Abstract
Interventions adopting augmented and virtual reality (AR/VR) modalities allow participants to explore and experience realistic scenarios, making them useful psycho-educational tools for mental illnesses. This scoping review aims to evaluate the effectiveness of AR/VR interventions in improving (1) knowledge, (2) attitudes, (3) empathy and (4) stigma regarding people with mental illnesses. Literature on published studies in English up till April 2022 was searched within several databases. Sixteen articles were included. The majority of studies were conducted in the West (93.8%), within undergraduates (68.8%) but also amongst high school students, patients, caregivers, public including online community, and covered conditions including psychotic illnesses, dementia, anxiety and depression. A preponderance of these included studies which employed AR/VR based interventions observed improvements in knowledge (66.7%), attitudes (62.5%), empathy (100%) and reduction of stigma (71.4%) pertaining to people with mental illnesses. In the context of relatively limited studies, extant AR/VR based interventions could potentially improve knowledge, attitudes, empathy and decrease stigma regarding people with mental illness. Further research needs to be conducted in larger and more diverse samples to investigate the relatively beneficial effects of different AR/VR modalities and the durability of observed improvements of relevant outcomes of interests over time for different mental conditions.
Keywords: virtual reality, augmented reality, mental health literacy, help-seeking, empathy, stigma
1. Introduction
About 11% of the worldwide population suffer from a mental illness [1] and these mental illnesses remain the leading cause of substantial illness burden internationally in terms of disability adjusted life years [2]. Of note, people with mental illness often face challenges such as discrimination [3] and being literate in such conditions will allow people to have better understanding of people who suffer from mental illnesses [4].
Mental health literacy is defined as the knowledge and awareness of mental illness, including prevention, identification and management of these conditions [5]. Having a good level of mental health literacy can enhance the insight into mental illness, promote early help seeking, recovery and psychosocial functioning [6] and foster better attitudes towards patients with mental illness [7]. In addition, better awareness of mental illness has been associated with better employment [8], treatment adherence [9], stronger therapeutic alliance and lower clinical severity [10]. Regarding empathy, it is the ability to stand in the shoes of others and understand another’s experiences [11]. Empathy is said to have destigmatizing effects and therefore enhance positive attitudes towards people experiencing mental illness [12]. Concerning stigma about mental illnesses, it can be viewed as a set of unwarranted and negative beliefs and attitudes about mental illness, which can potentially influence discrimination, exclusion and fear of people experiencing mental illnesses [13].
Augmented reality (AR) uses technology to combine real and digital information so that participants experience the virtual and real contexts as one [14] and AR was used in the prominent Pokémon GO game [15]. Conversely, virtual reality (VR) excludes stimulus from the real-world setting. Virtual reality consists of two types: (1) desktop virtual reality and (2) immersive reality [16]. The former allows participants to control the virtual surroundings on a computer screen while immersive reality requires the use of a headset, earphones and controllers, which detects body movements to fully immerse participants in the virtual world.
AR and VR (AR/VR) technologies are gaining popularity in the field of healthcare and health professions education [17] as they allow participants to immerse in realistic simulations thus serving as a useful tool in training and learning [18]. VR has also been utilized in psychotherapy for the past two decades [19]. Since then, the use of VR as a treatment modality has grown. Of note, there are recent studies examining the effectiveness of AR/VR-based therapeutic modalities in the management of patients with neurodevelopmental spectrum conditions (such as autism spectrum disorders, attention deficit hyperactivity disorders) [20,21,22,23], anxiety disorders (such as phobias) [24,25,26,27], obsessive compulsive disorder [28,29,30], post-traumatic stress disorder [31], and cognitive impairments in the elderly [32,33]. In comparison, there are fewer studies specifically elucidating the effectiveness of AR/VR based interventions as a psychoeducational tool such as in improving understanding of mental illnesses, engendering more positive attitudes regarding people with mental illnesses [34,35] and reduction of stigma [36,37].
In light of increasing interest in the use of AR/VR-based modalities within the mental healthcare setting, this scoping review aims to evaluate the effectiveness (as evidenced by improvements in ratings) of AR/VR-based interventions in improving (1) knowledge, (2) attitudes, (3) empathy and (4) stigma pertaining to people with mental illnesses.
2. Methodology
A scoping review is useful for exploring the literature broadly to identify the extant evidence on a specific topic of interest [38]. This scoping review was conducted according to the methodology of the Joanna Briggs Institute for scoping reviews [38]. We adopted a modified Arksey and O’Malley methodological framework for conducting scoping reviews updated by Levac et al. (2010) to guide the study. The first step involves identifying the main research question addressed by this review: what is the effectiveness (evidenced by improvements in ratings) of AR/VR based interventions on (1) understanding, (2) attitudes, (3) empathy and (4) stigma related to people with mental illness?
The second step involves identification of relevant studies [39]. We searched several databases (CINAHL, Cochrane Central Register of Controlled Trials, Embase, PsycINFO, Pubmed, Science Direct and Scopus) for relevant studies that examined the research question from database inception until April 2022. Keywords and combination of keywords for the literature search included: ‘virtual reality’ OR ‘(augment* reality)’ AND ‘knowledge’, ‘attitude’, ‘empathy’, ‘stigma’; ‘(virtual reality)’ OR ‘(augment* reality)’ AND ‘knowledge’ OR ‘attitude’ OR ‘empathy’ OR ‘(social distance)’ OR ‘stigma OR depression OR schizophrenia OR bipolar disorder. The inclusion criteria are as follows: (A) primary research studies on the effectiveness of AR/VR-based interventions with relevant outcomes of interest regarding people with mental illnesses, and (B) articles must be published in English. Studies were not limited by population. Studies were excluded if they were non empirical papers, opinion articles, dissertations or did not include primary outcomes of interest.
The third step involves study selection. We manually screened the abstracts of identified reports to evaluate whether they met the inclusion criteria, before reviewing full reports of these studies. Two independent reviewers simultaneously screened the titles and abstracts. In case of any inconsistency between reviewers, the disagreement was resolved by thorough discussion within the team and a third reviewer.
