF-β/Smad from the source. circHIPK3 [22], miR-433 [23], miR-425-5p [24], miR-142-3p [25], and miR-29b [26] can regulate the expression of TGF-β to activate or inhibit the TGF-β/Smad signaling pathway. Among them, circHIPK3 and miR-29 have attracted extensive attention from researchers. In 2016, Jeck W R et al. used RNA sequencing analysis and found for the first time that circHIPK3 (has-circ-0000284) was massively expressed in human glans fibroblasts [27]. circHIPK3 has nine direct binding sites and 18 potential binding sites for miRNAs. This means that circHIPK3 can function by binding to different miRNAs [28]. The maternal gene of circHIPK3, HIPK3 (home domain interacting protein kinase 3), is located on human chromosome 11 and is a member of the HIPKs family, which is abundant in human tissues and has a high reverse cleavage rate [29]. The second exon of HIPK3 is more prone to 3′ and 5′ splicing at its canonical splicing site and is driven by the base complementary pairing of ALU repeats in its flanking intron to form circHIPK3. circHIPK3 plays a dual role in cancer [30] and a pro-fibrotic role in fibrotic diseases. In myocardial fibrosis induced by hypoxia, circHIPK3 promotes the expression of TGF-β2, activates TGF-β/Smad, and induces FMT through the competitive binding of miR-152-3p [22]. It also can induce FMT in other ways; for example, in TGF-β-induced pulmonary fibrosis, circHIPK3 ① enhances the expression of FOXK2 by competitively binding to miR-30-3p, promoting the glycolysis level of embryonic lung fibroblasts, induces FMT [31] and ② binds competitively to miR-338-3p, improving the expression of SOX4 and COL1A to induce FMT [32]. There are three members of the miR-29 family: miR-29a, miR-29b (miR-29b-1/miR-29b-2), and miR-29c. Among them, miR-29a is localized in the cytoplasm, while miR-29b/c is localized in the nucleus, which enables miR-29a/b/c to function in different ways [33]. The miR-29 coding gene is adjacent to the CD46/34 coding genes. miR-29a and miR-29b-1 are located in the q32.3 region of human chromosome 7, while miR-29b-2 and miR-29c are located in the q32.2 region of human chromosome 1 [34]. Different members of miR-29 all contain a seed sequence with a length of 7 nt, so their predicted target genes are highly overlapping; however, they each contain unique sequences and play different functions. miR-29 is not expressed or has a low expression in embryonic tissues but is widely expressed in mature tissues. A large number of studies have reported that miR-29 plays a dual role in tumor progression [35]. Its inhibitory effect on fibrosis should not be ignored. For example, Yuan R et al. found that miR-29a in the exosomes of human adipose-derived mesenchymal stem cells (hADSCs) could directly bind to TGF-β2 and inhibit the TGF-β/Smad signaling pathway, thereby inhibiting the formation of pathological scars [36]. lncRNA H19 can target miR-29b to regulate the activity of oral mucosal fibroblasts [37]. Yang J et al. constructed an in vitro silicosis cell model with miR-29c overexpression and inhibition and found that miR-29c could inhibit the SiO2-induced trans-differentiation of lung fibroblasts in vitro [38]. lncRNA TUG1 can competitively bind miR-29c to promote the hypoxia-induced FMT process of cardiac fibroblasts [39]. Thus, circHIPK3 and the miR-29 family are fibrosis therapeutic targets worthy of further study.
TGFβR as the downstream target of ncRNA
TGFβR Ⅰ and TGFβR Ⅱ are important receptor molecules in TGF-β/Smad signal transduction. The inhibition of TGFβR Ⅰ/TGFβR Ⅱ activity can inhibit the activation of the TGF-β/Smad signaling pathway. Previous studies have shown that miR-101a [40], miR-130 [41], miR-let-7i-5p [42], miR-133a [43], miR-125b-5p [44], and lncRNA SNHG20 [45] target TGFβR Ⅰ. miR-30c [46], miR-370 [47], and miR-9-5p [48] target TGFβR Ⅱ. miR-23b-3p [49] and miR-21 [50] target TGFβR Ⅲ. Among these, miR-let-7 has been thoroughly studied. miR-let-7, the first known miRNA in humans, was discovered in Caenorhabditis elegans in 2000. It is about 21 nucleotides in length, and its precursor molecule is a stem-loop folded structure with 70 nucleotides. The miR-let-7 family consists of 13 members, including let-7a, b, c, d, e, f, i, miR-98, and miR-202, which are located on nine different chromosomes [51]. Let7 family members are under-expressed at the embryonic stage but are increased in differentiated cells. Xu C et al. found that miR-let-7i-5p in the exosomes of human umbilical cord mesenchymal stem cells was found to target TGFβR Ⅰ on embryonic lung fibroblasts, the phosphorylation of TGFβR Ⅰ was blocked, the level of phosphorylated Smad3 was reduced, and the TGF-β/Smad signaling pathway was inhibited. The failure of embryonic lung fibroblasts to convert into myofibroblasts alleviates silico-induced silicosis [42].
Smads family as the downstream target of ncRNA
Smad2/3: Smad2/3 plays an indispensable role in the TGF-β/Smad signaling pathway as a downstream molecule that first responds to the TGFβR activation signal. The inhibition of Smad2/3 phosphorylation partially blocks the activation of the TGF-β/Smad pathway. miR-27a-3p [52] targets Smad2, and circAMD1 can competitively bind to miR-27a-3p to promote the proliferation and collagen synthesis of human dermal fibroblasts [53]. miR-370 [47], lncRNA GAS5 [54], and lncRNA CRNDE [55] target Smad3. miR-335-3p [56] targets Smad2/3 simultaneously. lncRNAs GAS5 and CRNDE have attracted the attention of many researchers. lncRNA GAS5, with a gene position of 1q25.1 and a length of 630nt, was first discovered in the stalled mouse fibroblast NIH3T3 [57]. lncRNA GAS5 plays an important role in the occurrence and development of tissue and organ fibrosis, but its role is twofold [58]. For example, in TGF-β-induced myocardial fibrosis and renal fibrosis, the expression of lncRNA GAS5 is decreased in myocardial fibroblasts and up-regulated in renal fibroblasts, playing inhibitory and promoting roles [59,60]. Tang R et al. found that lncRNA GAS5 was down-regulated in both TGF-beta- and bleomycin-treated skin fibroblasts and the overexpression of GAS5 inhibited the TGF-beta-induced activation of fibroblasts. The mechanism of action is as follows: lncRNA GAS5 directly binds to Smad3 and promotes the binding of Smad3 to protein phosphatase 1A (PPM1A) (a Smad3 de-phosphorylase), which dephosphorylates Smad3 and inhibits the activation of downstream pathways [54]. lncRNA GAS5 can also regulate the process of fibrosis through a variety of other pathways, which is a potential therapeutic target for fibrosis. CRNDE (muscle neoplasia differentially expressed), which is located on human chromosome 16 and has a length of 1059nt, plays a dual role in fibrotic disease. The knockdown of CRNDE expression in embryonic lung fibroblasts can alleviate the LPS-induced inflammatory response by inhibiting the phenotype change in embryonic lung fibroblasts [61]. Instead, the overexpression of CRNDE can alleviate synovial fibrosis in rats with osteoarthritis (OA) [62]. Zheng D et al. found that in myocardial fibrosis caused by diabetic cardiomyopathy, the expression of CRNDE was activated by Smad3 and was thus enriched in myocardial fibroblasts; however, increased CRNDE, in turn, inhibited the transcriptional activation of target genes by Smad3, thus inhibiting the differentiation of fibroblasts into myofibroblasts [55]. More studies are needed to elucidate the mechanism of action of CRNDE in FMT.
Smad4: As a central regulator of the TGF-β/Smad signaling pathway, the reduced phosphorylation of Smad4 leads to the inability of Smads to form effective complexes in the nucleus, thereby attenuating or interrupting TGF-β signaling. Both miR-146a [63] and miR-27-3p [64] can directly target Smad4 to regulate Smad4 expression and phosphorylation. miR-146, with a length of 20nt, is the first miRNA considered to regulate the immune system and has attracted the attention of researchers. There are two subtypes of miR-146a and miR-146b, which only have two nucleotide differences at the 3′ end. The former encoding gene is located in the second exon region of human chromosome 5, while the latter is located in the q24–26 region of human chromosome 10 [65]. In myocardial fibrosis caused by myocardial injury, the N-terminal peptide C0–C1f of the myocardial binding protein C can activate the NF-κB pathway through TLR4 to cause inflammation and delay TGF-β-induced fibroblast activation; miR-146 can inhibit the C0-C1f function [66]. These results suggest that miR-146 also plays an important role in fibrosis. Studies have found that the expression of miR-146a is up-regulated in the process of human skin FMT induced by TGF-β1. Bioinformatics predict that Smad4 is the downstream target of miR-146a. Real-time quantitative PCR and Western blot experiments have shown that miR-146a mimics can significantly down-regulate the expression of Smad4 and ultimately affect the generation of α-SMA in myofibroblast differentiation [63].
Smad7: Smad7 negatively regulates the TGF-β/Smad signaling pathway, which can competitively bind to Smad2/3 receptors and prevent Smad2/3 phosphorylation, thereby preventing TGF-β/Smad signaling pathway activation. miR-92a [67], miR-21 [68], miR-877-3p [69], and circHNRNPH1 [70] can affect the TGF-β/Smad signaling pathway by regulating the level of Smad7. In myocardial fibrosis after ischemia, circHNRNPH1 competitively binds to miR-216-5p, induces the expression of Smad7 to accelerate the degradation of TGF-β1, inhibits the migration of myofibroblasts and the expression of α-SMA and col-Ⅰ, and alleviates the progression of myocardial fibrosis.
3.2. PI3K/AKT Signaling Pathway
The PI3K/AKT signaling pathway is another important fibrotic pathway that plays an important role in a variety of fibrotic diseases. It has been reported that the PI3K/AKT signaling pathway is a key signaling node in idiopathic pulmonary fibrosis (IPF), and PI3K/AKT inhibitors can inhibit the progression of IPF, which has been verified in clinical trials [71]. Similarly, in oral submucosal fibrosis, PDGF can make oral mucosal fibroblasts differentiate into myofibroblasts through the PI3K/AKT signaling pathway [72]. Its mechanism of action is as follows: extracellular growth factors, such as fibroblast growth factor (FGF), vascular endothelial growth factor (VEGF), and insulin (INS), bind to the corresponding receptors on fibroblasts, activating the G-protein-coupled receptor or receptor complex protein kinase PTK signal, stimulating PI3K to translocate from the cytoplasm to the cell membrane. The activated PI3K catalyzes the phosphorylation of phosphatidylinositol 4.5-diphosphate (PI (4,5) P2) to generate PIP3. AKT and upstream inositol-3-phosphate-dependent protein kinase 1 (PDK1) interact with PIP3 through the PH domain of PI3K. PDK1 activates threonine phosphorylation at 308 within AKT to activate AKT. Phosphorylated AKT regulates the mammalian target of rapamycin (mTOR), hypoxia-inducible factor-1α (HIF-1α), and the reactive oxygen species (ROS) system, which are involved in the transcription of fibrotic genes, finally promoting the phenotypic change in fibroblasts.
ncRNA in the PI3K/AKT Pathway
Studies have shown that miR-718 [73], miR-29 [74], miR-126 [75], miR-21 [76], miR-338-3p [77], miR-503 [78], miR-424 [79], lncRNA N341773 [80], lncRNA PFAL [81], lncRNA GAS5 [82], etc., can affect the activation of the PI3K/AKT signaling pathway. Among them, PTEN (phosphate and tension homology deleted on chromosome ten) is a crucial protein regulating the PI3K/AKT signaling pathway. It has lipid phosphatase activity and can dephosphorylate PIP3: the downstream target molecule of PI3K. miR-718 [73], miR-21 [76], and miR-338-3p [77] can directly bind to PTEN, inhibit the expression of PTEN, reduce its inhibitory effect on PI3K/AKT, and promote the progression of fibrosis. miR-21 has been shown to be dysregulated in a variety of diseases. miR-21 is a microRNA with a length of 22 nucleotides that widely exists in eukaryotes. It is the most richly expressed miRNA in the body and also one of the earliest miRNAs discovered. The miR-21 encoding gene is located in the tenth intron region of the q23.2 region of human chromosome 17, close to the vacuole membrane protein 1 (VMP1) gene. The miR-21 sequence has an independent promoter region, and its precursor can initiate transcription autonomously and become mature miR-21. The sequence also contains conserved enhancer elements, including signal transducers and activators of transcription, enhancer-binding proteins, etc., which can improve the transcription level of miR-21. The binding of miR-21 and PTEN has been confirmed in a variety of cell lines. In hypertrophic scars and renal fibrosis, miR-21 induces fibroblasts to differentiate into myofibroblasts through the PTEN/AKT signaling pathway [76,83]. Studies by several teams have proved that lncRNA and circRNA can exert their physiological functions through the competitive binding of miR-21, such as lncRNA GAS5 [84] and circPTPN12 [85].
