Abstract
Autosomal dominant polycystic kidney disease, autosomal recessive polycystic kidney disease, and nephronophthisis are hereditary disorders with the occurrence of numerous cysts in both kidneys, often causing chronic and end-stage renal failure. Animal models have played an important role in recent advances in research not only on disease onset and progressive mechanisms but also on the development of therapeutic interventions. For a long time, spontaneous animal models have been used as the primary focus for human diseases; however, after the identification of the nucleotide sequence of the responsible genes, PKD1, PKD2, PKHD1, and NPHPs, various types of genetically modified models were developed by genetic and reproductive engineering techniques and played the leading role in the research field. In this review, we present murine models of hereditary renal cystic diseases, discussing their potential benefits in the development of therapeutic strategies.
Keywords: cystic kidney, animal model, spontaneous, mutation, gene targeting
1. Introduction
Recently, research on hereditary renal cystic diseases such as polycystic kidney disease (PKD) and nephronophthisis (NPHP) has exponentially progressed, facilitating the ongoing identification of genetic variants that lead to the development of adult PKD with the use of laboratory animals [1]. This review focuses on the utility of laboratory rodent models in the development of treatment strategies for renal cystic diseases.
PKD, a typical hereditary disease of the kidney, is classified based on the responsible gene and mode of inheritance [2]. In adults, autosomal dominant PKD (ADPKD) is the most common inherited renal disorder [3]. In addition to the involvement of both the kidneys, cysts frequently develop in the liver as well as the pancreas, and systemic hypertension and cerebral aneurysms are common comorbid conditions [4]. Clinical manifestations commonly begin between the ages of 30 and 50 years, and by the age of 70 years, nearly 50% of patients develop end-stage renal disease [5]. Approximately 85% of patients who develop ADPKD are found to have mutations in PKD1, whereas the remaining 15% have mutations in PKD2 [6]. The pathological conditions caused by PKD1 mutations have been reported to progress faster than those caused by PKD2 [7]. With regard to PKD1 mutations, patients with truncated mutations have been reported to progress faster than those with nontruncated mutations [8]. This contrasts with autosomal recessive PKD (ARPKD), which is caused by PKHD1 mutations and characterized by enlarged renal collecting ducts and congenital hepatic fibrosis [9]. The onset of clinical symptoms of ARPKD typically occurs in the fetal or neonatal period or, at times, as late as early childhood [10]. Prenatal diagnosis with immediate transfer of the neonate to a neonatal intensive care unit improves the survival rate to at least 1 month and is associated with survival up to the age of 5 years in 85% of babies who survive past the first 30 days [11].
PKD1 and PKD2 encode Polycystin-1 (PC-1) and Polycystin-2 (PC-2/TRPP2), respectively. PC-1, which functions as a mechanosensor of intraluminal fluid flow, interacts with PC-2/TRPP2, which has calcium (Ca2+) channel activity in its C-terminus [12]. The PKHD1 gene product fibrocystin/polyductin (FPC) has a long extracellular domain and interacts with the N-terminus of PC-2 [13].
Approximately 5–25% of cases of premature renal failure are directly attributable to NPHP, a disease caused by Nphp mutations and characterized by the presence of numerous cysts in the renal medulla that is typically detected during childhood [14]. ADPKD, ARPKD, and NPHP are referred to as “ciliopathies” because of the presence of their gene products in primary cilia. The exacerbation of their associated pathological conditions results in increased cellular proliferation, inflammation, fibrosis, and accumulation of cystic fluid [15].
To elucidate the pathogenesis of PKD and test the efficacy of the candidate drugs, spontaneous and genetically modified laboratory animal models are the primary source of development information. The revelation of the nucleotide sequences of PKD1, PKD2, and PKHD1 has led to the development of various genetically modified animals, including transgenic animals with a foreign gene inserted, knockout (KO) animals with a specific gene disrupted, conditional KO (CKO) animals with cells forming a specific organ intentionally damaged or genetically disrupted at specific locations, knock-in animal models with hypomorphic genetic mutations, and genome-editing animal models that have been modified using new techniques such as the CRISPR/Cas9 method [16,17,18,19]. This study introduces the use of animal models in research on renal cystic disease and characterizes different animal model strains.
2. Spontaneous Model Animals
Spontaneous renal cysts in model animals were identified in the early 1980s before the discovery of the responsible genes. Cys1, Nphp3, Anks6 (also called Pkdr1/Nphp16), and Pkhd1 have since been identified as responsible for the development of renal cysts in murine strains in the cpk mouse, pcy mouse, Han:SPRD-Cy/+ rat (commonly known as the Cy rat), and PCK rat, respectively. Their gene products were reported to be present in cilia proteins such as PC-1, PC-2, and FPC, which are the products of the expressions of ADPKD genes Pkd1 and Pkd2 and the ARPKD gene Pkhd1, respectively [20]. The characteristics of the aforementioned spontaneous animal models are listed below.
2.1. cpk Mice
Renal disorders in cpk mice are caused by a mutation in Cys1. The gene product, cystin, regulates myc expression through its interaction with the tumor suppressor necdin. Cys1 was confirmed to be orthologous mouse gene for humans with ARPKD [21]. A study has also been reported that M2-like macrophages from cpk mice contribute to the progression of cystic cell proliferation, cyst growth, and development of fibrosis. Treatments that block the emergence of these types of immune cells are thought to be emerging medications that prevent disease progression [22].
2.2. pcy Mice
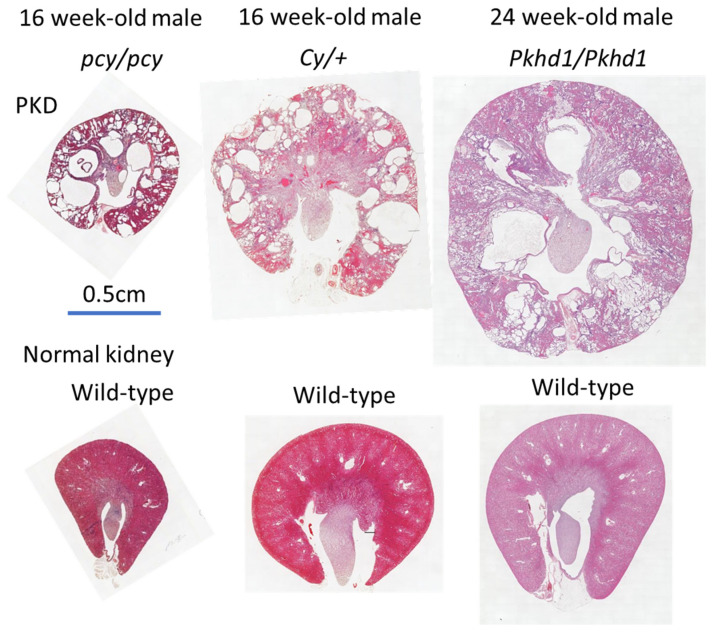
The dilation of the distal tubules along the corticomedullary junction leads to the formation of renal cysts throughout the nephron in pcy mice (Figure 1) [23]. Disease progression in pcy mice, which occurs more rapidly in females than in males, is relatively gradual, leading to a shortened lifespan of 40–50 weeks secondary to renal failure, compared with up to 3 years in native mice [24]. The renal pathology is caused by the missense mutation (T1841G) of Nphp3 on chromosome 9 [25]. Consequently, the production of cyclooxygenase (COX) increases, whereas that of lipoxygenase (LOX) decreases in the kidneys of pcy mice, suggesting that altered eicosanoids are involved in NPHP progression. Therefore, the manipulation of these levels and balances with pharmaceutical drugs may have potential therapeutic benefits [26]. A recent report showed that a phosphate-restricted diet in pcy mice increased the serum levels of calcium and expression levels of Klotho, inhibited renal cyst formation, and activated the signaling cascades involved in the development of renal fibrosis [27].