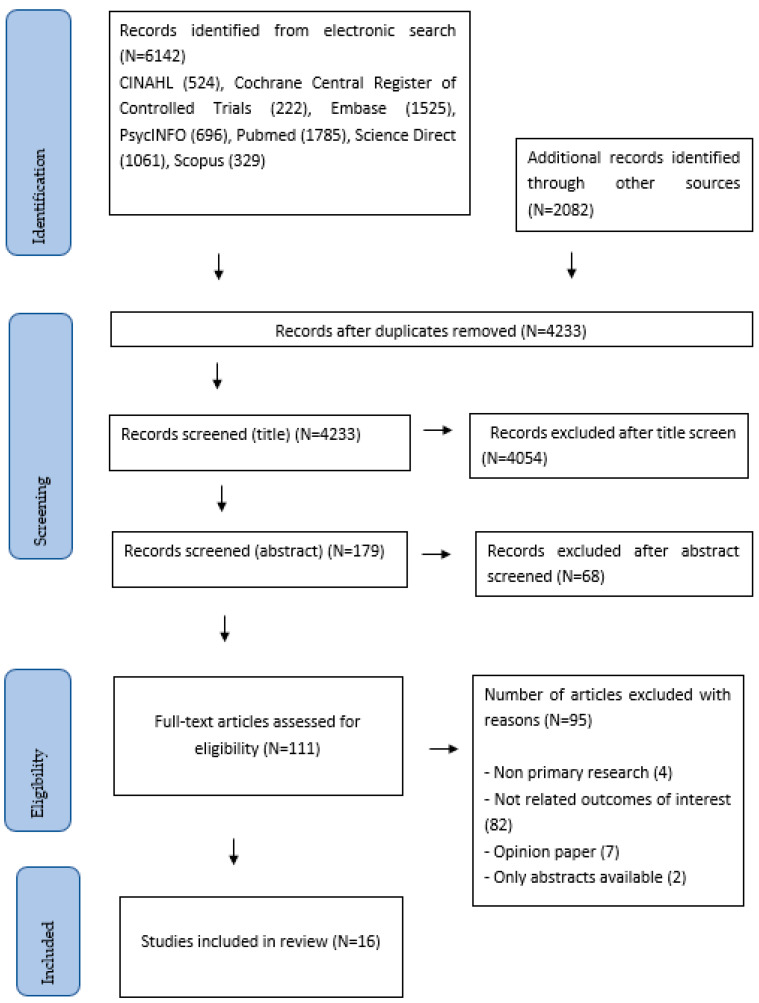
The fourth and fifth steps involve charting, collating and reporting the results. For each included study, we extracted variables including the author, year of publication, characteristics of participants, AR/VR based interventions, and the main findings. The preceding data were organized and summarized into a table to facilitate independent, critical assessment by the readers. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart for this review is shown in Figure 1 [40].
Figure 1.
Search strategy.
3. Results
3.1. Description of Studies
Overall, 16 studies were included in this review (Table 1). The number of participants ranged from 16 to 579 in each group and included undergraduates (11 of 16 studies, 68.8%), high school students, patients, caregivers and the public, including online community. Four studies were randomized controlled trials [36,41,42,43]. Ten studies adopted quasi-experimental design. One study was a descriptive study [44] and another a prospective cohort study [45]. Six studies were conducted in United States, three studies in Australia, two studies in Spain and one study each in Brazil, The Netherlands, Germany, Ireland and Hong Kong, respectively. Only one study examined AR-based intervention [46] while the remaining 15 studies examined the use of VR, with two utilizing a Virtual Dementia Tour intervention [47,48]. AR/VR interventions ranged from virtual interactions with characters (4 of 16 studies, 25%) [36,44,49,50], environments (4 of 16 studies, 25%) [34,41,51,52] and assuming a specific character within the study (2 of 16 studies, 13%) [43,53]. Some interventions (4 of 16 studies, 25%) also allowed the participants to experience perceptual or sensory disturbances such as auditory hallucinations [35,46,47,48]. The other interventions (2 of 16 studies, 13%) allowed participants to view scenarios of characters suffering from mental illnesses [42,45]. Please see Appendix A for Cochrane’s risk of bias rating for each study.
Table 1.
Details of included studies.
| Author Country/Setting |
Design/ Participant |
Intervention | Control | Outcome Measures | Knowledge | Attitudes | Empathy | Stigma |
|---|---|---|---|---|---|---|---|---|
| [51] United States |
2 arm quasi-experimental Patients with schizophrenia and healthy control |
G1: Patients with schizophrenia, n = 25 - Participants interact with surroundings, objects in a virtual environment using mouse. They were asked to take pills with virtual distractions (siren, ringing doorbells). |
G2: Healthy control, n = 16 - same intervention |
Pre - The Medication Management Ability Assessment (MMAA) - Continuous Performance Test |
↑ Better pill selection, less time discrepancy when taking medications and greater MMAA score with reminder notes, clock |
Nil | Nil | Nil |
| [47] United States |
Pre, post single group quasi-experimental Nursing under-graduates from 3 classes |
G1: Virtual Dementia Tour, n = 163 - equipment that altered participants’ vision, hearing and touch - complete 5 tasks - 10 min |
Pre group | Pre, post - Dementia Attitudes Scale - Knowledge about Memory Loss and Care - Healthcare tour survey Post only - Students’ reflection |
↑ Improvement noted post-test although it did not reach significant levels |
↑ Significant improvement at post-intervention |
↑ Students’ reflection highlighted that patients with dementia required empathy and sensitivity. Students affirmed the need to support caregivers and families. |
Nil |
| [49] Spain |
Post only single group quasi- experimental Psychology under-graduates aged 18 to 28 |
G1: Stigma-Stop, n = 26 | Nil | Post only - Open ended questions and the following questions rated ‘yes’ and ‘no’: (1) Whether character is emotionally well? (2) Whether participant can help the character? (3) Whether participant had similar experience? |
-- Most participants rated characters as emotionally unwell: a. 96%- panic disorder with agoraphobia b. 96% for schizophrenia c. 73% for bipolar disorder d. 100% for depression |
-- Most participants felt they could help the character: a. 100%- panic disorder with agoraphobia b. 88% for schizophrenia c. 79% for bipolar disorder d. 92% for depression |
Nil | ↓ Participants’ open-ended answers showed reduction of stigma. |
| [36] Spain |
2 arm pre post RCT High school students aged 14–18, from 24 classes |
G1: Stigma-Stop, n = 484 from 21 classes - Non immersive virtual reality game presenting four characters experiencing depression, bipolar disorder, schizophrenia, panic disorder with agoraphobia. |
G2: n = 68 from 3 classes | Pre, post - Student Attitudes toward Schizophrenia measures stereotypes and other aggressiveness |
-- Most participants rated characters as emotionally unwell: a. 96.8%- panic disorder with agoraphobia b. 86.8% for schizophrenia c. 61.8% for bipolar disorder d. 96.1% for depression |
-- About half to most of the participants felt they could help the character: a. 82.4%- panic disorder with agoraphobia b. 62.5% for schizophrenia c. 53% for bipolar disorder d. 90% for depression |
Nil | ↓ Stigma-Stop group had significantly lower stigma |
| [34] Australia |
Pre-post single group quasi- experimental Public and psychology under-graduates |
G1: VR, n = 50 - with head mounted display, headphones and Xbox controller, - virtual environment with VH environmental sounds and voices suggestive of danger - 10–15 min |
Pre group | Pre, post - Knowledge * about psychosis - Attitude ^ by Reavley and Jorm (2011) - Empathy by clinical empathy scale |
↑ Significant improvement at post-test |
↑ Significant improvement in attitude scores at post-test |
↑ Significant improvement in empathy scores at post-test |
Nil |
| [35] Australia |
Pre-post 2 arm quasi-experimental Medicine and pharmacy under-graduates |
G1: Australia Vic Virtual Dementia Experience, n= 80 - multisensory, virtual simulation to allow participants to experience perceptual and cognitive difficulties by patients - 1.5 h |
G2: Waitlist control group, n = 198 - curriculum as usual |
Pre post - Dementia Attitudes Scale |
Nil | ↑ Intervention group had significantly better attitude scores at post-test |
Nil | Nil |
| [44] United States |
Descriptive study Nursing students, n = 126 |
G1: VR condition, n = 126 - Students viewed virtual neighbourhood with two houses: one belonged to someone with schizophrenia, another with depression. Students enter house and interact with patient. - Students were given case studies on the patients. - 45–60 min |
Nil | Post only - * 35-item Second Life (SL) Simulation Evaluation Survey - Two open-ended questions regarding feedback about stimulation |