3.3. MAPK Signaling Pathway
In recent years, the role of the MAPK signaling pathway in fibrosis has attracted more and more researchers’ attention. MAPK, a mitogen-activated kinase that phosphorylates both serine/threonine and tyrosine, involves four distinct signaling pathways: ① Ras-Raf-MEK1/2-ERK1/2 ② the JNK cascade ③ the P38 cascade, and ④ the BMK1 (ERK5) cascade, all of which are protein kinase cascades in nature, including three core members: MAPK kinase kinase (MKKK), MAPK kinase (MKK), and MAPK; these three kinases that are activated sequentially regulate a variety of physiological/pathological processes. Among them, Ras-Raf-MEK1/2-ERK1/2 and the JNK cascade are the two most significant MAPK pathways. Cai Z et al. found that BMP4 regulates the proliferation, apoptosis, activation, and differentiation of fibroblasts by inhibiting the ERK/p38 MAPK signaling pathway [86], proving that the MAPK signaling pathway is also involved in the regulation of the fibrosis process. Its mechanism of action is as follows: extracellular growth factors, such as EGF and FGF, bind to and activate tyrosine kinase receptors, such as EGFR and FGFR, on the membrane of fibroblasts, and the latter binds to the adaptor protein GRB2 to recruit guanylate activating factors (SOS) to the cell membrane can convert RAS from inactive RAS-GDP to active RAS-GTP. The activated Raf kinase further binds to MEK1/2 and activates ERK1/2. ERK can enter the nucleus and phosphorylate FOS, MYC, SP1, and other transcription factors to regulate the activation and differentiation of fibroblasts. JNK has three subtypes: JNK1, 2, and 3. Stress signals, such as ultraviolet light, heat shock, cytokines, growth factors, and some G-protein-coupled receptors, can be transmitted to MAPKKK through the Rho subfamily (Rac, Rho), one of the RAS family small molecule G proteins and further activate MEK4/7 and JNK in turn. After activation, JNK can act on a variety of downstream transcription factors (JUN, ELK1, ETS2, etc.) and ultimately promote the expression of fibrosis-related genes.
ncRNA in the MAPK Pathway
miR-21 [87], miR-127-3p [88], miR-43 [23], miR-32-5p [89], miR-338-3p [90], miR-155 [91], miR-22 [92], miR-503 [78], lncRNA FENDRR [93], and circEP400 [94] can affect the activation of the MAPK signaling pathway and regulate the differentiation of fibroblasts into myofibroblasts. We found that most of these ncRNAs did not directly target molecules in the MAPK pathway but targeted some proteins regulating the MAPK signaling pathway, such as PDCD4, DUSP1, SPRY1, etc.
PDCD4 (programmed cell death factor 4) can inhibit JNK activity and c-jun phosphorylation and then inhibit the expression and phosphorylation of the eukaryotic translation initiation factor eIF4E. Liao Y.-W. et al. found that miR-21 was up-regulated and PDCD4 was down-regulated in activated oral submucosal fibroblasts. The Luciferase reporter assay proved that miR-21 and PDCD4 have binding sites, so miR-21 directly binds to PDCD4 and partially blocks the inhibitory effect of PDCD4 on JNK activity, thereby promoting the differentiation of oral fibroblasts into myofibroblasts [95].
DUSP1 (dual specificity phosphatases 1), a member of the mammalian protein kinase (MPK) family, is an important negative feedback regulator of the MAPK signal transduction pathway. DUSP1 has phosphatase activity, which mainly dephosphorylates activated MAPK family members, especially tyrosine and threonine phosphate groups in p38 MAPK kinase and JNK kinase, thereby inhibiting the activity of the MAPK pathway. Shen J. et al. treated cardiac fibroblasts with high glucose, and the expression of miR-32-5p was up-regulated, while DUSP1 was down-regulated. The Luciferase reporter assay demonstrated that miR-32-5p could directly target DUSP1, and the MAPK signaling pathway was activated, which promoted the activation and differentiation of cardiac fibroblasts [89].
Spry1 (Sprouty 1) can significantly inhibit the Raf-ERK1/2 and p38 MAPK pathways by inhibiting the phosphorylation of ERK and p38. The study of Li D. et al. showed that, after miR-21 knockdown, Ang-II-induced myofibroblast differentiation was partially inhibited, while the expression of Spry1 was significantly increased, which further inhibited the activation of ERK1/2, indicating that miR-21 could activate the MAPK signaling pathway by targeting Spry1 and finally regulate the fibroblast to myofibroblast transition [96].
In addition, another circRNA affecting the JNK/MAPK pathway is circFgfr2, which also attracted our attention. circFgfr2 is produced by the fibroblast growth factor 2 (FGF2) gene. circFgfr2 competitively binds miR-133 and then promotes the expression of the mitogen-activated protein kinase 20 (Map3k20) gene to activate the JNK/MAPK pathway during skeletal muscle development and myogenesis. The activation of the JNK/MAPK pathway inhibits the activation of the downstream target KLF4. KLF4 can bind to the promoter of circFgfr2 to further improve the expression of circFgfr2. Therefore, a negative feedback regulation loop is formed [97]. Since circFgfr2 can activate the JNK/MAPK pathway and regulate KLF4 expression, it is also likely to affect the FMT process.
3.4. Wnt/β-Catenin Signaling Pathway
Wnt/β-catenin signaling is a potentially momentous therapeutic target for a variety of fibrotic diseases. The study of Li X. et al. found that betulinic acid (an anti-tumor and antiviral drug) could inhibit bleomycin-induced pulmonary fibrosis by interfering with the Wnt/β-catenin signaling pathway and inhibiting the differentiation of fibroblasts into myofibroblasts in idiopathic pulmonary fibrosis [98]. The mechanism is as follows: Wnt protein binds to wnt receptors, such as Frizzled (Fz) and low-density lipoprotein receptor-associated proteins on fibroblasts, and can recruit the Dishevelled protein in the cytoplasm to inhibit the activity of the destruction complex (which ubiquitizes and degrades β-catenin) formed by glycogen synthesis kinase 3 (GSK3) and others. This enables β-catenin to accumulate and localize in the nucleus, bind to the TCF/LEF family of transcription factors, and initiate the transcription of downstream fibrotic genes.
ncRNA in the Wnt/β-Catenin Pathway
miR-126 [99], miR-33a-3p [100], miR-154 [101], miR-29c [102], miR-142-3p [25], miR-27a-3p [103,104], and lncRNA safe [105] can affect the activation of the WNT/β-catenin signaling pathway and regulate the differentiation of fibroblasts into myofibroblasts. Among them, both miR-33a-3p and miR-154 target DKK to regulate the Wnt/β-catenin signaling pathway. The Dickkopf-associated protein (DKK) is a secreted protein that can form a ternary complex with the transmembrane proteins KREMEN and LRP5/6 to promote the internalization of LRP5/6 and inhibit the binding of LRP5/6 to wnt, thereby inhibiting the Wnt/β-catenin signaling pathway. Henderson, J et al. transfected miR-33a-3p mimics into skin fibroblasts, and then detected the expression of DKK-1 by ELISA and found that miR-33a-3p could activate the Wnt/β-catenin signaling pathway by reducing the expression of DKK-1. Sun and Ly et al. found a direct correlation between miR-154 expression, DKK2 expression, and myofibroblast differentiation. They also demonstrated that miR-154 is directly bound to DKK2. Therefore, miR-154 can activate the Wnt/β-catenin signaling pathway by down-regulating the expression of DKK2 [101].
3.5. Other Signaling Pathways
3.5.1. JAK/STAT Signaling Pathway
Papaioannou I et al. found that STAT3 can bind to the COL1A2 gene simultaneously with JunB as an enhancer, recruit RNA polymerase to promote COL1A2 expression and regulate fibroblasts to differentiate into myofibroblasts [106]. Therefore, the JAK/STAT signaling pathway is involved in the FMT process. The mechanism is as follows: JAK is a non-receptor tyrosine kinase. When cytokines (e.g., IL-6, IFN-α/β), hormones, and growth factors (e.g., EGF, PDGF, IGF) bind to the corresponding receptors on fibroblasts (such receptors do not have kinase activity, but their intracellular segment has a binding site for tyrosine kinase JAK), the receptor becomes polymerized. JAK molecules bound to their intracellular segment can be close to each other and need to be phosphorylated to be activated. Activated JAK molecules can phosphorylate STATs, and the phosphorylated STATs undergo dimerization. STAT dimers enter the nucleus and bind to specific regulatory sequences, thus activating the transcription of fibrotic genes. STATs are then dephosphorylated and returned to the cytosol as a monomer waiting to participate in the next signal transduction. miR-210-5p can regulate the JAK/STAT signaling pathway and then regulate the FMT process. Wei, SY et al. found that miR-210-5p was upregulated in human dermal fibroblasts treated with TGF-β. By binding STAT5A and inhibiting its expression, the STAT3 signaling pathway was activated to promote the differentiation of human dermal fibroblasts into myofibroblasts [107].
3.5.2. Notch Signaling
Unlike the above pathways, the Notch signaling pathway is activated only when two cells come into contact with each other because its ligands and receptors are membrane proteins (the ligands of the above pathways are secreted proteins). Yue Z. et al. found that by blocking the Notch signaling pathway in myofibroblasts, the expression of the pro-apoptotic factors Ngfr and Septin4 were up-regulated, the apoptosis of myofibroblasts was accelerated, fibrosis was reversed, and the progression of liver fibrosis was inhibited [108]. Thus, the Notch signaling pathway also plays an indispensable role in fibrotic diseases. Its mechanism of action is as follows: when the Notch ligand and receptor of adjacent cells bind, the Notch protein is spliced three times under the action of integrin metalloproteinase 10 (ADAM10) and γ-secretase, and the active structure of NICD is detached from the Notch protein and released into the cytoplasm and then into the nucleus. It is combined with transcription repressor CSL to inhibit CSL activity and recruit the transcription activator protein family MAML to form an NICD–CSL–MAML ternary complex to promote the transcription of HES, HEY, and other transcription factors, which can promote the expression of downstream fibrotic genes. Several ncRNAs, such as miR-16-5p [109], miR-30d [110], miR-21 [111], and lncRNA HOTAIR [112], can regulate the Notch signaling pathway and affect the fibrosis process. miR-16-5p was down-regulated, and NOTCH2 was up-regulated in the fibrotic tissues of patients with systemic sclerosis. In vitro experiments confirmed that miR-16-5p could directly bind to NOTCH2 and inhibit the expression of collagen and α-SMA, thereby affecting the transformation of fibroblasts. The overexpression of lncRNA HOTAIR in human dermal fibroblasts can down-regulate the expression of miR-34a, activate the Notch signaling pathway, promote the expression of GLI2, and mediate the expression of downstream fibrotic genes. miR-30d and miR-21 have been reported to target jagged1 to regulate the Notch signaling pathway. Jagged1 (JAG1) is a Notch ligand. If the expression of Jagged1 is decreased, the Notch pathway will be blocked or inhibited. The overexpression of the miR-30d attenuated TGF-beta-1-induced proliferation of lung fibroblasts, as well as α-SMA and collagen I expression, is produced by directly binding to the 3’-UTR of JAG1. Restoring miR-30d expression to inhibit the TGF-beta-1-induced activation of JAG1/Notch signaling may be a promising strategy for the treatment of pulmonary fibrosis.
Blocking or inhibiting the activation of signaling pathways and signal conduction is essential to inhibit FMT and alleviate the symptoms of fibrosis. ncRNA can regulate the activation of signaling pathways to a significant degree which, in turn, affects FMT. However, the same signaling pathway is regulated by multiple ncRNAs, which is effective for clinical diagnosis but brings a certain difficulty to drug development. Therefore, finding highly specific ncRNAs is the goal of future research.
4. ncRNA Regulates FMT by Directly Affecting the Expression of Nuclear Transcription Factors
Nuclear transcription factors are one of the trans-acting factors, which are important proteins with DNA binding activity. They can initiate the transcription of related genes and regulate their transcription efficiency by binding to the promoters or enhancers of cis-regulatory elements. Cell differentiation and phenotypic switching are mediated by key transcription factors whose functions are finely regulated at the transcriptional, translational, and posttranslational levels. ncRNA regulates the expression of fibrosis-related genes by regulating the expression of transcription factors. Several transcription factors, such as DYRK2, SIRT1, KLF4, NLRC5, CREB, ARID3A, ZEB, SP1, YBX1, and SOX4, have been reported to be regulated by ncRNA. For example, the ZEB family (E-box zinc finger structural protein family) are a necessary transcription factor in embryonic development, including ZEB1 and ZEB2 protein transcription factors. The miR-200 family has been reported to target the ZEB family to regulate FMT. The miR-200 family contains miR-200a, 200b, 200c, miR-141, and miR-429, among which the coding gene of miR-200a/b/miR-429 is located in the p36.33 region of chromosome 1. However, miR-200c and miR-141 were localized in the p13.31 region of chromosome 12. Liao and YW et al. found that the treatment of oral mucosal fibroblasts with arecoline reduced the expression of miR-200b, and the overexpression of miR-200b could target ZEB2 to reduce the expression of the α-SMA gene and thus inhibit the differentiation of mucosal fibroblasts [113]. Lu and My et al., also found that the expression of miR-200c was down-regulated in oral submucosal fibrosis specimens and oral mucosal fibroblasts treated with arecoline. ZEB1 is a direct target of miR-200c, and the decreased expression of miR-200c attenuates its inhibitory effect on ZEB1 and promotes the expression of α-SMA [114].
5. Conclusions and Prospective
Endothelial cells, interstitial cells, fibroblasts, and other cells can be activated and differentiated into myofibroblasts with a stronger collagen synthesis ability under physical and chemical stimulations such as inflammation. This promotes the excessive accumulation of ECM in damaged tissues, leading to the formation of fibrosis. In liver fibrosis, hepatic stellate cells can be activated and differentiated into myofibroblast-like cells, which are the main source of liver myofibroblasts. miR-29b was found to inhibit the differentiation of liver stellate cells by inhibiting the activation of TGF-β/Smad [26]. On the contrary, miR-21 can target PTEN to activate the PI3K/AKT pathway and promote the differentiation of liver stellate cells [115]. However, for most fibrotic diseases, the activation of fibroblasts inherent in tissues and their phenotypic changes into myofibroblasts are the main pathological features of their development. In this review, we summarized the ncRNAs that have played an important role in regulating FMT in recent years. miR-21, miR-29, miR-30, miR-let-7, miR-145, miR-146, and miR-200 have received widespread attention from researchers because they can regulate FMT in various ways (as shown in Figure 2 and Figure 3). Multiple lncRNAs and circRNAs have also been reported to regulate FMT by competitively binding to these downstream microRNAs. Compared with biological small-molecule agents, RNA therapy is more accessible to the target. This provides a new method for the diagnosis, treatment, and prognosis of fibrotic disease. However, the following limitations still exist: (1) Some ncRNAs play opposite roles in different diseases, and even their roles in different models of the same disease are controversial. (2) Most of the ncRNAs reported so far are at the tissue and cell level, which still need invasive examination. For the purpose of non-invasive diagnosis, it is of high clinical significance to study the pathogenesis of ncRNAs with an abnormal expression in saliva, urine, and serum. (3) Most of the ncRNA studies are still only in the laboratory stage, and there is still a long way to go before their clinical application. Gallant-Behm et al. found in a clinical trial that the use of miR-29 mimics inhibited collagen expression and the development of fibroplasia in patients’ incisional skin wounds, offering an entirely new treatment for skin fibrosis [116]. However, RNA therapy has problems with immune-related toxicity and other adverse effects, and further optimization of the drug delivery method is needed.
