Abstract
Introduction: A rupture of the Achilles tendon with a delay in diagnosis or treatment for more than 6 weeks is considered a chronic tear. Local tendon transfer procedures can be used in chronic Achilles tendon ruptures. This study evaluated the outcome, return to sport, and complications of local tendon transfer in patients with chronic Achilles tendon rupture. Material and methods: The present study was conducted according to the PRISMA 2020 guidelines. PubMed, Google Scholar, Embase, and Web of Science databases were accessed in November 2022. Results: Data were retrieved from 23 articles (463 patients, mean age 50.9 ± 13.5 years). The mean duration of the follow-up was 58.3 ± 76.8 months. The VAS improved by 1.8/10 (p = 0.4), the AOFAS by 33.4/100 (p < 0.0001), and the ATRS by 32.5/100 (p = 0.0001) points. Patients were able to return to sport after a mean of 19.6 ± 16.4 weeks. A total of 79% of patients were able to return to their previous activities. The rate of complications was 13.3%. Conclusions: The use of local tendon transfer for chronic Achilles tendon ruptures using the FHL or PB tendon resulted in good clinical outcomes and a reliable return to daily activities and sports. The rate of complications reflects the chronicity of the condition and the technical complexity of the procedure. Level of evidence: IV.
Keywords: Achilles tendon, tendon transfer, mid-portion Achilles’ chronic ruptures
1. Introduction
Classically located within 2–7 cm of its distal insertion on the calcaneus [1], tears of the Achilles tendon (AT), the strongest tendon in the human body [2], are frequently not diagnosed in a timely fashion, and a rupture with a delay in diagnosis or treatment for more than 6 weeks is considered a chronic tear [1].
Tendon transfer procedures can be used in Achilles tendinopathy and chronic ruptures [3,4]. Various techniques have been described for AT reconstruction and augmentation, including local tendon transfers (flexor hallucis longus, peroneus brevis, flexor digitorum longus, and peroneus longus) and grafts (autograft, allograft, and synthetic graft) [5].
The transfer of the flexor hallucis longus (FHL) tendon was first described by Hansen in 1991 [6]. Several modifications have been described since, including single or double incisions, short or long transfer, different methods of fixation, and an open or endoscopic approach, and it is now the most commonly published technique to reconstruct a chronic tear [4]. This procedure has several advantages: the FHL tendon is easy to harvest given its proximity to the AT and can be harvested with small incisions, minimizing the risk of neurovascular injury and wound healing complications [4]. Transfer of the peroneus brevis (PB) tendon was popularized by Perez-Teuffer in 1974 [7]. PB is suitable for patients with a tendon gap inferior to 6 cm and has a low rate of wound healing complications [8]. The transfer of the flexor digitorum longus (FDL) tendon was described by Mann et al. in 1991 [9]. It is an alternative in the treatment of these injuries, with low complications and donor site morbidity [10]. Transfers of the peroneus longus (PL) tendon have also been reported but are less commonly used in clinical practice [11]. The choice of the optimal technique is still debated, and no consensus has been reached. The present study analyzes in a systematic fashion the differences between the various local tendon transfers in the management of chronic Achilles tendon ruptures, evaluating clinical outcomes, complications, and return to sport.
2. Material and Methods
2.1. Search Strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the 2020 PRISMA statement [12]. It was registered on the International Prospective Register of Systematic Reviews (PROSPERO; Registration No. CRD42022384213).
2.2. Eligibility Criteria
All the prospective and retrospective studies reporting local tendon transfer for the management of chronic Achilles tendon tears were accessed. According to the authors language capabilities, articles in English, Italian, German, and Spanish were eligible. Reviews, opinions, letters, and editorials were not considered. Animal, biomechanics, computational, and cadaveric studies were not eligible.
The PICOT algorithm was preliminarily pointed out:
P (Problem): Chronic rupture of the mid-portion Achilles tendon;
I (Intervention): Transfer;
C (Comparison): FHL, PB, FDL, and PL tendon transfers;
O (Outcomes): Clinical outcomes, complications, and return to sport;
T (Timing): ≥6 months of follow-up.
In November 2022, PubMed, Web of Science, Google Scholar, and Embase databases were accessed. No time constraints were used for the search. The following keywords were used in combination: Achilles tendon, tendon transfer, mid-portion Achilles chronic ruptures, mid portion Achilles rupture, main body Achilles rupture, main body Achilles chronic rupture.
2.3. Selection and Data Collection
Two authors independently performed the database search. All the resulting titles were screened, and if suitable, the abstracts were accessed. The full text of the abstracts that matched the topic of interest was accessed. The bibliography of the full-text articles was also screened by hand to identify other eligible articles for inclusion. Disagreements were debated, and the final decision was made by a third senior author.