↑ Second Life Simulation, as a teaching modality, was moderately effective. |
Nil | Nil | Nil |
| [45] United States |
Pre- and post-intervention study 4th year nursing undergraduates |
G1: VR, n = 149 - one virtual simulation case study weekly on depression, bipolar disorder, anxiety, alcohol withdrawal and schizophrenia - 30 min, student can repeat simulation |
G2: Non-simulation group, n = 150 | Post only - Two vignettes, schizophrenia and depression. Participants answer about their perception of helpfulness of certain people (including healthcare workers, traditional healers, family and friends), specific medications and interventions (e.g., physical activity, massage, relaxation, specific therapies). |
↑ For perceived helpfulness of pharmacological interventions, intervention group was less likely to rate antipsychotics and sleeping pills as ‘do not know’ for the depression vignette. Control group was more likely than G1 to rate psychiatric hospital admission and electroconvulsive therapy as ‘do not know’. |
-- Both groups agreed solving the problem by self as unhelpful. |
Nil | Nil |
| [50] Australia |
Pre post single group quasi-experimental Students and public |
G1: Visit with Viv, n = 35: - VR about Viv, who recounts her experiences of dementia > life-size in art gallery, > Occulus Quest VR headset in university, n = 36 - 15–20 min |
Pre group | Pre post - comprehensive state empathy scale - Change in emotional distance scale |
Nil | Nil | ↑ Significant improvement in empathy scores from pre-test |
↓ Significant reduction in stigma levels at post-test |
| [46] Brazil |
Pre post single group quasi-experimental Medical students from 3 universities |
G1: AR, n = 21 - figures and voices from narratives of three patients with schizophrenia - voices included whispers, commanding and threatening speech - 3 min |
Pre group | Pre post - Schizophrenia stigma * Post only - Evaluate environment simulation |
Nil | ↑ Significant increase in the average score of help-giving at post-test |
↑ Increase in empathy |
↑ Increase in stigma especially in fear, pity and segregation. |
| [48] Ireland |
Pre post repeated single group quasi-experimental Health professionals, voluntary groups and public |
G1: Virtual Dementia Tour + watching another group doing distortion session, n = 240 - 2 h - 10 min of sensory distortion - 30 min debriefing |
Pre group | Pre post, follow up at 3 months * Tool that measures empathy, understanding of behaviours and role of the person in care decisions. |
↑ Significant improvement in understanding of behavioural impact of dementia across time points |
Nil | ↑ Significant improvement in empathy across time |
Nil |
| [41] United States |
4 arm post only RCT Psychology research participant pool and university community |
G1: VR condition, n = 26 - Participant plays the character of someone experiencing schizophrenia, visiting a pharmacist asking for prescription refill. - 4.5 min G2: Empathy condition, n = 26 - Participants were asked to pen their thoughts about experiencing VH and AH while getting prescription - 1 min G3: VR+ empathy condition, n = 26 - Empathy before VR condition |
G4: control, n = 26 No intervention control group |
Post only - Empathy 12-items - Social Distance Scale - Attitudes Toward People with Schizophrenia, 7 items - Evaluation of simulation - Pre-existing attitudes towards people with schizophrenia, 8 items |
Nil | ↑ Intervention group had better attitudes but this did not reach significant levels |
↑ Significant improvement in empathy in intervention groups using VR |
↓ VR group had significantly lower stigma |
| [42] Germany |
3 arm post only RCT Majority are students from university, n = 114 |
G1: VR, n = 31 - Young male actor speaking about his experiences with schizophrenia, including how his loved ones cope with it. G2: regular video, n = 45 - Similar as the VR but fixed perspective |
G3: No intervention control group, n = 38 | Post only - Stigma with four related constructs: anxiety *, social proximity ^, empathy (by Kinnebrock et al., 2010, - Benevolence (using Community-Attitudes-Toward-the-Mentally Ill Inventory) |
Nil | Nil | Nil | ↑ VR contact did not decrease stigmatization compared with control but had increased stigmatization compared with video. |
| [53] The Netherlands Alzheimer’s Society |
Pre post single group quasi-experimental Informal caregivers caring for those with dementia |
G1: VR, n = 35 360-degree simulation movie on virtual reality (first person view) and e-course, n = 42- different scenes of interactions e.g., confronted by daughter about remote control in cupboard and she talks to people on the phone about you - 13 min |
Pre group | Pre, post - Empathy measured by Person-centeredness subscale of Approach to Dementia questionnaire and ‘perspective-taking’ subscale of Interpersonal Reactivity Index |
Nil | Nil | ↑ Significant improvement using the perspective-taking subscale |
Nil |
| [52] United States |
Post only single group quasi- experimental Second Life Users |
G1: Second Life VR, n = 579 - Character toured environment, experiencing hallucinations including voices, posters changing text to profanities, floor that fall away, TV that encourage suicide and gun with voices telling character to commit suicide, and own reflection with bleeding eyes. |
Nil | Post only - Questions about understanding of hallucinations |
-- Intervention group had improvements of understanding of (1) AH- 76.86% (2) VH- 69.91% (3) Schizophrenia- 73.9% |
Nil | Nil | Nil |
| [43] Hong Kong |
3 arm pre post RCT University students 18 years old and above |
G1: Immersive animation, n = 82 Participants played a character, Yan, who had mixed anxiety and depression, and who was speaking with an uncle. Pop up messages illustrated problems in Uncle’s communication. G2: Text condition, n = 80 Participants read same story in 2D effect, without immersive experience. All 3 groups: 10 min, had VR headset, Oculus Go. |
G3: Control, n = 82 Exoplanet VR video, 360° |
Pre, post, 1 week follow up: - Stigma by 21-item Public Stigma and Acceptance Scale - 7-item Sense of Embodiment Scale * - Story Transportation |
Nil | Nil | Nil | ↓ Immersive animation and text condition had significantly lower public stigma at post-test and follow up compared with the control group. Immersive animation vs. text condition did not have significantly different stigma levels between them. |
AH = auditory hallucinations; AR = augmented reality; diff = difference; G = group; M = Mean; MMAA = Medication Management Ability Assessment’ min = minutes; sig = significantly; VH = visual hallucinations; * constructed by authors; ^ modified by authors, ↑ = increased, ↓ = decreased, -- = non-quantitative measurement.
