Abstract
Background: The COVID-19 pandemic represents one of the world’s most important challenges for global public healthcare. Various studies have found an association between severe vitamin D deficiency and COVID-19-related outcomes. Vitamin D plays a crucial role in immune function and inflammation. Recent data have suggested a protective role of vitamin D in COVID-19-related health outcomes. The purpose of this meta-analysis and trial sequential analysis (TSA) was to better explain the strength of the association between the protective role of vitamin D supplementation and the risk of mortality and admission to intensive care units (ICUs) in patients with COVID-19. Methods: We searched four databases on 20 September 2022. Two reviewers screened the randomized clinical trials (RCTs) and assessed the risk of bias, independently and in duplicate. The pre-specified outcomes of interest were mortality and ICU admission. Results: We identified 78 bibliographic citations. After the reviewers’ screening, only five RCTs were found to be suitable for our analysis. We performed meta-analyses and then TSAs. Vitamin D administration results in a decreased risk of death and ICU admission (standardized mean difference (95% CI): 0.49 (0.34–0.72) and 0.28 (0.20–0.39), respectively). The TSA of the protective role of vitamin D and ICU admission showed that, since the pooling of the studies reached a definite sample size, the positive association is conclusive. The TSA of the protective role of vitamin D in mortality risk showed that the z-curve was inside the alpha boundaries, indicating that the positive results need further studies. Discussion: The results of the meta-analyses and respective TSAs suggest a definitive association between the protective role of vitamin D and ICU hospitalization.
Keywords: vitamin D, COVID-19, ICU hospitalization, mortality, meta-analysis, trial sequential analysis
1. Introduction
The pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) responsible for coronavirus disease 2019 (COVID-19) has had a catastrophic effect on global healthcare systems, becoming a major public healthcare challenge worldwide. Since the first cases in early December 2019, there have been 613,793,706 confirmed cases of COVID-19, including 6,532,674 deaths, as of 22 September 2022 [1]. Elderly people with comorbidities, such as hypertension, cardiovascular disease, diabetes, chronic obstructive pulmonary disease, and chronic renal insufficiency, are more likely to be affected by a more severe form of COVID-19, with a higher mortality rate [2,3,4,5,6,7]. Although there have been advances in preventing and treating COVID-19 through the utilization of effective vaccines and antiviral drugs, interest in the nutraceutical approach [8], particularly in vitamin D [9,10], as a means to promote the immune response and reduce the inflammatory response has been growing. COVID-19 is characterized by high levels of inflammatory markers, including C-reactive protein (CRP), and increased levels of inflammatory cytokines and chemokines [11,12]. In this sense, various data have demonstrated the anti-inflammatory, antioxidant, and immunomodulatory properties of vitamin D [13,14,15], in addition to the importance of vitamin D for bone health, as well as its role in extra-skeletal function. On the one hand, vitamin D maintains pulmonary barrier function, determines the production of antimicrobial peptides, and enhances neutrophil activity, boosting the innate response [16], and it shifts the adaptive immune response to a more T helper cell-2 (Th2) type [17]. On the other hand, vitamin D reduces the production of pro-inflammatory cytokines, such as IL-6, IL-8, IL-9, IL-12, TNF alfa, and IFN gamma, and by blocking NK-kB pathways and, consequently, the production of IL-4, IL-5, and IL-10, it increases the anti-inflammatory response [18]. Moreover, patients suffering from chronic obstructive pulmonary disease with a low baseline vitamin D status have been reported to receive more significant clinical benefits from a vitamin D intervention than those with a high baseline vitamin D status [19,20]. Jolliffe and colleagues found that vitamin D supplementation could reduce the risk of asthma exacerbations needing systemic corticosteroids, especially in subjects with baseline serum hydroxyvitamin D (25OHD) levels < 25 nmol/L [21]. In addition, vitamin D supplementation induces a beneficial effect in preventing acute respiratory infections and reducing their complications [22,23]. At present, there are conflicting data regarding the impact of vitamin D supplementation on COVID-19 severity and mortality.
Some studies have found that 25OHD supplementation is a risk factor for higher in-hospital mortality in patients with COVID-19 and that it does not significantly reduce hospital length of stay [24,25,26]. Other studies have found that vitamin D interventions reduce the risk of mortality and disease severity. Bolus vitamin D supplementation has been associated with less severe COVID-19 and better survival rates in frail elderly populations. Cholecalciferol and calcifediol treatment therapies have been associated with reduced mortality risk in acutely hospitalized patients with COVID-19. In patients with advanced chronic kidney disease, treatment with calcitriol has been found to reduce the risk of COVID-19 mortality [9,27,28,29,30,31,32]. Varikasuvu and colleagues also showed a significant effect of a vitamin D intervention on COVID-19 RT-PCR positivity [33]. A recent systematic review and meta-analysis has suggested that vitamin D supplementation has no significant impact on the risk of COVID-19 infection. In contrast, it showed that vitamin D supplementation provides protective effects against mortality and intensive care unit (ICU) admission in patients with COVID-19 [34]. In light of the above, this study aimed to perform new sensitive analyses of current randomized controlled trials and then trial sequential analyses (TSAs) in order to verify the existence of a clear and definitive association between vitamin D supplementation and its beneficial effect on COVID-19-related risk of death and ICU hospitalization.
2. Results and Discussion
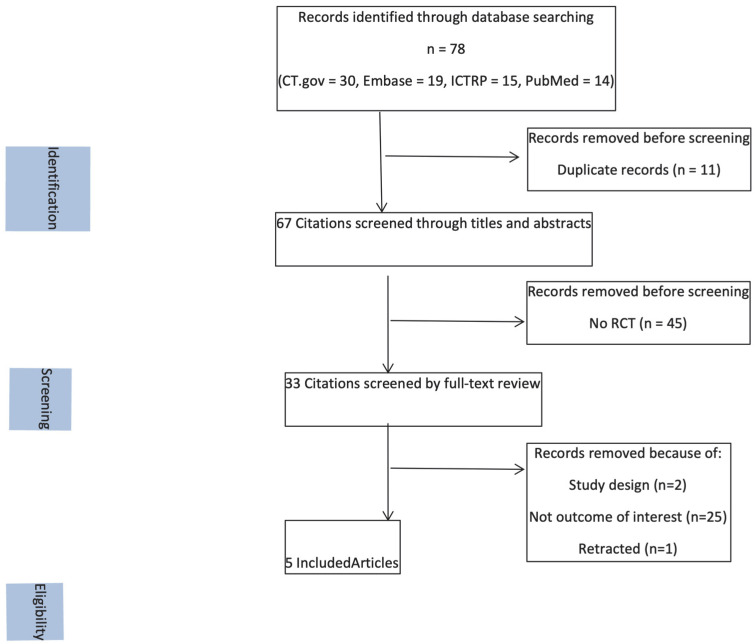
The search string that we used retrieved 78 bibliographic citations. We found 14 citations on PubMed, 30 on CT.gov, 19 on Embase, and 15 on ICTRP. Eleven citations were excluded because of duplicate records. Sixty-seven citations were screened by title and abstract because they were considered to be relevant. Forty-five citations were excluded because they were not randomized clinical trials. Two citations were excluded because of their study design, and twenty-five citations were also excluded because they had no outcomes of interest. Six relevant studies were considered for this meta-analysis. However, the study conducted by Lakkireddy [35] was retracted because the allocation method was not appropriate for randomized clinical trials. Finally, only five studies were included in this meta-analysis. Figure 1 shows the flowchart of the study selection process.
Figure 1.
Flowchart of the study selection process: the flowchart shows the selection process regarding the retrieved citations; randomized controlled trials of treatment and studies not pertinent were excluded, such as studies that did not have outcomes of interest.
Table 1 shows a summary of the ROB2 assessment.
Table 1.
ROB2 assessment for each randomized clinical trial regarding the association of vitamin D supplementation with ICU admission and risk of death. Green indicates a low risk of bias; yellow indicates some concerns for risk of bias; red indicates a high risk of bias.
| ROB2: A Revised Cochrane Risk-of-Bias Tool for Randomized Trials | ||||||
|---|---|---|---|---|---|---|
| R | D | Mi | Me | S | O | |
| Sabico (2021) [32] |

