Abstract
Nanotechnology takes the lead in providing new therapeutic options for cancer patients. In the last decades, lipid-based nanoparticles—solid lipid nanoparticles (SLNs), nanostructured lipid carriers (NLCs), liposomes, and lipid–polymer hybrid nanoparticles—have received particular interest in anticancer drug delivery to solid tumors. To improve selectivity for target cells and, thus, therapeutic efficacy, lipid nanoparticles have been functionalized with antibodies that bind to receptors overexpressed in angiogenic endothelial cells or cancer cells. Most papers dealing with the preclinical results of antibody-conjugated nanoparticles claim low systemic toxicity and effective tumor inhibition, which have not been successfully translated into clinical use yet. This review aims to summarize the current “state-of-the-art” in anticancer drug delivery using antibody-functionalized lipid-based nanoparticles. It includes an update on promising candidates that entered clinical trials and some explanations for low translation success.
Keywords: cancer, active targeting, functionalization, antibodies, lipid nanoparticles, SLN, NLC, liposomes, antibody-conjugated nanoparticles
1. Introduction
Chemotherapy, whether alone or combined with other therapies, is the norm for cancer treatment. However, the widespread push to develop nanotechnology-based drug delivery systems comes from the need to overcome the limitations of systemically administered chemotherapeutics, namely short blood circulation time, non-specific distribution in the body, and the development of drug resistance. The size, shape, and surface of nanoparticles can be tailored to escape immediate clearance and enable an efficient delivery to the tumor site [1].
In contrast to normal tissues and organs, many solid tumors have leaky vasculature, along with defective lymphatic drainage, which facilitates the passive accumulation of nanoparticles (100–400 nm in diameter) in the tumor interstitium by the enhanced permeability and retention (EPR) effect [2].
Although passive targeting still occurs initially, active targeting is envisioned as the most promising strategy for improving binding affinity and specificity for tumor cells. For that, the nanoparticle surface can be modified with ligands that bind to receptors overexpressed in angiogenic endothelial cells or cancer cells [3]. In the case of targeting tumor vasculature or certain hematological malignancies, achieving sufficient binding affinity for endothelial cells is critical due to the hemodynamics that nanoparticles experience. Typically, active targeting involves the conjugation of nanoparticles to one or more targeting moieties that interact specifically with receptors that are either uniquely expressed or overexpressed in the tumor compared to normal tissues. If internalizing receptors are targeted, the ligand facilitates the transport of nanoparticles into the cells through a specific pathway once they reach the tumor [4]. For intracellular drug delivery, nanoparticles should be internalized quickly via receptor-mediated endocytosis after specific ligand–receptor interaction. The ability of such actively targeted nanoparticles to bypass drug efflux pumps alleviates the emergence of multidrug resistance [5]. Instead, nanoparticles targeting non-internalizing receptors will remain attached to the target cell surface and release the drug outside, which may also kill nearby cancer cells by the “bystander effect” [6].
In this review, we provide a brief overview of nanoparticle functionalization with antibodies, focusing on the use of these targeting ligands and the most common coupling strategies. Then the current “state-of-the-art” in anticancer drug delivery using antibody-functionalized lipid-based nanoparticles is summarized, including an update on candidates that have entered the clinical testing phase.
2. Functionalizing Nanoparticles with Antibodies
The repertoire of ligands conjugated to tumor-targeted nanoparticles is greatly expanded (e.g., antibodies, aptamers, peptides, polysaccharides, and small molecules, such as folate). Among them, antibodies, also known as immunoglobulins (Ig), have gained considerable popularity because of their unique in vivo properties and high specificity [7].
Within the five classes of immunoglobulins (IgG, IgA, IgM, IgD, and IgE) distinguished by the type of heavy chain, IgG is the most abundant in human serum [8]. The IgG molecule is a heterodimeric protein composed of two light (L) chains and two heavy (H) chains. Whereas the light chain consists of one N-terminal variable (VL) domain and one C-terminal constant (CL) domain, each heavy chain contains one variable (VH) and three constant (CH1, CH2, and CH3) domains. The IgG Y-shaped structure can be divided into two fragments connected by a very flexible hinge region: the antigen-binding fragment (Fab) region, corresponding to the two arms of the antibody molecule, and the fragment crystallizable (Fc) region, referring to its stem region. The N-terminal ends of the light and heavy chains collectively form the antigen-binding site, where a total of six hypervariable amino acid sequences termed “complementary determining regions” reside [9,10]. Several functional groups on the amino acids of antibodies can participate in conjugation, namely amino (N-terminal or lysine side chain), sulfhydryl (cysteines in the hinge region), and carboxyl (C-terminal or aspartic and glutamic acids side chain). Additionally, carbohydrate residues in the CH2 domains can be reactive after the periodate oxidation of cis-diols to aldehydes [11].
Considering the hydrodynamic radius of the antibody (~20 nm), the size of the functionalized nanoparticle is expected to increase up to 40 nm in proportion to the number of ligands [12]. Since smaller particles allow for deeper penetration into the tumor, antibody fragments (e.g., antigen-binding fragments and single-chain variable fragments) offer a clear advantage over the whole antibody. The primary way to produce an antigen-binding fragment (Fab) is antibody cleavage using proteases, such as papain for monovalent Fab fragments or pepsin for F(ab)2 fragments, in which the two arms remain linked. The F(ab)2 dimer may then be reduced to yield two Fab’ fragments with C-terminal sulfhydryl groups [13]. Alternatively, the VH and VL domains coupled by a flexible and short peptide linker make up the single-chain variable fragment (scFv), commonly obtained by phage display or cloning from mouse hybridoma [14].
To improve physicochemical properties and tumor-targeting accuracy, surface conjugation of functional groups or biomolecules to nanoparticles—also called functionalization—is being extensively studied.
The chemistry behind functionalization with antibodies includes adsorption, covalent conjugation (carbodiimide, maleimide, and “click” chemistries), and avidin–biotin interaction and was reviewed in detail by Marques et al. [15]. It is established that the coupling method should ensure a stable bond and allow for control of the ligand density. Ideally, the Fc region would be attached to the nanoparticle surface, leaving the Fab region oriented in such a way that interaction with the antigen is possible [16]. Although adsorption (i.e., physical adsorption and ionic binding) is the simplest and less time-consuming technique, covalent bonds outperform hydrophobic and electrostatic interactions in terms of stability and reproducibility. As such, carbodiimide and maleimide chemistries persist across the literature, as they benefit from easy-to-follow protocols and acceptable conjugation efficiency at a relatively low cost. In the case of nanoparticles containing surface carboxyl groups, these groups are activated by using 1-ethyl-3-(-3-dimethylaminopropyl) carbodiimide (EDC) and N-hydroxysuccinimide (NHS) before reacting with the primary amines of antibodies. However, other coupling strategies that result in oriented immobilization are preferred. More precisely, site-specific free sulfhydryl groups that are generated by antibody reduction or thiolation in the Fc region can be conjugated to the maleimide-activated amino groups of the nanoparticle, yielding a thioether linkage. Another option is based on the non-covalent, albeit very strong, interaction between strept(avidin)-coated nanoparticles and Fc-specific biotinylated antibodies. Even so, compared to direct covalent coupling, the final avidin–biotin complex requires an expensive multistep protocol with less efficient antibody binding, as observed by Wartlick et al. [17].
3. Antibody-Functionalized Lipid Nanoparticles for Anticancer Drug Delivery
Particles within the size range of 10 to 1000 nm are defined as nanoparticles. Therapeutic agents (i.e., drugs, proteins, and genetic material) can also be adsorbed or chemically conjugated to the nanoparticle surface, but those that are dissolved, entrapped, or encapsulated into the nanoparticle will benefit from enhanced chemical stability and protection against degradation [18]. Another distinctive feature of nanoparticles is the large surface area/volume ratio compared to bulk materials upon reduction of particle size to the nanoscale [19]. In view of a highly customizable surface, nanoparticles can be modified to avoid major obstacles to successful delivery. For instance, as surface coating with polyethylene glycol (PEG) imparts “stealth” properties to the nanoparticles, PEGylation is a common approach to decrease immunogenicity and safeguard against the mononuclear phagocyte system [20]. Furthermore, to improve the delivery efficiency of nanoparticles, attention has been paid to conjugation with targeting ligands that bind to receptors overexpressed in the target tissues or cells.
Nanoparticles can be made of a variety of materials, namely polymers, lipids, and metals. Moreover, nano-antioxidants have been designed to overcome the oxidative degradation of organic and inorganic materials by slowing the overall rate of autoxidation [21]. Nevertheless, since the first clinical approval of Doxil® in 1995, lipid-based nanoparticles remain the most prevalent class (33%) among nanomedicines on the market or under clinical trials [22]. In addition to AIDS-related Kaposi’s sarcoma (1995), this doxorubicin (DOX)-loaded PEGylated liposome (Doxil®) was FDA-approved in recurrent ovarian cancer (1998), metastatic breast cancer (2003), and multiple myeloma (2007) [23]; hence, it was a real breakthrough in cancer nanomedicine and lipid-based drug delivery systems.
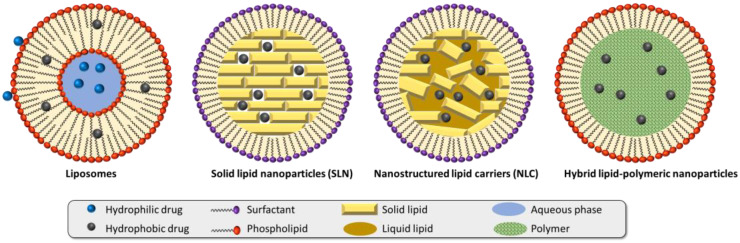
Lipid-based nanoparticles include liposomes, solid lipid nanoparticles (SLNs), nanostructured lipid carriers (NLCs), and hybrid lipid–polymeric nanoparticles (Figure 1).
Figure 1.
Different types of lipid nanoparticles. Adapted with permission from [24]. Copyright 2022, John Wiley & Sons.
As drug delivery systems, lipid nanoparticles usually consist of hydrophilic or hydrophobic drug(s), lipids generally recognized as safe (GRAS), and surfactant(s) to form and stabilize the dispersion. Low toxicity potential, ease of preparation with limited use of organic solvents, and feasibility of scale-up production give them an edge over polymer and inorganic nanoparticles [24,25].
Regarding the development of actively targeted lipid nanoparticles, two general strategies exist: (i) one-pot assembly of lipids and targeting ligands and (ii) post-insertion of targeting ligands into preformed lipid nanoparticles. Still, the former is likely to cause the targeting ligands to be encapsulated or oriented to the nanoparticle core, making them inaccessible for receptor interaction [26]. Therefore, it comes as no surprise that post-insertion functionalization is preferred. In most cases, lipid nanoparticles are preformed by mixing structural lipids with PEG–lipids (e.g., 1,2-distearoyl-sn-glycero-3-phosphoethanolamine–polyethylene glycol, abbreviated to DSPE–PEG) containing different terminal groups, such as amino, carboxyl, maleimide, or NHS (e.g., DSPE–PEG–NH2, DSPE–PEG–COOH, DSPE–PEG–maleimide, DSPE–PEG–NHS, etc.), followed by modification with antibodies. Few examples of physical coating and streptavidin–biotin interaction can be found in antibody-functionalized drug-loaded lipid nanoparticles. While antibody fragments have been used occasionally, monoclonal antibodies (mAbs) are still at the forefront of antibody ligands. In 1975, hybridoma technology enabled the large-scale production of mAbs, which are antibodies against a single portion (epitope) of a specific antigen. To address clinical efficacy and safety issues, mAbs evolved from murine (suffix-omab) to chimeric (-ximab), humanized (-zumab), and, later, human (-umab). Whereas chimeric mAbs combine murine variable domains and human constant domains, in humanized mAbs, only CDRs are of non-human origin [27].
The utilization of antibody-conjugated lipid nanoparticles in anticancer drug delivery is discussed below, with several examples organized by nanoparticle type.
3.1. Antibody-Functionalized SLN
The lipids used to produce SLN are solid at both room temperature and human body temperature [28].
