Abstract
Previous studies have generally reported the association between serum uric acid (SUA) and diabetic complications, but large-scale research exploring the above association in U.S. adults with diabetes is limited. To explore the association between SUA and chronic complications of diabetes among U.S. patients aged ≥40, we used data from the National Health and Nutrition Examination Survey 1999–2008. SUA was divided into three levels: T1 (SUA ≥ 420 μmol/L), T2 (300 ≤ SUA < 420 μmol/L), and T3 (SUA < 300 μmol/L). Binary logistic regression and restricted cubic spline analysis were applied to evaluate the association between SUA and chronic complications of diabetes. A trend test was performed as the SUA increased substantially. After full-adjusted confounding factors, patients in the T3 group had a lower risk of diabetic kidney disease, cardiovascular disease, and peripheral neuropathy compared with the T1 group, with a OR (95% CIs) of 0.33 (0.21–0.52), 0.56 (0.36–0.87), and 0.49 (0.27–0.89), respectively. The restricted cubic spline showed a significant positive relationship between SUA and cardiovascular disease and diabetic kidney disease in diabetes patients, but not peripheral neuropathy. Maintaining a SUA of less than 300 μmol/L might be protective against the risk of cardiovascular disease, diabetic kidney disease, and peripheral neuropathy other than diabetic retinopathy compared with a SUA of more than 420 μmol/L in U.S. diabetes patients aged 40 and over.
Keywords: uric acid, diabetic chronic complications, cardiovascular disease, diabetic kidney disease, diabetic peripheral neuropathy, diabetic retinopathy
1. Introduction
Diabetes mellitus (DM), a complex and common metabolic disorder, occurs when the β cells of islets are unable to synthesize sufficient insulin or when the body is unable to use the insulin effectively. The prevalence of diabetes in adults has nearly doubled since 1980 (4.7% to 8.5%), with a steady increase globally, especially in middle-income countries [1,2]. Numerous previous studies have improved the understanding of pathogenesis of diabetes, whereas the prevalence of diabetes remains high due to changes in dietary patterns and related metabolic disorders, such as obesity and dyslipidemia. People with diabetes need continuous medical care and self-management education. Current treatments generally focus on slowing disease progression and preventing diabetic complications [3,4]. A chronic complication of DM is damage of blood vessels, due to long-term elevation of serum glucose levels, segmented under diabetic macrovascular disease and microvascular disease by vessel sizes [4]. Serum glucose variability and variability of blood pressure, obesity, and dyslipidemia are common risk factors for diabetic complications [5]. Previous studies suggested that uric acid (UA) might correlated with the development of diabetic complications, whereas the evidence was controversial [6,7,8,9]. Lu et al. found that SUA was associated with an increased prevalence of diabetic kidney disease (DKD) and cardiovascular disease (CVD) in men and postmenopausal women with DM [7].
Serum uric acid (SUA) is the ultimate product of purine metabolism [10]. Approximately two-thirds of UA is excreted by the kidneys and one-third is excreted by the gastrointestinal tract, and its synthesis and excretion are balanced under physiological conditions [11]. The onset of hyperuricemia is associated with overproduction or underexcretion of SUA [12]. Epidemiological studies suggested that the overall prevalence of hyperuricemia and gout has increased over the past decades [13,14]. Hyperuricemia is the precursor of gout, and apart from the involvement of joints, it is often accompanied by various comorbidities, including CVD, diabetes, chronic kidney disease, obesity, and dyslipidemia [10,15,16]. Hyperuricemia is positively correlated with the incidence of type 2 DM and the risk of DM reaching up to 27% in gout patients with SUA > 9 mg/dL [17,18]. The potential mechanism might be that hyperuricemia is correlated with increased insulin resistance and decreased release of insulin [18,19].
Previous clinical studies suggested that higher UA was correlated with a higher risk of CVD, DKD, and peripheral neuropathy (PN) in diabetes [6,7,8,9]. However, in their study of 4767 DM participants, Lu et al. found that SUA was not related to diabetic retinopathy (DR) in Chinese adults [7]. Previous research has generally reported the association between SUA and one certain type of diabetic complications, but large-scale research exploring the above association in U.S. adults with diabetes is limited. We performed this study with a nationally representative sample of U.S. DM patients whose data were obtained from the National Health and Nutrition Examination Survey (NHANES) 1999–2008 to investigate the relationship between SUA and diabetic chronic complications. We first explored the above relationship using NHANES data. Logistic regression analysis and restricted cubic spline analysis were used to detect the above relationship with a nationally representative sample.
2. Materials and Methods
2.1. Data Collection and Sample
NHANES collects the nutritional and health information of the U.S. population, which is conducted by the Centers for Disease Control and Prevention of America every 2 years. The survey consists of an in-home interview and physical examination, as well as urine and blood sample collection taken at a mobile examination center [20]. As the examinations on fundus and peripheral neuropathy were only performed in participants aged ≥40 years, our study only involved participants aged 40 and over. Our study was conducted following the Declaration of Helsinki [21].
2.2. Definitions and Measurement
Diabetes was defined as participants who met one of the followings: (1) self-reported diabetes; (2) participants with fasting glucose ≥7.0 mmol/L or HbA1C ≥ 6.5%; (3) currently receiving insulin or hypoglycemic drugs.
2.2.1. Diabetic Kidney Disease
DKD was defined as diabetes with impaired glomerular filtration rate (GFR) and/or the presence of albuminuria. Albuminuria was defined as a ratio of urine albumin to creatinine (ACR) ≥ 30 mg/g. The estimation of GFR (eGFR) used the equation (eGFR = 141 × min (Scr/κ, 1)α × max (Scr/κ, 1)−1.209 × 0.993Age × 1.018 [if female] × 1.159 [if black]) and impaired GFR was defined as a GFR < 60 mL/min/1.73 m2 [22,23].