Figure 1.
Macrophotographs in the hematoxylin and eosin-stained kidneys of pcy mice and Cy rats and the PAS-stained kidneys of PCK rats.
2.3. Cy Rats
In Cy rats, the missense mutation in Anks6 on chromosome 5 causes an R823W substitution of SamCystin, the native gene product, which results in a renal cystic disorder [28,29]. The phenotype exhibits incomplete dominance in homozygotes (Cy/Cy), which are known to rapidly develop renal cysts and cause death by ~3 weeks of age [30]. Heterozygotes (Cy/+) exhibit a slower disease progression, with an average lifespan of ~1 year in males and 18 months in females (Figure 1) [25]. Recent studies have shown that a 3D capsule device overlaying the entire kidney of a Cy/+ rat reduced the kidney weight, size of the renal cysts, and proliferation rate of both cystic epithelial cells and macrophage infiltration [31].
2.4. PCK Rats
PCK rats develop renal and hepatic disorders because of the deletion of the Pkhd1 exon 36, which is orthologous to the human gene responsible for ARPKD [32,33]. The PCK rats develop Caroli’s disease, which is characterized by the dilation of the intrahepatic bile ducts and hepatic fibrosis and cysts derived from the collecting ducts, which spread throughout the renal nephrons (Figure 1) [34]. The lifespan of females is over 6 months longer than the 18-month lifespan of males [25]. Tolvaptan, an arginine vasopressin (AVP) V2-receptor antagonist developed in Japan, has shown beneficial effects on PCK rats [35]. Subsequently, it has been approved in many countries and has become the world’s first drug used to treat ADPKD [36]. Previous studies have also reported that increasing water intake significantly ameliorated disease progression in PCK rats by reducing AVP secretion into the blood from the posterior pituitary gland [37].
3. Genetically Modified Models
The goal of research in genetically mediated diseases is to determine whether its manifestation is caused by the gain or loss of function caused by the expression of the mutation. Transgenic models are useful when gain-of-function is the etiology, whereas KO or gene-targeting models are useful when renal disorders are caused by loss of function, with gene mutations occurring in all cells from the embryonic and fetal stages [38,39].
3.1. KO and CKO Mice
Owing to embryonic lethality in KO homozygous mice, CKO animals were developed with induced mutations limited to specific tissues/cells or introduced at controlled times during organ development. In some CKO animals [40,41,42], it is possible to control the rate of disease progression and cause gene disruption in specific organs through flox mice, which have a gene locus flanking the target region using the Cre-loxP system, and mating with Cre-expressing mice [43].
In ADPKD CKO model mice presenting with mitochondrial dysfunction, the administration of MitoQuinone, a mitochondrion-specific antioxidant, caused the inactivation of ERK/MAPK signaling, reduction of intracellular superoxide levels, and inhibition of cellular proliferation in cystic epithelia [44]. Further, in CKO model mice, the administration of Mdivi-1, a mitogenic protein DRP-1 inhibitor, suppressed disease progression [45].
By contrast, the Yes-associated protein (YAP) was identified as a key transcription factor in the Hippo signaling pathway [46]. CKO mice showed an increase in actomyosin contraction, YAP nuclear translocation, and YAP transcriptional activity [47]. Fasudil reversed YAP activation and suppressed renal disease progression [48]. In other CKO mice, reducing YAP expression with an antisense oligonucleotide did not ameliorate renal cystic disease; however, it did overexpress the downstream targets of the WNT and TGF-β pathways, Myc, Acta2, and Vim [49]. Further studies on the role of YAP in PKD progression deserve serious consideration.
Cyclic adenosine monophosphate (cAMP) is known to mediate cell proliferation and fluid secretion of renal cystic epithelia in PKD [50]. In the CKO mouse, the administration of a pharmacological inhibitor of the cAMP response element binding protein (CREB) and a dominant-negative inhibitor of CREB suppressed renal cystic area expansion [51]. The reduction of the intracellular cAMP concentration by SR59230A, a selective β3-adrenergic receptor antagonist, suppressed renal cystic disease progression in other CKO mice [52].
Macrophage recruitment and interstitial inflammation are involved in the exacerbation of PKD pathology by promoting cystic growth. Tumor necrosis factor-like weak inducer of apoptosis (TWEAK) and its receptor, the fibroblast growth factor, inducible 14 (Fn14), were expressed in the macrophages of affected mice [53]. Their overexpression was detected in two kinds of CKO mice, in which the administration of TWEAK led to the exacerbation of PKD, and treatment with anti-TWEAK antibodies ameliorated PKD, resulting in improved survival [54].
Interferon regulatory factor-5 (IRF5) is a transcription factor associated with renal cyst-promoting cytokines in macrophages. An injection of the IRF5 antisense oligonucleotide into CKO mice reduced the number of macrophages, IRF5 expression in the identified macrophages, and renal cystic disease severity [55].
3.2. Double-Mutant Mice
Several studies have used double-mutant models in which a target gene is mutated other than the CKO gene responsible for PKD. In this regard, the Pkd1RC/RC Pkd2+/− mouse presenting with congenital renal cysts shows moderate renal disease progression, where cysts continue to grow proportionally with the ferritin level [56]. Treatment with ciclopirox olamine salt, an antifungal agent, reduced renal cyst progression and improved renal function by decreasing the ferritin level [57].
In another Pkhd1-Cre; Pkd2flox/flox; miR-214−/− model mouse, increased accumulation of pericystic macrophages was detected with an upregulation of the inflammatory TLR4/IFN-γ/STAT1 signaling pathway [58]. miR-214, a microRNA, restrained cyst-associated inflammation (by inhibiting TLR4) and attenuated cyst growth [59]. In a study aimed at elucidating the effect of microRNA, the administration of RGLS4326, an anti-miR-17 oligonucleotide, suppressed the progression of PKD in CKO mice [60].
The procedure for renal fibrosis suppression in double-mutant PKD models with YAP gene deletion or renal collecting duct-specific gene CCN2 deletion has included the administration of verteporfin, the YAP inhibitor that is known to have an inhibitory effect on the fibrotic process [61].
3.3. Knock-in Mice
A knock-in model with hypomorphic alterations in the mitochondrial morphology was identified in Pkd1RC/RC and Pkd1null/RC mice, corresponding to a disease variant in the ADPKD phenotype [62,63]. Recently, these strains have been used in the experimental administration of drugs affecting the signaling pathways altered by Pkd1 mutations. The following drugs showed ameliorative effects on renal disease progression (Table 1): AMPK activators, metformin [64], lixivaptan (a novel AVPR2 antagonist), with R-568 (a calcium receptor agonist for a combined inhibitory effect) [65], BLU2864, a PKA inhibitor [66], a CFTR-trafficking and processing modulator, VX-809, [67], nintedanib, a tyrosine kinase inhibitor [68], and a combination treatment with tolvaptan (an AVPV2 receptor antagonist), and pasireotide (a somatostatin analog) [69].
Table 1.
