Abstract
Background: Instability is a common complication following total hip arthroplasty (THA). The dual mobility cup (DMC) allows a reduction in the dislocation rate. The goal of this systematic review was to clarify the different uses and outcomes according to the indications of the cemented DMC (C-DMC). Methods: A systematic review was performed using the keywords “Cemented Dual Mobility Cup” or “Cemented Tripolar Cup” without a publication year limit. Of the 465 studies identified, only 56 were eligible for the study. Results: The overall number of C-DMC was 3452 in 3426 patients. The mean follow-up was 45.9 months (range 12–98.4). In most of the cases (74.5%) C-DMC was used in a revision setting. In 57.5% DMC was cemented directly into the bone, in 39.6% into an acetabular reinforcement and in 3.2% into a pre-existing cup. The overall dislocation rate was 2.9%. The most frequent postoperative complications were periprosthetic infections (2%); aseptic loosening (1.1%) and mechanical failure (0.5%). The overall revision rate was 4.4%. The average survival rate of C-DMC at the last follow-up was 93.5%. Conclusions: C-DMC represents an effective treatment option to limit the risk of dislocations and complications for both primary and revision surgery. C-DMC has good clinical outcomes and a low complication rate.
Keywords: hip arthroplasty, dual mobility cup, cemented dual mobility, dislocation, instability, hip revision
1. Introduction
The use of the dual mobility cup (DMC) is an established practice in hip replacement surgery, which could ensure higher implant stability, physiological mobility of the hip joint and reduce wear. DMC is considered one of the major current strategies to prevent and treat hip instability, which is the first reason for total hip arthroplasty (THA) revision. The excellent long-term results of DMC justify their steady increase in recent years, both in primary complex cases and in recurrent hip instability after THA [1,2,3,4,5].
DMC can be used as the first implant surgery in complex cases of osteoarthritis (OA), including obese patients or those with neuromuscular or neurological diseases; and in fractures, such as acetabular fractures, femoral neck fractures (FNF), or pathological fractures [6,7,8,9]. Another common use of DMC is in revision surgery of total or partial hip arthroplasties or following the failure of a previous osteosynthesis [10,11].
In complex cases, including bone defects, DMC can be cemented directly into the bone or acetabular brace, such as primary or revision surgery [12,13]. While many reviews in the literature investigate and describe DMC [14,15], there is no specific analysis of cemented DMC (C-DMC).
The study aims to provide a systematic review concerning the C-DMC and a specific analysis of its application, in terms of complications, clinical results, survivorship rate, and radiographic findings. Secondary objectives are to describe the outcomes of primary and revision surgery and with or without acetabular reinforcement.
2. Materials and Methods
2.1. Search Strategy and Design
A systematic literature review was performed following the 2009 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines. The following online electronic databases were used: Cochrane Database of Systematic Reviews, PubMed, EMBASE and Google Scholar. The search strategy had no data limit and was conducted until 31 December 2021. The following keywords, and their MeSH terms in any possible combination, were used: “Cemented Dual Mobility Cup” OR “Cemented Tripolar Cup”. A minimum mean follow-up of 1 year was considered to allow the evaluation of all early complications and outcomes.
2.2. Eligibility Criteria
Inclusion criteria were (1) patients undergoing C-DMC for any reason; (2) all levels of evidence; (3) full-text articles in indexed journals; (4) studies in English; (4) human studies; (5) mean follow-up of at least 12 months. Exclusion criteria were (1) nonoperative studies; (2) studies using different types of cups; (3) studies in which C-DMC was been used in less than 10% of cases; (4) studies in which DMC data were not specifically described; (5) reviews; (6) surveys or case reports; (7) book chapters; (8) congress abstract; (9) surgical technical reports; (10) expert opinions or letters to the editor; (11) cadaveric or animal studies.
2.3. Study Selection
The study selection was conducted by two independent reviewers (C.G. and M.G.). Articles were identified based on the title and abstract. If necessary, full-text articles were obtained to screen. After excluding the unacceptable studies, the full texts of the remaining studies were assessed. Any disagreements between reviewers were resolved through discussion with a third author (D.E.). Finally, the included articles’ references have been evaluated to highlight further relevant items useful for the search. In the case of multiple studies involving the same case series with different follow-ups, only the manuscript with the longest follow-up was selected.
2.4. Data Extraction and Analysis
A standard data extraction form was used which included the following: (1) study details: author, year, country, study design, level of evidence; (2) study population: cohort, population size, gender, age at the time of surgery, body mass index (BMI); (3) follow-up information: patients at follow-up, mean follow-up, patients lost to follow-up; (4) surgical approach to the hip; (5) C-DMC information: number, implant, cement, graft, primary or revision procedure, “cup-in-cup” technique, acetabular reinforcement; (6) outcomes: preoperative and postoperative Harris Hip Score (HSS), postoperative Postel Merle d’Aubigné (PMA); (7) postoperative complications: mechanical failures, aseptic loosening, infections, dislocations, intra-prosthetic dislocations (IPD); (8) radiographic complications: peri-acetabular radiolucent lines (RLLs), Brooker heterotopic ossification (HO); (9) survivorship rate. In the presence of comparative studies, in which the C-DMC are compared with different treatment techniques, only the C-DMC data were obtained for the study; while in the presence of overall values with the other different cups, these values were not taken into consideration for the statistics.
2.5. Methodological Quality Assessment
The study quality of all included studies was evaluated using the MINORS (Methodological Index for Non-Randomized Studies) criteria. Each item was scored from 0 to 2, with maximum scores of 16 for non-comparative studies and 24 for comparative studies. Each study included was scored by 2 authors (C.G. and M.G.).
2.6. Statistical Analysis
The kappa (k) value was used to evaluate consensus among reviewers in item selection. The agreement was classified as poor when k < 0.30, partial 0.30 < k < 0.60 and total with k > 0.60. Given the high heterogeneity among the studies, a meta-analysis was not performed; however, indirect comparisons were made.
3. Results
3.1. Literature Search and Study Characteristics
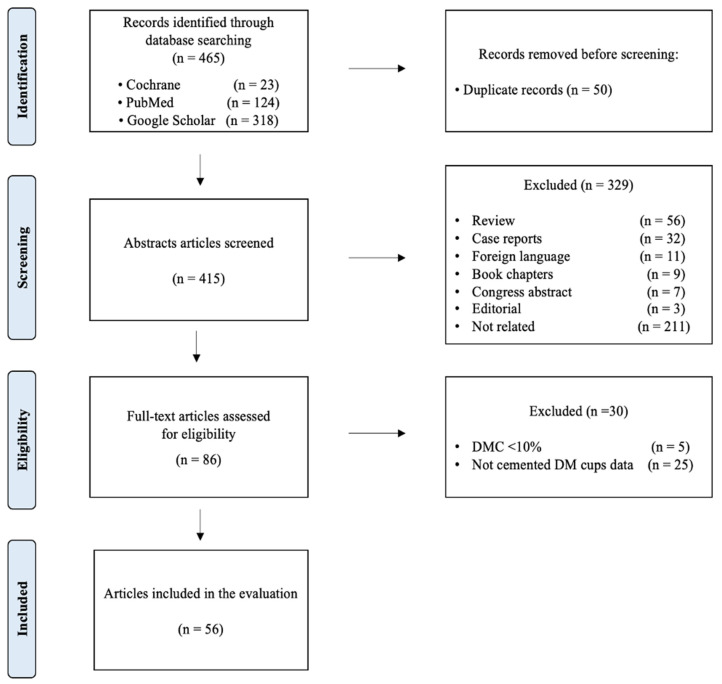
The initial search found 465 studies. After removing the duplicates, the remaining items were screened based on the title and abstract. The full texts of the remaining 86 articles were examined. Finally, according to the eligibility criteria, 56 articles were included in the systematic review [12,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] (Figure 1).
Figure 1.
Prisma Flowchart from the identification to the inclusion.
Among the reviewers, there was excellent agreement involving the title (k = 0.90; 95% CI, 0.88 to 0.92), the abstract (k = 0.91; 95% CI, 0.89 to 0.93), and the full text (k = 0.93; 95% CI, 0.92 to 0.94). Of the selected articles published between 2008 and 2021, ten reports are comparative studies (17.9%).
Most of the studies were retrospective (n = 44, 78.6%), while the remaining were prospective (n = 12, 21.4%). Forty-two (75%) studies were level IV evidence, 12 (21.4%) studies were level III, and two (3.6%) studies were level I.
The mean MINORS score was 11 (range 10–14) and 20 (range 17–24), for the non-comparative and comparative studies, respectively.
Most of the studies were conducted in France (28.1%), Egypt and the United States (both 10.7%) (Table 1).
Table 1.
Characteristics of studies included in the review.
| Author | Year | Nationality | Type | Level of Evidence | Number of Patiens | Males | Females | Mean Age (SD) [Range] | BMI (kg/m2) (SD) [Range] | Cemented DMC | Patients at Follow-Up |
Follow-up (Months) (SD) [Range] | MINORS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Langlais | 2008 | france | Retrospective | IV | 82 | / | / | 72 [65–86] | / | 88 | 79 | 36 [24–60] | 12 |
| Philippot | 2009 | france | Retrospective | IV | 51 | / | / | 68.7 [34–92] | / | 51 | 51 | 60.4 (±17.6) [24–112] | 12 |
| Tarasevicius | 2010 | Sweden | Retrospective comparative | III | 42 | / | / | 75 (±10) | 42 | 42 | 12 | 19 | |
| Schneider | 2011 | France | Retrospective | IV | 96 | 25 | 71 | 69.9 [34–95] | / | 96 | 77 | 41 (±29) [1–101] | 11 |
| Civinini | 2012 | Italy | Prospective | IV | 24 | / | / | 69 [51.3–82.4] | / | 24 | 24 | 39.6 [24–60] | 14 |
| Hailer | 2012 | Sweden | Retrospective | IV | 200 | / | / | / | / | 200 | 200 | 24 | 10 |
| Pattyn | 2012 | Belgium | Retrospective | IV | 36 | 16 | 20 | 70.4 [46–93] | / | 37 | 36 | 16 [6–27] | 11 |
| Mukka | 2013 | Sweden | Retrospective | IV | 34 | 13 | 21 | 75.7 [58–90] | / | 34 | 34 | 18 [6–36] | 11 |
| Toro-Ibarguen | 2014 | Spain | Retrospective | IV | 14 | / | / | 67.8 [29–90] | / | 14 | 14 | 64.8 | 10 |
| Wegrzyn | 2014 | france | Prospective | IV | 61 | 29 | 32 | 67 (±10) | 26 (±9) | 61 | 61 | 89 (±23) [60–138] | 10 |
| Haen | 2015 | France | Retrospective | IV | 64 | / | / | 79.8 (±11.1) [40–95] | / | 66 | 42 | 50.4 | 12 |
| Simian | 2015 | France | Retrospective | IV | 47 | / | / | 67.9 (±9.3) [38–90] | / | 47 | 47 | 87.6 [60–137] | 11 |
| van Heumen | 2015 | The Netherlands | Retrospective | IV | 46 | / | / | 67 [32–90] | 27.2 [16.6–43.0] | 46 | 46 | 29 [12–66] | 11 |
| Carulli C | 2016 | Italy | Retrospective | IV | 11 | 13 | 18 | 75.4 [71–86] | / | 11 | 11 | 45.6 [24–84] | 11 |
| Luthra | 2016 | Oman | Retrospective | IV | 63 | 35 | 30 | 61 [23–91] | / | 63 | 63 | 60 [18–72] | 11 |
| Plummer | 2016 | USA | Retrospective | IV | 11 | / | / | 64 (42–87) | 28.6 [20.8–43.6] | 11 | 11 | 28.8 [24–48] | 12 |
| Hamadouche | 2017 | France | Retrospective | IV | 51 | 12 | 39 | 71.4 (±11.5) [41.1–91.8] | 26.4 (±6.5) [17.6–56.6] | 51 | 30 | 98.4 [60–156] | 10 |
| Lebeau | 2017 | France | Retrospective | IV | 62 | 20 | 42 | 70.5 (±11.1) [36–94] | 27.2 (±4.8) [19.5–43] | 62 | 62 | 76.8 [60–108] | 10 |
| Mohaddes | 2017 | Sweden | Retrospective comparative | III | 436 | 154 | 282 | 75 (±9) | / | 436 | 436 | 37.2 | 20 |
| Nabil | 2017 | Egypt | Prospective | IV | 12 | / | / | 56.6 [34–63] | / | 12 | 12 | 24 | 20 |
| Stambough | 2017 | USA | Retrospective | IV | 8 | / | / | 60.6 [51–71] | / | 8 | 8 | 34.8 [24–63.6] | 12 |
| Bruggemann | 2018 | Sweden | Retrospective comparative | III | 69 | 34 | 35 | 67 [35–88] | / | 69 | 44 | 58.8 [6–106.8] | 17 |
| Chalmers | 2018 | USA | Retrospective | IV | 18 | 6 | 12 | 64 [37–81] | 28 [19–47] | 18 | 18 | 36 [24–60] | 12 |
| Evangelista | 2018 | USA | Retrospective | IV | 18 | 9 | 9 | 62 [30–86] | 29 [19–37] | 18 | 16 | 36 [25–56] | 11 |
| Hipfl | 2018 | Germany | Retrospective | IV | 15 | / | / | 70 [42–85] | 26 [17–38] | 15 | 15 | 47 [25–84] | 11 |
| Kavcic | 2018 | Slovenia | Retrospective | IV | 174 | 47 | 127 | 76.8 [54–98] | / | 174 | 156 | 92.4 [60–120] | 11 |