In 2011, the development of cationic SLN functionalized with a monoclonal antibody (mAb) directed against the epidermal growth factor receptor (EGFR) represented the first step in antibody-mediated strategies using drug-loaded SLN in cancer therapy. By using the microemulsion technique and EDC/NHS, Kuo and Liang fabricated anti-EGFR mAb-grafted cationic SLN encapsulating carmustine [29] and DOX [30] to target and inhibit the propagation of glioblastoma (GBM). When the concentration of cationic surfactants was 1 mM, the authors achieved the smallest particle size and maximal entrapment efficiency. Moreover, a high percentage of cacao butter in the lipid phase led to enhanced viability of human brain microvascular endothelial cells (HBMECs). Evidence from studies in EGFR-overexpressing U-87 MG glioma cells supported the antiproliferative effects of the targeted SLN, as well as the significance of surface anti-EGFR mAb for efficient drug delivery. Given that melanotransferrin (MTf) is found on HBMEC and U-87 MG cells, Kuo et al. [31] conjugated similar SLN with MTf antibody to deliver etoposide (ETP) across the blood–brain barrier for GBM therapy. Based on cell viability and Transwell assays, it is apparent that MTf antibody-conjugated ETP-loaded SLN had tolerable toxicity to HBMEC and human astrocytes, along with augmented transcytosis and growth inhibition of U-87 MG cells. As the design considerations become more complex, dual-targeted approaches for ETP delivery to GBM make the scene. More precisely, SLN contains two targeting ligands: MTf antibody plus tamoxifen to extend drug residence time within the brain parenchyma [32]; and anti-EGFR mAb and 83-14 mAb that bind strongly to the human insulin receptor on HBMEC prior to receptor-mediated endocytosis and subsequent brain delivery [33].
In another work, Kim et al. [34] performed studies in preclinical mouse models of lung or breast cancer, using paclitaxel (PTX)-containing low-density lipoprotein-mimicking SLN bearing the tumor-targeting antibodies cetuximab (CTX) or trastuzumab (TZM). The antitumor activity of these targeted SLN has exceeded that of the commercial formulations of PTX (Taxol® and Genexol-PM), emphasizing the convenience of using nanocarriers and further adding targeting moieties to their surface. Together with the targeting ability, the antibody ligand may also have synergistic antitumor effects with the encapsulated drug. A case in point is the synergistic activity of the encapsulated oxaliplatin and tumor-necrosis-factor-related apoptosis-inducing ligand (TRAIL) mAb via SLN that elicited a 1.5-fold increase in cytotoxicity in HT-29 (colorectal cancer) cells compared to the free drug [35].
To improve internalization in breast cancer cells, Souto et al. [36] explored the streptavidin–biotin interaction to link cationic SLN with CAB51, a compact antibody against the human epidermal growth factor receptor 2 (HER2). The results showing that the targeting moiety enhanced cellular uptake in HER2-overexpressing BT-474 breast cancer cells inspired this author to adopt the same coupling strategy to engineer anti-HER2 CB11-modified cationic SLN for site-specific delivery of perillaldehyde 1,2-epoxide [37].
Triple-negative breast cancer (TNBC) is the most aggressive breast cancer subtype, accounting for approximately 10–15% of all cases. Attempts to cure TNBC are often frustrated by the lack of expression of estrogen, progesterone, and HER2 receptors. Some researchers sought to address this issue by functionalizing drug-loaded SLN with antibodies against receptors overexpressed in TNBC cells: exon v6-containing cluster of differentiation 44 isoform (CD44v6) [38], receptor for advanced glycation end-products (RAGE) [39], and death receptor 5 (DR5) [40]. Cavaco et al. [38] decorated PTX entrapped in SLN (SLNPTX) with polyethylene glycol-phosphatidylethanolamine and expected its hydroxyl groups to bind to the N-terminal amino groups of anti-CD44v6 mAb. Differences in MDA-MB-436 cell viability between the free drug and SLNPTX can be attributed to the ability of nanoparticles to evade drug efflux transporters, thus promoting an increase in intracellular accumulation of PTX. However, the attached antibody failed to ameliorate the therapeutic efficacy of PTX compared to SLNPTX–PEG, thereby suggesting limitations in receptor-mediated endocytosis. By contrast, the internalization and cytotoxic effect of diallyl disulfide were significantly improved with an anti-RAGE antibody as the targeting ligand [39]. Additionally, an increase in cell death was observed following the treatment of MDA-MB-231 cells with anti-DR5 mAb-conjugated SLN of gamma-secretase inhibitor, which aligns with higher tumor regression in a breast cancer mouse model compared to non-targeted SLN or the free drug given intravenously (10 mg/kg) twice a week for four weeks [40]. Building upon the success of these in vitro and in vivo studies, Kumari et al. [41] hypothesized that introducing a second ligand, such as delta-like ligand 4 (DLL4) mAb, into this nanosystem would allow for the precise delivery to TNBC, reduction of side effects, and synergistic benefits.
A summary of these research papers is given in Table 1.
Table 1.
Antibody-functionalized SLN for anticancer drug delivery.
| Lipids | Drug | Ligands | Coupling Method | Cancer Cell (In Vitro) | Cancer (In Vivo) | Ref. |
|---|---|---|---|---|---|---|
| Cacao butter, SA DSPE–PEG2000–COOH |
Carmustine | EGFR mAb | Carbodiimide | U-87 MG (glioblastoma) |
. | [29] |
| Cacao butter, SA DSPE–PEG2000–COOH |
Doxorubicin | EGFR mAb | Carbodiimide | U-87 MG (glioblastoma) |
- | [30] |
| Tripalmitin, cacao butter Cardiolipin, DSPE–PEG2000–COOH |
Etoposide | MTf Ab | Carbodiimide | U-87 MG (glioblastoma) |
- | [31] |
| Compritol® 888 ATO, tripalmitin, Ch, SA, DSPE–PEG2000–COOH |
Etoposide | MTf Ab Tamoxifen |
Carbodiimide | U-87 MG (glioblastoma) |
- | [32] |
| Compritol® 888 ATO, tripalmitin Stearic acid, DSPE–PEG2000–COOH |
Etoposide | EGFR mAb 83-14 mAb |
Carbodiimide | U-87 MG (glioblastoma) |
- | [33] |
| Cholesteryl oleate, triolein Ch, DOPE, DC-cholesterol |
Paclitaxel | Cetuximab Trastuzumab |
Maleimide | NCI-H1975, NCI-H1650 NCI-H520, PC9, SK-BR-3 |
Lung Breast |
[34] |
| SA | Oxaliplatin | TRAIL mAb | Carbodiimide | HT-29 (colorectal) | - | [35] |
| Compritol® 888 ATO | - | CAB51 | Streptavidin-biotin | MCF-7, BT-474 (breast) | - | [36] |
| Compritol® 888 ATO | Perillaldehyde 1,2-epoxide |
CB11 | Streptavidin-biotin | MCF-7 (breast) | - | [37] |
| Precirol® ATO 5, PEG–PE | Paclitaxel | CD44v6 mAb | Hydroxyl-amino | MDA-MB-436 (TNBC) | - | [38] |
| Palmitic acid | Diallyl disulfide | RAGE Ab | Carbodiimide | MDA-MB-231 (TNBC) |
- | [39] |
| SA | DAPT | DR5 mAb | Carbodiimide | MDA-MB-231 | Breast | [40] |
CD44v6, CD44 variant 6; Ch, cholesterol; DAPT, N-[N-(3,5-difluorophenacetyl)-L-alanyl]-S-phenylglycine t-butyl ester; DC-cholesterol, 3β-[N-(N′,N′-dimethylaminutesoethane)-carbamoyl] cholesterol hydrochloride; DOPE, 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine; DR5, death receptor 5; DSPE, 1,2-distearoyl-sn-glycero-3-phosphoethanolamine; EGFR, epidermal growth factor receptor; HER2, human epidermal growth factor receptor 2; MTf, melanotransferrin; PEG, polyethylene glycol; PEG–PE, polyethylene glycol–phosphatidylethanolamine; RAGE, receptor for advanced glycation end-products; SA, stearic acid; TNBC, triple-negative breast cancer; TRAIL, tumor-necrosis-factor-related apoptosis-inducing ligand.
3.2. Antibody-Functionalized NLC
By including liquid lipids, NLC were endowed with great advantages over SLN, namely improved stability and high drug loading with minimal drug leakage during storage, arising from a less ordered crystalline structure [42].
The application of antibody-functionalized NLC in cancer chemotherapy has been somewhat scarce. Still, the recent literature contains some examples described in this section and listed in Table 2.
Table 2.
Antibody-functionalized NLC for anticancer drug delivery.
| Lipids | Drug | Ligands | Coupling Method | Cancer Cell (In Vitro) | Cancer (In Vivo) | Ref. |
|---|---|---|---|---|---|---|
| SA Glyceryl monostearate Middle chain triglycerides DSPE–PEG–NH2 |
Docetaxel | Flk-1(A-3) mAb | BS3 crosslinker | HepG2 (HCC) A549 (lung) B16 (melanoma) |
Melanoma | [43] |
| SA Oleic acid DSPE–PEG2000–NHS |
Doxorubicin | EGFRvIII mAb | Amine-reactive crosslinker |
HC2 20d2/c | - | [44] |
| Cholesterol Castor oil SA Fatty amines NHS–PEG3K–maleimide |
Docetaxel | Trastuzumab | Maleimide | MDA-MB-468 BT-474 (breast) |
- | [45] |
| Glyceryl monostearate or lecithin Oleic acid or Labrafac® |
Curcumin Imatinib |
Rituximab | Ionic adsorption | Jurkat and Ramos (lymphoma) |
- | [46] |
| Oleic acid Compritol® 888 ATO Soybean phosphatidylcholine DSPE–PEG–maleimide |
Paclitaxel 5-Demethylnobiletin |
Cetuximab | Maleimide | A549 | Lung | [47] |
| Glycerin monostearate Soybean oil |
Irinotecan prodrug Quercetin | Conatumumab | Carbodiimide | HT-29 | Colorectal | [48] |
| DSPE–PEG2000–maleimide Caprylic/capric triglyceride PEG–40 hydrogenated castor oil |
Docetaxel | Bevacizumab | Maleimide | U-87 MG A172 |
Glioblastoma | [49] |
BS3, bis(sulfosuccinimidyl)suberate; DSPE, 1,2-distearoyl-sn-glycero-3-phosphoethanolamine; EGFR, epidermal growth factor receptor; HCC, hepatocellular carcinoma; mAb, monoclonal antibody; NHS, N-hydroxysuccinimide; PEG, polyethylene glycol; SA, stearic acid.
Taking advantage of vascular endothelial growth factor receptor 2 (VEGFR-2) overexpression in cancer cells and tumor neovasculature, Liu et al. [43] pioneered the “one-double targeting” strategy, meaning one ligand for double (tumor and vascular) targeting, with Flk-1(A-3) mAb. Due to the increased accumulation of docetaxel (DTX) in both tumor tissue and tumor vasculature, Flk-1 mAb-targeted DTX-loaded NLC showed better antitumor efficacy than non-targeted NLC and Duopafei® (free DTX) against three human (HepG2, A549, and B16) cell lines and one malignant melanoma mouse model (dosage of 20 mg/kg).
For the targeting ligand coupled to DOX-loaded NLC by a post-insertion technique, Abdolahpour et al. [44] prepared a mAb directed against EGFRvIII. While evaluating the potential of the targeted NLC to increase cellular uptake, the authors observed that the uptake percentage in HC2 20d2/c (EGFRvIII-transfected NIH-3T3) cells was higher than that of NIH-3T3 cells, indicating that this antibody can specifically target EGFRvIII-overexpressing cells.
After developing Herceptin® (TZM)-conjugated NLC containing DTX for HER2-positive breast cancer [45], Varshosaz et al. [46] employed rituximab to target CD20 receptors in lymphoma cells and selected the optimal NLC formulation co-loaded with curcumin and imatinib (a tyrosine kinase inhibitor). The optimal formulation containing lecithin and 25% of oleic acid was physically coated with a 20% rituximab solution, yielding an antibody coupling efficiency of 89 ± 0.15%. The treatment of Ramos (CD20-positive) B cells with the mixture of curcumin (15 µg/mL)/imatinib (5 µg/mL) (IC50 of 2.3 ± 0.1 µg/mL) and uncoated curcumin/imatinib-loaded NLC (IC50 of 2.9 ± 0.2 µg/mL) induced lower cytotoxicity than rituximab-coated curcumin/imatinib-loaded NLC with an IC50 of 1.4 µg/mL.
