Abstract
Background: Understanding trends in pneumonia-associated hospitalizations can help to quantify the burden of disease and identify risk conditions and at-risk populations. This study evaluated characteristics of hospitalizations due to pneumonia that occurred in Italy in a 10-year period from 2010 to 2019. Methods: All hospitalizations with a principal or secondary diagnosis of pneumonia over the 10-year period were included, which were identified by hospital discharges for all-cause pneumonia and pneumococcal pneumonia in the anonymized hospital discharge database of the Italian Health Ministry. Results: A total of 2,481,213 patients were hospitalized for pneumonia between 2010 and 2019; patients aged 75–86 years accounted for 30.1% of hospitalizations. Most hospitalizations (88.1%) had an unspecified pneumonia discharge code. In-hospital death was recorded in 13.0% of cases. The cumulative cost for pneumonia hospitalizations of the 10-year period were EUR 11,303,461,591. Over the observation period, the incidence rate for hospitalized all-cause pneumonia in any ages increased from 100 per 100,000 in 2010 to over 160 cases per 100,000 per year in 2019 (p < 0.001). Overall, there was a significant increase in annual percent changes in hospitalization rates (+3.47 per year), in-hospital death (+4.6% per year), and costs (+3.95% per year) over the 10-year period. Conclusions: Our analysis suggests that hospitalizations for pneumonia are increasing over time in almost all age groups, especially in the elderly. Given the substantial burden of pneumonia in terms of mortality, healthcare resources, and economic costs, greater public health efforts should thus be made to promote vaccinations against influenza and pneumococcus, particularly in high-risk groups.
Keywords: pneumonia, hospitalizations, Italy, mortality
1. Introduction
Community-acquired pneumonia (CAP) is defined as an acute infection of the lung that is acquired outside of a hospital setting [1]. Streptococcus pneumoniae and respiratory viruses are the most frequently identified pathogens in patients with CAP [1]. CAP is a leading cause of morbidity and mortality, especially in the elderly and in patients who are immunocompromised [1]. In addition to age, various chronic comorbidities such as heart disease, pulmonary disorders, and diabetes can increase the risk of pneumonia [2,3]. In a study from Spain, for example, the risk of hospitalization due to pneumococcal disease in patients with CAP and an underlying cardiac, respiratory, or metabolic comorbidity was 73-fold higher than that in patients with no comorbidity [4]. In the US, the observed annual age-adjusted incidence of patients hospitalized with CAP is 649 cases per 100,000 adults, corresponding to more than 15 million hospitalizations annually, with a mortality rate of 6.5% [5].
The etiology of CAP is often difficult to determine, due to difficulties in collecting representative respiratory specimens and inaccurate methods for microbial detection. Even with extensive testing, the cause of pneumonia can be identified in roughly one-third of patients [6]. Treatment of CAP usually is empirically later adapted according to the identified causative pathogen [1,7].
The incidence of pneumonia hospitalizations has been steadily increasing in recent years [8]. Understanding the burden and trends of community-pneumonia-associated hospitalizations can thus help to provide useful information to quantify the burden of the disease and identify at high-risk populations. Herein, we report incidence rates for CAP hospitalizations in adults in Italy between 2010 and 2019 and describe the demographics, underlying risk factors, and standard-of care etiological diagnosis among hospitalized pneumonia patients.
2. Materials and Methods
2.1. Study Design
This is a retrospective cohort study of the anonymized hospital discharge database of the Italian Health Ministry, summarized as part of a report from Crea Sanità, Rome, Italy, an independent center that carries out economic healthcare evaluations. Data of annual pneumonia hospitalizations in adults aged ≥ 18 years of age/in people of all ages for a 10-year period between 2010 and 2019 were extracted. All-cause pneumonia as the key outcome of interest was defined as ICD 9 CM 480–486 in a principal or secondary diagnosis position pneumonia (Table S1). Case definitions for other pneumonia definitions are defined in supplemental Table S2 and case definitions for underlying comorbidities are described in supplemental Table S3. In addition, the following variables were collected: patient’s place of residency, date of hospital admission, age, sex, length of stay (in days), disposition on admission, discharge disposition, diagnosis related groups (drg), drg weight (measured as the ratio of the mean episode cost in a drg group to the mean cost of episodes in all drgs), and hospitalization costs (in euro).
2.2. Statistical Analysis
Qualitative data are summarized as absolute frequencies and incidence rates (IR; cases per 100,000 population at risk per year). Denominators for incidence rates were calculated using the census population in Italy from 2010 to 2019. Quantitative data are reported as the mean (standard deviation, SD) if normally distributed, otherwise as a median (interquartile range, IQR). Join point analysis was used to evaluate trends over time of hospitalization rates, and average percentage change (APC) and average annual percent change (AAPC) were calculated. According to several studies, the join point analysis is often used to summarize trends in disease and mortality rates, and it is a common estimator that uses a linear model on the log of the age-standardized rates [9].