2.2.2. Cardiovascular Disease
CVD was determined by a combination of standardized medical status questionnaires and self-reported physician diagnoses. Participants were asked the following 5 questions: (1) Have you ever been told that you have congestive heart failure? (2) Have you ever been told that you have coronary heart disease? (3) Have you ever been told that you have angina pectoris? (4) Have you ever been told that you have had a heart attack? (5) Have you ever been told that you have had a stroke?”. If the participant replied “yes” to any of the five questions, then he or she would be diagnosed with CVD [24].
2.2.3. Peripheral Neuropathy
Participants lay on the examination table during the exam. Technicians applied slight pressure to the bottom of each of the participant’s feet at 3 sites with a standard monofilament: (1) plantar-first metatarsal head, (2) plantar-hallux, and (3) plantar-fifth metatarsal head. The above sites were tested in a non-sequential order by the examinee to allow for better discrimination of sensation, and then the number of insensate areas of each foot was calculated. Having at least one insensate site on either foot was diagnosed as PN, corresponding to a reduced sensation to touch [25].
2.2.4. Diabetic Retinopathy
An ophthalmic digital imaging system was used to assess the presence of retinal diseases. Graders evaluated digital images at Wisconsin University. The levels of retinopathy were defined according to the grade protocol. A severity level ≥14 was defined as the presence of retinopathy, and a severity level of 10 to 13 was defined as the absence of retinopathy [26].
2.3. Inclusion and Exclusion Criteria
51,602 participants aged 18 and over were enrolled in the NHANES between 1999 and 2008. Exclusion criteria were as followed: (1) age < 40 year; (2) participants whose SUA data were not available; (3) self-reported malignancy disease; (4) being pregnant or breastfeeding; (5) participants without diabetes.
After screening complete data on urine ACR, serum creatinine, or standardized medical status questionnaires, 3075 and 3106 diabetic patients aged 40 and over were involved in the analysis of DKD and CVD, respectively.
After screening complete data on peripheral neuropathy and fundus photography examinations, 1453 and 1233 diabetic patients aged 40 and over were involved in the analysis of PN and DR, respectively.
2.4. Variables
Variables in our study included age, sex, race, and education level. A waist circumference of more than 102 cm in men or more than 88 cm in women is defined as elevated waist circumference. Poverty income ratio (PIR) was used to define family income, with a PIR lower than 1.0 representing that live under the poverty line. This study also included total cholesterol, triglyceride, glycohemoglobin, and smoking status. The history of hypertension is defined as the self-reported diagnosis of hypertension by a doctor. The interval between the age at screening and the age at which they were first told they had diabetes was used to calculate the duration of diabetes (year). DM patients who were diagnosed less than 1 year were counted as half a year.
2.5. Statistical Analysis
All statistical analyses in our study were conducted with SPSS 23 and R 4.2.2. Non-normally distributed continuous variables were described with median (interquartile range). The Kruskal–Wallis test was used to compare the median among different SUA groups. The categorical variables were described with numbers (percentages) and the Chi-square test was used to compare the percentages among different SUA groups. The Bonferroni test was applied for the intergroup comparison. SUA in our study was divided into three levels: T1 (SUA ≥ 420 μmol/L), T2 (300 ≤ SUA < 420 μmol/L), and T3 (SUA < 300 μmol/L). T1 group was the reference group. Binary logistic regression explored the association between SUA and chronic complications of diabetes. Age, race, and gender were adjusted in Model 1, and Model 2 was additionally adjusted for hypertension, waist circumference, smoking, PIR, education, serum lipids, glycohemoglobin, and duration of diabetes. A trend test was performed as the SUA levels increased and logistic regression was performed to calculate the ORs with per SD increase in UA. We performed restricted cubic spline analysis with 3 knots of the SUA levels to characterize the dose–response relationship between SUA and diabetic complications in logistic regression Model 2. A two-sided p < 0.05 was considered statistically significant.
3. Results
3.1. Clinical Features of Included DM Patients
We summarized the clinical features of the involved diabetes patients for the analysis of cardiovascular disease (Table 1). The mean age was 64.12 ± 11.67 years and the mean duration was 12.87 ± 13.66 years. The mean eGFR of patients was 79.9 ± 25.03 mL/min/1.73 m2 and the mean SUA was 341.85 ± 96.26 μmol/L. A greater proportion of males belonged to the highest SUA levels (p < 0.01). With the increasing SUA levels, the median of HbA1c gradually decreased (p < 0.01), while the median of triglyceride, waist circumference, and creatinine gradually increased (p < 0.01). The proportion of smoking and prevalence of hypertension gradually increased with the increase of SUA levels (p < 0.01). The clinical characteristics of involved DM patients for the analysis of DKD, PN, and DR are presented in Tables S1–S3. The percentage of patients with different diabetic chronic complications across different SUA levels are presented in Table 2. The proportion of DKD, CVD, and PN gradually increased with the increase of SUA levels (p < 0.05).
Table 1.