With the aim of attenuating off-target toxicity and overcoming resistance to monotherapy, NLC carrier systems and drug combination have garnered some interest in recent years. For instance, Guo et al. [47] highlighted synergistic combination therapy in lung cancer by preparing CTX-functionalized NLC co-encapsulating PTX and 5-demethylnobiletin. The presence of CTX resulted in the highest drug accumulation in the tumor tissue and the most remarkable tumor-growth inhibition from 1010.23 to 211.18 mm3 at the end of the study in PTX-resistant-lung-cancer-bearing mice. Upon intravenous (i.v.) injection every three days into mice bearing colorectal cancer xenografts, Liu et al. [48] verified a reduction of tumor growth without systemic toxicity through the decoration of NLC co-delivering irinotecan prodrug (2 mg/kg) and quercetin (2 mg/kg) with conatumumab/AMG 655 (anti-DR5 mAb).
Very recently, DTX-loaded NLC containing DSPE–PEG2000–maleimide was successfully coupled to thiolated bevacizumab (BVZ). The fabricated nanoformulation (BVZ-NLC-DTX) selectively induced cell death by apoptosis in vascular endothelial growth factor (VEGF)-overexpressing GBM cells (U-87 MG and A172), but not in peripheral blood mononuclear cells. Unlike free DTX (5 mg/kg, i.v.), BVZ-NLC-DTX (5 mg/kg, i.v.) was able to reduce up to 70% of tumor volume after a 15-day treatment in an orthotopic C6 glioma rat model [49].
3.3. Antibody-Functionalized Liposomes
Liposomes are a subtype of lipid-based nanoparticles mainly composed of phospholipids, which are amphiphilic molecules containing a hydrophilic head and a hydrophobic tail [50]. Although SLN and NLC were introduced as an alternative due to stability problems, liposomes are still the carrier of choice for many researchers with the goal of treating cancer with antibody-conjugated drug-loaded nanoparticles.
Targeted cancer therapies using antibody-functionalized liposomes are divided into angiogenesis-associated targeting, uncontrolled cell-proliferation targeting, and tumor-cell targeting that can be seen in subsequent sections.
3.3.1. Angiogenesis-Associated Targeting
Angiogenesis is one of the hallmarks of cancer, as it allows the tumor to receive enough oxygen and nutrients to thrive [51]. In this strategy, liposomes encapsulating anticancer drugs are conjugated to antibodies that bind to receptors overexpressed in angiogenic endothelial cells, thus capitalizing on both antiangiogenic and cytotoxic effects to improve therapeutic efficacy. The suppression of blood-vessel growth within the tumor and normalization of tumor vasculature are the key mechanisms that underpin the antiangiogenic contribution to cancer cell killing [52]. To date, the angiogenic targets of antibody-functionalized liposomes for cancer therapy have been VEGF and its receptors, as well as matrix metalloproteinases.
Considering the prevalence of VEGF and VEGFR-2 in tumor cells and endothelium, as well as the low level of VEGF-induced endocytosis of VEGFR-2 in normal cells compared to tumor cells, it is possible to achieve efficient targeted delivery of nanoparticles to VEGF- and VEGFR-2-positive tumors. One prominent approach to angiogenesis-based targeting via VEGF/VEGFR-2 system involves targeting VEGF to inhibit its binding to VEGFR-2. Kuesters and Campbell [53] described the modification of PEGylated cationic liposomes with BVZ (anti-VEGF mAb) through the addition of neutravidin and biotinylated BVZ. From the experiments with human pancreatic cancer (Capan-1, HPAF-II, and PANC-1) and endothelial (MS1-VEGF and HMEC-1) cell lines, it became evident that BVZ increases or maintains the uptake of liposomes in the presence of VEGF but hinders non-specific cellular uptake when VEGF is absent. Recently, anti-VEGF mAb-conjugated PEGylated pH-sensitive liposomes were developed to augment the therapeutic efficacy of DTX in breast cancer while minimizing its side effects [54]. This nanosystem was a vast improvement over the marketed formulation Taxotere®, which showed a higher percentage of tumor burden of ~75% (vs. ~35%) in breast-tumor-bearing rats receiving a single dose equivalent to 2 mg/kg of free DTX. Additionally, Shein et al. [55] offered the first insight into the active targeting of liposomes to the brain tumor, using a mAb directed against VEGF. These targeted liposomes were then worked up into a more sophisticated liposomal formulation of cisplatin by coupling thiolated mAbs directed against VEGF and VEGFR-2 via maleimide chemistry [56]. Summarizing the in vitro data, the targeting moieties facilitated the uptake of the targeted liposomes in C6 and U-87 MG glioma cells, known for high VEGF and VEGFR-2 expression, leading to higher cytotoxicity than non-targeted and non-specific IgG–liposomes.
Only one of the articles reviewed [57] reported the use of an antibody targeting the membrane type 1-matrix metalloproteinase (MT1-MMP), particularly a Fab’ fragment derived from an anti-human MT1-MMP mAb (222-1D8). Compared to unmodified liposomes, modification with Fab’222-1D8 did not alter the tumor accumulation of PEGylated liposomes but appeared to accelerate their uptake in MT1-MMP-positive HT1080 fibrosarcoma cells after reaching the tumor via the EPR effect. The in vivo results also proved the utility of DOX-loaded Fab’222 1D8-modified liposomes from the point of view of antitumor activity.
3.3.2. Uncontrolled Cell Proliferation Targeting
Here, drug-loaded liposomes are functionalized with antibodies directed against receptors involved in cancer-cell proliferation that are overexpressed in tumor cells, such as the human epidermal growth factor receptors and transferrin receptors. This strategy holds a particular promise for eradicating metastatic cells or small tumors that are devoid of new blood vessels.
To control the risk of idiosyncratic drug reactions and adverse reactions to afatinib combined with CTX, Lu et al. [58] developed liposomes loaded with that drug and coupled with CTX (IMC-C225 or Erbitux), a chimeric IgG1 mAb that binds to the extracellular domain of EGFR. In a non-small cell lung cancer (NSCLC) xenograft model with EGFR overexpression, those immunoliposomes showed a strongly enhanced ability for drug delivery and tumor growth inhibition.
Targetability to EGFR-overexpressing tumors can also be applied to stimuli-responsive nanocarriers. This is evidenced by sterically stabilized CTX-modified pH-responsive liposomes encapsulating gemcitabine (GEM) that were tested in A549 lung adenocarcinoma cells and NSCLC-bearing nude mice [59]. The apoptotic index in mice receiving the targeted liposomal formulation of GEM (160 mg/kg) was higher than that of other treatment groups and PBS-treated mice, and a good correlation between apoptosis and antitumor activity was found.
The absence of estrogen, progesterone and HER2 receptors has led to a concept of treating TNBC with EGFR-targeted liposomes carrying celecoxib [60], simvastatin [61], and PTX and piperine [62] with promising in vitro outcomes.
Following the functionalization of 5-fluorouracil (5-FU)-loaded liposomes with CTX, Petrilli et al. [63] investigated the influence of the administration route (topical or subcutaneous administration) on liposomal drug delivery in squamous cell carcinoma induced in immunosuppressed mice. According to the histological analysis, topical administration of 5-FU-loaded immunoliposomes using iontophoresis was more effective than subcutaneous injection in reducing cell proliferation and the remaining cells were less aggressive.
In another work [64], liposomes containing oxaliplatin were prepared and coupled via thioether linkage to whole CTX or Fab’ fragments derived from CTX. The site-directed conjugation to monovalent CTX-Fab’ fragments rendered liposomes with enhanced tumor accumulation (2916.0 ± 507.84 ng/g) compared to CTX (1546.02 ± 362.41 ng/g) or in the absence of targeting ligands (891.06 ± 155.1 ng/g), which also improved efficacy in mice inoculated with EGFR-positive colorectal cancer cells and treated with three i.v. 2.5 mg/kg doses at days 12, 15, and 18 post-cancer-cell implantation.
Eloy and colleagues [65] were the first to report on CTX-modified liposomes for the selective delivery of DTX to prostate cancer after preparing TZM-functionalized liposomes encapsulating rapamycin alone [66] or with PTX [67] to treat HER2-positive breast cancer. While TZM (anti-HER2 mAb) and rapamycin acted synergistically in SK-BR-3 cells, particularly via liposomes, the role of the antibody in mediating synergism between rapamycin and PTX was confirmed and attributed to improved cell uptake.
Also known as ErbB2 or CD340, HER2 regulates cell growth and proliferation and is one of the most used surface receptors to target liposomes for breast cancer and others, such as prostate cancer [68]. A growing number of therapeutic agents, namely bleomycin [69], DTX [70,71], curcumin and resveratrol [72], idarubicin [73], and epirubicin [74], have been proposed as payloads in breast cancer targeting, using TZM-conjugated liposomes. With liposomes linked to listeriolysin O and TZM, the amount of bleomycin needed to reduce tumor cell growth and viability is nearly 57,000-fold lower than the concentration required if the drug is administered extracellularly [69]. Based on the pharmacokinetic profile of TZM-coated vitamin E liposomes in male Sprague-Dawley rats, the half-life of DTX was 1.9 and 10 times longer than PEG-coated DTX-loaded vitamin E liposomes and a marketed formulation of DTX, respectively. Moreover, the area under the curve (97,740 ng.h/mL) was 3.47 times higher than that of DTX upon i.v. injection at an equivalent dose of 7 mg/kg [70]. Data from the in vivo distribution studies by Rodallec et al. [71] suggested that grafting TZM onto liposomes increases internalization rather than tumor localization. When compared to reference treatments (i.e., DTX + TZM or TZM emtansine), TZM-modified stealth liposomal DTX has greater efficacy in different breast cancer models (2D, 3D spheroids, and orthotopic xenograft mice). By coating liposomes with TZM, there was a dramatic increase in the antiproliferative effects of curcumin and resveratrol in HER2-overexpressing breast cancer cells [72]. The works by Amin et al. [73] and Khaleseh et al. [74] showed that such a drug delivery system could be a good choice for anthracyclines as well and provided a promising background for further in vivo studies.
The transferrin receptor (TfR) is another target for tumor-targeted delivery of liposomes using antibodies, of which OX26 mAb is the most representative ligand. By making use of the non-covalent (streptavidin–biotin) interaction, Schnyder et al. [75] described a new method of coupling biotinylated PEG–liposomes with streptavidin-linked OX26 mAb. The potential of biotinylated immunoliposomes to bypass P-glycoprotein (P-gp) in multidrug-resistant RBE4 brain capillary endothelial cells was manifested by a 2- to 3-fold enhancement in intracellular accumulation of daunomycin compared to the free drug. More recently, cisplatin-loaded PEGylated liposomes functionalized with OX26 mAb were found to be internalized in C6 cells more efficiently than non-functionalized liposomes, as well as having higher potency for enhanced therapeutic efficacy and less toxicity in brain-tumor-bearing Wistar rats [76]. In addition, Kim et al. [77] decorated cationic liposomes encapsulating temozolomide (TMZ) with an anti-TfR scFv to cross the blood–brain barrier and target GBM once in the brain parenchyma. The authors demonstrated that systemic administration of this novel formulation prolonged survival in mice bearing intracranial GBM. Furthermore, its improved efficacy in both TMZ-sensitive and TMZ-resistant tumors compared to standard TMZ was accompanied by a reduction in toxicity.
3.3.3. Tumor-Cell Targeting
Tumor-cell targeting involves many of the aforementioned targets, as well as others specific to the type of cancer.
Due to the lack of oxygen, carbonic anhydrase IX (CA IX) is overexpressed in 80% of NSCLC. Yang’s group conjugated anti-CA IX antibody to DSPE–PEG–maleimide in the preformed DTX-loaded liposomes via sulfhydryl-reactive crosslinker chemistry [78]. A fluorescence-based flow cytometry assay was carried out in A549 cells and revealed that the binding affinity of targeted liposomes was 1.65-fold higher than non-targeted liposomes in CA IX-positive NSCLC cells. Later, by restraining tumor growth and prolonging the median survival time of up to 90 days in an orthotopic mouse model, they revalidated this strategy to deliver triptolide to human NSCLC via the pulmonary route [79].
The consistent expression of disialoganglioside (GD2) antigen in neuroblastoma cells and its limited expression in normal tissues outside the central nervous system opened the possibility of using this target in the treatment of neuroblastoma. To illustrate, liposomal formulations decorated with an anti-GD2 antibody and loaded with etoposide [80] and sepantronium bromide (YM155) [81] have been produced.
