Abstract
The glycosides of two flavonoids, naringin and naringenin, are found in various citrus fruits, bergamots, tomatoes, and other fruits. These phytochemicals are associated with multiple biological functions, including neuroprotective, antioxidant, anticancer, antiviral, antibacterial, anti-inflammatory, antiadipogenic, and cardioprotective effects. The higher glutathione/oxidized glutathione ratio in 3-NP-induced rats is attributed to the ability of naringin to reduce hydroxyl radical, hydroperoxide, and nitrite. However, although progress has been made in treating these diseases, there are still global concerns about how to obtain a solution. Thus, natural compounds can provide a promising strategy for treating many neurological conditions. Possible therapeutics for neurodegenerative disorders include naringin and naringenin polyphenols. New experimental evidence shows that these polyphenols exert a wide range of pharmacological activity; particular attention was paid to neurodegenerative diseases such as Alzheimer’s and Parkinson’s diseases, as well as other neurological conditions such as anxiety, depression, schizophrenia, and chronic hyperglycemic peripheral neuropathy. Several preliminary investigations have shown promising evidence of neuroprotection. The main objective of this review was to reflect on developments in understanding the molecular mechanisms underlying the development of naringin and naringenin as potential neuroprotective medications. Furthermore, the configuration relationships between naringin and naringenin are discussed, as well as their plant sources and extraction methods.
Keywords: naringin, naringenin, polyphenols, neurological disease, dietary interventions
1. Introduction
The term “neurological disease” is often used to refer to anything that affects the nervous system. In the brain, spinal cord, or other nerves, structural, metabolic, or electrical dysfunctions may cause a broad range of symptoms. These symptoms include altered states of consciousness, convulsions, muscular weakness, poor coordination, a loss of feeling, and a lack of sensation. Other symptoms include disorientation, pain, and discomfort. Extensive study has led to the discovery of several neurological abnormalities, some of which are somewhat common while others are relatively uncommon [1,2]. Some of these problems are inherited while others are not. Neurology and clinical neuropsychology can identify and treat these illnesses using the appropriate diagnostic and therapeutic methods. Although encased in the skull and spinal vertebrae and chemically isolated by the blood–brain barrier, the brain and spinal cord are susceptible organs [3]. Because of their placement just beneath the epidermis, nerves are nevertheless vulnerable to harm despite the protective layers of tissue around them. Individual neurons and the neural circuits and nerves they form are susceptible to damage to their electrical and structural integrity [4].
Phytochemicals may be broken down into several different classes, such as flavanols, flavan-3-ols, isoflavones, flavanones, anthocyanidins, and flavones [5]. It has been shown that flavonoids promote apoptosis and decrease metastasis, angiogenesis, and proliferation in the setting of carcinogenesis by interfering with various cell signaling pathways. The flavanone-7-O-glycoside naringin is found in many plants, while citrus fruits are the most common place to find it. A flavanone called naringenin is its main component [6,7]. Many different signaling pathways and signaling molecules are affected by this chemical. Its pharmacological properties include but are not limited to an antioxidant, an anti-inflammatory, an anti-apoptotic, an anti-tumor, and an anti-viral, as well as effects on metabolic syndrome, bone regeneration, neurological illnesses, cardiovascular disease, and genetic damage [8]. Naringin may cause drug interactions due to its ability to inhibit cytochrome P450 enzymes, including CYP3A4 and CYP1A2 [9].
Neurological disorders may be alleviated with the help of naringenin (4′,5,7-trihydroxy flavanone), a flavonoid abundant in the peels of citrus fruits (particularly grapes and tomatoes) [10]. Among the top dietary sources of this noteworthy flavonoid are grapefruits and oranges. A few of the many medical advantages of this drug include preventing or reversing weight gain, enhancing metabolic health, and restoring typical lipid profiles in patients with dyslipidemia [11]. Among naringenin’s many biological properties is an antioxidant effect. It has been shown that they may help with pain, inflammation, kidney health, and even nerve function. Research has revealed that naringenin may help reduce pain and inflammation associated with several medical disorders [12]. Mechanistically, naringenin is a pleiotropic molecule that inhibits leukocyte recruitment, pro-inflammatory cytokine release, and cytokine-induced analgesia by modulating transient receptor potential (TRP) channels and triggering the nitric oxide (NO)/cyclic guanosine monophosphate (cGMP)/protein kinase G(PKG)/adenosine triphosphate (ATP The compound’s low bioavailability and limited brain access are significant roadblocks to broader use despite naringenin’s promise in treating neurological diseases [13,14]. The therapeutic potential of naringin and naringenin for various symptoms related to neurological diseases has been shown by encouraging results from preclinical investigations [15].
The principal objective of this review was to report on the progress made toward understanding the molecular mechanisms behind the development of naringin and naringenin as potential neuroprotective therapeutics. Additionally, the configuration links between naringin and naringenin, as well as their plant sources and extraction methods, are described.
2. Methodology
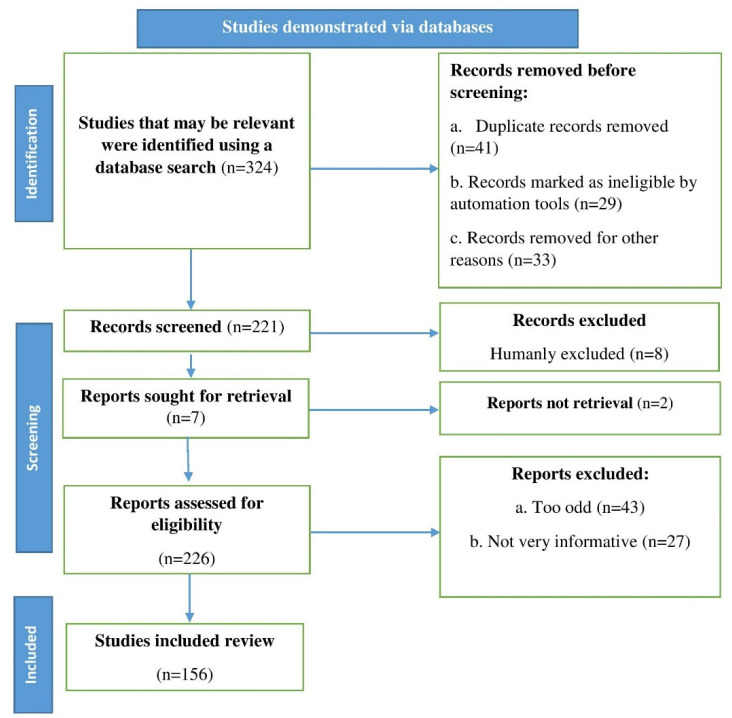
The keywords naringin and naringenin, neurological diseases, botanical sources, and neuroprotective action were used to search the following databases: PubMed, Scopus, and Web of Science. Up to 2022, English-language research reports, reviews, and original research articles were considered and studied. An algorithm was used that followed the flowchart in Figure 1 and had all of the steps and requirements for choosing the required literature, in accordance with the recommendations of Page et al. [16].
Figure 1.
Flowchart depicting the steps to be followed when selecting published data for the current study; n stands for the number of literature reports.
3. Naringin and Naringenin
The flavanone naringenin and the glycosylated derivative naringin are in high concentrations in grapefruit and other citrus fruits. The antioxidant and anti-inflammatory properties of flavonoids have gained widespread recognition [17]. When naringenin is added to SH-SY5Y cells or when 6-OHDA is injected into mice, the cells are protected in an Nrf2-dependent manner, just like the dopaminergic neurons [18]. This is due to the complete elimination of protective effects and expression of Nrf2-dependent cytoprotective genes after treatment with Nrf2 short interfering RNA [19]. Naringenin prevented rotenone-induced structural alterations in muscle and motor impairment in rat models when given after the administration of the medication. The expression of DJ-1 and chaperone-associated E3 ligase was increased in the striatum and SN after treatment with naringenin [20]. Target proteins are ubiquitinated by DJ-1 and a chaperone-associated E3 ligase and then sent on to be degraded by the proteasome. In a rotenone model of Parkinson’s disease, naringenin was found to have neuroprotective effects [21,22]. Naringin may aid dopaminergic neuron recovery after injury if given soon after the damage occurs. Dopaminergic neurons were preserved, GDNF levels in the SN were restored, and the number of ionized calcium-binding adaptor molecule 1 (Iba-1) and tumor necrosis factor-alpha (TNF-α) immunoreactive neurons in the striatum were reduced after pretreatment with naringin in rats with a unilateral MPP+-lesion. Eukaryotic initiation factor 4E-binding protein 1 (4E-BP1) and growth differentiation and neurotrophic factor (GDNF) were upregulated in the SN after a single injection of naringin [23].
On top of that, it is an effective antioxidant. During fasting and stimulated states, rapid glucose uptake is impaired in BC. Insulin stimulates phosphoinositide 3-kinase PIP3/Akt and mitogen-activated protein kinase (MAPK) activity, and naringenin prevents this MAPK. It decreases TNF-α and COX-2 levels and raises the transcription factor Nrf2 [24,25].
4. Botanical Sources
Flavonoids are phenolic compounds associated with a wide range of biological functions. There are more than 4000 different flavonoids known to science, most of which are found in their natural, unaltered plant-based forms. Flavonoids can be a dietary supplement [26,27]. Grapefruit and other citrus fruits get their distinctive bitter taste from flavonoid naringin. Although the number of flavonoids taken from food may be large and the flavonoids exhibit potential biological action, they have attracted significantly less attention than flavanols and isoflavones [28,29].
In most cases, the researchers focused on flavanols and isoflavones—intracellular cycling of naringenin, hesperidin, and its glycosylated derivatives, naringenin, hesperidin, and rutin. Grapefruit, bergamot, sour orange, tart cherry, tomato, chocolate, Greek oregano, water mint, and beans are all foods and plants that contain norepinephrine or its glycosides [29,30].
5. Neuroprotective Action
5.1. Alzheimer’s Disease
Alzheimer’s disease (AD) is the most common type of dementia in the industrialized world and is a severe public health problem [31]. Several different molecular processes caused AD, but its exact pathophysiology is still poorly understood. In several pre-clinical studies, naringin and some of its derivatives, such as naringenin, changed these pathways in ways that could be used to treat AD [32,33]. The disease is caused by the death of cholinergic neurons in the frontal lobe and the formation of Amyloid-β (Aβ) plaques outside the body [34].
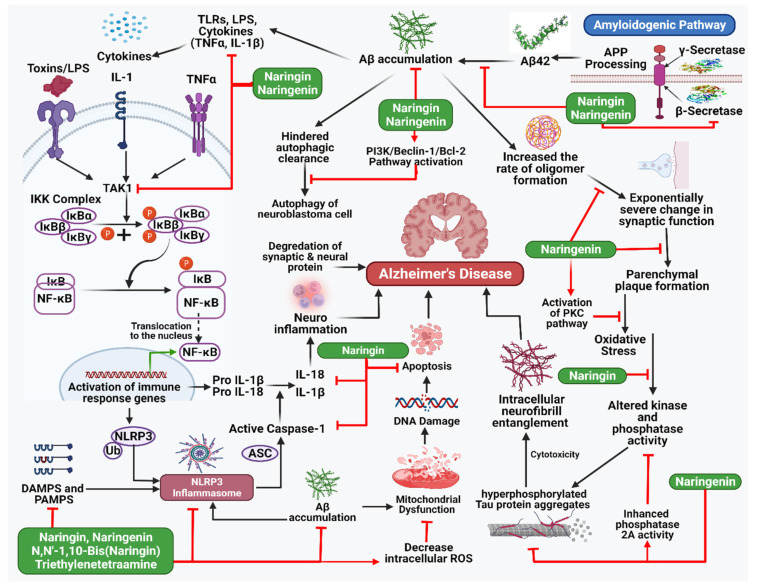
Memantine, an antagonist of the NMDA glutamate receptor, breaks down at a much slower rate than acetylcholinesterase (AChE) inhibitors, such as donepezil aricept, which is often used to treat the symptoms of AD [35,36]. Synaptic dysfunction, in which synapses are damaged, cells are killed, and mental impairments occur, results from consuming too much. This dysfunction can be fixed entirely with the proper treatment. It is essential to understand how Aβ is currently in charge of producing and storing memories and how this affects synaptic plasticity in the brain network. Evidence suggests that calcium/calmodulin-dependent protein kinase II (CaMKII) is a critical synaptic target for Aβ-induced synaptic depression [37,38]. Several plant species high in flavonoids have been used in traditional medicine for hundreds of years. Epidemiological and dietary studies on both people and animals have shown that these flavonoids protect against and slow down neurodegeneration, especially regarding the cognitive decline that accompanies aging [39]. The flavonoid glycoside naringin, found in citrus fruits in large amounts, is effective against many diseases and conditions, such as cancer, inflammation, ulcers, osteoporosis, and apoptosis. Naringin has been shown to improve behavior and thinking in animal models of epilepsy caused by kainic acid and Huntington’s disease caused by 3-nitropropionic acid [40]. The effects of colchicine and D-galactose on learning and memory are also undone by treatment with naringin. Naringenin has been shown to improve insulin signaling and cognitive ability in the brain and reduce the effects of intracerebroventricular-streptozotocin on neurodegeneration caused by AD (Table 1 and Figure 2) [41].