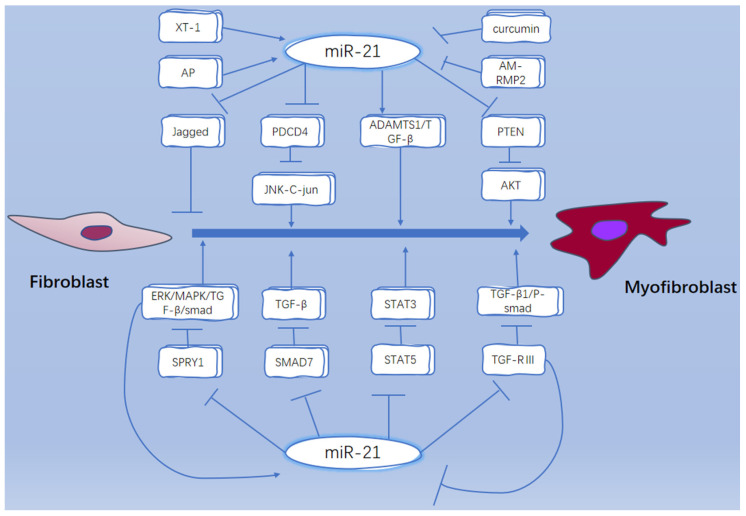
Figure 2.
miR-21 regulates FMT through different pathways. miR-21 regulates FMT process by targeting different downstream factors such as jagged1, PDCD4, PTEN, SPRY1, Smad7, STAT5, etc. XT-1 and AP can promote the expression of miR-21, while curcumin and AM-PMP2 can inhibit the expression of miR-21; miR-21 is a potential therapeutic target for fibrosis.
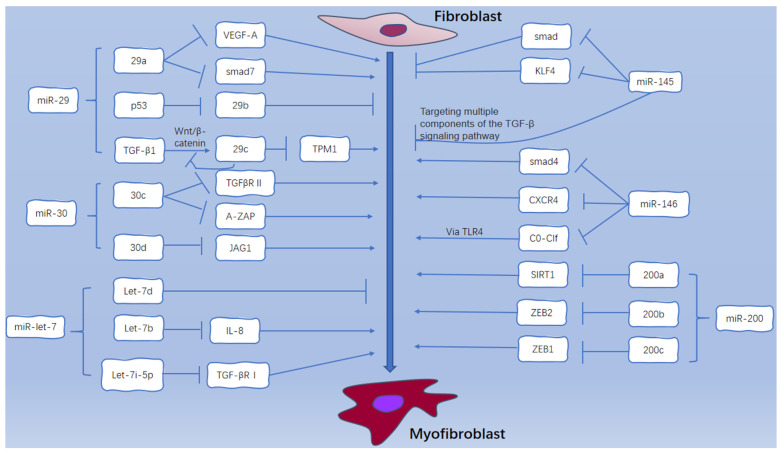
Figure 3.
miR-29, miR-30, miR-let-7, miR-145, miR-146, and miR-200 regulate FMT through different pathways: miR-29a targets VEGF-A and Smad7; TGF-β can promote the expression of miR-29c through wnt/β-catenin, and elevated miR-29c in turn inhibits the activation of wnt/β-catenin pathway. miR-30c targets TGF-β R Ⅱ and A-ZAP; miR-30d targets JAG1. let-7b targets IL-8 and let-7i-5p targets TGF-β R Ⅰ. miR-145 targets Smad4 and Smad families. miR-146 targets Smad4, CXCR4 and C0-C1f. miR-200a targets SIRT1, miR-200b targets ZEB2, and miR-200c targets ZEB1.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms24021801/s1. Table S1: The potential ncRNA biomarker for FMT. References are cited in [117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227,228,229,230,231,232,233,234,235] are cited in the supplementary materials.
Author Contributions
H.Z. wrote the manuscript and designed the figures; J.W. contributed to the modification of the manuscript; Y.Z. and D.W. conceived the idea. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was funded by the National Natural Science Foundation of China (31370210) and the Natural Science Foundation of Hunan Province, China (2020JJ4881, 2022JJ30695).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Hinz B., Lagares D. Evasion of apoptosis by myofibroblasts: A hallmark of fibrotic diseases. Nat. Rev. Rheumatol. 2020;16:11–31. doi: 10.1038/s41584-019-0324-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rockey D.C., Bell P.D., Hill J.A. Fibrosis—A Common Pathway to Organ Injury and Failure. N. Engl. J. Med. 2015;372:1138–1149. doi: 10.1056/NEJMra1300575. [DOI] [PubMed] [Google Scholar]
- 3.Tomasek J.J., Gabbiani G., Hinz B., Chaponnier C., Brown R.A. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat. Rev. Mol. Cell Biol. 2002;3:349–363. doi: 10.1038/nrm809. [DOI] [PubMed] [Google Scholar]
- 4.Zhao B., Guan H., Liu J.-Q., Zheng Z., Zhou Q., Zhang H., Su L.-L., Hu D.-H. Hypoxia drives the transition of human dermal fibroblasts to a myofibroblast-like phenotype via the TGF-beta 1/Smad3 pathway. Int. J. Mol. Med. 2017;39:153–159. doi: 10.3892/ijmm.2016.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y., Zhang J., Zhou Q., Wang H., Xie S., Yang X., Ji P., Zhang W., He T., Liu Y., et al. Linagliptin inhibits high glucose-induced transdifferentiation of hypertrophic scar-derived fibroblasts to myofibroblasts via IGF/Akt/mTOR signalling pathway. Exp. Dermatol. 2019;28:19–27. doi: 10.1111/exd.13800. [DOI] [PubMed] [Google Scholar]
- 6.Liu B., Liu Y., Wang L., Hou C., An M. The effects of pressure intervention on wound healing and scar formation in a Bama minipig model. Burns. 2019;45:413–422. doi: 10.1016/j.burns.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Gurtner G.C., Dauskardt R.H., Wong V.W., Bhatt K.A., Wu K., Vial I.N., Padois K., Korman J.M., Longaker M.T. Improving Cutaneous Scar Formation by Controlling the Mechanical Environment Large Animal and Phase I Studies. Ann. Surg. 2011;254:217–225. doi: 10.1097/SLA.0b013e318220b159. [DOI] [PubMed] [Google Scholar]
- 8.Plotkin L.I., Wallace J.M. MicroRNAs and osteocytes. Bone. 2021;150:115994. doi: 10.1016/j.bone.2021.115994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pu M., Chen J., Tao Z., Miao L., Qi X., Wang Y., Ren J. Regulatory network of miRNA on its target: Coordination between transcriptional and post-transcriptional regulation of gene expression. Cell Mol. Life Sci. 2019;76:441–451. doi: 10.1007/s00018-018-2940-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu M., Fu P., Qu L., Liu J., Lin A. Long Noncoding RNAs, New Critical Regulators in Cancer Immunity. Front. Oncol. 2020;10:550987. doi: 10.3389/fonc.2020.550987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kopp F., Mendell J.T. Functional Classification and Experimental Dissection of Long Noncoding RNAs. Cell. 2018;172:393–407. doi: 10.1016/j.cell.2018.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kong S., Tao M., Shen X., Ju S. Translatable circRNAs and lncRNAs: Driving mechanisms and functions of their translation products. Cancer Lett. 2020;483:59–65. doi: 10.1016/j.canlet.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Zhou J., Wang B., Bin X., Xie C., Li B., Liu O., Tang Z. CircHIPK3: Key Player in Pathophysiology and Potential Diagnostic and Therapeutic Tool. Front. Med. 2021;8:615417. doi: 10.3389/fmed.2021.615417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanniford D., Ulloa-Morales A., Karz A., Berzoti-Coelho M.G., Moubarak R.S., Sanchez-Sendra B., Kloetgen A., Davalos V., Imig J., Wu P., et al. Epigenetic Silencing of CDR1as Drives IGF2BP3-Mediated Melanoma Invasion and Metastasis. Cancer Cell. 2020;37:55. doi: 10.1016/j.ccell.2019.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang M., Zhao K., Xu X., Yang Y., Yan S., Wei P., Liu H., Xu J., Xiao F., Zhou H., et al. A peptide encoded by circular form of LINC-PINT suppresses oncogenic transcriptional elongation in glioblastoma. Nat. Commun. 2018;9:4475. doi: 10.1038/s41467-018-06862-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li X., Yang L., Chen L.-L. The Biogenesis, Functions, and Challenges of Circular RNAs. Mol. Cell. 2018;71:428–442. doi: 10.1016/j.molcel.2018.06.034. [DOI] [PubMed] [Google Scholar]
- 17.Salzman J., Chen R.E., Olsen M.N., Wang P.L., Brown P.O. Cell-Type Specific Features of Circular RNA Expression. PLos Genet. 2013;9:E1003777. doi: 10.1371/annotation/f782282b-eefa-4c8d-985c-b1484e845855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang L., Wang Y., Yu F., Li X., Gao H., Li P. CircHIPK3 Plays Vital Roles in Cardiovascular Disease. Front. Cardiovasc. Med. 2021;8:733248. doi: 10.3389/fcvm.2021.733248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xie Y., Yuan X., Zhou W., Kosiba A.A., Shi H., Gu J., Qin Z. The circular RNA HIPK3 (circHIPK3) and its regulation in cancer progression: Review. Life Sci. 2020;254:117252. doi: 10.1016/j.lfs.2019.117252. [DOI] [PubMed] [Google Scholar]
- 20.Wilson S.E. TGF beta-1,-2 and-3 in the modulation of fibrosis in the cornea and other organs. Exp. Eye Res. 2021;207:108594. doi: 10.1016/j.exer.2021.108594. [DOI] [PubMed] [Google Scholar]
- 21.Saadat S., Noureddini M., Mahjoubin-Tehran M., Nazemi S., Shojaie L., Aschner M., Maleki B., Abbasi-kolli M., Rajabi Moghadam H., Alani B., et al. Pivotal Role of TGF-beta/Smad Signaling in Cardiac Fibrosis: Non-coding RNAs as Effectual Players. Front. Cardiovasc. Med. 2021;7:588347. doi: 10.3389/fcvm.2020.588347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu W., Wang Y., Qiu Z., Zhao R., Liu Z., Chen W., Ge J., Shi B. CircHIPK3 regulates cardiac fibroblast proliferation, migration and phenotypic switching through the miR-152-3p/TGF-beta 2 axis under hypoxia. PeerJ. 2020;8:9796. doi: 10.7717/peerj.9796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tho L., Bei Y., Chen P., Lei Z., Fu S., Zhang H., Xu J., Che L., Chen X., Sluijter J.P.G., et al. Crucial Role of miR-433 in Regulating Cardiac Fibrosis. Theranostics. 2016;6:2068–2083. doi: 10.7150/thno.15007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duan M., Zhang Y., Zhang H., Meng Y., Qian M., Zhang G. Epidermal stem cell-derived exosomes promote skin regeneration by downregulating transforming growth factor-beta 1 in wound healing. Stem. Cell Res. Ther. 2020;11:452. doi: 10.1186/s13287-020-01971-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cai L., Chao G., Li W., Zhu J., Li F., Qi B., Wei Y., Chen S., Zhou G., Lu X., et al. Activated CD4(+) T cells-derived exosomal miR-142-3p boosts post-ischemic ventricular remodeling by activating myofibrobiast. Aging. 2020;12:7380–7396. doi: 10.18632/aging.103084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liang C., Bu S., Fan X. Suppressive effect of microRNA-29b on hepatic stellate cell activation and its crosstalk with TGF-beta 1/Smad3. Cell Biochem. Funct. 2016;34:326–333. doi: 10.1002/cbf.3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jeck W.R., Sorrentino J.A., Wang K., Slevin M.K., Burd C.E., Liu J., Marzluff W.F., Sharpless N.E. Circular RNAs are abundant, conserved, and associated with ALU repeats. RNA. 2013;19:141–157. doi: 10.1261/rna.035667.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng Q., Bao C., Guo W., Li S., Chen J., Chen B., Luo Y., Lyu D., Li Y., Shi G., et al. Circular RNA profiling reveals an abundant circHIPK3 that regulates cell growth by sponging multiple miRNAs. Nat. Commun. 2016;7:11215. doi: 10.1038/ncomms11215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liang D.M., Wilusz J.E. Short intronic repeat sequences facilitate circular RNA production. Genes Dev. 2014;28:2233–2247. doi: 10.1101/gad.251926.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fu Y., Sun H. Biogenesis, cellular effects, and biomarker value of circHIPK3. Cancer Cell Int. 2021;21:256. doi: 10.1186/s12935-021-01956-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu Q., Cheng D., Li G., Liu Y., Li P., Sun W., Ma D., Ni C. CircHIPK3 regulates pulmonary fibrosis by facilitating glycolysis in miR-30a-3p/FOXK2-dependent manner. Int. J. Biol. Sci. 2021;17:2294–2307. doi: 10.7150/ijbs.57915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang J.-X., Lu J., Xie H., Wang D.-p., Ni H.-E., Zhu Y., Ren L.-H., Meng X.-X., Wang R.-L. circHIPK3 regulates lung fibroblast-to-myofibroblast transition by functioning as a competing endogenous RNA. Cell Death Dis. 2019;10:182. doi: 10.1038/s41419-019-1430-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liao J.-Y., Ma L.-M., Guo Y.-H., Zhang Y.-C., Zhou H., Shao P., Chen Y.-Q., Qu L.-H. Deep Sequencing of Human Nuclear and Cytoplasmic Small RNAs Reveals an Unexpectedly Complex Subcellular Distribution of miRNAs and tRNA 3’ Trailers. PLoS ONE. 2010;5:e0010563. doi: 10.1371/journal.pone.0010563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dohner K., Brown J., Hehmann U., Hetzel C., Stewart J., Lowther G., Scholl C., Frohling S., Cuneo A., Tsui L.C., et al. Molecular cytogenetic characterization of a critical region in bands 7q35-q36 commonly deleted in malignant myeloid disorders. Blood. 1998;92:4031–4035. doi: 10.1182/blood.V92.11.4031. [DOI] [PubMed] [Google Scholar]
- 35.Kwon J.J., Factora T.D., Dey S., Kota J. 1 A Systematic Review of miR-29 in Cancer. Mol. Ther.-Oncolytics. 2019;12:173–194. doi: 10.1016/j.omto.2018.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yuan R., Dai X., Li Y., Li C., Liu L. Exosomes from miR-29a-modified adipose-derived mesenchymal stem cells reduce excessive scar formation by inhibiting TGF-beta 2/Smad3 signaling. Mol. Med. Rep. 2021;24:12398. doi: 10.3892/mmr.2021.12398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu C.-C., Liao Y.-W., Hsieh P.-L., Chang Y.-C. Targeting lncRNA H19/miR-29b/COL1A1 Axis Impedes Myofibroblast Activities of Precancerous Oral Submucous Fibrosis. Int. J. Mol. Sci. 2021;22:2216. doi: 10.3390/ijms22042216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang J., Zhang Y., Huang L., Lan Y.J., Zhang Q. The inhibition effect of miR-29c on lung fibroblasts transdifferentiation induced by SiO(2) Chin. J. Ind. Hyg. Occup. Dis. 2019;37:321–326. doi: 10.3760/cma.j.issn.1001-9391.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 39.Zhu Y., Feng Z., Jian Z., Xiao Y. Long noncoding RNA TUG1 promotes cardiac fibroblast transformation to myofibroblasts via miR-29c in chronic hypoxia. Mol. Med. Rep. 2018;18:3451–3460. doi: 10.3892/mmr.2018.9327. [DOI] [PubMed] [Google Scholar]