3.2. Knowledge about Mental Illnesses
Nine studies examined the effects of VR interventions on knowledge and awareness of mental illness with the majority (six of nine studies) showing increased knowledge about these conditions [34,44,45,47,48,51]. In terms of nature of mental conditions, three studies examined knowledge about a range of mental illnesses [36,45,49]. Five studies examined knowledge about specific disorders, namely, psychotic conditions [34,52], dementia [47,48] and one study evaluated knowledge about both depression and schizophrenia [44]. Another study examined the effects of VR intervention on medication adherence amongst patients with schizophrenia [51].
In terms of nature of intervention, the study by Formosa et al. (2018) allowed participants to interact within a virtual reality intervention that simulated danger, and found significant improvement in knowledge about the psychotic disorder. Stigma-Stop is a video game that allows players to interact virtually with characters with mental illnesses. After utilizing Stigma-Stop, more than 85% of the high school students in Spain could identify panic disorder, depression and schizophrenia, although only slightly more than half could identify bipolar disorder [36]. This was largely congruent with the findings amongst psychology undergraduates in Spain [49]. Second Life (SL) simulation, involving players in a virtual reality environment, as a teaching modality, was deemed moderately effective as a psycho-educational modality [44]. In an earlier study, participants indicated greater understanding of schizophrenia, auditory and visual hallucinations after using Second Life intervention [52]. Among nursing undergraduates in the United States, the intervention group assigned with the VR case study was less likely to rate ‘do not know’ when asked about the effectiveness of hospital admission and electroconvulsive therapy indicating better knowledge [45]. One study found that reminder notes and clock in the virtual environment aided in better understanding of medication adherence [51]. Two studies used Virtual Dementia Tours whereby participants experienced changes in sensory perception while engaging in everyday tasks [47,48] with conflicting findings of improved knowledge about dementia in one study [48], but not the other [47].
3.3. Attitudes toward People with Mental Illnesses
Eight studies examined the effects of AR/VR based intervention on attitudes towards people with mental illness and more than half (five of eight studies) showed improvement of attitudes following the intervention [34,35,41,46,47]. In terms of the nature of mental illness, three studies examined attitudes towards a range of mental illnesses [36,45,49], three related to psychotic disorders [34,41,46] and two studies examined attitudes towards people with dementia [35,47].
For qualitative findings that were conducted in two studies in Spain, at least half of the participants felt that they were able to help the character with schizophrenia or bipolar and more than 80% of them felt being able to help the character with depression or panic disorder after following Stigma-Stop intervention [36,49]. In a separate study by Liu et al. (2020), participants from both VR and control groups acknowledged the need for external help beyond self, thus suggesting no difference in attitudes between the two groups.
3.4. Empathy
Seven studies examined empathy towards people either with dementia [47,48,50,53] or psychotic conditions [34,41,46], and found improvements of empathy across all studies following the intervention. Specific empathy scales included the Clinical Empathy Scale [34], Comprehensive State Empathy Scale [50], and 12 item Empathy Scale [41]. In the study by Wijma et al. (2018), improvement in empathy was observed in the “Perspective-taking” subscale of Interpersonal Reactivity Index but not in the “Person centeredness” subscale.
3.5. Stigma Regarding People with Mental Illnesses
Seven studies examined stigma towards people with dementia [50], psychotic illnesses [41,42,46], mixed anxiety and depression [43] or a range of mental illnesses [36,49]. Most studies (five out of seven studies) found reduction of stigma for both within [36,50] and between group comparisons [36,41,43] while two studies did not [42,46].
Amongst medical students in Brazil, stigma levels were increased post-intervention [46], and students considered the VR characters with schizophrenia more dangerous than pre-intervention. Similarly, in Germany, VR intervention increased stigma when compared with both video and no intervention control groups [42].
4. Discussion
Overall, the majority of studies included in this scoping review were conducted in the West (93.8%), within undergraduates (68.8%) but also amongst high school students, patients, caregivers, public including online community, and covered conditions including psychotic illnesses, dementia, anxiety and depression. Amid the variety of AR/VR modalities employed within the included studies, the preponderance of these studies observed improvements in knowledge (66.7%), attitudes (62.5%), empathy (100%) and reduced stigma (71.4%) regarding people with mental illnesses.
4.1. Knowledge about Mental Illnesses
We found that the AR/VR interventions used in this review were beneficial in increasing knowledge of mental illness. The VR interventions employed in the included studies allowed participants to interact with virtual characters with mental illnesses or experience perceptual or sensory abnormalities that patients with schizophrenia or dementia experience. Such patient experiences made possible through AR/VR modalities allow the participants to gain insights into the relevant mental illnesses and could impact positively on learning outcomes [54]. For example, AR/VR modalities can enhance intrinsic motivation, engagement and facilitate deeper learning in the context of life such as scenarios [54,55,56]. These benefits have rendered learning using AR/VR more fruitful than traditional learning [57]. Of note, VR have been increasingly utilized in health professions education amongst medical students, nursing students, allied health and even patients and their caregivers [58,59,60,61]. Amongst healthcare students, virtual reality interventions have been observed to improve skill competencies, and better appreciation of symptom and illness [62]. Earlier studies have found that AR/VR interventions can be adopted to manage conditions such as specific phobias, autism spectrum disorder, psychotic conditions, substance related disorders, depression and eating disorders [23,24,63,64]. In our review, we observed that VR intervention could help to assess and enhance medication adherence amongst patients with schizophrenia (Baker et al., 2006).
4.2. Attitude towards People with Mental Illnesses
It was observed that the AR/VR interventions improved participants’ attitudes towards people with mental illness. AR/VR-based simulations have the ability to expose participants to realistic experiences such as visual and auditory hallucinations, enhance understanding of the unique journeys that people with mental illnesses undergo and thereby foster better patient engagement [65,66]. The current findings are in agreement with that of an earlier review of AR/VR-based interventions in dementia which found that such modalities can potentially enhance knowledge and attitudes of healthcare professionals and trainees towards people with neurocognitive disorders [67].
4.3. Empathy
It was found that the AR/VR-based interventions were largely effective in improving participants’ empathy towards people with mental illnesses. This was consistent across all intervention types including viewing of immersive VR videos of characters with mental disorders and VR interventions that allowed participants to experience perceptual disturbances. This was also consistent with earlier findings that suggested that improvements in empathy were not dependent on the nature of VR intervention [68]. The affinity between the VR character and participant was more important than the specific VR design [42,69]. Likewise, the effectiveness of the VR intervention in enhancing empathy was not dependent on whether or not the VR intervention allowed participants to adopt the protagonist character as both types of VR interventions were equally effective in some studies [34,35,44,47,51,70].
Empathy allows the observer to stand in the place of the other person, and experience compassion and loving kindness towards others whilst preserving one’s sense of identity, thoughts and emotions [71]. Training programs that have included the use of VR interventions have found increased empathy towards patients with specific conditions such as dementia [72], Alzheimer’s disease [73], hearing and vision loss [73] among carers, medical and nursing students.
4.4. Stigma
The misconception that people with mental disorders are unpredictable, violent or aggressive has been seen across societies [74]. Within this review, various VR modalities proved effective in reducing stigma towards mental illnesses, for example, Stigma-Stop (for range of mental conditions), Visit with Viv (for dementia), simulated hallucinations using VR that allowed participants to experience psychopathology (for psychotic disorders) and immersive animation in which participants played a character with mixed depression and anxiety (for affective and anxiety conditions).
