Abstract
Objective
Anxiety sensitivity (AS) has been identified as a transdiagnostic cognitive risk factor for a wide range of affective disorders, including conditions within the obsessive compulsive (OC) spectrum. A growing body of research has demonstrated that directly reducing AS leads to subsequent reductions of other psychiatric symptoms, including anxiety, worry, and mood. To date, no study has examined the efficacy of a brief AS intervention on reducing OC and hoarding symptoms.
Method
Non-treatment seeking young adults (N=104; 83.7% female; 81.7% Caucasian) were selected for having elevated levels of AS, and were then randomized into a single-session, computer-assisted AS intervention or a control condition. OC and hoarding symptoms were assessed at post-treatment, as well as at one week and one month follow-ups.
Results
Results revealed that the intervention, but not the control condition, reduced OC symptoms across the post-intervention follow-up period. Mediation analysis demonstrated that changes in AS mediated changes in OC symptoms due to the intervention. In contrast, the intervention did not have a specific effect on reducing hoarding symptoms.
Conclusions
These findings have important ramifications for understanding the relationship between AS and OC spectrum symptoms, and raise interesting treatment and prevention implications.
Keywords: anxiety sensitivity, obsessive compulsive symptoms, hoarding, prevention
Introduction
Anxiety sensitivity (AS), or “fear of fear,” is a trait-like characteristic reflecting a propensity to fear anxiety-related sensations (Reiss and McNally, 1985). Individuals with elevated levels of AS fear the experience of anxious arousal, as well as the potential physical, psychological, and social consequences of anxiety (Reiss et al., 1986). Unlike trait anxiety, which reflects a general predisposition to respond fearfully to a wide array of stressors, AS centers on a more specific tendency to respond fearfully to anxiety symptoms themselves (McNally, 2002, Taylor, 1999). For example, individuals high in AS may misconstrue benign bodily sensations – such as a racing heart – as being suggestive of heart problems, whereas individuals with low levels of AS will simply regard the sensations as unpleasant. Although AS was originally proposed as a unidimensional construct (Taylor et al., 1992), the latent structure of AS reflects a hierarchical model consisting of one higher order factor (i.e., general AS) and three lower order factors, including physical, cognitive, and social concerns (Zinbarg et al., 1997).
Much of the initial work on AS focused on its relationship to panic and agoraphobia (Schmidt et al., 1997). However, more recent research has demonstrated associations between AS and a wide range of psychopathology. Since AS intensifies anxious reactions and fear-related responding, which in turn, elicit greater tendencies toward avoidance behaviors and fear-conditioning (Reiss, 1991, Taylor, Koch, 1992), AS is thought to have particular relevance for disorders wherein avoidance plays a key role. In line with this hypothesis, AS has been associated in the development and maintenance of numerous anxiety-related conditions, including social anxiety disorder, generalized anxiety disorder, and post-traumatic stress disorder (Deacon and Abramowitz, 2006, Rodriguez et al., 2004). AS has also been linked with substance use disorders, eating disorders, and increased suicidality (Anestis et al., 2008, Capron et al., 2012, Schmidt et al., 2007a). These data suggest that AS may serve as a transdiagnostic risk factor for a wide range of psychiatric syndromes (Boswell et al., 2013).
A growing body of research has indicated that greater levels of AS are likewise associated with various conditions across the obsessive-compulsive (OC) spectrum, which includes conditions characterized by compulsivity and impulsivity (American Psychiatric Association, 2013). In particular, AS has been examined extensively in relation to Obsessive Compulsive Disorder (OCD). OCD is characterized by recurrent and intrusive cognitions and/or images (i.e., obsessions) that bring about distress, as well as persistent behaviors (i.e., compulsions) aimed at neutralizing or defusing the distress associated with the obsessions (American Psychiatric Association, 2013). Significant associations between AS and OCD have been established across a number of investigations with both nonclinical and clinical samples, as well as in studies using different measures of AS and OC symptoms (Robinson and Freeston, 2014). For example, Keough and colleabues (2010) examined the associations between AS and OC symptoms in a large (N = 418) sample of undergraduate students and found significant correlations among these symptoms, which remained significant after accounting for other relevant constructs. Similarly, a recent investigation (Raines et al., 2014) found that AS and OC symptoms were significantly associated in a sample of treatment-seeking patients with a primary OCD diagnosis, despite controlling for comorbid anxiety and depression diagnoses.
Hoarding Disorder, characterized by extreme difficulties with discarding one’s possessions and accompanying debilitating clutter (American Psychiatric Association, 2013), is a second condition within the OC spectrum that has been associated with greater levels of AS. Hoarding was historically considered to reflect a symptom dimension of OCD; however, converging evidence from multiple lines of research have supported the current conceptualization of hoarding as a discrete, multifaceted syndrome, separate from OCD (Mataix-Cols et al., 2010). A number of investigations have demonstrated specific associations between AS and hoarding. For example, using a large, unselected nonclinical sample, Coles and colleagues (2003) found a strong relationship between AS and hoarding behaviors that was similar in strength to that between OCD and hoarding. Additionally, AS contributed significant, unique variance in predicting hoarding behaviors, even when specific hoarding cognitions were included in the model. A multi-study investigation (Timpano et al., 2009) found significant associations between AS and hoarding even after controlling for relevant covariates, including OC symptoms. Finally, a study with a large non-selected clinical sample (N=210) found an association between AS and hoarding, even after covarying for general levels of depression (Medley et al., 2013).