2.4. Methodological Quality Assessment
Two authors independently performed the methodological quality assessment using the Coleman Methodology Score (CMS). The CMS is a 10 item scale designed to rate the methodological quality of the included studies [13]. These items evaluated study size, mean follow-up, number of surgical procedures, type of study, diagnostic certainty, description of surgical procedure, postoperative rehabilitation, outcome measures, outcome assessment, and selection process. The final score ranges between 0 and 100, with a score of 100 indicating the highest reported methodological quality [13]. (Table 1 and Table 2).
Table 1.
Methodological Quality Assessment: Coleman Methodological Score.
| Authors, Years | Part A: Only One Score to Be Given for Each of the 7 Sections | ||||||
|---|---|---|---|---|---|---|---|
| Study Size | Mean Follow-Up | Surgical Approach | Type of Study | Description of Diagnosis | Descriptions of Surgical Technique | Description of Postoperative Rehabilitation | |
| Abubeih et al., 2018 [14] | 4 | 4 | 10 | 10 | 5 | 10 | 5 |
| Ahn et al., 2022 [15] | 4 | 7 | 10 | 0 | 5 | 10 | 5 |
| Alauddinet al., 2022 [16] | 4 | 0 | 10 | 10 | 5 | 5 | 0 |
| Alhaug et al., 2019 [17] | 4 | 7 | 10 | 0 | 5 | 10 | 5 |
| Elias et al., 2007 [18] | 4 | 4 | 10 | 0 | 5 | 10 | 5 |
| Khalid et al., 2019 [19] | 0 | 4 | 10 | 0 | 5 | 10 | 5 |
| Koh et al., 2019 [20] | 4 | 4 | 0 | 0 | 5 | 10 | 5 |
| Lever et al., 2018 [21] | 4 | 10 | 10 | 0 | 5 | 10 | 5 |
| Lui et al., 2012 [22] | 0 | 7 | 10 | 10 | 5 | 10 | 0 |
| Maffulli et al., 2010 [8] | 4 | 7 | 10 | 10 | 5 | 10 | 5 |
| Maffulli et al., 2012 [23] | 4 | 10 | 10 | 10 | 5 | 10 | 5 |
| Maffulli et al., 2015 [24] | 4 | 7 | 10 | 0 | 5 | 10 | 5 |
| Maffulli et al., 2018 [25] | 4 | 4 | 7 | 10 | 5 | 10 | 5 |
| Mahajan et al., 2009 [26] | 4 | 4 | 10 | 0 | 5 | 10 | 5 |
| Miao et al., 2016 [27] | 4 | 4 | 10 | 0 | 5 | 10 | 5 |
| Oksanen et al., 2014 [28] | 0 | 4 | 10 | 0 | 5 | 10 | 5 |
| Ozer et al., 2018 [29] | 4 | 10 | 10 | 10 | 5 | 10 | 5 |
| Pintore et al., 2001 [30] | 7 | 7 | 7 | 10 | 5 | 10 | 5 |
| Singh et al., 2014 [31] | 4 | 4 | 10 | 0 | 5 | 10 | 5 |
| Tay et al., 2010 [32] | 0 | 4 | 10 | 10 | 5 | 10 | 5 |
| Vega et al., 2018 [33] | 4 | 4 | 10 | 0 | 5 | 10 | 5 |
| Wegrzyn et al., 2010 [5] | 0 | 10 | 10 | 0 | 5 | 10 | 5 |
| Yeoman et al., 2012 [34] | 0 | 0 | 10 | 10 | 5 | 10 | 5 |
Table 2.
Methodological Quality Assessment: Coleman Methodological Score.
| Authors, Years | Part B: Scores May Be Given for Each Option in Each of the Three Sections If Applicable | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Criteria | Procedure Used to Assess Outcomes | Description of the Subject Selection Process | ||||||||||
| Outcome Measures Clearly Defined | Timing of Outcome Assessment Clearly Stated | Use of Outcome Criteria That Have Reported Reliability | General Health Measure Included | Participants Recruited | Investigator Independent of Surgeon | Written Assessment | Completion of Assessment by Patients Themselves with Minimal Investigator Assistance | Selection Criteria Reported and Unbiased | Recruitment Rate Reported > 80% | Recruitment Rate Reported < 80% | ||
| Abubeih et al., 2018 [14] | 2 | 2 | 3 | 0 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 80 |
| Ahn et al., 2022 [15] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 76 |
| Alauddin et al., 2022 [16] | 2 | 2 | 3 | 0 | 5 | 0 | 0 | 3 | 5 | 5 | 0 | 59 |
| Alhaug et al., 2019 [17] | 2 | 2 | 3 | 0 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 73 |
| Elias et al., 2007 [18] | 2 | 2 | 3 | 0 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 70 |
| Khalid et al., 2019 [19] | 2 | 2 | 3 | 0 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 66 |
| Koh et al., 2019 [20] | 2 | 2 | 3 | 0 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 60 |
| Lever et al., 2018 [21] | 2 | 2 | 3 | 0 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 76 |
| Lui et al., 2012 [22] | 2 | 2 | 3 | 0 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 74 |
| Maffulli et al., 2010 [8] | 2 | 2 | 3 | 0 | 5 | 0 | 3 | 3 | 5 | 5 | 0 | 79 |
| Maffulli et al., 2012 [23] | 2 | 2 | 3 | 0 | 5 | 0 | 3 | 3 | 5 | 5 | 0 | 82 |