Whilst initial efforts to eradicate melanoma lesions focused on eliminating CD20-positive melanoma cancer-initiating cells with CD20 antibody-conjugated vincristine-loaded liposomes [82], recent attention was directed towards the expression of melanoma antigen A1 [83] and the programmed death-ligand 1 (PD-L1) [84] in melanoma cells. Since PD-L1 expression has been detected in 50% of gastric cancer patients, this receptor is also a target candidate for nanoparticle internalization in gastric cancer cells. Accordingly, the overall goal of improving the co-delivery of PTX and tariquidar (P-gp inhibitor) to multidrug-resistant SGC7901/ADR xenograft tumors could be achieved with anti-PD-L1 mAb-conjugated liposomes [85].
Within the scope of combination therapy, synergistic effects have been observed in pancreatic cancer cells when GEM was co-encapsulated with PTX in liposomes functionalized with the antibody fragment [86].
To refine the therapeutic efficacy of Doxil® in hepatocellular carcinoma (HCC), Wang et al. [87] chose a post-insertion strategy to modify PEGylated liposomal DOX with the bivalent fragment HAb18 F(ab’)2 named Metuximab, which resulted in increased antitumor efficacy in CD147-overexpressing liver cancer cells and Huh-7 tumor xenografts. Concurrently, Lu et al. [88] constructed anti-CD44 antibody-modified liposomes to enhance the therapeutic index of timosaponin AIII in HCC. CD44 has also been recognized as a marker for cancer stem cells and is frequently expressed in several malignancies, including ovarian and colon cancers. As such, an anti-human CD44 mAb was employed to direct glycosylated PTX-loaded liposomes to CD44-positive ovarian cancer cells with great success [89].
Regarding colon cancer treatment, researchers proved the feasibility of coupling Doxil® with anti-CD44 mAb [90] and anti-CD133 mAb [91] and accomplished higher therapeutic efficacy compared to other treatments (non-targeted Doxil® and free DOX) against CD44-positive C-26 cells (in vitro and in vivo) and CD133-positive HT-29 cells, respectively. Based on preliminary findings [92], the progression of metastatic colorectal cancer could be haltered by 5-FU-loaded liposomes covalently linked to an antibody against the Frizzled 10 protein.
At the end of this subsection, Table 3 summarizes antibody-functionalized liposomes reported in papers from 2017 to 2022.
Table 3.
Antibody-functionalized liposomes for anticancer drug delivery.
| Lipids | Drug | Ligands | Coupling Method | Cancer Cell (In Vitro) | Cancer (In Vivo) | Ref. |
|---|---|---|---|---|---|---|
| Soya lecithin, Ch, DOPE CHEMS, DSPE–PEG–COOH |
Docetaxel | VEGF mAb | Carbodiimide | MCF-7 | Breast | [54] |
| HSPC, Ch, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Afatinib | Cetuximab | Maleimide | A549 H1975 |
NSCLC | [58] |
| HSPC, DSPC, Ch, DSPE–PEG DSPE–PEG–maleimide |
Simvastatin | Cetuximab | Maleimide | MDA-MB-231 | TNBC | [61] |
| HSPC, Ch (TPGS and TPGS–COOH) |
Paclitaxel Piperine |
Cetuximab | Carbodiimide | MDA-MB-231 (TNBC) | - | [62] |
| DSPC, Ch DSPE–PEG–maleimide |
5-Fluorouracil | Cetuximab | Maleimide | A431 B16F10 |
Squamous cell carcinoma | [63] |
| SPC, Ch, DSPE–PEG2000 DSPE–PEG–maleimide |
Docetaxel | Cetuximab | Maleimide | DU145 PC-3 (prostate) |
- | [65] |
| SPC, Ch, DSPE–PEG2000 DSPE–PEG–maleimide |
Rapamycin | Trastuzumab | Maleimide | MDA-MB-231 SK-BR-3 (breast) |
- | [66] |
| SPC, Ch, DSPE–PEG2000 DSPE–PEG–maleimide |
Rapamycin Paclitaxel |
Trastuzumab | Maleimide | 4T1 SK-BR-3 |
Breast | [67] |
| SPC, Ch DSPE–PEG2000–NHS |
Doxorubicin Simvastatin |
Trastuzumab | Amine-reactive crosslinker |
PC3 | Prostate | [68] |
| Phosphatidylcholine Phosphatidylglycerol Ch, maleimide–PEG |
Docetaxel | Trastuzumab | Maleimide | SK-BR-3 | Breast | [71] |
| SPC, Ch, DSPE–PEG DSPE–PEG–maleimide |
Idarubicin | Trastuzumab | Maleimide | MCF-7 SK-BR-3 (breast) |
- | [73] |
| DOPE, Ch | Epirubicin | Trastuzumab | Carbodiimide | MCF-7, MDA-MB-453 BT-20 (breast) |
- | [74] |
| Lecithin, Ch, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Cisplatin | OX26 mAb | Maleimide | C6 | Glioma | [76] |
| SPC, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Triptolide | CA IX Ab | Maleimide | A549 | NSCLC | [79] |
| DPPC, Ch, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Sepantronium bromide |
GD2 Ab | Maleimide | IMR32 KCNR |
Neuroblastoma | [81] |
| HSPC, Ch, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Doxorubicin | scFv G8 Hyb3 |
Maleimide | MZ2Mel43, G43 Mel2A, Mel78 |
Melanoma | [83] |
| HSPC, Ch, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Doxorubicin | PD-L1 mAb | Maleimide | B16-OVA | Melanoma | [84] |
| Egg phosphatidylcholine DOPE, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Paclitaxel Tariquidar |
PD-L1 mAb | Maleimide | SGC7901/ADR | Gastric | [85] |
| DPPC, Ch, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Paclitaxel | Ab fragment | Maleimide | BxPC3 (pancreatic) | - | [86] |
| DSPE–PEG2000–maleimide | Doxil® | Metuximab | Maleimide | Huh-7, HepG2 HCC 3736 |
HCC | [87] |
| DSPC, DSPE–PEG2000 DSPE–PEG2000–maleimide |
Timosaponin AIII | CD44 Ab | Maleimide | HepG2 | HCC | [88] |
| DPPC, Ch, mPEG–DSPE DSPE–PEG2000–maleimide |
Glycosylated paclitaxel | CD44 mAb | Maleimide | SK-OV-3, OVCAR-3 OVK18 |
Ovarian | [89] |
| mPEG2000–DSPE DSPE–PEG3400–NHS |
Doxil® | CD133 mAb | Amine-reactive crosslinker |
HT-29 (colorectal) | - | [91] |
| Ch, Phosphatidylcholine Stearylamine, DSPE–PEG2000 DSPE–PEG2000–COOH |
5-Fluorouracil | FZD10 Ab | Carbodiimide | CaCo-2 CoLo-205 (colorectal) |
- | [92] |
CA, carbonic anhydrase; CD, cluster of differentiation; Ch, cholesterol; CHEMS, cholesteryl hemisuccinate; DOPE, 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine; DPPC, 1,2-dipalmitoyl-sn-glycero-3-phosphocholine; DSPC, 1,2-distearoyl-sn-glycero-3-phosphocholine; DSPE, 1,2-distearoyl-sn-glycero-3-phosphoethanolamine; FZD10, frizzled 10 protein; GD2, disialoganglioside; HCC, hepatocellular carcinoma; HSPC, hydrogenated soy phosphatidylcholine; NHS, N-hydroxysuccinimide; NSCLC, non-small cell lung cancer; PD-L1, programmed death-ligand 1; PEG, polyethylene glycol; SPC, soy phosphatidylcholine; TNBC, triple-negative breast cancer; TPGS, PEGylated vitamin E succinate; VEGF, vascular endothelial growth factor.
3.3.4. Other Antibody-Functionalized Lipid-Based Nanoparticles
Another notable subset of lipid-based nanoparticles is commonly referred to as lipid–polymer hybrid (LPH) nanoparticles. These core–shell-type systems encompass attributes of lipids and polymers, as they consist of an inner lipid layer surrounding the polymer core that encapsulates the drug and an outer lipid–PEG layer, which prevents immune recognition and extends in vivo circulation time [93]. Since the outermost layer can be modified with different targeting ligands, such as antibodies, targeted cancer therapies using LPH nanoparticles (Table 4) are becoming increasingly popular.
Table 4.
Other antibody-functionalized lipid nanoparticles for anticancer drug delivery.
| Nanocarrier | Drug | Ligands | Coupling Method | Cancer Cell (In Vitro) | Cancer (In Vivo) | Ref. |
|---|---|---|---|---|---|---|
| Lipid–polymer hybrid NP | Paclitaxel | CEA half-Ab | Maleimide | BxPC-3 XPA-3 (pancreatic) |
- | [94] |
| Lipid–polymer hybrid NP | Adriamycin | EGFR Fab’ | Maleimide | SMMC-7721 HepG2 Huh7 |
HCC | [95] |
| Lipid–polymer hybrid NP | Salinomycin | CD44 Fab’ | Maleimide | DU145 22RV1 |
Prostate | [96] |
| Lipid–polymer hybrid NP | Cisplatin 5-Fluorouracil |
Trastuzumab | Carbodiimide | BE-3 | Esophageal | [97] |
| Lipid–polymer hybrid NP | Ara-C | CD33 mAb or Fab’ | Maleimide | HL-60 | AML | [98] |
| Lipid nanovesicles | - | EGFR mAb | Maleimide | DU145 (prostate) A431 (epidermoid carcinoma) |
- | [99] |
| Niosome | Daunorubicin | CD123 | Maleimide | NB4 THP-1 |
AML | [101] |
| Cubosome | Paclitaxel | EGFR 528 Fab’ | Maleimide | HEY | Ovarian | [102] |
AML, acute myeloid leukemia; Ara-C, 1-β-D-arabinofuranosylcytosine; CD, cluster of differentiation; CEA, carcinoembryonic antigen; EGFR, epidermal growth factor receptor; HCC, hepatocellular carcinoma; NP, nanoparticle.
The core of LPH nanoparticles usually comprises biodegradable polymers, such as polylactic-co-glycolic acid (PLGA). Hu et al. [94] conjugated LPH nanoparticles to a half-antibody against the carcinoembryonic antigen, overexpressed in 90% of pancreatic tumors. These authors confirmed the integrity of the PLGA core–lipid shell structure after internalization in BxPC-3 pancreatic cells, as well as the superior cytotoxicity of targeted PTX-loaded nanoparticles compared to non-targeted counterparts. In a therapeutic approach for HCC chemotherapy, a PLGA core containing adriamycin was covered by soybean lecithin/DSPE–PEG in the shell and further coated with anti-EGFR Fab’ [95]. More recently, Wei et al. [96] designed salinomycin-loaded PLGA-lipid nanoparticles linked to anti-CD44 Fab’ to eliminate prostate-cancer-initiating cells.
To achieve the targeted co-delivery of cisplatin and 5-FU to HER2-overexpressing esophageal adenocarcinoma, TZM was conjugated to the surface of LPH nanoparticles formulated by the unique combination of DSPE–PEG–COOH, soy phosphatidylcholine, and poly(ε-caprolactone) [97].
Compared to the whole antibody molecule, anti-CD33 Fab’-decorated LPH nanoparticles had longer circulation times in naïve mice and enabled higher levels of 1-β-D-arabinofuranosylcytosine in blood. Unfortunately, when it comes to prolonging the survival of leukemic mice, the incorporation of a pH-sensitive copolymer made of dioctadecyl, N-isopropyl acrylamide and methacrylic acid did not add any benefit to the formulation [98].
Differently, Leung et al. [99] reported the chemical conjugation of organic–inorganic hybrid nanovesicles to anti-EGFR mAbs, which retain the ability to bind to EGFR and inhibit A431 epidermoid carcinoma cell proliferation. It is noteworthy that the surface polysiloxane network makes these lipid nanovesicles more morphologically stable than conventional liposomes. Another alternative to liposomes are niosomes, that is to say, lipid nanovesicles based on non-ionic surfactants [100]. Anti-CD123 antibodies conjugated to maleimide–PEG2000–DSPE were incorporated into daunorubicin-loaded niosomes via a post-insertion technique for treating acute myeloid leukemia. The obtained niosomes were tested in NB4 and THP-1 cells and CD123-overexpressing leukemic mice, showing higher cytotoxicity and prolonged survival time [101].