|

|

|

|

|

|
| Castillo (2020) [36] |

|

|

|

|

|

|
| Torres (2022) [37] |

|

|

|

|

|

|
| Murai (2021) [26] |

|

|

|

|

|

|
| Nogues (2021) [38] |

|

|

|

|

|

|
Legend: R—bias arising from the randomization process; D—bias due to deviations from intended interventions; Mi—bias due to missing outcome data; Me—bias in measurement of the outcome; S—bias in selection of the reported results; O—overall risk of bias; +  low risk of bias; −
low risk of bias; −  high risk of bias; ?
high risk of bias; ?  some concerns.
some concerns.
Only the study conducted by Murai had a low risk of bias according to the ROB2 assessment. A summary of the included studies and their characteristics is provided in Table 2 [26,32,36,37,38].
Table 2.
Characteristics of studies of the effects of vitamin D supplementation on COVID-19-related ICU admission and mortality.
| Reference | Design, Setting |
Participants | Duration of Intervention |
Treatment Arms | Outcomes | Efficacy |
|---|---|---|---|---|---|---|
| Sabico et al., 2021 [32] | RCT, Saudi Arabia |
Patients hospitalized with COVID-19 infection (20–75 years old, male: 47.8%) |
2 weeks | Intervention: 5.000 IU/day vitamin D (n = 36); Control: 1.000 IU/day vitamin D (n = 33) |
ICU admission and mortality | Yes |
| Castillo et al., 2020 [36] | RCT, Spain |
Patients hospitalized with COVID-19 infection (53.14 ± 1 0.77 years old, male: 59.0%) |
4 weeks | Intervention: 21.280 IU/day vitamin D on days 1, 3, and 7 and then weekly until discharge or ICU admission (n = 50); Control: no vitamin D supplementation (n = 26) | ICU admission and mortality | Yes |
| Torres et al., 2022 [37] | RCT, Spain |
Patients hospitalized with COVID-19 infection (53–74 years old, male: 60%) |
8–29 days | Intervention: 10.000 IU/day vitamin D (n = 41); Control: 2.000 IU/day vitamin D (n = 44) |
ICU admission and mortality | Yes |
| Murai et al., 2021 [26] | RCT, Brazil |
Patients hospitalized with COVID-19 infection (56.2 ± 14.4 years old, male: 46.1%) | 20 days | Intervention: 200.000 IU vitamin D (n = 120); Control: placebo (n = 120) |
ICU admission and mortality | No |
| Nogues et al., 2021 [38] | RCT, Spain |
Patients hospitalized with COVID-19 infection (30–80 years old, male: 56.0%) | 30 days | Intervention: vitamin D: 21.620 IU on day 1 and 10.810 IU on days 3, 7, 15, and 30 (n = 551); Control: placebo (n = 379) |
ICU admission and mortality | Yes |
ICU = intensive care unit.
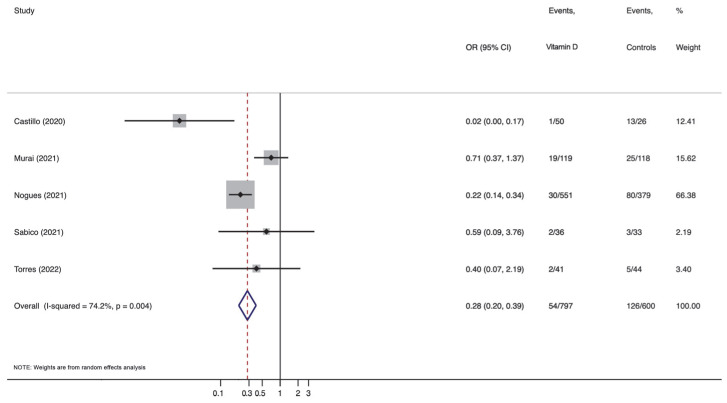
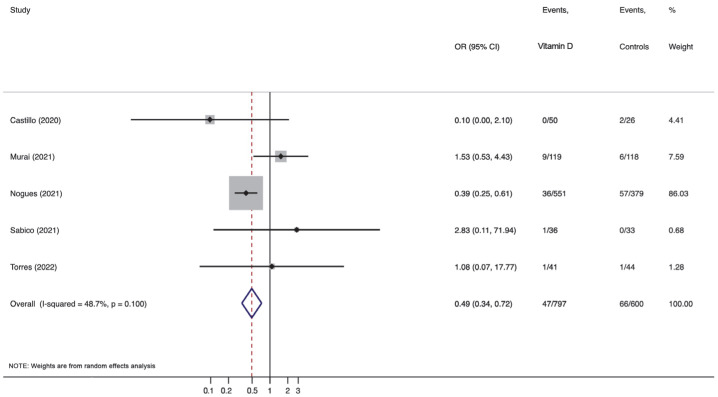
Each randomized clinical trial was investigated in detail for this meta-analysis. The randomized clinical trials that were taken into consideration were heterogeneous in different aspects. All studies included subjects hospitalized with COVID-19. Three out of five studies had a small sample size of patients. Only Nogues [38] recruited more than 800 patients, and Murai [26] included 240 subjects. The studies conducted by Murai [26], Sabico [32], and Torres [37] were multi-center studies, while the trials conducted by Castillo [36] and Nogues [38] were single-center studies. Castillo et al. [36] used an allocation ratio of 2:1. In contrast, the other studies used an allocation ratio of 1:1. In the study conducted by Sabico [32], patients were allocated to receive either standard vitamin D therapy (1000 IU) or 5000 IU of vitamin D for 14 days. Murai and colleagues randomly assigned a single oral dose of 200,000 IU of vitamin D3 or a placebo [26]. In the trial conducted by Castillo [36], eligible patients were allocated at a calcifediol:no calcifediol ratio of 2:1 to take oral 21.280 IU/day vitamin D on days 1, 3, and 7 and then weekly until discharge or ICU admission. In the study conducted by Nogues [38], the following were administered: 21.620 IU of vitamin D on day 1; 10.810 IU of vitamin D on days 3, 7, 15, and 30; or a placebo. In the study conducted by Torres and colleagues [37], the subjects received 2.000 IU/day or 10.000 IU/day of vitamin D. Forest plots are shown in Figure 2 and Figure 3.
Figure 2.
Forest plot of the association of protective effect of vitamin D supplementation with intensive care unit admission in patients hospitalized with COVID-19. CI, confidence interval; OR, odds ratio [26,32,36,37,38].
Figure 3.
Forest plot of the association of protective effect of vitamin D supplementation with mortality in patients hospitalized with COVID-19. CI, confidence interval; OR, odds ratio [26,32,36,37,38].
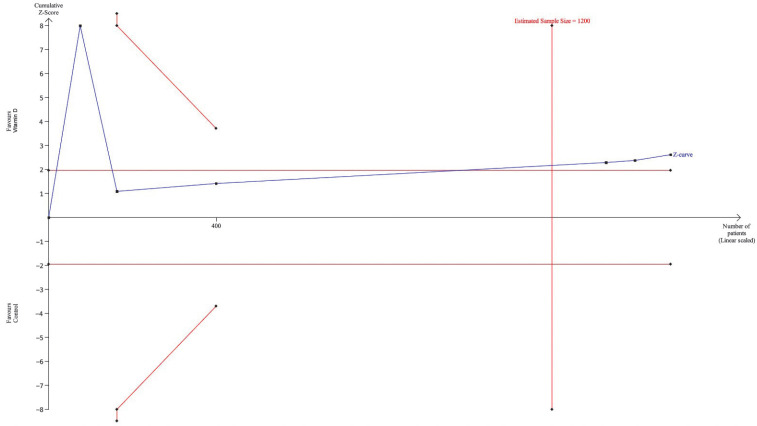
Regarding ICU admission, Figure 2 shows a strong association between vitamin D interventions and protective effect on ICU admission. Vitamin D administration results in a reduced risk of ICU admission (standardized mean difference (95% CI): 0.28 (0.20–0.39)). The meta-analysis showed a high grade of heterogeneity (I2 = 74.2%), which was found to be significant (p = 0.004). Figure 3 shows a significant protective effect of vitamin D administration on mortality. Vitamin D administration results in a reduced risk of death (standardized mean difference (95% CI): 0.49 (0.34–0.72)). The meta-analysis showed non-appreciable heterogeneity (I2 = 48.7%), which was found to be non-significant (p = 0.100). Figure 4 shows the first TSA, which examined vitamin D and ICU admission.
Figure 4.
Trial sequential analysis of the positive association of protective effect of vitamin D supplementation with intensive care unit admission in patients hospitalized with COVID-19. The cumulative z-curve crosses the trial sequential alpha boundary, suggesting that the positive result is conclusive.
The TSA showed a clear association between vitamin D administration and the protective effect on ICU admission in the study conducted by Nogues. The pooling of randomized clinical trials reached a definite sample size. The positive result of TSA is conclusive. Figure 5 shows the second TSA, which examined vitamin D and mortality.
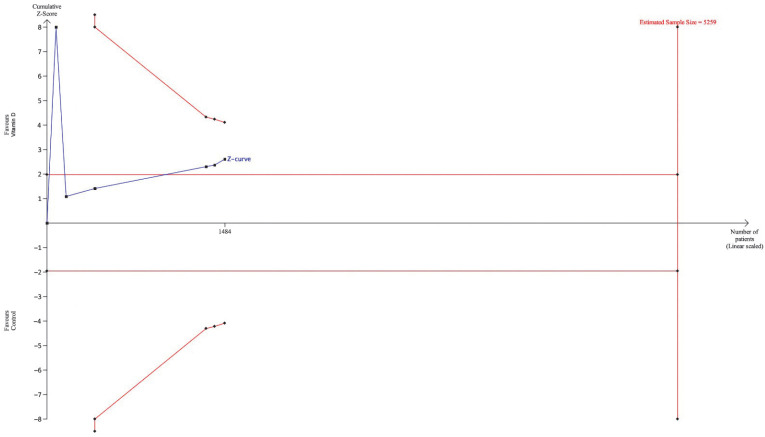
Figure 5.
Trial sequential analysis of the false-positive association of protective effect of vitamin D supplementation with mortality in patients hospitalized with COVID-19. The cumulative z-curve is inside the futile boundaries, suggesting that further studies are necessary to confirm the association.
The TSA showed a false-positive association between vitamin D supplementation and protective effect on the risk of death, so further studies are necessary to confirm this association. Indeed, the z-curve was inside the alpha boundaries. In the first case, our sequential analysis showed that, although the z-curve did not cross the computed alfa boundaries, the pooling of data reached the definite sample size, demonstrating that the positive data are conclusive. In the second case, the TSA showed a z-curve inside the alpha boundaries, suggesting that further studies are necessary to confirm the association.
The pandemic of coronavirus diseases 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has involved hundreds of millions of people with different clinical spectra ranging from asymptomatic to severe conditions, including acute respiratory distress syndrome and multiorgan failure.