| Maffulli et al., 2015 [24] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 76 |
| Maffulli et al., 2018 [25] | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 3 | 5 | 5 | 0 | 76 |
| Mahajan et al., 2009 [26] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 73 |
| Miao et al., 2016 [27] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 73 |
| Oksanen et al., 2014 [28] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 0 | 0 | 64 |
| Ozer et al., 2018 [29] | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 3 | 5 | 5 | 0 | 85 |
| Pintore et al., 2001 [30] | 2 | 2 | 3 | 3 | 5 | 0 | 3 | 3 | 5 | 5 | 0 | 82 |
| Singh et al., 2014 [31] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 73 |
| Tay et al., 2010 [32] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 79 |
| Vega et al., 2018 [33] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 73 |
| Wegrzyn et al., 2010 [5] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 75 |
| Yeoman et al., 2012 [34] | 2 | 2 | 3 | 3 | 5 | 4 | 3 | 3 | 5 | 5 | 0 | 75 |
2.5. Data items
Two authors independently performed data extraction. The following data were extracted: generalities (author, year, and type of study), demographic baseline (number of samples and mean age), mean follow-up, mean BMI, and surgical intervention (FHL transfer and PB transfer). The primary outcome of interest was the clinical outcome: the Visual Analogue Scale (VAS), the American Orthopaedic Foot and Ankle Society (AOFAS), and the Achilles tendon Total Rupture Score (ATRS). The secondary outcome of interest was complications. The third outcome of interest was a return to sports.
2.6. Outcomes
The scales used to evaluate clinical outcome were the VAS, AOFAS, and ATRS.
In 1921, Hayes and Patterson introduced the Visual Analogue Scale (VAS) as a pain rating scale [34], measuring the frequency and intensity of pain. It consists of a 10 cm line, the left end of which represents a state of “no pain”, while the right one represents “the worst pain”. The patients mark on the line the point that matches their perception of their current state [35].
The American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Score combined a clinical reported (developed by Kitaoka et al. in 1994 [36]) and a patient reported part to evaluate the outcome of treatment in patients with ankle or hindfoot injury. This rating system is divided into three categories: pain (40 points), function (50 points), and alignment (10 points), with nine questions in each for a total of 100 points. Zero stands for severe pain or impairment; 100 for no pain. Though widely used, the AOFAS score has not been validated.
The Achilles tendon Total Rupture Score (ATRS) measures the outcome related to symptoms and physical activity after treatment in patients with total AT rupture. The scale ranged from 0 = major limitations/symptoms to 100 = no limitations/symptoms and has now been cross-culturally validated in several languages [37]. To date, only the ATRS is a condition-specific PROM.
2.7. Statistical Analysis
The statistical analysis was performed using IBM SPSS version 25. Mean and standard deviation were used for descriptive statistics. For continuous variables, the mean difference effect measure was used. The paired t-test was used with values of p < 0.05 considered statistically significant.
3. Results
3.1. Study Selection
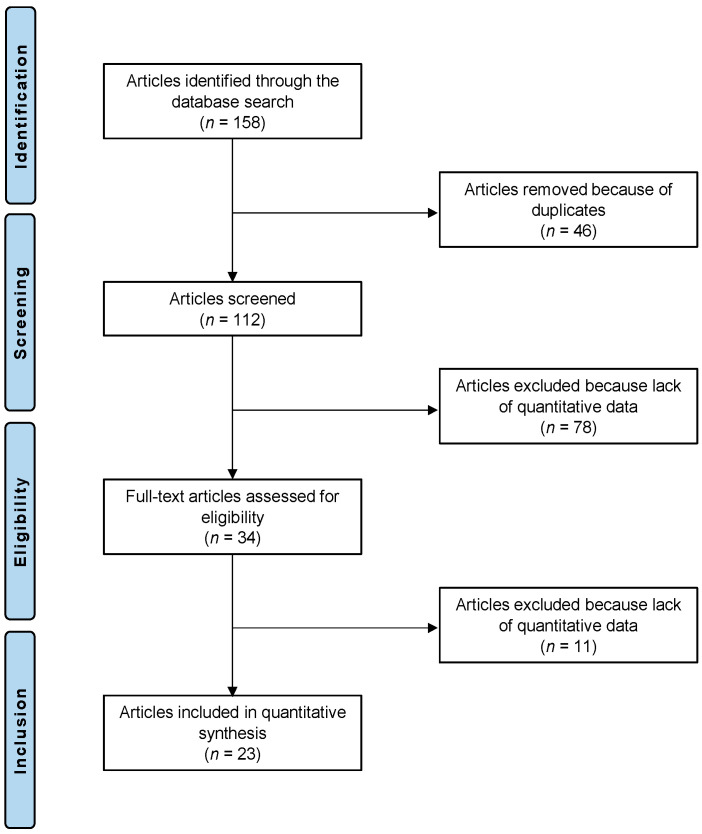
The initial literature search resulted in 158 studies. Of them, 46 were excluded as being duplicates. Another 78 were not eligible: not matching the topic (n = 63), focusing on surgical technique with no outcome data (n = 8), type of study (n = 3), full text not accessible (n = 2), or uncertain results (n = 2). This left 34 articles for inclusion. An additional 11 studies were excluded as they did not report quantitative data under the outcomes of interest. This resulted in 23 studies left for analysis. We placed our main focus on the FHL and PB transfers since studies on other transfers matching the inclusion criteria for the current study had not been carried out. The results of the literature search are shown in Figure 1.