Finally, Zhai and colleagues [102] proposed liquid-crystalline lipid carriers (i.e., cubosomes) as targeted delivery vehicles for PTX in aggressive ovarian cancer. By adding DSPE–PEG–maleimide to the formulation, it was possible to functionalize cubic-phase lipid nanoparticles with EGFR 528 Fab’. Still, this surface modification did not improve their performance either in vitro or in vivo compared to PTX-loaded cubosomes without the antibody.
3.4. Clinical Trials
Although the literature portrays a picture of potential therapeutic benefits and low systemic toxicity, the number of antibody-functionalized nanoparticles available to cancer patients is drastically below expectation, partially owing to a translational gap between preclinical and clinical studies. None of these nanoconjugates has been approved so far, but several candidates for the treatment of solid tumors have entered the clinical testing phase, including (i) anti-TfR scFv-modified liposomes carrying plasmid DNA (e.g., SGT-53 and SGT-94) [103,104]; (ii) a dendritic cell-targeted liposomal vaccine called Lipovaxin-MM [105]; (iii) bacterially derived mini- or nano-cells (EnGeneIC delivery vehicles or EDV) coupled to bispecific antibodies (e.g., Erbitux®EDVsPAC, EGFR(V)-EDV-Dox, and EEDVsMit) [106,107]; and (iv) antibody-directed liposomes encapsulating chemotherapeutic drugs (e.g., MM-310, MM-302, C225-ILs-Dox, and MCC-465) [108,109,110,111].
Whereas MM-310 is an anti-ephrin A2 scFv attached to liposome encapsulating a DTX prodrug, MM-302 and C225-ILs-dox stem from the modification of a liposomal formulation resembling Doxil® with post-inserted anti-HER scFv and CTX Fab’, respectively.
A study [112] using multiple tumor-xenografted mice was the basis for initiating a phase 1 clinical trial (NCT03076372) to assess the safety and efficacy of MM-310 in multiple solid tumors. Kamoun et al. [113] determined its preclinical efficacy in four ephrin A2-positive patient-derived xenograft models of bladder cancer, either as a monotherapy or in combination with GEM.
A phase 1 dose-escalation study (NCT01304797) evaluated the safety, tolerability, and pharmacokinetics of MM-302 as a monotherapy, in combination with TZM, or TZM plus cyclophosphamide in patients with advanced HER2-positive breast cancer. This study is now completed, and the recommended dose for a phase 2 study was MM-302 30 mg/m2 in combination with 6 mg/kg TZM every 3 weeks. In addition, Espelin et al. [114] demonstrated the synergistic antitumor activity of MM-302 combined with TZM in human xenograft models of breast and gastric cancer. This work provided the preclinical foundation for the HERMIONE clinical trial (NCT02213744) in anthracycline-naïve patients with locally advanced/metastatic HER2-positive breast cancer patients receiving MM-302 plus TZM versus the chemotherapy of physician’s choice (GEM, capecitabine, or vinorelbine) plus TZM. Unfortunately, in 2016, Merrimack Pharmaceuticals decided to halt further development of MM-302 due to negative outcomes. Later, in 2019, the observation of cumulative peripheral neuropathy in a phase 1 study precluded the possibility of continuing the development of MM-310.
After a phase 1 dose-escalation trial (NCT01702129) in advanced solid tumors, C225-ILs-Dox was clinically evaluated in patients with relapsed or refractory high-grade gliomas (NCT03603379). Although the delivery of C225-ILs-dox to glioblastoma tissue was demonstrated, no other definitive conclusions can be drawn from this trial, as there was no control group, and only a few patients were treated [115]. The DOX-loaded PEGylated immunoliposome termed MCC-465 utilizes the F(ab’)2 fragment of human GAH mAb as the targeting ligand, which positively reacts to over 90% of gastric cancer tissues but negatively to all normal tissues. A phase 1 study of MCC-465 conducted in patients with metastatic gastric cancer established the recommended dose of 32.5 mg/m2 for a phase 2 study with a 3-week schedule, but recent updates are missing [111].
4. Conclusions
As drug delivery systems, lipid-based nanoparticles offer many advantages, including biocompatibility, self-assembly, enhancement of drug solubility and bioavailability, high loading capacity, ease of production and modulation of drug release, cost-effectiveness, and feasibility of scale-up. Consequently, this type of nanocarrier has gained significant attention from researchers in both academia and industry over the past two to three decades. With the advances in bioconjugation and antibody engineering techniques, the development of antibody-functionalized lipid nanoparticles for anticancer drug delivery has been widespread, generating promising results in vitro and in small animal models. However, only a small number of these targeted nanomedicines have progressed into early clinical evaluation, and none has reached the market yet. Therefore, understanding the reasons for their underperformance in clinical settings is critical to guide future directions.
First, the physical characterization of nanoparticles deserves a robust strategy and suitable protocols, as it could help accelerate the shift from lab to industrial-scale production and anticipate their behavior in vivo [116]. In the quest for new knowledge regarding nanoparticle interactions with biological components, the use of different tools, such as computational analysis, mathematical modeling, and microfluidic platforms, should also be intensified.
Still, we must be aware that only a tiny fraction (less than 14 out of 1 million) of nanoparticles with an active targeting moiety can enter the solid tumor after intravenous injection [117], so it is convenient to consider local administration (e.g., intratumoral injection) whenever possible [118].
Many recent studies have simply outlined the toxic effects of nanoparticles, but only a few have systematically addressed their potentially adverse impact on mammalian target organs and after chronic exposure [119,120]. In addition to the assessment of bulk material safety, researchers should perform a thorough characterization of the nanoparticles, including analysis of batch-to-batch differences regarding consistency, stability, sterility and endotoxin quantification, blood contact properties, and in vivo cytotoxicity and immunotoxicology, to prevent toxicity-related clinical failure [121]. Accordingly, standardized guidelines to obtain nanotoxicological profiles should be implemented and followed to evaluate the potential risk in patients [122].
The discrepancy between preclinical and clinical observations is also explained by artificial rodent tumors that fail to mimic human tumors regarding transport and delivery. Accordingly, the development of in vivo models that closely reflect human cancer biology (e.g., high-fidelity patient-derived xenografts, humanized or genetically engineered mouse models, etc.) will certainly increase their predictive power.
Besides pathophysiological differences between animal model species and humans, heterogeneity amongst patients and tumor types or within the same patient over time, in terms of molecular and phenotypic features and the extent of the EPR effect, can also limit the clinical success of nanomedicines. Therefore, it is recommended to quantify the EPR effect in patient tumors to identify those who would benefit most from the treatment with therapeutic nanoparticles. Selecting the right patients is pivotal to the success of clinical trials, as well as finding the most suitable payload/combination regimen and trial size.
Despite the lack of translation progress, active targeting of nanoparticles remains an exciting research topic for cancer therapy, as antibody-conjugated lipid nanoparticles incorporating novel classes of therapeutics (e.g., RNA-based and gene editing therapeutics) other than cytotoxic drugs and kinase inhibitors are emerging. Looking to the future, one can expect more interdisciplinary research collaborations to open new avenues for the development of tumor-targeted lipid nanoparticle systems and, thus, hasten their clinical validation.
Author Contributions
Conceptualization, A.C.M.; writing—original draft preparation, A.C.M.; writing—review and editing, P.C.C., S.V. and M.H.A.; supervision, M.H.A. and P.C.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was financed by national funds from FCT—Fundação para a Ciência e a Tecnologia, I.P., in the scope of the project UIDP/04378/2020 and UIDB/04378/2020 of the Research Unit on Applied Molecular Biosciences—UCIBIO and the project LA/P/0140/2020 of the Associate Laboratory Institute for Health and Bioeconomy—i4HB. Ana Camila Marques gratefully acknowledges FCT for financial support (grant reference: 2020.06766.BD).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Steichen S.D., Caldorera-Moore M., Peppas N.A. A review of current nanoparticle and targeting moieties for the delivery of cancer therapeutics. Eur. J. Pharm. Sci. 2013;48:416–427. doi: 10.1016/j.ejps.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakamura Y., Mochida A., Choyke P.L., Kobayashi H. Nanodrug delivery: Is the enhanced permeability and retention effect sufficient for curing cancer? Bioconjug. Chem. 2016;27:2225–2238. doi: 10.1021/acs.bioconjchem.6b00437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Danhier F., Feron O., Préat V. To exploit the tumor microenvironment: Passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J. Control. Release. 2010;148:135–146. doi: 10.1016/j.jconrel.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 4.Pearce A.K., O’Reilly R.K. Insights into Active Targeting of Nanoparticles in Drug Delivery: Advances in Clinical Studies and Design Considerations for Cancer Nanomedicine. Bioconjug. Chem. 2019;30:2300–2311. doi: 10.1021/acs.bioconjchem.9b00456. [DOI] [PubMed] [Google Scholar]
- 5.Engelberg S., Modrejewski J., Walter J.G., Livney Y.D., Assaraf Y.G. Cancer cell-selective, clathrin-mediated endocytosis of aptamer decorated nanoparticles. Oncotarget. 2018;9:20993–21006. doi: 10.18632/oncotarget.24772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allen T.M. Ligand-targeted therapeutics in anticancer therapy. Nat. Rev. Cancer. 2002;2:750–763. doi: 10.1038/nrc903. [DOI] [PubMed] [Google Scholar]
- 7.Farahavar G., Abolmaali S.S., Gholijani N., Nejatollahi F. Antibody-guided nanomedicines as novel breakthrough therapeutic, diagnostic and theranostic tools. Biomater. Sci. 2019;7:4000–4016. doi: 10.1039/C9BM00931K. [DOI] [PubMed] [Google Scholar]
- 8.Vidarsson G., Dekkers G., Rispens T. IgG subclasses and allotypes: From structure to effector functions. Front. Immunol. 2014;5:520. doi: 10.3389/fimmu.2014.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feige M.J., Hendershot L.M., Buchner J. How antibodies fold. Trends Biochem. Sci. 2010;35:189–198. doi: 10.1016/j.tibs.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffman W., Lakkis F.G., Chalasani G. B cells, antibodies, and more. Clin. J. Am. Soc. Nephrol. 2016;11:137–154. doi: 10.2215/CJN.09430915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pietersz G.A., Wang X., Yap M.L., Lim B., Peter K. Therapeutic targeting in nanomedicine: The future lies in recombinant antibodies. Nanomedicine. 2017;12:1873–1889. doi: 10.2217/nnm-2017-0043. [DOI] [PubMed] [Google Scholar]