| Ozden | 2018 | Turkey | Prospective | IV | 14 | 3 | 11 | 64.5 [33–89] | 28.8 (±5.2) [18.7–36.2] | 15 | 14 | 38.1 [24–98] | 13 |
| Rashed | 2018 | Egypt | Prospective | IV | 31 | 16 | 15 | 66.4 (± 5.9) | / | 32 | 31 | 12 | 13 |
| Spaans | 2018 | The Netherlands | Retrospective comparative | III | 96 | 38 | 58 | 73.1 (±8.5) | 26.3 (4.5) | 102 | 96 | 27.6 [3–84] | 19 |
| Stucinskas | 2018 | Lithuanian | Retrospective | IV | 236 | 96 | 151 | 72 (±12) | / | 236 | 236 | 24 | 10 |
| Tabori-Jensen | 2018 | Denmark | Prospective comparative | III | 56 | 10 | 46 | 76.5 (42–93) | / | 56 | 56 | 36 | 19 |
| Wegrzyn | 2018 | France | Prospective | IV | 126 | 48 | 78 | 64 (±13) | 24 (±4) | 131 | 126 | 33 (±17) | 12 |
| Assi | 2019 | Lebanon | Retrospective comparative | III | 16 | 3 | 13 | 69.2 (±14.8) | / | 16 | 16 | 72.9 (±40.5) | 20 |
| Dikmen | 2019 | Turkey | Prospective | IV | 30 | 3 | 27 | 66.1 [33–89] | 26.8 (±7.2) [19.7–36.2] | 30 | 30 | 42.2 [24.6–75.1] | 12 |
| Fathy | 2019 | Egypt | Prospective | IV | 20 | 12 | 8 | 66.8 [55–80] | / | 20 | 20 | 24 | 14 |
| Gabor | 2019 | USA | Retrospective | IV | 38 | 18 | 20 | 62.7 (±9.7) | 29.7 (±7.0) | 38 | 38 | 17.9 | 10 |
| Giunta | 2019 | France | Retrospective | IV | 27 | 23 | 4 | 68.5 (±8.1) [60–84] | / | 27 | 25 | 48 [12–84] | 12 |
| Plummer | 2019 | USA | Retrospective | IV | 19 | / | / | 64 [48–81] | 27.9 [18.5–38] | 19 | 13 | 24 | 12 |
| Schmidt-Braekling | 2019 | Germany | Retrospective | IV | 79 | 24 | 55 | 68.5 [41–87] | 26.8 [18.6–41.5] | 79 | 71 | 63.6 [24–122.4] | 12 |
| Wheelton | 2019 | England (UK) | Retrospective | IV | 54 | 12 | 42 | 78 [49–97] | / | 54 | 54 | 22.8 [6–60] | 11 |
| de l’Escalopier | 2020 | France | Retrospective | III | 76 | 23 | 58 | 71 [31–90] | 25.2 [17.2–38] | 76 | 63 | 76.8 [36–144] | 10 |
| Lannes | 2020 | Switzerland | Retrospective comparative | III | 26 | 15 | 11 | 78 (±6) [66–88] | / | 26 | 25 | 12 [1–96] | 19 |
| Lavignac | 2020 | France | Retrospective | IV | 71 | 27 | 64 | 62 (±10.5) [38–88] | / | 71 | 71 | 28.2 (±2.9) [0.3–124.8] | 10 |
| Mahmoud | 2020 | Egypt | Prospective | IV | 20 | 11 | 9 | 65.85 (±5.58) [58–78] | / | 20 | 20 | 24 | 14 |
| Sayac | 2020 | France | Retrospective | IV | 74 | 24 | 50 | 70 (±11.3) [34–88] | / | 77 | 39 | 128.4 [25.2–194.4] | 12 |
| Schmidt | 2020 | France | Retrospective comparative | IV | 59 | / | / | 69 (±13.2) [19–92] | 26.5 (±5.1) [17–46] | 59 | 59 | 24 [12–141.6] | 20 |
| Tabori-Jensen | 2020 | Denmark | Prosective randomized trial | I | 29 | 14 | 15 | 75 [70–82] | 28 [23–39] | 29 | 29 | 24 | 24 |
| Wegrzyn | 2020 | Switzerland | Retrospective | IV | 28 | 17 | 11 | 82 [74–93] | 25 [20–39] | 28 | 28 | 42 [24–60] | 12 |
| Bellova | 2021 | Germany | Retrospective | IV | 33 | / | / | 78.6 (±7.1) [63–93] | / | 33 | 19 | 28.5 (±17.3) [3–64] | 10 |
| Bozon | 2021 | france | Retrospective comparative | III | 23 | 12 | 11 | 67 (±10) | 24 (±3) | 23 | 23 | 108 (±12) | 18 |
| Elkhadrawe | 2021 | Egypt | Prospective | IV | 31 | 16 | 15 | 66.6 (±6.3) | / | 32 | 30 | 12 | 13 |
| Lamo Espinosa | 2021 | Spain | Retrospective | IV | 68 | 15 | 53 | 81.7 (± 6.4) | / | 68 | 68 | 49 (±22.6) | 12 |
| Moreta | 2021 | Spain | Retrospective | IV | 10 | / | / | 79.2 [71–87] | 27.5 [19–34] | 10 | 10 | 42 [24–72] | 12 |
| Rashed | 2021 | Egypt | Prospective | I | 31 | 16 | 15 | 66.38 [63.9–68.7] | / | 31 | 30 | 12 | 23 |
| Unter Ecker | 2021 | Germany | Retrospective | III | 216 | 96 | 120 | 69 (±9) | 29 (±7) | 216 | 216 | 69 [60–110] | 10 |
| Uriarte | 2021 | Spain | Retrospective comparative | IV | 44 | 13 | 31 | 76.3 (±6.7) | 25.8 (±4.1) | 44 | 44 | 49.2 | 20 |
| Totals and proportions | 3426 | 1018 (37.1%) | 1729 (62.9%) | Mean: 26.8 kg/m2 | 3452 | 3239 (94.5%) |
3.2. Overall Demographic Data
The overall number of patients was 4675 (4701 hips). Finally, 3452 C-DMC in 3426 patients were found. The patients who reached the last follow-up and who were evaluated for clinical and radiographic outcomes are 3162 (92.3%).
Females are more represented (62.9%) than males (37.1%). The mean age at the time of surgery was of 71.5 years (mean range 67–82), only one study doesn’t have the mean age value. The mean follow-up was 45.9 months (range 12–98.4). The mean BMI was 26.8 kg/m2 (range 24–29.7) (Table 1, Table 2 and Table 3).
Table 2.
Cemented dual mobility cup: surgical information.
| Author | Year | Cemented DMC | Posterior Approach | Lateral Approach | Anterior Approach | Extensile Approach | Avantage (Zimmer Biomet) | Polarcup (Smith and Nephew) | Ecofit (Implantcast) | Tornier | ADM (Stryker) | MDM (Stryker) | Medial Cup (Aston Medical) | SaturneTM (Amplitude) | Novae (SERF) | Symbol Cup DM (Dedienne santé) | Quattro (Lepine) | Apogee (Biotechni Inc.) | ADES (ZimmerBiomet) | DMS (SEM) | Cement Palacos R+G (Heraeus) | CMW Type 3 with Gentamycin (DePuy) | Antibiotic-Loaded Cement Simplex (Stryker) | Graft | AutoGraft | AlloGraft | Synthetic Graft |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Langlais | 2008 | 88 | 40 | 0 | 0 | 48 | 0 | 0 | 0 | 0 | 0 | 0 | 88 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Philippot | 2009 | 51 | / | / | / | / | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 51 | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | / | / |
| Tarasevicius | 2010 | 42 | 42 | 0 | 0 | 0 | 42 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Schneider | 2011 | 96 | 96 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 96 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 91 | 0 | 0 | 0 |
| Civinini | 2012 | 24 | / | / | / | / | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | / | / | / | 0 | 0 | 1 | 0 | 0 | 30 | 0 | 30 | 0 |
| Hailer | 2012 | 200 | / | / | / | / | 200 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pattyn | 2012 | 37 | 37 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 37 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mukka | 2013 | 34 | 34 | 0 | 0 | 0 | 34 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Toro-Ibarguen | 2014 | 14 | / | / | / | / | 0 | 14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Wegrzyn | 2014 | 61 | 61 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 61 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 61 | 0 | 61 | 0 |
| Haen | 2015 | 66 | 66 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 66 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 3 | 1 | 2 | 0 |
| Simian | 2015 | 47 | 47 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 47 | 0 | 0 | 0 | 23 | 0 | 23 | 0 |
| van Heumen | 2015 | 46 | 46 | 0 | 0 | 0 | 46 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 0 |
| Carulli C | 2016 | 11 | 0 | 11 | 0 | 0 | 11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | / | / |
| Luthra | 2016 | 63 | 65 | 0 | 0 | 0 | 63 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Plummer | 2016 | 11 | 10 | 0 | 0 | 1 | 0 | 3 | 0 | 0 | 6 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hamadouche | 2017 | 51 | 17 | 3 | 0 | 31 | 0 | 0 | 0 | 0 | 0 | 0 | 51 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 15 | 1 | 13 | 1 |
| Lebeau | 2017 | 62 | 62 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 62 | 0 | 0 | 0 | 1 | 0 | 0 | 58 | 0 | 58 | 0 |
| Mohaddes | 2017 | 436 | 283 | 0 | 140 | 0 | 436 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Nabil | 2017 | 12 | 0 | 12 | 0 | 0 | / | / | / | / | / | / | / | / | / | / | / | / | / | / | 0 | 0 | 0 | 1 | 0 | 1 | 0 |
| Stambough | 2017 | 8 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Bruggemann | 2018 | 69 | 0 | 69 | 0 | 0 | 69 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 16 | 0 | 0 | 0 |
| Chalmers | 2018 | 18 | 11 | 0 | 7 | 0 | 0 | 0 | 0 | 0 | 18 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Evangelista | 2018 | 18 | 0 | 0 | 0 | 0 | 0 | 18 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hipfl | 2018 | 15 | 0 | 0 | 0 | 0 | 0 | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 15 | 0 | 15 | 0 |
| Kavcic | 2018 | 174 | 0 | 0 | 174 | 0 | 174 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ozden | 2018 | 15 | 15 | 0 | 0 | 0 | 0 | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 |
| Rashed | 2018 | 32 | 32 | 0 | 0 | 0 | 0 | 0 | 32 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Spaans | 2018 | 102 | 102 | 0 | 0 | 0 | 102 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 102 | 0 | 102 | 0 |
| Stucinskas | 2018 | 236 | 236 | 8 | 3 | 0 | 227 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Tabori-Jensen | 2018 | 56 | 56 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 56 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Wegrzyn | 2018 | 131 | 131 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 131 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Assi | 2019 | 16 | 16 | 0 | 0 | 0 | / | / | / | / | / | / | / | / | / | / | / | / | / | / | 0 | 0 | 0 | 16 | 0 | 0 | 0 |
| Dikmen | 2019 | 30 | 30 | 0 | 0 | 0 | 0 | 30 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 14 | 0 | 0 | 0 |
| Fathy | 2019 | 20 | 0 | 20 | 0 | 0 | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 |
| Gabor | 2019 | 38 | 27 | 11 | 0 | 0 | 0 | 38 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 18 | 0 | 18 | 0 |
| Giunta | 2019 | 27 | 27 | 0 | 6 | 0 | 0 | 0 | 0 | 27 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 6 | 0 | 0 |
| Plummer | 2019 | 19 | 19 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 19 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 19 | 0 | 0 | 19 |
| Schmidt-Braekling | 2019 | 79 | / | / | / | / | 60 | 0 | 19 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Wheelton | 2019 | 54 | 0 | 0 | 0 | 0 | / | / | / | / | / | / | / | / | / | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| de l’Escalopier | 2020 | 76 | 0 | 0 | 0 | 76 | 0 | 0 | 0 | 0 | 0 | 0 | 76 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 39 | 0 | 39 | 0 |
| Lannes | 2020 | 26 | 26 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 26 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lavignac | 2020 | 71 | 0 | 0 | 0 | 0 | / | / | / | / | / | / | / | / | / | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mahmoud | 2020 | 20 | 0 | 20 | 0 | 0 | / | / | / | / | / | / | / | / | / | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sayac | 2020 | 77 | 77 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 77 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Schmidt | 2020 | 59 | 59 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 59 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Tabori-Jensen | 2020 | 29 | 29 | 0 | 0 | 0 | 29 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Wegrzyn | 2020 | 28 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 28 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Bellova | 2021 | 33 | 33 | 0 | 0 | 0 | 0 | 29 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Bozon | 2021 | 23 | 23 | 0 | 0 | 0 | 0 | 0 | 0 | 23 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 21 | 0 | 21 | 0 |
| Elkhadrawe | 2021 | 32 | 32 | 0 | 0 | 0 | / | / | / | / | / | / | / | / | / | / | / | / | / | / | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lamo Espinosa | 2021 | 68 | 0 | 0 | 68 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 51 | 0 | 0 | 0 | 11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Moreta | 2021 | 10 | 4 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Rashed | 2021 | 31 | 31 | 0 | 0 | 0 | 0 | 0 | 31 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Unter Ecker | 2021 | 216 | 216 | 0 | 0 | 0 | 216 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Uriarte | 2021 | 44 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 44 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
Table 3.