Figure 1.
PRISMA flow diagram of the present systematic review.
3.2. Study Risk of Bias Assessment
The length of follow-up was acceptable in most studies. Surgical technique, diagnosis, and rehabilitation protocols were generally well described. The size of the study and the retrospective design of most of the included studies represented the main limitations highlighted by the CMS. Outcome measures, assessment timing, and selection processes were also clearly defined by most studies. Finally, the mean Coleman Methodology Score of 73.8 (range: 59–85) attests to the overall good quality of the methodological assessment (Table 1 and Table 2).
3.3. Study Characteristics and Results of Individual Studies
A total of 463 patients were identified; 25.1% (120 of 463) were females. The mean length of the follow-up was 58.3 ± 76.8 months. The mean age was 50.9 ± 13.5 years, and the mean BMI was 26.8 ± 0.9 kg/m2. The generalities of the included studies are shown in Table 3.
Table 3.
Generalities and patient baseline databases.
| Author et al., Year | Journal Name | Design | Technique | Follow-Up (Months) | Patients (n) | Age (Mean) | Female (n) |
|---|---|---|---|---|---|---|---|
| Abubeih et al., 2018 [14] | Int Orthop | Prospective | open FHL | 15 | 21 | 40.3 | 6 |
| Ahn et al., 2022 [15] | J Foot Ankle Surg | Retrospective | open FHL | 57 | 28 | 51 | 11 |
| Alauddin et al., 2022 [16] | Mymensingh Med J | Prospective | open FHL | 6 | 21 | 39.5 | |
| Alhaug et al., 2019 [17] | Foot Ankle Surg | Retrospective | open FHL | 54 | 21 | 54.5 | 6 |
| Elias et al., 2007 [18] | Foot Ankle Int | Retrospective | open FHL | 24.4 | 15 | 55.8 | 5 |
| Khalid et al., 2019 [19] | Foot Ankle Spec | Retrospective | endoscopic FHL | 30.9 | 10 | 58.4 | 5 |
| Koh et al., 2019 [20] | Foot Ankle Surg | Retrospective | open FHL | 12 | 29 | 56 | 13 |
| Lever et al., 2018 [21] | Bone Joint J | Retrospective | open FHL | 73 | 20 | 53 | 4 |
| Lui et al., 2012 [22] | Foot Ankle Spec | Prospective | endoscopic FHL | 37 | 5 | 46 | 2 |
| Maffulli et al., 2010 [8] | Am J Sports Med | Prospective | open PB | 48.4 | 32 | 47.13 | 4 |
| Maffulli et al., 2012 [23] | J Bone Joint Surg Am | Prospective | open PB | 186 | 16 | 55.6 | 0 |
| Maffulli et al., 2015 [24] | Bone Joint J | Retrospective | mini-open PB | 55.2 | 17 | 39 | 3 |
| Maffulli et al., 2018 [25] | Foot Ankle Surg | Prospective | mini-open FHL | 35.8 | 21 | 42.7 | 9 |
| mini-open PB | 36.4 | 20 | 45.8 | 6 | |||
| Mahajan et al., 2009 [26] | J Orthop Surg | Retrospective | open FHL | 12 | 36 | 70 | 12 |
| Miao et al., 2016 [27] | Indian J Orthop | Retrospective | mini-open FHL | 32.2 | 32 | 42.1 | 14 |
| Oksanen et al., 2014 [28] | Foot Ankle Surg | Retrospective | open FHL | 27 | 7 | 53 | 3 |
| Ozer et al., 2018 [29] | J Foot Ankle Surg | Prospective | open FHL | 280 | 19 | 47.4 | 1 |
| Pintore et al., 2001 [30] | J Trauma | Prospective | open PB | 53 | 21 | 43.3 | 1 |
| Singh et al., 2014 [31] | J Orthop Surg | Retrospective | mini-open PB | 12 | 22 | 28 | |
| Tay et al., 2010 [32] | Ann Acad Med Singap | Prospective | open FHL | 24 | 6 | 59.5 | |
| Vega et al., 2018 [33] | Foot Ankle Int | Retrospective | endoscopic FHL | 30.5 | 22 | 69 | 6 |
| Wegrzyn et al., 2010 [5] | Int Orthop | Retrospective | open FHL | 79 | 11 | 44 | 4 |
| Yeoman et al., 2012 [34] | Foot (Edinb) | Prospective | open FHL | 6 | 11 | 52.6 | 5 |
FHL: flexor hallucis longus; PB: p eroneus brevis.