A p-value < 0.05 was considered statistically significant. Analyses were performed using R Software analysis (version 4.0.5, R Foundation for Statistical Computing, Vienna, Austria) and, as for joinpoint analysis, the packages “Segmented” and “Strucchange” were used (RStudio Team. RStudio: Integrated Development for R. RStudio; PBC: Boston, MA, USA, 2020).
3. Results
3.1. General Characteristics of Hospitalizations for Pneumonia
During the period from 2010 to 2019, there were a total of 2,481,213 hospital discharges for pneumonia (Table 1), of which 89.3% in the adult population (2,215,864 hospitalizations, IR = 440.3 per 100,000 per year). Somewhat more hospitalizations were seen among men (55.3%) than in women (44.7%), for an IR of 468.5 per 100,000 in males and 357.0 per 100,000 in females. Patients from 75–86 years (IR: 1688.5 per 100,000 per year) accounted for 30.1% of all hospitalizations for pneumonia, and the age group from 18–45 years (IR: 71.2 per 100,000 per year) had the lowest number of hospitalizations (6.1%). A slight increase in the number of hospitalizations with pneumonia as the main diagnosis is apparent starting around 2014.
Table 1.
General characteristics of hospitalizations for pneumonia in Italy from 2010 to 2019.
| Total Number of Pneumonia Hospitalizations |
Incidence Rate Per 100,000 |
% | ||
|---|---|---|---|---|
| Total | 2,481,213 | 411.2 | 100% | |
| Gender | ||||
| Male | 1,372,040 | 468.5 | 55.3% | |
| Female | 1,109,103 | 357 | 44.7% | |
| Age (years) | ||||
| <18 | 265,354 | 264.9 | 10.7% | |
| 18–45 | 150,804 | 71.2 | 6.1% | |
| 46–65 | 330,032 | 196.1 | 13.3% | |
| 66–75 | 411,426 | 651.1 | 16.6% | |
| 76–85 | 747,507 | 1688.50 | 30.1% | |
| >85 | 576,095 | 3681.60 | 23.2% | |
| Year | ||||
| 2010 | 218,152 | 365.4 | 8.8% | |
| 2011 | 223,389 | 374.1 | 9.0% | |
| 2012 | 220,349 | 369.0 | 8.9% | |
| 2013 | 229,607 | 384.6 | 9.3% | |
| 2014 | 241,632 | 404.7 | 9.7% | |
| 2015 | 255,607 | 428.1 | 10.3% | |
| 2016 | 246,460 | 412.8 | 9.9% | |
| 2017 | 267,217 | 447.5 | 10.8% | |
| 2018 | 282,850 | 473.7 | 11.4% | |
| 2019 | 295,950 | 495.7 | 11.9% |
Absolute and relative frequencies of specified bacterial, viral and fungal causes are shown in Table 2. Pneumococcal pneumonia was responsible for about 20% of cases, followed by pneumonia from other specified bacteria (17%). Mycoplasma was responsible for almost 13% of cases and pseudomonas in 12%. A multitude of other micro-organisms and viruses were responsible for the remaining cases in smaller proportions.
Table 2.
Absolute and relative frequencies of specified bacterial, viral and fungal causes.