Clinical characteristics of the involved diabetes patients for the analysis of cardiovascular disease (n = 3106).
| SUA Levels | SUA ≤ 300 | 300 < SUA ≤ 420 | SUA > 420 | p Value |
|---|---|---|---|---|
| Age (year) † | 62 (19) | 65 (17) | 67 (16) | <0.01 |
| Males (%) ‡ | 492 (43.3) | 726 (53.6) | 387 (62.9) | <0.01 |
| Race (%) ‡ | <0.01 | |||
| Mexican American | 367 (32.3) | 321 (23.7) | 60 (9.8) | |
| Other Hispanic | 83 (7.3) | 75 (5.5) | 25 (4.1) | |
| Non-Hispanic White | 417 (36.7) | 580 (42.8) | 285 (46.3) | |
| Non-Hispanic Black | 225 (19.8) | 340 (25.1) | 221 (35.9) | |
| Other race | 45 (4.0) | 38 (2.8) | 24 (3.9) | |
| Education level (%) ‡ | <0.01 | |||
| Less than 9th grade | 331 (29.1) | 358 (26.4) | 109 (17.7) | |
| 9–11th grade | 243 (21.4) | 234 (17.3) | 131 (21.3) | |
| High school graduate | 222 (19.5) | 304 (22.5) | 165 (26.8) | |
| College or AA degree | 238 (20.9) | 284 (21.0) | 131 (21.3) | |
| College graduate or above | 103 (9.1) | 173 (12.7) | 79 (12.8) | |
| Waist circumference (cm) † | 101.9 (17.5) | 107.6 (19.3) | 110.3 (19.5) | <0.01 |
| Cholesterol (mmol/L) † | 5.04 (1.47) | 4.91 (1.50) | 4.89 (1.53) | 0.178 |
| Triglyceride (mmol/L) † | 1.72 (1.37) | 1.82 (1.55) | 1.91 (1.48) | <0.01 |
| Creatinine (μmol/L) † | 70.7 (26.52) | 79.6 (26.54) | 99.0 (51.27) | <0.01 |
| Poverty income ratio < 1 (%) ‡ | 238 (22.9) | 275 (22.2) | 98 (17.7) | 0.042 |
| Serum uric acid (μmol/L) † | 255.8 (53.6) | 350.9 (53.6) | 469.9 (71.3) | <0.01 |
| Glycohemoglobin (%) † | 7.2 (2.4) | 6.7 (1.5) | 6.6 (1.3) | <0.01 |
| Taking insulin now (%) ‡ | 208 (18.5) | 221 (16.5) | 130 (21.3) | 0.074 |
| Fasting glucose (mmol/L) † | 7.88 (4.94) | 7.22 (3.27) | 7.22 (2.77) | <0.01 |
| Duration of diabetes (year) † | 9 (13) | 8 (14) | 10 (15) | 0.034 |
| Hypertension (%) ‡ | 602 (52.9) | 911 (67.3) | 481 (78.2) | <0.01 |
| Smoked at least 100 cigarettes in life (%) ‡ | 568 (50.0) | 733 (54.1) | 366 (59.5) | <0.01 |
SUA: Serum uric acid. Data are number of subjects (percentage) or medians (interquartile ranges). † The Kruskal–Wallis test was used to compare the median values among participants in different groups. ‡ Chi-square test was used to compare the percentage among participants in different groups.
Table 2.
The number (percentage) of patients with different chronic complications of diabetes across different serum uric acid levels.
| SUA Levels | SUA ≤ 300 | 300 < SUA ≤ 420 | SUA > 420 | p Value |
|---|---|---|---|---|
| Diabetic kidney disease (%) ‡ | 397 (35.6) | 621 (46.0) | 380 (62.4) | <0.01 |
| Cardiovascular disease (%) ‡ | 252 (22.2) | 385 (28.4) | 252 (41.0) | <0.01 |
| Peripheral neuropathy (%) ‡ | 140 (25.0) | 179 (27.8) | 84 (33.6) | 0.041 |
| Diabetic retinopathy (%) ‡ | 148 (35.0) | 186 (34.1) | 93 (35.1) | 0.947 |
SUA: Serum uric acid. Data are number of subjects (percentage). ‡ Chi-square test was used to compare the percentage among participants in different groups.
The clinical features of DM patients with or without different diabetic chronic complications are shown in Tables S4–S7. Patients with different complications had longer disease course and serum creatinine compared with patients without corresponding complication (p < 0.05). Diabetic complications accounted for greater proportion among patients receiving insulin therapy or hypertensive patients (p < 0.05).