- 12.Gu F.X., Karnik R., Wang A.Z., Alexis F., Levy-Nissenbaum E., Hong S., Langer R.S., Farokhzad O.C. Targeted nanoparticles for cancer therapy. Nano Today. 2007;2:14–21. doi: 10.1016/S1748-0132(07)70083-X. [DOI] [Google Scholar]
- 13.Crivianu-Gaita V., Romaschin A., Thompson M. High efficiency reduction capability for the formation of Fab’ antibody fragments from F(ab)2 units. Biochem. Biophys. Rep. 2015;2:23–28. doi: 10.1016/j.bbrep.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khantasup K., Chantima W., Sangma C., Poomputsa K., Dharakul T. Design and Generation of Humanized Single-chain Fv Derived from Mouse Hybridoma for Potential Targeting Application. Monoclon. Antib. Immunodiagn. Immunother. 2015;34:404–417. doi: 10.1089/mab.2015.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marques A.C., Costa P.J., Velho S., Amaral M.H. Functionalizing nanoparticles with cancer-targeting antibodies: A comparison of strategies. J. Control. Release. 2020;320:180–200. doi: 10.1016/j.jconrel.2020.01.035. [DOI] [PubMed] [Google Scholar]
- 16.Cardoso M.M., Peca I.N., Roque A.C. Antibody-conjugated nanoparticles for therapeutic applications. Curr. Med. Chem. 2012;19:3103–3127. doi: 10.2174/092986712800784667. [DOI] [PubMed] [Google Scholar]
- 17.Wartlick H., Michaelis K., Balthasar S., Strebhardt K., Kreuter J., Langer K. Highly specific HER2-mediated cellular uptake of antibody-modified nanoparticles in tumour cells. J. Drug Target. 2004;12:461–471. doi: 10.1080/10611860400010697. [DOI] [PubMed] [Google Scholar]
- 18.Ioele G., Chieffallo M., Occhiuzzi M.A., De Luca M., Garofalo A., Ragno G., Grande F. Anticancer Drugs: Recent Strategies to Improve Stability Profile, Pharmacokinetic and Pharmacodynamic Properties. Molecules. 2022;27:5436. doi: 10.3390/molecules27175436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y., Li M., Gao X., Chen Y., Liu T. Nanotechnology in cancer diagnosis: Progress, challenges and opportunities. J. Hematol. Oncol. 2019;12:137. doi: 10.1186/s13045-019-0833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suk J.S., Xu Q., Kim N., Hanes J., Ensign L.M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016;99:28–51. doi: 10.1016/j.addr.2015.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Valgimigli L., Baschieri A., Amorati R. Antioxidant activity of nanomaterials. J. Mater. Chem. B. 2018;6:2036–2051. doi: 10.1039/C8TB00107C. [DOI] [PubMed] [Google Scholar]
- 22.Shan X., Gong X., Li J., Wen J., Li Y., Zhang Z. Current approaches of nanomedicines in the market and various stage of clinical translation. Acta Pharm. Sin. B. 2022;12:3028–3048. doi: 10.1016/j.apsb.2022.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barenholz Y. Doxil®—The first FDA-approved nano-drug: Lessons learned. J. Control. Release. 2012;160:117–134. doi: 10.1016/j.jconrel.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 24.Xu L., Wang X., Liu Y., Yang G., Falconer R.J., Zhao C.-X. Lipid Nanoparticles for Drug Delivery. Adv. NanoBiomed Res. 2022;2:2100109. doi: 10.1002/anbr.202100109. [DOI] [Google Scholar]
- 25.Chaudhuri A., Kumar D.N., Shaik R.A., Eid B.G., Abdel-Naim A.B., Md S., Ahmad A., Agrawal A.K. Lipid-Based Nanoparticles as a Pivotal Delivery Approach in Triple Negative Breast Cancer (TNBC) Therapy. Int. J. Mol. Sci. 2022;23:10068. doi: 10.3390/ijms231710068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menon I., Zaroudi M., Zhang Y., Aisenbrey E., Hui L. Fabrication of active targeting lipid nanoparticles: Challenges and perspectives. Mater. Today Adv. 2022;16:100299. doi: 10.1016/j.mtadv.2022.100299. [DOI] [Google Scholar]
- 27.Bernett M.J., Karki S., Moore G.L., Leung I.W., Chen H., Pong E., Nguyen D.H., Jacinto J., Zalevsky J., Muchhal U.S., et al. Engineering fully human monoclonal antibodies from murine variable regions. J. Mol. Biol. 2010;396:1474–1490. doi: 10.1016/j.jmb.2009.12.046. [DOI] [PubMed] [Google Scholar]
- 28.Duan Y., Dhar A., Patel C., Khimani M., Neogi S., Sharma P., Siva Kumar N., Vekariya R.L. A brief review on solid lipid nanoparticles: Part and parcel of contemporary drug delivery systems. RSC Adv. 2020;10:26777–26791. doi: 10.1039/D0RA03491F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kuo Y.C., Liang C.T. Inhibition of human brain malignant glioblastoma cells using carmustine-loaded catanionic solid lipid nanoparticles with surface anti-epithelial growth factor receptor. Biomaterials. 2011;32:3340–3350. doi: 10.1016/j.biomaterials.2011.01.048. [DOI] [PubMed] [Google Scholar]
- 30.Kuo Y.C., Liang C.T. Catanionic solid lipid nanoparticles carrying doxorubicin for inhibiting the growth of U87MG cells. Colloids Surf. B Biointerfaces. 2011;85:131–137. doi: 10.1016/j.colsurfb.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 31.Kuo Y.C., Chao I.W. Conjugation of melanotransferrin antibody on solid lipid nanoparticles for mediating brain cancer malignancy. Biotechnol. Prog. 2016;32:480–490. doi: 10.1002/btpr.2214. [DOI] [PubMed] [Google Scholar]
- 32.Kuo Y.C., Wang I.H. Enhanced delivery of etoposide across the blood-brain barrier to restrain brain tumor growth using melanotransferrin antibody- and tamoxifen-conjugated solid lipid nanoparticles. J. Drug Target. 2016;24:645–654. doi: 10.3109/1061186X.2015.1132223. [DOI] [PubMed] [Google Scholar]
- 33.Kuo Y.C., Lee C.H. Dual targeting of solid lipid nanoparticles grafted with 83-14 MAb and anti-EGF receptor for malignant brain tumor therapy. Life Sci. 2016;146:222–231. doi: 10.1016/j.lfs.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 34.Kim J.H., Kim Y., Bae K.H., Park T.G., Lee J.H., Park K. Tumor-Targeted Delivery of Paclitaxel Using Low Density Lipoprotein-Mimetic Solid Lipid Nanoparticles. Mol. Pharm. 2015;12:1230–1241. doi: 10.1021/mp500737y. [DOI] [PubMed] [Google Scholar]
- 35.Tummala S., Gowthamarajan K., Satish Kumar M.N., Praveen T.K., Yamjala K., Tripuraneni N.S., Prakash A. Formulation and optimization of oxaliplatin immuno-nanoparticles using Box-Behnken design and cytotoxicity assessment for synergistic and receptor-mediated targeting in the treatment of colorectal cancer. Artif. Cells Nanomed. Biotechnol. 2016;44:1835–1850. doi: 10.3109/21691401.2015.1111226. [DOI] [PubMed] [Google Scholar]
- 36.Souto E.B., Doktorovova S., Campos J.R., Martins-Lopes P., Silva A.M. Surface-tailored anti-HER2/neu-solid lipid nanoparticles for site-specific targeting MCF-7 and BT-474 breast cancer cells. Eur. J. Pharm. Sci. 2019;128:27–35. doi: 10.1016/j.ejps.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 37.Souto E.B., Souto S.B., Zielinska A., Durazzo A., Lucarini M., Santini A., Horbańczuk O.K., Atanasov A.G., Marques C., Andrade L.N., et al. Perillaldehyde 1,2-epoxide Loaded SLN-Tailored mAb: Production, Physicochemical Characterization and In Vitro Cytotoxicity Profile in MCF-7 Cell Lines. Pharmaceutics. 2020;12:161. doi: 10.3390/pharmaceutics12020161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cavaco M.C., Pereira C., Kreutzer B., Gouveia L.F., Silva-Lima B., Brito A.M., Videira M. Evading P-glycoprotein mediated-efflux chemoresistance using Solid Lipid Nanoparticles. Eur. J. Pharm. Biopharm. 2017;110:76–84. doi: 10.1016/j.ejpb.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 39.Siddhartha V.T., Pindiprolu S., Chintamaneni P.K., Tummala S., Nandha Kumar S. RAGE receptor targeted bioconjuguate lipid nanoparticles of diallyl disulfide for improved apoptotic activity in triple negative breast cancer: In vitro studies. Artif. Cells Nanomed. Biotechnol. 2018;46:387–397. doi: 10.1080/21691401.2017.1313267. [DOI] [PubMed] [Google Scholar]
- 40.Pindiprolu S., Krishnamurthy P.T., Dev C., Chintamaneni P.K. DR5 antibody conjugated lipid-based nanocarriers of gamma-secretase inhibitor for the treatment of triple negative breast cancer. Chem. Phys. Lipids. 2021;235:105033. doi: 10.1016/j.chemphyslip.2020.105033. [DOI] [PubMed] [Google Scholar]
- 41.Kumari M., Krishnamurthy P.T., Pinduprolu S.K.S.S., Sola P. DR-5 and DLL-4 mAb Functionalized SLNs of Gamma-Secretase Inhibitors- An Approach for TNBC Treatment. Adv. Pharm. Bull. 2021;11:618–623. doi: 10.34172/apb.2021.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khosa A., Reddi S., Saha R.N. Nanostructured lipid carriers for site-specific drug delivery. Biomed. Pharmacother. 2018;103:598–613. doi: 10.1016/j.biopha.2018.04.055. [DOI] [PubMed] [Google Scholar]
- 43.Liu D., Liu F., Liu Z., Wang L., Zhang N. Tumor specific delivery and therapy by double-targeted nanostructured lipid carriers with anti-VEGFR-2 antibody. Mol. Pharm. 2011;8:2291–2301. doi: 10.1021/mp200402e. [DOI] [PubMed] [Google Scholar]
- 44.Abdolahpour S., Toliyat T., Omidfar K., Modjtahedi H., Wong A.J., Rasaee M.J., Kashanian S., Paknejad M. Targeted delivery of doxorubicin into tumor cells by nanostructured lipid carriers conjugated to anti-EGFRvIII monoclonal antibody. Artif. Cells Nanomed. Biotechnol. 2018;46:89–94. doi: 10.1080/21691401.2017.1296847. [DOI] [PubMed] [Google Scholar]
- 45.Varshosaz J., Davoudi M.A., Rasoul-Amini S. Docetaxel-loaded nanostructured lipid carriers functionalized with trastuzumab (Herceptin) for HER2-positive breast cancer cells. J. Liposome Res. 2018;28:285–295. doi: 10.1080/08982104.2017.1370471. [DOI] [PubMed] [Google Scholar]
- 46.Varshosaz J., Jandaghian S., Mirian M., Sajjadi S.E. Co-delivery of rituximab targeted curcumin and imatinib nanostructured lipid carriers in non-Hodgkin lymphoma cells. J. Liposome Res. 2021;31:64–78. doi: 10.1080/08982104.2020.1720718. [DOI] [PubMed] [Google Scholar]
- 47.Guo S., Zhang Y., Wu Z., Zhang L., He D., Li X., Wang Z. Synergistic combination therapy of lung cancer: Cetuximab functionalized nanostructured lipid carriers for the co-delivery of paclitaxel and 5-Demethylnobiletin. Biomed. Pharmacother. 2019;118:109225. doi: 10.1016/j.biopha.2019.109225. [DOI] [PubMed] [Google Scholar]
- 48.Liu Y., Zhang H., Cui H., Zhang F., Zhao L., Liu Y., Meng Q. Combined and targeted drugs delivery system for colorectal cancer treatment: Conatumumab decorated, reactive oxygen species sensitive irinotecan prodrug and quercetin co-loaded nanostructured lipid carriers. Drug Deliv. 2022;29:342–350. doi: 10.1080/10717544.2022.2027573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Di Filippo L.D., Lobato Duarte J., Hofstätter Azambuja J., Isler Mancuso R., Tavares Luiz M., Hugo Sousa Araújo V., Delbone Figueiredo I., Barretto-de-Souza L., Miguel Sábio R., Sasso-Cerri E., et al. Glioblastoma multiforme targeted delivery of docetaxel using bevacizumab-modified nanostructured lipid carriers impair in vitro cell growth and in vivo tumor progression. Int. J. Pharm. 2022;618:121682. doi: 10.1016/j.ijpharm.2022.121682. [DOI] [PubMed] [Google Scholar]