| ICD9-CM Diagnosis Code | ICD9-CM Diagnosis Description | Diagnostic Groups | Total Specified Cases 2010–2019 | % Specified Cases out of Total Specified Cases 2010–2019 |
|---|---|---|---|---|
| 481 | Pneumococcal pneumonia (Streptococcus pneumoniae) | Specified Pneumonia bacterial | 53,879 | 20.44% |
| 482.89 | Pneumonia from other specified bacteria | Specified Pneumonia bacterial | 44,947 | 17.05% |
| 483.0 | Mycoplasma Pneumoniae pneumonia | Specified Pneumonia bacterial | 33,532 | 12.72% |
| 482.1 | Pseudomonas pneumonia | Specified Pneumonia bacterial | 32,106 | 12.18% |
| 482.41 | Staphylococcus aureus pneumonia | Specified Pneumonia bacterial | 18,239 | 6.92% |
| 482.0 | Klebsiella pneumoniae pneumonia | Specified Pneumonia bacterial | 15,824 | 6.00% |
| 487.0 | Influenza with pneumonia | Specified Pneumonia viral | 14,779 | 5.61% |
| 482.82 | Escherichia coli pneumonia [E. coli] | Specified Pneumonia bacterial | 7226 | 2.74% |
| 484.6 | Pneumonia in aspergillosis | Specified Pneumonia fungi | 6525 | 2.47% |
| 483.1 | Chlamydia Pneumonia | Specified Pneumonia bacterial | 6061 | 2.30% |
| 482.2 | Haemophilus influenzae pneumonia (H. influenzae) | Specified Pneumonia bacterial | 5777 | 2.19% |
| 482.30 | Streptococcus pneumonia, unspecified | Specified Pneumonia bacterial | 5301 | 2.01% |
| 480.1 | Respiratory syncytial virus pneumonia | Specified Pneumonia viral | 4914 | 1.86% |
| 482.40 | Staph pneumonia, unspecified | Specified Pneumonia bacterial | 3094 | 1.17% |
| 482.39 | Pneumonia from other Streptococci | Specified Pneumonia bacterial | 2597 | 0.99% |
| 484.1 | Cytomegalovirus pneumonia | Specified Pneumonia viral | 2548 | 0.97% |
| 480.0 | Adenovirus Pneumonia | Specified Pneumonia viral | 2359 | 0.89% |
| 480.2 | Parainfluenza virus pneumonia | Specified Pneumonia viral | 2154 | 0.82% |
| 482.31 | Streptococcus pneumonia, group A | Specified Pneumonia bacterial | 965 | 0.37% |
| 482.32 | Streptococcus pneumonia, group B | Specified Pneumonia bacterial | 390 | 0.15% |
| 484.3 | Pneumonia in whooping cough | Specified Pneumonia bacterial | 225 | 0.09% |
| 480.3 | SARS pneumonia—Associated coronavirus | Specified Pneumonia viral | 163 | 0.06% |
| 484.5 | Pneumonia in anthrax | Specified Pneumonia bacterial | 20 | 0.01% |
| 482.4 | Staph pneumonia | Specified Pneumonia bacterial | 14 | 0.01% |
3.2. Clinical Characteristics of Patients Hospitalized for Pneumonia
Pneumonia was recorded in the primary diagnostic field in 55.4% of cases and in any secondary diagnostic field in 44.6% of cases (Table 3). The vast number of hospitalizations (88.1%) had an unspecified diagnosis (unspecified pneumonia, 31.6%; unspecified bacterial pneumonia, 20.7%; unspecified bronchopneumonia, 35.8%). The median length of hospitalization was 12.3 days (IQR 12.1–12.5); median drg was 1.32 (IQR 1.27–1.36). Regarding comorbidities, 27.3% had at least one comorbidity; chronic respiratory disease (17.7%) was the most frequent, followed by cancer (11.1%) and diabetes (10.9%). While most patients (71.6%) had a routine discharge, of note, in-hospital death was recorded in 13.0% of cases (Table 4). Lastly, over the time period analyzed, average costs for hospitalization amounted to EUR 1,130,346.15 per year.
Table 3.
Clinical and administrative characteristics of hospitalizations for pneumonia in Italy from 2010 to 2019.
| Total Number of Pneumonia Hospitalizations |
Incidence Rate Per 100,000 |
% * | ||
|---|---|---|---|---|
| ICD-9 Pneumonia Code Position | ||||
| Principal position | 1,374,227 | 227.7 | 55.4% | |
| Second position | 1,106,991 | 183.4 | 44.6% | |
| ICD-19 Pneumonia Code | ||||
| Unspecified pneumonia | 783,574 | 129.8 | 31.6% | |
| Unspecified pneumonia viral | 25,290 | 4.2 | 1.0% | |
| Unspecified pneumonia bacterial | 514,174 | 85.2 | 20.7% | |
| Unspecified bronchopneumonia | 889,320 | 147.4 | 35.8% | |
| Specified pneumonia viral | 24,265 | 4.00 | 1.0% | |
| Specified pneumonia bacterial | 224,320 | 37.20 | 9.0% | |
| Specified pneumonia fungal | 5719 | 0.90 | 0.2% | |
| Other | 10,110 | 1.70 | 0.4% | |
| Coinfection | 4441 | 0.70 | 0.2% | |
| Comorbidities | ||||
| Chronic respiratory disease | 438,730 | 72.7 | 17.7% | |
| Chronic cardiovascular disease | 173,437 | 28.7 | 7.0% | |
| Chronic kidney disease | 170,136 | 28.2 | 6.9% | |
| Cancer | 274,394 | 45.5 | 11.1% | |
| Diabetes mellitus | 271,262 | 45 | 10.9% | |
| At least one comorbidity | 677,903 | 112.3 | 27.3% | |
| At least two comorbidities | 230,401 | 38.2 | 9.3% | |
| Three or more comorbidities | 52,023 | 8.6 | 2.1% | |
| Discharge disposition | ||||
| Routine discharge | 1,775,817 | 294.3 | 71.6% | |
| Transfer | 191,474 | 31.7 | 7.7% | |
| In-hospital death | 322,474 | 53.4 | 13.0% | |
| Other | 191,453 | 31.7 | 7.7% | |
* column percentages.