3.2. Serum Uric Acid and Diabetic Kidney Disease
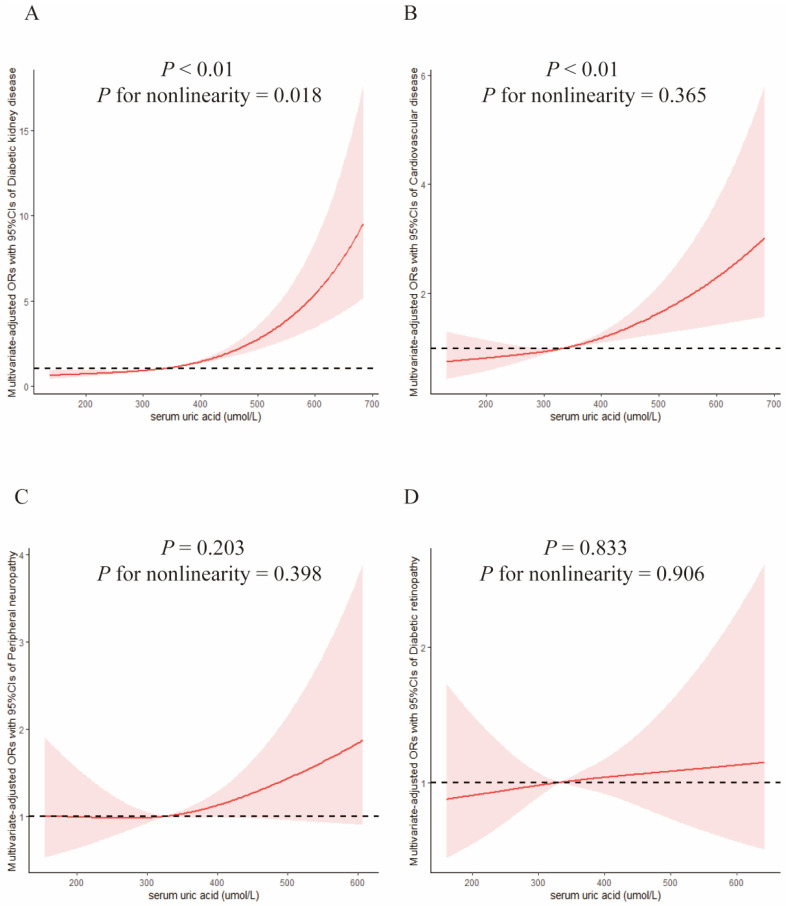
The crude ORs (95% CIs) of DKD were 0.48 (0.38–0.60) and 0.30 (0.23–0.40) in T2 and T3, respectively versus T1 group. In Model 1, the adjusted ORs (95% CIs) were 0.49 (0.39–0.63) and 0.34 (0.25–0.45), respectively, versus T1 group. In Model 2, the ORs (95% Cis) were 0.53 (0.38–0.74) and 0.33 (0.21–0.52), respectively, versus T1 of SUA. The trend test suggested that the ORs of DKD among different SUA groups gradually decreased (p for trend < 0.01) in all three models. Table 3 presented the results of binary logistic regression between SUA levels and the risk of DKD. Figure 1A presented the dose–response relationship between SUA and DKD. Uric acid was positively associated with the risk of DKD and presented a nonlinear dose–response relationship (p < 0.01, p for nonlinearity = 0.018). The reference point (OR = 1.0) of uric acid in the restricted cubic spline analysis was 334.41 μmol/L.
Table 3.
Weighted odds ratios (95% confidence intervals) for chronic complication of people with diabetes across different levels of serum uric acid (SUA) (n = 3106).
| Case/Participants | Crude † | Model 1 † | Model 2 † | |
|---|---|---|---|---|
| Cardiovascular disease | ||||
| SUA > 420 | 615/3106 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| 300 < SUA ≤ 420 | 1354/3106 | 0.54 (0.41–0.70) ** | 0.58 (0.44–0.77) ** | 0.61 (0.41–0.90) * |
| SUA ≤ 300 | 1137/3106 | 0.42 (0.32–0.56) ** | 0.54 (0.39–0.73) ** | 0.56 (0.36–0.87) * |
| p for trend | <0.01 | <0.01 | <0.05 | |
| Diabetic kidney disease | ||||
| SUA > 420 | 609/3075 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| 300 < SUA ≤ 420 | 1350/3075 | 0.48 (0.38–0.60) ** | 0.49 (0.39–0.63) ** | 0.53 (0.38–0.74) ** |
| SUA ≤ 300 | 1116/3075 | 0.30 (0.23–0.40) ** | 0.34 (0.25–0.45) ** | 0.33 (0.21–0.52) ** |
| p for trend | <0.01 | <0.01 | <0.01 | |
| Diabetic peripheral neuropathy | ||||
| SUA > 420 | 250/1453 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| 300 < SUA ≤ 420 | 643/1453 | 0.59 (0.42–0.84) ** | 0.65 (0.45–0.94) * | 0.59 (0.36–0.95) * |
| SUA ≤ 300 | 560/1453 | 0.49 (0.33–0.73) ** | 0.62 (0.40–0.97) * | 0.49 (0.27–0.89) * |
| p for trend | <0.01 | 0.07 | <0.05 | |
| Diabetic retinopathy | ||||
| SUA > 420 | 265/1233 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref) |
| 300 < SUA ≤ 420 | 545/1233 | 0.89 (0.56–1.44) | 1.00 (0.61–1.64) | 1.01 (0.54–1.91) |
| SUA ≤ 300 | 423/1233 | 0.97 (0.66–1.43) | 1.20 (0.77–1.86) | 0.89 (0.53–1.50) |
| p for trend | 0.99 | 0.35 | 0.62 |
SUA: Serum uric acid. † Calculated using binary logistic regression. Model 1 adjusted for age, gender, and race. Model 2 adjusted for poverty–income ratio, waist circumference, smoking status, education level, hypertension, serum triglyceride, total cholesterol, courses of diabetes (year), and HbA1c. * p < 0.05. ** p < 0.01.
Figure 1.
Examination of the dose–response relationship between serum uric acid (μmol/L) and the risk of diabetic chronic complications by restricted cubic splines model. The restricted cubic splines model adjusted for age, gender, race, poverty–income ratio, waist circumference, smoking status, education level, hypertension, serum triglyceride, total cholesterol, courses of diabetes, and HbA1c. (A) Diabetic kidney disease; (B) Cardiovascular disease; (C) Peripheral neuropathy; (D) Diabetic retinopathy.
3.3. Serum Uric Acid and Cardiovascular Disease
The ORs (95% CIs) of CVD were 0.54 (0.41–0.70) and 0.42 (0.32–0.56) in T2 and T3, respectively, versus the T1 group. In Model 2, the ORs (95% CIs) were 0.61 (0.41–0.90) and 0.56 (0.36–0.87), respectively, versus the T1 group. The trend test suggested that the ORs of CVD among different groups gradually decreased (p for trend < 0.05) in all three models. Detailed results are shown in Table 3. The dose–response relationship between uric acid and CVD is presented in Figure 1B. SUA levels were positively associated with the risk of CVD in diabetic patients aged 40 and over (p < 0.01, p for nonlinearity = 0.36). The reference point (OR = 1.0) of uric acid in the restricted cubic spline analysis was 332.41 μmol/L.