SARS-CoV-2 can upregulate angiotensin II (Ang II) by negatively regulating the expression of ACE2. Ang II interacts with Ang II type 1 receptor (AT1R) to regulate nuclear factor-κb (NF-κB) signaling pathways, as well as the activation of macrophages, determining an overproduction of pro-inflammatory cytokines [39]. Among these, IL-6 causes an uncontrolled release of cytokines [40]. IL-6 represents a functional marker of cellular senescence, and its age-dependent increase may be consistent with the age-dependent increase in COVID-19 mortality [40,41]. More recent studies have also highlighted the potential roles of ACE2 in regulating immune responses rather than simply being a viral linkage receptor in COVID-19 [40,42,43,44,45,46]. The dysregulation of ACE2 induced by SARS-CoV-2 infection may further cause cytokine storms and pneumonia. This increased cytokine production is usually defined as a “cytokine storm” [39,47,48]. It also triggers a pathogenic inflammatory immune response, leading to severe multiorgan failure and death in patients with COVID-19 [49,50,51].
2.1. Cytokine Storm
The term cytokine storm is used to describe hyperactive immune responses that can be triggered by a variety of factors, including autoimmune diseases, immunotherapy, and viral infections [52,53].
Cytokine storms determine the elimination of pathogenic microbes; however, they cause tissue toxicity, affecting various organs [54,55]. Cytokine release syndrome (CRS), a type of systemic inflammatory syndrome induced by cytokine storms, has been previously reported in patients infected with SARS-CoV and MERS-CoV. During viral infection, damage-associated molecular patterns (DAMPs), endogenous danger molecules released from damaged cells, and cells with pathogen-associated molecular patterns (PAMPs) that are conserved in molecular structures produced by microorganisms activate the innate immune system by interacting with pattern recognition receptors (PRRs), the antiviral responses in nearby cells, and they recruit innate and adaptive immune cells, such as macrophages, natural killer (NK) cells, and gamma delta (gd T) cells [56,57,58,59]. Downward interferon production contributes to the intracellular antiviral protection of neighboring epithelial cells. Although they may limit the spread of the virus, the release of IL-6 and IL-1b from other immune cells triggers the recruitment of neutrophils and T cells. T-cell activation or immune cell lysis stimulates the secretion of IFN-γ and TNF-α, which activates immune and endothelial cells, further releasing pro-inflammatory cytokines in a positive feedback loop [55].
Xu et al. found that patients with COVID-19 admitted to ICUs had higher levels of plasma inflammatory cytokines IL-2, IL-7, IL-10, granulocyte colony-stimulating factor (G-CSF), IFN-γ, and MCP and TNF-α than patients not in ICUs [60]. This cytokine production underlines the presence of Th1 and Th2 in COVID-19. At the same time, monocyte activation may indicate that cytokine storms are closely correlated with the alteration in the balance between innate and adaptive immunity. In this sense, Iwasaki and Medzhitov showed that the level of IL-6 was markedly higher in severe cases than in mild and moderate cases. Still, the levels of CD4+ T cells, CD8+ T cells, and NK cells were decreased, indicating immunosuppression in severe COVID-19 [61,62,63].
Meanwhile, T lymphocyte cells have been found to be overactivated during cytokine storms in patients with COVID-19, and it has been found that they may be accompanied by severe immune dysfunction [64]. A cytokine storm can directly damage the pulmonary capillary mucosa, promote alveolar edema, and further induce the spread of inflammatory cytokines, causing damage to the alveolar structure, which leads to bilateral lung infiltration and severe hypoxemia, resulting in dysfunction in pulmonary ventilation [65]. In the same way, cytokine storms have also been found to be associated with the sequence and severity of organ dysfunction in multiple organ dysfunction syndromes [66]. Hence, cytokine storms may be considered an essential factor in influencing the fate of patients with COVID-19 and multiple organ dysfunction syndromes.
2.2. Vitamin D
Exposure to inflammatory cytokines expresses the enzyme 25-hydroxyvitamin D-1α-hydroxylase (CYP27B1), which converts 25-hydroxyvitamin D [25 (OH) D into the active form, 1,25-dihydroxyvitamin or calcitriol (CT) [1,25 (OH)2 D] [67]. At the same time, 1,25 (OH)2 D develops the antimicrobial activities of macrophages and monocytes recruited to the inflammatory site. Furthermore, 1,25 (OH)2 D suppresses the expressions of Toll-like receptors on monocytes and inhibits the output of different inflammatory cytokines, such as IL-2, IL-6, and IL-17 [49,50,68]. Moreover, various experimental studies have shown the modulation of endothelial function and vascular permeability by vitamin D and its metabolites [51,69,70]. Vitamin D and its metabolites exert pleiotropic effects on the vascular endothelium in local and systemic inflammation, providing active protection against vascular dysfunction and tissue damage [8,71]. This is crucial in preventing COVID-19-induced ARDS development, representing the most common life-threatening indication for ICU admission [60]. In addition, 1,25(OH)2D inhibits immunoglobulin synthesis and, therefore, could potentially interfere with the immune system, and 1,25(OH)2D also regulates B-cell activity. High levels of 1,25(OH)2D appear to attenuate the immunoglobulin immune response through various mechanisms [72,73,74]. 1,25(OH)2D contributes to a reduction in autoantibody production by controlling B-cell activity and transforming B cells into plasma cells [72,75,76].
2.3. Vitamin D Supplementation
Various studies conducted before the SARS-CoV-2 pandemic showed that patients who received vitamin D supplements had a lower risk of acute respiratory infections and a shorter duration of symptoms [77]. Vitamin D-deficient patients and subjects not receiving bolus doses may benefit the most [23,78]. In addition, protection has been associated with the administration of daily doses of 400–1000 IU for up to 12 months [78].
This study was performed to analyze and determine the reliability of the evidence regarding the association between the protective effect of vitamin D supplementation and the risk of death and ICU admission in patients with COVID-19.
At present, some studies [32,35,79] evaluating the effects of supplementation on inflammation do not show a significant reduction in serum CRP levels in vitamin D-supplemented groups of subjects with COVID-19. On the contrary, a previous meta-analysis has indicated that daily vitamin D supplementation (ranging from 400 to 7143 IU for 8 to 48 weeks) significantly decreases the level of circulating CRP [80]. Vitamin D supplementation could block the nuclear factor kappa B (NF-κB) pathway, which, in turn, may reduce systemic inflammation and the production of CRP [80]. A recent overview of systematic reviews [10] has suggested the potential benefits of vitamin D supplementation that significantly reduce CRP in patients with diabetes and COVID-19.