Table 4.
Annual percent changes in hospitalization rates for pneumonia in Italy from 2010 to 2019 stratified by different variables.
| Variable | Annual Percent Change | p-Value | |
|---|---|---|---|
| Raw hospitalization rates | +3.47 | <0.001 | |
| Gender | Male | +3.08 | <0.001 |
| Female | +3.93 | <0.001 | |
| Age (years) | <18 | −4.25 | 0.004 |
| 18–45 | −1.02 | 0.304 | |
| 46–65 | +3.67 | <0.001 | |
| 66–75 | +3.53 | <0.001 | |
| 76–85 | +4.32 | 0.003 | |
| >85 | +7.49 | 0.003 | |
| Diagnosis (Position) | Pneumonia in first diagnosis | +1.35 | 0.011 |
| Pneumonia in secondary diagnosis | +6.18 | 0.003 | |
| Diagnosis | Unspecified pneumonia | +5.48 | 0.002 |
| Unspecified pneumonia viral | +4.60 | 0.009 | |
| Unspecified pneumonia bacterial | +5.86 | <0.001 | |
| Unspecified bronchopneumonia | +0.10 | 0.761 | |
| Specified pneumonia viral | +11.62 | 0.003 | |
| Specified pneumonia bacterial | +3.33 | 0.003 | |
| Specified pneumonia fungi | +6.38 | 0.001 | |
| Other | +5.99 | <0.001 | |
| Coinfection | +16.11 | 0.001 | |
| Comorbidities | Chronic respiratory diseases | +3.60 | <0.001 |
| Chronic cardiovascular diseases | +2.85 | <0.001 | |
| Chronic kidney diseases | +5.21 | <0.001 | |
| Cancer | +3.02 | <0.001 | |
| Diabetes | +1.86 | <0.001 | |
| Comorbidities (number) | At least one comorbidity | +3.76 | <0.001 |
| At least two comorbidities | +2.90 | <0.001 | |
| Three or more comorbidities | +2.19 | 0.002 | |
| Discharge disposition | Routine discharge | +2.13 | 0.001 |
| Transfer | +9.08 | <0.001 | |
| In-hospital death | +4.56 | <0.001 | |
| Other | +9.00 | <0.001 | |
| Hospitalization costs (euro) | +3.95 | <0.001 | |
| In-hospital death | +4.60 | <0.001 | |
| Length of stay (days) | +0.31 | 0.038 | |
| DRG weight * | +0.57 | 0.003 |
* Measured as the ratio of the mean episode cost in a drg group to the mean cost of episodes in all drgs.
3.3. Trends in Hospitalizations over Time
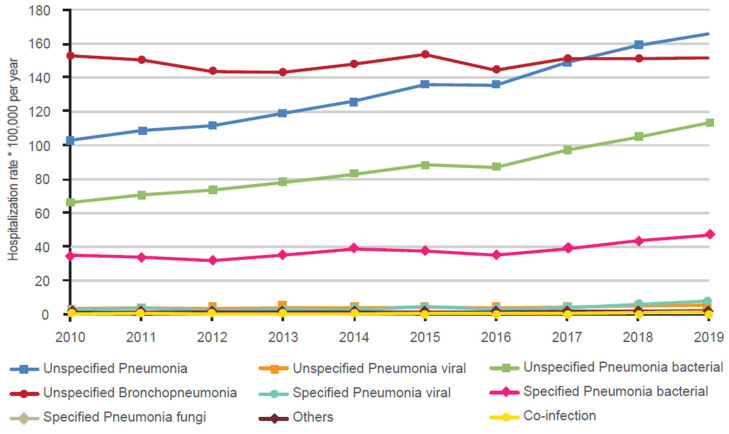
Trends in rates of hospitalizations for pneumonia according to clinical diagnosis are shown in Figure 1. While most of the different diagnoses for pneumonia appeared to be relatively stable during the analyzed time period, there was a marked and steady increase in hospitalizations for unspecified pneumonia from slightly more than 100 cases per 100,000 per year in 2010 to over 160 per 100,000 in 2019 as well as unspecified bacterial pneumonia (from about 65 per 100,000 to in 2010 to about 95 per 100,000 in 2019). With few exceptions, over 2010–2019 there was a significant increase in annual percent changes in hospitalization rates for pneumonia in Italy considering all variables assessed. Significant increases were seen in both men and women, in all age groups except for <18 years and 18–45 years, and in unspecified and specified diagnoses (except unspecified bronchopneumonia). In particular, hospitalization rates in subjects aged <18 years decreased significantly over time by 4.25% per year (from 341.2 per 100,000 in 2010 to 255.4 per 100,000 in 2019; p < 0.001). Moreover, significant increases were observed for all comorbidities as well as discharge diagnoses, including in-hospital death. Accordingly, costs for hospitalization and median length of stay also significantly increased by 3.95% and 0.31 (days per year), respectively.