Figure 2.
Illustration representing the site of action of naringin and naringenin in Alzheimer’s disease pathway.
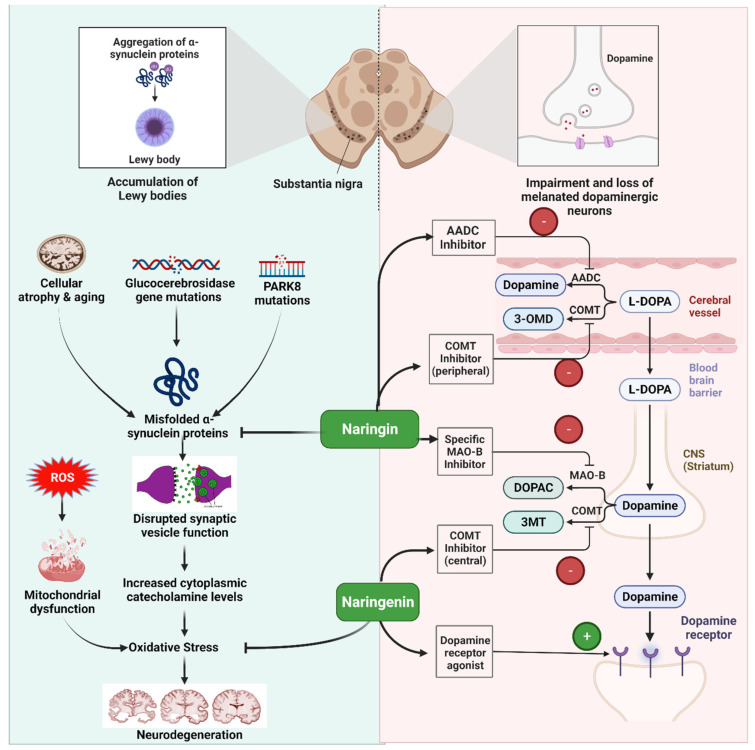
5.2. Parkinson’s Disease
Parkinson’s disease (PD) is a degenerative neurological disease that results in impaired motor function due to dopaminergic neuropathy in the substantia nigra [42,43,44]. Genetic predisposition may play a role in developing mitochondrial damage and oxidative stress; however, additional molecular routes exist. In recent years, oxidative stress has been investigated as a potential mechanism in neurodegeneration, which is only one example of many similarities between AD and PD. The antioxidant properties of flavonoids, alkaloids, and other polyphenols are coming to the fore. Plant chemicals may modulate enzymes and metabolic signaling pathways to reduce ROS production. Bioactive metabolite flavonoids have anti-oxidative actions on the liver’s metabolic pathway [45,46,47].
The antioxidant and neuroprotective properties of naringin have been studied. Asahina and Inubuse found the blueprints for naringin in 1928 [48,49]. Naringenin is linked to naringin through the C-7 hydroxyl group. Metabolites of naringenin may be found in phases I and II of the drug’s metabolism. Glucose is the source of naringin’s bitter flavor. It reacts with potassium hydroxide or other essential substances to form 1,3-diphenylpropan-1-one, which has a scent reminiscent of menthol [50,51,52]. It has been shown that naringin may neutralize ROS, scavenge superoxide, suppress xanthine oxide, decrease lipid peroxidation, and decrease the permeability of oxygen-stimulated K+ erythrocytes. Naringin’s antioxidant potentials may aid in treating neurology and diabetes. Degeneration of nerve cells in the striatum and substantia nigra pars compacta kills dopamine-producing brain cells, leading to Parkinson’s disease (Table 1 and Figure 3) [53]. Neurons in the substantia nigra are affected as microglia are activated, and protein clumps form. Causes of neurodegeneration include oxidative stress, dopamine depletion, and neuroinflammation. In addition to boosting dopamine, naringenin also reduces inflammation [54]. By activating Nrf2/ARE and its downstream target genes, including HO-1 and glutathione cysteine ligase regulatory subunit, naringenin protects mice against 6-hydroxydopamine-induced dopaminergic neurodegeneration and oxidative damage. By inhibiting and caspase 3, naringenin was able to prevent apoptosis. Grapefruit suppresses CYP3A4 much more so than naringin. With less naringin than grapefruit juice, orange juice also stops CYP3A4. Preclinical tests have shown that naringin is not transformed into naringenin in cultivated cells [55,56,57].
Table 1.
Preclinical findings on the use of naringin and naringenin polyphenols in neurological disorders.
| Disease | Compound | Dose/Conc. | Study Model | Findings | References |
|---|---|---|---|---|---|
| Alzheimer Disease | Naringin | 50, 100 and 200 mg/kg; PO) for twentyone days | ICV-STZ rats | Restoration of cognitive deficits in ICV-STZ rat along with mitigation of mitochondrial dysfunction mediated oxido-nitrosative stress and cytokine release | [58] |
| Naringin | 50 or 100 mg/kg/day | APPswe/PSΔE9 transgenic mice | Reduction in plaque burden and an increase in glucose uptake through the inhibition of GSK-3β activity | [59] | |
| Naringin | 40 and 80 mg/kg | Wistar rats | Protection against ICV β-A1–42 and intranasal manganese induced memory dysfunction possibly due to its antioxidant, anti-inflammatory, anti-amyloidogenesis | [60] | |
| Naringin | 100 mg/kg/day | Mice | Neuroprotective effects through a variety of mechanisms, including amyloid β metabolism, Tau protein hyperphosphorylation, acetyl cholinergic system, glutamate receptor system, oxidative stress and cell apoptosis | [61] | |
| Naringenin | 70–210 µg/mL | PC12 cells | Inhibition of AChE activity | [62] | |
| Naringenin | 50 mg/kg | Male albino Wistar rats | Reduced oxidative stress markers: 4-HNE, MDA, TBARS, H2O2, PC, GSH in the hippocampus; Increase antioxidant level: GPx, GR, GST, SOD, CAT and Na+/K+-ATPase in the hippocampus | [63] | |
| Naringenin | 25, 50 and 100 mg/kg | Male Sprague-Dawley rats | Increased the mRNA expression of INS and INSR in cerebral cortex and hippocampus. In addition, NAR reversed ICV-STZ induced Tau hyper-phosphorylation in both hippocampus and cerebral cortex through downregulation of GSK-3β activity | [41] | |
| Naringenin | 25, 50 and 100 μM and 1.5, 3.0 and 4.5 mg/kg | PC12 cells and male ICR mice | Decreased ROS level and LDH activity | [64] | |
| Naringenin | 25 and 50 mg/kg | Male Sprague-Dawley rats | Decreased oxidative stress by depleting elevated lipid peroxide and nitric oxide and elevating reduced glutathione levels and exert cholinergic function through the inhibition of elevated ChE activity | [65] | |
| Naringin dihydrochalcone | 100 mg/kg | APPswe/PS1ΔE9 (APP/PS1) transgenic mice | Reduction in amyloid plaque burden and Aβ levels, suppression of neuroinflammation and promotion of neurogenesis | [66] | |
| Naringin | 40 and 80 mg/kg, PO | Male Wistar rats | Improvement in the cognitive performance and attenuated oxidative damage, as evidenced by lowering of malondialdehyde level and nitrite concentration and restoration of superoxide dismutase, catalase, glutathione S-transferase, and reduced glutathione levels, and acetylcholinesterase activity | [67] | |
| Naringin | 30 or 60 mg/kg/day | NMRI male mice | Reduction of Aβ plaque numbers in CA1, CA3, and DG areas of the hippocampus | [68] | |
| Naringin | 25, 50 and 100 mg/kg PO | Westar rats | Reduced lipid peroxidation, restored reduced superoxide dismutase and catalase) and acetylcholine esterase activity were significantly decreased | [69] | |
| N,N′-1,10-Bis(Naringin) Triethylenetetraamine | 10–200 μM | PC12 cells | Deceased the level of ROS in Cu2+-Aβ1-42-treated PC12 cells and elevate the SOD activity in Cu2+-Aβ1-42-treated PC12 cells | [70] | |
| Naringin | 2.5, 5 and 10 mg/kg | Swiss mice | Increased the activities of superoxide dismutase and catalase, and glutathione and decreased malondialdehyde and nitrite contents, and reduced brain acetylcholinesterase activity in mice brains | [71] | |
| Naringin | 80 mg/kg | Wistar albino rats | Improvement of the Aβ-induced cholinergic dysfunction and increase in the activity of AChE in rat hippocampus, prefrontal cortex, and amygdala. Furthermore, naringin attenuated Aβ-induced decrease in mitochondrial function, integrity, and bioenergetics as well as mitochondrial and cytosolic calcium level in all the brain regions. Moreover, reversal of Aβ-induced increase in apoptosis and level of mitochondrial calcium uniporter and decrease in the level of hemeoxygenase-1 | [72] | |
| Naringenin | 100 mg/kg, orally | male Wistar rats | Lowered hippocampal MDA content | [73] | |
| Parkinson Disease | Naringin | 80 mg/kg | rat model | Protection of the nigrostriatal DA projection by increasing glial cell line-derived neurotrophic factor expression and decreasing TNF-a expression in DA neurons and microglia |
[74] |
| Naringin | 8 or 80 mg/kg per day | Female Sprague Dawley (SD) rats | Increased the level of GDNF in DA neurons, contributing to neuroprotection in the MPP+ rat model of PD, with activation of mammalian target of rapamycin complex 1 and pre-treatment with naringin could attenuate the level of TNF-α in the substantia nigra of MPP+-treated brains | [75] | |
| Naringin | 80 mg/kg | male Wistar albino rats | Neuroprotective activity against rotenone-induced toxicity in the animals possibly through Nrf2-mediated pathway | [76] | |
| Naringin | 50, 100 and 200 mg/kg | Swiss albino mice | Reduction in haloperidol-induced cataleptic scores in both bar test and block test | [77] | |
| Naringenin | 25, 50, 100 mg/kg/b.w, PO | male C57BL/6J mice | Reversed the toxic effects of MPTP by reducing LPO levels and increasing the activities of glutathione reductase and catalase along with improved behavioral performance | [78] | |
| Naringenin | 50 mg/kg, orally | albino Wister rats | Improved oxidative stress status by decreasing MDA and increasing glutathione content | [79] | |
| Naringenin | 50, 100 mg/kg | male Sprague-Dawley rats BV-2 and MN9D cell lines |
Inhibition of microglia-induced neuroinflammation via NLRP3 inflammasome inactivation | [80] | |
| Naringenin | 25, 50, and 100 mM | SH-SY5Y Cell Line | Reduction of the ROS production by decreasing oxidative stress markers such as LPO and NO and increasing SOD level. In addition, pretreatment with NGN decreased the inflammatory markers such as TNF-α and NF-κβ in MPP+-treated SH-SY5Y cells. Further, NGN decreased the pro-apoptotic marker—Bax—and increased the anti-apoptotic marker—Bcl-2—in MPP+-induced SH-SY5Y cells | [81] | |
| Naringenin | 40 μM | Primary rat mesencephalic cultures | Decreased TH-positive neurons and TUNEL positive neurons | [82] | |
| Naringenin | 50 mg/kg | Male Sprague-Dawley rats | Restoration of dopamine concentrations due to neuroprotective effects rather than compensatory effects by remaining TH-positive cells after 6-OHDA lesioning | [83] | |
| Naringenin | 20, 40 and 80 mM (in vitro) 70 mg/kg, orally (in vivo) | Human neuroblastoma SH-SY5Y cells and male C57BL/6 mice | Activated Nrf2/ARE pathway in dopaminergic (in vitro) Up regulated protein levels of Nrf2/ARE genes (in vivo) Reduced striatal oxidative stress and subsequent apoptotic signalling cascades in striatum (in vivo) |
[84] | |
| Naringenin | 12.5 μM and 25 μM | SH-SY5Y Human Neuroblastoma cell line | Downregulation of the expression of some Parkinsonian genes such as casp9, lrrk2, and polg and upregulate pink1 | [85] | |
| Naringenin | 25, 50, and 100 mg/ kg/p.o | Male C57BL/6J mice | Reduced NO content and restored SOD activity, also downregulated TNF-α and IL-1β expression | [86] | |
| Naringenin | 10 and 50 µM | Female Wistar rats | Enhanced astroglial neurotrophic effects on DA neurons through the regulation of Nrf2 activation, | [87] | |
| Anxiety and depression | Naringenin | 5, 10 and 20 mg/kg | Male ICR mice | Increased hippocampal 5-HT, NE and GR levels, and reduced serum corticosterone levels | [88] |
| Naringenin | 5, 10 and 20 mg/kg | Male ICR mice | Up-regulation of BDNF | [89] | |
| Naringenin | 10, 25 and 50 mg/kg | Swiss mice | Naringenin (25–50 mg/ kg) ameliorated the hypolocomotion, depressive- and anxiety-like behaviors in hypoxic mice Naringenin (10 mg/kg) increases BDNF expression but did not significantly (p < 0.05) alter corticosterone and catalase contents. The increased expressions of iNOS and NF-kB as well as loss of amygdala neuronal cells were reduced by naringenin (10 mg/kg) |