3.4. Results of Syntheses
All the patient-reported outcome measures (PROMs) significantly improved at the last follow-up (Table 4). The VAS reduced by 1.8/10 (p = 0.4), the AOFAS improved by 34.3/100 (p < 0.0001), and the ATRS improved by 41.3/100 (p = 0.0001) (Table 4).
Table 4.
Patient-reported outcome measures.
| Endpoint | Baseline | Last Follow-Up | Mean Deviation | p-Value |
|---|---|---|---|---|
| VAS | 2.6 ± 0.6 | 0.8 ± 0.8 | −1.8 | 0.04 |
| AOFAS hindfoot | 57.1 ± 8.5 | 91.4 ± 4.7 | 34.3 | <0.0001 |
| ATRS | 44.4 ± 19.2 | 85.7 ± 7.5 | 41.3 | <0.0001 |
VAS: Visual Analogue Scale; AOFAS hindfoot: American Orthopaedic Foot and Ankle Society hindfoot; ATRS: Achilles tendon Total Rupture Score.
Calf circumference did not improve significantly (p = 0.08). Patients were able to return to their daily activities at a mean of 13.7 ± 8.3 weeks and to sports at a mean of 19.6 ± 16.4 weeks. A total of 79% of patients were able to return to practice the previous activity. The overall rate of complications was 12.7% (59 complications in 463 procedures) (Table 5).
Table 5.
Complications.
| Complications | FHL (338 Procedures) | PB (128 Procedures) | |||
|---|---|---|---|---|---|
| Open | Mini-Open | Endoscopic | Open | Mini-Open | |
| Pain | 2 | ||||
| Superficial infection | 11 | 5 | |||
| Deep infection | 4 | ||||
| Deep venous thrombosis | 1 | ||||
| Focal numbness | 4 | ||||
| Wound complications | 9 | 1 | 1 | 2 | |
| Scar adhesion | 1 | ||||
| Weak push-off | 3 | ||||
| Hypertrophic scarring of the incision | 2 | ||||
| Re-rupture | 1 | ||||
| Claw toes | 2 | ||||
| Reduced skin sensation | 6 | ||||
| Neurological complications | 4 | ||||
4. Discussion
Several local tendon transfers have been described, but the tendons most commonly used in transfers for chronic ruptures of the Achilles tendon are those of the FHL and PB.
The transfer of the flexor hallucis longus (FHL) tendon is the most reported, carrying, at least theoretically, a series of advantages over other local tendon transfers:
The FHL is the second strongest plantar flexor muscle of the ankle;
Its axis of action is in line with that of the AT;
It maintains normal ankle muscle balance;
Its harvest carries a low risk of iatrogenic neurovascular injury;
It increases the vascularity of the reconstruction given its low-lying muscle belly [32].
A potential undesired effect of FHL harvest is the loss of plantar flexion of the interphalangeal joint of the hallux, with decreased plantar flexion and push-off strength [5]. However, despite the weakness of plantar flexion of the hallux, most patients do not report noticeable deformities or weakness and resume their pre-injury daily activities [14].
The morbidity associated with FHL tendon transfer seems not to be clinically relevant, even in running sports that require good push-off or balance [5].
In the present systematic review, the rate of complications following the use of FHL transfers is 14.8%. Of the 338 patients, the major complications were one deep vein thrombosis, four deep infections, and one re-rupture [17] (Table 5).
The tendon of the peroneus brevis (PB) is well vascularized. The transfer allows the blood supply from the musculotendinous junction to be maintained, providing a robust reinforcement to the AT [38].
The two peroneal muscles contribute only 4% of the capacity for plantar flexion, while the PB tendon contributes approximately 28% of the total eversion strength [38]. Intuitively, the use of the PB tendon may cause a strength deficit in eversion of the ankle and not affect plantar flexion [30]. The peroneus longus is the major evertor of the hindfoot, and it may take over some of the functions of the PB, reducing subjective weakness in ankle function after PB tendon transfer [39]. Human cadaveric models have been used to assess the mechanical properties of AT reconstruction with the PB and FHL [40]. The outcomes were similar in terms of stiffness (16.5 ± 6.3 N/mm (PB) vs. 14.0 ± 3.8 N/mm (FHL)), energy to failure (3656.0 ± 2720.3 J (PB) vs. 2406.7 ± 1621.8 J (FHL)), and mode of failure. The force to failure of the PB tendon transfer was higher compared to the FHL (348.8 ± 124.9 N (PB) vs. 241.5 ±8 2.2 N (FHL)), and this difference was statistically significant, although it may not be clinically relevant. The authors of [40] reported good clinical results in the use of PB, with a final ATRS of 92.5 associated with a low rate of complications. In fact, patients did not experience deep vein thrombosis nor re-rupture, and five superficial infections were managed with oral antibiotics [8].