Animal models and their applications are based on recently reported novel findings.
| Gene | Strain/Gene Name | Treatment/Analysis/ Administration |
Results/Effects | References |
|---|---|---|---|---|
| Cy Rat | ||||
| Nphp16 | Han:SPRD-Cy/+ | 3D capsule device | Suppression of the PKD progression. | [31] |
| Nphp16 | Han:SPRD-Cy/+ | MitoQuinone, a mitochondria-specific antioxidant | Inactivation of ERK/MAPK. Reduction of intracellular superoxide. Inhibited proliferation of the epithelial cysts. | [44] |
| pcy Mouse | ||||
| Nphp3 | Pcy | RGLS4326, an anti-miR-17 oligonucleotide | Suppression of the PKD progression. | [60] |
| PCK Rat | ||||
| Pkhd1 | PCK | Lixivaptan, a novel V2R antagonist and R-568, a calcium receptor agonist | Decrease in the cAMP level. Suppression of the PKA activity. Decrease in the phosphorylated AMPK and ERK. Suppression of the PKD progression. Suppression of fibrosis. | [67] |
| KO and CKO Mice | ||||
| Pkd1 | Pkd1flox/flox; Ksp-Cre | MitoQuinone, a mitochondria-specific antioxidant | Inactivation of ERK/MAPK. Reduction of intracellular superoxide. Inhibited proliferation of epithelial cysts. | [44] |
| Pkd1 | Pkd1flox/−; Ksp-Cre | - | Disturbances in mitochondrial structure and function. Decreased expression of the fusion-promoting proteins OPA1 and MFN1. Increased expression of the mitogenic protein DRP1. | [45] |
| Mdivi-1, a DRP-1 inhibitor | Suppression of the PKD progression. Improvement of the renal function. | |||
| Pkd1 | Pkd1flox/−; Ksp-Cre | - | Increased actomyosin contraction. YAP nuclear translocation. Enhanced YAP transcriptional activity. | [48] |
| Fasudil, a protein kinase inhibitor | Inhibition of Rho kinase (ROCK)-dependent actomyosin contraction. Inhibition of YAP activity. | |||
| Pkd1 | iKspPkd1 del | Antisense oligonucleotides | Downregulation of YAP, a key transcription factor in the Hippo signaling pathway, but upregulation of downstream targets Myc, Acta2, and Vim, in the WNT and TGF-β pathways. | [49] |
| Pkd1 | Pkd1fl/fl; Cre/Esr1+ | - | Increase of phosphorylated CREB (p-CREB) and of active histone modifications (H3K4me3 and H3K27ac). | [51] |
| 666-15, a pharmacological inhibitor of CREB (cAMP response element binding protein) | Inhibition of the expansion of the cystic area. | |||
| Pkd1fl/fl; Cdh16-Cre | Genetic inhibition with a dominant-negative inhibitor of CREB (A-CREB) | Inhibition of the cystic area expansion. | ||
| Gene | Strain/Gene Name |
Treatment/Analysis/
Administration |
Results/Effects | References |
| KO and CKO Mice continued | ||||
| Pkd1 | Pkd1fl/fl; Pax8rtTA; TetO-Cre | SR59230A, a selective β3-adrenergic receptor antagonist | Reduction of cAMP concentration. Inhibition of the PKD progression. Partial improvement of the renal function. | [52] |
| Pkd1 |
Pkd1cond/cond; Tam-Cre2, Pkd1cond/cond; Tam-Cre1 |
- | Overexpression of TWEAK (Tumor necrosis factor-like weak inducer of apoptosis) and Fn14 (fibroblast growth factor-inducible 14). | [54] |
| TWEAK (Tumor necrosis factor-like weak inducer of apoptosis) anti-TWEAK |
Exacerbation of PKD progression. Suppression of PKD progression. Improvement of the survival rate. Decrease in cell proliferation, NF-κB pathway activation, fibrosis, apoptosis, and macrophage infiltration. | |||
| Pkd1 | Pkd1f/f; Cre-ERTM | IRF5 (Interferon regulatory factor 5) antisense oligonucleotides | Suppression of PKD progression. Reduced number of macrophages. Reduced homeostasis. Decreased expression of the IRF5 in the macrophages. | [55] |
|
Pkd1
Pkd2 |
Pkd1RC/RC Pkd2+/−, Pkd1RC/RC Pkd2+/+ |
- | Cystic formation. Elevated ferritin levels. | [57] |
| CPX (Ciclopirox; 6-Cyclohexyl-1-hydroxy-4-methyl-2(1H)-pyridone) or its olamine salt (CPX-O) | Suppression of PKD progression. Decreased ferritin levels. | |||
|
Pkd1
Pkd2 |
Ksp-Cre; Pkd1fl/fl, Pkhd1-Cre; Pkd2fl/fl, Pkd1RC/RC, Pkhd1-Cre; Pkd2fl/fl; miR-214−/− | Inhibition of miR-214 (double mutant) |
Exacerbation of PKD progression. Increased Tlr4 expression (inflammatory TLR4/IFN-γ/STAT1 signaling pathway). Increased accumulation of the pericystic macrophages. | [59] |
| Pkd2 | Pkhd1-Cre; Pkd2F/F | RGLS4326, an anti-miR-17 oligonucleotide | Suppression of PKD progression. | [60] |
| Pkd1 | Pkd1f/f; Pkhd1cre, Pkd1f/f; Yapf/f; Pkhd1cre, Pkd1f/f; CCN2f/f; Pkhd1cre | Verteporfin, a YAP inhibitor Deletion of YAP gene (double mutant) Deletion of CCN2, a renal collecting duct-specific gene (double mutant) |
Inhibition of renal fibrosis. | [61] |
| Pkd1 | Pkd1f/f; Pkhd1-Cre | Nintedanib, which selectively inhibits PDGFR, FGFR, and VEGFR | Suppression of PKD progression. Reduced proliferation of epithelial cysts. Decreased expression of growth factors including YAP. | [68] |
| Pkd1 | Pkd1fox/ − ; Ksp-Cre | Curcumin and ginkgolide B | Suppression of EGFR/ERK1/2, JNK, PI3K/mTOR, and p38 signaling pathways. | [70] |
| Pkd1 | Pkd1loxp/loxp; Ksp-Cre | Cardamomine nominated from natural product library screening | Inhibition of PKD progression. Inhibition of renal cyst development and interstitial fibrosis. | [71] |
| Pkd1 | Pkd1fl/fl; Pkhd1-Cre | Vorasertib, an inhibitor of Plk1 (Polo-like kinase 1) | Suppression of PKD progression by the antioxidant action pathway of peroxiredoxin 5 (Prdx5)-Polo-like kinase 1 (Plk1). | [72] |
| Pkd1 | Pkd1fl/fl; Pax8rtTA; TetO-Cre | Hydroxyfasudil, a ROCK (Rho-associated coiled-coil containing protein kinase) inhibitor | Suppression of PKD progression. Reduction of centrosome RhoGAP (ARHGAP). Suppression of ROCK signaling pathway. | [73] |
| Pkd1 | Pkd1fl/fl; Pax8rtTA; TetO-Cre | - | Increased activity of calcium-dependent CAPN (Calpain) protease. | [74] |
| CAPN (Calpain) inhibitor | Restoration of lysosomal function. CTSB processing/activity, autophagosome and lysosomal fusion. | |||
| Gene | Strain/Gene Name |
Treatment/Analysis/
Administration |
Results/Effects | References |
| KO and CKO Mice continued | ||||
| Pkd1 | Pkd1fox/fox; Nestincre, Pkd1fox/−; Nestincre | Secondhand smoke exposure | Acceleration of PKD progression. Increased tubular cell proliferation and apoptosis. Promotion of renal fibrosis. Reduction of glutathione level. Decreased contractile function and structural parameters in the heart. Noticeable reduction of body weight. | [75] |
| Pkd1 | KspCreERT2; Pkd1lox/lox | - | Increased expression of the transmembrane Protein 16A (TMEM16A) and the cystic fibrosis transmembrane conductance regulator (CFTR). Increase of the cystic area. | [76] |
| TMEM16A(transmembrane Protein 16A) antagonists niclosamide and benzbromarone TMEM16A-specific inhibitor Ani9 |
Inhibition of TMEM16A. Reduced expansion of the cystic area. Suppression of the abnormal proliferation of the epithelial cysts. |
|||
| Pkd2 | Pkd2−/− | DA1(dopamine receptor 1) antagonist, SCH23390 | Suppression of disease progression in PKD. Restored sensitivity of flow-activated Na+ and HCO3− transport. | [77] |
| Pkd2 | Pkhd1-Cre; Pkd2F/F; miR-21−/− | Inhibition of miR-21 (double mutant) |