- 40.Zhao X., Wang K., Liao Y., Zeng Q., Li Y., Hu F., Liu Y., Meng K., Qian C., Zhang Q., et al. MicroRNA-101a Inhibits Cardiac Fibrosis Induced by Hypoxia via Targeting TGF beta RI on Cardiac Fibroblasts. Cell Physiol. Biochem. 2015;35:213–226. doi: 10.1159/000369689. [DOI] [PubMed] [Google Scholar]
- 41.Feng Y., Bao Y., Ding J., Li H., Liu W., Wang X., Guan H., Chen Z. MicroRNA-130a attenuates cardiac fibrosis after myocardial infarction through TGF-beta/Smad signaling by directly targeting TGF-beta receptor 1. Bioengineered. 2022;13:5779–5791. doi: 10.1080/21655979.2022.2033380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu C., Hou L., Zhao J., Wang Y., Jiang F., Jiang Q., Zhu Z., Tian L. Exosomal let-7i-5p from three-dimensional cultured human umbilical cord mesenchymal stem cells inhibits fibroblast activation in silicosis through targeting TGFBR1. Ecotoxicol. Environ. Saf. 2022;233:113302. doi: 10.1016/j.ecoenv.2022.113302. [DOI] [PubMed] [Google Scholar]
- 43.Ukey S., Jain A., Dwivedi S., Choudhury C., Vishnoi J.R., Chugh A., Purohit P., Pareek P., Elhence P., Misra S., et al. Study of MicroRNA (miR-221-3p, miR-133a-3p, and miR-9-5p) Expressions in Oral Submucous Fibrosis and Squamous Cell Carcinoma. Indian J. Clin. Biochem. 2022 doi: 10.1007/s12291-022-01035-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang Y., Pan Y., Liu Y., Li X., Tang L., Duan M., Li J., Zhang G. Exosomes derived from human umbilical cord blood mesenchymal stem cells stimulate regenerative wound healing via transforming growth factor-beta receptor inhibition. Stem Cell Res. Ther. 2021;12:434. doi: 10.1186/s13287-021-02517-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cheng D., Xu Q., Liu Y., Li G., Sun W., Ma D., Ni C. Long noncoding RNA-SNHG20 promotes silica-induced pulmonary fibrosis by miR-490-3p/TGFBR1 axis. Toxicology. 2021;451:152683. doi: 10.1016/j.tox.2021.152683. [DOI] [PubMed] [Google Scholar]
- 46.Xu J., Wu H., Chen S., Qi B., Zhou G., Cai L., Zhao L., Wei Y., Liu S. MicroRNA-30c suppresses the pro-fibrogenic effects of cardiac fibroblasts induced by TGF-beta 1 and prevents atrial fibrosis by targeting TGF beta RII. J. Cell Mol. Med. 2018;22:3045–3057. doi: 10.1111/jcmm.13548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rodriguez P., Sassi Y., Troncone L., Benard L., Ishikawa K., Gordon R.E., Lamas S., Laborda J., Hajjar R.J., Lebeche D. Deletion of delta-like 1 homologue accelerates fibroblast-myofibroblast differentiation and induces myocardial fibrosis. Eur. Heart J. 2019;40:967–978. doi: 10.1093/eurheartj/ehy188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miguel V., Busnadiego O., Fierro-Fernandez M., Lamas S. Protective role for miR-9-5p in the fibrogenic transformation of human dermal fibroblasts. Fibrogenesis Tissue Repair. 2016;9:7. doi: 10.1186/s13069-016-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang Z., Xiao Z., Guo H., Fang X., Liang J., Zhu J., Yang J., Li H., Pan R., Yuan S., et al. Novel role of the clustered miR-23b-3p and miR-27b-3p in enhanced expression of fibrosis-associated genes by targeting TGFBR3 in atrial fibroblasts. J. Cell Mol. Med. 2019;23:3246–3256. doi: 10.1111/jcmm.14211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liang H., Zhang C., Ban T., Liu Y., Mei L., Piao X., Zhao D., Lu Y., Chu W., Yang B. A novel reciprocal loop between microRNA-21 and TGF beta RIII is involved in cardiac fibrosis. Int. J. Biochem. Cell Biol. 2012;44:2152–2160. doi: 10.1016/j.biocel.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 51.Su J.-L., Chen P.-S., Johansson G., Kuo M.-L. Function and regulation of let-7 family microRNAs. MicroRNA. 2012;1:34–39. doi: 10.2174/2211536611201010034. [DOI] [PubMed] [Google Scholar]
- 52.Cui H., Banerjee S., Xie N., Ge J., Liu R.-M., Matalon S., Thannickal V.J., Liu G. MicroRNA-27a-3p Is a Negative Regulator of Lung Fibrosis by Targeting Myofibroblast Differentiation. Am. J. Respir. Cell Mol. Biol. 2016;54:843–852. doi: 10.1165/rcmb.2015-0205OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Su P., Qiao Q., Ji G., Zhang Z. CircAMD1 regulates proliferation and collagen synthesis via sponging miR-27a-3p in P63-mutant human dermal fibroblasts. Differentiation. 2021;119:10–18. doi: 10.1016/j.diff.2021.04.002. [DOI] [PubMed] [Google Scholar]
- 54.Tang R., Wang Y.-C., Mei X., Shi N., Sun C., Ran R., Zhang G., Li W., Staveley-O’Carroll K.F., Li G., et al. LncRNA GAS5 attenuates fibroblast activation through inhibiting Smad3 signaling. Am. J. Physiol.-Cell Physiol. 2020;319:C105–C115. doi: 10.1152/ajpcell.00059.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zheng D., Zhang Y., Hu Y., Guan J., Xu L., Xiao W., Zhong Q., Ren C., Lu J., Liang J., et al. Long noncoding RNA Crnde attenuates cardiac fibrosis via Smad3-Crnde negative feedback in diabetic cardiomyopathy. FEBS J. 2019;286:1645–1655. doi: 10.1111/febs.14780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gao Q., Yang K., Chen D., Song Y., Qiao W., Sun X., Meng L., Bian Z. Antifibrotic Potential of MiR-335-3p in Hereditary Gingival Fibromatosis. J. Dent. Res. 2019;98:1140–1149. doi: 10.1177/0022034519863300. [DOI] [PubMed] [Google Scholar]
- 57.Schneider C., King R.M., Philipson L. Genes specifically expressed at growth arrest of mammalian cells. Cell. 1988;54:787–793. doi: 10.1016/S0092-8674(88)91065-3. [DOI] [PubMed] [Google Scholar]
- 58.Xiang Z., Liqing Y., Qingqing Y., Qiang H., Hongbo C. Retard or exacerbate: Role of long non-coding RNA growth arrest-specific 5 in the fibrosis. Cytokine Growth Factor Rev. 2022;67:89–104. doi: 10.1016/j.cytogfr.2022.06.001. [DOI] [PubMed] [Google Scholar]
- 59.She Q., Shi P., Xu S.-S., Xuan H.-Y., Tao H., Shi K.-H., Yang Y. DNMT1 Methylation of LncRNA GAS5 Leads to Cardiac Fibroblast Pyroptosis via Affecting NLRP3 Axis. Inflammation. 2020;43:1065–1076. doi: 10.1007/s10753-020-01191-3. [DOI] [PubMed] [Google Scholar]
- 60.Wang W., Jia Y.-J., Yang Y.-L., Xue M., Zheng Z.-J., Wang L., Xue Y.-M. LncRNA GAS5 exacerbates renal tubular epithelial fibrosis by acting as a competing endogenous RNA of miR-96-5p. Biomed. Pharmacother. 2020;121:109411. doi: 10.1016/j.biopha.2019.109411. [DOI] [PubMed] [Google Scholar]
- 61.Dong Z.-G., Yang Y.-P., Jiang Z.-J. Knockdown CRNDE alleviates LPS-induced inflammation injury via FOXM1 in WI-38 cells. Biomed. Pharmacother. 2018;103:1678–1687. doi: 10.1016/j.biopha.2018.04.192. [DOI] [PubMed] [Google Scholar]
- 62.Zhang Z., Yang P., Wang C., Tian R. LncRNA CRNDE hinders the progression of osteoarthritis by epigenetic regulation of DACT1. Cell Mol. Life Sci. 2022;79:405. doi: 10.1007/s00018-022-04427-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Qi Y., Cui S., Liu L., Liu B., Wang T., Yan S., Tian H., Huang X. Expression and role of miR-146a and SMAD4 in placental tissue of pregnant women with preeclampsia. J. Obstet. Gynaecol. Res. 2022;48:2151–2161. doi: 10.1111/jog.15323. [DOI] [PubMed] [Google Scholar]
- 64.Dong M., Wang X., Tong L., Wang J., Yang Y., Liu Y., Jing Y., Zhao H., Chen J. Mir-27a-3p attenuates bronchiolitis obliterans in vivo via the regulation of dendritic cells’ maturation and the suppression of myofibroblasts’ differentiation. Clin. Transl. Med. 2020;10:140. doi: 10.1002/ctm2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nakasa T., Miyaki S., Okubo A., Hashimoto M., Nishida K., Ochi M., Asahara H. Expression of MicroRNA-146 in rheumatoid arthritis synovial tissue. Arthritis Rheum. 2008;58:1284–1292. doi: 10.1002/art.23429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yogeswaran A., Troidl C., McNamara J.W., Wilhelm J., Truschel T., Widmann L., Aslam M., Hamm C.W., Sadayappan S., Lipps C. The C0-C1f Region of Cardiac Myosin Binding Protein-C Induces Pro-Inflammatory Responses in Fibroblasts via TLR4 Signaling. Cells. 2021;10:1326. doi: 10.3390/cells10061326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang X., Morelli M.B., Matarese A., Sardu C., Santulli G. Cardiomyocyte-derived exosomal microRNA-92a mediates post-ischemic myofibroblast activation both in vitro and ex vivo. ESC Heart Fail. 2020;7:285–289. doi: 10.1002/ehf2.12584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bai J., Zhang M., Ding X., Yang X., Zheng D., Mou H., Ruan X., Feng Y., Han H., Wang S. MicroRNA-21a-5p regulates TGF-beta 1-induced myofibroblast transformation of rabbit keratocytes by targeting Smad7. Scienceasia. 2022;48:57–61. doi: 10.2306/scienceasia1513-1874.2022.011. [DOI] [Google Scholar]
- 69.Wang C., Gu S., Cao H., Li Z., Xiang Z., Hu K., Han X. miR-877-3p targets Smad7 and is associated with myofibroblast differentiation and bleomycin-induced lung fibrosis. Sci. Rep. 2016;6:30122. doi: 10.1038/srep30122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li W., Wang Y., Deng Y., Ni H., Shen G., Liu X., Li J., Wang F. Epigenetic Control of circHNRNPH1 in Postischemic Myocardial Fibrosis through Targeting of TGF-beta Receptor Type I. Mol. Ther.-Nucleic Acids. 2021;25:93–104. doi: 10.1016/j.omtn.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang J., Hu K., Cai X., Yang B., He Q., Wang J., Weng Q. Targeting PI3K/AKT signaling for treatment of idiopathic pulmonary fibrosis. Acta Pharm. Sin. B. 2022;12:18–32. doi: 10.1016/j.apsb.2021.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang J., You J., Gong D., Xu Y., Yang B., Jiang C. PDGF-BB induces conversion, proliferation, migration, and collagen synthesis of oral mucosal fibroblasts through PDGFR-beta/PI3K/ AKT signaling pathway. Cancer Biomark. 2021;30:407–415. doi: 10.3233/CBM-201681. [DOI] [PubMed] [Google Scholar]
- 73.Kalantari P., Harandi O.F., Agarwal S., Rus F., Kurt-Jones E.A., Fitzgerald K.A., Caffrey D.R., Golenbock D.T. miR-718 represses proinflammatory cytokine production through targeting phosphatase and tensin homolog (PTEN) J. Biol. Chem. 2017;292:5634–5644. doi: 10.1074/jbc.M116.749325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang T., Liang Y., Lin Q., Liu J., Luo F., Li X., Zhou H., Zhuang S., Zhang H. MiR-29 mediates TGF1-induced extracellular matrix synthesis through activation of PI3K-AKT pathway in human lung fibroblasts. J. Cell Biochem. 2013;114:1336–1342. doi: 10.1002/jcb.24474. [DOI] [PubMed] [Google Scholar]
- 75.Li H., Tian X., Ruan Y., Xing J., Meng Z. Asiatic acid alleviates Ang-II induced cardiac hypertrophy and fibrosis via miR-126/PIK3R2 signaling. Nutr. Metab. 2021;18:71. doi: 10.1186/s12986-021-00596-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhao S., Li W., Yu W., Rao T., Li H., Ruan Y., Yuan R., Li C., Ning J., Li S., et al. Exosomal miR-21 from tubular cells contributes to renal fibrosis by activating fibroblasts via targeting PTEN in obstructed kidneys. Theranostics. 2021;11:8660–8673. doi: 10.7150/thno.62820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rackow A.R., Judge J.L., Woeller C.F., Sime P.J., Kottmann R.M. miR-338-3p blocks TGF8-induced myofibroblast differentiation through the induction of PTEN. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2022;322:L385–L400. doi: 10.1152/ajplung.00251.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wu Q., Han L., Gui W., Wang F., Yan W., Jiang H. MiR-503 suppresses fibroblast activation and myofibroblast differentiation by targeting VEGFA and FGFR1 in silica-induced pulmonary fibrosis. J. Cell Mol. Med. 2020;24:14339–14348. doi: 10.1111/jcmm.16051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Huang Y., Xie Y., Abel P.W., Wei P., Plowman J., Toews M.L., Strah H., Siddique A., Bailey K.L., Tu Y. TGF-beta 1-induced miR-424 promotes pulmonary myofibroblast differentiation by targeting Slit2 protein expression. Biochem. Pharmacol. 2020;180:114172. doi: 10.1016/j.bcp.2020.114172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Huang C., Yang Y., Liu L. Interaction of long noncoding RNAs and microRNAs in the pathogenesis of idiopathic pulmonary fibrosis. Physiol. Genom. 2015;47:463–469. doi: 10.1152/physiolgenomics.00064.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li X., Yu T., Shan H., Jiang H., Sun J., Zhao X., Su W., Yang L., Shan H., Liang H. lncRNA PFAL promotes lung fibrosis through CTGF by competitively binding miR-18a. FASEB J. 2018;32:5285–5297. doi: 10.1096/fj.201800055R. [DOI] [PubMed] [Google Scholar]