Figure 1.
Trends in hospitalization rates over time according to clinical diagnosis in Italy (2010–2019).
4. Discussion
Pneumonia represents a serious public health issue that is associated with high medical burden and substantial economic costs, in addition to hospitalizations and mortality in individuals of all age groups [10]. Herein, we studied hospitalizations and in-hospital mortality in patients with main and secondary diagnoses of pneumonia in Italy over a 10-year period spanning 2010–2019. During this period, there were almost 2.5 million hospitalizations for pneumonia and more than 322,000 related in-hospital deaths. One of the main findings from our analysis arises that hospitalizations for unspecified pneumonia have steadily increased by about 60% during 2010–2019, with an in-hospital mortality rate of 13%. The increased number of hospitalizations for pneumonia was also apparent across all age groups and comorbidities assessed. In addition, during the 10-year period, total costs for hospitalization for pneumonia were well over EUR 11,000,000,000, confirming the huge economic burden of pneumonia for healthcare systems. In particular, considering that before the SARS-CoV-2 the total Italian health fund was about EUR 110 billion per year, we can estimate that hospitalizations for pneumonia in Italy every year requires more than 1% of total healthcare expenditure.
The annual incidence of hospitalizations for pneumonia observed herein are broadly similar to those reported in a US study assessing hospitalizations for CAP with an annual incidence of 649 patients per 100,000 adults using data from 2014–2016 [5]. In that analysis, mortality at 30 days was 13%, which compares well to the 13% observed herein (in-hospital deaths). In a Dutch study, in-hospital mortality from CAP in patients aged ≥65 years was 11.3% [11]. Similar to our data, the mean duration of hospitalization was 12.1 days [11] compared to a median of 12.3 in our study. As expected, the incidence of hospitalizations for pneumonia also increased with age as seen herein, with a rate of 69 per 100,000 in those 18–24 years and 3951 per 100,000 in those ≥85 years [5]. However, from our data it can be noted that the incidence rate among those <18 years was almost double that seen in the 18–45 year age group. Similar results were reported in a study from Canada, wherein hospitalizations for all-cause pneumonia were highest in children <5 years and in adults >70 years of age and rates of mortality (11.6–12.3%) similar to those observed in our study [12]. However, over time we found a statistically significant reduction in hospitalization rates in subjects aged <18 years, which could be in large part attributable to the increased pneumococcal vaccination coverage observed in children in Italy during the study period [13]. Our results are also relevant considering older that individuals who are hospitalized very often have comorbidities and complications that have a negative impact on health and recovery. In fact, admissions in patients ≥65 years of age represented 69.9% of all hospitalizations.
The increasing number of hospitalizations with an unspecified diagnosis of pneumonia from 2010–2019 is of further interest, with significant increases seen across all age subgroups and comorbidities. First, this indicates that bacterial testing is often not performed in-hospital, as previously reported [14]. Second, it highlights the need for preventive strategies as noted in recent studies, which stress the use of pneumococcal vaccination in older individuals and in those with risk factors such as chronic obstructive pulmonary disease, male gender, and diabetes [15,16]. Third, the lack of an etiologic diagnosis may increase the risk of overuse, inappropriate, or inefficient antimicrobial therapy and, ultimately, the selection of resistant and multi-drug resistant bacteria [17].
It is well known that pneumonia hospitalization trends in general population can be significantly modified by pneumococcal, influenza and COVID-19 vaccination coverage. In particular, influenza vaccination has been associated with reduced severity of CAP and improved overall survival during influenza seasons in patients with CAP [18]. In recent years, SARS-CoV-2 has also contributed to the pneumonia burden of diseases, although in our study this pathogen had no impact [19]. However, some studies have suggested that COVID-19 vaccines provide high protection against pneumonia and reduce severity of pneumonia [20,21].