- 50.Nakhaei P., Margiana R., Bokov D.O., Abdelbasset W.K., Jadidi Kouhbanani M.A., Varma R.S., Marofi F., Jarahian M., Beheshtkhoo N. Liposomes: Structure, Biomedical Applications, and Stability Parameters With Emphasis on Cholesterol. Front. Bioeng. Biotechnol. 2021;9:705886. doi: 10.3389/fbioe.2021.705886. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 51.Saman H., Raza S.S., Uddin S., Rasul K. Inducing Angiogenesis, a Key Step in Cancer Vascularization, and Treatment Approaches. Cancers. 2020;12:1172. doi: 10.3390/cancers12051172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jain R.K. Antiangiogenic therapy for cancer: Current and emerging concepts. Oncology. 2005;19:7–16. [PubMed] [Google Scholar]
- 53.Kuesters G.M., Campbell R.B. Conjugation of bevacizumab to cationic liposomes enhances their tumor-targeting potential. Nanomedicine. 2010;5:181–192. doi: 10.2217/nnm.09.105. [DOI] [PubMed] [Google Scholar]
- 54.Jain S., Deore S.V., Ghadi R., Chaudhari D., Kuche K., Katiyar S.S. Tumor microenvironment responsive VEGF-antibody functionalized pH sensitive liposomes of docetaxel for augmented breast cancer therapy. Mater. Sci. Eng. C. 2021;121:111832. doi: 10.1016/j.msec.2020.111832. [DOI] [PubMed] [Google Scholar]
- 55.Shein S.A., Nukolova N.V., Korchagina A.A., Abakumova T.O., Kiuznetsov I.I., Abakumov M.A., Baklaushev V.P., Gurina O.I., Chekhonin V.P. Site-directed delivery of VEGF-targeted liposomes into intracranial C6 glioma. Bull. Exp. Biol. Med. 2015;158:371–376. doi: 10.1007/s10517-015-2765-4. [DOI] [PubMed] [Google Scholar]
- 56.Shein S.A., Kuznetsov I.I., Abakumova T.O., Chelushkin P.S., Melnikov P.A., Korchagina A.A., Bychkov D.A., Seregina I.F., Bolshov M.A., Kabanov A.V., et al. VEGF- and VEGFR2-targeted liposomes for cisplatin delivery to glioma cells. Mol. Pharm. 2016;13:3712–3723. doi: 10.1021/acs.molpharmaceut.6b00519. [DOI] [PubMed] [Google Scholar]
- 57.Hatakeyama H., Akita H., Ishida E., Hashimoto K., Kobayashi H., Aoki T., Yasuda J., Obata K., Kikuchi H., Ishida T., et al. Tumor targeting of doxorubicin by anti-MT1-MMP antibody-modified PEG liposomes. Int. J. Pharm. 2007;342:194–200. doi: 10.1016/j.ijpharm.2007.04.037. [DOI] [PubMed] [Google Scholar]
- 58.Lu X., Liu S., Han M., Yang X., Sun K., Wang H., Mu H., Du Y., Wang A., Ni L., et al. Afatinib-loaded immunoliposomes functionalized with cetuximab: A novel strategy targeting the epidermal growth factor receptor for treatment of non-small-cell lung cancer. Int. J. Pharm. 2019;560:126–135. doi: 10.1016/j.ijpharm.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 59.Kim I.Y., Kang Y.S., Lee D.S., Park H.J., Choi E.K., Oh Y.K., Son H.J., Kim J.S. Antitumor activity of EGFR targeted pH-sensitive immunoliposomes encapsulating gemcitabine in A549 xenograft nude mice. J. Control. Release. 2009;140:55–60. doi: 10.1016/j.jconrel.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 60.Limasale Y.D., Tezcaner A., Özen C., Keskin D., Banerjee S. Epidermal growth factor receptor-targeted immunoliposomes for delivery of celecoxib to cancer cells. Int. J. Pharm. 2015;479:364–373. doi: 10.1016/j.ijpharm.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 61.Matusewicz L., Filip-Psurska B., Psurski M., Tabaczar S., Podkalicka J., Wietrzyk J., Ziółkowski P., Czogalla A., Sikorski A.F. EGFR-targeted immunoliposomes as a selective delivery system of simvastatin, with potential use in treatment of triple-negative breast cancers. Int. J. Pharm. 2019;569:118605. doi: 10.1016/j.ijpharm.2019.118605. [DOI] [PubMed] [Google Scholar]
- 62.Burande A.S., Viswanadh M.K., Jha A., Mehata A.K., Shaik A., Agrawal N., Poddar S., Mahto S.K., Muthu M.S. EGFR Targeted Paclitaxel and Piperine Co-loaded Liposomes for the Treatment of Triple Negative Breast Cancer. AAPS PharmSciTech. 2020;21:151. doi: 10.1208/s12249-020-01671-7. [DOI] [PubMed] [Google Scholar]
- 63.Petrilli R., Eloy J.O., Saggioro F.P., Chesca D.L., de Souza M.C., Dias M.V.S., da Silva L.L.P., Lee R.J., Lopez R.F.V. Skin cancer treatment effectiveness is improved by iontophoresis of EGFR-targeted liposomes containing 5-FU compared with subcutaneous injection. J. Control. Release. 2018;283:151–162. doi: 10.1016/j.jconrel.2018.05.038. [DOI] [PubMed] [Google Scholar]
- 64.Zalba S., Contreras A.M., Haeri A., ten Hagen T.L.M., Navarro I., Koning G., Garrido M.J. Cetuximab-oxaliplatin-liposomes for epidermal growth factor receptor targeted chemotherapy of colorectal cancer. J. Control. Release. 2015;210:26–38. doi: 10.1016/j.jconrel.2015.05.271. [DOI] [PubMed] [Google Scholar]
- 65.Eloy J.O., Ruiz A., de Lima F.T., Petrilli R., Raspantini G., Nogueira K.A.B., Santos E., de Oliveira C.S., Borges J.C., Marchetti J.M., et al. EGFR-targeted immunoliposomes efficiently deliver docetaxel to prostate cancer cells. Colloids Surf. B Biointerfaces. 2020;194:111185. doi: 10.1016/j.colsurfb.2020.111185. [DOI] [PubMed] [Google Scholar]
- 66.Eloy J.O., Petrilli R., Brueggemeier R.W., Marchetti J.M., Lee R.J. Rapamycin-loaded Immunoliposomes Functionalized with Trastuzumab: A Strategy to Enhance Cytotoxicity to HER2-positive Breast Cancer Cells. Anticancer Agents Med. Chem. 2017;17:48–56. doi: 10.2174/1871520616666160526103432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eloy J.O., Petrilli R., Chesca D.L., Saggioro F.P., Lee R.J., Marchetti J.M. Anti-HER2 immunoliposomes for co-delivery of paclitaxel and rapamycin for breast cancer therapy. Eur. J. Pharm. Biopharm. 2017;115:159–167. doi: 10.1016/j.ejpb.2017.02.020. [DOI] [PubMed] [Google Scholar]
- 68.Li N., Xie X., Hu Y., He H., Fu X., Fang T., Li C. Herceptin-conjugated liposomes co-loaded with doxorubicin and simvastatin in targeted prostate cancer therapy. Am. J. Transl. Res. 2019;11:1255–1269. [PMC free article] [PubMed] [Google Scholar]
- 69.Kullberg M., Mann K., Anchordoquy T.J. Targeting Her-2+ Breast Cancer Cells with Bleomycin Immunoliposomes Linked to LLO. Mol. Pharm. 2012;9:2000–2008. doi: 10.1021/mp300049n. [DOI] [PubMed] [Google Scholar]
- 70.Raju A., Muthu M.S., Feng S.S. Trastuzumab-conjugated vitamin E TPGS liposomes for sustained and targeted delivery of docetaxel. Expert Opin. Drug Deliv. 2013;10:747–760. doi: 10.1517/17425247.2013.777425. [DOI] [PubMed] [Google Scholar]
- 71.Rodallec A., Sicard G., Giacometti S., Carre M., Maia T., Valette M., Bouquet F., Savina A., Lacarelle B., Ciccolini J., et al. Tumor uptake and associated greater efficacy of anti-Her2 immunoliposome does not rely on Her2 expression status: Study of a docetaxel-trastuzumab immunoliposome on Her2+ breast cancer model (SKBR3) Anti-Cancer Drugs. 2020;31:463–472. doi: 10.1097/CAD.0000000000000878. [DOI] [PubMed] [Google Scholar]
- 72.Catania A., Barrajón-Catalán E., Nicolosi S., Cicirata F., Micol V. Immunoliposome encapsulation increases cytotoxic activity and selectivity of curcumin and resveratrol against HER2 overexpressing human breast cancer cells. Breast Cancer Res. Treat. 2013;141:55–65. doi: 10.1007/s10549-013-2667-y. [DOI] [PubMed] [Google Scholar]
- 73.Amin M., Pourshohod A., Kheirollah A., Afrakhteh M., Gholami-Borujeni F., Zeinali M., Jamalan M. Specific delivery of idarubicin to HER2-positive breast cancerous cell line by trastuzumab-conjugated liposomes. J. Drug Deliv. Sci. Technol. 2018;47:209–214. doi: 10.1016/j.jddst.2018.07.017. [DOI] [Google Scholar]
- 74.Khaleseh F., Hemmati Azandaryani A., Fathian Kolahkaj F., Khazaei M., Derakhshandeh K. Enhancement of in vitro antitumour activity of epirubicin in HER2+ breast cancer cells using immunoliposome formulation. IET Nanobiotechnol. 2021;15:257–265. doi: 10.1049/nbt2.12012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schnyder A., Krähenbühl S., Drewe J., Huwyler J. Targeting of daunomycin using biotinylated immunoliposomes: Pharmacokinetics, tissue distribution and in vitro pharmacological effects. J. Drug Target. 2005;13:325–335. doi: 10.1080/10611860500206674. [DOI] [PubMed] [Google Scholar]
- 76.Ashrafzadeh M.S., Akbarzadeh A., Heydarinasab A., Ardjmand M. In vivo Glioblastoma Therapy Using Targeted Liposomal Cisplatin. Int. J. Nanomed. 2020;15:7035–7049. doi: 10.2147/IJN.S255902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim S.S., Rait A., Kim E., DeMarco J., Pirollo K.F., Chang E.H. Encapsulation of temozolomide in a tumor-targeting nanocomplex enhances anti-cancer efficacy and reduces toxicity in a mouse model of glioblastoma. Cancer Lett. 2015;369:250–258. doi: 10.1016/j.canlet.2015.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wong B.C., Zhang H., Qin L., Chen H., Fang C., Lu A., Yang Z. Carbonic anhydrase IX-directed immunoliposomes for targeted drug delivery to human lung cancer cells in vitro. Drug Des. Dev. Ther. 2014;8:993–1001. doi: 10.2147/dddt.S63235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lin C., Wong B.C.K., Chen H., Bian Z., Zhang G., Zhang X., Kashif Riaz M., Tyagi D., Lin G., Zhang Y., et al. Pulmonary delivery of triptolide-loaded liposomes decorated with anti-carbonic anhydrase IX antibody for lung cancer therapy. Sci. Rep. 2017;7:1097. doi: 10.1038/s41598-017-00957-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Brown B.S., Patanam T., Mobli K., Celia C., Zage P.E., Bean A.J., Tasciotti E. Etoposide-loaded immunoliposomes as active targeting agents for GD2-positive malignancies. Cancer Biol. Ther. 2014;15:851–861. doi: 10.4161/cbt.28875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gholizadeh S., Dolman E.M., Wieriks R., Sparidans R.W., Hennink W.E., Kok R.J. Anti-GD2 immunoliposomes for targeted delivery of the survivin inhibitor sepantronium bromide (YM155) to neuroblastoma tumor cells. Pharm. Res. 2018;35:85. doi: 10.1007/s11095-018-2373-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Song H., Su X., Yang K., Niu F., Li J., Song J., Chen H., Li B., Li W., Qian W., et al. CD20 antibody-conjugated immunoliposomes for targeted chemotherapy of melanoma cancer initiating cells. J. Biomed. Nanotechnol. 2015;11:1927–1946. doi: 10.1166/jbn.2015.2129. [DOI] [PubMed] [Google Scholar]