Other studies have also found that a decreased CD4/CD8 ratio is associated with low 25(OH)D levels [81] and that the administration of 5000–10,000 IU of vitamin D3 is attributable to an increase in the CD4/CD8 ratio, reflecting immune regulation [76,82]. Serum 25(OH)D level ≤ 11.4 ng/mL is associated with the stimulation of Th2 and the downregulation of Th17 cell polarization of adaptive immunity in patients with COVID-19 [83]. In this sense, the trial conducted by Torres and colleagues showed that the administration of a high dose of vitamin D equal to 10,000 IU/day leads to an increase in anti-inflammatory cytokines, such as IL10, and higher levels of CD4+ T cells, which may contribute to decreasing the inflammatory state in severe forms of COVID-19. The trial conducted by Sabico also showed that 5000 IU of vitamin D supplementation reduced the time to recover and decreased IL-6 levels.
Similarly, heterogeneous results concerning the association between vitamin D status and COVID-19-related ICU admission and mortality rate [84,85,86,87] are available. A recent study [33] analyzed randomized clinical trials about vitamin D supplementation and COVID-19 outcomes, while Hosseini et al. [34] included both randomized clinical trials and non-randomized intervention studies for their analysis. The data from the first meta-analysis outlined the beneficial effects of vitamin D interventions on COVID-19 severity and RT-PCR positivity. At the same time, Hosseini highlighted the protective effects provided by vitamin D, demonstrating lower rates of ICU admission and mortality.
However, as previously demonstrated [88], meta-analyses cannot be a pure exercise of pooling data, and TSA seems to be a valuable instrument for drawing non-biased conclusions. Meta-analyses are conducted to summarize the effects of an intervention, assess the strength of evidence, and establish statistical significance in studies that have conflicting results. Nevertheless, an in-depth critical appraisal could include potential biases that could produce false-positive results. The great importance of our analysis is that, despite the presence of randomized clinical trials with some concerns about the risk of bias, the new meta-analyses and TSAs found a significant association between the protective role of vitamin D supplementation and ICU hospitalization in patients with COVID-19. At the same time, TSAs underlined the need for further studies to confirm the significant association between the beneficial effect of vitamin D supplementation and mortality.
The second strength of our study lies in the fact that we focused on randomized clinical trials investigating vitamin D interventions within the framework of COVID-19, excluding other respiratory infections.
In our opinion, due to the sample size and the precision of the effect, we propose Nogues’ protocol, which has positive effects on hospitalization in intensive care and mortality. In patients hospitalized with COVID-19, the protocol to administer consists of the administration of 21,620 IU on day 1 and 10,810 IU on days 3, 7, 15, and 30.
Regarding our analysis, it is worth highlighting that, even though the presence of statistical heterogeneity and a large effect size were observed and only a small number of studies qualified for the analysis, the new meta-analyses performed and the TSAs, about vitamin D interventions and ICU admission and risk of death in patients hospitalized with COVID-19, confirm the presence of a strong association between the protective effect provided by vitamin D against ICU admission. It is important that, to confirm the beneficial effect of vitamin D on mortality in the context of COVID-19, studies with a consistent sample size must be carried out, and the period of investigation, the duration of the vitamin D intervention, and the time until follow-up evaluations should be long enough to achieve adequate vitamin D serum levels.
3. Methods
3.1. Eligibility Criteria
A systematic search regarding the association between vitamin D supplementation and effect on the risk of death and ICU admission in patients with COVID-19 was performed. Studies were included if they met the following criteria: involving participants with no gender or ethnicity restrictions, who were tested for SARS-CoV-2, and who were aged 18 years or older and investigating any type of vitamin D supplementation in comparison with placebo, the standard of care, or no treatment. We excluded all other kinds of studies, studies that administered additional agents or agents other than vitamin D, studies that did not test for SARS-CoV-2 infection, and studies with missing assessments of mortality and ICU admission. The review protocol was entered into the International Prospective Register of Systematic Reviews of the Centre for Reviews and Dissemination (PROSPERO) database (Registry number: CRD42022374151).
3.2. Search Methods
On 20 September 2022, at 02:00 p.m. (GMT-5, Bethesta, MD, USA), a literature search was performed on MEDLINE, PubMed Central, and the Cochrane Library, using the search strings below.
The search strategy was as follows: ((vitamin D OR vitamin D OR ergocalciferols OR ergocalciferols OR (ergocalciferols OR ergocalciferols OR ergocalciferol) OR (cholecalciferol OR cholecalciferol OR cholecalciferols OR colecalciferol ) OR (calcitriol OR calcitriol OR calcitriols)) AND (inflammation OR inflammation OR inflammations OR inflammations OR (inflammatories OR inflammatory) OR TNF OR (interleukine OR interleukines OR interleukins OR interleukins OR interleukin) OR (cytokin OR cytokine s OR cytokines OR cytokines OR cytokine OR cytokinic OR cytokins)) AND (COVID OR SARS-CoV2)) in Title Abstract Keyword—in Trials (word variations were searched for).
3.3. Study Selection
The retrieved citations were independently screened by two authors (M.B.R. and S.S.). Once pertinent studies were identified, the full publications were retrieved and reviewed separately by the two investigators in order to determine their suitability for final inclusion. Any disagreement was resolved by discussion with a third reviewer (C.S.).
3.4. Data Extraction, Coding, and Analysis
Two authors (R.M.B and S.S.) collected the data from all included articles using a pre-tested form, individuated duplicates, and prepared a flowchart of the excluded and included studies. C.S. and A.C. independently verified the entire process.
3.5. Risk of Bias and Quality Assessment
Two authors (M.B.R. and S.S.) assessed the quality of the included randomized clinical trials using ROB2 (version 2 of the Cochrane risk-of-bias tool for randomized trials) [89]. ROB2 is a recommended tool included in Cochrane Reviews for the assessment of the risk of bias in randomized trials. ROB2 is structured into a fixed set of domains of bias, focusing on different aspects of a trial, in particular, random sequence generation, allocation concealment, the blinding of participants and personnel, the blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. A proposed judgement about the risk of bias arising from each domain is made. The judgement can be a “low” or “high” risk of bias or can express “some concerns”.
3.6. Dosage of Vitamin D
The data of the patients were extracted and tabulated according to the results of each trial.
3.7. Methodological and Sensitive Analysis
3.7.1. Data Extraction and Statistical Analysis