The present systematic review reported a rate of complications in the use of PB tendon transfer of 7% in 128 patients, five of whom experienced superficial infections and four wound complications (Table 5). Due to the lack of relevant data, it was not possible to directly compare the complications of FHL and PB or to analyse which surgical technique leads to a higher rate of complications.
The return to daily activities and the return to sport were only reported in three and four studies, respectively; seventy-nine and ninety-nine patients were evaluated; patients were able to return to daily activities in 13.7 weeks and return to sport in 19.6 weeks. Maffulli et al. reported a slower return to sport in PB tendon transfer patients compared to FHL transfer patients, but a higher percentage of PB transfer patients eventually returned to sport compared to FHL transfer patients [25].
The use of flexor digitorum longus (FDL) tendon transfer has been described in two reports; however, these were excluded since they described its use in the management of Achilles tendinopathy. The FDL tendon transfer is an alternative operative technique that keeps the FHL tendon intact, preserves push-off strength, and minimizes gait disturbances [10]. However, De Cesar Netto et al. reported a patient with weakness of plantar flexion of the lesser toes, without balance or gait disturbances [10]. In addition to the transfer of the tendon of the FDL, they also performed a turndown of the central third of the proximal aspect of the AT or a hamstring allograft reconstruction [10].
The peroneal longus (PL) tendon has a stronger failure load than the tendon of the PB [11]. However, the use of the PL tendon may cause a long-lasting strength deficit in eversion of the ankle, especially at a higher angular velocity, more evident than in the transfer of the PB [38].
This study has several limitations. First, the retrospective design and the lack of blinding in most of the included studies. Given the lack of quantitative data available for inclusion, it was not possible to analyze the results of each transfer separately. Moreover, we excluded several studies because most of them did not separate data on patients with chronic AT rupture from patients with Achilles tendinopathy and acute AT rupture, while others did not differentiate mid-portion ruptures from ruptures of the insertion of the AT. Furthermore, the inhomogeneity of the evaluation scales prevents an adequate comparison between the studies. Given the lack of relevant quantitative data, further subgroup analyses were not possible. Further investigations are required to validate the results of the present study in a clinical setting.
5. Conclusions
The use of local tendon transfer for chronic Achilles tendon ruptures using the FHL or PB tendon showed good clinical outcomes and allowed a reliable return to daily activities and sports. Better-quality future studies are needed to ascertain which surgical procedures are most advantageous for these patients.
Abbreviations
| AOFAS | American Orthopaedic Foot and Ankle Society |
| AT | Achilles tendon |
| ATRS | Achilles tendon Total Rupture Score |
| BMI | Body Mass Index |
| CMS | Coleman Methodology Score |
| FDL | flexor digitorum longus |
| FHL | flexor hallucis longus |
| IBM SPSS | International Business Machines Statistical Package for the Social Sciences |
| PB | peroneus brevis |
| PICOT | Problem, Intervention, Comparison, Outcomes, Timing |
| PL | peroneous longus |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROMs | patient-reported outcome measures |
| VAS | Visual Analogue Scale |
Author Contributions
Conceptualization, writing—revision and final approval, N.M.; writing—revision and final approval, S.Z.; writing—revision and final approval, G.M.; interpretation of results and final approval, F.M.; conceptualization, revision, and final approval, F.O. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Maffulli N. Rupture of the Achilles tendon. J. Bone Jt. Surg. Am. 1999;81:1019–1036. doi: 10.2106/00004623-199907000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Viidik A. Tensile strength properties of Achilles tendon systems in trained and untrained rabbits. Acta Orthop. Scand. 1969;40:261–272. doi: 10.3109/17453676908989506. [DOI] [PubMed] [Google Scholar]
- 3.Hahn F., Meyer P., Maiwald C., Zanetti M., Vienne P. Treatment of chronic achilles tendinopathy and ruptures with flexor hallucis tendon transfer: Clinical outcome and MRI findings. Foot Ankle Int. 2008;29:794–802. doi: 10.3113/FAI.2008.0794. [DOI] [PubMed] [Google Scholar]