Cemented dual mobility cup: surgical setting.
| Author | Year | Cemented DMC | Primary Setting | Revision Setting | No Acetabular Reinforcement | Acetabular Reinforcement | Cup-in-Cup |
|---|---|---|---|---|---|---|---|
| Langlais | 2008 | 88 | 0 | 88 | 7 | 81 | 0 |
| Philippot | 2009 | 51 | 0 | 51 | 0 | 51 | 0 |
| Tarasevicius | 2010 | 42 | 42 | 0 | 42 | 0 | 0 |
| Schneider | 2011 | 96 | 0 | 96 | 0 | 96 | 0 |
| Civinini | 2012 | 24 | 0 | 24 | 0 | 24 | 0 |
| Hailer | 2012 | 200 | 0 | 200 | / | / | 0 |
| Pattyn | 2012 | 37 | 0 | 37 | 0 | 37 | 0 |
| Mukka | 2013 | 34 | 9 | 25 | 34 | 0 | 0 |
| Toro-Ibarguen | 2014 | 14 | 0 | 14 | 0 | 14 | 0 |
| Wegrzyn | 2014 | 61 | 0 | 61 | 0 | 61 | 0 |
| Haen | 2015 | 66 | 32 | 34 | 66 | 0 | 0 |
| Simian | 2015 | 47 | 0 | 47 | 24 | 23 | 0 |
| van Heumen | 2015 | 46 | 0 | 46 | 46 | 0 | 0 |
| Carulli C | 2016 | 11 | 0 | 11 | 11 | 0 | 0 |
| Luthra | 2016 | 63 | 30 | 33 | 63 | 0 | 0 |
| Plummer | 2016 | 11 | 0 | 11 | 0 | 11 | 0 |
| Hamadouche | 2017 | 51 | 0 | 51 | 29 | 22 | 0 |
| Lebeau | 2017 | 62 | 0 | 62 | 0 | 62 | 0 |
| Mohaddes | 2017 | 436 | 0 | 436 | 436 | 0 | 0 |
| Nabil | 2017 | 12 | 12 | 0 | 11 | 1 | 0 |
| Stambough | 2017 | 8 | 0 | 8 | 0 | 0 | 8 |
| Bruggemann | 2018 | 69 | 0 | 69 | 0 | 69 | 0 |
| Chalmers | 2018 | 18 | 0 | 18 | 0 | 0 | 18 |
| Evangelista | 2018 | 18 | 0 | 18 | 0 | 0 | 18 |
| Hipfl | 2018 | 15 | 0 | 15 | 0 | 15 | 0 |
| Kavcic | 2018 | 174 | 173 | 1 | 174 | 0 | 0 |
| Ozden | 2018 | 15 | 0 | 15 | 6 | 9 | 0 |
| Rashed | 2018 | 32 | 32 | 0 | 32 | 0 | 0 |
| Spaans | 2018 | 102 | 0 | 102 | 102 | 0 | 0 |
| Stucinskas | 2018 | 236 | 0 | 236 | 236 | 0 | 0 |
| Tabori-Jensen | 2018 | 56 | 56 | 0 | 56 | 0 | 0 |
| Wegrzyn | 2018 | 131 | 131 | 0 | 0 | 131 | 0 |
| Assi | 2019 | 16 | 0 | 16 | 0 | 16 | 0 |
| Dikmen | 2019 | 30 | 0 | 30 | 11 | 19 | 0 |
| Fathy | 2019 | 20 | 0 | 20 | 20 | 0 | 0 |
| Gabor | 2019 | 38 | 0 | 38 | 27 | 11 | 0 |
| Giunta | 2019 | 27 | 27 | 0 | 4 | 23 | 0 |
| Plummer | 2019 | 19 | 19 | 0 | 0 | 19 | 0 |
| Schmidt-Braekling | 2019 | 79 | 0 | 79 | 0 | 79 | 0 |
| Wheelton | 2019 | 54 | 0 | 54 | 54 | 0 | 0 |
| de l’Escalopier | 2020 | 76 | 0 | 76 | 23 | 53 | 0 |
| Lannes | 2020 | 26 | 26 | 0 | 0 | 26 | 0 |
| Lavignac | 2020 | 71 | 71 | 0 | 0 | 71 | 0 |
| Mahmoud | 2020 | 20 | 15 | 5 | 20 | 0 | 0 |
| Sayac | 2020 | 77 | 0 | 77 | 0 | 77 | 0 |
| Schmidt | 2020 | 59 | 0 | 59 | 0 | 59 | 0 |
| Tabori-Jensen | 2020 | 29 | 29 | 0 | 29 | 0 | 0 |
| Wegrzyn | 2020 | 28 | 0 | 28 | 0 | 0 | 28 |
| Bellova | 2021 | 33 | 0 | 33 | 0 | 0 | 33 |
| Bozon | 2021 | 23 | 0 | 23 | 0 | 23 | 0 |
| Elkhadrawe | 2021 | 32 | 32 | 0 | 32 | 0 | 0 |
| Lamo Espinosa | 2021 | 68 | 68 | 0 | 68 | 0 | 0 |
| Moreta | 2021 | 10 | 0 | 10 | 0 | 0 | 10 |
| Rashed | 2021 | 31 | 31 | 0 | 31 | 0 | 0 |
| Unter Ecker | 2021 | 216 | 0 | 216 | NA | NA | NA |
| Uriarte | 2021 | 44 | 44 | 0 | 44 | 0 | 0 |
| Totals and proportions | 3452 | 879 (25.5%) | 2573 (74.5%) | 1738 (57.2%) | 1183 (39%) | 115 (3.8%) |
3.3. Operative Technique and Implants
Overall, 3452 C-DMCs are included. The posterolateral approach was the most used surgical approach (75.3%). The anterior approach was used in 14% of cases, the lateral approach in 5.3% of cases, and an extensive approach was used in 5.4% of cases. The most used implant was the Avantage dual mobility cup (Zimmer Biomet©, Warsaw, IN, USA), used in 17 studies and 54.2% of all cases, followed by the DM Novae cemented cup (Serf©, Décines-Charpieux, France) (7 studies, 14.2%) (Table 2 and Table 3).
3.4. Complications and Cup Survival Rate
The overall dislocation rate from 51 studies was 3.1%. The systematic review reported 7 cases of IPD, in four different studies. The overall IPD rate is 0.2%. The most frequent postoperative complications were periprosthetic infections (3%); aseptic loosening (1.3%) and mechanical failure (0.5%). A total of 138 revisions are reported (revision rate of 4%), in 48 studies reporting data eligible for the study. The average survival rate of the DMC at the last follow-up was evaluated in 43 studies (76.8%). At 45.9 months follow-up, the overall survival rate was 93.5% (range 83.1–100) (Table 4).
Table 4.
Cemented dual mobility cup: complications.
| Author | Year | C-DMC | Dislocations | Intra-Prosthetic Dislocations | Infection | Aseptic Loosening | Mechanical Failure | Revisions | Cup-Survivorship |
|---|---|---|---|---|---|---|---|---|---|
| Langlais | 2008 | 88 | 0 | 1 | 2 | 0 | 0 | 3 | 100% |
| Philippot | 2009 | 51 | 6 | 0 | 3 | 2 | 1 | / | 86.8% |
| Tarasevicius | 2010 | 42 | 0 | 0 | 0 | 0 | 0 | 0 | 87% |
| Schneider | 2011 | 96 | 11 | 0 | 5 | 1 | 2 | 4 | 96% |
| Civinini | 2012 | 24 | 0 | 0 | 1 | 0 | 0 | 1 | 100% |
| Hailer | 2012 | 200 | 3 | 0 | 4 | 4 | 2 | 10 | / |
| Pattyn | 2012 | 37 | 2 | 0 | 1 | 0 | 1 | 2 | 97% |
| Mukka | 2013 | 34 | 2 | 0 | 3 | 0 | 0 | 0 | 91.2% |
| Toro-Ibarguen | 2014 | 14 | 1 | 0 | / | / | / | / | 91.2% |
| Wegrzyn | 2014 | 61 | 0 | 0 | 0 | 0 | 1 | 0 | 96% |
| Haen | 2015 | 66 | 0 | 0 | 0 | 1 | 0 | 1 | 100% |
| Simian | 2015 | 47 | 1 | 0 | 6 | 0 | 0 | / | 100% |
| van Heumen | 2015 | 46 | 0 | 0 | 2 | 1 | 0 | 3 | 100% |
| Carulli C | 2016 | 11 | 0 | 0 | 0 | 0 | 0 | 0 | / |
| Luthra | 2016 | 63 | 1 | 0 | 1 | 0 | 0 | 1 | / |
| Plummer | 2016 | 11 | 1 | 0 | 2 | 0 | 2 | 4 | 98% |
| Hamadouche | 2017 | 51 | 1 | 2 | 2 | 2 | 0 | 7 | 93% |
| Lebeau | 2017 | 62 | 1 | 0 | 7 | 5 | 0 | 8 | 75.2% |
| Mohaddes | 2017 | 436 | 7 | 0 | 15 | 2 | 2 | 10 | 89% |
| Nabil | 2017 | 12 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Stambough | 2017 | 8 | 2 | 0 | 0 | 0 | 0 | / | 98.5% |
| Bruggemann | 2018 | 69 | 1 | 0 | 0 | 2 | 0 | 2 | 94.6% |
| Chalmers | 2018 | 18 | 2 | 1 | 0 | 0 | 0 | 2 | 92.3% |
| Evangelista | 2018 | 18 | 0 | 0 | 0 | 0 | 0 | 0 | / |
| Hipfl | 2018 | 15 | 1 | 0 | 2 | 0 | 0 | / | 91.9% |
| Kavcic | 2018 | 174 | 0 | 0 | 2 | 0 | 0 | 0 | 98% |
| Ozden | 2018 | 15 | 0 | 0 | 0 | 2 | 0 | 2 | 100% |
| Rashed | 2018 | 32 | 0 | 0 | 1 | 0 | 0 | 1 | 96% |
| Spaans | 2018 | 102 | 3 | 0 | 1 | 4 | 0 | 5 | / |
| Stucinskas | 2018 | 236 | 5 | 0 | 5 | 1 | 0 | 11 | / |
| Tabori-Jensen | 2018 | 56 | 1 | 0 | 0 | 1 | 0 | / | 100% |
| Wegrzyn | 2018 | 131 | 3 | 0 | 4 | 0 | 0 | 0 | 93% |
| Assi | 2019 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 98.80% |
| Dikmen | 2019 | 30 | 1 | 0 | 1 | 2 | 0 | 3 | / |
| Fathy | 2019 | 20 | 1 | 0 | 0 | 0 | 0 | 0 | 96.80% |
| Gabor | 2019 | 38 | 1 | 0 | 1 | 0 | 0 | 1 | 93.75 |
| Giunta | 2019 | 27 | 3 | 0 | 0 | 0 | 0 | 0 | / |
| Plummer | 2019 | 19 | 0 | 0 | 2 | 0 | 0 | 1 | 72.1% |
| Schmidt-Braekling | 2019 | 79 | 2 | 0 | 5 | 4 | 0 | 9 | 90% |
| Wheelton | 2019 | 54 | 0 | 0 | 1 | 0 | 0 | 1 | 95.8% |
| de l’Escalopier | 2020 | 76 | 2 | 3 | 2 | 1 | 0 | / | / |
| Lannes | 2020 | 26 | 2 | 0 | 2 | 0 | 0 | 2 | 85% |
| Lavignac | 2020 | 71 | 1 | 0 | 10 | 4 | 6 | / | 83.10% |
| Mahmoud | 2020 | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Sayac | 2020 | 77 | 7 | 0 | 2 | 3 | 0 | 6 | 85% |
| Schmidt | 2020 | 59 | 4 | 0 | / | / | / | 13 | 95.6% |
| Tabori-Jensen | 2020 | 29 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Wegrzyn | 2020 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | / |
| Bellova | 2021 | 33 | 2 | 0 | 1 | 0 | 1 | 2 | 97.3% |
| Bozon | 2021 | 23 | 1 | 0 | 3 | 2 | 0 | 2 | 93% |
| Elkhadrawe | 2021 | 32 | 0 | 0 | 1 | 0 | 0 | 1 | 98% |
| Lamo Espinosa | 2021 | 68 | 0 | 0 | 0 | 1 | 0 | 1 | / |
| Moreta | 2021 | 10 | 1 | 0 | 0 | 0 | 0 | 1 | 92.2% |
| Rashed | 2021 | 31 | 0 | 0 | 1 | 0 | 0 | 0 | / |
| Unter Ecker | 2021 | 216 | 24 | 0 | 0 | 0 | 0 | 17 | 100% |
| Uriarte | 2021 | 44 | 0 | 0 | 2 | 0 | 0 | 1 | / |
| Totals and proportions | 3452 | 107 (3.1%) | 7 (0.2%) | 103 (3%) | 45 (1.3%) | 18 (0.5%) | 138 (4%) | Mean: 93.5% | |
3.5. Radiographic Outcomes
Among the systematic review, 36 studies (64.3%) showed radiological information about peri-acetabular radiolucent lines (RLLs), and only 26 studies (46.4%) investigated Brooker HO. The rate of periacetabular RLLs was 3.2%, while the HO rate was 6.7% (Table 5).
Table 5.