The data on the patients, methods, outcomes, and results were extracted using a data extraction form. Cumulative meta-analyses were performed. Meta-analyses were performed with a fixed-effects model or a random-effects model where necessary. Heterogeneity was investigated by using the I2 statistic, with significance set at p < 0.05. A random-effects model or a fixed-effects model was used to perform the meta-analysis according to the heterogeneity. A Forest plot was used to graphically summarize the pieces of evidence from the various studies. STATA Version 17.0 (StataCorp, College Station, TX, USA) was used to perform all the analyses. Moreover, we performed trial sequential analyses.
3.7.2. Trial Sequential Analysis
To avoid the increased risk of random errors in the cumulative meta-analyses, we performed trial sequential analyses (TSAs) because the best available evidence may not be synonymous with “sufficient evidence” or “strong evidence”. The threshold for a statistically significant result was adjusted according to the strength of the evidence and the number of significance tests performed according to the “law of the iterated logarithm”. We computed alpha boundaries to test the positive results and futility boundaries to test the negative results [90]. False-positive results are indicated by a z-curve within the computed alpha boundaries. On the contrary, false-negative results are indicated by a z-curve that does not cross the computed futility boundaries. In our study, TSAs were performed by G.N. The analyses were performed using Trial Sequential Analysis Viewer (TSA Viewer) (Computed Program; Version 0.9.5.10 Beta. Copenhagen: Copenhagen Trial Unit, Centre for Clinical Intervention Research, Rigs Hospitalet, 2016) [91].
4. Conclusions
The current evidence supports the benefits of vitamin D interventions in patients hospitalized with COVID-19 due to the protective effect provided by vitamin D against ICU admission and mortality. A meta-analysis per se does not allow us to state whether the results are truly positive or false-positive. In addition, the inclusion of studies with large effect sizes and significant heterogeneity separates us from the truth. For this reason, a TSA is mandatory to verify the reliability of meta-analysis results [92]. In conclusion, the positive results highlighted again and now validated by TSAs suggest that an indisputable association between vitamin D supplementation and the protective effect on ICU admission can be considered definitive evidence. On the contrary, further studies are needed to assess the utilization of vitamin D regarding the risk of death in patients hospitalized with COVID-19.
Author Contributions
Conceptualization, S.C. and C.A.; methodology, S.C., G.N. and C.A.; software, G.N.; validation, S.C. and C.A.; formal analysis, R.M.B. and S.S.; investigation, R.M.B., S.S. and C.A.; resources, R.M.B. and S.S.; data curation, G.N., R.M.B. and S.S.; writing—original draft preparation, C.A.; writing—review and editing, C.A., S.C. and M.L.M.; visualization, G.N.; supervision, S.C.; project administration, C.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The ENFARMA S.R.L. company contributed only to publication costs and did not influence in any way the conception and writing of the manuscript.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.COVID-19 Map. [(accessed on 22 September 2022)]. Available online: https://coronavirus.jhu.edu/map.html.
- 2.Gallo G., Calvez V., Savoia C. Hypertension and COVID-19: Current Evidence and Perspectives. High Blood Press. Cardiovasc. Prev. 2022;29:115–123. doi: 10.1007/s40292-022-00506-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bansal M. Cardiovascular Disease and COVID-19. Diabetes Metab. Syndr. 2020;14:247–250. doi: 10.1016/j.dsx.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corrao S., Pinelli K., Vacca M., Raspanti M., Argano C. Type 2 Diabetes Mellitus and COVID-19: A Narrative Review. Front. Endocrinol. 2021;12:609470. doi: 10.3389/fendo.2021.609470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh D., Mathioudakis A.G., Higham A. Chronic Obstructive Pulmonary Disease and COVID-19: Interrelationships. Curr. Opin. Pulm. Med. 2022;28:76–83. doi: 10.1097/MCP.0000000000000834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gibertoni D., Reno C., Rucci P., Fantini M.P., Buscaroli A., Mosconi G., Rigotti A., Giudicissi A., Mambelli E., Righini M., et al. COVID-19 Incidence and Mortality in Non-Dialysis Chronic Kidney Disease Patients. PLoS ONE. 2021;16:e0254525. doi: 10.1371/journal.pone.0254525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fattouch K., Corrao S., Augugliaro E., Minacapelli A., Nogara A., Zambelli G., Argano C., Moscarelli M. Cardiac Surgery Outcomes in Patients with Coronavirus Disease 2019 (COVID-19): A Case-Series Report. J. Thorac. Cardiovasc. Surg. 2022;163:1085–1092.e3. doi: 10.1016/j.jtcvs.2020.09.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Corrao S., Mallaci Bocchio R., Lo Monaco M., Natoli G., Cavezzi A., Troiani E., Argano C. Does Evidence Exist to Blunt Inflammatory Response by Nutraceutical Supplementation during COVID-19 Pandemic? An Overview of Systematic Reviews of Vitamin D, Vitamin C, Melatonin, and Zinc. Nutrients. 2021;13:1261. doi: 10.3390/nu13041261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cicero A.F.G., Fogacci F., Borghi C. Vitamin D Supplementation and COVID-19 Outcomes: Mounting Evidence and Fewer Doubts. Nutrients. 2022;14:3584. doi: 10.3390/nu14173584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Argano C., Mallaci Bocchio R., Lo Monaco M., Scibetta S., Natoli G., Cavezzi A., Troiani E., Corrao S. An Overview of Systematic Reviews of the Role of Vitamin D on Inflammation in Patients with Diabetes and the Potentiality of Its Application on Diabetic Patients with COVID-19. Int. J. Mol. Sci. 2022;23:2873. doi: 10.3390/ijms23052873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H., Zhang L., Zhou X., Du C., et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herold T., Jurinovic V., Arnreich C., Lipworth B.J., Hellmuth J.C., von Bergwelt-Baildon M., Klein M., Weinberger T. Elevated Levels of IL-6 and CRP Predict the Need for Mechanical Ventilation in COVID-19. J. Allergy Clin. Immunol. 2020;146:128–136.e4. doi: 10.1016/j.jaci.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mutt S.J., Hyppönen E., Saarnio J., Järvelin M.-R., Herzig K.-H. Vitamin D and Adipose Tissue—More than Storage. Front. Physiol. 2014;5:228. doi: 10.3389/fphys.2014.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang Y., Liu J., Zhang D., Xu Z., Ji J., Wen C. Cytokine Storm in COVID-19: The Current Evidence and Treatment Strategies. Front. Immunol. 2020;11:1708. doi: 10.3389/fimmu.2020.01708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dhawan M., Priyanka, Choudhary O.P. Immunomodulatory and Therapeutic Implications of Vitamin D in the Management of COVID-19. Hum. Vaccin. Immunother. 2022;18:2025734. doi: 10.1080/21645515.2022.2025734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greiller C.L., Martineau A.R. Modulation of the Immune Response to Respiratory Viruses by Vitamin D. Nutrients. 2015;7:4240–4270. doi: 10.3390/nu7064240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bikle D.D. Vitamin D Metabolism, Mechanism of Action, and Clinical Applications. Chem. Biol. 2014;21:319–329. doi: 10.1016/j.chembiol.2013.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bui L., Zhu Z., Hawkins S., Cortez-Resendiz A., Bellon A. Vitamin D Regulation of the Immune System and Its Implications for COVID-19: A Mini Review. SAGE Open Med. 2021;9:20503121211014070. doi: 10.1177/20503121211014073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lehouck A., Mathieu C., Carremans C., Baeke F., Verhaegen J., Van Eldere J., Decallonne B., Bouillon R., Decramer M., Janssens W. High Doses of Vitamin D to Reduce Exacerbations in Chronic Obstructive Pulmonary Disease. Ann. Intern. Med. 2012;156:105–114. doi: 10.7326/0003-4819-156-2-201201170-00004. [DOI] [PubMed] [Google Scholar]