- 4.Yassin M., Gupta V., Martins A., Mahadevan D., Bhatia M. Patient reported outcomes and satisfaction following single incision Flexor Hallucis Longus (FHL) augmentation for chronic Achilles tendon pathologies. J. Clin. Orthop. Trauma. 2021;23:101650. doi: 10.1016/j.jcot.2021.101650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wegrzyn J., Luciani J.F., Philippot R., Brunet-Guedj E., Moyen B., Besse J.L. Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int. Orthop. 2010;34:1187–1192. doi: 10.1007/s00264-009-0859-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansen S.T. Trauma to the heel cord. Disorders of the Foot and Ankle. Med. Surg. Manag. 1991;2:2355–2360. [Google Scholar]
- 7.Perez Teuffer A. Traumatic rupture of the Achilles Tendon. Reconstruction by transplant and graft using the lateral peroneus brevis. Orthop. Clin. N. Am. 1974;5:89–93. [PubMed] [Google Scholar]
- 8.Maffulli N., Spiezia F., Longo U.G., Denaro V. Less-invasive reconstruction of chronic achilles tendon ruptures using a peroneus brevis tendon transfer. Am. J. Sports Med. 2010;38:2304–2312. doi: 10.1177/0363546510376619. [DOI] [PubMed] [Google Scholar]
- 9.Mann R.A., Holmes G.B., Jr., Seale K.S., Collins D.N. Chronic rupture of the Achilles tendon: A new technique of repair. J. Bone Jt. Surg. Am. 1991;73:214–219. doi: 10.2106/00004623-199173020-00009. [DOI] [PubMed] [Google Scholar]
- 10.de Cesar Netto C., Chinanuvathana A., Fonseca L.F.D., Dein E.J., Tan E.W., Schon L.C. Outcomes of flexor digitorum longus (FDL) tendon transfer in the treatment of Achilles tendon disorders. Foot Ankle Surg. 2019;25:303–309. doi: 10.1016/j.fas.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Wang C.C., Lin L.C., Hsu C.K., Shen P.H., Lien S.B., Hwa S.Y., Pan R.Y., Lee C.H. Anatomic reconstruction of neglected Achilles tendon rupture with autogenous peroneal longus tendon by EndoButton fixation. J. Trauma. 2009;67:1109–1112. doi: 10.1097/TA.0b013e3181a73f02. [DOI] [PubMed] [Google Scholar]
- 12.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coleman B.D., Khan K.M., Maffulli N., Cook J.L., Wark J.D. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Scand. J. Med. Sci. Sport. Rev. Artic. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 14.Abubeih H., Khaled M., Saleh W.R., Said G.Z. Flexor hallucis longus transfer clinical outcome through a single incision for chronic Achilles tendon rupture. Int. Orthop. 2018;42:2699–2704. doi: 10.1007/s00264-018-3976-x. [DOI] [PubMed] [Google Scholar]
- 15.Ahn J., Jeong B.O. Return to Sports Activities after Flexor Hallucis Longus Transfer for Neglected Achilles Tendon Rupture. J. Foot Ankle Surg. 2022;61:1263–1266. doi: 10.1053/j.jfas.2022.02.015. [DOI] [PubMed] [Google Scholar]
- 16.Alauddin M., Hossain M.Z., Rahman M.M., Roy M.K., Minto M.R., Islam M.A., Islam M.K., Islam M.S., Saha M.K., Mahmud A.A., et al. Management of Neglected Rupture of Tendoachilles with Long Gap by Flexor Hallucis Longus Tendon Transfer. Mymensingh Med. J. 2022;31:861–868. [PubMed] [Google Scholar]
- 17.Alhaug O.K., Berdal G., Husebye E.E., Hvaal K. Flexor hallucis longus tendon transfer for chronic Achilles tendon rupture. A retrospective study. Foot Ankle Surg. 2019;25:630–635. doi: 10.1016/j.fas.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Elias I., Besser M., Nazarian L.N., Raikin S.M. Reconstruction for missed or neglected Achilles tendon rupture with V-Y lengthening and flexor hallucis longus tendon transfer through one incision. Foot Ankle Int. 2007;28:1238–1248. doi: 10.3113/FAI.2007.1238. [DOI] [PubMed] [Google Scholar]
- 19.Khalid M.A., Weiss W.M., Iloanya M., Panchbhavi V.K. Dual Purpose Use of Flexor Hallucis Longus Tendon for Management of Chronic Achilles Tendon Ruptures. Foot Ankle Spec. 2019;12:345–349. doi: 10.1177/1938640018803695. [DOI] [PubMed] [Google Scholar]
- 20.Koh D., Lim J., Chen J.Y., Singh I.R., Koo K. Flexor hallucis longus transfer versus turndown flaps augmented with flexor hallucis longus transfer in the repair of chronic Achilles tendon rupture. Foot Ankle Surg. 2019;25:221–225. doi: 10.1016/j.fas.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 21.Lever C.J., Bosman H.A., Robinson A.H.N. The functional and dynamometer-tested results of transtendinous flexor hallucis longus transfer for neglected ruptures of the Achilles tendon at six years’ follow-up. Bone Jt. J. 2018;100:584–589. doi: 10.1302/0301-620X.100B5.BJJ-2017-1053.R1. [DOI] [PubMed] [Google Scholar]
- 22.Lui T.H. Treatment of chronic noninsertional Achilles tendinopathy with endoscopic Achilles tendon debridement and flexor hallucis longus transfer. Foot Ankle Spec. 2012;5:195–200. doi: 10.1177/1938640011434508. [DOI] [PubMed] [Google Scholar]