Cemented dual mobility cup: radiographic and functional outcomes.
| Author | Patiens | Patients at Follow-Up | Acetabular Components Radiolucent Lines |
Brooker Heterotopic Ossification |
Pre-Operative HHS | Post-Operative HHS | Pre-Operative PMA | Post-Operative PMA |
|---|---|---|---|---|---|---|---|---|
| Langlais | 82 | 79 | 2 | / | 26.2 | 87.4 ± 12.1 | / | / |
| Philippot | 51 | 51 | / | / | / | 59.4 ± 22.2 (29–91) | / | / |
| Tarasevicius | 42 | 42 | 3 | / | / | 82 ± 18 (40–100) | 11 ± 3 | 15.5 ± 3 (11–18) |
| Schneider | 96 | 77 | 0 | / | / | 77 (25–100) | / | / |
| Civinini | 24 | 24 | 3 | 4 | / | / | / | / |
| Hailer | 200 | 200 | 0 | / | 47 (37–60) | 81 (62–98) | / | / |
| Pattyn | 36 | 36 | 15 | / | 48 (32–68) | 86 (66–95) | / | / |
| Mukka | 34 | 34 | 0 | / | / | / | 12.9 (5–18) | 16.3 (10–18) |
| Toro-Ibarguen | 14 | 14 | / | / | 42.8 ± 6.7 (34–60) | 87.3 ± 5.8 (75–98) | / | / |
| Wegrzyn | 61 | 61 | / | / | / | / | / | / |
| Haen | 64 | 42 | 0 | 2 | / | 92.6 ± 11.1 | / | / |
| Simian | 47 | 51 | / | / | 46 (40–79) | 65 (41–97) | / | / |
| van Heumen | 46 | 46 | 1 | / | 40 (23–44) | 86 (79–96) | / | / |
| Carulli C | 11 | 11 | 0 | / | 50 (35–78) | 78 (49–95) | / | / |
| Luthra | 63 | 63 | / | / | / | 70.4 ± 23 (24–90) | / | 14.3 ± 4.2 (7–18) |
| Plummer | 11 | 11 | 3 | 0 | / | / | / | 15.5 ± 1.9 (9–18) |
| Hamadouche | 51 | 30 | 0 | 0 | / | / | / | / |
| Lebeau | 62 | 62 | 9 | / | / | / | 13.5 ± 4.0 (8–18) | 16.3 ± 1.6 (13–18) |
| Mohaddes | 436 | 436 | 0 | / | 30 (15–51) | 71 (40–89) | / | / |
| Nabil | 12 | 12 | 0 | 0 | 31.7 (20–81) | 84.5 (32–100) | / | / |
| Stambough | 8 | 12 | / | / | / | / | 10.31 | 15.61 |
| Bruggemann | 69 | 44 | 3 | / | / | / | / | 16.1 |
| Chalmers | 18 | 18 | 0 | 6 | / | 72.36 ± 11.65 | / | / |
| Evangelista | 18 | 16 | / | / | / | / | / | / |
| Hipfl | 15 | 15 | 2 | / | 49 ± 16 (17–90) | 73 ± 21 (24–99) | 11 ± 3 (3–18) | 14.4 ± 3.6 (3–18) |
| Kavcic | 174 | 156 | 0 | 0 | / | / | / | / |
| Ozden | 14 | 14 | / | / | 25.95 ± 9.91 (14–44) | 92.45 ± 2.74 (88–98) | / | / |
| Rashed | 31 | 31 | / | / | / | / | / | / |
| Spaans | 96 | 96 | 0 | 0 | 49.3 (33–62) | 71.3 (22–91) | 10.1 | 12.8 |
| Stucinskas | 236 | 236 | / | / | / | 67 (±14) | / | / |
| Tabori-Jensen | 56 | 56 | / | 0 | 39.4 | 87.6 | / | / |
| Wegrzyn | 126 | 25 | 0 | 0 | 42 | 86 (49–93) | / | / |
| Assi | 16 | 16 | / | / | / | / | / | / |
| de l’Escalopier | 76 | 63 | 0 | 0 | 45 | 90 | / | / |
| Dikmen | 30 | 30 | 0 | 0 | 34 (27–41) | 82 (66–95) | / | / |
| Fathy | 20 | 20 | 2 | 0 | / | 92.8 (88.2–97.4) | / | / |
| Gabor | 38 | 38 | 0 | 2 | / | 92.8 (SD 11.1) | / | / |
| Giunta | 27 | 25 | 0 | 0 | 39.95 (6–84) | / | 8.05 (3–16) | / |
| Moreta | 10 | 10 | 4 | 29 | 39.5 ± 9.6 [37–43] | 71.3 ± 14 | 8.1 ± 2.5 [7–9] | 15.3 ± 2.2 [15–16] |
| Plummer | 19 | 13 | / | / | / | / | / | / |
| Sayac | 74 | 39 | / | / | / | 73.0 (24–99) | / | / |
| Schmidt | 59 | 59 | 6 | 17 | / | / | 9.6 ± 3.06 (2–16) | 15.5 ± 2.32 (7–18) |
| Schmidt-Braekling | 79 | 71 | 3 | 0 | / | 80.4 ± 12.9 (51–98) | / | 15.2 ± 2 (11–18) |
| Wheelton | 54 | 54 | / | / | / | / | / | / |
| Lannes | 26 | 25 | / | / | / | / | / | / |
| Lavignac | 71 | 91 | / | / | / | / | / | / |
| Mahmoud | 20 | 20 | 0 | 0 | 56 (±12) | 92 (8.7) | / | / |
| Rashed | 31 | 30 | 9 | 7 | / | 78.8 (31–100) | / | / |
| Tabori-Jensen | 29 | 29 | / | / | / | / | / | / |
| Wegrzyn | 28 | 28 | / | / | / | / | 5.48 (SD 2.41) | 10.5 (SD 3.82) |
| Bellova | 33 | 19 | 4 | 16 | / | 76.9 (16.8) | / | 13.1 (3.3) |
| Bozon | 23 | 23 | 0 | 0 | / | / | / | / |
| Elkhadrawe | 31 | 30 | 3 | 0 | 53 ± 19 | 79 ± 13 | / | / |
| Lamo Espinosa | 68 | 68 | 0 | 0 | 37 ± 8 | 84 ± 7 | / | / |
| Unter Ecker | 216 | 216 | 0 | 0 | 71 (69–74) | 88 (82–95) | / | / |
| Uriarte | 44 | 44 | / | 0 | / | / | / | / |
| Totals and proportions | 3426 | 3162 (92.3%) | 72 (3.2%) | 83 (6.7%) | Mean: 43 | Mean: 76.7 | Mean: 10.4 | Mean: 14.7 |
3.6. Functional Outcomes
The preoperative level of function was assessed with the HHS in 22 studies (59.3%). The mean preoperative HHS value was on average 43. The mean postoperative HHS value, evaluated in 34 studies (60.7%), was 76.7 (Table 5). The mean pre-operative PMA was 10.4 in 10 studies (17.9%). Instead, the post-operative PMA was 14.7, in 14 studies (25%) (Table 5).
3.7. Cemented Dual Mobility Cups in the Primary Setting
C-DMCs were used in 25.5% of cases as the primary setting, in 19 different studies (33.9%). In 40.5% of those cases, C-DMCs were used for the treatment of FNF, in 27.9% of cases as a treatment of OA complex cases, in 25.2% of cases as a treatment of pathological lesions (all cases of peri-acetabular metastasis cases except one case of pathological femur fracture) [59].
Finally, in 6.4% of the cases, a C-DMC was used in the treatment of acetabular fractures (Table 6).
Table 6.
Cemented dual mobility cup in the primary setting.
| Author | Year | C-DMC Primary Setting | Primary (FNF) | Primary (AO) | Primary (Oncology) | Primary (Acetabular Fracture) | No Acetabular Reinforcement | Acetabular Reinforcement | Dislocations | Intra-Prosthetic Dislocations | Revisions | Mechanical Failure | Aseptic Loosening | Infection | Posterior Approach | Lateral Approach | Anterior Approach | Cup-Survivorship |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tarasevicius | 2010 | 42 | 42 | 0 | 0 | 0 | 42 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 42 | 0 | 0 | 100% |
| Mukka | 2013 | 9 | 0 | 9 | 0 | 0 | 9 | 0 | 2 | 0 | 0 | 0 | 0 | 3 | 9 | 0 | 0 | 94.1% |
| Haen | 2015 | 32 | 12 | 20 | 0 | 0 | 32 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 32 | 0 | 0 | 98% [94–100] |
| Luthra | 2016 | 30 | 9 | 18 | 0 | 3 | 30 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 30 | 0 | 0 | 98% |
| Nabil | 2017 | 12 | 0 | 12 | 0 | 0 | 11 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | 0 | 100% |
| Kavcic | 2018 | 173 | 88 | 85 | 0 | 0 | 173 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 173 | 100% |
| Rashed | 2018 | 32 | 32 | 0 | 0 | 0 | 32 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 32 | 0 | 0 | 93.75% |
| Tabori-Jensen | 2018 | 56 | 56 | 0 | 0 | 0 | 56 | 0 | / | 0 | / | 0 | 1 | 0 | 56 | 0 | 0 | / |
| Wegrzyn | 2018 | 131 | 0 | 0 | 131 | 0 | 0 | 131 | 3 | 0 | 0 | 0 | 0 | 4 | 131 | 0 | 0 | / |
| Giunta | 2019 | 27 | 0 | 0 | 0 | 27 | 4 | 23 | 3 | 0 | 0 | 0 | 0 | 0 | 27 | 0 | 6 | / |
| Plummer | 2019 | 19 | 0 | 0 | 19 | 0 | 0 | 19 | 0 | 0 | 1 | 0 | 0 | 2 | 19 | 0 | 0 | / |
| Lannes | 2020 | 26 | 0 | 0 | 0 | 26 | 0 | 26 | 2 | 0 | 2 | 0 | 0 | 2 | 26 | 0 | 0 | 92.3% |
| Lavignac | 2020 | 71 | 0 | 0 | 71 | 0 | 0 | 71 | 1 | 0 | / | 6 | 4 | 10 | / | / | / | / |
| Mahmoud | 2020 | 15 | 10 | 4 | 1 | 0 | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 15 | 0 | 100% |
| Tabori-Jensen | 2020 | 29 | 0 | 29 | 0 | 0 | 29 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 29 | 0 | 0 | 100% |
| Elkhadrawe | 2021 | 32 | 32 | 0 | 0 | 0 | 32 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 32 | 0 | 0 | 100% |
| Lamo Espinosa | 2021 | 68 | 0 | 68 | 0 | 0 | 68 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 68 | 98.5% |
| Rashed | 2021 | 31 | 31 | 0 | 0 | 0 | 31 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 31 | 0 | 0 | / |
| Uriarte | 2021 | 44 | 44 | 0 | 0 | 0 | 44 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | / | / | / | 97.3% [93.5–100] |
| Totals and proportions | 879 | 356 (40.5%) | 245 (27.9%) | 222 (25.2%) | 56 (6.4%) | 608 (69.2%) | 271 (30.8%) | 12 (1.5%) | 0 | 9 (1.2%) | 6 (0.7%) | 7 (0.8%) | 29 (8.1%) | 496 (64.4%) | 27 (3.5%) | 247 (32.1%) | Mean: 98.5 % | |
3.8. Cemented Dual Mobility Cups in the Revision Setting
In 74.5% of cases, a C-DMC was used in the revision setting, such as the revision of previous THA or fixation failures. The use of C-DMC in revision cases was described in 42 studies (75%) (Table 7).
Table 7.
Cemented dual mobility cup in the revision setting.