Suppressed expansion of cyst area by regulating apoptosis and proliferation of epithelial cells, and interstitial inflammation. | [78] |
| Pkd1 | Pkd1RC/RC | - | Increased expression of IGF-1 pathway genes. | [79] |
| Pkd1RC/RC; Pappa+/–, Pkd1RC/RC; Pappa–/– | Deletion of PAPP-A (Pregnancy Associated Plasma Protein A) gene (double mutant) |
Inhibition of disease progression in PKD. | ||
| Pkd1 |
Pkd1flox/flox; Ksp-Cre Pkd1flox/flox; Aqp2-Cre |
- | Increased activity of the focal adhesion kinase (FAK). | [80] |
| FAK (focal adhesion kinase) inhibitors (double mutant) |
Suppression of PKD progression. Inhibition of FSK/Src activity. Upregulation of ERK and mTOR signaling pathways. | |||
| Pkd1 | Pkd1F/RC | - | Increased methionine and S-adenosylmethionine (SAM). | [81] |
| Pkd1RC/RC | Dietary restriction of methionine | Dietary restriction of methionine. | ||
| Ksp-Cre; Pkd1F/RC; Mettl3F/F | Deletion of Mettl3 gene, a key component of SAM (double mutant) |
Delayed expansion of cysts. | ||
| Pkd1 | KspCreERT2; Pkd1lox/lox; Tmem16alox/lox | TMEM16A gene (double mutant) |
Inhibition of Ca2+ signaling pathway and cell proliferation. Increased CFTR expression. | [82] |
| Pkd1fl/fl; Cre/Esr1, | Quantitative proteomics | Promotion of the Nuclear Factor Erythroblast 2-Related Factor 2 (NRF2) degradation. | ||
| Pkd1fl/fl; Cre/Esr1; Nrf2 − / − | Deletion of NRF2 gene (double mutant) |
Increased ROS generation. Inhibition of the cystic area expansion. | ||
| Gene | Strain/Gene Name |
Treatment/Analysis/
Administration |
Results/Effects | References |
| Knock-in Mouse | ||||
| Pkd1 |
Pkd1RC/null, Pkd1RC/RC |
PKD1 targeted proteomic analysis | Reduction of TCA cycle, fatty acid oxidation, respiratory complexes, and endogenous antioxidants. | [62] |
| Overexpression of mitochondria-targeted catalase (mCAT) using an adeno-associated virus vector | Reduction of mitochondrial Reactive Oxygen Species (ROS) and oxidative damage. Improvement of disease progression in PKD. Partial improvement in the TCA cycle and fatty acid oxidation. | |||
| Pkd1 | Pkd1RC/RC | Eramipretide, a mit ochondrial protective tetrapeptide |
Attenuated ERK1/2 phosphorylation. Improved mitochondrial supercomplex formation. Improvement of PKD progression. | [63] |
| Pkd1 | Pkd1RC/RC | Metformin | Suppression of PKD progression. Reduction of cell proliferation markers. Reduction of inflammation and injury markers. | [64] |
| Pkd1 | Pkd1RC/RC | Lixivaptan, a novel Vasopressin Receptor 2 (V2R) antagonist and R-568, a calcium receptor agonist | Reduction of the cAMP levels. Suppression of the PKA activity. Reduction of phosphorylated AMPK and ERK. Suppression of PKD progression. Suppression of fibrosis. | [65] |
| Pkd1 | Pkd1RC/RC | BLU2864, a selective PRKACA (AMP-dependent protein kinase) inhibitor | Inhibition of PKA activity. Inhibition of cyst formation, growth-promoting pathways, and cyst formation. | [66] |
| Pkd1 | Pkd1RC/RC | VX-809, a modulator of CFTR trafficking and processing | Increased basolateral membrane co-localization of CFTR. Decreased HSP27. Inhibition of PKD progression. | [67] |
| Pkd1 | Pkd1RC/RC | Nintedanib, a receptor tyrosine kinase (RTK) inhibitor | Suppression of PKD progression. Suppression of the cell proliferation. Reduction of the growth factor and fibrosis expressions. | [68] |
| Pkd1 | Pkd1RC/RC | Administration of Extracellular Vesicle (EV)/exosomes, Increased expression of EV/exosomes | Promotion of cyst formation and fibrosis. Increased phosphorylation of AKT, S6, Rb, STAT3, ERK. |
[83] |
| GW4869 to inhibit exosome biogenesis/release | Suppression of cyst formation. | |||
| Pkd1 | Pkd1RC/RC | Targeted metabolomics approach | Alteration of the biosynthesis and metabolism of tryptophan and arginine. Increase of indoles, kynurenine, and polyamines. | [84] |
| Genome Editing | ||||
| Pkhd1 | Pkhd1C642* | Genome editing | Heterozygous Pkhd1C642* developed hepatic cysts. Homozygous Pkhd1C642* developed congenital hepatic fibrosis, inflammation of the portal field, fibrosis manifestations. | [85] |
| Nphp1 | Nphp1del2−20/del2−20 | Genome editing | Renal cysts. Thickening of the tubular basement membrane. Retinal degeneration. Abnormal spermatogenesis. | [86] |
| Using of AAV9 vectors | Partial rescue of both renal and retinal phenotypes. | |||
Reference numbers also serve as reference numbers in the text.
3.4. Genome Editing
Recently, model animals have been created using genome-editing techniques such as CRISPR/Cas9 [87]. For instance, in the Pkhd1C642* mouse with a predicted truncating mutation in the middle of exon 20, a cluster of five truncating human mutations between Pkhd1G617fs and Pkhd1G644* was generated. In the heterozygous Pkhd1C642* mouse, hepatic cysts developed, whereas in the homozygous mouse, congenital hepatic fibrosis, inflammation of the portal field, and fibrosis manifestations developed, suggesting that the heterozygous PKHD1 mutation might cause cystic liver disorders [85]. Another gene-editing model in Nphp1del2−20/del2−20 mice mimicked human NPHP, with the development of renal cysts, thickening of the tubular basement membrane, retinal degeneration, and abnormal spermatogenesis. An adenoviral-associated-virus-9 vector was noted to partially rescue both renal and retinal phenotypes [86]. Further ingenuity in genome-editing techniques is certainly on the horizon because KO model animals inconsistently reflect the changes seen in human renal cystic diseases.
4. Discussion
This review described animal model research for the treatment of human renal cystic diseases, focusing on recently published papers.
For the drug treatment study, we recommend using several kinds of models. Specifically, phenotypically established spontaneous models, such as pcy mice, Cy rats, and PCK rats, which reliably exhibit pathology with relatively long lifespans of more than half a year, are suitable for medicine efficacy experiments. In the KO mouse model, the orthologous gene is always mutated; however, the pathology differs depending on the mutation site. The models’ lifespans are usually either too short or too long. It is suitable for the analysis of cystogenesis rather than medicine efficacy experiments, including preclinical trials. In the CKO model and the hypomorphic allele model, the orthologous gene is always mutated, and the pathology is constant, although it is necessary for a relatively long period. Therefore, it is suitable for both medicine efficacy experiments and analyses of cystogenesis (Pkd1flox/flox; Ksp-Cre, Pkd1RC/RC).
To determine the efficacy of treatments, kidney volume, kidney-weight-to-body-weight ratio, urine/plasma biomarkers (creatinine, urea nitrogen, L-FABP, etc.), renal cAMP concentrations, and/or histopathological indices (fibrosis index, cyst area, cell proliferation index, and target protein distribution) are important outcome indicators.