- 20.Martineau A.R., James W.Y., Hooper R.L., Barnes N.C., Jolliffe D.A., Greiller C.L., Islam K., McLaughlin D., Bhowmik A., Timms P.M., et al. Vitamin D3 Supplementation in Patients with Chronic Obstructive Pulmonary Disease (ViDiCO): A Multicentre, Double-Blind, Randomised Controlled Trial. Lancet Respir. Med. 2015;3:120–130. doi: 10.1016/S2213-2600(14)70255-3. [DOI] [PubMed] [Google Scholar]
- 21.Jolliffe D.A., Greenberg L., Hooper R.L., Griffiths C.J., Camargo C.A., Kerley C.P., Jensen M.E., Mauger D., Stelmach I., Urashima M., et al. Vitamin D Supplementation to Prevent Asthma Exacerbations: A Systematic Review and Meta-Analysis of Individual Participant Data. Lancet Respir. Med. 2017;5:881–890. doi: 10.1016/S2213-2600(17)30306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ginde A.A., Blatchford P., Breese K., Zarrabi L., Linnebur S.A., Wallace J.I., Schwartz R.S. High-Dose Monthly Vitamin D for Prevention of Acute Respiratory Infection in Older Long-Term Care Residents: A Randomized Clinical Trial. J. Am. Geriatr. Soc. 2017;65:496–503. doi: 10.1111/jgs.14679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martineau A.R., Jolliffe D.A., Hooper R.L., Greenberg L., Aloia J.F., Bergman P., Dubnov-Raz G., Esposito S., Ganmaa D., Ginde A.A., et al. Vitamin D Supplementation to Prevent Acute Respiratory Tract Infections: Systematic Review and Meta-Analysis of Individual Participant Data. BMJ. 2017;356:i6583. doi: 10.1136/bmj.i6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oristrell J., Oliva J.C., Subirana I., Casado E., Domínguez D., Toloba A., Aguilera P., Esplugues J., Fafián P., Grau M. Association of Calcitriol Supplementation with Reduced COVID-19 Mortality in Patients with Chronic Kidney Disease: A Population-Based Study. Biomedicines. 2021;9:509. doi: 10.3390/biomedicines9050509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cereda E., Bogliolo L., Lobascio F., Barichella M., Zecchinelli A.L., Pezzoli G., Caccialanza R. Vitamin D Supplementation and Outcomes in Coronavirus Disease 2019 (COVID-19) Patients from the Outbreak Area of Lombardy, Italy. Nutrition. 2021;82:111055. doi: 10.1016/j.nut.2020.111055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murai I.H., Fernandes A.L., Sales L.P., Pinto A.J., Goessler K.F., Duran C.S.C., Silva C.B.R., Franco A.S., Macedo M.B., Dalmolin H.H.H., et al. Effect of a Single High Dose of Vitamin D3 on Hospital Length of Stay in Patients with Moderate to Severe COVID-19: A Randomized Clinical Trial. JAMA. 2021;325:1053–1060. doi: 10.1001/jama.2020.26848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Annweiler G., Corvaisier M., Gautier J., Dubée V., Legrand E., Sacco G., Annweiler C. Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study. Nutrients. 2020;12:3377. doi: 10.3390/nu12113377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Annweiler C., Hanotte B., Grandin de l’Eprevier C., Sabatier J.-M., Lafaie L., Célarier T. Vitamin D and Survival in COVID-19 Patients: A Quasi-Experimental Study. J. Steroid Biochem. Mol. Biol. 2020;204:105771. doi: 10.1016/j.jsbmb.2020.105771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alcala-Diaz J.F., Limia-Perez L., Gomez-Huelgas R., Martin-Escalante M.D., Cortes-Rodriguez B., Zambrana-Garcia J.L., Entrenas-Castillo M., Perez-Caballero A.I., López-Carmona M.D., Garcia-Alegria J., et al. Calcifediol Treatment and Hospital Mortality Due to COVID-19: A Cohort Study. Nutrients. 2021;13:1760. doi: 10.3390/nu13061760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rastogi A., Bhansali A., Khare N., Suri V., Yaddanapudi N., Sachdeva N., Puri G.D., Malhotra P. Short Term, High-Dose Vitamin D Supplementation for COVID-19 Disease: A Randomised, Placebo-Controlled, Study (SHADE Study) Postgrad. Med. J. 2022;98:87–90. doi: 10.1136/postgradmedj-2020-139065. [DOI] [PubMed] [Google Scholar]
- 31.Ling S.F., Broad E., Murphy R., Pappachan J.M., Pardesi-Newton S., Kong M.-F., Jude E.B. High-Dose Cholecalciferol Booster Therapy Is Associated with a Reduced Risk of Mortality in Patients with COVID-19: A Cross-Sectional Multi-Centre Observational Study. Nutrients. 2020;12:3799. doi: 10.3390/nu12123799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sabico S., Enani M.A., Sheshah E., Aljohani N.J., Aldisi D.A., Alotaibi N.H., Alshingetti N., Alomar S.Y., Alnaami A.M., Amer O.E., et al. Effects of a 2-Week 5000 IU versus 1000 IU Vitamin D3 Supplementation on Recovery of Symptoms in Patients with Mild to Moderate COVID-19: A Randomized Clinical Trial. Nutrients. 2021;13:2170. doi: 10.3390/nu13072170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Varikasuvu S.R., Thangappazham B., Vykunta A., Duggina P., Manne M., Raj H., Aloori S. COVID-19 and Vitamin D (Co-VIVID Study): A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Expert Rev. Anti. Infect. Ther. 2022;20:907–913. doi: 10.1080/14787210.2022.2035217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hosseini B., El Abd A., Ducharme F.M. Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis. Nutrients. 2022;14:2134. doi: 10.3390/nu14102134. [DOI] [Google Scholar]
- 35.Lakkireddy M., Gadiga S.G., Malathi R.D., Karra M.L., Raju I.S.S.V.P.M., Ragini, Chinapaka S., Baba K.S.S.S., Kandakatla M. RETRACTED ARTICLE: Impact of Daily High Dose Oral Vitamin D Therapy on the Inflammatory Markers in Patients with COVID 19 Disease. Sci. Rep. 2021;11:10641. doi: 10.1038/s41598-021-90189-4. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Entrenas Castillo M., Entrenas Costa L.M., Vaquero Barrios J.M., Alcalá Díaz J.F., López Miranda J., Bouillon R., Quesada Gomez J.M. Effect of Calcifediol Treatment and Best Available Therapy versus Best Available Therapy on Intensive Care Unit Admission and Mortality among Patients Hospitalized for COVID-19: A Pilot Randomized Clinical Study. J. Steroid Biochem. Mol. Biol. 2020;203:105751. doi: 10.1016/j.jsbmb.2020.105751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Torres M., Casado G., Vigón L., Rodríguez-Mora S., Mateos E., Ramos-Martín F., López-Wolf D., Sanz-Moreno J., Ryan-Murua P., Taboada-Martínez M.L., et al. Changes in the Immune Response against SARS-CoV-2 in Individuals with Severe COVID-19 Treated with High Dose of Vitamin D. Biomed. Pharmacother. 