[90] | |
| Naringin | 10 mg/kg | Adult male Swiss mice | Alleviation of the depressive and anxiogenic behaviors evidenced by the increased preference to sucrose and open arm entries and duration in SPT and EPM respectively | [91] | |
| Naringin | 25–100 mg/kg, i.p | Swiss mice | Increased the levels of GAD67, glutathione and decrease AChE activities, pro-inflammatory cytokines (TNF-α, IL-6), malondialdehyde, nitrite concentrations | [92] | |
| Naringenin | 50 mg/kg/day | Adult male Wistar rats | Mitigation of morphological anomalies in the hippocampal CA1 region and cortex and upregulation of BDNF, Shh, GLI1, NKX2.2, and PAX6 | [93] | |
| Huntington’s disease | Naringenin | 0.2, 0.4 mM | C3H10T1/2 cells | Suppression of the protein aggregation caused by EGFP-polyQ97 in mammalian cells. | [94] |
| Naringin | 50, 100 mg/kg | Male Wistar rats | Protection against 3-nitropropionic acid induced neurotoxicity via nitric oxide mechanism | [95] | |
| Naringenin | 50 mg/kg b.w, PO | Albino Wistar rats | Improvement of the behavioral function and restored the activity of MAO and 5-HT levels and reduction of the activation of astrocytes against 3-NP induced neurotoxicity | [96] | |
| Naringin | 40, and 80 mg/kg | Adult male Sprague-Dawley rats | Modulation of oxido-nitrosative stress, neuroinflammatory, apoptotic markers and mitochondrial complex activity | [97] | |
| Naringin | (80 mg/kg b.w/day, orally) | Male Wistar rats | Enhancement of phase II and antioxidant gene expressions via Nrf2 activation | [98] | |
| Naringin | 10 µM | PC12 cells | Modulation in expressions of B-cell lymphoma 2 and Bcl-2-associated X protein and enhancement of the nuclear translocation of Nrf2 | [99] | |
| Ischemic brain injury | Naringin | 50 and 100 mg/kg | Male Wistar rats | Restoration of reduced glutathione and catalase activity and mitochondrial enzyme activities in cortex, striatum, cerebellum | [100] |
| Naringin | 106 mg/kg/day | male C57BL/6 strain mice | Suppression of neuronal cell death, reversed the reduction in the level of phosphorylated calcium-calmodulin-dependent protein kinase II, had the tendency to reverse the reduction in the level of glutathione, and blockade of excessive activation of microglia and astrocytes | [101] | |
| Naringin | 40, 80 mg/kg | Male Sprague-Dawley rats | Improvement of early brain injury (EBI), including subarachnoid hemorrhage (SAH) severity, neurologic deficits, brain edema and blood-brain barrier integrity by attenuating SAH-induced oxidative stress and apoptosis, and reduction of the oxidative damage and apoptosis by inhibiting the activation of MAPK signaling pathway | [102] | |
| Naringenin | 50 and 100 mg/kg | Male Sprague–Dawley rats | Down-regulation of NOD2, RIP2, NF-κB, MMP-9 and up-regulation of claudin-5 expression | [103] | |
| Naringin | 80, 120, or 160 mg/kg/ day | SH-SY5Y cells | Reduced 3-nitrotyrosine formation, NADPH oxidase, and iNOS expression. Increased nNOS, p47, and p67 expression. Decreased mitophagy | [104] | |
| Naringin | 100 mg/kg/day | Adult Wistar male rats | Continual treatment increased SOD activity, decreased MDA, NO, iNOS, and IL-1β. It also improved rats’ behavioral performance | [105] | |
| Spinal cord injury |
Naringin | 20, 40 mg/kg | Female Sprague-Dawley rat | Upregulation of the expression of NKx2.2 and 2′3′-cyclic nucleotide 3′-phosphodiesterase, and inhibition of β-catenin expression and GSK-3β phosphorylation | [106] |
| Naringenin | 5, 10, 15 mM | Male Wistar rats | Suppression of MMP-9 activity and upregulation of GSH, catalase and MMP-2 activation | [107] | |
| Naringenin | 50–100 mg/kg | Female Wistar rats | Repression of miR-223 | [108] | |
| Naringin | 25, 50, and 100 mg/kg | Adult Sprague Dawley rats | Reduction of TNF-α, IL-8 as well as MDAcontent and elevation of IL-10 as well as SOD activity | [109] | |
| Chronic hyperglycemic peripheral neuropathy | Naringenin | 50, 100 and 200 mg/kg | Male Sprague Dawley rats | Inhibition of upregulated expression of TNF-α, IL-1β and MCP-1 level; GFAP and Mac-1 mRNA expression | [110] |
| Naringenin | 25 and 50 mg/kg | Male Sprague Dawley rats | Increase GSH level and decrease MDA and NO level | [111] | |
| Naringin | 50 and 100 mg/kg, b.w | Rat model of OXL- induced peripheral neuropathy |
Improved the level of superoxide dismutase, catalase, glutathione peroxidase, nuclear factor erythroid 2-related factor 2, Heme oxygenase-1, nuclear factor-κ B, tumor necrosis factor-α, interleukin-1β, Bax, Bcl-2, caspase-3, paraoxonase, mitogen-activated protein kinase 14, neuronal nitric oxide synthase (nNOS), acetylcholinesterase, and arginase 2 | [112] |
4-HNE: 4-hydroxynonenal, TBARS: Thiobarbituric reactive substances, H2O2: Hydrogen peroxide, PC: Protein carbonyl, GSH: Reduced glutathione, GPx: Glutathione peroxidase, GR: Glutathione reductase, GST: Glutathione-S-transferase, SOD: Superoxide dismutase, CAT: catalase, GSK-3β: Glycogen synthase kinase-3β, ROS: Reactive oxygen species, AchE: Acetylcholine esterase, DA: Dopaminergic, LPO: Lipid peroxidation, MPTP: 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine, 5-HT: Serotonin, NE: Norepinephrine, BDNF: brain-derived neurotrophic factor, MDA: Malondialdehyde.
Figure 3.
Illustration representing the site of action of naringin and naringenin in Parkinson’s disease.
5.3. Cerebral Ischemia
Cerebral ischemia is a disorder that may trigger a cascade of unfavorable biochemical responses in the brain, leading to malfunction of key brain regions and, commonly, neuropathy [113,114]. An inflammatory reaction and the production of ROS following an ischemia event may damage brain tissue and lead to neuronal death [115]. Ischemia-induced damage involves several kinases, including mitogen-activated protein kinases, extracellular signal-regulated kinases, signal transducers and activators of transcription 1, calcium/calmodulin-dependent kinases, etc. ROS initiate the caspase cascade and encourage the synthesis of pro-inflammatory cytokines including interleukin (IL)-1, IL-6, and tumor necrosis factor-alpha, all of which contribute to cell death. Although progress has been made, a full understanding of the molecular mechanisms behind post-ischemic neuronal damage remains elusive. However, naringin and naringenin have been shown to have a neuroprotective effect after ischemia [116,117,118,119].
Naringin lowers cholesterol, prevents blood clots, and improves blood circulation and nutrient supply [100]. In addition, naringin protects against central nervous and cardiovascular diseases. To investigate the role of NFKB1 in OGD/R + injured PC12 cells, the previous study measured the components of the HIF-1α/AKT/mTOR signal path. HIF-1α, phosphorylated AKT, and mTOR were all higher in the OGD/R + naringin, OGD/R + si-NFKB1, and OGD/R + naringin + si-NFKB1 groups than in the OGD/R group. Significantly higher levels of HIF-1α, activated kinase AKT, and mTOR signals were expressed in the OGD/R + si-NFKB1 group (p < 0.01). In conclusion, naringin targets NFKB1 and modifies PC12 cell proliferation and apoptosis by affecting HIF-1α, p-AKT, and p-mTOR levels [120,121,122,123].
There is evidence that naringenin may help reduce the adverse effects of oxidative stress on the body, making it a potentially beneficial treatment option for various chronic illnesses. In addition to modulating the activity of antioxidant enzymes and regulating the expression of antioxidant genes, the flavonoid may have direct antioxidant effects, such as scavenging reactive species and reducing oxidative damage [124,125]. When Nrf2 is activated, antioxidant defenses are enhanced by maintaining redox equilibrium and decreasing oxidative stress and inflammation. TNF-α and IL-1β, two key inflammatory activators, are elevated in response to oxidative stress, whereas naringenin suppresses mRNA expression in the substantia nigra, hippocampus, and BV2 microglial cells [126,127]. For example, studies on rat hippocampus and BV cells have revealed that naringenin reduces NF-kB activation. Naringenin inhibited NF-kB, COX-2, iNOS, and their immunoreactivity, preventing the inflammatory cascade that leads to neurological diseases [51,128].
5.4. Anxiety and Depression
Anxiety and depression are two of the most common mental illnesses, both of which have complex origins at the intersection of several biological systems. Li et al. performed the first studies on the antidepressant effects of naringin and naringenin. The chemicals were tested on mice models of depression brought on by chronic unpredictable mild stress (CUMS) [129]. Anxiety may cause a variety of uncomfortable physical and emotional symptoms, including but not limited to: irritation, impatience, weariness, difficulty concentrating, a racing heart, chest pain, and an upset stomach. Anxiety comes in a variety of forms, and each is treated differently [130]. The serotonergic and noradrenergic systems have been connected to mood disorders such as depression and anxiety. The serotonergic system has far-reaching effects on cognitive processes in the brain, in addition to its role in regulating mood and appetite. Memory and focus are only two of the cognitive functions that are controlled by the noradrenergic system. Increases in serotonin (5-HT) and norepinephrine (NE) receptors, activation of brain-derived neurotrophic factor (BDNF), and decreased blood corticosterone are hypothesized to underlie NRG’s antidepressant-like effects [131,132]. It inhibits monoamine oxidase, which may also help those who are depressed. Increased rearing activity, decreased immobility, and increased social communication was seen in mice administered NRG intraperitoneally (at doses of 2.5, 5, and 10 mg/kg), which is consistent with anti-depressant-like and anxiolytic-like effects. Reductions were seen in nitrosative stress, lipid peroxidation, and cholinergic transmission. Mental diseases, often known as mental illnesses or psychiatric disorders, are characterized by persistent patterns of thinking or behavior that significantly impair an individual’s capacity to function in everyday life. Both the frequency and length of time that these symptoms will persist are unknown at this time. Various diseases and disorders have been identified, and each has its signs. In some instances, seeking the assistance of a clinical psychologist or psychiatrist specializing in evaluating and managing mental health conditions may be beneficial [133,134,135,136].