In both spontaneous and genetically modified models, disease progression is often variable. Thus, the number of control vehicle animals should not be too small when conducting a preclinical efficacy trial, and each group should include a sufficient number of animals to determine efficacy accurately. The clinical presentation of human and rodent PKD is most pronounced in adulthood. However, it is generally desirable to start preclinical trials during the early stage when there are few clinical features and continue until clinical symptoms appear in the control vehicle group. Both male and female animals should be used because of clinical evidence of gender hormone influence. Because PKD is a kidney disease, the concentration and quality of proteins in chow during the treatment should be considered. Moreover, since animal welfare and humane care are important, animal experiments should follow the ARRIVE 2.0 guidelines (https://arriveguidelines.org/arrive-guidelines, accessed on 1 November 2022).
To increase the credibility of the results, the use of multiple models, including spontaneous and genetically modified models, or mouse and rat models, is effective because the same drug may have both beneficial and adverse effects on different animal models. This indicates the difficulty in determining which model is relevant or not.
Based on our experience with numerous model animals for drug efficacy studies, some of the existing models exhibit disease progression too early and others too late, and some are appropriate as pathological models; however, the responsible gene is not orthologous to human patients. Further efforts are required to develop pathological models of human PKD.
5. Summary and Conclusions
Several representative models of renal cystic disease were reviewed in this article; however, it is difficult to exhaustively cover them all. We listed the models with their applications based on recently reported novel findings (Table 1). As mentioned, these models may become useful for the development of new therapeutic options based on the discovery of novel signaling pathways and involve the verification of factors in the exacerbation of PKD. Medications may have variable rates of response and efficacy when administered to different animal models, and the use of multiple animal strains has been proven critical in the development of effective therapeutic options. In this review, we studied animals that spontaneously developed renal cysts and genetically modified animals with their respective benefits. Currently, the number of studies on animal models of renal cystic diseases is increasing exponentially compared with previous decades. We believe that this review will benefit those seeking to understand the utility and assist in the classification of animal models of human renal cystic diseases to make treatment available to all patients.
Author Contributions
Conceptualization, writing—original draft preparation, review, and editing: S.N. and T.Y. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Not applicable.
Conflicts of Interest
S.N. has received speaker/consultancy honoraria from Otsuka Pharmaceuticals. The funder had no role in the writing and publication of the manuscript.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Sekine A., Hidaka S., Moriyama T., Shikida Y., Shimazu K., Ishikawa E., Uchiyama K., Kataoka H., Kawano H., Kurashige M., et al. Cystic kidney diseases that require a differential diagnosis from autosomal dominant polycystic kidney disease (ADPKD) J. Clin. Med. 2022;11:6528. doi: 10.3390/jcm11216528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mei C.-L., Xue C., Yu S.-Q., Dai B., Chen J.-H., Li Y., Chen L.-M., Liu Z.-S., Wu Y.-G., Hu Z., et al. Executive Summary: Clinical Practice Guideline for Autosomal Dominant Polycystic Kidney Disease in China. Kidney Dis. 2020;6:144–149. doi: 10.1159/000506288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cornec-Le Gall E., Alam A., Perrone R.D. Autosomal dominant polycystic kidney disease. Lancet. 2019;393:919–935. doi: 10.1016/S0140-6736(18)32782-X. [DOI] [PubMed] [Google Scholar]
- 4.Colbert G.B., Elrggal M.E., Gaur L., Lerma E.V. Update and review of adult polycystic kidney disease. Dis.-A-Mon. 2020;66:100887. doi: 10.1016/j.disamonth.2019.100887. [DOI] [PubMed] [Google Scholar]
- 5.Bergmann C., Guay-Woodford L.M., Harris P.C., Horie S., Peters D.J.M., Torres V.E. Polycystic kidney disease. Nat. Rev. Dis. Primers. 2018;4:50. doi: 10.1038/s41572-018-0047-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elisakova V., Merta M., Reiterova J., Baxova A., Kotlas J., Hirschfeldova K., Obeidova L., Tesar V., Stekrova J. Bilineal inheritance of pathogenic PKD1 and PKD2 variants in a Czech family with autosomal dominant polycystic kidney disease—A case report. BMC Nephrol. 2018;19:163. doi: 10.1186/s12882-018-0978-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong K., Zhang C., Tian X., Coman D., Hyder F., Ma M., Somlo S. Renal plasticity revealed through reversal of polycystic kidney disease in mice. Nat. Genet. 2021;53:1649–1663. doi: 10.1038/s41588-021-00946-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gall E.C.-L., Audrézet M.-P., Chen J.-M., Hourmant M., Morin M.-P., Perrichot R., Charasse C., Whebe B., Renaudineau E., Jousset P., et al. Type of PKD1 Mutation Influences Renal Outcome in ADPKD. J. Am. Soc. Nephrol. 2013;24:1006–1013. doi: 10.1681/ASN.2012070650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gallagher A.R., Somlo S. Loss of Cilia Does Not Slow Liver Disease Progression in Mouse Models of Autosomal Recessive Polycystic Kidney Disease. Kidney360. 2020;1:962–968. doi: 10.34067/KID.0001022019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goggolidou P., Richards T. The genetics of Autosomal Recessive Polycystic Kidney Disease (ARPKD) Biochim. Biophys. Acta Mol. Basis Dis. 2022;1868:166348. doi: 10.1016/j.bbadis.2022.166348. [DOI] [PubMed] [Google Scholar]
- 11.Guay-Woodford L.M., Desmond R.A. Autosomal Recessive Polycystic Kidney Disease: The Clinical Experience in North America. Pediatrics. 2003;111:1072–1080. doi: 10.1542/peds.111.5.1072. [DOI] [PubMed] [Google Scholar]
- 12.MacKay C.E., Floen M., Leo M.D., Hasan R., Garrud T.A.C., Fernández-Peña C., Singh P., Malik K.U., Jaggar J.H. A plasma membrane-localized polycystin-1/polycystin-2 complex in endothelial cells elicits vasodilation. eLife. 2022;11:e74765. doi: 10.7554/eLife.74765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim I., Li C., Liang D., Chen X.-Z., Coffy R.J., Ma J., Zhao P., Wu G. Polycystin-2 Expression Is Regulated by a PC2-binding Domain in the Intracellular Portion of Fibrocystin. J. Biol. Chem. 2008;283:31559–31566. doi: 10.1074/jbc.M805452200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hildebrandt F., Zhou W. Nephronophthisis-Associated Ciliopathies. J. Am. Soc. Nephrol. 2007;18:1855–1871. doi: 10.1681/ASN.2006121344. [DOI] [PubMed] [Google Scholar]
- 15.Malik S.A., Modarage K., Goggolidou P. The Role of Wnt Signalling in Chronic Kidney Disease (CKD) Genes. 2020;11:496. doi: 10.3390/genes11050496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vogel P., Read R.W., Hansen G.M., Powell D.R. Histopathology is required to identify and characterize myopathies in high-throughput phenotype screening of genetically engineered mice. Vet. Pathol. 2021;58:1158–1171. doi: 10.1177/03009858211030541. [DOI] [PubMed] [Google Scholar]