- 82.Tan L., Xie Y., Yuan Y., Hu K. LncRNA GAS5 as miR-26a-5p Sponge Regulates the PTEN/PI3K/Akt Axis and Affects Extracellular Matrix Synthesis in Degenerative Nucleus Pulposus Cells in vitro. Front. Neurol. 2021;12:653341. doi: 10.3389/fneur.2021.653341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhu H.-Y., Li C., Bai W.-D., Su L.-L., Liu J.-Q., Li Y., Shi J.-H., Cai W.-X., Bai X.-Z., Jia Y.-H., et al. MicroRNA-21 Regulates hTERT via PTEN in Hypertrophic Scar Fibroblasts. PLoS ONE. 2014;9:E0097114. doi: 10.1371/journal.pone.0097114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fan Y., Zhao X., Ma J., Yang L. LncRNA GAS5 Competitively Combined With miR-21 Regulates PTEN and Influences EMT of Peritoneal Mesothelial Cells via Wnt/beta-Catenin Signaling Pathway. Front. Physiol. 2021;12:654951. doi: 10.3389/fphys.2021.654951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Song M., Zhao G., Sun H., Yao S., Zhou Z., Jiang P., Wu Q., Zhu H., Wang H., Dai C., et al. circPTPN12/miR-21-5 p/Delta Np63 alpha pathway contributes to human endometrial fibrosis. Elife. 2021;10:65735. doi: 10.7554/eLife.65735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cai Z., Guo H., Qian J., Liu W., Li Y., Yuan L., Zhou Y., Lin R., Xie X., Yang Q., et al. Effects of bone morphogenetic protein 4 on TGF-beta 1-induced cell proliferation, apoptosis, activation and differentiation in mouse lung fibroblasts via ERK/p38 MAPK signaling pathway. PeerJ. 2022;10:13775. doi: 10.7717/peerj.13775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sun Q., Miao J., Luo J., Yuan Q., Cao H., Su W., Zhou Y., Jiang L., Fang L., Dai C., et al. The feedback loop between miR-21, PDCD4 and AP-1 functions as a driving force for renal fibrogenesis. J. Cell Sci. 2018;131:jcs202317. doi: 10.1242/jcs.202317. [DOI] [PubMed] [Google Scholar]
- 88.Auler M., Bergmeier V., Georgieva V.S., Pitzler L., Frie C., Nuechel J., Eckes B., Hinz B., Brachvogel B. miR-127-3p Is an Epigenetic Activator of Myofibroblast Senescence Situated within the MicroRNA-Enriched Dlk1-Dio3-Imprinted Domain on Mouse Chromosome 12. J. Investig. Dermatol. 2021;141:1076–1086. doi: 10.1016/j.jid.2020.11.011. [DOI] [PubMed] [Google Scholar]
- 89.Shen J., Xing W., Liu R., Zhang Y., Xie C., Gong F. MiR-32-5p influences high glucose-induced cardiac fibroblast proliferation and phenotypic alteration by inhibiting DUSP1. BMC Mol. Biol. 2019;20:21. doi: 10.1186/s12867-019-0135-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Huang C., Wang R., Lu J., He Y., Wu Y., Ma W., Xu J., Wu Z., Feng Z., Wu M. MicroRNA-338-3p as a therapeutic target in cardiac fibrosis through FGFR2 suppression. J. Clin. Lab. Anal. 2022;36:e24584. doi: 10.1002/jcla.24584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zheng L., Xu C.-C., Chen W.-D., Shen W.-L., Ruan C.-C., Zhu L.-M., Zhu D.-L., Gao P.-J. MicroRNA-155 regulates angiotensin II type 1 receptor expression and phenotypic differentiation in vascular adventitial fibroblasts. Biochem. Biophys. Res. Commun. 2010;400:483–488. doi: 10.1016/j.bbrc.2010.08.067. [DOI] [PubMed] [Google Scholar]
- 92.Kuse N., Kamio K., Azuma A., Matsuda K., Inomata M., Usuki J., Morinaga A., Tanaka T., Kashiwada T., Atsumi K., et al. Exosome-Derived microRNA-22 Ameliorates Pulmonary Fibrosis by Regulating Fibroblast-to-Myofibroblast Differentiation in Vitro and in Vivo. J. Nippon. Med. Sch. 2020;87:118–128. doi: 10.1272/jnms.JNMS.2020_87-302. [DOI] [PubMed] [Google Scholar]
- 93.Qian G., Jin X., Zhang L. LncRNA FENDRR Upregulation Promotes Hepatic Carcinoma Cells Apoptosis By Targeting miR-362-5p Via NPR3 and p38-MAPK Pathway. Cancer Biother. Radiopharm. 2020;35:629–639. doi: 10.1089/cbr.2019.3468. [DOI] [PubMed] [Google Scholar]
- 94.Yu Y., Sun B., Wang Z., Yang M., Cui Z., Lin S., Jin M., Yi C. Exosomes From M2 Macrophage Promote Peritendinous Fibrosis Posterior Tendon Injury via the MiR-15b-5p/FGF-1/7/9 Pathway by Delivery of circRNA-Ep400. Front. Cell Dev. Biol. 2021;9:1557. doi: 10.3389/fcell.2021.595911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liao Y.-W., Tsai L.-L., Lee Y.-H., Hsieh P.-L., Yu C.-C., Lu M.-Y. miR-21 promotes the fibrotic properties in oral mucosa through targeting PDCD4. J. Dent. Sci. 2022;17:677–682. doi: 10.1016/j.jds.2021.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li D., Mao C., Zhou E., You J., Gao E., Han Z., Fan Y., He Q., Wang C. MicroRNA-21 Mediates a Positive Feedback on Angiotensin II-Induced Myofibroblast Transformation. J. Inflamm. Res. 2020;13:1007–1020. doi: 10.2147/JIR.S285714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yan J., Yang Y., Fan X., Liang G., Wang Z., Li J., Wang L., Chen Y., Adetula A.A., Tang Y., et al. circRNAome profiling reveals circFgfr2 regulates myogenesis and muscle regeneration via a feedback loop. J. Cachexia Sarcopenia Muscle. 2022;13:696–712. doi: 10.1002/jcsm.12859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Li X., Liu X., Deng R., Gao S., Jiang Q., Liu R., Li H., Miao Y., Zhai Y., Zhang S., et al. Betulinic acid attenuated bleomycin-induced pulmonary fibrosis by effectively intervening Wnt/beta-catenin signaling. Phytomedicine. 2021;81:153428. doi: 10.1016/j.phymed.2020.153428. [DOI] [PubMed] [Google Scholar]
- 99.Ortiz-Quintero B., Buendia-Roldan I., Gustavo Ramirez-Salazar E., Balderas-Martinez Y.I., Lizbeth Ramirez-Rodriguez S., Martinez-Espinosa K., Selman M. Circulating microRNA Signature Associated to Interstitial Lung Abnormalities in Respiratory Asymptomatic Subjects. Cells. 2020;9:1556. doi: 10.3390/cells9061556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Henderson J., Pryzborski S., Stratton R., O’Reilly S. Wnt antagonist DKK-1 levels in systemic sclerosis are lower in skin but not in blood and are regulated by microRNA33a-3p. Exp. Dermatol. 2021;30:162–168. doi: 10.1111/exd.14136. [DOI] [PubMed] [Google Scholar]
- 101.Sun L.-Y., Bie Z.-D., Zhang C.-H., Li H., Li L.-D., Yang J. MiR-154 directly suppresses DKK2 to activate Wnt signaling pathway and enhance activation of cardiac fibroblasts. Cell Biol. Int. 2016;40:1271–1279. doi: 10.1002/cbin.10655. [DOI] [PubMed] [Google Scholar]
- 102.Huang H., Huang X., Luo S., Zhang H., Hu F., Chen R., Huang C., Su Z. The MicroRNA MiR-29c Alleviates Renal Fibrosis via TPM1-Mediated Suppression of the Wnt/beta-Catenin Pathway. Front. Physiol. 2020;11:331. doi: 10.3389/fphys.2020.00331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Liu L.-j., Qian H., Hu K., Zhang Z.-z., He J.-b. miR-27a-3p inhibited synthesis of Col I and Col III in pulmonary fibroblasts through Wnt3a/beta-eatenin signaling pathway. Chin. Pharmacol. Bull. 2019;35:229–234. doi: 10.3969/j.issn.1001-1978.2019.02.017. [DOI] [Google Scholar]
- 104.Liu L., Qian H., Hu K., Wang L., Zhang Z., Yin H., He J. miR-27a-3p inhibits pulmonary fibrosis by blocking Wnt3a/beta-catenin pathway in rats. Chin. J. Cell. Mol. Immunol. 2018;34:1015–1020. [PubMed] [Google Scholar]
- 105.Hao K., Lei W., Wu H., Wu J., Yang Z., Yan S., Lu X.-A., Li J., Xia X., Han X., et al. LncRNA-Safe contributes to cardiac fibrosis through Safe-Sfrp2-HuR complex in mouse myocardial infarction. Theranostics. 2019;9:7282–7297. doi: 10.7150/thno.33920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Papaioannou I., Xu S., Denton C.P., Abraham D.J., Ponticos M. STAT3 controls COL1A2 enhancer activation cooperatively with JunB, regulates type I collagen synthesis posttranscriptionally, and is essential for lung myofibroblast differentiation. Mol. Biol. Cell. 2018;29:84–95. doi: 10.1091/mbc.E17-06-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wei S., Qiu Y. MiR-210-5p regulates STAT3 activation by targeting STAT5A in the differentiation of dermal fibroblasts. 3 Biotech. 2021;11:243. doi: 10.1007/s13205-021-02777-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yue Z., Jiang Z., Ruan B., Duan J., Song P., Liu J., Han H., Wang L. Disruption of myofibroblastic Notch signaling attenuates liver fibrosis by modulating fibrosis progression and regression. Int. J. Biol. Sci. 2021;17:2135–2146. doi: 10.7150/ijbs.60056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yao Q., Xing Y., Wang Z., Liang J., Lin Q., Huang M., Chen Y., Lin B., Xu X., Chen W. MiR-16-5p suppresses myofibroblast activation in systemic sclerosis by inhibiting NOTCH signaling. Aging. 2021;13:2640–2654. doi: 10.18632/aging.202308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhao S., Xiao X., Sun S., Li D., Wang W., Fu Y., Fan F. MicroRNA-30d/JAG1 axis modulates pulmonary fibrosis through Notch signaling pathway. Pathol. Res. Pract. 2018;214:1315–1323. doi: 10.1016/j.prp.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 111.Zhou X.-L., Xu H., Liu Z.-B., Wu Q.-C., Zhu R.-R., Liu J.-C. miR-21 promotes cardiac fibroblast-to-myofibroblast transformation and myocardial fibrosis by targeting Jagged1. J. Cell Mol. Med. 2018;22:3816–3824. doi: 10.1111/jcmm.13654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wasson C.W., Ross R.L., Wells R., Corinaldesi C., Georgiou I.C., Riobo-Del Galdo N.A., Del Galdo F. Long non-coding RNA HOTAIR induces GLI2 expression through Notch signalling in systemic sclerosis dermal fibroblasts. Arthritis Res. Ther. 2020;22:286. doi: 10.1186/s13075-020-02376-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Liao Y.-W., Yu C.-C., Hsieh P.-L., Chang Y.-C. miR-200b ameliorates myofibroblast transdifferentiation in precancerous oral submucous fibrosis through targeting ZEB2. J. Cell Mol. Med. 2018;22:4130–4138. doi: 10.1111/jcmm.13690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lu M.-Y., Yu C.-C., Chen P.-Y., Hsieh P.-L., Peng C.-Y., Liao Y.-W., Yu C.-H., Lin K.-H. miR-200c inhibits the arecoline-associated myofibroblastic transdifferentiation in buccal mucosal fibroblasts. J. Formos. Med. Assoc. 2018;117:791–797. doi: 10.1016/j.jfma.2018.05.016. [DOI] [PubMed] [Google Scholar]
- 115.Wei J., Feng L., Li Z., Xu G., Fan X. MicroRNA-21 activates hepatic stellate cells via PTEN/Akt signaling. Biomed. Pharmacother. 2013;67:387–392. doi: 10.1016/j.biopha.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 116.Gallant-Behm C.L., Piper J., Lynch J.M., Seto A.G., Hong S.J., Mustoe T.A., Maari C., Pestano L.A., Dalby C.M., Jackson A.L., et al. A MicroRNA-29 Mimic (Remlarsen) Represses Extracellular Matrix Expression and Fibroplasia in the Skin. J. Investig. Dermatol. 2019;139:1073–1081. doi: 10.1016/j.jid.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 117.Dai C., Tao H., Shi K.-H., Xu S.-S. Effect of miR-369-5p on cardiac fibroblast activation and proliferation in SD rats. Chin. Pharmacol. Bull. 2018;34:1693–1696. doi: 10.3969/j.issn.1001-1978.2018.12.014. [DOI] [Google Scholar]
- 118.Schnittert J., Kuninty P.R., Bystry T.F., Brock R., Storm G., Prakash J. Anti-microRNA targeting using peptide-based nanocomplexes to inhibit differentiation of human pancreatic stellate cells. Nanomedicine. 2017;12:1369–1384. doi: 10.2217/nnm-2017-0054. [DOI] [PubMed] [Google Scholar]