However, two interventions found an increase in stigma levels involving an AR modality with simulated hallucinations [46], and a VR intervention whereby a character spoke about his experiences with schizophrenia [42]. There are several possible reasons to explain the increase in stigma. First, mere simulation of schizophrenia may not reduce stigma unless participants can internalize such experiences and reflect on what people with mental disorders are truly experiencing [41]. Second, the construct of stigma is complex and influenced by various factors such as internalized perspectives (micro level), interactions with people with mental illnesses (meso level) and the integrated experience involving the milieu of the healthcare setting (macro level) [75]. Furthermore, these factors may also interact with other aspects such as knowledge, attitudes and aspects of empathy to affect stigma [12,76,77]. Third, the affinity between the VR character and the participants and the likeability of the VR character are likely to influence research findings [42]. Fourth, there may be participants who were uncomfortable with VR, which can overwhelm their senses. Such sensations can be intimidating, unpleasant, thus limiting the participant’s ability to engage, reflecting an increase in stigma levels [42].
5. Limitations and Future Research Directions
This review had several limitations. First, there were limited studies which were mostly conducted in the West amongst undergraduates, hence more future studies are warranted especially in more diverse groups internationally including within Asia. Second, the majority of the included studies had small to modest sample sizes with variable measures of outcomes. Some studies had no control group, randomization and blinding. Third, this review did not limit papers according to population, which might have contributed to the heterogeneity of the findings of included studies. Fourth, the interventions varied in terms of the types of headsets and nature of AR/VR modalities. Future research can focus on the evaluation of AR/VR-based tools in larger samples of participants (such as residents in training and healthcare professionals across different disciplines) and comparison of different AR versus VR modalities. This can be performed across different sites and adopt a standard set of rating scales over time to better evaluate the impact of such AR/VR interventions in enhancing mental health literacy, positive attitudes, empathy and reduction in stigma towards people with mental illnesses.
6. Conclusions
In the context of limited studies, AR/VR based interventions were found to potentially improve knowledge, attitudes, empathy and reduce stigma related to people with mental illnesses. Further research is needed to investigate the relative beneficial effects of the different AR/VR modalities and the durability of observed improvements in outcomes of interests over time for different mental conditions.
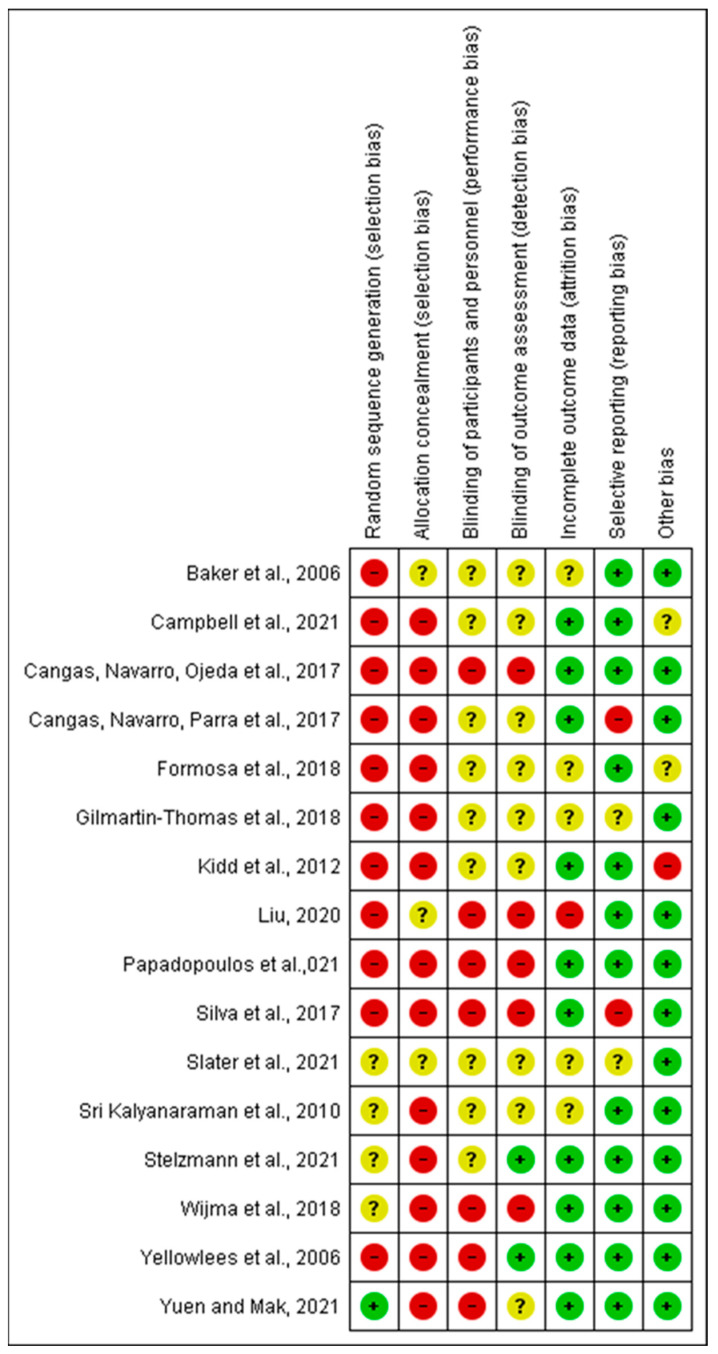
Appendix A
Figure A1.
(+): low risk of bias, (-): high risk of bias, (?): unknown risk of bias [34,35,36,41,42,43,44,45,46,47,48,49,50,51,52,53].
Author Contributions
Conceptualization, K.S. and J.L.T.; Methodology, K.S., J.L.T. and H.X.; Formal Analysis, J.L.T., K.S. and H.X.; Writing—Original Draft Preparation, J.L.T. and K.S.; Writing—Review and Editing, J.L.T., K.S. and H.X.; Supervision, K.S.; Funds acquisition, K.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The study was funded by West Region Department Fund, Institute of Mental Health.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Dattani S., Ritchie H., Roser M. Mental Health. [(accessed on 18 November 2021)]. Available online: https://ourworldindata.org/mental-health.