- 17.Shakya M., Lindberg I. Mouse Models of Human Proprotein Convertase Insufficiency. Endocr. Rev. 2021;42:259–294. doi: 10.1210/endrev/bnaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ren Z.-L., Zhang H.-B., Li L., Yang Z.-L., Jiang L. Characterization of two novel knock-in mouse models of syndromic retinal ciliopathy carrying hypomorphic Sdccag8 mutations. Zool. Res. 2022;43:442–456. doi: 10.24272/j.issn.2095-8137.2021.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim J.H., Yu J., Kim H.K., Kim J.Y., Kim M.S., Cho Y.G., Bae S., Kang K.K., Jung Y.J. Genome editing of golden SNP-carrying lycopene epsilon-cyclase (LcyE) gene using the CRSPR-Cas9/HDR and geminiviral replicon system in rice. Int. J. Mol. Sci. 2022;23:10383. doi: 10.3390/ijms231810383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richards T., Modarage K., Malik S.A., Goggolidou P. The cellular pathways and potential therapeutics of Polycystic Kidney Disease. Biochem. Soc. Trans. 2021;49:1171–1188. doi: 10.1042/BST20200757. [DOI] [PubMed] [Google Scholar]
- 21.Yang C., Harafuji N., O’Connor A.K., Kesterson R.A., Watts J.A., Majmundar A.J., Braun D.A., Lek M., Laricchia K.M., Fathy H.M., et al. Cystin genetic variants cause autosomal recessive polycystic kidney disease associated with altered Myc expression. Sci. Rep. 2021;11:18274. doi: 10.1038/s41598-021-97046-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Swenson-Fields K.I., Vivian C.J., Salah S.M., Peda J.D., Davis B.M., van Rooijen N., Wallace D.P., Fields T.A. Macrophages promote polycystic kidney disease progression. Kidney Int. 2013;83:855–864. doi: 10.1038/ki.2012.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torres J.A., Rezaei M., Broderick C., Lin L., Wang X., Hoppe B., Cowley B.D., Savica V., Torres V.E., Khan S., et al. Crystal deposition triggers tubule dilation that accelerates cystogenesis in polycystic kidney disease. J. Clin. Investig. 2019;129:4506–4522. doi: 10.1172/JCI128503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shibazaki S., Yu Z., Nishio S., Tian X., Thomson R.B., Mitobe M., Louvi A., Velazquez H., Ishibe S., Cantley L.G., et al. Cyst formation and activation of the extracellular regulated kinase pathway after kidney specific inactivation of Pkd1. Hum. Mol. Genet. 2008;17:1505–1516. doi: 10.1093/hmg/ddn039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nagao S., Kugita M., Yoshihara D., Yamaguchi T. Animal Models for Human Polycystic Kidney Disease. Exp. Anim. 2012;61:477–488. doi: 10.1538/expanim.61.477. [DOI] [PubMed] [Google Scholar]
- 26.Yamaguchi T., Lysecki C., Reid A., Nagao S., Aukema H.M. Renal Cyclooxygenase Products are Higher and Lipoxygenase Products are Lower in Early Disease in the pcy Mouse Model of Adolescent Nephronophthisis. Lipids. 2013;49:39–47. doi: 10.1007/s11745-013-3859-2. [DOI] [PubMed] [Google Scholar]
- 27.Takenaka T., Kobori H., Inoue T., Miyazaki T., Suzuki H., Nishiyama A., Ishii N., Hayashi M. Klotho supplementation ameliorates blood pressure and renal function in DBA/2-pcy mice, a model of polycystic kidney disease. Am. J. Physiol. Physiol. 2020;318:F557–F564. doi: 10.1152/ajprenal.00299.2019. [DOI] [PubMed] [Google Scholar]
- 28.Neudecker S., Walz R., Menon K., Maier E., Bihoreau M.-T., Obermüller N., Kränzlin B., Gretz N., Hoffmann S.C. Transgenic Overexpression of Anks6(p.R823W) Causes Polycystic Kidney Disease in Rats. Am. J. Pathol. 2010;177:3000–3009. doi: 10.2353/ajpath.2010.100569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nagao S., Morita M., Kugita M., Yoshihara D., Yamaguchi T., Kurahashi H., Calvet J.P., Wallace D.P. Polycystic kidney disease in Han:SPRD Cy rats is associated with elevated expression and mislocalization of SamCystin. Am. J. Physiol. Physiol. 2010;299:F1078–F1086. doi: 10.1152/ajprenal.00504.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaspareit-Rittinghausen J., Rapp K., Deerberg F., Wcislo A., Messow C. Hereditary Polycystic Kidney Disease Associated with Osteorenal Syndrome in Rats. Vet. Pathol. 1989;26:195–201. doi: 10.1177/030098588902600302. [DOI] [PubMed] [Google Scholar]
- 31.Bae K.T., Kumamoto K., Yoshimura A., Kugita M., Horie S., Yamaguchi T., Bae J.T., Nagao S. Novel 3D capsule device to restrict kidney volume expansion on polycystic kidney progression: Feasibility study in a rat model. J. Nephrol. 2021;35:1033–1040. doi: 10.1007/s40620-021-01160-5. [DOI] [PubMed] [Google Scholar]
- 32.Wang X., Wu Y., Ward C.J., Harris P.C., Torres V.E. Vasopressin Directly Regulates Cyst Growth in Polycystic Kidney Disease. J. Am. Soc. Nephrol. 2007;19:102–108. doi: 10.1681/ASN.2007060688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mason S.B., Liang Y., Sinders R.M., Miller C.A., Eggleston-Gulyas T., Crisler-Roberts R., Harris P.C., Ii V.H.G. Disease Stage Characterization of Hepatorenal Fibrocystic Pathology in the PCK Rat Model of ARPKD. Anat. Rec. 2010;293:1279–1288. doi: 10.1002/ar.21166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sanzen T., Harada K., Yasoshima M., Kawamura Y., Ishibashi M., Nakanuma Y. Polycystic Kidney Rat Is a Novel Animal Model of Caroli’s Disease Associated with Congenital Hepatic Fibrosis. Am. J. Pathol. 2001;158:1605–1612. doi: 10.1016/S0002-9440(10)64116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Torres V.E. Role of Vasopressin Antagonists. Clin. J. Am. Soc. Nephrol. 2008;3:1212–1218. doi: 10.2215/CJN.05281107. [DOI] [PubMed] [Google Scholar]
- 36.Sans-Atxer L., Joly D. Tolvaptan in the treatment of autosomal dominant polycystic kidney disease: Patient selection and special considerations. Int. J. Nephrol. Renov. Dis. 2018;11:41–51. doi: 10.2147/IJNRD.S125942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nagao S., Nishii K., Katsuyama M., Kurahashi H., Marunouchi T., Takahashi H., Wallace D.P. Increased Water Intake Decreases Progression of Polycystic Kidney Disease in the PCK Rat. J. Am. Soc. Nephrol. 2006;17:2220–2227. doi: 10.1681/ASN.2006030251. [DOI] [PubMed] [Google Scholar]
- 38.Wang H., Cui J., Yang C., Rosenblum J.S., Zhang Q., Song Q., Pang Y., Fang F., Sun M., Dmitriev P., et al. A Transgenic Mouse Model of Pacak–Zhuang Syndrome with An Epas1 Gain-of-Function Mutation. Cancers. 2019;11:667. doi: 10.3390/cancers11050667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lam H.C., Siroky B.J., Henske E.P. Renal disease in tuberous sclerosis complex: Pathogenesis and therapy. Nat. Rev. Nephrol. 2018;14:704–716. doi: 10.1038/s41581-018-0059-6. [DOI] [PubMed] [Google Scholar]