3.4. Serum Uric Acid and Peripheral Neuropathy
In Model 2, the multivariate-adjusted ORs (95% CIs) of PN were 0.59 (0.36–0.95) and 0.49 (0.27–0.89), respectively, versus T1 group. The trend test suggested that the ORs of PN among different SUA levels gradually decreased in crude model and full-adjusted Model 2 (p for trend < 0.05). Detailed results are shown in Table 3. Figure 1C presents dose–response relationship between SUA and PN. The reference point (OR = 1.0) of uric acid in the restricted cubic spline analysis was 327.27 μmol/L, and SUA was not significantly associated with the risk of PN among diabetic patients aged 40 and over (p = 0.20).
3.5. Serum Uric Acid and Diabetic Retinopathy
The relationship between SUA and DR and the trend test was insignificant in all three models (p for trend > 0.05). Detailed results are shown in Table 3. Figure 1D presented the dose–response relationship between SUA and DR. The reference point (OR = 1.0) of uric acid in the restricted cubic spline analysis was 333.69 μmol/L and uric acid was not significantly associated with the risk of DR in diabetic patients aged 40 and over (p = 0.83).
3.6. ORs of Diabetic Complications with per SD Increase of Uric Acid
We performed logistic regression to calculate the ORs per SD increase in UA, and the results are shown in Table 4. Uric acid was positively correlated with the risk of DKD and CVD after fully adjusting the confounding factors, and the ORs with per SD increase in SUA was 1.61 (1.35–1.92) and 1.21 (1.04–1.42). Uric acid was positively associated with the risk of PN in the crude model and the ORs with per SD increase in uric acid was 1.23 (1.06–1.43). However, SUA was not correlated with the risk of DR and PN in Model 2.
Table 4.
Weighted odds ratios (95% confidence intervals) for chronic complications of people with diabetes with the increase per standard deviation uric acid.
| Crude † | Model 1 † | Model 2 † | |
|---|---|---|---|
| Diabetic kidney disease | 1.64 (1.49–1.82) ** | 1.59 (1.44–1.75) ** | 1.61 (1.35–1.92) ** |
| Cardiovascular disease | 1.41 (1.27–1.56) ** | 1.29 (1.16–1.44) ** | 1.21 (1.04–1.42) * |
| Peripheral neuropathy | 1.23 (1.06–1.43) ** | 1.19 (0.95–1.32) | 1.23 (0.97–1.55) |
| Diabetic retinopathy | 0.99 (0.85–1.15) | 0.92 (0.77–1.10) | 0.99 (0.81–1.22) |
† Calculated using binary logistic regression. Model 1 adjusted for age, gender and race. Model 2 adjusted for poverty–income ratio, waist circumference, smoking status, education level, hypertension, serum triglyceride, total cholesterol, courses of diabetes (year), HbA1c. * p < 0.05. ** p < 0.01.
4. Discussion
Our study found that SUA levels ≤ 300 μmol/L might be a protective factor for the incidence of DKD, CVD, and PN compared with patients with a SUA level > 420 μmol/L. No correlation was observed between SUA and diabetic retinopathy. Uric acid was positively correlated with the risk of diabetic kidney disease and cardiovascular disease with per increase of SD. Restricted cubic spline revealed that SUA was positively associated with the risk of CVD and CVD.
Previous studies usually reported the relationship between SUA and one certain type of diabetic complication, and there were limited large-scale studies exploring the above association. We used a large nationally representative cohort among the U.S. population, fully adjusted for the potential covariates, and analyzed the relationship of SUA with different diabetic chronic complications at the same time, which increased the statistical strength and reliability of our results. This is the first study that used restricted cubic splines to explore the above relationship. Previous studies usually only reported the relationship between SUA and diabetic complications, and we have also provided specific targets of SUA management for DM patients.
The pathophysiological mechanisms between SUA and chronic complications remain unclear. Potential mechanisms might be that increased SUA levels lead to the increase of ROS and promote the expression of inflammatory cytokine. For instance, IL-1β, IL-6, and TNF-α might lead to inflammation in vessels [27]. UA-mediated oxidative stress is associated with DNA damage, lipid peroxidation, and cellular damage [28]. UA is associated with endothelial dysfunction through inhibiting migration and proliferation of endothelial cells, NO bioavailability, and secretion in endothelial cells. Activation of RAAS induced high intraglomerular pressure, vascular dysfunction, and inflammation, and then led to cardiovascular and renal complications [27,29].