| Author | Year | C-DMC Revision Setting | No Acetabular Reinforcement | Acetabular Reinforcement | Cup-in-Cup | Posterior/Posterolateral Approach | Lateral Approach | Anterior/Anterolateral Approach | Extensile Approach | Graft | Complications (Dislocations) | Complications (IPD) | Complications (Revisions) | Complications (Mechanical Failure) | Complications (Aseptic Loosening) | Complications (Infection) | Cup-Survivorship |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Langlais | 2008 | 88 | 7 | 81 | 0 | 40 | 0 | 0 | 48 | 0 | 0 | 1 | 3 | 0 | 0 | 2 | 94.6% |
| Philippot | 2009 | 51 | 0 | 51 | 0 | / | / | / | / | / | 6 | 0 | / | 1 | 2 | 3 | 98.8% |
| Schneider | 2011 | 96 | 0 | 96 | 0 | 96 | 0 | 0 | 0 | 91 | 11 | 0 | 4 | 2 | 1 | 5 | 95.6% (95% CI, 93.3–97.7%) |
| Civinini | 2012 | 24 | 0 | 24 | 0 | / | / | / | / | 30 | 0 | 0 | 1 | 0 | 0 | 1 | 97% (95% CI, 82–98%) |
| Hailer | 2012 | 200 | / | / | 0 | / | / | / | / | 0 | 3 | 0 | 10 | 2 | 4 | 4 | 93% (95% CI, 90–97%) |
| Pattyn | 2012 | 37 | 0 | 37 | 0 | 37 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 1 | 0 | 1 | / |
| Mukka | 2013 | 25 | 25 | 0 | 0 | 25 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 3 | 94.11% |
| Toro-Ibarguen | 2014 | 14 | 0 | 14 | 0 | / | / | / | / | 0 | 1 | 0 | / | / | / | / | / |
| Wegrzyn | 2014 | 61 | 0 | 61 | 0 | 61 | 0 | 0 | 0 | 61 | 0 | 0 | 0 | 1 | 0 | 0 | 98% |
| Haen | 2015 | 34 | 34 | 0 | 0 | 34 | 0 | 0 | 0 | 3 | 0 | 0 | 1 | 0 | 1 | 0 | 98% (95% CI, 94–100%) |
| Simian | 2015 | 47 | 24 | 23 | 0 | 47 | 0 | 0 | 0 | 23 | 1 | 0 | / | 0 | 0 | 6 | 90% (95% CI, 84–95%) |
| van Heumen | 2015 | 46 | 46 | 0 | 0 | 46 | 0 | 0 | 0 | 6 | 0 | 0 | 3 | 0 | 1 | 2 | 93% (95% CI, 79–98%) |
| Carulli C | 2016 | 11 | 11 | 0 | 0 | 0 | 11 | 0 | 0 | / | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Luthra | 2016 | 33 | 33 | 0 | 0 | 33 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 98% |
| Plummer | 2016 | 11 | 0 | 11 | 0 | 10 | 0 | 0 | 1 | 0 | 1 | 0 | 4 | 2 | 0 | 2 | / |
| Hamadouche | 2017 | 51 | 29 | 22 | 0 | 17 | 3 | / | 31 | 15 | 1 | 2 | 7 | 0 | 2 | 2 | 75.2 ± 9.3% (95% CI, 56.9–93.5%) |
| Lebeau | 2017 | 62 | 0 | 62 | 0 | 62 | 0 | 0 | 0 | 58 | 1 | 0 | 8 | 0 | 5 | 7 | 91.9% |
| Mohaddes | 2017 | 436 | 436 | 0 | 0 | 285 | / | 140 | / | 0 | 7 | 0 | 10 | 2 | 2 | 15 | 96% |
| Stambough | 2017 | 8 | 0 | 0 | 8 | 8 | 0 | 0 | 0 | 1 | 2 | 0 | / | 0 | 0 | 0 | 85% |
| Bruggemann | 2018 | 69 | 0 | 69 | 0 | 0 | 69 | 0 | 0 | 16 | 1 | 0 | 2 | 0 | 2 | 0 | 96% (95% CI, 90–100%) |
| Chalmers | 2018 | 18 | 0 | 0 | 18 | 11 | 0 | 7 | 0 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | / |
| Evangelista | 2018 | 18 | 0 | 0 | 18 | / | / | / | / | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Hipfl | 2018 | 15 | 0 | 15 | 0 | / | / | / | / | 15 | 1 | 0 | / | 0 | 0 | 2 | 89 (72–96) |
| Ozden | 2018 | 15 | 6 | 9 | 0 | 15 | 0 | 0 | 0 | 5 | 0 | 0 | 2 | 0 | 2 | 0 | 93% (95% CI, 88–98.7%) |
| Spaans | 2018 | 102 | 102 | 0 | 0 | 102 | 0 | 0 | 0 | 102 | 3 | 0 | 5 | 0 | 4 | 1 | 95.8% (3 months–7 years) (95% CI, 91.7–99.9%) |
| Stucinskas | 2018 | 236 | 236 | 0 | 0 | / | / | / | / | 0 | 5 | 0 | 11 | 0 | 1 | 5 | 95.14% |
| Assi | 2019 | 16 | 0 | 16 | 0 | 16 | 0 | 0 | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| de l’Escalopier | 2019 | 76 | 23 | 53 | 0 | 0 | 0 | 0 | 76 | 39 | 2 | 3 | / | 0 | 1 | 2 | 91.2 ± 3.8% |
| Dikmen | 2019 | 30 | 11 | 19 | 0 | 30 | 0 | 0 | 0 | 14 | 1 | 0 | 3 | 0 | 2 | 1 | 91.2% (95% CI, 81.6–100%) |
| Fathy | 2019 | 20 | 20 | 0 | 0 | 0 | 20 | 0 | 0 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 100% |
| Gabor | 2019 | 38 | 27 | 11 | 0 | 27 | 11 | 0 | 0 | 18 | 1 | 0 | 1 | 0 | 0 | 1 | / |
| Moreta | 2019 | 10 | 0 | 0 | 10 | 4 | 0 | 6 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | / |
| Sayac | 2019 | 77 | 0 | 77 | 0 | 77 | 0 | 0 | 0 | 0 | 7 | 0 | 6 | 0 | 3 | 2 | 92.2% |
| Schmidt | 2019 | 59 | 0 | 59 | 0 | 59 | 0 | 0 | 0 | 0 | 4 | 0 | 13 | / | / | / | 72.1% |
| Schmidt-Braekling | 2019 | 79 | 0 | 79 | 0 | / | / | / | / | 0 | 2 | 0 | 9 | 0 | 4 | 5 | 85% |
| Wheelton | 2019 | 54 | 54 | 0 | 0 | / | / | / | / | 0 | 0 | 0 | 1 | 0 | 0 | 1 | / |
| Mahmoud | 2020 | 5 | 5 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Wegrzyn | 2020 | 28 | 0 | 0 | 28 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Bellova | 2021 | 33 | 0 | 0 | 33 | 33 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 1 | 0 | 1 | 86.8% |
| Bozon | 2021 | 23 | 0 | 23 | 0 | 23 | 0 | 0 | 0 | 21 | 1 | 0 | 2 | 0 | 2 | 3 | 87% (95% CI, 94.7–72.3) |
| Unter Ecker | 2021 | 216 | / | / | / | 216 | 0 | 0 | 0 | 0 | 24 | 0 | 17 | 0 | 0 | 0 | 96% |
| Totals and proportions | 2572 | 1129 (52.4%) | 912 (42.3%) | 115 (5.3%) | 1442 (77.1%) | 119 (6.4%) | 153 (8.2%) | 156 (8.3%) | 538 (21.4%) | 97 (3.8%) | 7 (0.3%) | 131 (5.1%) | 12 (0.5%) | 39 (1.5%) | 78 (3%) | 93.6% |
3.9. Acetabular Reinforcement
In most cases (57.5%), the C-DMCs were used without acetabular reinforcement, cementing the acetabular component directly on the bone resulting in a low loosening rate and good cup survivorship, between 93 and 100% at the last followup (Table 8).
Table 8.
Cemented DMC without acetabular reinforcement.
| Author | Year | C-DMC without Acetabular Reinforcement | Primary Setting | Revision Setting | Graft | Dislocations | IPD | Mechanical Failure | Aseptic Loosening | Infection | Revisions | Cup-Survivorship |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tarasevicius | 2010 | 42 | 42 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Mukka | 2013 | 34 | 9 | 25 | 0 | 2 | 0 | 0 | 0 | 3 | 3 | 94.1% |
| Carulli C | 2015 | 11 | 0 | 11 | / | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Haen | 2015 | 66 | 32 | 34 | 3 | 0 | 0 | 0 | 1 | 0 | 1 | 98% |
| Simian | 2015 | 24 | 0 | 24 | / | / | 0 | 0 | 0 | / | / | / |
| van Heumen | 2015 | 46 | 0 | 46 | 6 | 0 | 0 | 0 | 1 | 2 | 3 | 93% |
| Luthra | 2016 | 63 | 30 | 33 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 98% |
| Hamadouche | 2017 | 29 | 0 | 29 | / | / | / | 0 | / | / | / | / |
| Mohaddes | 2017 | 436 | 0 | 436 | 0 | 7 | 0 | 2 | 2 | 15 | 10 | 96% |
| Nabil | 2017 | 11 | 11 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Kavcic | 2018 | 174 | 173 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 100% |
| Ozden | 2018 | 6 | 0 | 6 | / | 0 | 0 | 0 | / | 0 | / | / |
| Rashed | 2018 | 32 | 32 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 93.75% |
| Spaans | 2018 | 102 | 0 | 102 | 102 | 3 | 0 | 0 | 4 | 1 | 5 | 95.8% |
| Stucinskas | 2018 | 236 | 0 | 236 | 0 | 5 | 0 | 0 | 1 | 5 | 11 | 94.9% |
| Tabori-Jensen | 2018 | 56 | 56 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | / | / |
| de l’Escalopier | 2019 | 23 | 0 | 23 | / | / | / | 0 | / | / | / | / |
| Dikmen | 2019 | 11 | 0 | 11 | / | / | 0 | 0 | / | / | / | / |
| Fathy | 2019 | 20 | 0 | 20 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 100% |
| Gabor | 2019 | 27 | 0 | 27 | / | / | 0 | 0 | 0 | / | / | / |
| Wheelton | 2019 | 54 | 0 | 54 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 100% |
| Mahmoud | 2020 | 20 | 15 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Rashed | 2020 | 31 | 31 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 96.8% |
| Tabori-Jensen | 2020 | 29 | 29 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Elkhadrawe | 2021 | 32 | 32 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 100% |
| Lamo Espinosa | 2021 | 68 | 68 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 98.5% |
| Uriarte | 2021 | 44 | 44 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 93.3% |
| Totals and proportions | 1727 | 604 (35%) | 1123 (65%) | 116 (7.3%) | 19 (1.2%) | 0 | 2 (0.1%) | 11 (0.7%) | 35 (2.2%) | 39 (2.5%) | Mean: 96.9% |
In 39.6% of the total cases, in 30 studies, a DMC was cemented into an acetabular reinforcement.
The most common AR used were the Kerboull cross-plates and Burch–Schneider Cage (Table 9).
Table 9.
Cemented DMC with acetabular reinforcement.
| Author | Year | C-DMC with Acetabular Reinforcement |
Acetabular Reinforcement |
Primary Setting | Revision Setting | Graft | Dislocations | Intra-Prosthetic Dislocations | Mechanical Failure | Aseptic Loosening | Infection | Revisions | Cup-Survivorship |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Langlais | 2008 | 81 | Kerboull Cross-Plate | 0 | 81 | 0 | 0 | 1 | 0 | 0 | 2 | 3 | 94.6% |
| Philippot | 2009 | 51 | 7 Novae Arm cage/Kerboull cross (44) | 0 | 51 | / | 6 | 0 | 1 | 2 | 3 | / | 98.80% |
| Schneider | 2011 | 96 | 70 Kerboull cross-plate, 6 Burch-Schneider antiprotrusio cage, 20 custom-fit Novae ARM cage | 0 | 96 | 91 | 11 | 0 | 2 | 1 | 5 | 4 | 95.6% |
| Civinini | 2012 | 24 | Contour acetabular ring (Smith & Nephew, London, UK) | 0 | 24 | 30 | 0 | 0 | 0 | 0 | 1 | 1 | 97% |
| Pattyn | 2012 | 37 | 35 Ganz ring (Zimmer Inc., Warsaw, IN, USA), 2 Burch Schneider ring (Zimmer Inc., Warsaw, IN, USA) | 0 | 37 | 0 | 2 | 0 | 1 | 0 | 1 | 2 | / |
| Toro-Ibarguen | 2014 | 14 | 15 Protrusio cage [DePuy Orthopaedics, Inc, Warsaw, IN], 22 Contour [Smith and Nephew Richards, Memphis, TN, USA] | 0 | 14 | 0 | 1 | 0 | / | / | / | / | / |
| Wegrzyn | 2014 | 61 | Kerboull Cross-Plate | 0 | 61 | 61 | 0 | 0 | 1 | 0 | 0 | 0 | 98% |
| Simian | 2015 | 23 | Ganz Reinforcement Ring (Zimmer, Warsaw, IN, USA) | 0 | 23 | / | / | 0 | 0 | 0 | / | / | / |
| Plummer | 2016 | 11 | / | 0 | 11 | 0 | 1 | 0 | 2 | 0 | 2 | 4 | / |
| Hamadouche | 2017 | 22 | Kerboull acetabular reinforcement | 0 | 22 | / | / | / | 0 | / | / | / | / |
| Lebeau | 2017 | 62 | 47 Müller ring, 8 Burch-Schneider ring, 4 Link reinforcement | 0 | 62 | 58 | 1 | 0 | 0 | 5 | 7 | 8 | 91.9% |
| Bruggemann | 2018 | 69 | / | 0 | 69 | 16 | 1 | 0 | 0 | 2 | 0 | 2 | 96% |
| Hipfl | 2018 | 15 | titanium acetabular cage (Zimmer Biomet) | 0 | 15 | 15 | 2 | 0 | 0 | 0 | 2 | / | 89% |
| Ozden | 2018 | 9 | Contour Acetabular Reinforcement Ring (Smith & Nephew) | 0 | 9 | / | 0 | 0 | 0 | / | 0 | / | / |
| Wegrzyn | 2018 | 131 | Kerboull cross-plate or Burch-Schneider anti-protrusio cage | 131 | 0 | 0 | 3 | 0 | 0 | 0 | 4 | 0 | / |
| Assi | 2019 | 16 | Kerboull cross-plate | 0 | 16 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Dikmen | 2019 | 19 | Contour Acetabular Reconstruction Ring (Smith & Nephew) | 0 | 19 | / | / | 0 | 0 | / | / | / | / |
| Gabor | 2019 | 11 | / | 0 | 11 | / | / | 0 | 0 | 0 | / | / | / |
| Giunta | 2019 | 23 | Kerboull cross-plate | 23 | 0 | 6 | 3 | 0 | 0 | 0 | 0 | 0 | / |
| Plummer | 2019 | 19 | triflange titanium acetabular cage (Restoration GAP Acetabular Cup; Stryker) | 19 | 0 | 19 | 0 | 0 | 0 | 0 | 2 | 1 | / |
| Schmidt-Braekling | 2019 | 79 | Burch–Schneider Cage (Zimmer, Warsaw, IN, USA) | 0 | 79 | 0 | 2 | 0 | 0 | 4 | 5 | 9 | 85% |
| de l’Escalopier | 2020 | 53 | Kerboull acetabular reinforcement device (KARD, Zimmer-Biomet, Warsaw, IN, USA) | 0 | 53 | / | / | / | 0 | / | / | / | / |
| Lannes | 2020 | 26 | Ganz ring (Zimmer-Biomet®, Warsaw, IN, USA) | 26 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 2 | 92.3% |
| Lavignac | 2020 | 71 | Kerboull cross-plate, Muller ring, Burch-Schneider cage | 71 | 0 | 0 | 1 | 0 | 6 | 4 | 10 | / | / |
| Sayac | 2020 | 77 | Kerboull cross-plate, Burch-Schneider antiprotrusio cage, custom-fit Novae ARM cage | 0 | 77 | 0 | 7 | 0 | 0 | 3 | 2 | 6 | 92.2% |
| Schmidt | 2020 | 59 | Kerboull cross-plate, Burch-Schneider ring, or jumbo metal-back | 0 | 59 | 0 | 4 | 0 | / | / | / | 13 | 72.1% |
| Bozon | 2021 | 23 | Kerboull reinforcement device (316 L, Aston Medical, Saint-Étienne, France) | 0 | 23 | 21 | 1 | 0 | 0 | 2 | 3 | 2 | 87% |
| Totals and proportions | 1182 | 270 (22.8%) | 912 (77.2%) | 333 (33.5%) | 48 (4.5%) | 1 (0.09%) | 13 (1.2%) | 23 (2.3%) | 51 (5.2%) | 57 (6.4%) | Mean: 91.7% | ||
3.10. Cup-in-Cup Technique
DMC was cemented into a pre-existing cup following the “cup-in-cup” technique, in 106 cases (3.1%) (Table 3). In all cases, this procedure was used as a revision setting after the failure of a previous THA (Table 10).