2022;150:112965. doi: 10.1016/j.biopha.2022.112965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nogues X., Ovejero D., Pineda-Moncusí M., Bouillon R., Arenas D., Pascual J., Ribes A., Guerri-Fernandez R., Villar-Garcia J., Rial A., et al. Calcifediol Treatment and COVID-19-Related Outcomes. J. Clin. Endocrinol. Metab. 2021;dgab405:e4017–e4027. doi: 10.1210/clinem/dgab405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banu N., Panikar S.S., Leal L.R., Leal A.R. Protective Role of ACE2 and Its Downregulation in SARS-CoV-2 Infection Leading to Macrophage Activation Syndrome: Therapeutic Implications. Life Sci. 2020;256:117905. doi: 10.1016/j.lfs.2020.117905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jiang F., Yang J., Zhang Y., Dong M., Wang S., Zhang Q., Liu F.F., Zhang K., Zhang C. Angiotensin-Converting Enzyme 2 and Angiotensin 1-7: Novel Therapeutic Targets. Nat. Rev. Cardiol. 2014;11:413–426. doi: 10.1038/nrcardio.2014.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D.M.E., Fouchier R.A.M. Isolation of a Novel Coronavirus from a Man with Pneumonia in Saudi Arabia. N. Engl. J. Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 42.Liu F., Long X., Zou W., Fang M., Wu W., Li W., Zhang B., Zhang W., Chen X., Zhang Z. Highly ACE2 Expression in Pancreas May Cause Pancreas Damage After SARS-CoV-2 Infection. Clin. Gastroenterol. Hepatol. 2020;18:2128–2130. doi: 10.1016/j.cgh.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Šestan M., Marinović S., Kavazović I., Cekinović Đ., Wueest S., Turk Wensveen T., Brizić I., Jonjić S., Konrad D., Wensveen F.M., et al. Virus-Induced Interferon-γ Causes Insulin Resistance in Skeletal Muscle and Derails Glycemic Control in Obesity. Immunity. 2018;49:164–177.e6. doi: 10.1016/j.immuni.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 44.Yang J.-K., Lin S.-S., Ji X.-J., Guo L.-M. Binding of SARS Coronavirus to Its Receptor Damages Islets and Causes Acute Diabetes. Acta Diabetol. 2010;47:193–199. doi: 10.1007/s00592-009-0109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Philips B.J., Meguer J.-X., Redman J., Baker E.H. Factors Determining the Appearance of Glucose in Upper and Lower Respiratory Tract Secretions. Intensive Care Med. 2003;29:2204–2210. doi: 10.1007/s00134-003-1961-2. [DOI] [PubMed] [Google Scholar]
- 46.Rao S., Lau A., So H.-C. Exploring Diseases/Traits and Blood Proteins Causally Related to Expression of ACE2, the Putative Receptor of SARS-CoV-2: A Mendelian Randomization Analysis Highlights Tentative Relevance of Diabetes-Related Traits. Diabetes Care. 2020;43:1416–1426. doi: 10.2337/dc20-0643. [DOI] [PubMed] [Google Scholar]
- 47.Li X., Geng M., Peng Y., Meng L., Lu S. Molecular Immune Pathogenesis and Diagnosis of COVID-19. J. Pharm. Anal. 2020;10:102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nile S.H., Nile A., Qiu J., Li L., Jia X., Kai G. COVID-19: Pathogenesis, Cytokine Storm and Therapeutic Potential of Interferons. Cytokine Growth Factor Rev. 2020;53:66–70. doi: 10.1016/j.cytogfr.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ota K., Dambaeva S., Kim M.W.-I., Han A.-R., Fukui A., Gilman-Sachs A., Beaman K., Kwak-Kim J. 1,25-Dihydroxy-Vitamin D3 Regulates NK-Cell Cytotoxicity, Cytokine Secretion, and Degranulation in Women with Recurrent Pregnancy Losses. Eur. J. Immunol. 2015;45:3188–3199. doi: 10.1002/eji.201545541. [DOI] [PubMed] [Google Scholar]
- 50.Klopot A., Hance K.W., Peleg S., Barsony J., Fleet J.C. Nucleo-Cytoplasmic Cycling of the Vitamin D Receptor in the Enterocyte-Like Cell Line, Caco-2. J. Cell. Biochem. 2007;100:617–628. doi: 10.1002/jcb.21087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ma R., Deng X.L., Du G.L., Li C., Xiao S., Aibibai Y., Zhu J. Active Vitamin D3, 1,25-(OH)2D3, Protects against Macrovasculopathy in a Rat Model of Type 2 Diabetes Mellitus. Genet. Mol. Res. 2016;15:15028113. doi: 10.4238/gmr.15028113. [DOI] [PubMed] [Google Scholar]
- 52.Shimabukuro-Vornhagen A., Gödel P., Subklewe M., Stemmler H.J., Schlößer H.A., Schlaak M., Kochanek M., Böll B., von Bergwelt-Baildon M.S. Cytokine Release Syndrome. J. Immunother. Cancer. 2018;6:56. doi: 10.1186/s40425-018-0343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee D.W., Gardner R., Porter D.L., Louis C.U., Ahmed N., Jensen M., Grupp S.A., Mackall C.L. Current Concepts in the Diagnosis and Management of Cytokine Release Syndrome. Blood. 2014;124:188–195. doi: 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zaim S., Chong J.H., Sankaranarayanan V., Harky A. COVID-19 and Multiorgan Response. Curr. Probl. Cardiol. 2020;45:100618. doi: 10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Klinkhammer J., Schnepf D., Ye L., Schwaderlapp M., Gad H.H., Hartmann R., Garcin D., Mahlakõiv T., Staeheli P. IFN-λ Prevents Influenza Virus Spread from the Upper Airways to the Lungs and Limits Virus Transmission. Elife. 2018;7:e33354. doi: 10.7554/eLife.33354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Medzhitov R. Recognition of Microorganisms and Activation of the Immune Response. Nature. 2007;449:819–826. doi: 10.1038/nature06246. [DOI] [PubMed] [Google Scholar]
- 57.Mangalmurti N., Hunter C.A. Cytokine Storms: Understanding COVID-19. Immunity. 2020;53:19–25. doi: 10.1016/j.immuni.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harker J.A., Lewis G.M., Mack L., Zuniga E.I. Late Interleukin-6 Escalates T Follicular Helper Cell Responses and Controls a Chronic Viral Infection. Science. 2011;334:825–829. doi: 10.1126/science.1208421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Azkur A.K., Akdis M., Azkur D., Sokolowska M., van de Veen W., Brüggen M., O’Mahony L., Gao Y., Nadeau K., Akdis C.A. Immune Response to SARS-CoV-2 and Mechanisms of Immunopathological Changes in COVID-19. Allergy. 2020;75:1564–1581. doi: 10.1111/all.14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., et al. Pathological Findings of COVID-19 Associated with Acute Respiratory Distress Syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Iwasaki A., Medzhitov R. Regulation of Adaptive Immunity by the Innate Immune System. Science. 2010;327:291–295. doi: 10.1126/science.1183021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Corrao S., Gervasi F., Di Bernardo F., Natoli G., Raspanti M., Catalano N., Argano C. Immunological Characteristics of Non-Intensive Care Hospitalized COVID-19 Patients: A Preliminary Report. J. Clin. Med. 2021;10:849. doi: 10.3390/jcm10040849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Corrao S., Gervasi F., Di Bernardo F., Argano C. Immune Response Failure in Paucisymptomatic Long-Standing SARS-CoV-2 Spreaders. Clin. Pract. 2021;11:151–161. doi: 10.3390/clinpract11010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Braciale T.J., Sun J., Kim T.S. Regulating the Adaptive Immune Response to Respiratory Virus Infection. Nat. Rev. Immunol. 2012;12:295–305. doi: 10.1038/nri3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Newton A.H., Cardani A., Braciale T.J. The Host Immune Response in Respiratory Virus Infection: Balancing Virus Clearance and Immunopathology. Semin. Immunopathol. 2016;38:471–482. doi: 10.1007/s00281-016-0558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhou Y., Fu B., Zheng X., Wang D., Zhao C., Qi Y., Sun R., Tian Z., Xu X., Wei H. Pathogenic T-Cells and Inflammatory Monocytes Incite Inflammatory Storms in Severe COVID-19 Patients. Natl. Sci. Rev. 2020;7:998–1002. doi: 10.1093/nsr/nwaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu P.T., Stenger S., Li H., Wenzel L., Tan B.H., Krutzik S.R., Ochoa M.T., Schauber J., Wu K., Meinken C., et al. Toll-like Receptor Triggering of a Vitamin D-Mediated Human Antimicrobial Response. Science. 2006;311:1770–1773. doi: 10.1126/science.1123933. [DOI] [PubMed] [Google Scholar]