Pneumococcal pneumonia was responsible for about one-fifth of all cases of hospitalizations for pneumonia in the present study. Vaccination against pneumococcus has been available since 1983, and immunization has substantially reduced the burden of pneumococcal disease in children and the elderly [22]. A study on the efficacy of a polysaccharide conjugate vaccine (PCV), PCV-13, against vaccine-type pneumococcal pneumonia has reported a vaccine efficacy of 46% among older adults and 40% among older adults with underlying at-risk conditions [23,24]. A vaccine effectiveness of around 70% has been reported for PCV-13 in older adults hospitalized for vaccine-type community-acquired pneumonia in the US [25]. These results are in contrast to a more recent analysis of PPV-23 which suggested that the vaccine does not prevent hospitalizations due to community-acquired pneumonia [26]. However, it would seem intuitive that the introduction of vaccines covering additional subtypes would be advantageous [27]. In most countries, the polysaccharide PCV-13 or PPV-23 vaccines (or both) are currently recommended in older individuals [1].
Notwithstanding, while rates of pneumococcal disease caused by specific serotypes of Streptococcus pneumoniae may decrease substantially with vaccination, pneumonia caused by other serotypes may increase proportionally and thus continuous monitoring should be implemented in order to evaluate the epidemiological impact of pneumococcal disease and vaccination strategies. In a study in England, for example, the rate of pneumococcal disease caused by PCV-7 types decreased by 97% after the introduction of the PCV-7 vaccine, although the rates of pneumonia caused by non-PCV-7 serotypes later doubled [28]. In a recent analysis in the US, it was noted that compared to PCV13, the additional serotypes covered by PCV-15 and PCV-20 still have a substantial contribution to the clinical and economic burden of pneumococcal disease [29]. The newly licensed PCV-20 and PCV-15 help to address the unmet need of protecting adults against the increased burden of pneumococcal disease due to serotypes not included in PCV13. The long-term benefits of vaccination with next-generation vaccines will depend on the evolution of pneumococcal serotypes over time, which is difficult to predict.
There are limitations to our study. Hospital claims data are subject to outcome misclassification and bias, which may have impacted the validity of our findings. This aspect depends on the quality of the codifying report, and we cannot exclude variation of the codification process occurred between different regions or in different years. Additionally, our analysis has only included hospitalized pneumonia cases and no conclusions can be drawn on the overall CAP burden in Italy. In this sense, it should be also noted that the difficulty in microbial detection and the lack of information about pneumococcal vaccination status in hospitalized patients may also affect the true trends of pneumococcal pneumonia as well as the evaluation of vaccine effectiveness.
Despite these limitations, our study shows that hospitalizations for pneumonia have increased between 2010 and 2019, especially in the elderly and frail subjects. Unfortunately, there is no data on the current coverage of pneumococcal vaccination in subjects ≥65 years of age. Our data highlight that pneumonia is responsible for the substantial burden in terms of mortality, healthcare resources, and economic costs. Greater public health efforts should thus be made to promote vaccination against respiratory infectious diseases, especially in subjects at a higher risk for severe sequelae.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines11010187/s1, Table S1: ICD 9 CM codes used to identify hospitalizations for pneumonia; Table S2: ICD 9 CM codes used to identify the different possible underlying comorbidities observed in each hospitalization; Table S3: ICD 9 CM codes used to identify the different possible causes of pneumonia.
Author Contributions
Conceptualization, A.P., E.A.M., E.A. and F.V.; All authors (A.P., E.A.M., E.A., F.V., D.d., C.C., B.P. and F.S.) made substantial contributions to drafting this review article. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
According to the Italian law, this study did not require ethical approval.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data analysed in this study will be made available, as aggregates, following reasonable request sent to the corresponding Author of the article.
Conflicts of Interest
The authors declare the following financial interests/personal relationships, which may be regarded as potential competing interests: A.P. and E.A.M. are employees of Pfizer and may hold Pfizer stock or stock options. F.V. and E.A. received funding/support from Pfizer. D.d’, C.C., B.P. and F.S. have no conflicts of interest regarding this manuscript.