Table 10.
Cemented DMC: cup-in-cup technique.
| Author | Year | Cemented DMC | Dislocations | IPD | Revisions | Mechanical Failure | Aseptic Loosening | Infections | Acetabular Components RLLs | Brooker HO | Preoperative HHS | Postperative HHS | Preoperative PMA | Postoperative PMA | Revisions | Posterior Approach | Lateral Approach | Anterior Approach | Follow-up (Months) (SD) [Range] | Cup-Survivorship |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stambough | 2017 | 8 | 2 | 0 | 2 | 0 | 0 | 1 | / | / | / | / | / | 8 | 8 | 0 | 0 | 34.8 [24–63.6] | 85% | |
| Chalmers | 2018 | 18 | 2 | 1 | 2 | 0 | 0 | 0 | 0 | / | 47 [37–60] | 81 [62-98] | / | / | 18 | 11 | 0 | 7 | 36 [24–60] | / |
| Evangelista | 2018 | 18 | 0 | 0 | 0 | 0 | 0 | 0 | / | / | 46 [40–79] | 65 [41–97] | / | / | 18 | 0 | 0 | 0 | 36 [25–56] | 100% |
| Wegrzyn | 2020 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 71 [69–74] | 88 [82–95] | / | / | 28 | 28 | 0 | 0 | 42 [24–60] | 100% |
| Bellova | 2021 | 33 | 2 | 0 | 2 | 1 | 0 | 1 | / | / | / | 59.4 (±22.2) [29–91] | / | / | 33 | 33 | 0 | 0 | 28.5 (±17.3) [3–64] | 86.8% |
| Moreta | 2021 | 10 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 49.3 [33–62] | 71.3 [22–91] | 10.1 | 12.8 | 10 | 4 | 0 | 6 | 42 [24–72] | / |
| Totals and proportions | 115 | 4.7% | 0.9% | 4.7% | 0.9% | 0% | 0.9% | 0% | 0% | Mean: 56.4 | Mean: 74.8 | Mean: 10.1 | Mean: 12.8 | 100% | 86.6% | 0% | 13.4% | Mean: 35.7 | Mean: 93.6% | |
3.11. Acetabular Bone Grafting
In the current study, the use of bone grafting was observed in 22 (39.3%) manuscripts. Overall, acetabular bone grafting has been used in 16.3% of C-DMC. In most cases, it was an allograft (93.2%), while in a minor part it was a synthetic graft (4.9%) or autograft (1.9%).
Acetabular bone grafting was used in 3% of the primary C-DMC setting and in 19% of the revision C-DMC setting. In cases where an acetabular reinforcement was utilized, acetabular bone grafting was used in 24.2% of cases, while only in 9.8% of cases in the absence of acetabular reinforcement (Table 2).
4. Discussion
This review allowed us to appreciate the satisfactory results of C-DMC. Dislocation rates found are low and the survivorship of the implants in both primary and revision surgery is satisfactory. Clinically, the improvement of the functional outcomes is significant, and radiologically, RLLs are rare.
The clinical and radiographic outcomes of cementless DMCs are excellent at medium and long follow-ups with an overall survivorship of 95% at 10-year follow-ups and demonstrated low revision and dislocation rates, without major polyethylene wear concerns [16,68,69,70,71,72,73,74,75,76,77,78,79,80].
4.1. Cemented Dual Mobility Cup in the Setting of Primary Surgery
In the present study, was observed the use of C-DMC in a primary setting in about a quarter of the surgeries (25.5%). C-DMC is an established treatment of hip OA, especially in association with other comorbidities that could increase the risk of dislocation and loosening, such as acetabular deficiency, abductor deficiency, prior acetabular fracture fixation or high-demanding physical activity patients [32].
Tabori-Jensen et al. [61] in a randomized controlled study in elderly osteoarthrosis patients with 2 years’ follow-up comparing cementless DMC with C-DMC have demonstrated that cemented fixation of the Avantage DMC seems safer in elderly patients, with less implant migration.
Moreover, C-DMC represents an option in the management of FNF. In those cases, Tarasevicius et al. [15] reported a 100% survival rate one year after treatment of 42 patients with C-DMC. Lamo-Espinosa et al. [67], in a series of 69 elderly (>75 years) and frail patients with a high risk of instability with a median follow-up time of 49.04 months, reported only one case of revision due to aseptic loosening.
Another well-recognized use of C-DMC is in cases of pathological fractures. Lavignac et al. [58] used DMC in the treatment of peri-acetabular metastasis, but although the rate of complications and revisions is low, the mean patient survivorship was 19.5 months due to the progression of the primary disease. Similarly, Wegrzyn et al. [46], in a continuous series of 131 cases of periacetabular metastatic disease treated using a DMC cemented into an acetabular reinforcement device, observed an improvement in the postoperative functional outcome and pain relief, no mechanical failure or aseptic loosening of the acetabular reconstruction and a dislocation rate of 2%.
Finally, in some cases of acetabular fractures, C-DMC could be used. In those cases, it is associated with the combined treatment of fracture reduction and fixation. As reported by Giunta et al. [38], primary C-DMC for acetabular fracture in the elderly population might be a good therapeutic option that allows a return to previous daily life activity. Lannes et al. [57] found that DMC combined with internal fixation, also known as the combined hip procedure (CHP), could be an efficient procedure in selected elderly patients, with a lower level of revision rate compared to the ORIF group alone. In the CHP group, internal fixation was performed before the hip replacement. When the anterior column was involved, a suprapectineal quadrilateral buttress plate was used through a modified Stoppa approach; otherwise, a Kocher-Langenbeck approach was performed with a posterior column or wall osteosynthesis [81,82].
These findings are important and demonstrate that primary surgery with C-DMC is an excellent treatment in complex cases of OA, FNF, acetabular fractures or periacetabular metastases in terms of survival and reduced number of complications.
4.2. Cemented Dual Mobility Cup in the Setting of Revision Surgery
As demonstrated by the results of the study, the most frequent use of C-DMC is in revision settings (74.5%).
In cases of failure of a previous THA, C-DMC has shown an excellent role in avoiding further failures and reducing the number of complications. In fact, from the Swedish Hip Arthroplasty Register, Hailer, et al. [18] revealed in a series of 228 patients that DMCs for revision due to instability are associated with a low rate (8%) of re-revisions due to dislocation.
In patients with first-time revision hip arthroplasty due to dislocation, Mohaddes et al. [31] found better short to mid-term implant survival for C-DMC compared with cemented polyethylene cups at four years of follow-up. Stucinskas et al. [44], from the Lithuanian arthroplasty register, observed a significantly lower short-term re-revision rate for dislocations at five-year follow-up, in patients treated with C-DMC (2%) compared to different surgical concepts (9%) when used for first-time hip revisions due to recurrent dislocations.
As emerges from the results of the current review, C-DMC is a valid option in a revision setting with a dislocation rate of 3% and a survival rate of approximately 95% (with a mean follow-up of 49.6 months).
4.3. Cemented Dual Mobility Cup into an Acetabular Reinforcement
In the present study, DMC was cemented in an acetabular reinforcement in the revision setting in 83.6%, while in the primary setting only in 16.4% of the cases.
Neri et al. [74] suggested the use of DMC cemented into a reinforcement cage (Kerboull cross-plate or custom reinforcement cage) in cases of acetabular defects 2C or more according to Paprosky’s classification. In a single-center continuous series of 62 patients, Lebeau et al. [30] evidenced that DMC cemented into an acetabular reinforcement at a minimum FU of five years presented good outcomes (PMA 14, HHS score 73) and only 2 cases of dislocation, while Brüggemann et al. [35], in a case series of 69 patients, demonstrated a 4-year survival of 96% and only one case of dislocation.
4.4. Cemented Dual Mobility Cup into a Pre-Existing Cup
Among the studies, a minor part (3.2%) of the DMCs was cemented into a pre-existing cup following the surgical technique described by Blumenfeld [83], known as the “Cup-in-cup” technique. This technique, developed for the treatment of acetabular defects, in the current study showed good results in terms of fewer complications and guaranteed a survival rate of 93.6% at a mean follow-up of 35.7 months (Table 10).
4.5. Bone Grafting
In the current study, the use of bone grafting was observed in 16.3% of C-DMC. In most cases, bone grafting was used in a revision setting, in combination with acetabular reinforcement, using an allograft. Bone grafting could help the surgeon in cases of loss of acetabular bone stock and unstable components fixation and can be easily combined with cemented fixation of the DMC [84].
4.6. C-DMC Complications and Outcomes
In the current review, the overall dislocation rate was 2.9%, and at 45.9 months follow-up, the overall survival rate was 93.5%. These data are similar to the mean rates of dislocation and medium-term survival of single-mobility THA or cementless DMC [25,85,86]. These results must be considered even more due to the use of the C-DMC especially in complex cases or in revision settings.
The overall IPD rate was 0.2%. First described in 2004 by Lecuire [87], intra-prosthetic dislocation (IPD) is a specific complication of DMC. IPD is defined as excessive “wear” of the head-liner interface which induces the separation of the head from the polyethylene, but the present systematic review reported only 7 cases of IPD, showing that this complication is now extremely rare.
Overall, C-DMC demonstrates to be a valid treatment in primary complex cases, such as in revision settings, in terms of survival and reduced number of complications.
The greatest strength of the article is to represent the only systematic review specifically focused on the C-DMC present in the literature. Moreover, over three thousand C-DMCs are considered in the systematic review. Limitations of the study are represented by the low average level of evidence, most of the studies have a level IV of evidence. Furthermore, the nature of the inclusion criteria may have minimally altered the results, due to the wide heterogeneity of the patients included. However, it is assumed that in such a large case series, this possible bias could be minimized.
5. Conclusions
The use of C-DMCs is an option used mainly in THA revision surgery, although it also exists in a primary setting. It represents an effective treatment option with good clinical outcomes. The complication rate remains moderate, with a low rate of dislocation in both primary and revision surgery. The loosening and revision rates are also low. These results can be observed whether the implant is cemented directly into the bone or cemented in acetabular reinforcement or a previous well-fixed cup. An acetabular reinforcement was used in almost 40% of cases.”
Author Contributions
G.C. and G.M. wrote the manuscript. G.C., G.M., E.D. and S.G. collected the data. C.B. provided data analysis. E.S. and S.L. are the senior authors who designed the study and reviewed the manuscript. The authors approved the submitted version. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.
Conflicts of Interest
G.C., G.M., E.D., S.G. and C.B.: No conflict of interest. E.S.: institutional research support from Corin. S.L.: Consultant for Stryker, Smith and Nephew, Heraeus, Depuy Synthes. Institutional research support to Lepine and Amplitude. Editorial Board for Journal of Bone and Joint Surgery (Am).