- 68.Weeres M.A., Robien K., Ahn Y.-O., Neulen M.-L., Bergerson R., Miller J.S., Verneris M.R. The Effects of 1,25 Dihydroxyvitamin D3 (1,25(OH)2D3) on In Vitro Human Natural Killer Cell DevelopmentFrom Hematopoietic Stem Cells. J. Immunol. 2014;193:3456–3462. doi: 10.4049/jimmunol.1400698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim D.-H., Meza C.A., Clarke H., Kim J.-S., Hickner R.C. Vitamin D and Endothelial Function. Nutrients. 2020;12:575. doi: 10.3390/nu12020575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Molinari C., Uberti F., Grossini E., Vacca G., Carda S., Invernizzi M., Cisari C. 1α,25-Dihydroxycholecalciferol Induces Nitric Oxide Production in Cultured Endothelial Cells. CPB. 2011;27:661–668. doi: 10.1159/000330075. [DOI] [PubMed] [Google Scholar]
- 71.Grant W.B., Lahore H., McDonnell S.L., Baggerly C.A., French C.B., Aliano J.L., Bhattoa H.P. Evidence That Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020;12:988. doi: 10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Heine G., Niesner U., Chang H.-D., Steinmeyer A., Zügel U., Zuberbier T., Radbruch A., Worm M. 1,25-Dihydroxyvitamin D(3) Promotes IL-10 Production in Human B Cells. Eur. J. Immunol. 2008;38:2210–2218. doi: 10.1002/eji.200838216. [DOI] [PubMed] [Google Scholar]
- 73.Shirakawa A.-K., Nagakubo D., Hieshima K., Nakayama T., Jin Z., Yoshie O. 1,25-Dihydroxyvitamin D3 Induces CCR10 Expression in Terminally Differentiating Human B Cells. J. Immunol. 2008;180:2786–2795. doi: 10.4049/jimmunol.180.5.2786. [DOI] [PubMed] [Google Scholar]
- 74.Channappanavar R., Perlman S. Pathogenic Human Coronavirus Infections: Causes and Consequences of Cytokine Storm and Immunopathology. Semin. Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Amento E.P., Bhalla A.K., Kurnick J.T., Kradin R.L., Clemens T.L., Holick S.A., Holick M.F., Krane S.M. 1 Alpha,25-Dihydroxyvitamin D3 Induces Maturation of the Human Monocyte Cell Line U937, and, in Association with a Factor from Human T Lymphocytes, Augments Production of the Monokine, Mononuclear Cell Factor. J. Clin. Investig. 1984;73:731–739. doi: 10.1172/JCI111266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Geldmeyer-Hilt K., Heine G., Hartmann B., Baumgrass R., Radbruch A., Worm M. 1,25-Dihydroxyvitamin D3 Impairs NF-ΚB Activation in Human Naïve B Cells. Biochem. Biophys. Res. Commun. 2011;407:699–702. doi: 10.1016/j.bbrc.2011.03.078. [DOI] [PubMed] [Google Scholar]
- 77.Abioye A.I., Bromage S., Fawzi W. Effect of Micronutrient Supplements on Influenza and Other Respiratory Tract Infections among Adults: A Systematic Review and Meta-Analysis. BMJ Global Health. 2021;6:e003176. doi: 10.1136/bmjgh-2020-003176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jolliffe D.A., Camargo C.A., Sluyter J.D., Aglipay M., Aloia J.F., Ganmaa D., Bergman P., Bischoff-Ferrari H.A., Borzutzky A., Damsgaard C.T., et al. Vitamin D Supplementation to Prevent Acute Respiratory Infections: A Systematic Review and Meta-Analysis of Aggregate Data from Randomised Controlled Trials. Lancet Diabetes Endocrinol. 2021;9:276–292. doi: 10.1016/S2213-8587(21)00051-6. [DOI] [PubMed] [Google Scholar]
- 79.Caballero-García A., Pérez-Valdecantos D., Guallar P., Caballero-Castillo A., Roche E., Noriega D.C., Córdova A. Effect of Vitamin D Supplementation on Muscle Status in Old Patients Recovering from COVID-19 Infection. Medicina. 2021;57:1079. doi: 10.3390/medicina57101079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen N., Wan Z., Han S.-F., Li B.-Y., Zhang Z.-L., Qin L.-Q. Effect of Vitamin D Supplementation on the Level of Circulating High-Sensitivity C-Reactive Protein: A Meta-Analysis of Randomized Controlled Trials. Nutrients. 2014;6:2206–2216. doi: 10.3390/nu6062206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chen S., Sims G.P., Chen X.X., Gu Y.Y., Chen S., Lipsky P.E. Modulatory Effects of 1,25-Dihydroxyvitamin D3 on Human B Cell Differentiation. J. Immunol. 2007;179:1634–1647. doi: 10.4049/jimmunol.179.3.1634. [DOI] [PubMed] [Google Scholar]
- 82.Lemire J.M., Adams J.S., Sakai R., Jordan S.C. 1 Alpha,25-Dihydroxyvitamin D3 Suppresses Proliferation and Immunoglobulin Production by Normal Human Peripheral Blood Mononuclear Cells. J. Clin. Investig. 1984;74:657–661. doi: 10.1172/JCI111465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Karonova T.L., Kudryavtsev I.V., Golovatyuk K.A., Aquino A.D., Kalinina O.V., Chernikova A.T., Zaikova E.K., Lebedev D.A., Bykova E.S., Golovkin A.S., et al. Vitamin D Status and Immune Response in Hospitalized Patients with Moderate and Severe COVID-19. Pharmaceuticals. 2022;15:305. doi: 10.3390/ph15030305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pal R., Banerjee M., Bhadada S.K., Shetty A.J., Singh B., Vyas A. Vitamin D Supplementation and Clinical Outcomes in COVID-19: A Systematic Review and Meta-Analysis. J. Endocrinol. Investig. 2022;45:53–68. doi: 10.1007/s40618-021-01614-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shah K., Saxena D., Mavalankar D. Vitamin D Supplementation, COVID-19 and Disease Severity: A Meta-Analysis. QJM. 2021;114:hcab009. doi: 10.1093/qjmed/hcab009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rawat D., Roy A., Maitra S., Shankar V., Khanna P., Baidya D.K. Vitamin D Supplementation and COVID-19 Treatment: A Systematic Review and Meta-Analysis. Diabetes Metab. Syndr. 2021;15:102189. doi: 10.1016/j.dsx.2021.102189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chiodini I., Gatti D., Soranna D., Merlotti D., Mingiano C., Fassio A., Adami G., Falchetti A., Eller-Vainicher C., Rossini M., et al. Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes. Front. Public Health. 2021;9:1968. doi: 10.3389/fpubh.2021.736665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Corrao S., Natoli G., Argano C. Nonalcoholic Fatty Liver Disease Is Associated with Intrahepatic Cholangiocarcinoma and Not with Extrahepatic Form: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis. Eur. J. Gastroenterol. Hepatol. 2021;33:62–68. doi: 10.1097/MEG.0000000000001684. [DOI] [PubMed] [Google Scholar]
- 89.Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.-Y., Corbett M.S., Eldridge S.M., et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 90.Wetterslev J., Jakobsen J.C., Gluud C. Trial Sequential Analysis in Systematic Reviews with Meta-Analysis. BMC Med. Res. Methodol. 2017;17:39. doi: 10.1186/s12874-017-0315-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.TSA–Ctu.Dk. [(accessed on 22 September 2022)]. Available online: https://ctu.dk/tsa/
- 92.Corrao S., Natoli G., Argano C., Scichilone N. Gastroesophageal Reflux Disease and Idiopathic Pulmonary Fibrosis: No Data for Supporting a Relationship After a Systematic Review. Chest. 2019;156:190–192. doi: 10.1016/j.chest.2019.03.042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.