Neuronal inflammatory mediator release exacerbates tissue damage and reactive oxygen and nitrogen species (ROS/RNS) production, perpetuating the neuronal degeneration in stress-induced neuropsychiatric diseases, including depression and cognitive loss. Decreased antioxidant defenses in neurons promote neuroinflammation and neurodegeneration [137]. Several mediators and intracellular signaling molecules have been connected to neuroinflammatory responses to hypoxia damage. When hypoxia occurs, inflammatory transcription factors, including the NF-κB pathway, are activated, increasing pro-inflammatory cytokine production [137]. Physical changes in the brain’s dendritic arbourization and synaptic architecture have been linked to psychological and neurological issues, including depression, anxiety, and memory loss. Naringenin, a dietary flavanone, may be abundant in various foods, including citrus fruits, vegetables, and other berries and nuts [138]. Chronic illnesses and ailments may benefit from consuming a diet high in NG-rich fruits and vegetables. Animal pharmacokinetic studies have shown that NG rapidly undergoes intermediate glucuronide metabolism in the liver and readily crosses the blood–brain barrier (BBB). NG’s high permeability across the BBB has been attributed to its association with a broad range of CNS effects. However, the oral bioavailability of naringenin is limited by its metabolism in the liver and its degradation by bacterial enzymes in the colon. Lowered levels of inflammatory mediators were seen in rats, including TNF-α, cyclooxygenase-2, and inducible nitric oxide synthase (iNOS). Studies of naringenin’s effects on the brain and spinal cord show it may help treat various neurological disorders [139,140,141].
5.5. Schizophrenia
Schizophrenia is a disabling brain illness characterized by a wide range of neurotic symptoms including but not limited to hallucinations, delusions, cognitive impairment, disorganized speech, and aberrant motor activities [142]. Many different causes contribute to the development of schizophrenia. These include structural brain abnormalities, impaired neurotransmission, and stress-induced signaling cascades. Disruptions in epidermal growth factor (EGF) signaling and abnormalities in the processing or expression of the EGF receptors ErbB1 and ErbB2 are common in all schizophrenias [143]. As the pathophysiology of schizophrenia worsens, oxidative stress has been suspected to be a contributing factor. Several signs of oxidative stress, including ROS, reduced antioxidant enzyme activity (catalase), depleted glutathione, and oxidized lipids, have been associated with schizophrenia [144].
Schizophrenia and apoptosis have been connected via both intrinsic (mitochondrial death) and extrinsic (death receptor) pathways [145]. Cytochrome C interacts with pro- apoptotic and anti-apoptotic proteins to trigger the release of activated caspase-3 (primarily Bax and Bcl-2). Diabetes was prevented in streptozotocin-treated rats by administration of naringin, which inhibited the production of inflammatory and oxidative stress mediators [146]. Reduced free radical production, decreased release of proinflammatory cytokines (such as interleukin-6 and TNF-α), and down-regulation of inflammatory proteins such as NF-κB have all been linked to its anti-inflammatory effects in diabetic, chronic bronchitis, and walker carcinosarcoma rats. To evaluate if naringenin protects interendothelial tight junctions, we analyzed the expression and localization of ZO-1, occludin, claudin-1, and claudin-2 across experimental groups. ZO-1 protein expression was significantly reduced in the TNF-α treated group compared to the control group (p < 0.05) [147,148,149,150,151].
However, in TNF-α induced RIMVECs (p < 0.05), treatment with naringin dramatically increased ZO-1 protein expression. Immunofluorescence’s structured cell death also showed ZO-1 distribution. As proposed here, the medication that acts as a positive allosteric modulator of GABA neurotransmission from chandelier neurons is thought to improve the function of dorsolateral prefrontal cortex circuitry in people with schizophrenia by increasing gamma-band synchronization of pyramidal neuron activity [152,153,154,155].
6. Concluding Remarks and Future Directions
Although technological advances have substantially sped up research on phytochemicals, we still have a long way to go before we gather more definitive evidence regarding the neurotherapeutic benefits of herbal medicines. Our data and other researchers’ data lead us to believe that naringin and naringenin may be beneficial as neurotherapeutic medications because of their ability to alter several signaling pathways. The outcomes thus far are in line with this theory.
Despite the limitations of ongoing clinical studies, naringenin and naringin are promising therapies for various neurological conditions, including AD, PD, cerebral ischemia, anxiety, depression, schizophrenia, and chronic hyperglycemic peripheral neuropathy. Given these obstacles, it is essential that pharmacokinetic research on naringin and naringenin administration be performed, that more accurate dosage designs for different illnesses be developed, and that innovative drug delivery strategies be developed to boost bioavailability in healthcare situations.
Abbreviations
| PD | Parkinson’s disease |
| TRP | Transient receptor potential |
| NO | Nitric oxide |
| cGMP | Cyclic guanosine monophosphate |
| PKG | Protein kinase G |
| MAPK | Mitogen-activated protein kinase |
| GDNF | Growth differentiation and neurotrophic factor |
| AD | Alzheimer’s disease |
| Aβ | Amyloid-β |
| AChE | Acetylcholinesterase |
| CaMKII | Calcium/calmodulin-dependent protein kinase II |
| GSH | Reduced glutathione |
| GPx | Glutathione peroxidase |
| GST | Glutathione-S-transferase |
| SOD | Superoxide dismutase |
| ROS | Reactive oxygen species |
| LPO | Lipid peroxidation |
| MDA | Malondialdehyde |
| 5-HT | Serotonin |
| NE | Norepinephrine |
| BBB | Blood–brain barrier |
| iNOS | Inducible nitric oxide synthase |
Author Contributions
Conceptualization, T.B.E., F.I., R.D. and S.M.; data curation, T.B.E., F.I., R.D. and S.M.; formal analysis, T.B.E., F.I., N.N., H.S., R.D. and S.M.; investigation, T.B.E., F.I., N.N., H.S., R.D. and S.M.; methodology, T.B.E., F.I., N.N., H.S., R.D. and S.M.; project administration, M.M.A., A.H.A. and R.S.; resources, M.M.A., A.H.A., R.S. and T.B.E.; supervision, T.B.E.; validation, M.M.A., A.H.A., R.S. and T.B.E.; visualization, T.B.E., F.I., R.D. and S.M.; writing—original draft, T.B.E., F.I., R.D. and S.M.; writing—review and editing, M.M.A., A.H.A., R.S. and T.B.E. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Patel V., Chisholm D., Dua T., Laxminarayan R., Medina-Mora M.E. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities. Volume 4. The International Bank for Reconstruction and Development/The World Bank; Washington, DC, USA: 2016. [PubMed] [Google Scholar]
- 2.Zis P., Hadjivassiliou M. Treatment of Neurological Manifestations of Gluten Sensitivity and Coeliac Disease. Curr. Treat. Options Neurol. 2019;21:10. doi: 10.1007/s11940-019-0552-7. [DOI] [PubMed] [Google Scholar]
- 3.Ludvigsson J.F., Bai J.C., Biagi F., Card T.R., Ciacci C., Ciclitira P.J., Green P.H.R., Hadjivassiliou M., Holdoway A., Van Heel D.A. Diagnosis and Management of Adult Coeliac Disease: Guidelines from the British Society of Gastroenterology. Gut. 2014;63:1210–1228. doi: 10.1136/gutjnl-2013-306578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sapone A., Bai J.C., Ciacci C., Dolinsek J., Green P.H.R., Hadjivassiliou M., Kaukinen K., Rostami K., Sanders D.S., Schumann M. Spectrum of Gluten-Related Disorders: Consensus on New Nomenclature and Classification. BMC Med. 2012;10:13. doi: 10.1186/1741-7015-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fuhr U., Kummert A.L. The Fate of Naringin in Humans: A Key to Grapefruit Juice-drug Interactions? Clin. Pharmacol. Ther. 1995;58:365–373. doi: 10.1016/0009-9236(95)90048-9. [DOI] [PubMed] [Google Scholar]
- 6.Alam M.A., Subhan N., Rahman M.M., Uddin S.J., Reza H.M., Sarker S.D. Effect of Citrus Flavonoids, Naringin and Naringenin, on Metabolic Syndrome and Their Mechanisms of Action. Adv. Nutr. 2014;5:404–417. doi: 10.3945/an.113.005603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang J., Gao W., Liu Z., Zhang Z., Liu C. Systematic Analysis of Main Constituents in Rat Biological Samples after Oral Administration of the Methanol Extract of Fructus aurantii by HPLC-ESI-MS/MS. Iran. J. Pharm. Res. 2014;13:493–503. doi: 10.22037/ijpr.2014.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramesh E., Alshatwi A.A. Naringin Induces Death Receptor and Mitochondria-Mediated Apoptosis in Human Cervical Cancer (SiHa) Cells. Food Chem. Toxicol. 2013;51:97–105. doi: 10.1016/j.fct.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 9.Romagnolo D.F., Selmin O.I. Flavonoids and Cancer Prevention: A Review of the Evidence. J. Nutr. Gerontol. Geriatr. 2012;31:206–238. doi: 10.1080/21551197.2012.702534. [DOI] [PubMed] [Google Scholar]
- 10.Bharti S., Rani N., Krishnamurthy B., Arya D.S. Preclinical Evidence for the Pharmacological Actions of Naringin: A Review. Planta Med. 2014;80:437–451. doi: 10.1055/s-0034-1368351. [DOI] [PubMed] [Google Scholar]
- 11.Esaki S., Nishiyama K., Sugiyama N., Nakajima R., Takao Y., Kamiya S. Preparation and Taste of Certain Glycosides of Flavanones and of Dihydrochalcones. Biosci. Biotechnol. Biochem. 1994;58:1479–1485. doi: 10.1271/bbb.58.1479. [DOI] [PubMed] [Google Scholar]
- 12.Felgines C., Texier O., Morand C., Manach C., Scalbert A., Régerat F., Remesy C., Felgines C., Texier O., Morand C., et al. Bioavailability of the Flavanone Naringenin and Its Glycosides in Rats. Am. J. Physiol. Gastrointest. Liver Physiol. 2000;279:G1148–G1154. doi: 10.1152/ajpgi.2000.279.6.G1148. [DOI] [PubMed] [Google Scholar]