- 119.Szczerba E., Zajkowska A., Bochowicz A., Pankiewicz K., Szewczyk G., Opolski G., Maciejewski T., Malecki M., Fijalkowska A. Downregulated expression of microRNAs associated with cardiac hypertrophy and fibrosis in physiological pregnancy and the association with echocardiographically-evaluated myocardial function. Biomed. Rep. 2020;13:41. doi: 10.3892/br.2020.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zanotti S., Gibertini S., Blasevich F., Bragato C., Ruggieri A., Saredi S., Fabbri M., Bernasconi P., Maggi L., Mantegazza R., et al. Exosomes and exosomal miRNAs from muscle-derived fibroblasts promote skeletal muscle fibrosis. Matrix Biol. 2018;74:77–100. doi: 10.1016/j.matbio.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 121.Yi M., Liu B., Tang Y., Li F., Qin W., Yuan X. Irradiated Human Umbilical Vein Endothelial Cells Undergo Endothelial-Mesenchymal Transition via the Snail/miR-199a-5p Axis to Promote the Differentiation of Fibroblasts into Myofibroblasts. Biomed. Res. Int. 2018;2018:4135806. doi: 10.1155/2018/4135806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cardenas C.L.L., Henaoui I.S., Courcot E., Roderburg C., Cauffiez C., Aubert S., Copin M.-C., Wallaert B., Glowacki F., Dewaeles E., et al. miR-199a-5p Is Upregulated during Fibrogenic Response to Tissue Injury and Mediates TGFbeta-Induced Lung Fibroblast Activation by Targeting Caveolin-1. PLos Genet. 2013;9:1003291. doi: 10.1371/journal.pgen.1003291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yang P.-Y., Ho D.C.-Y., Chen S.-H., Hsieh P.-L., Liao Y.-W., Tsai L.-L., Yu C.-C., Fang C.-Y. Down-regulation of miR-29c promotes the progression of oral submucous fibrosis through targeting tropomyosin-1. J. Formos. Med. Assoc. 2022;121:1117–1122. doi: 10.1016/j.jfma.2021.10.006. [DOI] [PubMed] [Google Scholar]
- 124.Lian X., Chen X., Sun J., An G., Li X., Wang Y., Niu P., Zhu Z., Tian L. MicroRNA-29b inhibits supernatants from silica-treated macrophages from inducing extracellular matrix synthesis in lung fibroblasts. Toxicol. Res. 2017;6:878–888. doi: 10.1039/C7TX00126F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zou Y., Kong M. Tetrahydroxy stilbene glucoside alleviates palmitic acid-induced inflammation and apoptosis in cardiomyocytes by regulating miR-129-3p/Smad3 signaling. Cell Mol. Biol. Lett. 2019;24:5. doi: 10.1186/s11658-018-0125-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wang F., Zhao X.-Q., Liu J.-N., Wang Z.-H., Wang X.-L., Hou X.-Y., Liu R., Gao F., Zhang M.-X., Zhang Y., et al. Antagonist of microRNA-21 improves balloon injury-induced rat iliac artery remodeling by regulating proliferation and apoptosis of adventitial fibroblasts and myofibroblasts. J. Cell Biochem. 2012;113:2989–3001. doi: 10.1002/jcb.24176. [DOI] [PubMed] [Google Scholar]
- 127.Yang H.-W., Yu C.-C., Hsieh P.-L., Liao Y.-W., Chu P.-M., Yu C.-H., Fang C.-Y. Arecoline enhances miR-21 to promote buccal mucosal fibroblasts activation. J. Formos. Med. Assoc. 2021;120:1108–1113. doi: 10.1016/j.jfma.2020.10.019. [DOI] [PubMed] [Google Scholar]
- 128.Singh P., Srivastava A.N., Sharma R., Mateen S., Shukla B., Singh A., Chandel S. Circulating MicroRNA-21 Expression as a Novel Serum Biomarker for Oral Sub-Mucous Fibrosis and Oral Squamous Cell Carcinoma. Asian Pac. J. Cancer Prev. 2018;19:1053–1057. doi: 10.22034/APJCP.2018.19.4.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wang J., Guo R., Ma X., Wang Y., Zhang Q., Zheng N., Zhang J., Li C. Liraglutide inhibits AngII-induced cardiac fibroblast proliferation and ECM deposition through regulating miR-21/PTEN/PI3K pathway. Cell Tissue Bank. 2022 doi: 10.1007/s10561-022-10021-9. [DOI] [PubMed] [Google Scholar]
- 130.Schipper J., Westerhuis J.J., Beddows I., Madaj Z., Monsma D., Hostetter G., Kiupel M., Conejo-Garcia J.R., Sempere L.F. Loss of microRNA-21 leads to profound stromal remodeling and short survival in K-Ras-driven mouse models of pancreatic cancer. Int. J. Cancer. 2020;147:2265–2278. doi: 10.1002/ijc.33041. [DOI] [PubMed] [Google Scholar]
- 131.Li N., Wang Z., Gao F., Lei Y., Li Z. Melatonin ameliorates renal fibroblast-myofibroblast transdifferentiation and renal fibrosis through miR-21-5p regulation. J. Cell Mol. Med. 2020;24:5615–5628. doi: 10.1111/jcmm.15221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yao Q., Cao S., Li C., Mengesha A., Kong B., Wei M. Micro-RNA-21 regulates TGF-beta-induced myofibroblast differentiation by targeting PDCD4 in tumor-stroma interaction. Int. J. Cancer. 2011;128:1783–1792. doi: 10.1002/ijc.25506. [DOI] [PubMed] [Google Scholar]
- 133.Gong C., Nie Y., Qu S., Liao J.-Y., Cui X., Yao H., Zeng Y., Su F., Song E., Liu Q. miR-21 Induces Myofibroblast Differentiation and Promotes the Malignant Progression of Breast Phyllodes Tumors. Cancer Res. 2014;74:4341–4352. doi: 10.1158/0008-5472.CAN-14-0125. [DOI] [PubMed] [Google Scholar]
- 134.Liu G., Friggeri A., Yang Y., Milosevic J., Ding Q., Thannickal V.J., Kaminski N., Abraham E. miR-21 mediates fibrogenic activation of pulmonary fibroblasts and lung fibrosis. J. Exp. Med. 2010;207:1589–1597. doi: 10.1084/jem.20100035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jiang C., Guo Y., Yu H., Lu S., Meng L. Pleiotropic microRNA-21 in pulmonary remodeling: Novel insights for molecular mechanism and present advancements. Allergy Asthma Clin. Immunol. 2019;15:33. doi: 10.1186/s13223-019-0345-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kilari S., Cai C., Zhao C., Sharma A., Chernogubova E., Simeon M., Wu C.-C., Song H.-L., Maegdefessel L., Misra S. The Role of MicroRNA-21 in Venous Neointimal Hyperplasia: Implications for Targeting miR-21 for VNH Treatment. Mol. Ther. 2019;27:1681–1693. doi: 10.1016/j.ymthe.2019.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chen H.-C., Tseng Y.-K., Chi C.-C., Chen Y.-H., Yang C.-M., Huang S.-J., Lee Y.-C., Liou H.-H., Tsai K.-W., Ger L.-P. Genetic variants in microRNA-146a (C > G) and microRNA-1269b (G > C) are associated with the decreased risk of oral premalignant lesions, oral cancer, and pharyngeal cancer. Arch. Oral Biol. 2016;72:21–32. doi: 10.1016/j.archoralbio.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 138.Yang J., Yu X., Xue F., Li Y., Liu W., Zhang S. Exosomes derived from cardiomyocytes promote cardiac fibrosis via myocyte-fibroblast cross-talk. Am. J. Transl. Res. 2018;10:4350–4366. [PMC free article] [PubMed] [Google Scholar]
- 139.Al-Harbi B., Hendrayani S.-F., Silva G., Aboussekhra A. Let-7b inhibits cancer-promoting effects of breast cancer-associated fibroblasts through IL-8 repression. Oncotarget. 2018;9:17825–17838. doi: 10.18632/oncotarget.24895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Huleihel L., Ben-Yehudah A., Milosevic J., Yu G., Pandit K., Sakamoto K., Yousef H., LeJeune M., Coon T.A., Redinger C.J., et al. Let-7d microRNA affects mesenchymal phenotypic properties of lung fibroblasts. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2014;306:L534–L542. doi: 10.1152/ajplung.00149.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhang S., Jia X., Zhang Q., Zhang L., Yang J., Hu C., Shi J., Jiang X., Lu J., Shen H. Neutrophil extracellular traps activate lung fibroblast to induce polymyositis-related interstitial lung diseases via TLR9-miR-7-Smad2 pathway. J. Cell Mol. Med. 2020;24:1658–1669. doi: 10.1111/jcmm.14858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yang K., Shi J., Hu Z., Hu X. The deficiency of miR-214-3p exacerbates cardiac fibrosis via miR-214-3p/NLRC5 axis. Clin. Sci. 2019;133:1845–1856. doi: 10.1042/CS20190203. [DOI] [PubMed] [Google Scholar]
- 143.Dong H., Dong S., Zhang L., Gao X., Lv G., Chen W., Shao S. MicroRNA-214 exerts a Cardio-protective effect by inhibition of fibrosis. Anat. Rec.-Adv. Integr. Anat. Evol. Biol. 2016;299:1348–1357. doi: 10.1002/ar.23396. [DOI] [PubMed] [Google Scholar]
- 144.Sun M., Yu H., Zhang Y., Li Z., Gao W. MicroRNA-214 Mediates Isoproterenol-induced Proliferation and Collagen Synthesis in Cardiac Fibroblasts. Sci. Rep. 2015;5:18351. doi: 10.1038/srep18351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Conde E., Gimenez-Moyano S., Martin-Gomez L., Rodriguez M., Edurne Ramos M., Aguado-Fraile E., Blanco-Sanchez I., Saiz A., Laura Garcia-Bermejo M. HIF-1 alpha induction during reperfusion avoids maladaptive repair after renal ischemia/reperfusion involving miR127-3p. Sci. Rep. 2017;7:41099. doi: 10.1038/srep41099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hogan T.B., Tiwari N., Nagaraja M.R., Shetty S.K., Fan L., Shetty R.S., Bhandary Y.P., Shetty S. Caveolin-1 peptide regulates p53-microRNA-34a feedback in fibrotic lung fibroblasts. Iscience. 2022;25:104022. doi: 10.1016/j.isci.2022.104022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bulvik R., Biton M., Berkman N., Breuer R., Wallach-Dayan S.B. Forefront: MiR-34a-Knockout Mice with Wild Type Hematopoietic Cells, Retain Persistent Fibrosis Following Lung Injury. Int. J. Mol. Sci. 2020;21:2228. doi: 10.3390/ijms21062228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhang C., Zhang Y., Zhu H., Hu J., Xie Z. MiR-34a/miR-93 target c-Ski to modulate the proliferaton of rat cardiac fibroblasts and extracellular matrix deposition in vivo and in vitro. Cell Signalling. 2018;46:145–153. doi: 10.1016/j.cellsig.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 149.Kanno Y., Shu E., Niwa H., Seishima M., Ozaki K.-i. MicroRNA-30c attenuates fibrosis progression and vascular dysfunction in systemic sclerosis model mice. Mol. Biol. Rep. 2021;48:3431–3437. doi: 10.1007/s11033-021-06368-z. [DOI] [PubMed] [Google Scholar]
- 150.Bajor A., Ratuszny D., Gras C., Pielen A., Boergel M., Framme C., Blasczyk R., Figueiredo C. Inhibition of miR-145 as a strategy to prevent corneal scarring. Investig. Ophthalmol. Visual Sci. 2015;56:4917. [Google Scholar]
- 151.Song H.-F., He S., Li S.-H., Wu J., Yin W., Shao Z., Du G.-q., Wu J., Li J., Weisel R.D., et al. Knock-out of MicroRNA 145 impairs cardiac fibroblast function and wound healing post-myocardial infarction. J. Cell Mol. Med. 2020;24:9409–9419. doi: 10.1111/jcmm.15597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Naito Y., Yasuno K., Tagawa H., Sakamoto N., Oue N., Yashiro M., Sentani K., Goto K., Shinmei S., Oo H.Z., et al. MicroRNA-145 is a potential prognostic factor of scirrhous type gastric cancer. Oncol. Rep. 2014;32:1720–1726. doi: 10.3892/or.2014.3333. [DOI] [PubMed] [Google Scholar]
- 153.Ly T.-D., Riedel L., Fischer B., Schmidt V., Hendig D., Distler J., Kuhn J., Knabbe C., Faust I. microRNA-145 mediates xylosyltransferase-I induction in myofibroblasts via suppression of transcription factor KLF4. Biochem. Biophys. Res. Commun. 2020;523:1001–1006. doi: 10.1016/j.bbrc.2019.12.120. [DOI] [PubMed] [Google Scholar]
- 154.Gras C., Ratuszny D., Hadamitzky C., Zhang H., Blasczyk R., Figueiredo C. miR-145 Contributes to Hypertrophic Scarring of the Skin by Inducing Myofibroblast Activity. Mol. Med. 2015;21:296–304. doi: 10.2119/molmed.2014.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ratuszny D., Gras C., Bajor A., Boerger A.-K., Pielen A., Boergel M., Framme C., Blasczyk R., Figueiredo C. miR-145 Is a Promising Therapeutic Target to Prevent Cornea Scarring. Hum. Gene Ther. 2015;26:698–707. doi: 10.1089/hum.2014.151. [DOI] [PubMed] [Google Scholar]
- 156.Yang S., Cui H., Xie N., Icyuz M., Banerjee S., Antony V.B., Abraham E., Thannickal V.J., Liu G. miR-145 regulates myofibroblast differentiation and lung fibrosis. FASEB J. 2013;27:2382–2391. doi: 10.1096/fj.12-219493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Melling G.E., Flannery S.E., Abidin S.A., Clemmens H., Prajapati P., Hinsley E.E., Hunt S., Catto J.W.F., Della Coletta R., Mellone M., et al. A miRNA-145/TGF-beta 1 negative feedback loop regulates the cancer-associated fibroblast phenotype. Carcinogenesis. 2018;39:798–807. doi: 10.1093/carcin/bgy032. [DOI] [PubMed] [Google Scholar]