- 40.Chen J., Li P., Song L., Bai L., Huen M.S.Y., Liu Y., Lu L.Y. 53BP1 loss rescues embryonic lethality but not genomic instability of BRCA1 total knockout mice. Cell Death Differ. 2020;27:2552–2567. doi: 10.1038/s41418-020-0521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vidalin O., Muslmani M., Estienne C., Echchakir H., Abina A.M. In vivo target validation using gene invalidation, RNA interference and protein functional knockout models: It is the time to combine. Curr. Opin. Pharmacol. 2009;9:669–676. doi: 10.1016/j.coph.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 42.Chenouard V., Remy S., Tesson L., Ménoret S., Ouisse L.H., Cherifi Y., Anegon I. Advances in genome editing and application to the generation of genetically modified rat models. Front. Genet. 2021;12:615491. doi: 10.3389/fgene.2021.615491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhao L., Zhao J., Zhang Y., Wang L., Zuo L., Niu A., Zhang W., Xue X., Zhao S., Sun C., et al. Generation and identification of a conditional knockout allele for the PSMD11 gene in mice. BMC Dev. Biol. 2021;21:4. doi: 10.1186/s12861-020-00233-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ishimoto Y., Inagi R., Yoshihara D., Kugita M., Nagao S., Shimizu A., Takeda N., Wake M., Honda K., Zhou J., et al. Mitochondrial Abnormality Facilitates Cyst Formation in Autosomal Dominant Polycystic Kidney Disease. Mol. Cell. Biol. 2017;37:00337-17. doi: 10.1128/MCB.00337-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cassina L., Chiaravalli M., Boletta A. Increased mitochondrial fragmentation in polycystic kidney disease acts as a modifier of disease progression. FASEB J. 2020;34:6493–6507. doi: 10.1096/fj.201901739RR. [DOI] [PubMed] [Google Scholar]
- 46.Yang T., Heng C., Zhou Y., Hu Y., Chen S., Wang H., Yang H., Jiang Z., Qian S., Wang Y., et al. Targeting mammalian serine/threonine-protein kinase 4 through Yes-associated protein/TEA domain transcription factor-mediated epithelial-mesenchymal transition ameliorates diabetic nephropathy orchestrated renal fibrosis. Metabolism. 2020;108:154258. doi: 10.1016/j.metabol.2020.154258. [DOI] [PubMed] [Google Scholar]
- 47.Leuenroth S.J., Bencivenga N., Igarashi P., Somlo S., Crews C.M. Triptolide Reduces Cystogenesis in a Model of ADPKD. J. Am. Soc. Nephrol. 2008;19:1659–1662. doi: 10.1681/ASN.2008030259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nigro E.A., Distefano G., Chiaravalli M., Matafora V., Castelli M., Gritti A.P., Bachi A., Boletta A. Polycystin-1 Regulates Actomyosin Contraction and the Cellular Response to Extracellular Stiffness. Sci. Rep. 2019;9:16640. doi: 10.1038/s41598-019-53061-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Formica C., Kunnen S., Dauwerse J.G., Mullick A.E., Dijkstra K.L., Scharpfenecker M., Peters D.J.M., the DIPAK Consortium Reducing YAP expression in Pkd1 mutant mice does not improve the cystic phenotype. J. Cell. Mol. Med. 2020;24:8876–8882. doi: 10.1111/jcmm.15512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Casarella A., Nicotera R., Zicarelli M.T., Urso A., Presta P., Deodato F., Bolignano D., De Sarro G., Andreucci M., Russo E., et al. Autosomic dominant polycystic kidney disease and metformin: Old knowledge and new insights on retarding progression of chronic kidney disease. Med. Res. Rev. 2021;42:629–640. doi: 10.1002/med.21850. [DOI] [PubMed] [Google Scholar]
- 51.Liu Z., Liu Y., Dang L., Geng M., Sun Y., Lu Y., Fang Z., Xiong H., Chen Y. Integrative Cistromic and Transcriptomic Analyses Identify CREB Target Genes in Cystic Renal Epithelial Cells. J. Am. Soc. Nephrol. 2021;32:2529–2541. doi: 10.1681/ASN.2021010101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schena G., Carmosino M., Chiurlia S., Onuchic L., Mastropasqua M., Maiorano E., Schena F.P., Caplan M.J. β3 adrenergic receptor as potential therapeutic target in ADPKD. Physiol. Rep. 2021;9:e15058. doi: 10.14814/phy2.15058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Méndez-Barbero N., Gutiérrez-Munoz C., Blázquez-Serra R., Martín-Ventura J.L., Blanco-Colio L.M. Tumor necrosis factor-like weak inducer of apoptosis (TWEAK)/fibroblast growth factor-inducible 14 (Fn14) axis in cardiovascular diseases: Progress and challenges. Cells. 2020;9:405. doi: 10.3390/cells9020405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cordido A., Nuñez-Gonzalez L., Martinez-Moreno J.M., Lamas-Gonzalez O., Rodriguez-Osorio L., Perez-Gomez M.V., Martin-Sanchez D., Outeda P., Chiaravalli M., Watnick T., et al. TWEAK Signaling Pathway Blockade Slows Cyst Growth and Disease Progression in Autosomal Dominant Polycystic Kidney Disease. J. Am. Soc. Nephrol. 2021;32:1913–1932. doi: 10.1681/ASN.2020071094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zimmerman K.A., Huang J., He L., Revell D.Z., Li Z., Hsu J.-S., Fitzgibbon W.R., Hazard E.S., Hardiman G., Mrug M., et al. Interferon Regulatory Factor-5 in Resident Macrophage Promotes Polycystic Kidney Disease. Kidney360. 2020;1:179–190. doi: 10.34067/KID.0001052019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gainullin V.G., Hopp K., Ward C.J., Hommerding C.J., Harris P.C. Polycystin-1 maturation requires polycystin-2 in a dose-dependent manner. J. Clin. Investig. 2015;125:607–620. doi: 10.1172/JCI76972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Radadiya P.S., Thornton M.M., Puri R.V., Yerrathota S., Dinh-Phan J., Magenheimer B., Subramaniam D., Tran P.V., Zhu H., Bolisetty S., et al. Ciclopirox olamine induces ferritinophagy and reduces cyst burden in polycystic kidney disease. J. Clin. Investig. 2021;6:e141299. doi: 10.1172/jci.insight.141299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhou J., Li X. Non-Coding RNAs in Hereditary Kidney Disorders. Int. J. Mol. Sci. 2021;22:3014. doi: 10.3390/ijms22063014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lakhia R., Yheskel M., Flaten A., Ramalingam H., Aboudehen K., Ferrè S., Biggers L., Mishra A., Chaney C., Wallace D.P., et al. Interstitial microRNA miR-214 attenuates inflammation and polycystic kidney disease progression. JCI Insight. 2020;5:e133785. doi: 10.1172/jci.insight.133785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lee E.C., Valencia T., Allerson C., Schairer A., Flaten A., Yheskel M., Kersjes K., Li J., Gatto S., Takhar M., et al. Discovery and preclinical evaluation of anti-miR-17 oligonucleotide RGLS4326 for the treatment of polycystic kidney disease. Nat. Commun. 2019;10:4148. doi: 10.1038/s41467-019-11918-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dwivedi N., Tao S., Jamadar A., Sinha S., Howard C., Wallace D.P., Fields T.A., Leask A., Calvet J.P., Rao R. Epithelial Vasopressin Type-2 Receptors Regulate Myofibroblasts by a YAP-CCN2–Dependent Mechanism in Polycystic Kidney Disease. J. Am. Soc. Nephrol. 2020;31:1697–1710. doi: 10.1681/ASN.2020020190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Daneshgar N., Baguley A.W., Liang P.I., Wu F., Chu Y., Kinter M.T., Benavides G.A., Johnson M.S., Darley-Usmar V., Zhang J., et al. Metabolic derangement in polycystic kidney disease mouse models is ameliorated by mitochondrial-targeted antioxidants. Commun. Biol. 2021;4:1200. doi: 10.1038/s42003-021-02730-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Daneshgar N., Liang P.-I., Lan R.S., Horstmann M.M., Pack L., Bhardwaj G., Penniman C.M., O’Neill B.T., Dai D.-F. Elamipretide treatment during pregnancy ameliorates the progression of polycystic kidney disease in maternal and neonatal mice with PKD1 mutations. Kidney Int. 2021;101:906–911. doi: 10.1016/j.kint.2021.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pastor-Soler N.M., Li H., Pham J., Rivera D., Ho P.-Y., Mancino V., Saitta B., Hallows K.R. Metformin improves relevant disease parameters in an autosomal dominant polycystic kidney disease mouse model. Am. J. Physiol. Physiol. 2022;322:F27–F41. doi: 10.1152/ajprenal.00298.2021. [DOI] [PubMed] [Google Scholar]