- 13.Jadeja R.N., Devkar R.V. Chapter 47—Polyphenols and Flavonoids in Controlling Non-Alcoholic Steatohepatitis. In: Watson R.R., Preedy V.R., Zibadi S., editors. Polyphenols in Human Health and Disease. Academic Press; San Diego, CA, USA: 2014. pp. 615–623. [Google Scholar]
- 14.Manchope M.F., Ferraz C.R., Borghi S.M., Rasquel-Oliveira F.S., Franciosi A., Bagatim-Souza J., Dionisio A.M., Casagrande R., Verri W.A. Chapter 38—Therapeutic Role of Naringenin to Alleviate Inflammatory Pain. In: Rajendram R., Patel V.B., Preedy V.R., Martin C.R., editors. Treatments, Mechanisms, and Adverse Reactions of Anesthetics and Analgesics. Academic Press; Cambridge, MA, USA: 2022. pp. 443–455. [Google Scholar]
- 15.Li Z.-X., Cao Y., Yan P. Topological Insulators and Semimetals in Classical Magnetic Systems. Phys. Rep. 2021;915:1–64. doi: 10.1016/j.physrep.2021.02.003. [DOI] [Google Scholar]
- 16.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Syst. Rev. 2021;10:89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abaza M.S.I., Orabi K.Y., Al-Quattan E., Al-Attiyah R.J. Growth Inhibitory and Chemo-Sensitization Effects of Naringenin, a Natural Flavanone Purified from Thymus Vulgaris, on Human Breast and Colorectal Cancer. Cancer Cell Int. 2015;15:1–19. doi: 10.1186/s12935-015-0194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ademosun A.O., Oboh G., Passamonti S., Tramer F., Ziberna L., Boligon A.A., Athayde M.L. Inhibition of Metalloproteinase and Proteasome Activities in Colon Cancer Cells by Citrus Peel Extracts. J. Basic Clin. Physiol. Pharmacol. 2015;26:471–477. doi: 10.1515/jbcpp-2013-0127. [DOI] [PubMed] [Google Scholar]
- 19.Hsiu S.-L., Huang T.-Y., Hou Y.-C., Chin D.-H., Chao P.-D.L. Comparison of Metabolic Pharmacokinetics of Naringin and Naringenin in Rabbits. Life Sci. 2002;70:1481–1489. doi: 10.1016/S0024-3205(01)01491-6. [DOI] [PubMed] [Google Scholar]
- 20.Moghaddam R.H., Samimi Z., Moradi S.Z., Little P.J., Xu S., Farzaei M.H. Naringenin and Naringin in Cardiovascular Disease Prevention: A Preclinical Review. Eur. J. Pharmacol. 2020;887:173535. doi: 10.1016/j.ejphar.2020.173535. [DOI] [PubMed] [Google Scholar]
- 21.Zhang L., Song L., Zhang P., Liu T., Zhou L., Yang G., Lin R., Zhang J. Solubilities of Naringin and Naringenin in Different Solvents and Dissociation Constants of Naringenin. J. Chem. Eng. Data. 2015;60:932–940. doi: 10.1021/je501004g. [DOI] [Google Scholar]
- 22.Fujioka K., Greenway F., Sheard J., Ying Y. The Effects of Grapefruit on Weight and Insulin Resistance: Relationship to the Metabolic Syndrome. J. Med. Food. 2006;9:49–54. doi: 10.1089/jmf.2006.9.49. [DOI] [PubMed] [Google Scholar]
- 23.Ishii K., Furuta T., Kasuya Y. Determination of Naringin and Naringenin in Human Plasma by High-Performance Liquid Chromatography. J. Chromatogr. B Biomed. Sci. Appl. 1996;683:225–229. doi: 10.1016/0378-4347(96)00114-4. [DOI] [PubMed] [Google Scholar]
- 24.Lee C.-H., Jeong T.-S., Choi Y.-K., Hyun B.-H., Oh G.-T., Kim E.-H., Kim J.-R., Han J.-I., Bok S.-H. Anti-Atherogenic Effect of Citrus Flavonoids, Naringin and Naringenin, Associated with Hepatic ACAT and Aortic VCAM-1 and MCP-1 in High Cholesterol-Fed Rabbits. Biochem. Biophys. Res. Commun. 2001;284:681–688. doi: 10.1006/bbrc.2001.5001. [DOI] [PubMed] [Google Scholar]
- 25.Renugadevi J., Prabu S.M. Naringenin Protects against Cadmium-Induced Oxidative Renal Dysfunction in Rats. Toxicology. 2009;256:128–134. doi: 10.1016/j.tox.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 26.Cook N.C., Samman S. Flavonoids—Chemistry, Metabolism, Cardioprotective Effects, and Dietary Sources. J. Nutr. Biochem. 1996;7:66–76. doi: 10.1016/0955-2863(95)00168-9. [DOI] [Google Scholar]
- 27.Choudhury R., Chowrimootoo G., Srai K., Debnam E., Rice-Evans C.A. Interactions of the Flavonoid Naringenin in the Gastrointestinal Tract and the Influence of Glycosylation. Biochem. Biophys. Res. Commun. 1999;265:410–415. doi: 10.1006/bbrc.1999.1695. [DOI] [PubMed] [Google Scholar]
- 28.Croft K.D. The Chemistry and Biological Effects of Flavonoids and Phenolic Acids A. Ann. N. Y. Acad. Sci. 1998;854:435–442. doi: 10.1111/j.1749-6632.1998.tb09922.x. [DOI] [PubMed] [Google Scholar]
- 29.Scalbert A., Williamson G. Dietary Intake and Bioavailability of Polyphenols. J. Nutr. 2000;130:2073S–2085S. doi: 10.1093/jn/130.8.2073S. [DOI] [PubMed] [Google Scholar]
- 30.Pietta P., Minoggio M., Bramati L. Plant Polyphenols: Structure, Occurrence and Bioactivity. Stud. Nat. Prod. Chem. 2003;28:257–312. doi: 10.1016/S1572-5995(03)80143-6. [DOI] [Google Scholar]
- 31.Navipour E., Neamatshahi M., Barabadi Z., Neamatshahi M., Keykhosravi A. Epidemiology and Risk Factors of Alzheimer’s Disease in Iran: A Systematic Review. Iran. J. Public Health. 2019;48:2133–2139. doi: 10.18502/ijph.v48i12.3544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pedersen W.A., McMillan P.J., Kulstad J.J., Leverenz J.B., Craft S., Haynatzki G.R. Rosiglitazone Attenuates Learning and Memory Deficits in Tg2576 Alzheimer Mice. Exp. Neurol. 2006;199:265–273. doi: 10.1016/j.expneurol.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 33.Rajmohan R., Reddy P.H. Amyloid-Beta and Phosphorylated Tau Accumulations Cause Abnormalities at Synapses of Alzheimer’s Disease Neurons. J. Alzheimer’s Dis. 2017;57:975–999. doi: 10.3233/JAD-160612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jin H., Wang W., Zhao S., Yang W., Qian Y., Jia N., Feng G. Aβ-HBc Virus-like Particles Immunization without Additional Adjuvant Ameliorates the Learning and Memory and Reduces Aβ Deposit in PDAPP Mice. Vaccine. 2014;32:4450–4456. doi: 10.1016/j.vaccine.2014.06.051. [DOI] [PubMed] [Google Scholar]
- 35.Gauthier S., Scheltens P., Cummings J. Alzheimer’s Disease and Related Disorders. CRC Press; Boca Raton, FL, USA: 2005. [Google Scholar]
- 36.Mimura M., Yano M. Memory Impairment and Awareness of Memory Deficits in Early-Stage Alzheimer’s Disease. Rev. Neurosci. 2006;17:253–266. doi: 10.1515/REVNEURO.2006.17.1-2.253. [DOI] [PubMed] [Google Scholar]
- 37.Fakhri S., Abbaszadeh F., Dargahi L., Jorjani M. Astaxanthin: A Mechanistic Review on Its Biological Activities and Health Benefits. Pharmacol. Res. 2018;136:1–20. doi: 10.1016/j.phrs.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 38.Bao X.-Q., Li N., Wang T., Kong X.-C., Tai W.-J., Sun H., Zhang D. FLZ Alleviates the Memory Deficits in Transgenic Mouse Model of Alzheimer’s Disease via Decreasing Beta-Amyloid Production and Tau Hyperphosphorylation. PLoS ONE. 2013;8:e78033. doi: 10.1371/journal.pone.0078033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mimura M. Memory Impairment and Awareness of Memory Deficits in Early-Stage Alzheimer’s Disease. Tohoku J. Exp. Med. 2008;215:133–140. doi: 10.1620/tjem.215.133. [DOI] [PubMed] [Google Scholar]
- 40.Obulesu M., Jhansilakshmi M. Neuroinflammation in Alzheimer’s Disease: An Understanding of Physiology and Pathology. Int. J. Neurosci. 2014;124:227–235. doi: 10.3109/00207454.2013.831852. [DOI] [PubMed] [Google Scholar]
- 41.Yang W., Ma J., Liu Z., Lu Y., Hu B., Yu H. Effect of Naringenin on Brain Insulin Signaling and Cognitive Functions in ICV-STZ Induced Dementia Model of Rats. Neurol. Sci. 2014;35:741–751. doi: 10.1007/s10072-013-1594-3. [DOI] [PubMed] [Google Scholar]
- 42.Burke R.E., O’Malley K. Axon Degeneration in Parkinson’s Disease. Exp. Neurol. 2013;246:72–83. doi: 10.1016/j.expneurol.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Savitt J.M., Dawson V.L., Dawson T.M. Diagnosis and Treatment of Parkinson Disease: Molecules to Medicine. J. Clin. Investig. 2006;116:1744–1754. doi: 10.1172/JCI29178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shulman J.M., De Jager P.L., Feany M.B. Parkinson’s Disease: Genetics and Pathogenesis. Annu. Rev. Pathol. Mech. Dis. 2011;6:193–222. doi: 10.1146/annurev-pathol-011110-130242. [DOI] [PubMed] [Google Scholar]
- 45.Dexter D.T., Jenner P. Parkinson Disease: From Pathology to Molecular Disease Mechanisms. Free Radic. Biol. Med. 2013;62:132–144. doi: 10.1016/j.freeradbiomed.2013.01.018. [DOI] [PubMed] [Google Scholar]
- 46.AlDakheel A., Kalia L.V., Lang A.E. Pathogenesis-Targeted, Disease-Modifying Therapies in Parkinson Disease. Neurotherapeutics. 2014;11:6–23. doi: 10.1007/s13311-013-0218-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Olanow C.W., Tatton W.G. Etiology and Pathogenesis of Parkinson’s Disease. Annu. Rev. Neurosci. 1999;22:123. doi: 10.1146/annurev.neuro.22.1.123. [DOI] [PubMed] [Google Scholar]
- 48.Zbarsky V., Datla K.P., Parkar S., Rai D.K., Aruoma O.I., Dexter D.T. Neuroprotective Properties of the Natural Phenolic Antioxidants Curcumin and Naringenin but Not Quercetin and Fisetin in a 6-OHDA Model of Parkinson’s Disease. Free Radic. Res. 2005;39:1119–1125. doi: 10.1080/10715760500233113. [DOI] [PubMed] [Google Scholar]
- 49.Golechha M., Chaudhry U., Bhatia J., Saluja D., Arya D.S. Naringin Protects against Kainic Acid-Induced Status Epilepticus in Rats: Evidence for an Antioxidant, Anti-Inflammatory and Neuroprotective Intervention. Biol. Pharm. Bull. 2011;34:360–365. doi: 10.1248/bpb.34.360. [DOI] [PubMed] [Google Scholar]
- 50.Ahmed S., Khan H., Aschner M., Hasan M.M., Hassan S.T.S. Therapeutic Potential of Naringin in Neurological Disorders. Food Chem. Toxicol. 2019;132:110646. doi: 10.1016/j.fct.2019.110646. [DOI] [PubMed] [Google Scholar]
- 51.Raza S.S., Khan M.M., Ahmad A., Ashafaq M., Islam F., Wagner A.P., Safhi M.M. Neuroprotective Effect of Naringenin Is Mediated through Suppression of NF-ΚB Signaling Pathway in Experimental Stroke. Neuroscience. 2013;230:157–171. doi: 10.1016/j.neuroscience.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 52.Harrison W.T.A., Yathirajan H.S., Sarojini B.K., Narayana B., Anilkumar H.G. Do C—H⋯ O and C—H⋯ π Interactions Help to Stabilize a Non-Centrosymmetric Structure for Racemic 2, 3-Dibromo-1, 3-Diphenylpropan-1-One? Acta Crystallogr. Sect. C Cryst. Struct. Commun. 2005;61:o728–o730. doi: 10.1107/S0108270105036942. [DOI] [PubMed] [Google Scholar]