- 158.Wang Y.-S., Li S.-H., Guo J., Mihic A., Wu J., Sun L., Davis K., Weisel R.D., Li R.-K. Role of miR-145 in cardiac myofibroblast differentiation. J. Mol. Cell. Cardiol. 2014;66:94–105. doi: 10.1016/j.yjmcc.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 159.Liakouli V., Cipriani P., Di Benedetto P., Panzera N., Ruscitti P., Pantano I., Berardicurti O., Carubbi F., Esteves F., Mavria G., et al. Epidermal Growth Factor Like-domain 7 and miR-126 are abnormally expressed in diffuse Systemic Sclerosis fibroblasts. Sci. Rep. 2019;9:4589. doi: 10.1038/s41598-019-39485-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zhang L., Yin H., Jiao L., Liu T., Gao Y., Shao Y., Zhang Y., Shan H., Zhang Y., Yang B. Abnormal Downregulation of Caveolin-3 Mediates the Pro-Fibrotic Action of MicroRNA-22 in a Model of Myocardial Infarction. Cell Physiol. Biochem. 2018;45:1641–1653. doi: 10.1159/000487732. [DOI] [PubMed] [Google Scholar]
- 161.Li J., Yue S., Fang J., Zeng J., Chen S., Tian J., Nie S., Liu X., Ding H. MicroRNA-10a/b inhibit TGF-beta/Smad-induced renal fibrosis by targeting TGF-beta receptor 1 in diabetic kidney disease. Mol. Ther.-Nucleic Acids. 2022;28:488–499. doi: 10.1016/j.omtn.2022.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Fang C.-Y., Yu C.-C., Liao Y.-W., Hsieh P.L., Ohiro Y., Chu P.M., Huang Y.-C., Yu C.-H., Tsai L.-L. miR-10b regulated by Twist maintains myofibroblasts activities in oral submucous fibrosis. J. Formos. Med. Assoc. 2020;119:1167–1173. doi: 10.1016/j.jfma.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 163.Chugh A., Purohit P., Vishnoi J.R., Kaur A., Modi A., Mishra S., Sharma P., Rodha M.S., Pareek P., Bhattacharya S., et al. Correlation of hsa miR-101-5p and hsa miR-155-3p Expression With c-Fos in Patients of Oral Submucous Fibrosis (OSMF) and Oral Squamous Cell Carcinoma (OSCC) J. Maxillofac. Oral Surg. 2021 doi: 10.1007/s12663-021-01668-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Chou M.-Y., Fang C.-Y., Hsieh P.-L., Liao Y.-W., Yu C.-C., Lee S.-S. Depletion of miR-155 hinders the myofibroblast activities and reactive oxygen species generation in oral submucous fibrosis. J. Formos. Med. Assoc. 2022;121:467–472. doi: 10.1016/j.jfma.2021.06.028. [DOI] [PubMed] [Google Scholar]
- 165.Artlett C.M., Sassi-Gaha S., Hope J.L., Feghali-Bostwick C.A., Katsikis P.D. Mir-155 is overexpressed in systemic sclerosis fibroblasts and is required for NLRP3 inflammasome-mediated collagen synthesis during fibrosis. Arthritis Res. Ther. 2017;19:144. doi: 10.1186/s13075-017-1331-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.He W., Huang H., Xie Q., Wang Z., Fan Y., Kong B., Huang D., Xiao Y. MiR-155 Knockout in Fibroblasts Improves Cardiac Remodeling by Targeting Tumor Protein p53-Inducible Nuclear Protein 1. J. Cardiovasc. Pharmacol. Ther. 2016;21:423–435. doi: 10.1177/1074248415616188. [DOI] [PubMed] [Google Scholar]
- 167.Ghafouri-Fard S., Abak A., Talebi S.F., Shoorei H., Branicki W., Taheri M., Dilmaghani N.A. Role of miRNA and lncRNAs in organ fibrosis and aging. Biomed. Pharmacother. 2021;143:112132. doi: 10.1016/j.biopha.2021.112132. [DOI] [PubMed] [Google Scholar]
- 168.Shen S., Wang X., Xu D., Tao L., Wu X., Xiao J., Li X. Mir-195-3p/-5p Decrease Cardiac Fibroblast Proliferation and the Transdifferentiation into Myofibroblasts. Circ. Res. 2015;117:1580982. doi: 10.1161/res.117.suppl_1.167. [DOI] [Google Scholar]
- 169.You K., Li S.-Y., Gong J., Fang J.-H., Zhang C., Zhang M., Yuan Y., Yang J., Zhuang S.-M. MicroRNA-125b Promotes Hepatic Stellate Cell Activation and Liver Fibrosis by Activating RhoA Signaling. Mol. Ther.-Nucleic Acids. 2018;12:57–66. doi: 10.1016/j.omtn.2018.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Nagpal V., Rai R., Place A.T., Murphy S.B., Verma S.K., Ghosh A.K., Vaughan D.E. MiR-125b Is Critical for Fibroblast-to-Myofibroblast Transition and Cardiac Fibrosis. Circulation. 2016;133:291–301. doi: 10.1161/CIRCULATIONAHA.115.018174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Bie Z.-D., Sun L.-Y., Geng C.-L., Meng Q.-G., Lin X.-J., Wang Y.-F., Wang X.-F., Yang J. MiR-125b regulates SFRP5 expression to promote growth and activation of cardiac fibroblasts. Cell Biol. Int. 2016;40:1224–1234. doi: 10.1002/cbin.10677. [DOI] [PubMed] [Google Scholar]
- 172.Xia W., Li M., Jiang X., Huang X., Gu S., Ye J., Zhu L., Hou M., Zan T. Young fibroblast-derived exosomal microRNA-125b transfers beneficial effects on aged cutaneous wound healing. J. Nanobiotechnol. 2022;20:144. doi: 10.1186/s12951-022-01348-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Duru N., Zhang Y., Gernapudi R., Wolfson B., Lo P.-K., Yao Y., Zhou Q. Loss of miR-140 is a key risk factor for radiation-induced lung fibrosis through reprogramming fibroblasts and macrophages. Sci. Rep. 2016;6:39572. doi: 10.1038/srep39572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhang X., Chen Q., Song H., Jiang W., Xie S., Huang J., Kang G. MicroRNA-375 prevents TGF-beta-dependent transdifferentiation of lung fibroblasts via the MAP2K6/P38 pathway. Mol. Med. Rep. 2020;22:1803–1810. doi: 10.3892/mmr.2020.11261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ji Y., Qiu M., Shen Y., Gao L., Wang Y., Sun W., Li X., Lu Y., Kong X. MicroRNA-327 regulates cardiac hypertrophy and fibrosis induced by pressure overload. Int. J. Mol. Med. 2018;41:1909–1916. doi: 10.3892/ijmm.2018.3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Akerman A.W., Collins E.N., Peterson A.R., Collins L.B., Harrison J.K., DeVaughn A., Townsend J.M., Vanbuskirk R.L., Riopedre-Maqueira J., Reyes A., et al. miR-133a Replacement Attenuates Thoracic Aortic Aneurysm in Mice. J. Am. Heart Assoc. 2021;10:19862. doi: 10.1161/JAHA.120.019862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Wei P., Xie Y., Abel P.W., Huang Y., Ma Q., Li L., Hao J., Wolff D.W., Wei T., Tu Y. Transforming growth factor (TGF)-beta 1-induced miR-133a inhibits myofibroblast differentiation and pulmonary fibrosis. Cell Death Dis. 2019:10. doi: 10.1038/s41419-019-1873-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Liu Z.-Y., Lu M., Liu J., Wang Z.-N., Wang W.-W., Li Y., Song Z.-J., Xu L., Liu Q., Li F.-H. MicroRNA-144 regulates angiotensin II-induced cardiac fibroblast activation by targeting CREB. Exp. Ther. Med. 2020;20:2113–2121. doi: 10.3892/etm.2020.8901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li Y., Zhang J., Zhang W., Liu Y., Li Y., Wang K., Zhang Y., Yang C., Li X., Shi J., et al. MicroRNA-192 regulates hypertrophic scar fibrosis by targeting SIP1. J. Mol. Histol. 2017;48:357–366. doi: 10.1007/s10735-017-9734-3. [DOI] [PubMed] [Google Scholar]
- 180.Cui J., Qi S., Liao R., Su D., Wang Y., Xue S. MiR-574-5p promotes the differentiation of human cardiac fibroblasts via regulating ARID3A. Biochem. Biophys. Res. Commun. 2020;521:427–433. doi: 10.1016/j.bbrc.2019.09.107. [DOI] [PubMed] [Google Scholar]
- 181.Xu S.-S., Ding J.-F., Shi P., Shi K.-H., Tao H. DNMT1-Induced miR-152-3p Suppression Facilitates Cardiac Fibroblast Activation in Cardiac Fibrosis. Cardiovasc. Toxicol. 2021;21:984–999. doi: 10.1007/s12012-021-09690-x. [DOI] [PubMed] [Google Scholar]
- 182.Li L., Bounds K.R., Chatterjee P., Gupta S. MicroRNA-130a, a Potential Antifibrotic Target in Cardiac Fibrosis. J. Am. Heart Assoc. 2017;6:e006763. doi: 10.1161/JAHA.117.006763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Guo F., Carter D.E., Leask A. miR-218 regulates focal adhesion kinase-dependent TGF beta signaling in fibroblasts. Mol. Biol. Cell. 2014;25:1151–1158. doi: 10.1091/mbc.e13-08-0451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Xian S., Li J., Zhang Z. miR-26b inhibits isoproterenol-induced cardiac fibrosis via the Keap1/Nrf2 signaling pathway. Exp. Ther. Med. 2020;19:2067–2074. doi: 10.3892/etm.2020.8455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Levy M.Z., Rabinowicz N., Kohon M.Y., Shalom A., Berl A., Hornik-Lurie T., Drucker L., Matalon S.T., Levy Y. MiRNAs in Systemic Sclerosis Patients with Pulmonary Arterial Hypertension: Markers and Effectors. Biomedicines. 2022;10:629. doi: 10.3390/biomedicines10030629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Heindryckx F., Binet F., Ponticos M., Rombouts K., Lau J., Kreuger J., Gerwins P. Endoplasmic reticulum stress enhances fibrosis through IRE1 alpha-mediated degradation of miR-150 and XBP-1 splicing. EMBO Mol. Med. 2016;8:729–744. doi: 10.15252/emmm.201505925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Deng P., Chen L., Liu Z., Ye P., Wang S., Wu J., Yao Y., Sun Y., Huang X., Ren L., et al. MicroRNA-150 Inhibits the Activation of Cardiac Fibroblasts by Regulating c-Myb. Cell Physiol. Biochem. 2016;38:2103–2122. doi: 10.1159/000445568. [DOI] [PubMed] [Google Scholar]
- 188.Ren L., Yang C., Dou Y., Zhan R., Sun Y., Yu Y. MiR-541-5p regulates lung fibrosis by targeting cyclic nucleotide phosphodiesterase 1A. Exp. Lung Res. 2017;43:249–258. doi: 10.1080/01902148.2017.1349210. [DOI] [PubMed] [Google Scholar]
- 189.Liu C.-M., Liao Y.-W., Hsieh P.-L., Yu C.-H., Chueh P.J., Lin T., Yang P.-Y., Yu C.-C., Chou M.-Y. miR-1246 as a therapeutic target in oral submucosa fibrosis pathogenesis. J. Formos. Med. Assoc. 2019;118:1093–1098. doi: 10.1016/j.jfma.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 190.Qu C., Liu X., Ye T., Wang L., Liu S., Zhou X., Wu G., Lin J., Shi S., Yang B. miR-216a exacerbates TGF-beta-induced myofibroblast transdifferentiation via PTEN/AKT signaling. Mol. Med. Rep. 2019;19:5345–5352. doi: 10.3892/mmr.2019.10200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Huang J., Zhang H., Fan X., Guo J. Inhibition of miR-497 Attenuates Oral Submucous Fibrosis by Inhibiting Myofibroblast Transdifferentiation in Buccal Mucosal Fibroblasts. Oral Health Prev. Dent. 2022;20:339–348. doi: 10.3290/j.ohpd.b3276183. [DOI] [PubMed] [Google Scholar]
- 192.Chai C.Y., Tai I.C., Zhou R., Song J.L., Zhang C.Y., Sun S.R. MicroRNA-9-5p inhibits proliferation and induces apoptosis of human hypertrophic scar fibroblasts through targeting peroxisome proliferator-activated receptor beta. Biol. Open. 2020;9:bio051904. doi: 10.1242/bio.051904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Han B., Zhang Y., Xiao Y., Shi B., Wu H., Liu D. Adipose-Derived Stem Cell-Derived Extracellular Vesicles Inhibit the Fibrosis of Fibrotic Buccal Mucosal Fibroblasts via the MicroRNA-375/FOXF1 Axis. Stem Cells Int. 2021;2021:9964159 . doi: 10.1155/2021/9964159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Zeng C., Wang Y.-L., Xie C., Sang Y., Li T.-J., Zhang M., Wang R., Zhang Q., Zheng L., Zhuang S.-M. Identification of a novel TGF-beta-miR-122-fibronectin 1/serum response factor signaling cascade and its implication in hepatic fibrogenesis. Oncotarget. 2015;6:12224–12233. doi: 10.18632/oncotarget.3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Xu M., Fang S., Xie A. Posttranscriptional control of PLOD1 in adipose-derived stem cells regulates scar formation through altering macrophage polarization. Ann. Transl. Med. 2021;9:4978. doi: 10.21037/atm-21-4978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wang Q.-G., Cheng B.C.-Y., He Y.-Z., Li L.-J., Ling Y., Luo G., Wang L., Liang S., Zhang Y. miR-320a in serum exosomes promotes myocardial fibroblast proliferation via regulating the PIK3CA/Akt/mTOR signaling pathway in HEH2 cells. Exp. Ther. Med. 2021;22:10305. doi: 10.3892/etm.2021.10305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Huang Y., Xie Y., Bailey K., Toews M.L., Abel P.W., Tu Y. TGF-beta 1-induced miR-424 Mediates Pulmonary Myofibrolast Differentiation via Targeting Slit2. FASEB J. 2019;33:114172. doi: 10.1096/fasebj.2019.33.1_supplement.681.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Li Y., Zhang J., Shi J., Liu K., Wang X., Jia Y., He T., Shen K., Wang Y., Liu J., et al. Exosomes derived from human adipose mesenchymal stem cells attenuate hypertrophic scar fibrosis by miR-192-5p/IL-17RA/Smad axis. Stem. Cell Res. Ther. 2021;12:221. doi: 10.1186/s13287-021-02290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Wu Y., Luan J., Jiao C., Zhang S., Ma C., Zhang Y., Fu J., Lai E.Y., Kopp J.B., Pi J., et al. circHIPK3 Exacerbates Folic Acid-Induced Renal Tubulointerstitial Fibrosis by Sponging miR-30a. Front. Physiol. 2022;12:715567. doi: 10.3389/fphys.2021.715567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Ding F., Lu L., Wu C., Pan X., Liu B., Zhang Y., Wang Y., Wu W., Yan B., Zhang Y., et al. circHIPK3 prevents cardiac senescence by acting as a scaffold to recruit ubiquitin ligase to degrade HuR. Theranostics. 2022;12:7550–7566. doi: 10.7150/thno.77630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.He X., Ou C. CircRNA circHIPK3: A novel therapeutic target for angiotensin II-induced cardiac fibrosis. Int. J. Cardiol. 2020;312:98. doi: 10.1016/j.ijcard.2020.03.034. [DOI] [PubMed] [Google Scholar]