- 65.Di Mise A., Wang X., Ye H., Pellegrini L., Torres V.E., Valenti G. Pre-clinical evaluation of dual targeting of the GPCRs CaSR and V2R as therapeutic strategy for autosomal dominant polycystic kidney disease. FASEB J. 2021;35:e21874. doi: 10.1096/fj.202100774R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang X., Jiang L., Thao K., Sussman C.R., LaBranche T., Palmer M., Harris P.C., McKnight G.S., Hoeflich K.P., Schalm S., et al. Protein Kinase A Downregulation Delays the Development and Progression of Polycystic Kidney Disease. J. Am. Soc. Nephrol. 2022;33:1087–1104. doi: 10.1681/ASN.2021081125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yanda M.K., Cebotaru L. VX-809 mitigates disease in a mouse model of autosomal dominant polycystic kidney disease bearing the R3277C human mutation. FASEB J. 2021;35:e21987. doi: 10.1096/fj.202101315R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jamadar A., Suma S.M., Mathew S., Fields T.A., Wallace D.P., Calvet J.P., Rao R. The tyrosine-kinase inhibitor Nintedanib ameliorates autosomal-dominant polycystic kidney disease. Cell Death Dis. 2021;12:947. doi: 10.1038/s41419-021-04248-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hopp K., Hommerding C.J., Wang X., Ye H., Harris P.C., Torres V.E. Tolvaptan plus Pasireotide Shows Enhanced Efficacy in a PKD1 Model. J. Am. Soc. Nephrol. 2015;26:39–47. doi: 10.1681/ASN.2013121312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li Y., Gao J., Yang X., Li T., Yang B., Aili A. Combination of curcumin and ginkgolide B inhibits cystogenesis by regulating multiple signaling pathways. Mol. Med. Rep. 2021;23:195. doi: 10.3892/mmr.2021.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.He J., Zhou H., Meng J., Zhang S., Li X., Wang S., Shao G., Jin W., Geng X., Zhu S., et al. Cardamonin retards progression of autosomal dominant polycystic kidney disease via inhibiting renal cyst growth and interstitial fibrosis. Pharmacol. Res. 2020;155:104751. doi: 10.1016/j.phrs.2020.104751. [DOI] [PubMed] [Google Scholar]
- 72.Agborbesong E., Zhou J.X., Li L.X., Calvet J.P., Li X. Antioxidant enzyme peroxiredoxin 5 regulates cyst growth and ciliogenesis via modulating Plk1 stability. FASEB J. 2022;36:e22089. doi: 10.1096/fj.202101270RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Streets A.J., Prosseda P.P., Ong A.C. Polycystin-1 regulates ARHGAP35-dependent centrosomal RhoA activation and ROCK signaling. J. Clin. Investig. 2020;5:e135385. doi: 10.1172/jci.insight.135385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Peintner L., Venkatraman A., Waeldin A., Hofherr A., Busch T., Voronov A., Viau A., Kuehn E.W., Köttgen M., Borner C. Loss of PKD1/polycystin-1 impairs lysosomal activity in a CAPN (calpain)-dependent manner. Autophagy. 2021;17:2384–2400. doi: 10.1080/15548627.2020.1826716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sousa M.V., Amaral A.G., Freitas J.A., Murata G.M., Watanabe E.H., Balbo B.E., Tavares M.D., Hortegal R.A., Rocon C., Souza L.E., et al. Smoking accelerates renal cystic disease and worsens cardiac phenotype in Pkd1-deficient mice. Sci. Rep. 2021;11:14443. doi: 10.1038/s41598-021-93633-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cabrita I., Kraus A., Scholz J.K., Skoczynski K., Schreiber R., Kunzelmann K., Buchholz B. Cyst growth in ADPKD is prevented by pharmacological and genetic inhibition of TMEM16A in vivo. Nat. Commun. 2020;11:4320. doi: 10.1038/s41467-020-18104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Du Z., Tian X., Ma M., Somlo S., Weinstein A.M., Wang T. Restoration of proximal tubule flow–activated transport prevents cyst growth in polycystic kidney disease. J. Clin. Investig. 2021;6:e146041. doi: 10.1172/jci.insight.146041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lakhia R., Hajarnis S., Williams D., Aboudehen K., Yheskel M., Xing C., Hatley M., Torres V.E., Wallace D.P., Vishal Patel V. MicroRNA-21 Aggravates Cyst Growth in a Model of Polycystic Kidney Disease. J. Am. Soc. Nephrol. 2016;27:2319. doi: 10.1681/ASN.2015060634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kashyap S., Hein K.Z., Chini C.C., Lika J., Warner G.M., Bale L.K., Torres V.E., Harris P.C., Oxvig C., Conover C.A., et al. Metalloproteinase PAPP-A regulation of IGF-1 contributes to polycystic kidney disease pathogenesis. J. Clin. Investig. 2020;5:e135700. doi: 10.1172/jci.insight.135700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.He J., Zhang S., Qiu Z., Li X., Huang H., Jin W., Xu Y., Shao G., Wang L., Meng J., et al. Inhibiting Focal Adhesion Kinase Ameliorates Cyst Development in Polycystin-1–Deficient Polycystic Kidney Disease in Animal Model. J. Am. Soc. Nephrol. 2021;32:2159–2174. doi: 10.1681/ASN.2020111560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ramalingam H., Kashyap S., Cobo-Stark P., Flaten A., Chang C.M., Hajarnis S., Hein K.Z., Lika J., Warner G.M., Espindola-Netto J.M., et al. A methionine-Mettl3-N(6)-methyladenosine axis promotes polycystic kidney disease. Cell Metab. 2021;33:1234–1247.e7. doi: 10.1016/j.cmet.2021.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lu Y., Sun Y., Liu Z., Lu Y., Zhu X., Lan B., Mi Z., Dang L., Li N., Zhan W., et al. Activation of NRF2 ameliorates oxidative stress and cystogenesis in autosomal dominant polycystic kidney disease. Sci. Transl. Med. 2020;12:eaba3613. doi: 10.1126/scitranslmed.aba3613. [DOI] [PubMed] [Google Scholar]
- 83.Ding H., Li L.X., Harris P.C., Yang J., Li X. Extracellular vesicles and exosomes generated from cystic renal epithelial cells promote cyst growth in autosomal dominant polycystic kidney disease. Nat. Commun. 2021;12:4548. doi: 10.1038/s41467-021-24799-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hopp K., Kleczko E.K., Gitomer B.Y., Chonchol M., Klawitter J., Christians U., Klawitter J. Metabolic reprogramming in a slowly developing orthologous model of polycystic kidney disease. Am. J. Physiol. Physiol. 2022;322:F258–F267. doi: 10.1152/ajprenal.00262.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shan D., Rezonzew G., Mullen S., Roye R., Zhou J., Chumley P., Revell D.Z., Challa A.K., Kim H., Lockhart M.E., et al. Heterozygous Pkhd1C642* mice develop cystic liver disease and proximal tubule ectasia that mimics radiographic signs of medullary sponge kidney. Am. J. Physiol. Physiol. 2019;316:F463–F472. doi: 10.1152/ajprenal.00181.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Li D., Hu M., Chen H., Wu X., Wei X., Lin H., Gao X., Wang H., Li M., Ong A.C.M., et al. An Nphp1 knockout mouse model targeting exon 2–20 demonstrates characteristic phenotypes of human nephronophthisis. Hum. Mol. Genet. 2021;31:232–243. doi: 10.1093/hmg/ddab239. [DOI] [PubMed] [Google Scholar]
- 87.Zarei A., Razban V., Hosseini S.E., Tabei S.M.B. Creating cell and animal models of human disease by genome editing using CRISPR/Cas9. J. Gene Med. 2019;21:e3082. doi: 10.1002/jgm.3082. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.