Lu et al. found a positive correlation between SUA levels and the prevalence of CVD and DKD, but not with that of DR in diabetic patients of Han Nationality [7], and a meta-analysis in 2016 found that hyperuricemia was correlated with an increased risk of PN [8]. Another study found that higher SUA concentration was associated with increased risk of developing eGFR decline among type 2 DM cases [9], which were consistent with our results. However, the first previous published study is limited to exploring the issue among Han nationality, which means it does not take into account other ethnic groups who might have different backgrounds. Additionally, the meta-analysis has failed to address the relationship between uric acid and various diabetic chronic complications. Based on the limitations of the previous research, our study makes an attempt to engage different ethnic groups and explore the relationship of SUA with different diabetic chronic complications. Furthermore, Liu et al. found that elevated uric acid levels were associated with a higher risk of increase in severity of DR over a 3-year follow-up [30]. Hayashino et al. found that both lower and higher uric acid levels were independently correlated with the risk of progression in albuminuria other than the development of albuminuria [31], and Cai’s newly published research suggested that low SUA level was closely correlated with PN [32]. These findings were inconsistent with our study. However, Liu’s study was a hospital-based but not a community-based study. Hayashino’s study used single urine ACR measurements but failed to combine GFR for the evaluation of DKD and Cai’s study was limited to type 2 DM patients without hyperuricemia. We used a large representative nationwide sample, and GFR was also considered in the definition of DKD. Our study makes attempts to involve DM patients with different SUA levels, which makes our results more convincing. In addition, the statistical analysis, study population, and adjusted covariates differed in the above-mentioned research. For instance, age, sex, eGFR, HbA1C, and duration of DM were adjusted in Seok Kang’s research [33], while systolic/diastolic blood pressure, serum lipid, and waist circumference were adjusted in Liu’s study [30], and our study additionally adjusted race, education levels, and poverty income ratio, which might lead to the different results. Participants involved in the above-mentioned research had different characteristics. Lu’s published study was limited to men aged ≥18 years and postmenopausal women [7]. The prevalence of chronic complications was lower in younger DM patients, which might hinder the discovery of a significant correlation. Our study involved DM patients aged 40 and over whose prevalence of diabetic complications was higher compared with younger patients. The age difference of the involved participants means the different proportions of type 1 and type 2 DM in the study population, which might also influence the results.
We found a significant correlation between SUA and PN in binary logistic regression analysis, but it became insignificant in restricted cubic spline analysis. Different references used in the above analysis might be potential explanations. Binary logistic regression analysis took patients with SUA > 420 μmol/L as a reference, while the reference point of uric acid in the restricted cubic spline was 327.27 μmol/L. In addition, SUA was transformed into an ordered variable in logistic regression analysis, while SUA was a continuous variable in restricted cubic spline analysis. It did not make sense that SUA levels were negatively correlated with HbA1c in our study, but it was consistent with some previous studies [7,31,34]. More patients in the higher SUA group receiving insulin therapy might explain this phenomenon.
The limitations of our study are as follows. Primarily, it was hard to determine causal associations, as it was a cross-sectional study. Further mendelian randomization studies, basic research, and large-scale cohort studies are required to confirm the causality. Due to the limited availability of data, we applied data from NHANES 1999 to 2008. It was difficult to include all potential covariates, some of which might be considered outdated. SUA in our study was only measured once while UA was a dynamic variable, which might be affected by the diet and cause some bias. Due to the limitation of data on oral glucose tolerance tests, some patients with diabetes might not be included. Finally, keeping a common quartile range for both genders may cause some bias.
The prevalence of hyperuricemia is gradually increasing with improved living conditions and changes in dietary patterns. It is controversial whether to initiate urate-lowering therapy (ULT) for asymptomatic hyperuricemia patients. The 2020 American College of Rheumatology Guideline recommends against initiating any pharmacologic ULT in individuals with asymptomatic hyperuricemia [35], while the Japanese Society of Gout recommends initiating drug therapy when the SUA reaches 8.0 mg/dL or more [36]. From our study, more attention should be paid to the SUA levels for patients with DM and maintaining a SUA level of less than 300 μmol/L might be protective against the risk of diabetic chronic complications.
5. Conclusions
We found that maintaining SUA levels at less than 300 μmol/L might be protective against the risk of DKD, CVD, and PN other than DR compared with patients with SUA values more than 420 μmol/L. We hope our study can provide valuable evidence for the management of diabetic patients with hyperuricemia. Future prospective studies are necessary to confirm the relationship between SUA and diabetic chronic complications and the protective effect of urate-lowering therapy.
Acknowledgments
Thanks for Jiayi Yi from Fuwai hospital for his guidance in R programming.
Abbreviations
| ACR | ratio of urine albumin to creatinine |
| CVD | cardiovascular disease |
| DKD | diabetic kidney disease |
| DM | diabetes mellitus |
| DR | diabetic retinopathy |
| eGFR | estimation of the glomerular filtration rate |
| NHANES | National Health and Nutrition Examination Surveys |
| PIR | poverty income ratio |
| PN | peripheral neuropathy |
| ROS | reactive oxygen species |
| SUA | serum uric acid |
| ULT | urate lowering therapy |
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12020725/s1, Table S1. Clinical features of the involved diabetes patients for the analysis of diabetic kidney disease (n = 3075). Table S2. Clinical features of the involved diabetes patients for the analysis of diabetic peripheral neuropathy (n = 1453). Table S3. Clinical features of the involved diabetes patients for the analysis of diabetic retinopathy (n = 1233). Table S4. Clinical features of diabetic patients aged 40 and over with or without diabetic kidney disease (n = 3075). Table S5. Clinical features of diabetic patients aged 40 and over with or without cardiovascular disease (n = 3106). Table S6. Clinical features of diabetic patients aged 40 and over with or without diabetic peripheral neuropathy (n = 1453). Table S7. Clinical features of diabetic patients aged 40 and over with or without diabetic retinopathy (n = 1233).
Author Contributions
All authors helped to perform the research. Design: Y.H., Y.Z. and X.Z. Conduct/data collection: Y.C., H.D., S.W. and H.Z. Analysis: Y.H., J.W., Y.Y. and X.H. Writing manuscript: Y.H., Y.Z. and X.Z. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
National Center for Health Statistics’ Research Ethics Review Board approved all data collection protocols. Written informed consent was obtained from all participants, and all data was de-identified by the NCHS.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study. Patients signed informed consent regarding publishing their data and photographs.