- 202.Wu Y., Wu M., Yang J., Li Y., Peng W., Wu M., Yu C., Fang M. Silencing CircHIPK3 Sponges miR-93-5p to Inhibit the Activation of Rac1/PI3K/AKT Pathway and Improves Myocardial Infarction-Induced Cardiac Dysfunction. Front. Cardiovasc. Med. 2021;8:645378. doi: 10.3389/fcvm.2021.645378. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 203.Wu N., Li C., Xu B., Xiang Y., Jia X., Yuan Z., Wu L., Zhong L., Li Y. Circular RNA mmu_circ_0005019 inhibits fibrosis of cardiac fibroblasts and reverses electrical remodeling of cardiomyocytes. BMC Cardiovasc. Disord. 2021;21:308. doi: 10.1186/s12872-021-02128-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Du W.W., Xu J., Yang W., Wu N., Li F., Zhou L., Wang S., Li X., He A.T., Du K.Y., et al. A Neuroligin Isoform Translated by circNlgn Contributes to Cardiac Remodeling. Circ. Res. 2021;129:568–582. doi: 10.1161/CIRCRESAHA.120.318364. [DOI] [PubMed] [Google Scholar]
- 205.Zhang L., Chi X., Luo W., Yu S., Zhang J., Guo Y., Ren Q., Zhang W. Lung myofibroblast transition and fibrosis is regulated by circ0044226. Int. J. Biochem. Cell Biol. 2020;118:105660. doi: 10.1016/j.biocel.2019.105660. [DOI] [PubMed] [Google Scholar]
- 206.Zheng S., Hu C., Lin H., Li G., Xia R., Zhang X., Su D., Li Z., Zhou Q., Chen R. circCUL2 induces an inflammatory CAF phenotype in pancreatic ductal adenocarcinoma via the activation of the MyD88-dependent NF-kappa B signaling pathway. J. Exp. Clin. Cancer Res. 2022;41:71. doi: 10.1186/s13046-021-02237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Zhou B., Yu J.-W. A novel identified circular RNA, circRNA_010567, promotes myocardial fibrosis via suppressing miR-141 by targeting TGF-beta 1. Biochem. Biophys. Res. Commun. 2017;487:769–775. doi: 10.1016/j.bbrc.2017.04.044. [DOI] [PubMed] [Google Scholar]
- 208.Zhao Q., Liu J., Deng H., Ma R., Liao J.-Y., Liang H., Hu J., Li J., Guo Z., Cai J., et al. Targeting Mitochondria-Located circRNA SCAR Alleviates NASH via Reducing mROS Output. Cell. 2020;183:76. doi: 10.1016/j.cell.2020.08.009. [DOI] [PubMed] [Google Scholar]
- 209.Ge X., Sun Y., Tang Y., Lin J., Zhou F., Yao G., Su X. Circular RNA HECTD1 knockdown inhibits transforming growth factor-beta/small mothers against decapentaplegic (TGF-beta/Smad) signaling to reduce hypertrophic scar fibrosis. Bioengineered. 2022;13:7303–7315. doi: 10.1080/21655979.2022.2048771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Ding K., Li D., Zhang R., Zuo M. Circ_0047339 promotes the activation of fibroblasts and affects the development of urethral stricture by targeting the miR-4691-5p/TSP-1 axis. Sci. Rep. 2022;12:14746. doi: 10.1038/s41598-022-19141-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Cheng X., Ai K., Yi L., Liu W., Li Y., Wang Y., Zhang D. The mmu_circRNA_37492/hsa_circ_0012138 function as potential ceRNA to attenuate obstructive renal fibrosis. Cell Death Dis. 2022;13:207. doi: 10.1038/s41419-022-04612-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Savary G., Dewaeles E., Diazzi S., Buscot M., Nottet N., Fassy J., Courcot E., Henaoui I.-S., Lemaire J., Martis N., et al. The Long Noncoding RNA DNM3OS Is a Reservoir of FibromiRs with Major Functions in Lung Fibroblast Response to TGF-beta and Pulmonary Fibrosis. Am. J. Respir. Crit. Care Med. 2019;200:184–198. doi: 10.1164/rccm.201807-1237OC. [DOI] [PubMed] [Google Scholar]
- 213.Piccoli M.-T., Gupta S.K., Viereck J., Foinquinos A., Samolovac S., Kramer F.L., Garg A., Remke J., Zimmer K., Batkai S., et al. Inhibition of the Cardiac Fibroblast- Enriched lncRNA Meg3 Prevents Cardiac Fibrosis and Diastolic Dysfunction. Circ. Res. 2017;121:575. doi: 10.1161/CIRCRESAHA.117.310624. [DOI] [PubMed] [Google Scholar]
- 214.Li J., Zhang X., Wang T., Li J., Su Q., Zhong C., Chen Z., Liang Y. The MIR155 host gene/microRNA-627/HMGB1/NF-kappa B loop modulates fibroblast proliferation and extracellular matrix deposition. Life Sci. 2021:269. doi: 10.1016/j.lfs.2021.119085. [DOI] [PubMed] [Google Scholar]
- 215.Su H., Xie J., Wen L., Wang S., Chen S., Li J., Qi C., Zhang Q., He X., Zheng L., et al. LncRNA Gas5 regulates Fn1 deposition via Creb5 in renal fibrosis. Epigenomics. 2021;13:699–713. doi: 10.2217/epi-2020-0449. [DOI] [PubMed] [Google Scholar]
- 216.Lin C.-Y., Liao Y.-W., Hsieh P.-L., Lu M.-Y., Peng C.-Y., Chu P.-M., Yang H.-W., Huang Y.-F., Yu C.-C., Yu C.-H. LncRNA GAS5-AS1 inhibits myofibroblasts activities in oral submucous fibrosis. J. Formos. Med. Assoc. 2018;117:727–733. doi: 10.1016/j.jfma.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 217.Zhou X.-H., Chai H.-X., Bai M., Zhang Z. LncRNA-GAS5 regulates PDCD4 expression and mediates myocardial infarction-induced cardiomyocytes apoptosis via targeting MiR-21. Cell Cycle. 2020;19:1363–1377. doi: 10.1080/15384101.2020.1750257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Tao H., Shi P., Zhao X.-D., Xuan H.-Y., Ding X.-S. MeCP2 inactivation of LncRNA GAS5 triggers cardiac fibroblasts activation in cardiac fibrosis. Cell Signalling. 2020:74. doi: 10.1016/j.cellsig.2020.109705. [DOI] [PubMed] [Google Scholar]
- 219.Chen J., Zhou R., Liang Y., Fu X., Wang D., Wang C. Blockade of lncRNA-ASLNCS5088-enriched exosome generation in M2 macrophages by GW4869 dampens the effect of M2 macrophages on orchestrating fibroblast activation. FASEB J. 2019;33:12200–12212. doi: 10.1096/fj.201901610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Wasson C.W., Abignano G., Hermes H., Malaab M., Ross R.L., Jimenez S.A., Chang H.Y., Feghali-Bostwick C.A., del Galdo F. Long non-coding RNA HOTAIR drives EZH2-dependent myofibroblast activation in systemic sclerosis through miRNA 34a-dependent activation of NOTCH. Ann. Rheum. Dis. 2020;79:507–517. doi: 10.1136/annrheumdis-2019-216542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Chen T., Guo Y., Wang J., Ai L., Ma L., He W., Li Z., Yu X., Li J., Fan X., et al. LncRNA CTD-2528L19.6 prevents the progression of IPF by alleviating fibroblast activation. Cell Death Dis. 2021;12:600. doi: 10.1038/s41419-021-03884-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Yang Y., Tai W., Lu N., Li T., Liu Y., Wu W., Li Z., Pu L., Zhao X., Zhang T., et al. lncRNA ZFAS1 promotes lung fibroblast-to-myofibroblast transition and ferroptosis via functioning as a ceRNA through miR-150-5p/SLC38A1 axis. Aging. 2020;12:9085–9102. doi: 10.18632/aging.103176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Zhang F., Fu X., Kataoka M., Liu N., Wang Y., Gao F., Liang T., Dong X., Pei J., Hu X., et al. Long noncoding RNA Cfast regulates cardiac fibrosis. Mol. Ther.-Nucleic Acids. 2021;23:377–392. doi: 10.1016/j.omtn.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Liang H., Pan Z., Zhao X., Liu L., Sun J., Su X., Xu C., Zhou Y., Zhao D., Xu B., et al. LncRNA PFL contributes to cardiac fibrosis by acting as a competing endogenous RNA of let-7d. Theranostics. 2018;8:1180–1194. doi: 10.7150/thno.20846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Bijkerk R., Au Y.W., Stam W., Duijs J.M.G.J., Koudijs A., Lievers E., Rabelink T.J., van Zonneveld A.J. Long Non-coding RNAs Rian and Miat Mediate Myofibroblast Formation in Kidney Fibrosis. Front. Pharmacol. 2019;10:215. doi: 10.3389/fphar.2019.00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Xiao T., Zou Z., Xue J., Syed B.M., Sun J., Dai X., Shi M., Li J., Wei S., Tang H., et al. LncRNA H19-mediated M2 polarization of macrophages promotes myofibroblast differentiation in pulmonary fibrosis induced by arsenic exposure. Environ. Pollut. 2021;268:115810. doi: 10.1016/j.envpol.2020.115810. [DOI] [PubMed] [Google Scholar]
- 227.Li W., Cheng B. Knockdown of LncRNA NEAT1 inhibits myofibroblast activity in oral submucous fibrosis through miR-760/TPM1 axis. J. Dent. Sci. 2022;17:707–717. doi: 10.1016/j.jds.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Zhang J., Wang H., Chen H., Li H., Xu P., Liu B., Zhang Q., Lv C., Song X. ATF3-activated accelerating effect of LINC00941/lncIAPF on fibroblast-to-myofibroblast differentiation by blocking autophagy depending on ELAVL1/HuR in pulmonary fibrosis. Autophagy. 2022;18:2636–2655. doi: 10.1080/15548627.2022.2046448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Cai W., Xu H., Zhang B., Gao X., Li S., Wei Z., Li S., Mao N., Jin F., Li Y., et al. Differential expression of lncRNAs during silicosis and the role of LOC103691771 in myofibroblast differentiation induced by TGF-beta 1. Biomed. Pharmacother. 2020;125:109980. doi: 10.1016/j.biopha.2020.109980. [DOI] [PubMed] [Google Scholar]
- 230.Wang J., Zhang S., Li X., Gong M. LncRNA SNHG7 promotes cardiac remodeling by upregulating ROCK1 via sponging miR-34-5p. Aging. 2020;12:10441–10456. doi: 10.18632/aging.103269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Lee Y.-H., Yu C.-C., Hsieh P.-L., Liao Y.-W., Yu C.-H., Su T.-R. Inhibition of lncRNA HOTTIP ameliorated myofibroblast activities and inflammatory cytokines in oral submucous fibrosis. J. Formos. Med. Assoc. 2021;120:1188–1193. doi: 10.1016/j.jfma.2020.11.013. [DOI] [PubMed] [Google Scholar]
- 232.Wu Q., Jiao B., Gui W., Zhang Q., Wang F., Han L. Long non-coding RNA SNHG1 promotes fibroblast-to-myofibroblast transition during the development of pulmonary fibrosis induced by silica particles exposure. Ecotoxicol. Environ. Saf. 2021;228:112938. doi: 10.1016/j.ecoenv.2021.112938. [DOI] [PubMed] [Google Scholar]
- 233.Kong N., Bao Y., Zhao H., Kang X., Tai X., Chen X., Guo W., Shen Y. Long Noncoding RNA LINC01518 Modulates Proliferation and Migration in TGF-beta 1-Treated Human Tenon Capsule Fibroblast Cells Through the Regulation of hsa-miR-216b-5p. Neuromolecular Med. 2022;24:88–96. doi: 10.1007/s12017-021-08662-2. [DOI] [PubMed] [Google Scholar]
- 234.Yu C.-H., Fang C.-Y., Yu C.-C., Hsieh P.-L., Liao Y.-W., Tsai L.-L., Chu P.-M. LINC00312/YBX1 Axis Regulates Myofibroblast Activities in Oral Submucous Fibrosis. Int. J. Mol. Sci. 2020;21:2979. doi: 10.3390/ijms21082979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Zhang L., Gao J., Gong A., Dong Y., Hao X., Wang X., Zheng J., Ma W., Song Y., Zhang J., et al. The Long Noncoding RNA LINC00963 Inhibits Corneal Fibrosis Scar Formation by Targeting miR-143-3p. DNA Cell Biol. 2021;41:1034. doi: 10.1089/dna.2021.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were created.