Funding Statement
Medical writing support was provided by MA-CRO Lifescience Srl and was funded by Pfizer. Editorial support was provided by MA-CRO Lifescience Srl and was funded by Pfizer. F.V. and E.A. received an honorarium from Pfizer in connection with the development of this manuscript.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Aliberti S., Dela Cruz C.S., Amati F., Sotgiu G., Restrepo M.I. Community-acquired pneumonia. Lancet. 2021;398:906–919. doi: 10.1016/S0140-6736(21)00630-9. [DOI] [PubMed] [Google Scholar]
- 2.Almirall J., Serra-Prat M., Bolibar I., Balasso V. Risk Factors for Community-Acquired Pneumonia in Adults: A Systematic Review of Observational Studies. Respiration. 2017;94:299–311. doi: 10.1159/000479089. [DOI] [PubMed] [Google Scholar]
- 3.Fung H.B., Monteagudo-Chu M.O. Community-acquired pneumonia in the elderly. Am. J. Geriatr. Pharmacother. 2010;8:47–62. doi: 10.1016/j.amjopharm.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Gil-Prieto R., Pascual-Garcia R., Walter S., Alvaro-Meca A., Gil-De-Miguel A. Risk of hospitalization due to pneumococcal disease in adults in Spain. The CORIENNE study. Hum. Vaccines Immunother. 2016;12:1900–1905. doi: 10.1080/21645515.2016.1143577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramirez J.A., Wiemken T.L., Peyrani P., Arnold F.W., Kelley R., Mattingly W.A., Nakamatsu R., Pena S., Guinn B.E., Furmanek S.P., et al. Adults Hospitalized With Pneumonia in the United States: Incidence, Epidemiology, and Mortality. Clin. Infect. Dis. 2017;65:1806–1812. doi: 10.1093/cid/cix647. [DOI] [PubMed] [Google Scholar]
- 6.Carugati M., Aliberti S., Reyes L.F., Franco Sadud R., Irfan M., Prat C., Soni N.J., Faverio P., Gori A., Blasi F., et al. Microbiological testing of adults hospitalised with community-acquired pneumonia: An international study. ERJ Open Res. 2018;4:00096-2018. doi: 10.1183/23120541.00096-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carugati M., Franzetti F., Wiemken T., Kelley R.R., Peyrani P., Blasi F., Ramirez J., Aliberti S. De-escalation therapy among bacteraemic patients with community-acquired pneumonia. Clin. Microbiol. Infect. 2015;21:936.e11–936.e18. doi: 10.1016/j.cmi.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 8.ECDC Surveillance Report. Invaasive Pneumococcal Disease. Annual Epidemiological Report. [(accessed on 4 December 2022)]. Available online: https://www.ecdc.europa.eu/en/surgical-site-infections/surveillance-and-disease-data/all-annual-epidemiological-reports.
- 9.Fay M.P., Tiwari R.C., Feuer E.J., Zou Z. Estimating average annual percent change for disease rates without assuming constant change. Biometrics. 2006;62:847–854. doi: 10.1111/j.1541-0420.2006.00528.x. [DOI] [PubMed] [Google Scholar]
- 10.Assefa M. Multi-drug resistant gram-negative bacterial pneumonia: Etiology, risk factors, and drug resistance patterns. Pneumonia. 2022;14:4. doi: 10.1186/s41479-022-00096-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vissink C.E., Huijts S.M., de Wit G.A., Bonten M.J., Mangen M.J. Erratum to: Hospitalization costs for community-acquired pneumonia in Dutch elderly: An observational study. BMC Infect. Dis. 2016;16:702. doi: 10.1186/s12879-016-2015-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McNeil S.A., Qizilbash N., Ye J., Gray S., Zanotti G., Munson S., Dartois N., Laferriere C. A Retrospective Study of the Clinical Burden of Hospitalized All-Cause and Pneumococcal Pneumonia in Canada. Can. Respir. J. 2016;2016:3605834. doi: 10.1155/2016/3605834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ministero Della Saulte [(accessed on 24 August 2022)]; Available online: https://www.salute.gov.it/portale/documentazione/p6_2_8_3_1.jsp?lingua=italiano&id=20.