Data Availability Statement
Datasets that support the conclusions of our research can be found in the public repository, as described below. The authors do not own the data. The Data are available from the National Center for Health Statistics (http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm, accessed on 15 August 2022).
Conflicts of Interest
The authors have no conflict of interest to declare.
Funding Statement
Our work was funded by the National Natural Science Foundation of China (Grant No. 81901667, Grant No. 82071841); 2019 Discipline Development Project of Peking Union Medical College (Grant No. 201920200106) and National High Level Hospital Clinical Research Funding (2022-PUMCH-B-044).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Balakumar P., Maung-U K., Jagadeesh G. Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol. Res. 2016;113 Pt A:600–609. doi: 10.1016/j.phrs.2016.09.040. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Global Report on Diabetes. [(accessed on 15 August 2022)]. Available online: https://www.who.int/publications/i/item/9789241565257.
- 3.American Diabetes Association Introduction: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2021;45((Suppl. S1)):S1–S2. doi: 10.2337/dc22-Sint. [DOI] [PubMed] [Google Scholar]
- 4.Forbes J.M., Cooper M.E. Mechanisms of Diabetic Complications. Physiol. Rev. 2013;93:137–188. doi: 10.1152/physrev.00045.2011. [DOI] [PubMed] [Google Scholar]
- 5.Ceriello A., Prattichizzo F. Variability of risk factors and diabetes complications. Cardiovasc. Diabetol. 2021;20:101. doi: 10.1186/s12933-021-01289-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verma S., Ji Q., Bhatt D.L., Mazer C.D., Al-Omran M., Inzucchi S.E., Wanner C., Ofstad A.P., Zwiener I., George J.T., et al. Association between uric acid levels and cardio-renal outcomes and death in patients with type 2 diabetes: A subanalysis of EMPA-REG OUTCOME. Diabetes Obes. Metab. 2020;22:1207–1214. doi: 10.1111/dom.13991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wan H., Wang Y., Chen Y., Fang S., Zhang W., Xia F., Wang N., Lu Y. Different associations between serum urate and diabetic complications in men and postmenopausal women. Diabetes Res. Clin. Pract. 2020;160:108005. doi: 10.1016/j.diabres.2020.108005. [DOI] [PubMed] [Google Scholar]
- 8.Yu S., Chen Y., Hou X., Xu N., Che K., Li C., Yan S., Wang Y., Wang B. Serum Uric Acid Levels and Diabetic Peripheral Neuropathy in Type 2 Diabetes: A Systematic Review and Meta-analysis. Mol. Neurobiol. 2016;53:1045–1051. doi: 10.1007/s12035-014-9075-0. [DOI] [PubMed] [Google Scholar]
- 9.Wang J., Yu Y., Li X., Li D., Xu C., Yuan J., Wei S., Li X., Yang K., Zheng D., et al. Serum uric acid levels and decreased estimated glomerular filtration rate in patients with type 2 diabetes: A cohort study and meta-analysis. Diabetes Metab. Res. Rev. 2018;34:e3046. doi: 10.1002/dmrr.3046. [DOI] [PubMed] [Google Scholar]
- 10.Gherghina M.-E., Peride I., Tiglis M., Neagu T.P., Niculae A., Checherita I.A. Uric Acid and Oxidative Stress—Relationship with Cardiovascular, Metabolic, and Renal Impairment. Int. J. Mol. Sci. 2022;23:3188. doi: 10.3390/ijms23063188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ichida K., Matsuo H., Takada T., Nakayama A., Murakami K., Shimizu T., Yamanashi Y., Kasuga H., Nakashima H., Nakamura T., et al. Decreased extra-renal urate excretion is a common cause of hyperuricemia. Nat. Commun. 2012;3:764. doi: 10.1038/ncomms1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hyndman D., Liu S., Miner J.N. Urate Handling in the Human Body. Curr. Rheumatol. Rep. 2016;18:34. doi: 10.1007/s11926-016-0587-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang M., Zhu X., Wu J., Huang Z., Zhao Z., Zhang X., Xue Y., Wan W., Li C., Zhang W., et al. Prevalence of Hyperuricemia Among Chinese Adults: Findings from Two Nationally Representative Cross-Sectional Surveys in 2015–16 and 2018–19. Front. Immunol. 2022;12:791983. doi: 10.3389/fimmu.2021.791983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu Y., Pandya B.J., Choi H.K. Prevalence of gout and hyperuricemia in the US general population: The National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011;63:3136–3141. doi: 10.1002/art.30520. [DOI] [PubMed] [Google Scholar]
- 15.Ponticelli C., Podestà M.A., Moroni G. Hyperuricemia as a trigger of immune response in hypertension and chronic kidney disease. Kidney Int. 2020;98:1149–1159. doi: 10.1016/j.kint.2020.05.056. [DOI] [PubMed] [Google Scholar]
- 16.Andres-Hernando A., Cicerchi C., Kuwabara M., Orlicky D.J., Sanchez-Lozada L.G., Nakagawa T., Johnson R.J., Lanaspa M.A. Umami-induced obesity and metabolic syndrome is mediated by nucleotide degradation and uric acid generation. Nat. Metab. 2021;3:1189–1201. doi: 10.1038/s42255-021-00454-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jia Z., Zhang X., Kang S., Wu Y. Serum uric acid levels and incidence of impaired fasting glucose and type 2 diabetes mellitus: A meta-analysis of cohort studies. Diabetes Res. Clin. Pract. 2013;101:88–96. doi: 10.1016/j.diabres.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 18.Mortada I. Hyperuricemia, Type 2 Diabetes Mellitus, and Hypertension: An Emerging Association. Curr. Hypertens. Rep. 2017;19:69. doi: 10.1007/s11906-017-0770-x. [DOI] [PubMed] [Google Scholar]
- 19.Han Y., Han X., Yin Y., Cao Y., Di H., Wu J., Zhang Y., Zeng X. Dose-Response Relationship of Uric Acid with Fasting Glucose, Insulin, and Insulin Resistance in a United States Cohort of 5148 Non-diabetic People. Front. Med. 2022;9:905085. doi: 10.3389/fmed.2022.905085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease, Control, and Prevention National Health and Nutrition Examination Survey. [(accessed on 15 August 2022)]; Available online: https://www.cdc.gov/nchs/nhanes/
- 21.World Medical Association Declaration of Helsinki Ethical Principles for Medical Research. Involving Human Subjects. [(accessed on 15 August 2022)]. Available online: https://www.wma.net/wp-content/uploads/2016/11/DoH-Oct2013-JAMA.pdf.