- 2.GBD Mental Disorders Collaborators Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–150. doi: 10.1016/S2215-0366(21)00395-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pescosolido B.A., Jensen P.S., Martin J.K., Perry B.L., Olafsdottir S., Fettes D. Public knowledge and assessment of child mental health problems: Findings from the National Stigma Study-Children. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47:339–349. doi: 10.1097/CHI.0b013e318160e3a0. [DOI] [PubMed] [Google Scholar]
- 4.Furnham A., Swami V. Mental health literacy: A review of what it is and why it matters. Int. Perspect. Psychol. 2018;7:240–257. doi: 10.1037/ipp0000094. [DOI] [Google Scholar]
- 5.Jorm A.F., Korten A.E., Jacomb P.A., Christensen H., Rodgers B., Pollitt P. “Mental health literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med. J. Aust. 1997;166:182–186. doi: 10.5694/j.1326-5377.1997.tb140071.x. [DOI] [PubMed] [Google Scholar]
- 6.Cheng H.L., Wang C., McDermott R.C., Kridel M., Rislin J.L. Self-stigma, mental health literacy, and attitudes toward seeking psychological help. J. Couns. Dev. 2018;96:64–74. doi: 10.1002/jcad.12178. [DOI] [Google Scholar]
- 7.Tay J.L., Tay Y.F., Klainin-Yobas P. Effectiveness of information and communication technologies interventions to increase mental health literacy: A systematic review. Early Interv. Psychiatry. 2018;12:1024–1037. doi: 10.1111/eip.12695. [DOI] [PubMed] [Google Scholar]
- 8.Błądziński P., Kalisz A., Adamczyk P., Arciszewska A., Mętel D., Daren A., Cechnicki A. Associations of insight and treatment adherence with employment status of people with schizophrenia. Postępy Psychiatrii Neurologii Adv. Psychiatry Neurol. 2019;28:21–33. doi: 10.5114/ppn.2018.81364. [DOI] [Google Scholar]
- 9.Garcia-Cabeza I., Victor F., de Portugal E. Relationship between insight, adherence and disability in the diagnose of paranoid schizophrenia. J. Ment. Health Clin. Psychol. 2018;2:6–10. doi: 10.29245/2578-2959/2018/6.1172. [DOI] [Google Scholar]
- 10.Novick D., Montgomery W., Treuer T., Aguado J., Kraemer S., Haro J.M. Relationship of insight with medication adherence and the impact on outcomes in patients with schizophrenia and bipolar disorder: Results from a 1-year European outpatient observational study. BMC Psychiatry. 2015;15:1–8. doi: 10.1186/s12888-015-0560-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moudatsou M., Stavropoulou A., Philalithis A., Koukouli S. The role of empathy in health and social care professionals. Healthcare. 2020;8:26. doi: 10.3390/healthcare8010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hecht M., Kloß A., Bartsch A. Stopping the Stigma. How Empathy and Reflectiveness Can Help Reduce Mental Health Stigma. Media Psychol. 2021;25:367–386. doi: 10.1080/15213269.2021.1963991. [DOI] [Google Scholar]
- 13.Henderson C., Gronholm P.C. Mental health related stigma as a ‘wicked problem’: The need to address stigma and consider the consequences. Int. J. Environ. Res. Public Health. 2018;15:1158. doi: 10.3390/ijerph15061158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Squire K., Klopfer E. Augmented reality simulations on handheld computers. J. Learn. Sci. 2007;16:371–413. doi: 10.1080/10508400701413435. [DOI] [Google Scholar]
- 15.Chong Y., Sethi D.K., Loh C.H.Y., Lateef F. Going forward with pokemon go. J. Emergencies Trauma Shock. 2018;11:243. doi: 10.4103/JETS.JETS_87_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee E.A.-L., Wong K.W., Fung C.C. How does desktop virtual reality enhance learning outcomes? A structural equation modeling approach. Comput. Educ. 2010;55:1424–1442. [Google Scholar]
- 17.Wu Y., Zhang M., Li X., Gan Y., Zhao C. Augment Reality-Based Teaching Practice. Biomed. Eng. Educ. 2021;1:237–241. doi: 10.1007/s43683-020-00040-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamilton D., McKechnie J., Edgerton E., Wilson C. Immersive virtual reality as a pedagogical tool in education: A systematic literature review of quantitative learning outcomes and experimental design. J. Comput. Educ. 2021;8:1–32. doi: 10.1007/s40692-020-00169-2. [DOI] [Google Scholar]
- 19.Rizzo A.S. Clinical virtual reality in mental health and rehabilitation: A brief review of the future!; Proceedings of the SPIE 11002, Infrared Technology and Applications XLV 2019; Baltimore, MD, USA. 14–18 April 2019; pp. 150–158. [Google Scholar]
- 20.Almurashi H., Bouaziz R., Alharthi W., Al-Sarem M., Hadwan M., Kammoun S. Augmented reality, serious games and picture exchange communication system for people with ASD: Systematic literature review and future directions. Sensors. 2022;22:1250. doi: 10.3390/s22031250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barba M.C., Covino A., De Luca V., De Paolis L.T., D’Errico G., Di Bitonto P., Di Gestore S., Magliaro S., Nunnari F., Paladini G.I. BRAVO: A gaming environment for the treatment of ADHD; Proceedings of the International Conference on Augmented Reality, Virtual Reality and Computer Graphics; Santa Maria al Bagno, Italy. 24–27 June 2019; pp. 394–407. [Google Scholar]
- 22.Goharinejad S., Goharinejad S., Hajesmaeel-Gohari S., Bahaadinbeigy K. The usefulness of virtual, augmented, and mixed reality technologies in the diagnosis and treatment of attention deficit hyperactivity disorder in children: An overview of relevant studies. BMC Psychiatry. 2022;22:1–13. doi: 10.1186/s12888-021-03632-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karami B., Koushki R., Arabgol F., Rahmani M., Vahabie A.-H. Effectiveness of Virtual/Augmented Reality-based therapeutic interventions on individuals with autism spectrum disorder: A comprehensive meta-analysis. Front. Psychiatry. 2021;12:887. doi: 10.3389/fpsyt.2021.665326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albakri G., Bouaziz R., Alharthi W., Kammoun S., Al-Sarem M., Saeed F., Hadwan M. Phobia Exposure Therapy Using Virtual and Augmented Reality: A Systematic Review. Appl. Sci. 2022;12:1672. doi: 10.3390/app12031672. [DOI] [Google Scholar]
- 25.Caponnetto P., Triscari S., Maglia M., Quattropani M.C. The Simulation Game—Virtual Reality Therapy for the Treatment of Social Anxiety Disorder: A Systematic Review. Int. J. Environ. Res. Public Health. 2021;18:13209. doi: 10.3390/ijerph182413209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hinze J., Röder A., Menzie N., Müller U., Domschke K., Riemenschneider M., Noll-Hussong M. Spider Phobia: Neural Networks Informing Diagnosis and (Virtual/Augmented Reality-Based) Cognitive Behavioral Psychotherapy—A Narrative Review. Front. Psychiatry. 2021;12:704174. doi: 10.3389/fpsyt.2021.704174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ma L., Mor S., Anderson P.L., Baños R.M., Botella C., Bouchard S., Cárdenas-López G., Donker T., Fernández-Álvarez J., Lindner P. Integrating virtual realities and psychotherapy: SWOT analysis on VR and MR based treatments of anxiety and stress-related disorders. Cogn. Behav. Ther. 2021;50:509–526. doi: 10.1080/16506073.2021.1939410. [DOI] [PubMed] [Google Scholar]