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Batailler: C., Fary C., Verdier R., Aslanian T., Caton J., Lustig S. The evolution of outcomes and indications for the dual-mobility cup: A systematic review. Int. Orthop. 2017;41:645–659. doi: 10.1007/s00264-016-3377-y. [DOI] [PubMed] [Google Scholar]
- 2.Blakeney W.G., Epinette J.A., Vendittoli P.A. Dual mobility total hip arthroplasty: Should everyone get one? EFORT Open Rev. 2019;4:541–547. doi: 10.1302/2058-5241.4.180045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heckmann N., Weitzman D.S., Jaffri H., Berry D.J., Springer B.D., Lieberman J.R. Trends in the use of dual mobility bearings in hip arthroplasty: An analysis of the American Joint Replacement Registry. Bone Jt. J. 2020;102((Suppl. SB)):27–32. doi: 10.1302/0301-620X.102B7.BJJ-2019-1669.R1. [DOI] [PubMed] [Google Scholar]
- 4.Darrith B., Courtney P.M., Della Valle C.J. Outcomes of dual mobility components in total hip arthroplasty: A systematic review of the literature. Bone Jt. J. 2018;100:11–19. doi: 10.1302/0301-620X.100B1.BJJ-2017-0462.R1. [DOI] [PubMed] [Google Scholar]
- 5.De Martino I., Triantafyllopoulos G.K., Sculco P.K., Sculco T.P. Dual mobility cups in total hip arthroplasty. World J. Orthop. 2014;5:180–187. doi: 10.5312/wjo.v5.i3.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cha Y.H., Yoo J.I., Kim J.T., Park C.H., Ahn Y.S., Choy W.S., Ha Y.C., Koo K.H. Dual mobility total hip arthroplasty in the treatment of femoral neck fractures. Bone Jt. J. 2020;102:1457–1466. doi: 10.1302/0301-620X.102B11.BJJ-2020-0610.R2. [DOI] [PubMed] [Google Scholar]
- 7.Hernigou P., Auregan J.C., Potage D., Roubineau F., Flouzat Lachaniette C.H., Dubory A. Dual-mobility implants prevent hip dislocation following hip revision in obese patients. Int. Orthop. 2017;41:469–473. doi: 10.1007/s00264-016-3316-y. [DOI] [PubMed] [Google Scholar]
- 8.Burgers P.T., Van Geene A.R., Van den Bekerom M.P., Van Lieshout E.M., Blom B., Aleem I.S., Bhandari M., Poolman R.W. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: A meta-analysis and systematic review of randomized trials. Int. Orthop. 2012;36:1549–1560. doi: 10.1007/s00264-012-1569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanders R.J.M., Swierstra B.A., Goosen J.H.M. The use of a dual-mobility concept in total hip arthroplasty patients with spastic disorders: No dislocations in a series of ten cases at midterm follow-up. Arch. Orthop. Trauma Surg. 2013;133:1011–1016. doi: 10.1007/s00402-013-1759-9. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez A.I., Bartolone P., Lubbeke A., Lozeron E.D., Peter R., Hoffmeyer P., Christofilopoulos P. Comparison of dual-mobility cup and unipolar cup for prevention of dislocation after revision total hip arthroplasty. Acta Orthop. 2017;88:18–23. doi: 10.1080/17453674.2016.1255482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boulat S., Neri T., Boyer B., Philippot R., Farizon F. Dual mobility cups in total hip arthroplasty after failed internal fixation of proximal femoral fractures. Orthop. Traumatol. Surg. Res. 2019;105:491–495. doi: 10.1016/j.otsr.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 12.Langlais F.L., Ropars M., Gaucher F., Musset T., Chaix O. Dual Mobility Cemented Cups Have Low Dislocation Rates in THA Revisions. Clin. Orthop. Relat. Res. 2008;466:389–395. doi: 10.1007/s11999-007-0047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamadouche M., Biau D.J., Huten D., Musset T., Gaucher F. The Use of a Cemented Dual Mobility Socket to Treat Recurrent Dislocation. Clin. Orthop. Relat. Res. 2010;468:3248–3254. doi: 10.1007/s11999-010-1404-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Philippot R., Adam P., Reckhaus M., Delangle F., Verdot F., Curvale G., Farizon F. Prevention of dislocation in total hip revision surgery using a dual mobility design. Orthop. Traumatol. Surg. Res. 2009;95:407–413. doi: 10.1016/j.otsr.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 15.Tarasevicius S., Busevicius M., Robertsson O., Wingstrand H. Dual mobility cup reduces dislocation rate after arthroplasty for femoral neck fracture. BMC Musculoskelet. Disord. 2010;11:175. doi: 10.1186/1471-2474-11-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schneider L., Philippot R., Boyer B., Farizon F. Revision total hip arthroplasty using a reconstruction cage device and a cemented dual mobility cup. Orthop. Traumatol. Surg. Res. 2011;97:807–813. doi: 10.1016/j.otsr.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Civinini R., Carulli C., Matassi F., Nistri L., Innocenti M. A Dual-mobility Cup Reduces Risk of Dislocation in Isolated Acetabular Revisions. Clin. Orthop. Relat. Res. 2012;470:3542–3548. doi: 10.1007/s11999-012-2428-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hailer N.P., Weiss R.J., Stark A., Kärrholm J. Dual-mobility cups for revision due to instability are associated with a low rate of re-revisions due to dislocation: 228 patients from the Swedish Hip Arthroplasty Register. Acta Orthop. 2012;83:566–571. doi: 10.3109/17453674.2012.742395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pattyn C., Audenaert E. Early complications after revision total hip arthroplasty with cemented dual-mobility socket and reinforcement ring. Acta Orthop. Belg. 2012;78:357–361. [PubMed] [Google Scholar]
- 20.Mukka S.S., Mahmood S.S., Sjödén G.O., Sayed-Noor A.S. Dual mobility cups for preventing early hip arthroplasty dislocation in patients at risk: Experience in a county hospital. Orthop. Rev. 2013;5:10. doi: 10.4081/or.2013.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Toro-Ibarguen A., Auñón-Martín I., Delgado-Díaz E., Moreno-Beamud J.A., Martínez-Leocadio M.A., Díaz-Martín A., Candel-García L. Analysis of the Results of Use of Bone Graft and Reconstruction Cages in a Group of Patients with Severe Acetabular Bone Defects. Adv. Orthop. Surg. 2014;2014:376963. doi: 10.1155/2014/376963. [DOI] [Google Scholar]
- 22.Wegrzyn J., Pibarot V., Jacquel A., Carret J.P., Béjui-Hugues J., Guyen O. Acetabular Reconstruction Using a Kerboull Cross-Plate, Structural Allograft and Cemented Dual-Mobility Cup in Revision THA at a Minimum 5-Year Follow-Up. J. Arthroplast. 2014;29:432–437. doi: 10.1016/j.arth.2013.05.030. [DOI] [PubMed] [Google Scholar]
- 23.Carulli C., Macera A., Matassi F., Civinini R., Innocenti M. The use of a dual mobility cup in the management of recurrent dislocations of hip hemiarthroplasty. J. Orthop. Traumatol. 2016;17:131–136. doi: 10.1007/s10195-015-0365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haen T.X., Lonjon G., Vandenbussche E. Can cemented dual-mobility cups be used without a reinforcement device in cases of mild acetabular bone stock alteration in total hip arthroplasty? Orthop. Traumatol. Surg. Res. 2015;101:923–927. doi: 10.1016/j.otsr.2015.09.027. [DOI] [PubMed] [Google Scholar]
- 25.Simian E., Chatellard R., Druon J., Berhouet J., Rosset P. Dual mobility cup in revision total hip arthroplasty: Dislocation rate and survival after 5 years. Orthop. Traumatol. Surg. Res. 2015;101:577–581. doi: 10.1016/j.otsr.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 26.Van Heumen M., Heesterbeek P.J.C., Swierstra B.A., Van Hellemondt G.G., Goosen J.H.M. Dual mobility acetabular component in revision total hip arthroplasty for persistent dislocation: No dislocations in 50 hips after 1–5 years. J. Orthopaed. Traumatol. 2015;16:15–20. doi: 10.1007/s10195-014-0318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamadouche M., Ropars M., Rodaix C., Musset T., Gaucher F., Biau D., Courpied J.P., Huten D. Five to thirteen year results of a cemented dual mobility socket to treat recurrent dislocation. Int. Orthop. 2017;41:513–519. doi: 10.1007/s00264-016-3343-8. [DOI] [PubMed] [Google Scholar]
- 28.Luthra J.S., Al Riyami A., Allami M.K. Dual mobility total hip replacement in a high risk population. SICOT-J. 2016;2:43. doi: 10.1051/sicotj/2016037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Plummer D.R., Christy J.M., Sporer S.M., Paprosky W.G., Della Valle C.J. Dual-Mobility Articulations for Patients at High Risk for Dislocation. J. Arthroplast. 2016;31:131–135. doi: 10.1016/j.arth.2016.03.021. [DOI] [PubMed] [Google Scholar]
- 30.Lebeau N., Bayle M., Belhaouane R., Chelli M., Havet E., Brunschweiler B., Mertl P. Total hip arthroplasty revision by dual-mobility acetabular cup cemented in a metal reinforcement: A 62 case series at a minimum 5 years’ follow-up. Orthop. Traumatol. Surg. Res. 2017;103:679–684. doi: 10.1016/j.otsr.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 31.Mohaddes M., Cnudde P., Rolfson O., Wall A., Kärrholm J. Use of dual-mobility cup in revision hip arthroplasty reduces the risk for further dislocation: Analysis of seven hundred and ninety one first-time revisions performed due to dislocation, reported to the Swedish Hip Arthroplasty Register. Int. Orthop. 2017;41:583–588. doi: 10.1007/s00264-016-3381-2. [DOI] [PubMed] [Google Scholar]
- 32.Nabil M. Dual Mobility Cups in Primary Total Hip Arthroplasty for Patients at Risk of Dislocation. MOJ Orthop. Rheumatol. 2017;7:00277. doi: 10.15406/mojor.2017.07.00277. [DOI] [Google Scholar]
- 33.Stambough J.B., Nam D., Haynes J.A., Sassoon A.A., Bohnenkamp F.C., Barrack R.L., Nunley R.M. Revision Total Hip Arthroplasty in the Setting of a Well-Fixed Cup: Early Report on the Cup-in-Cup Technique. J. Hip Surg. 2017;1:158–166. doi: 10.1055/s-0037-1608893. [DOI] [Google Scholar]
- 34.Assi C., Caton J., Fawaz W., Samaha C., Yammine K. Revision total hip arthroplasty with a Kerboull plate: Comparative outcomes using standard versus dual mobility cups. Int. Orthop. 2019;43:2245–2251. doi: 10.1007/s00264-018-4209-z. [DOI] [PubMed] [Google Scholar]
- 35.Brüggemann A., Mallmin H., Hailer N.P. Do dual-mobility cups cemented into porous tantalum shells reduce the risk of dislocation after revision surgery?: A retrospective cohort study on 184 patients. Acta Orthop. 2018;89:156–162. doi: 10.1080/17453674.2018.1432927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chalmers B.P., Ledford C.K., Taunton M.J., Sierra R.J., Lewallen D.G., Trousdale R.T. Cementation of a Dual Mobility Construct in Recurrently Dislocating and High Risk Patients Undergoing Revision Total Arthroplasty. J. Arthroplast. 2018;33:1501–1506. doi: 10.1016/j.arth.2017.11.055. [DOI] [PubMed] [Google Scholar]
- 37.Evangelista P., Okroj K., Plummer D., Della Valle C., Schwarzkopf R. Do Cemented Dual-Mobility Cups Confer Stability for Patients at High Risk of Dislocation in Revision Total Hip Arthroplasty? J. Hip Surg. 2018;2:088–091. doi: 10.1055/s-0038-1661341. [DOI] [Google Scholar]
- 38.Giunta J.C., Tronc C., Kerschbaumer G., Milaire M., Ruatti S., Tonetti J., Boudissa M. Outcomes of acetabular fractures in the elderly: A five year retrospective study of twenty seven patients with primary total hip replacement. Int. Orthop. 2019;43:2383–2389. doi: 10.1007/s00264-018-4204-4. [DOI] [PubMed] [Google Scholar]
- 39.Hipfl C., Janz V., Löchel J., Perka C., Wassilew G.I. Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: Mid-term Results of a Consecutive Series of 35 Cases. Bone Jt. J. 2018;100:1442–1448. doi: 10.1302/0301-620X.100B11.BJJ-2018-0481.R1. [DOI] [PubMed] [Google Scholar]
- 40.Kavčič G., Mirt P., Bedenčič K. Good mid-term clinical results of a cemented dual mobility cup: A single-centre experience. Hip Int. 2018;28:59–62. doi: 10.5301/hipint.5000529. [DOI] [PubMed] [Google Scholar]
- 41.Ozden V.E., Dikmen G., Beksac B., Tozun R. Dual-mobility bearings for patients with abductor-trochanteric complex insufficiency: Dual-mobility for abductor-trochanteric complex ınsufficiency. Hip Int. 2018;28:491–497. doi: 10.1177/1120700018757788. [DOI] [PubMed] [Google Scholar]
- 42.Rashed R.A., Sevenoaks H., Shabaan A.M., Choudry Q.A., Hammad A.S., Kasem M.S., El Khadrawe T.A., El Dakhakhny M.M. Functional outcome and health related quality of life after dual mobility cup total hip replacement for displaced femoral neck fractures in middle aged Egyptian patients. Injury. 2018;49:667–672. doi: 10.1016/j.injury.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 43.Spaans E.A., Koenraadt K.L.M., Wagenmakers R., van den Hout J.A.A.M., te Stroet M.A.J., Bolder S.B.T. Midterm survival analysis of a cemented dual-mobility cup combined with bone impaction grafting in 102 revision hip arthroplasties. Hip Int. 2018;28:161–167. doi: 10.5301/hipint.5000548. [DOI] [PubMed] [Google Scholar]
- 44.Stucinskas J., Kalvaitis T., Smailys A., Robertsson O., Tarasevicius S. Comparison of dual mobility cup and other surgical construts used for three hundred and sixty two first time hip revisions due to recurrent dislocations: Five year results from Lithuanian arthroplasty register. Int. Orthop. 2018;42:1015–1020. doi: 10.1007/s00264-017-3702-0. [DOI] [PubMed] [Google Scholar]