- 14.Amodio E., Costantino C., Boccalini S., Tramuto F., Maida C.M., Vitale F. Estimating the burden of hospitalization for pneumococcal pneumonia in a general population aged 50 years or older and implications for vaccination strategies. Hum Vaccines Immunother. 2014;10:1337–1342. doi: 10.4161/hv.27947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dirmesropian S., Liu B., Wood J.G., MacIntyre C.R., McIntyre P., Karki S., Jayasinghe S., Newall A.T. Pneumonia hospitalisation and case-fatality rates in older Australians with and without risk factors for pneumococcal disease: Implications for vaccine policy. Epidemiol. Infect. 2019;147:e118. doi: 10.1017/S0950268818003473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Konomura K., Nagai H., Akazawa M. Economic burden of community-acquired pneumonia among elderly patients: A Japanese perspective. Pneumonia. 2017;9:19. doi: 10.1186/s41479-017-0042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hillock N.T., Merlin T.L., Turnidge J., Karnon J. Modelling the Future Clinical and Economic Burden of Antimicrobial Resistance: The Feasibility and Value of Models to Inform Policy. Appl. Health Econ. Health Policy. 2022;20:479–486. doi: 10.1007/s40258-022-00728-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tessmer A., Welte T., Schmidt-Ott R., Eberle S., Barten G., Suttorp N., Schaberg T., Group C.S. Influenza vaccination is associated with reduced severity of community-acquired pneumonia. Eur. Respir. J. 2011;38:147–153. doi: 10.1183/09031936.00133510. [DOI] [PubMed] [Google Scholar]
- 19.Tang H.J., Lai C.C., Chao C.M. Changing Epidemiology of Respiratory Tract Infection during COVID-19 Pandemic. Antibiotics. 2022;11:315. doi: 10.3390/antibiotics11030315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murillo-Zamora E., Trujillo X., Huerta M., Rios-Silva M., Guzman-Esquivel J., Benites-Godinez V., Ochoa-Castro M.R., Guzman-Solorzano J.A., Mendoza-Cano O. COVID-19 vaccines provide better protection against related pneumonia than previous symptomatic infection. Int. J. Infect. Dis. 2022;120:142–145. doi: 10.1016/j.ijid.2022.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wada N., Li Y., Hino T., Gagne S., Valtchinov V.I., Gay E., Nishino M., Madore B., Guttmann C.R.G., Bond S., et al. COVID-19 Vaccination reduced pneumonia severity. Eur. J. Radiol. Open. 2022;9:100456. doi: 10.1016/j.ejro.2022.100456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim G.L., Seon S.H., Rhee D.K. Pneumonia and Streptococcus pneumoniae vaccine. Arch. Pharmacal Res. 2017;40:885–893. doi: 10.1007/s12272-017-0933-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suaya J.A., Jiang Q., Scott D.A., Gruber W.C., Webber C., Schmoele-Thoma B., Hall-Murray C.K., Jodar L., Isturiz R.E. Post hoc analysis of the efficacy of the 13-valent pneumococcal conjugate vaccine against vaccine-type community-acquired pneumonia in at-risk older adults. Vaccine. 2018;36:1477–1483. doi: 10.1016/j.vaccine.2018.01.049. [DOI] [PubMed] [Google Scholar]
- 24.Bonten M.J., Huijts S.M., Bolkenbaas M., Webber C., Patterson S., Gault S., van Werkhoven C.H., van Deursen A.M., Sanders E.A., Verheij T.J., et al. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N. Engl. J. Med. 2015;372:1114–1125. doi: 10.1056/NEJMoa1408544. [DOI] [PubMed] [Google Scholar]
- 25.McLaughlin J.M., Jiang Q., Isturiz R.E., Sings H.L., Swerdlow D.L., Gessner B.D., Carrico R.M., Peyrani P., Wiemken T.L., Mattingly W.A., et al. Effectiveness of 13-Valent Pneumococcal Conjugate Vaccine Against Hospitalization for Community-Acquired Pneumonia in Older US Adults: A Test-Negative Design. Clin. Infect. Dis. 2018;67:1498–1506. doi: 10.1093/cid/ciy312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chandler T., Furmanek S., Carrico R., Balcom D., Arnold F., Ramirez J. 23-Valent Pneumococcal Polysaccharide Vaccination Does Not Prevent Community-Acquired Pneumonia Hospitalizations Due to Vaccine-Type Streptococcus pneumoniae. Microorganisms. 2022;10:560. doi: 10.3390/microorganisms10030560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Torres A., Menendez R., Espana P.P., Fernandez-Villar J.A., Marimon J.M., Cilloniz C., Mendez R., Egurrola M., Botana-Rial M., Ercibengoa M., et al. The Evolution and Distribution of Pneumococcal Serotypes in Adults Hospitalized With Community-Acquired Pneumonia in Spain Using a Serotype-Specific Urinary Antigen Detection Test: The CAPA Study, 2011-2018. Clin. Infect. Dis. 2021;73:1075–1085. doi: 10.1093/cid/ciab307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ladhani S.N., Collins S., Djennad A., Sheppard C.L., Borrow R., Fry N.K., Andrews N.J., Miller E., Ramsay M.E. Rapid increase in non-vaccine serotypes causing invasive pneumococcal disease in England and Wales, 2000–2017: A prospective national observational cohort study. Lancet Infect. Dis. 2018;18:441–451. doi: 10.1016/S1473-3099(18)30052-5. [DOI] [PubMed] [Google Scholar]
- 29.Huang L., Wasserman M., Grant L., Farkouh R., Snow V., Arguedas A., Chilson E., Sato R., Perdrizet J. Burden of pneumococcal disease due to serotypes covered by the 13-valent and new higher-valent pneumococcal conjugate vaccines in the United States. Vaccine. 2022;40:4700–4708. doi: 10.1016/j.vaccine.2022.06.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data analysed in this study will be made available, as aggregates, following reasonable request sent to the corresponding Author of the article.