- 22.Levey A.S., Stevens L.A., Schmid C.H., Zhang Y.L., Castro A.F., 3rd, Feldman H.I., Kusek J.W., Eggers P., Van Lente F., Greene T., et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Boer I.H., Rue T.C., Hall Y.N., Heagerty P.J., Weiss N.S., Himmelfarb J. Temporal Trends in the Prevalence of Diabetic Kidney Disease in the United States. JAMA. 2011;305:2532–2539. doi: 10.1001/jama.2011.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu C., Liang J., Xu S., Liu Q., Xu J., Gu A. Increased serum levels of aldehydes are associated with cardiovascular disease and cardiovascular risk factors in adults. J. Hazard. Mater. 2020;400:123134. doi: 10.1016/j.jhazmat.2020.123134. [DOI] [PubMed] [Google Scholar]
- 25.National Health and Nutrition Examination Survey 1999–2000 Data Documentation, Codebook, and Frequencies Lower Extremity Disease—Peripheral Neuropathy (LEXPN) [(accessed on 15 August 2022)]; Available online: https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/LEXPN.htm#Protocol_and_Procedure.
- 26.National Health and Nutrition Examination Survey 2005–2006 Data Documentation, Codebook, and Frequencies Ophthalmology—Retinal Imaging (OPXRET_D) [(accessed on 15 August 2022)]; Available online: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/OPXRET_D.htm#Data_Processing_and_Editing.
- 27.Eid S., Sas K.M., Abcouwer S.F., Feldman E.L., Gardner T.W., Pennathur S., Fort P.E. New insights into the mechanisms of diabetic complications: Role of lipids and lipid metabolism. Diabetologia. 2019;62:1539–1549. doi: 10.1007/s00125-019-4959-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu M.-A., Sánchez-Lozada L.G., Johnson R.J., Kang D.-H. Oxidative stress with an activation of the renin–angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J. Hypertens. 2010;28:1234–1242. doi: 10.1097/HJH.0b013e328337da1d. [DOI] [PubMed] [Google Scholar]
- 29.Xiong Q., Liu J., Xu Y. Effects of Uric Acid on Diabetes Mellitus and Its Chronic Complications. Int. J. Endocrinol. 2019;2019:9691345. doi: 10.1155/2019/9691345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee J.-J., Yang I.-H., Kuo H.-K., Chung M.-S., Chen Y.-J., Chen C.-H., Liu R.-T. Serum uric acid concentration is associated with worsening in severity of diabetic retinopathy among type 2 diabetic patients in Taiwan—A 3-year prospective study. Diabetes Res. Clin. Pract. 2014;106:366–372. doi: 10.1016/j.diabres.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 31.Hayashino Y., Okamura S., Tsujii S., Ishii H. Association of serum uric acid levels with the risk of development or progression of albuminuria among Japanese patients with type 2 diabetes: A prospective cohort study [Diabetes Distress and Care Registry at Tenri (DDCRT 10)] Acta Diabetol. 2016;53:599–607. doi: 10.1007/s00592-015-0825-x. [DOI] [PubMed] [Google Scholar]
- 32.Zhuang Y., Huang H., Hu X., Zhang J., Cai Q. Serum uric acid and diabetic peripheral neuropathy: A double-edged sword. Acta Neurol. Belg. 2022 doi: 10.1007/s13760-022-01978-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim H.K., Lee M., Lee Y.-H., Lee B.-W., Cha B.-S., Kang E.S. Uric Acid Variability as a Predictive Marker of Newly Developed Cardiovascular Events in Type 2 Diabetes. Front. Cardiovasc. Med. 2021;8:775753. doi: 10.3389/fcvm.2021.775753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu Y., Li Q., Min R., Deng Y., Xu Y., Gao L. The association between serum uric acid and diabetic complications in patients with type 2 diabetes mellitus by gender: A cross-sectional study. PeerJ. 2021;9:e10691. doi: 10.7717/peerj.10691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.FitzGerald J.D., Dalbeth N., Mikuls T., Brignardello-Petersen R., Guyatt G., Abeles A.M., Gelber A.C., Harrold L.R., Khanna D., King C., et al. 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis Rheumatol. 2020;72:879–895. doi: 10.1002/art.41247. [DOI] [PubMed] [Google Scholar]
- 36.Yamanaka H. Japanese Guideline for the Management of Hyperuricemia and Gout: Second Edition. Nucleosides Nucleotides Nucleic Acids. 2011;30:1018–1029. doi: 10.1080/15257770.2011.596496. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Datasets that support the conclusions of our research can be found in the public repository, as described below. The authors do not own the data. The Data are available from the National Center for Health Statistics (http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm, accessed on 15 August 2022).