- 28.Cullen A.J., Dowling N.L., Segrave R., Carter A., Yücel M. Exposure therapy in a virtual environment: Validation in obsessive compulsive disorder. J. Anxiety Disord. 2021;80:102404. doi: 10.1016/j.janxdis.2021.102404. [DOI] [PubMed] [Google Scholar]
- 29.Dehghan B., Saeidimehr S., Sayyah M., Rahim F. The Effect of Virtual Reality on Emotional Response and Symptoms Provocation in Patients with OCD: A Systematic Review and Meta-Analysis. Front. Psychiatry. 2021;12:733584. doi: 10.3389/fpsyt.2021.733584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.García-Batista Z.E., Guerra-Peña K., Alsina-Jurnet I., Cano-Vindel A., Cantisano-Guzmán L.M., Nazir-Ferreiras A., Moretti L.S., Medrano L.A., Garrido L.E. Design and Validation of Augmented Reality Stimuli for the Treatment of Cleaning Obsessive-Compulsive Disorder. Front. Psychol. 2021;12:618874. doi: 10.3389/fpsyg.2021.618874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eshuis L., van Gelderen M., van Zuiden M., Nijdam M., Vermetten E., Olff M., Bakker A. Efficacy of immersive PTSD treatments: A systematic review of virtual and augmented reality exposure therapy and a meta-analysis of virtual reality exposure therapy. J. Psychiatr. Res. 2021;143:516–527. doi: 10.1016/j.jpsychires.2020.11.030. [DOI] [PubMed] [Google Scholar]
- 32.Georgiev D.D., Georgieva I., Gong Z., Nanjappan V., Georgiev G.V. Virtual reality for neurorehabilitation and cognitive enhancement. Brain Sci. 2021;11:221. doi: 10.3390/brainsci11020221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sejunaite K., Lanza C., Ganders S., Iljaitsch A., Riepe M. Augmented reality: Sustaining autonomous way-finding in the community for older persons with cognitive impairment. J. Frailty Aging. 2017;6:206–211. doi: 10.14283/jfa.2017.25. [DOI] [PubMed] [Google Scholar]
- 34.Formosa N.J., Morrison B.W., Hill G., Stone D. Testing the efficacy of a virtual reality-based simulation in enhancing users’ knowledge, attitudes, and empathy relating to psychosis. Aust. J. Psychol. 2018;70:57–65. doi: 10.1111/ajpy.12167. [DOI] [Google Scholar]
- 35.Gilmartin-Thomas J.F.-M., McNeil J., Powell A., Malone D.T., Wolfe R., Larson I.C., O’Reilly C.L., Kirkpatrick C.M., Kipen E., Petrovich T. Impact of a virtual dementia experience on medical and pharmacy students’ knowledge and attitudes toward people with dementia: A controlled study. J. Alzheimer’s Dis. 2018;62:867–876. doi: 10.3233/JAD-170982. [DOI] [PubMed] [Google Scholar]
- 36.Cangas A.J., Navarro N., Parra J., Ojeda J.J., Cangas D., Piedra J.A., Gallego J. Stigma-Stop: A serious game against the stigma toward mental health in educational settings. Front. Psychol. 2017;8:1385. doi: 10.3389/fpsyg.2017.01385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu J. VR-Assisted Curriculum on Depression for Stigma Reduction. [(accessed on 8 November 2021)]; Available online: https://clinicaltrials.gov/ct2/show/study/NCT03912597.
- 38.Peters M.D., Godfrey C.M., McInerney P., Soares C.B., Khalil H., Parker D. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. [(accessed on 1 December 2021)]. Available online: https://nursing.lsuhsc.edu/jbi/docs/reviewersmanuals/scoping-.pdf.
- 39.Levac D., Colquhoun H., O’Brien K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010;5:1–9. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 41.Sri Kalyanaraman S., Penn D.L., Ivory J.D., Judge A. The Virtual Doppelganger: Effects of a Virtual Reality Simulator on Perceptions of Schizophrenia. J. Nerv. Ment. Dis. 2010;198:437–443. doi: 10.1097/NMD.0b013e3181e07d66. [DOI] [PubMed] [Google Scholar]
- 42.Stelzmann D., Toth R., Schieferdecker D. Can intergroup contact in virtual reality (VR) reduce stigmatization against people with schizophrenia? J. Clin. Med. 2021;10:2961. doi: 10.3390/jcm10132961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yuen A.S., Mak W.W. The effects of immersive virtual reality in reducing public stigma of mental illness in the university population of Hong Kong: Randomized controlled trial. J. Med. Internet Res. 2021;23:e23683. doi: 10.2196/23683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kidd L.I., Knisley S.J., Morgan K.I. Effectiveness of a Second Life® simulation as a teaching strategy for undergraduate mental health nursing students. J. Psychosoc. Nurs. Ment. Health Serv. 2012;50:28–37. doi: 10.3928/02793695-20120605-04. [DOI] [PubMed] [Google Scholar]
- 45.Liu W. The Effects of Virtual Simulation on Undergraduate Nursing Students’ Mental Health Literacy: A Prospective Cohort Study. Issues Ment. Health Nurs. 2020;42:239–248. doi: 10.1080/01612840.2020.1793248. [DOI] [PubMed] [Google Scholar]
- 46.Silva R.D.D.C., Albuquerque S.G., Muniz A.D.V., Ribeiro S., Pinheiro P.R., Albuquerque V.H.C. Reducing the schizophrenia stigma: A new approach based on augmented reality. Comput. Intell. Neurosci. 2017;2017:2721846. doi: 10.1155/2017/2721846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Campbell D., Lugger S., Sigler G.S., Turkelson C. Increasing awareness, sensitivity, and empathy for Alzheimer’s dementia patients using simulation. Nurse Educ. Today. 2021;98:104764. doi: 10.1016/j.nedt.2021.104764. [DOI] [PubMed] [Google Scholar]
- 48.Slater P., Hasson F., Moore K., Sharkey F. Simulated Based Dementia Training: Impact on Empathic Understanding and Behaviour Among Professionals and Carers. Clin. Simul. Nurs. 2021;55:43–51. doi: 10.1016/j.ecns.2021.04.004. [DOI] [Google Scholar]
- 49.Cangas A.J., Navarro N., Ojeda J.J., Cangas D., Piedra J.A., Gallego J. Assessment of the usefulness and appeal of stigma-stop by psychology students: A serious game designed to reduce the stigma of mental illness. Mental Health. 2017;2:5. doi: 10.25046/aj020324. [DOI] [Google Scholar]
- 50.Papadopoulos C., Kenning G., Bennett J., Kuchelmeister V., Ginnivan N., Neidorf M. A visit with Viv: Empathising with a digital human character embodying the lived experiences of dementia. Dementia. 2021;20:2462–2477. doi: 10.1177/1471301221998888. [DOI] [PubMed] [Google Scholar]
- 51.Baker E.K., Kurtz M., Astur R.S. Virtual reality assessment of medication compliance in patients with schizophrenia. CyberPsychol. Behav. 2006;9:224–229. doi: 10.1089/cpb.2006.9.224. [DOI] [PubMed] [Google Scholar]