- 53.Gopinathan G., Teravainen H., Dambrosia J.M., Ward C.D., Sanes J.N., Stuart W.K., Evarts E.V., Calne D.B. Lisuride in Parkinsonism. Neurology. 1981;31:371. doi: 10.1212/WNL.31.4_Part_2.371. [DOI] [PubMed] [Google Scholar]
- 54.Kim H.D., Jeong K.H., Jung U.J., Kim S.R. Naringin Treatment Induces Neuroprotective Effects in a Mouse Model of Parkinson’s Disease in Vivo, but Not Enough to Restore the Lesioned Dopaminergic System. J. Nutr. Biochem. 2016;28:140–146. doi: 10.1016/j.jnutbio.2015.10.013. [DOI] [PubMed] [Google Scholar]
- 55.Kensler T.W., Wakabayashi N., Biswal S. Cell Survival Responses to Environmental Stresses via the Keap1-Nrf2-ARE Pathway. Annu. Rev. Pharmacol. Toxicol. 2007;47:89–116. doi: 10.1146/annurev.pharmtox.46.120604.141046. [DOI] [PubMed] [Google Scholar]
- 56.Lee J.-M., Johnson J.A. An Important Role of Nrf2-ARE Pathway in the Cellular Defense Mechanism. BMB Rep. 2004;37:139–143. doi: 10.5483/BMBRep.2004.37.2.139. [DOI] [PubMed] [Google Scholar]
- 57.Eagling V.A., Profit L., Back D.J. Inhibition of the CYP3A4-Mediated Metabolism and P-Glycoprotein-Mediated Transport of the HIV-1 Protease Inhibitor Saquinavir by Grapefruit Juice Components. Br. J. Clin. Pharmacol. 1999;48:543. doi: 10.1046/j.1365-2125.1999.00052.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sachdeva A.K., Kuhad A., Chopra K. Naringin Ameliorates Memory Deficits in Experimental Paradigm of Alzheimer’s Disease by Attenuating Mitochondrial Dysfunction. Pharmacol. Biochem. Behav. 2014;127:101–110. doi: 10.1016/j.pbb.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 59.Wang D., Gao K., Li X., Shen X., Zhang X., Ma C., Qin C., Zhang L. Long-Term Naringin Consumption Reverses a Glucose Uptake Defect and Improves Cognitive Deficits in a Mouse Model of Alzheimer’s Disease. Pharmacol. Biochem. Behav. 2012;102:13–20. doi: 10.1016/j.pbb.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 60.Kaur G., Prakash A. Involvement of the Nitric Oxide Signaling in Modulation of Naringin against Intranasal Manganese and Intracerbroventricular β-Amyloid Induced Neurotoxicity in Rats. J. Nutr. Biochem. 2020;76:108255. doi: 10.1016/j.jnutbio.2019.108255. [DOI] [PubMed] [Google Scholar]
- 61.Meng X., Fu M., Wang S., Chen W., Wang J., Zhang N. Naringin Ameliorates Memory Deficits and Exerts Neuroprotective Effects in a Mouse Model of Alzheimer’s Disease by Regulating Multiple Metabolic Pathways. Mol. Med. Rep. 2021;23:332. doi: 10.3892/mmr.2021.11971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Heo H.J., Kim M.J., Lee J.M., Choi S.J., Cho H.Y., Hong B., Kim H.K., Kim E., Shin D.H. Naringenin from Citrus Junos Has an Inhibitory Effect on Acetylcholinesterase and a Mitigating Effect on Amnesia. Dement. Geriatr. Cogn. Disord. 2004;17:151–157. doi: 10.1159/000076349. [DOI] [PubMed] [Google Scholar]
- 63.Khan M.B., Khan M.M., Khan A., Ahmed M.E., Ishrat T., Tabassum R., Vaibhav K., Ahmad A., Islam F. Naringenin Ameliorates Alzheimer’s Disease (AD)-Type Neurodegeneration with Cognitive Impairment (AD-TNDCI) Caused by the Intracerebroventricular- Streptozotocin in Rat Model. Neurochem. Int. 2012;61:1081–1093. doi: 10.1016/j.neuint.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 64.Heo H.J., Kim D.O., Shin S.C., Kim M.J., Kim B.G., Shin D.H. Effect of Antioxidant Flavanone, Naringenin, from Citrus Junos on Neuroprotection. J. Agric. Food Chem. 2004;52:1520–1525. doi: 10.1021/jf035079g. [DOI] [PubMed] [Google Scholar]
- 65.Rahigude A., Bhutada P., Kaulaskar S., Aswar M., Otari K. Participation of Antioxidant and Cholinergic System in Protective Effect of Naringenin against Type-2 Diabetes-Induced Memory Dysfunction in Rats. Neuroscience. 2012;226:62–72. doi: 10.1016/j.neuroscience.2012.09.026. [DOI] [PubMed] [Google Scholar]
- 66.Yang W., Zhou K., Zhou Y., An Y., Hu T., Lu J., Huang S., Pei G. Naringin Dihydrochalcone Ameliorates Cognitive Deficits and Neuropathology in APP/PS1 Transgenic Mice. Front. Aging Neurosci. 2018;10:169. doi: 10.3389/fnagi.2018.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kumar A., Dogra S., Prakash A. Protective Effect of Naringin, a Citrus Flavonoid, against Colchicine-Induced Cognitive Dysfunction and Oxidative Damage in Rats. J. Med. Food. 2010;13:976–984. doi: 10.1089/jmf.2009.1251. [DOI] [PubMed] [Google Scholar]
- 68.Jahanshahi M., Khalili M., Margedari A. Naringin Chelates Excessive Iron and Prevents the Formation of Amyloid-Beta Plaques in the Hippocampus of Iron-Overloaded Mice. Front. Pharmacol. 2021;12:518. doi: 10.3389/fphar.2021.651156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Prabhakar O. Naringin Attenuates Aluminum Induced Cognitive Deficits in Rats. Indian J. Pharm. Educ. Res. 2020;54:674–681. doi: 10.5530/ijper.54.3.117. [DOI] [Google Scholar]
- 70.Guo L., Sun B. N,N’-1,10-Bis(Naringin) Triethylenetetraamine, Synthesis and as a Cu(II) Chelator for Alzheimer’s Disease Therapy. Biol. Pharm. Bull. 2021;44:51–56. doi: 10.1248/bpb.b20-00574. [DOI] [PubMed] [Google Scholar]
- 71.Ben-Azu B., Nwoke E., Aderibigbe A., Omogbiya I., Ajayi A., Olonode E., Umukoro S., Iwalewa E. Possible Neuroprotective Mechanisms of Action Involved in the Neurobehavioral Property of Naringin in Mice. Biomed. Pharmacother. 2019;109:536–546. doi: 10.1016/j.biopha.2018.10.055. [DOI] [PubMed] [Google Scholar]
- 72.Varshney V., Garabadu D. Naringin Exhibits Mas Receptor-Mediated Neuroprotection Against Amyloid Beta-Induced Cognitive Deficits and Mitochondrial Toxicity in Rat Brain. Neurotox. Res. 2021;39:1023–1043. doi: 10.1007/s12640-021-00336-y. [DOI] [PubMed] [Google Scholar]
- 73.Ghofrani S., Joghataei M., Mohseni S., Baluchnejadmojarad T., Bagheri M., Khamse S., Roghani M. Naringenin Improves Learning and Memory in an Alzheimer’s Disease Rat Model: Insights into the Underlying Mechanisms. Eur. J. Pharmacol. 2015;764:195–201. doi: 10.1016/j.ejphar.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 74.Jung U., Kim S. Effects of Naringin, a Flavanone Glycoside in Grapefruits and Citrus Fruits, on the Nigrostriatal Dopaminergic Projection in the Adult Brain. Neural Regen. Res. 2014;9:1514. doi: 10.4103/1673-5374.139476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Leem E., Nam J., Jeon M., Shin W., Won S., Park S., Choi M., Jin B., Jung U., Kim S. Naringin Protects the Nigrostriatal Dopaminergic Projection through Induction of GDNF in a Neurotoxin Model of Parkinson’s Disease. J. Nutr. Biochem. 2014;25:801–806. doi: 10.1016/j.jnutbio.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 76.Garabadu D., Agrawal N. Naringin Exhibits Neuroprotection Against Rotenone-Induced Neurotoxicity in Experimental Rodents. NeuroMolecular Med. 2020;22:314–330. doi: 10.1007/s12017-019-08590-2. [DOI] [PubMed] [Google Scholar]
- 77.Kumar N., James R., Sinha S., Kinra M., Anuranjana P.V., Nandakumar K. Naringin Exhibited Anti-Parkinsonian like Effect against Haloperidol-Induced Catalepsy in Mice. Res. J. Pharm. Technol. 2021;14:662–666. doi: 10.5958/0974-360X.2021.00118.9. [DOI] [Google Scholar]
- 78.Sugumar M., Sevanan M., Sekar S. Neuroprotective Effect of Naringenin against MPTP-Induced Oxidative Stress. Int. J. Neurosci. 2018;129:534–539. doi: 10.1080/00207454.2018.1545772. [DOI] [PubMed] [Google Scholar]
- 79.Madani M., Attia A., ElSalalm R., El-Shenawy S., Arbid M. Neuropharmacological Effects of Naringenin, Harmine and Adenosine on Parkinsonism Induced in Rats. Der Pharm. Lett. 2016;8:45–57. [Google Scholar]
- 80.Chen C., Wei Y., He X., Li D., Wang G., Li J. Naringenin Produces Neuroprotection Against LPS-Induced Dopamine Neurotoxicity via the Inhibition of Microglial NLRP3 Inflammasome Activation. Front. Immunol. 2019;10:936. doi: 10.3389/fimmu.2019.00936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mani S., Sekar S., Chidambaram S.B., Sevanan M. Naringenin Protects against 1-Methyl-4-Phenylpyridinium-Induced Neuroinflammation and Resulting Reactive Oxygen Species Production in SH - SY5Y Cell Line: An In Vitro Model of Parkinson’s Disease. Pharmacogn. Mag. 2018:458–464. doi: 10.4103/pm.pm. [DOI] [Google Scholar]
- 82.Mercer L., Kelly B., Horne M., Beart P. Dietary Polyphenols Protect Dopamine Neurons from Oxidative Insults and Apoptosis: Investigations in Primary Rat Mesencephalic Cultures. Biochem. Pharmacol. 2005;69:339–345. doi: 10.1016/j.bcp.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 83.Kabir M.S.H., Hossain M.M., Kabir M.I., Rahman M.M., Hasanat A., Emran T.B., Rahman M.A. Phytochemical screening, Antioxidant, Thrombolytic, alpha-amylase inhibition and cytotoxic activities of ethanol extract of Steudnera colocasiifolia K. Koch leaves. J. Young Pharm. 2016;8:391. doi: 10.5530/jyp.2016.4.15. [DOI] [Google Scholar]
- 84.Lou H., Jing X., Wei X., Shi H., Ren D., Zhang X. Naringenin Protects against 6-OHDA-Induced Neurotoxicity via Activation of the Nrf2/ARE Signaling Pathway. Neuropharmacology. 2014;79:380–388. doi: 10.1016/j.neuropharm.2013.11.026. [DOI] [PubMed] [Google Scholar]
- 85.Kesh S., Rajesh R., Balakrishnan A. Naringenin Alleviates 6-Hydroxydopamine Induced Parkinsonism in SHSY5Y Cells and Zebrafish Model. Comp. Biochem. Physiol. Part C Toxicol. Pharmacol. 2021;239:108893. doi: 10.1016/j.cbpc.2020.108893. [DOI] [PubMed] [Google Scholar]
- 86.Mani S., Sekar S., Barathidasan R., Manivasagam T., Thenmozhi A.J., Sevanan M., Chidambaram S.B., Essa M.M., Guillemin G.J., Sakharkar M.K. Naringenin Decreases α -Synuclein Expression and Neuroinflammation in MPTP-Induced Parkinson’s Disease Model in Mice. Neurotox. Res. 2018;33:656–670. doi: 10.1007/s12640-018-9869-3. [DOI] [PubMed] [Google Scholar]
- 87.Wang G., Zhang B., He X., Li D., Shi J., Zhang F. Naringenin Targets on Astroglial Nrf2 to Support Dopaminergic Neurons. Pharmacol. Res. 2018;139:452–459. doi: 10.1016/j.phrs.2018.11.043. [DOI] [PubMed] [Google Scholar]