- 23.Maffulli N., Spiezia F., Pintore E., Longo U.G., Testa V., Capasso G., Denaro V. Peroneus brevis tendon transfer for reconstruction of chronic tears of the Achilles tendon: A long-term follow-up study. J. Bone Jt. Surg. Am. 2012;94:901–905. doi: 10.2106/JBJS.K.00200. [DOI] [PubMed] [Google Scholar]
- 24.Maffulli N., Oliva F., Costa V., Del Buono A. The management of chronic rupture of the Achilles tendon: Minimally invasive peroneus brevis tendon transfer. Bone Jt. J. 2015;97:353–357. doi: 10.1302/0301-620X.97B3.33732. [DOI] [PubMed] [Google Scholar]
- 25.Maffulli N., Oliva F., Maffulli G.D., Buono A.D., Gougoulias N. Surgical management of chronic Achilles tendon ruptures using less invasive techniques. Foot Ankle Surg. 2018;24:164–170. doi: 10.1016/j.fas.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 26.Mahajan R.H., Dalal R.B. Flexor hallucis longus tendon transfer for reconstruction of chronically ruptured Achilles tendons. J. Orthop. Surg. 2009;17:194–198. doi: 10.1177/230949900901700215. [DOI] [PubMed] [Google Scholar]
- 27.Miao X., Wu Y., Tao H., Yang D., Huang L. Reconstruction of Kuwada grade IV chronic achilles tendon rupture by minimally invasive technique. Indian J. Orthop. 2016;50:523–528. doi: 10.4103/0019-5413.189599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oksanen M.M., Haapasalo H.H., Elo P.P., Laine H.J. Hypertrophy of the flexor hallucis longus muscle after tendon transfer in patients with chronic Achilles tendon rupture. Foot Ankle Surg. 2014;20:253–257. doi: 10.1016/j.fas.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Ozer H., Ergisi Y., Harput G., Senol M.S., Baltaci G. Short-Term Results of Flexor Hallucis Longus Transfer in Delayed and Neglected Achilles Tendon Repair. J. Foot Ankle Surg. 2018;57:1042–1047. doi: 10.1053/j.jfas.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 30.Pintore E., Barra V., Pintore R., Maffulli N. Peroneus brevis tendon transfer in neglected tears of the Achilles tendon. J. Trauma. 2001;50:71–78. doi: 10.1097/00005373-200101000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Singh A., Nag K., Roy S.P., Gupta R.C., Gulati V., Agrawal N. Repair of Achilles tendon ruptures with peroneus brevis tendon augmentation. J. Orthop. Surg. 2014;22:52–55. doi: 10.1177/230949901402200114. [DOI] [PubMed] [Google Scholar]
- 32.Tay D., Lin H.A., Tan B.S., Chong K.W., Rikhraj I.S. Chronic Achilles tendon rupture treated with two turndown flaps and flexor hallucis longus augmentation—Two-year clinical outcome. Ann. Acad. Med. Singap. 2010;39:58–60. doi: 10.47102/annals-acadmedsg.V39N1p58. [DOI] [PubMed] [Google Scholar]
- 33.Vega J., Vilá J., Batista J., Malagelada F., Dalmau-Pastor M. Endoscopic Flexor Hallucis Longus Transfer for Chronic Noninsertional Achilles Tendon Rupture. Foot Ankle Int. 2018;39:1464–1472. doi: 10.1177/1071100718793172. [DOI] [PubMed] [Google Scholar]
- 34.Yeoman T.F., Brown M.J., Pillai A. Early post-operative results of neglected tendo-Achilles rupture reconstruction using short flexor hallucis longus tendon transfer: A prospective review. Foot. 2012;22:219–223. doi: 10.1016/j.foot.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 35.Delgado D.A., Lambert B.S., Boutris N., McCulloch P.C., Robbins A.B., Moreno M.R., Harris J.D. Validation of Digital Visual Analog Scale Pain Scoring with a Traditional Paper-based Visual Analog Scale in Adults. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018;2:e088. doi: 10.5435/JAAOSGlobal-D-17-00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kitaoka H.B., Alexander I.J., Adelaar R.S., Nunley J.A., Myerson M.S., Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 37.Nilsson-Helander K., Thomeé R., Silbernagel K.G., Thomeé P., Faxén E., Eriksson B.I., Karlsson J. The Achilles tendon Total Rupture Score (ATRS): Development and validation. Am. J. Sports Med. 2007;35:421–426. doi: 10.1177/0363546506294856. [DOI] [PubMed] [Google Scholar]
- 38.Clarke H.D., Kitaoka H.B., Ehman R.L. Peroneal tendon injuries. Foot Ankle Int. 1998;19:280–288. doi: 10.1177/107110079801900503. [DOI] [PubMed] [Google Scholar]
- 39.Gallant G.G., Massie C., Turco V.J. Assessment of eversion and plantar flexion strength after repair of Achilles tendon rupture using peroneus brevis tendon transfer. Am. J. Orthop. 1995;24:257–261. [PubMed] [Google Scholar]
- 40.Sebastian H., Datta B., Maffulli N., Neil M., Walsh W.R. Mechanical properties of reconstructed achilles tendon with transfer of peroneus brevis or flexor hallucis longus tendon. J. Foot Ankle Surg. 2007;46:424–428. doi: 10.1053/j.jfas.2007.07.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.