- 52.Yellowlees P.M., Cook J.N. Education about hallucinations using an internet virtual reality system: A qualitative survey. Acad. Psychiatry. 2006;30:534–539. doi: 10.1176/appi.ap.30.6.534. [DOI] [PubMed] [Google Scholar]
- 53.Wijma E.M., Veerbeek M.A., Prins M., Pot A.M., Willemse B.M. A virtual reality intervention to improve the understanding and empathy for people with dementia in informal caregivers: Results of a pilot study. Aging Ment. Health. 2018;22:1121–1129. doi: 10.1080/13607863.2017.1348470. [DOI] [PubMed] [Google Scholar]
- 54.Smith F. Beyond Reality: Augmented, Virtual, and Mixed Reality in the Library. ALA Editions; Chicago, IL, USA: 2019. Information literacy instruction using virtual reality; pp. 87–98. [Google Scholar]
- 55.Freina L., Ott M. A literature review on immersive virtual reality in education: State of the art and perspectives; Proceedings of the International Scientific Conference Elearning and Software for Education; Bucharest, Romania. 23–24 April 2015; pp. 1000–1007. [Google Scholar]
- 56.Pantelidis V.S. Reasons to use virtual reality in education and training courses and a model to determine when to use virtual reality. Themes Sci. Technol. Educ. 2010;2:59–70. [Google Scholar]
- 57.Webster R. Declarative knowledge acquisition in immersive virtual learning environments. Interact. Learn. Environ. 2016;24:1319–1333. doi: 10.1080/10494820.2014.994533. [DOI] [Google Scholar]
- 58.Alfalah S.F., Falah J.F., Alfalah T., Elfalah M., Muhaidat N., Falah O. A comparative study between a virtual reality heart anatomy system and traditional medical teaching modalities. Virtual Real. 2019;23:229–234. doi: 10.1007/s10055-018-0359-y. [DOI] [Google Scholar]
- 59.Fertleman C., Aubugeau-Williams P., Sher C., Lim A.-N., Lumley S., Delacroix S., Pan X. A discussion of virtual reality as a new tool for training healthcare professionals. Front. Public Health. 2018;6:44. doi: 10.3389/fpubh.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pillai A.S., Mathew P.S. Virtual and Augmented Reality in Mental Health Treatment. IGI Global; Hershey, PA, USA: 2019. Impact of virtual reality in healthcare: A review; pp. 17–31. [Google Scholar]
- 61.Plotzky C., Lindwedel U., Sorber M., Loessl B., König P., Kunze C., Kugler C., Meng M. Virtual reality simulations in nurse education: A systematic mapping review. Nurse Educ. Today. 2021;101:104868. doi: 10.1016/j.nedt.2021.104868. [DOI] [PubMed] [Google Scholar]
- 62.Wan W.H., Lam A.H.Y. The effectiveness of virtual reality-based simulation in health professions education relating to mental illness: A literature review. Health. 2019;11:646–660. doi: 10.4236/health.2019.116054. [DOI] [Google Scholar]
- 63.Tsai C.-F., Yeh S.-C., Huang Y., Wu Z., Cui J., Zheng L. The effect of augmented reality and virtual reality on inducing anxiety for exposure therapy: A comparison using heart rate variability. J. Healthc. Eng. 2018;2018:6357351. doi: 10.1155/2018/6357351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Geraets C.N., Van der Stouwe E.C., Pot-Kolder R., Veling W. Advances in immersive virtual reality interventions for mental disorders: A new reality? Curr. Opin. Psychol. 2021;41:40–45. doi: 10.1016/j.copsyc.2021.02.004. [DOI] [PubMed] [Google Scholar]
- 65.Bell I.H., Nicholas J., Alvarez-Jimenez M., Thompson A., Valmaggia L. Virtual reality as a clinical tool in mental health research and practice. Dialogues Clin. Neurosci. 2020;22:169. doi: 10.31887/DCNS.2020.22.2/lvalmaggia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Han S. An integrative review on augmented reality/virtual reality simulation programs in the mental health area for health professionals. Int. J. Contents. 2019;15:36–43. [Google Scholar]
- 67.Jones C., Jones D., Moro C. Use of virtual and augmented reality-based interventions in health education to improve dementia knowledge and attitudes: An integrative review. BMJ Open. 2021;11:e053616. doi: 10.1136/bmjopen-2021-053616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Herrera F., Bailenson J., Weisz E., Ogle E., Zaki J. Building long-term empathy: A large-scale comparison of traditional and virtual reality perspective-taking. PLoS ONE. 2018;13:e0204494. doi: 10.1371/journal.pone.0204494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pan X., Gillies M., Slater M. Virtual character personality influences participant attitudes and behavior–an interview with a virtual human character about her social anxiety. Front. Robot. AI. 2015;2:1. doi: 10.3389/frobt.2015.00001. [DOI] [Google Scholar]
- 70.Hoppe M., Baumann A., Tamunjoh P.C., Machulla T.-K., Woźniak P.W., Schmidt A., Welsch R. There Is No First- or Third-Person View in Virtual Reality: Understanding the Perspective Continuum; Proceedings of the CHI Conference on Human Factors in Computing Systems; New Orleans, LA, USA. 30 April–5 May 2022; pp. 1–13. [Google Scholar]
- 71.McCall C., Singer T. Understanding other Minds: Perspectives from Developmental Social Neuroscience. Oxford University Press; Oxford, UK: 2013. Empathy and the brain; pp. 194–209. [Google Scholar]
- 72.Ventura S., Badenes-Ribera L., Herrero R., Cebolla A., Galiana L., Baños R. Virtual reality as a medium to elicit empathy: A meta-analysis. Cyberpsychology Behav. Soc. Netw. 2020;23:667–676. doi: 10.1089/cyber.2019.0681. [DOI] [PubMed] [Google Scholar]
- 73.Dyer E., Swartzlander B.J., Gugliucci M.R. Using virtual reality in medical education to teach empathy. J. Med. Libr. Assoc. JMLA. 2018;106:498. doi: 10.5195/jmla.2018.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang Z., Sun K., Jatchavala C., Koh J., Chia Y., Bose J., Li Z., Tan W., Wang S., Chu W. Overview of stigma against psychiatric illnesses and advancements of anti-stigma activities in six Asian societies. Int. J. Environ. Res. Public Health. 2020;17:280. doi: 10.3390/ijerph17010280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gunasekaran S., Tan G.T.H., Shahwan S., Goh C.M.J., Ong W.J., Subramaniam M. The perspectives of healthcare professionals in mental health settings on stigma and recovery—A qualitative inquiry. BMC Health Serv. Res. 2022;22:1–16. doi: 10.1186/s12913-022-08248-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Martingano A.J., Hererra F., Konrath S. Virtual reality improves emotional but not cognitive empathy: A meta-analysis. Technol. Mind Behav. 2021;2:1–15. doi: 10.1037/tmb0000034. [DOI] [Google Scholar]
- 77.Ando S., Clement S., Barley E.A., Thornicroft G. The simulation of hallucinations to reduce the stigma of schizophrenia: A systematic review. Schizophr. Res. 2011;133:8–16. doi: 10.1016/j.schres.2011.09.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.