- 88.Yi L., Li J., Li H., Su D., Quan X., He X., Wang X. Antidepressant-like Behavioral, Neurochemical and Neuroendocrine Effects of Naringenin in the Mouse Repeated Tail Suspension Test. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2012;39:175–181. doi: 10.1016/j.pnpbp.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 89.Yi L., Liu B., Li J., Luo L., Liu Q., Geng D., Tang Y., Xia Y., Wu D. BDNF Signaling Is Necessary for the Antidepressant-like Effect of Naringenin. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2014;48:135–141. doi: 10.1016/j.pnpbp.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 90.Olugbemide A.S., Ben-Azu B., Bakre A.G., Ajayi A.M., Femi-Akinlosotu O., Umukoro S. Naringenin Improves Depressive- and Anxiety-like Behaviors in Mice Exposed to Repeated Hypoxic Stress through Modulation of Oxido-Inflammatory Mediators and NF-KB/BDNF Expressions. Brain Res. Bull. 2021;169:214–227. doi: 10.1016/j.brainresbull.2020.12.003. [DOI] [PubMed] [Google Scholar]
- 91.Anyanwu G.E., Atuadu V.O., Esom E.A., Nto J.N., Katchy A.U. Putative Role of Monoaminergic Systems in Antidepressant and Anxiolytic Effects of Naringin in Mice: An Interaction Study with Receptor Antagonists. J. Pharm. Res. Int. 2021;33:661–676. doi: 10.9734/jpri/2021/v33i47B33168. [DOI] [Google Scholar]
- 92.Oladapo O.M., Ben-azu B., Ajayi A.M., Emokpae O., Eneni A.O. Naringin Confers Protection against Psychosocial Defeat Stress-Induced Neurobehavioral Deficits in Mice: Involvement of Glutamic Acid Decarboxylase Isoform-67, Oxido-Nitrergic Stress, and Neuroinflammatory Mechanisms. J. Mol. Neurosci. 2020;71:431–445. doi: 10.1007/s12031-020-01664-y. [DOI] [PubMed] [Google Scholar]
- 93.Tayyab M., Farheen S., Mariyath M., Khanam P.M.N., Hossain M.M. Antidepressant and Neuroprotective Effects of Naringenin via Sonic Hedgehog-GLI1 Cell Signaling Pathway in a Rat Model of Chronic Unpredictable Mild Stress. Neuromol. Med. 2019;21:250–261. doi: 10.1007/s12017-019-08538-6. [DOI] [PubMed] [Google Scholar]
- 94.Yamagishi N., Yamamoto Y., Noda C., Hatayama T. Naringenin Inhibits the Aggregation of Expanded Polyglutamine Tract-Containing Protein through the Induction of Endoplasmic Reticulum Chaperone GRP78. Biol. Pharm. Bull. 2012;35:1836–1840. doi: 10.1248/bpb.b12-00451. [DOI] [PubMed] [Google Scholar]
- 95.Kumar P., Kumar A. Protective Effect of Hesperidin and Naringin against 3-Nitropropionic Acid Induced Huntington’ s like Symptoms in Rats: Possible Role of Nitric Oxide. Behav. Brain Res. 2010;206:38–46. doi: 10.1016/j.bbr.2009.08.028. [DOI] [PubMed] [Google Scholar]
- 96.Salman M., Sharma P., Alam I., Tabassum H. Naringenin Mitigates Behavioral Alterations and Provides Neuroprotection against 3-Nitropropinoic Acid-Induced Huntington’s Disease like Symptoms in Rats. Nutr. Neurosci. 2021;25:1–11. doi: 10.1080/1028415X.2021.1913319. [DOI] [PubMed] [Google Scholar]
- 97.Cui J., Wang G., Kandhare A.D., Mukherjee A.A., Bodhankar S.L. Neuroprotective Effect of Naringin, a Flavone Glycoside in Quinolinic Acid-Induced Neurotoxicity: Possible Role of PPAR-γ, Bax/Bcl-2, and Caspase-3. Food Chem. Toxicol. 2018;121:95–108. doi: 10.1016/j.fct.2018.08.028. [DOI] [PubMed] [Google Scholar]
- 98.Gopinath K., Sudhandiran G. Naringin modulates oxidative stress and inflammation in 3-nitropropionic acid-induced neurodegeneration through the activation of nuclear factor-erythroid 2-related factor-2 signalling pathway. Neuroscience. 2012;227:134–143. doi: 10.1016/j.neuroscience.2012.07.060. [DOI] [PubMed] [Google Scholar]
- 99.Kulasekaran G., Ganapasam S. Neuroprotective Efficacy of Naringin on 3-Nitropropionic Acid- Induced Mitochondrial Dysfunction through the Modulation of Nrf2 Signaling Pathway in PC12 Cells. Mol. Cell. Biochem. 2015;409:199–211. doi: 10.1007/s11010-015-2525-9. [DOI] [PubMed] [Google Scholar]
- 100.Gaur V., Aggarwal A., Kumar A. Protective Effect of Naringin against Ischemic Reperfusion Cerebral Injury: Possible Neurobehavioral, Biochemical and Cellular Alterations in Rat Brain. Eur. J. Pharmacol. 2009;616:147–154. doi: 10.1016/j.ejphar.2009.06.056. [DOI] [PubMed] [Google Scholar]
- 101.Okuyama S., Yamamoto K., Mori H., Sawamoto A., Amakura Y. Neuroprotective Effect of Citrus Kawachiensis (Kawachi Bankan) Peels, a Rich Source of Naringin, against Global Cerebral Ischemia/Reperfusion Injury in Mice. Biosci. Biotechnol. Biochem. 2018;82:1216–1224. doi: 10.1080/09168451.2018.1456320. [DOI] [PubMed] [Google Scholar]
- 102.Han Y., Su J., Liu X., Zhao Y., Wang C., Li X. Naringin Alleviates Early Brain Injury after Experimental Subarachnoid Hemorrhage by Reducing Oxidative Stress and Inhibiting Apoptosis. Brain Res. Bull. 2016;133:42–50. doi: 10.1016/j.brainresbull.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 103.Bai X., Zhang X., Chen L. Protective Effect of Naringenin in Experimental Ischemic Stroke: Down-Regulated NOD2, RIP2, NF-KappaB, MMP-9 and Up-Regulated Claudin-5 Expression. Neurochem. Res. 2014;39:1405–1415. doi: 10.1007/s11064-014-1326-y. [DOI] [PubMed] [Google Scholar]
- 104.Feng J., Chen X., Lu S., Li W., Yang D., Su W., Wang X. Naringin Attenuates Cerebral Ischemia-Reperfusion Injury Through Inhibiting Peroxynitrite-Mediated Mitophagy Activation. Mol. Neurobiol. 2018;55:9029–9042. doi: 10.1007/s12035-018-1027-7. [DOI] [PubMed] [Google Scholar]
- 105.Cui Q., Wang L., Wei Z., Qu W. Continual Naringin Treatment Benefits the Recovery of Traumatic Brain Injury in Rats Through Reducing Oxidative and Inflammatory Alterations. Neurochem. Res. 2014;39:1254–1262. doi: 10.1007/s11064-014-1306-2. [DOI] [PubMed] [Google Scholar]
- 106.Rong W., Pan Y., Cai X., Song F., Zhao Z., Xiao S., Zhang C. The Mechanism of Naringin-Enhanced Remyelination after Spinal Cord Injury. Neural Regen. Res. 2017;12:470. doi: 10.4103/1673-5374.202923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Fakhri S., Sabouri S., Kiani A., Farzaei M.H., Rashidi K. Intrathecal Administration of Naringenin Improves Motor Dysfunction and Neuropathic Pain Following Compression Spinal Cord Injury in Rats: Relevance to Its Antioxidant and Anti-Inflammatory Activities. Korean J. Pain. 2022;35:291–302. doi: 10.3344/kjp.2022.35.3.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Shi L., Tang P., Zhang W., Zhao Y., Zhang L., Zhang H. Naringenin Inhibits Spinal Cord Injury-Induced Activation of Neutrophils through MiR-223. Gene. 2016;592:128–133. doi: 10.1016/j.gene.2016.07.037. [DOI] [PubMed] [Google Scholar]
- 109.Wang L., Zhang Z., Wang H. Naringin Attenuates Cerebral Ischemia-Reperfusion Injury in Rats by Inhibiting Endoplasmic Reticulum Stress. Transl. Neurosci. 2021;12:190–197. doi: 10.1515/tnsci-2020-0170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hu C., Zhao Y. Analgesic Effects of Naringenin in Rats with Spinal Nerve Ligation-Induced Neuropathic Pain. Biomed. Rep. 2014;2:569–573. doi: 10.3892/br.2014.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kaulaskar S., Bhutada P., Rahigude A., Jain D., Harle U. Effects of Naringenin on Allodynia and Hyperalgesia in Rats with Chronic Constriction Injury-Induced Neuropathic Pain. J. Chin. Integr. Med. 2012;10:1482–1489. doi: 10.3736/jcim20121223. [DOI] [PubMed] [Google Scholar]
- 112.Semis H., Kandemir F., Caglayan C., Kaynar O., Genc A., Arıkan S. Protective Effect of Naringin against Oxaliplatin-induced Peripheral Neuropathy in Rats: A Behavioral and Molecular Study. J. Biochem. Mol. Toxicol. 2022;36:e23121. doi: 10.1002/jbt.23121. [DOI] [PubMed] [Google Scholar]
- 113.Yang J., Yuan L., Wen Y., Zhou H., Jiang W., Xu D., Wang M. Protective Effects of Naringin in Cerebral Infarction and Its Molecular Mechanism. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020;26:e918772. doi: 10.12659/MSM.918772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sveinsson O.A., Kjartansson O., Valdimarsson E.M. Cerebral Ischemia/Infarction-Diagnosis and Treatment. Laeknabladid. 2014;100:393–401. doi: 10.17992/lbl.2014.0708.553. [DOI] [PubMed] [Google Scholar]
- 115.Olmez I., Ozyurt H. Reactive Oxygen Species and Ischemic Cerebrovascular Disease. Neurochem. Int. 2012;60:208–212. doi: 10.1016/j.neuint.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 116.Tsung A., Klune J.R., Zhang X., Jeyabalan G., Cao Z., Peng X., Stolz D.B., Geller D.A., Rosengart M.R., Billiar T.R. HMGB1 Release Induced by Liver Ischemia Involves Toll-like Receptor 4–Dependent Reactive Oxygen Species Production and Calcium-Mediated Signaling. J. Exp. Med. 2007;204:2913–2923. doi: 10.1084/jem.20070247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ma L.L., Song L., Yu X.D., Yu T.X., Liang H., Qiu J.X. The Clinical Study on the Treatment for Acute Cerebral Infarction by Intra-Arterial Thrombolysis Combined with Mild Hypothermia. Eur. Rev. Med. Pharmacol. Sci. 2017;21:1999–2006. [PubMed] [Google Scholar]
- 118.Jeong H.S., Song H.-J., Kim S.-B., Lee J., Kang C.W., Koh H.-S., Shin J.E., Lee S.H., Kwon H.J., Kim J. A Comparison of Stent-Assisted Mechanical Thrombectomy and Conventional Intra-Arterial Thrombolysis for Acute Cerebral Infarction. J. Clin. Neurol. 2013;9:91–96. doi: 10.3988/jcn.2013.9.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bailey D.G., Arnold J.M.O., Strong H.A., Munoz C., Spence J.D. Effect of Grapefruit Juice and Naringin on Nisoldipine Pharmacokinetics. Clin. Pharmacol. Ther. 1993;54:589–594. doi: 10.1038/clpt.1993.195. [DOI] [PubMed] [Google Scholar]
- 120.Cao W., Feng S.-J., Kan M.-C. Naringin Targets NFKB1 to Alleviate Oxygen-Glucose Deprivation/Reoxygenation–Induced Injury in PC12 Cells via Modulating HIF-1α/AKT/MTOR-Signaling Pathway. J. Mol. Neurosci. 2021;71:101–111. doi: 10.1007/s12031-020-01630-8. [DOI] [PubMed] [Google Scholar]
- 121.Zhang Y., Zhang J., Wu C., Guo S., Su J., Zhao W., Xing H. Higenamine Protects Neuronal Cells from Oxygen-glucose Deprivation/Reoxygenation-induced Injury. J. Cell. Biochem. 2019;120:3757–3764. doi: 10.1002/jcb.27656. [DOI] [PubMed] [Google Scholar]