- 83.Saeed M., Zalba S., Seynhaeve A.L.B., Debets R., Ten Hagen T.L.M. Liposomes targeted to MHC-restricted antigen improve drug delivery and antimelanoma response. Int. J. Nanomed. 2019;14:2069–2089. doi: 10.2147/IJN.S190736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Merino M., Lozano T., Casares N., Lana H., Troconiz I.F., ten Hagen T.L.M., Kochan G., Berraondo P., Zalba S., Garrido M.J. Dual activity of PD-L1 targeted Doxorubicin immunoliposomes promoted an enhanced efficacy of the antitumor immune response in melanoma murine model. J. Nanobiotechnol. 2021;19:102. doi: 10.1186/s12951-021-00846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yu J., Hu F., Zhu Q., Li X., Ren H., Fan S., Qian B., Zhai B., Yang D. PD-L1 monoclonal antibody-decorated nanoliposomes loaded with Paclitaxel and P-gp transport inhibitor for the synergistic chemotherapy against multidrug resistant gastric cancers. Nanoscale Res. Lett. 2020;15:59. doi: 10.1186/s11671-019-3228-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yang W., Hu Q., Xu Y., Liu H., Zhong L. Antibody fragment-conjugated gemcitabine and paclitaxel-based liposome for effective therapeutic efficacy in pancreatic cancer. Mater. Sci. Eng. C. 2018;89:328–335. doi: 10.1016/j.msec.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 87.Wang J., Wu Z., Pan G., Ni J., Xie F., Jiang B., Wei L., Gao J., Zhou W. Enhanced doxorubicin delivery to hepatocellular carcinoma cells via CD147 antibody-conjugated immunoliposomes. Nanomed. Nanotechnol. Biol. Med. 2018;14:1949–1961. doi: 10.1016/j.nano.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 88.Lu L., Ding Y., Zhang Y., Ho R.J., Zhao Y., Zhang T., Guo C. Antibody-modified liposomes for tumor-targeting delivery of timosaponin AIII. Int. J. Nanomed. 2018;13:1927–1944. doi: 10.2147/IJN.S153107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Khayrani A.C., Mahmud H., Oo A.K.K., Zahra M.H., Oze M., Du J., Alam M.J., Afify S.M., Quora H.A.A., Shigehiro T., et al. Targeting Ovarian Cancer Cells Overexpressing CD44 with Immunoliposomes Encapsulating Glycosylated Paclitaxel. Int. J. Mol. Sci. 2019;20:1042. doi: 10.3390/ijms20051042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Arabi L., Badiee A., Mosaffa F., Jaafari M.R. Targeting CD44 expressing cancer cells with anti-CD44 monoclonal antibody improves cellular uptake and antitumor efficacy of liposomal doxorubicin. J. Control. Release. 2015;220:275–286. doi: 10.1016/j.jconrel.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 91.Dadashi Noshahr K., Shamsi F., Valtchev P., Kokhaei P., Hemati M., Reza Akbari Eidgahi M., Khaleghian A. Optimization of post-insertion method to conjugate Doxil with anti-CD133 monoclonal antibodies: Investigating the specific binding and cytotoxicity to colorectal cancer cells in vitro. Saudi Pharm. J. 2020;28:1392–1401. doi: 10.1016/j.jsps.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Scavo M.P., Cutrignelli A., Depalo N., Fanizza E., Laquintana V., Gasparini G., Giannelli G., Denora N. Effectiveness of a Controlled 5-FU Delivery Based on FZD10 Antibody-Conjugated Liposomes in Colorectal Cancer In vitro Models. Pharmaceutics. 2020;12:650. doi: 10.3390/pharmaceutics12070650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Garg N.K., Tandel N., Jadon R.S., Tyagi R.K., Katare O.P. Lipid-polymer hybrid nanocarrier-mediated cancer therapeutics: Current status and future directions. Drug Discov. Today. 2018;23:1610–1621. doi: 10.1016/j.drudis.2018.05.033. [DOI] [PubMed] [Google Scholar]
- 94.Hu C.M., Kaushal S., Tran Cao H.S., Aryal S., Sartor M., Esener S., Bouvet M., Zhang L. Half-antibody functionalized lipid-polymer hybrid nanoparticles for targeted drug delivery to carcinoembryonic antigen presenting pancreatic cancer cells. Mol. Pharm. 2010;7:914–920. doi: 10.1021/mp900316a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gao J., Xia Y., Chen H., Yu Y., Song J., Li W., Qian W., Wang H., Dai J., Guo Y. Polymer-lipid hybrid nanoparticles conjugated with anti-EGF receptor antibody for targeted drug delivery to hepatocellular carcinoma. Nanomedicine. 2014;9:279–293. doi: 10.2217/nnm.13.20. [DOI] [PubMed] [Google Scholar]
- 96.Wei J., Sun J., Liu Y. Enhanced targeting of prostate cancer-initiating cells by salinomycin-encapsulated lipid-PLGA nanoparticles linked with CD44 antibodies. Oncol. Lett. 2019;17:4024–4033. doi: 10.3892/ol.2019.10050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fu Q., Wang J., Liu H. Chemo-immune synergetic therapy of esophageal carcinoma: Trastuzumab modified, cisplatin and fluorouracil co-delivered lipid-polymer hybrid nanoparticles. Drug Deliv. 2020;27:1535–1543. doi: 10.1080/10717544.2020.1837294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Simard P., Leroux J.C. In vivo evaluation of pH-sensitive polymer-based immunoliposomes targeting the CD33 antigen. Mol. Pharm. 2010;7:1098–1107. doi: 10.1021/mp900261m. [DOI] [PubMed] [Google Scholar]
- 99.Leung S.L., Zha Z., Cohn C., Dai Z., Wu X. Anti-EGFR antibody conjugated organic-inorganic hybrid lipid nanovesicles selectively target tumor cells. Colloids Surf. B Biointerfaces. 2014;121:141–149. doi: 10.1016/j.colsurfb.2014.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Limongi T., Susa F., Marini M., Allione M., Torre B., Pisano R., di Fabrizio E. Lipid-Based Nanovesicular Drug Delivery Systems. Nanomaterials. 2021;11:3391. doi: 10.3390/nano11123391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Liu F.R., Jin H., Wang Y., Chen C., Li M., Mao S.J., Wang Q., Li H. Anti-CD123 antibody-modified niosomes for targeted delivery of daunorubicin against acute myeloid leukemia. Drug Deliv. 2017;24:882–890. doi: 10.1080/10717544.2017.1333170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhai J., Luwor R.B., Ahmed N., Escalona R., Tan F.H., Fong C., Ratcliffe J., Scoble J.A., Drummond C.J., Tran N. Paclitaxel-Loaded Self-Assembled Lipid Nanoparticles as Targeted Drug Delivery Systems for the Treatment of Aggressive Ovarian Cancer. ACS Appl. Mater. Interfaces. 2018;10:25174–25185. doi: 10.1021/acsami.8b08125. [DOI] [PubMed] [Google Scholar]
- 103.Pirollo K.F., Nemunaitis J., Leung P.K., Nunan R., Adams J., Chang E.H. Safety and Efficacy in Advanced Solid Tumors of a Targeted Nanocomplex Carrying the p53 Gene Used in Combination with Docetaxel: A Phase 1b Study. Mol. Ther. 2016;24:1697–1706. doi: 10.1038/mt.2016.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Siefker-Radtke A., Zhang X.Q., Guo C.C., Shen Y., Pirollo K.F., Sabir S., Leung C., Leong-Wu C., Ling C.M., Chang E.H., et al. A Phase l Study of a Tumor-targeted Systemic Nanodelivery System, SGT-94, in Genitourinary Cancers. Mol. Ther. 2016;24:1484–1491. doi: 10.1038/mt.2016.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gargett T., Abbas M.N., Rolan P., Price J.D., Gosling K.M., Ferrante A., Ruszkiewicz A., Atmosukarto I.I.C., Altin J., Parish C.R., et al. Phase I trial of Lipovaxin-MM, a novel dendritic cell-targeted liposomal vaccine for malignant melanoma. Cancer Immunol. Immunother. 2018;67:1461–1472. doi: 10.1007/s00262-018-2207-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Solomon B.J., Desai J., Rosenthal M., McArthur G.A., Pattison S.T., Pattison S.L., MacDiarmid J., Brahmbhatt H., Scott A.M. A First-Time-In-Human Phase I Clinical Trial of Bispecific Antibody-Targeted, Paclitaxel-Packaged Bacterial Minicells. PLoS ONE. 2015;10:e0144559. doi: 10.1371/journal.pone.0144559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Elshiaty M., Schindler H., Christopoulos P. Principles and Current Clinical Landscape of Multispecific Antibodies against Cancer. Int. J. Mol. Sci. 2021;22:5632. doi: 10.3390/ijms22115632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Huang Z.R., Tipparaju S.K., Kirpotin D.B., Pien C., Kornaga T., Noble C.O., Koshkaryev A., Tran J., Kamoun W.S., Drummond D.C. Formulation optimization of an ephrin A2 targeted immunoliposome encapsulating reversibly modified taxane prodrugs. J. Control. Release. 2019;310:47–57. doi: 10.1016/j.jconrel.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 109.Lee H., Shields A.F., Siegel B.A., Miller K.D., Krop I., Ma C.X., LoRusso P.M., Munster P.N., Campbell K., Gaddy D.F., et al. 64Cu-MM-302 Positron Emission Tomography Quantifies Variability of Enhanced Permeability and Retention of Nanoparticles in Relation to Treatment Response in Patients with Metastatic Breast Cancer. Clin. Cancer Res. 2017;23:4190–4202. doi: 10.1158/1078-0432.CCR-16-3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mamot C., Ritschard R., Wicki A., Stehle G., Dieterle T., Bubendorf L., Hilker C., Deuster S., Herrmann R., Rochlitz C. Tolerability, safety, pharmacokinetics, and efficacy of doxorubicin-loaded anti-EGFR immunoliposomes in advanced solid tumours: A phase 1 dose-escalation study. Lancet Oncol. 2012;13:1234–1241. doi: 10.1016/S1470-2045(12)70476-X. [DOI] [PubMed] [Google Scholar]
- 111.Matsumura Y., Gotoh M., Muro K., Yamada Y., Shirao K., Shimada Y., Okuwa M., Matsumoto S., Miyata Y., Ohkura H., et al. Phase I and pharmacokinetic study of MCC-465, a doxorubicin (DXR) encapsulated in PEG immunoliposome, in patients with metastatic stomach cancer. Ann. Oncol. 2004;15:517–525. doi: 10.1093/annonc/mdh092. [DOI] [PubMed] [Google Scholar]
- 112.Kamoun W.S., Kirpotin D.B., Huang Z.R., Tipparaju S.K., Noble C.O., Hayes M.E., Luus L., Koshkaryev A., Kim J., Olivier K., et al. Antitumour activity and tolerability of an EphA2-targeted nanotherapeutic in multiple mouse models. Nat. Biomed. Eng. 2019;3:264–280. doi: 10.1038/s41551-019-0385-4. [DOI] [PubMed] [Google Scholar]
- 113.Kamoun W., Swindell E., Pien C., Luus L., Cain J., Pham M., Kandela I., Huang Z.R., Tipparaju S.K., Koshkaryev A., et al. Targeting EphA2 in Bladder Cancer Using a Novel Antibody-Directed Nanotherapeutic. Pharmaceutics. 2020;12:996. doi: 10.3390/pharmaceutics12100996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Espelin C.W., Leonard S.C., Geretti E., Wickham T.J., Hendriks B.S. Dual HER2 Targeting with Trastuzumab and Liposomal-Encapsulated Doxorubicin (MM-302) Demonstrates Synergistic Antitumor Activity in Breast and Gastric Cancer. Cancer Res. 2016;76:1517–1527. doi: 10.1158/0008-5472.CAN-15-1518. [DOI] [PubMed] [Google Scholar]
- 115.Kasenda B., König D., Manni M., Ritschard R., Duthaler U., Bartoszek E., Bärenwaldt A., Deuster S., Hutter G., Cordier D., et al. Targeting immunoliposomes to EGFR-positive glioblastoma. ESMO Open. 2022;7:100365. doi: 10.1016/j.esmoop.2021.100365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hallan S.S., Sguizzato M., Esposito E., Cortesi R. Challenges in the Physical Characterization of Lipid Nanoparticles. Pharmaceutics. 2021;13:549. doi: 10.3390/pharmaceutics13040549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dai Q., Wilhelm S., Ding D., Syed A.M., Sindhwani S., Zhang Y., Chen Y.Y., MacMillan P., Chan W.C.W. Quantifying the Ligand-Coated Nanoparticle Delivery to Cancer Cells in Solid Tumors. ACS Nano. 2018;12:8423–8435. doi: 10.1021/acsnano.8b03900. [DOI] [PubMed] [Google Scholar]
- 118.Marques A.C., Costa P.J., Velho S., Amaral M.H. Stimuli-responsive hydrogels for intratumoral drug delivery. Drug Discov. Today. 2021;26:2397–2405. doi: 10.1016/j.drudis.2021.04.012. [DOI] [PubMed] [Google Scholar]
- 119.Wu T., Tang M. Review of the effects of manufactured nanoparticles on mammalian target organs. J. Appl. Toxicol. 2018;38:25–40. doi: 10.1002/jat.3499. [DOI] [PubMed] [Google Scholar]
- 120.Najahi-Missaoui W., Arnold R.D., Cummings B.S. Safe Nanoparticles: Are We There Yet? Int. J. Mol. Sci. 2020;22:385. doi: 10.3390/ijms22010385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.He H., Liu L., Morin E.E., Liu M., Schwendeman A. Survey of Clinical Translation of Cancer Nanomedicines-Lessons Learned from Successes and Failures. Acc. Chem. Res. 2019;52:2445–2461. doi: 10.1021/acs.accounts.9b00228. [DOI] [PubMed] [Google Scholar]
- 122.Bukhari S.I., Imam S.S., Ahmad M.Z., Vuddanda P.R., Alshehri S., Mahdi W.A., Ahmad J. Recent Progress in Lipid Nanoparticles for Cancer Theranostics: Opportunity and Challenges. Pharmaceutics. 2021;13:840. doi: 10.3390/pharmaceutics13060840. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.