- 45.Tabori-Jensen S., Frølich C., Hansen T.B., Bøvling S., Homilius M., Stilling M. Higher UHMWPE wear-rate in cementless compared with cemented cups with the Saturne® Dual-Mobility acetabular system. Hip Int. 2018;28:125–132. doi: 10.1177/1120700018768615. [DOI] [PubMed] [Google Scholar]
- 46.Wegrzyn J., Malatray M., Al-Qahtani T., Pibarot V., Confavreux C., Freyer G. Total Hip Arthroplasty for Periacetabular Metastatic Disease. An Original Technique of Reconstruction According to the Harrington Classification. J. Arthroplast. 2018;33:2546–2555. doi: 10.1016/j.arth.2018.02.096. [DOI] [PubMed] [Google Scholar]
- 47.De l’Escalopier N., Dumaine V., Auberger G., Babinet A., Courpied J.P., Anract P., Hamadouche M. Dual mobility constructs in revision total hip arthroplasty: Survivorship analysis in recurrent dislocation versus other indications at three to twelve-year follow-up. Int. Orthop. 2020;44:253–260. doi: 10.1007/s00264-019-04445-4. [DOI] [PubMed] [Google Scholar]
- 48.Dikmen G., Ozden V.E., Karaytug K., Tozun R. Dual-mobility cups in revision acetabular reconstructions: Short-term outcomes in high-risk patients for instability. Acta Orthop. Traumatol. Turc. 2019;53:329–333. doi: 10.1016/j.aott.2019.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fathy A., Ashoub M. The use of cemented dual mobility acetabular cup in revision hip arthroplasty. Egypt Orthop. J. 2019;54:168. doi: 10.4103/eoj.eoj_45_19. [DOI] [Google Scholar]
- 50.Gabor J.A., Feng J.E., Gupta S., Calkins T.E., Della Valle C.J., Vigdorchik J., Schwarzkopf R. Cementation of a monoblock dual mobility bearing in a newly implanted porous revision acetabular component in patients undergoing revision total hip arthroplasty. Arthroplast. Today. 2019;5:341–347. doi: 10.1016/j.artd.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moreta J., Uriarte I., Foruria X., Urra I., Aguirre U., Martínez-de Los Mozos J.L. Cementation of a dual-mobility cup into a well-fixed cementless shell in patients with high risk of dislocation undergoing revision total hip arthroplasty. Hip Int. 2021;31:97–102. doi: 10.1177/1120700019873617. [DOI] [PubMed] [Google Scholar]
- 52.Plummer D., Passen E., Alexander J., Vajapey S., Frantz T., Niedermeier S., Pettit R., Scharschmidt T. Rapid return to function and stability with dual mobility components cemented into an acetabular reconstructive cage for large osseous defects in the setting of periacetabular metastatic disease. J. Surg. Oncol. 2019;119:1155–1160. doi: 10.1002/jso.25463. [DOI] [PubMed] [Google Scholar]
- 53.Sayac G., Neri T., Schneider L., Philippot R., Farizon F., Boyer B. Low Revision Rates at More Than 10 Years for Dual-Mobility Cups Cemented Into Cages in Complex Revision Total Hip Arthroplasty. J. Arthroplast. 2020;35:513–519. doi: 10.1016/j.arth.2019.08.058. [DOI] [PubMed] [Google Scholar]
- 54.Schmidt A., Batailler C., Fary C., Servien E., Lustig S. Dual Mobility Cups in Revision Total Hip Arthroplasty: Efficient Strategy to Decrease Dislocation Risk. J. Arthroplast. 2020;35:500–507. doi: 10.1016/j.arth.2019.08.060. [DOI] [PubMed] [Google Scholar]
- 55.Schmidt-Braekling T., Sieber D., Gosheger G., Theil J.C., Moellenbeck B., Andreou D., Dieckmann R. Dislocation rates with combinations of anti-protrusio cages and dual mobility cups in revision cases: Are we safe? PLoS ONE. 2019;14:e0212072. doi: 10.1371/journal.pone.0212072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Neil Wheelton A., Myatt D., Helm A.T. Outcomes for cemented dual mobility cup to treat recurrent instability; A UK case series. J. Orthop. 2019;16:220–223. doi: 10.1016/j.jor.2019.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lannes X., Moerenhout K., Duong H.P., Borens O., Steinmetz S. Outcomes of combined hip procedure with dual mobility cup versus osteosynthesis for acetabular fractures in elderly patients: A retrospective observational cohort study of fifty one patients. Int. Orthop. 2020;44:2131–2138. doi: 10.1007/s00264-020-04757-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lavignac P., Prieur J., Fabre T., Descamps J., Niglis L., Carlier C., Bouthors C., Baron-Trocellier T., Sailhan F., Bonnevialle P., et al. Surgical treatment of peri-acetabular metastatic disease: Retrospective, multicentre study of 91 THA cases. Orthop. Traumatol. Surg. Res. 2020;106:1025–1032. doi: 10.1016/j.otsr.2020.03.032. [DOI] [PubMed] [Google Scholar]
- 59.Mahmoud A., Farag O., Mahmoud M., Ashoub M., Sallam A., Mohamed M. Cemented Dual Mobility Cups in Primary Total HIP Arthroplasty in Patients at High Risk of Dislocation. Ain Shams Med. J. 2020;71:801–815. doi: 10.21608/asmj.2020.141293. [DOI] [Google Scholar]
- 60.Rashed R.A.M., Sevenoaks H., Choudry Q.A., Kasem M.S., Elkhadrawe T.A., Eldakhakhny M.M. Comparison of functional outcome of cemented total hip replacement versus cemented dual-mobility cup total hip replacement for the management of displaced femoral neck fractures in the active elderly patients. HIP Int. 2021;31:683–690. doi: 10.1177/1120700020910414. [DOI] [PubMed] [Google Scholar]
- 61.Tabori-Jensen S., Mosegaard S.B., Hansen T.B., Stilling M. Inferior stabilization of cementless compared with cemented dual-mobility cups in elderly osteoarthrosis patients: A randomized controlled radiostereometry study on 60 patients with 2 years’ follow-up. Acta Orthop. 2020;91:246–253. doi: 10.1080/17453674.2020.1720978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wegrzyn J., Saugy C.A., Guyen O., Antoniadis A. Cementation of a Dual Mobility Cup Into an Existing Well-Fixed Metal Shell: A Reliable Option to Manage Wear-Related Recurrent Dislocation in Patients with High Surgical Risk. J. Arthroplast. 2020;35:2561–2566. doi: 10.1016/j.arth.2020.05.001. [DOI] [PubMed] [Google Scholar]
- 63.Bellova P., Koch F., Stiehler M., Hartmann A., Fritzsche H., Günther K.P., Goronzy J. Cementation of a dual mobility cup in a well-fixed acetabular component- a reliable option in revision total hip arthroplasty? BMC Musculoskelet. Disord. 2021;22:982. doi: 10.1186/s12891-021-04835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bozon O., Dagneaux L., Sanchez T., Gaillard F., Hamoui M., Canovas F. Influence of dual-mobility acetabular implants on revision cup and Kerboull-type reinforcement ring constructs survivorship in aseptic acetabular loosening. Orthop. Traumatol. Surg. Res. 2021;108:103071. doi: 10.1016/j.otsr.2021.103071. [DOI] [PubMed] [Google Scholar]
- 65.Unter Ecker N., Kocaoğlu H., Zahar A., Haasper C., Gehrke T., Citak M. What Is the Dislocation and Revision Rate of Dual-mobility Cups Used in Complex Revision THAs? Clin. Orthop. Relat. Res. 2021;479:280–285. doi: 10.1097/CORR.0000000000001467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Elkhadrawe T.A. Dual mobility cup as a treatment of displaced femoral neck fractures in elderly: Stability and function. Egypt. Orthop. J. 2021;56:95–99. [Google Scholar]
- 67.Lamo-Espinosa J.M., Gómez-Álvarez J., Gatica J., Suárez Á., Moreno V., Díaz de Rada P., Valentí-Azcárate A., Alfonso-Olmos M., San-Julián M., Valentí-Nin J.R. Cemented Dual Mobility Cup for Primary Total Hip Arthroplasty in Elder Patients with High-Risk Instability. Geriatrics. 2021;6:23. doi: 10.3390/geriatrics6010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Uriarte I., Moreta J., Jimenez I., Legarreta M.J., Martínez de los Mozos J.L. Dual-mobility cups in total hip arthroplasty after femoral neck fractures: A retrospective study comparing outcomes between cemented and cementless fixation. Injury. 2021;52:1467–1472. doi: 10.1016/j.injury.2020.12.032. [DOI] [PubMed] [Google Scholar]
- 69.Ullmark G. The unstable total hip arthroplasty. EFORT Open Rev. 2016;1:83–88. doi: 10.1302/2058-5241.1.000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guyen O. Constrained liners, dual mobility or large diameter heads to avoid dislocation in THA. EFORT Open Rev. 2016;1:197–204. doi: 10.1302/2058-5241.1.000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bousquet G., Gazielly D.F., Girardin P., Debiesse J.L., Relave M., Israeli A. The ceramic coated cementless total hip arthroplasty. Basic concepts and surgical technique. J. Orthop. Surg. Tech. 1985;1:15–28. [Google Scholar]
- 72.Grazioli A., Ek E.T., Rüdiger H.A. Biomechanical concept and clinical outcome of dual mobility cups. Int. Orthop. 2012;36:2411–2418. doi: 10.1007/s00264-012-1678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lachiewicz P.F., Watters T.S. The Use of Dual-mobility Components in Total Hip Arthroplasty. J. Am. Acad. Orthop. Surg. 2012;20:481–486. doi: 10.5435/JAAOS-20-08-481. [DOI] [PubMed] [Google Scholar]
- 74.Neri T., Boyer B., Batailler C., Klasan A., Lustig S., Philippot R., Farizon F. Dual mobility cups for total hip arthroplasty: Tips and tricks. SICOT-J. 2020;6:17. doi: 10.1051/sicotj/2020018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Patil N., Deshmane P., Deshmukh A., Mow C. Dual Mobility in Total Hip Arthroplasty: Biomechanics, Indications and Complications–Current Concepts. Indian J. Orthop. 2021;55:1202–1207. doi: 10.1007/s43465-021-00471-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Canetti R., Malatray M., Pibarot V., Wegrzyn J. Dual mobility cups associated with proximal femoral replacement in nontumoral indications: Results and complications. Orthop. Traumatol. Surg. Res. 2022;108:103029. doi: 10.1016/j.otsr.2021.103029. [DOI] [PubMed] [Google Scholar]
- 77.Bensen A.S., Jakobsen T., Krarup N. Dual mobility cup reduces dislocation and re-operation when used to treat displaced femoral neck fractures. Int. Orthop. 2014;38:1241–1245. doi: 10.1007/s00264-013-2276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chouteau J., Rollier J.C., Bonnin M.P., Saffarini M., Nover L., Chatelet J.C., Jacquot L. Absence of instabilities and intra-prosthetic dislocations at 7 to 11 years following THA using a fourth-generation cementless dual mobility acetabular cup. J. Exp. Orthop. 2020;7:51. doi: 10.1186/s40634-020-00265-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Acker A., Fischer J.F., Aminian K., Lécureux E., Jolles B.M. Total hip arthroplasty using a cementless dual-mobility cup provides increased stability and favorable gait parameters at five years follow-up. Orthop. Traumatol. Surg. Res. 2017;103:21–25. doi: 10.1016/j.otsr.2016.09.020. [DOI] [PubMed] [Google Scholar]
- 80.Chughtai M., Mistry J.B., Diedrich A.M., Jauregui J.J., Elmallah R.K., Bonutti P.M., Harwin S.F., Malkani A.L., Kolisek F.R., Mont M.A. Low Frequency of Early Complications With Dual-mobility Acetabular Cups in Cementless Primary THA. Clin. Orthop. Relat. Res. 2016;474:2181–2187. doi: 10.1007/s11999-016-4811-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ciolli G., De Mauro D., Rovere G., Smakaj A., Marino S., Are L., El Ezzo O., Liuzza F. Anterior intrapelvic approach and suprapectineal quadrilateral surface plate for acetabular fractures with anterior involvement: A retrospective study of 34 patients. BMC Musculoskelet. Disord. 2021;22((Suppl. S2)):1060. doi: 10.1186/s12891-021-04908-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Herscovici D., Lindvall E., Bolhofner B., Scaduto J.M. The Combined Hip Procedure: Open Reduction Internal Fixation Combined With Total Hip Arthroplasty for the Management of Acetabular Fractures in the Elderly. J. Orthop. Trauma. 2010;24:291–296. doi: 10.1097/BOT.0b013e3181b1d22a. [DOI] [PubMed] [Google Scholar]
- 83.Blumenfeld T.J., Bargar W.L. Surgical Technique: A Cup-in-Cup Technique to Restore Offset in Severe Protrusio Acetabular Defects. Clin. Orthop. Relat. Res. 2012;470:435–441. doi: 10.1007/s11999-011-2075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Garcia-Rey E., Madero E., Garcia-Cimbrelo E. THA Revisions using impaction allografting with Mesh is durable for medial but not lateral acetabular defects. Clin. Orthop. Relat. Res. 2015;473:3882–3891. doi: 10.1007/s11999-015-4483-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gundtoft P.H., Varnum C., Pedersen A.B., Overgaard S. The Danish Hip Arthroplasty Register. Clin. Epidemiol. 2016;8:509–514. doi: 10.2147/CLEP.S99498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mufarrih S.H., Qureshi N.Q., Masri B., Noordin S. Outcomes of total hip arthroplasty using dual-mobility cups for femoral neck fractures: A systematic review and meta-analysis. Hip Int. 2021;31:12–23. doi: 10.1177/1120700020926652. [DOI] [PubMed] [Google Scholar]
- 87.Lecuire F., Benareau I., Rubini J., Basso M. Luxation intra-prothétique dans la cupule à double mobilité de Bousquet. A propos de 7 cas [Intra-prosthetic dislocation of the Bousquet dual mobility socket] Rev. Chir. Orthop. Reparatrice Appar. Mot. 2004;90:249–255. doi: 10.1016/S0035-1040(04)70101-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.