- 122.Shu K., Zhang Y. Protodioscin Protects PC12 Cells against Oxygen and Glucose Deprivation-Induced Injury through MiR-124/AKT/Nrf2 Pathway. Cell Stress Chaperones. 2019;24:1091–1099. doi: 10.1007/s12192-019-01031-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang C., Yang Y.-H., Zhou L., Ding X.-L., Meng Y.-C., Han K. Curcumin Alleviates OGD/R-Induced PC12 Cell Damage via Repressing CCL3 and Inactivating TLR4/MyD88/MAPK/NF-ΚB to Suppress Inflammation and Apoptosis. J. Pharm. Pharmacol. 2020;72:1176–1185. doi: 10.1111/jphp.13293. [DOI] [PubMed] [Google Scholar]
- 124.Rahman J., Tareq A.M., Hossain M., Sakib S.A., Islam M.N., Ali M.H., Uddin A.B.M.N., Hoque M., Nasrin M.S., Emran T.B., et al. Biological evaluation, DFT calculations and molecular docking studies on the antidepressant and cytotoxicity activities of Cycas pectinata Buch. - Ham. Compounds. Pharmaceuticals. 2020;13:232. doi: 10.3390/ph13090232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tejera D., Heneka M.T. Microglia. Springer; New York, NY, USA: 2019. Microglia in Neurodegenerative Disorders; pp. 57–67. [DOI] [PubMed] [Google Scholar]
- 126.Abdel-Magied N., Shedid S.M. The Effect of Naringenin on the Role of Nuclear Factor (Erythroid-derived 2)-like2 (Nrf2) and Haem Oxygenase 1 (HO-1) in Reducing the Risk of Oxidative Stress-related Radiotoxicity in the Spleen of Rats. Environ. Toxicol. 2019;34:788–795. doi: 10.1002/tox.22745. [DOI] [PubMed] [Google Scholar]
- 127.Drishya S., Dhanisha S.S., Raghukumar P., Guruvayoorappan C. Amomum Subulatum Mitigates Total Body Irradiation-Induced Oxidative Stress and Associated Inflammatory Responses by Enhancing the Antioxidant Status and Regulating pro-Inflammatory Cytokines. J. Nutr. Biochem. 2022;107:109064. doi: 10.1016/j.jnutbio.2022.109064. [DOI] [PubMed] [Google Scholar]
- 128.Saha S., Buttari B., Panieri E., Profumo E., Saso L. An Overview of Nrf2 Signaling Pathway and Its Role in Inflammation. Molecules. 2020;25:5474. doi: 10.3390/molecules25225474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Li M., Fu Q., Li Y., Li S., Xue J., Ma S. Emodin Opposes Chronic Unpredictable Mild Stress Induced Depressive-like Behavior in Mice by Upregulating the Levels of Hippocampal Glucocorticoid Receptor and Brain-Derived Neurotrophic Factor. Fitoterapia. 2014;98:1–10. doi: 10.1016/j.fitote.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 130.Mitra S., Anjum J., Muni M., Das R., Rauf A., Islam F., Emran T.B., Semwal P., Hemeg H.A., Alhumaydhi F.A. Exploring the Journey of Emodin as a Potential Neuroprotective Agent: Novel Therapeutic Insights with Molecular Mechanism of Action. Biomed. Pharmacother. 2022;149:112877. doi: 10.1016/j.biopha.2022.112877. [DOI] [PubMed] [Google Scholar]
- 131.Mitra S., Lami M.S., Uddin T.M., Das R., Islam F., Anjum J., Hossain M.J., Emran T.B. Prospective multifunctional roles and pharmacological potential of dietary flavonoid narirutin. Biomed. Pharmacother. 2022;150:112932. doi: 10.1016/j.biopha.2022.112932. [DOI] [PubMed] [Google Scholar]
- 132.Halbreich U., Kahn L.S. Role of Estrogen in the Aetiology and Treatment of Mood Disorders. CNS Drugs. 2001;15:797–817. doi: 10.2165/00023210-200115100-00005. [DOI] [PubMed] [Google Scholar]
- 133.Bruce M.L., Raue P.J. Handbook of the Sociology of Mental Health. Springer; Berlin/Heidelberg, Germany: 2013. Mental Illness as Psychiatric Disorder; pp. 41–59. [Google Scholar]
- 134.Evans D.L., Foa E.B., Gur R.E., Hendin H., O’Brien C.P., Seligman M.E.P., Walsh B.T. Treating and Preventing Adolescent Mental Health Disorders: What We Know and What We Don’t Know. Oxford University Press; Oxford, UK: 2005. [Google Scholar]
- 135.Chtourou Y., Gargouri B., Kebieche M., Fetoui H. Naringin Abrogates Cisplatin-Induced Cognitive Deficits and Cholinergic Dysfunction through the down-Regulation of AChE Expression and INOS Signaling Pathways in Hippocampus of Aged Rats. J. Mol. Neurosci. 2015;56:349–362. doi: 10.1007/s12031-015-0547-0. [DOI] [PubMed] [Google Scholar]
- 136.Kwatra M., Jangra A., Mishra M., Sharma Y., Ahmed S., Ghosh P., Kumar V., Vohora D., Khanam R. Naringin and Sertraline Ameliorate Doxorubicin-Induced Behavioral Deficits through Modulation of Serotonin Level and Mitochondrial Complexes Protection Pathway in Rat Hippocampus. Neurochem. Res. 2016;41:2352–2366. doi: 10.1007/s11064-016-1949-2. [DOI] [PubMed] [Google Scholar]
- 137.Tallei T.E., Niode N.J., Idroes R., Zidan B.M.R.M., Mitra S., Celik I., Nainu F., Ağagündüz D., Emran T.B., Capasso R.A. Comprehensive Review of the Potential Use of Green Tea Polyphenols in the Management of COVID-19 Evid-based Complement. Altern. Med. 2021;2021:7170736. doi: 10.1155/2021/7170736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.D’Angelo S., Mele E., Di Filippo F., Viggiano A., Meccariello R. Sirt1 Activity in the Brain: Simultaneous Effects on Energy Homeostasis and Reproduction. Int. J. Environ. Res. Public Health. 2021;18:1243. doi: 10.3390/ijerph18031243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bhattacharya I., Domínguez A.P., Drägert K., Haas E., Battegay E.J. Hypoxia Potentiates Tumor Necrosis Factor-α Induced Expression of Inducible Nitric Oxide Synthase and Cyclooxygenase-2 in White and Brown Adipocytes. Biochem. Biophys. Res. Commun. 2015;461:287–292. doi: 10.1016/j.bbrc.2015.04.020. [DOI] [PubMed] [Google Scholar]
- 140.Matheus M.E., de Almeida Violante F., Garden S.J., Pinto A.C., Fernandes P.D. Isatins Inhibit Cyclooxygenase-2 and Inducible Nitric Oxide Synthase in a Mouse Macrophage Cell Line. Eur. J. Pharmacol. 2007;556:200–206. doi: 10.1016/j.ejphar.2006.10.057. [DOI] [PubMed] [Google Scholar]
- 141.Shin J.-S., Park Y.M., Choi J.-H., Park H.-J., Shin M.C., Lee Y.S., Lee K.-T. Sulfuretin Isolated from Heartwood of Rhus Verniciflua Inhibits LPS-Induced Inducible Nitric Oxide Synthase, Cyclooxygenase-2, and pro-Inflammatory Cytokines Expression via the down-Regulation of NF-ΚB in RAW 264.7 Murine Macrophage Cells. Int. Immunopharmacol. 2010;10:943–950. doi: 10.1016/j.intimp.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 142.Feifel D., Shilling P.D., MacDonald K. A Review of Oxytocin’s Effects on the Positive, Negative, and Cognitive Domains of Schizophrenia. Biol. Psychiatry. 2016;79:222–233. doi: 10.1016/j.biopsych.2015.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lisman J.E., Coyle J.T., Green R.W., Javitt D.C., Benes F.M., Heckers S., Grace A.A. Circuit-Based Framework for Understanding Neurotransmitter and Risk Gene Interactions in Schizophrenia. Trends Neurosci. 2008;31:234–242. doi: 10.1016/j.tins.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Obrosova I.G. Diabetes and the Peripheral Nerve. Biochim. Biophys. Acta Mol. Basis Dis. 2009;1792:931–940. doi: 10.1016/j.bbadis.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 145.Howes O., McCutcheon R., Stone J. Glutamate and Dopamine in Schizophrenia: An Update for the 21st Century. J. Psychopharmacol. 2015;29:97–115. doi: 10.1177/0269881114563634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Li P.-F., Dietz R., von Harsdorf R. P53 Regulates Mitochondrial Membrane Potential through Reactive Oxygen Species and Induces Cytochrome C-Independent Apoptosis Blocked by Bcl-2. EMBO J. 1999;18:6027–6036. doi: 10.1093/emboj/18.21.6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zou W., Xiao Z., Wen X., Luo J., Chen S., Cheng Z., Xiang D., Hu J., He J. The Anti-Inflammatory Effect of Andrographis paniculata (Burm. f.) Nees on Pelvic Inflammatory Disease in Rats through down-Regulation of the NF-ΚB Pathway. BMC Complement. Altern. Med. 2016;16:483. doi: 10.1186/s12906-016-1466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Stenvinkel P., Ketteler M., Johnson R.J., Lindholm B., Pecoits-Filho R., Riella M., Heimbürger O., Cederholm T., Girndt M. IL-10, IL-6, and TNF-α: Central Factors in the Altered Cytokine Network of Uremia—The Good, the Bad, and the Ugly. Kidney Int. 2005;67:1216–1233. doi: 10.1111/j.1523-1755.2005.00200.x. [DOI] [PubMed] [Google Scholar]
- 149.Yao Q., Pecoits-Filho R., Lindholm B., Stenvinkel P. Traditional and Non-Traditional Risk Factors as Contributors to Atherosclerotic Cardiovascular Disease in End-Stage Renal Disease. Scand. J. Urol. Nephrol. 2004;38:405–416. doi: 10.1080/00365590410031715. [DOI] [PubMed] [Google Scholar]
- 150.Higley M.J., Picciotto M.R. Neuromodulation by Acetylcholine: Examples from Schizophrenia and Depression. Curr. Opin. Neurobiol. 2014;29:88–95. doi: 10.1016/j.conb.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Futamura T., Toyooka K., Iritani S., Niizato K., Nakamura R., Tsuchiya K., Someya T., Kakita A., Takahashi H., Nawa H. Abnormal Expression of Epidermal Growth Factor and Its Receptor in the Forebrain and Serum of Schizophrenic Patients. Mol. Psychiatry. 2002;7:673–682. doi: 10.1038/sj.mp.4001081. [DOI] [PubMed] [Google Scholar]
- 152.Zhong J., Yu R., Zhou Q., Liu P., Liu Z., Bian Y. Naringenin Prevents TNF-α-Induced Gut-Vascular Barrier Disruption Associated with Inhibiting the NF-ΚB-Mediated MLCK/p-MLC and NLRP3 Pathways. Food Funct. 2021;12:2715–2725. doi: 10.1039/D1FO00155H. [DOI] [PubMed] [Google Scholar]
- 153.Bitanihirwe B.K.Y., Woo T.-U.W. Oxidative Stress in Schizophrenia: An Integrated Approach. Neurosci. Biobehav. Rev. 2011;35:878–893. doi: 10.1016/j.neubiorev.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Jarskog L.F., Glantz L.A., Gilmore J.H., Lieberman J.A. Apoptotic Mechanisms in the Pathophysiology of Schizophrenia. Prog. Neuro-Psychopharmacology Biol. Psychiatry. 2005;29:846–858. doi: 10.1016/j.pnpbp.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 155.Missonnier P., Hasler R., Perroud N., Herrmann F.R., Millet P., Richiardi J., Malafosse A., Giannakopoulos P., Baud P. EEG Anomalies in Adult ADHD Subjects Performing a Working Memory Task. Neuroscience. 2013;241:135–146. doi: 10.1016/j.neuroscience.2013.03.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used to support the findings of this study are included within the article.