Considered jointly, the literature reviewed above indicates that AS may serve as a risk factor for the development of both Hoarding Disorder and OCD. This possibility is particularly intriguing, given that AS has been identified as a malleable cognitive risk factor. Research has demonstrated that AS is responsive to change through certain cognitive behavioral interventions. Numerous investigations focused on the amelioration of panic disorder have demonstrated significant reductions in AS post-treatment (Schmidt et al., 2000, Westling and Öst, 1999). This research resulted in several investigations aimed at directly reducing AS among at-risk, nonclinical samples (Feldner et al., 2008, Gardenswartz and Craske, 2001). For instance, in the largest AS trial to date, Schmidt, Eggleston, et al. (2007b) randomly assigned 404 participants with elevated levels of AS to either receive a brief Anxiety Sensitivity Amelioration Training (ASAT), or a health and nutrition control training. Results indicated that individuals in the ASAT condition, compared to individuals in the control condition, evidenced greater reductions in AS (30% vs. 17%, respectively). Furthermore, these reductions were specific to AS compared to relevant cognitive vulnerability factors for anxiety.
Despite the growing body of literature indicating that AS is a highly malleable construct, as well as studies that have examined the associations between AS and various OC spectrum disorders, no research to date has examined the efficacy of an AS intervention on reductions in OC or hoarding symptoms. The purpose of the current study was to examine whether a brief intervention developed to reduce levels of AS would also be effective in reducing symptoms for two OC spectrum conditions. Our first aim was to examine the impact of an AS intervention (Keough and Schmidt, 2012) on OC symptoms at post-treatment, as well as one-week and one-month follow-ups. We furthermore sought to examine whether reduction in AS would be a potential mechanism by which the intervention would exert an influence on OC symptom reduction. Our second aim was to examine these same effects in relation to hoarding symptoms. We hypothesized that the AS intervention would reduce both OC and hoarding symptoms, and that it would do so through reductions in levels of AS.
Method
Participants
The sample consisted of 104 (83.7% female) undergraduate students who were identified as having elevated levels of AS (score of 1.5 SD above the ASI mean). Because AS is considered a transdiagnostic vulnerability for a range of affective disorders (Boswell, Farchione, 2013), this sampling technique ensured that we oversampled for individuals who may be at risk for anxiety and OC spectrum disorders. Sample size was determined prior to initiation of data collection via an a priori power analysis. Ages ranged from 18–28 (M = 18.9, SD =1.42) and 83.7% of participants were female. The racial/ethnic composition of the sample was generally representative of the University population at large: African American (8.7%), Asian American (4.8%), Caucasian (81.7%), and other (4.8%); 11.5% of participants were Hispanic/Latino. Forty-five percent of participants met criteria for at least one psychiatric disorder. See Keough & Schmidt (2012) for more details regarding the sample characteristics, including the CONSORT chart detailing participant flow, assignment, and drop-out.
Self-report measures
Anxiety Sensitivity Index-3 (ASI-3)
The ASI-3 (Taylor et al., 2007) is an 18-item questionnaire that assesses AS. Participants rate each item about the potential negative consequences of anxiety symptoms on a 5-point Likert scale from 0 (very little) to 4 (very much). The ASI-3 has shown excellent internal consistency and good content, convergent and discriminant validity across both nonclinical and clinical samples (Taylor, Zvolensky, 2007). In the current study, the ASI-3 demonstrated strong internal consistency across all assessment points (α’s=.88–.93).
Beck Depression Inventory (BDI)
The BDI (Beck et al., 1988) is a 21-item self-report measure of depressive symptoms. It has demonstrated excellent internal consistency and discriminant validity (Beck, Steer, 1988, Creamer et al., 1995). In the present study, the BDI demonstrated excellent internal consistency across all assessment points (α’s=.92–.95).
Obsessive Compulsive Inventory-Revised (OCIR)
The OCIR includes 18 self-report items that assess common OC symptoms (Foa et al., 2002). Participants rate the extent to which they have been bothered by each symptom on a 5-point Likert scale, from 0 (not at all) to 4 (very much). The OCIR has demonstrated good internal consistency and test-retest reliability (Foa, Huppert, 2002). For purposes of the current study, a modified OCIR total score was calculated by removing the three hoarding items, to reflect non-hoarding OCD symptoms only (OCIR-NH). In the current study, the modified total score exhibited excellent internal consistency across all assessment points (α’s=.92–.94).
Saving Inventory Revised (SIR)
The SIR (Frost et al., 2004) is a 23-item questionnaire that measures hoarding symptoms. Participants rate items on a 5-point scale, with higher scores representing greater hoarding symptom severity. The scale has demonstrated high internal consistency and acceptable convergent validity (Coles, Frost, 2003, Frost, Steketee, 2004). In the current sample, the SIR exhibited excellent internal consistency across all assessment points (α’s=.94–.96).
Penn State Worry Questionnaire (PSWQ)
The PSWQ (Meyer et al., 1990) is a 16-item measure that captures symptoms of generalized worry. Participants rate items on a 5-point scale, with higher scores representing greater generalized anxiety. The PSWQ has excellent internal consistency and discriminant validity (Meyer, Miller, 1990). The PSWQ had excellent internal consistency across all assessment points in the current study (α’s=.93–.94).
Procedure
The current study was part of a broader investigation designed to establish a brief intervention for AS reduction (see Keough and Schmidt, 2012). Participants (N=104) were screened through an introductory psychology participant pool. They were invited to participate if they scored at least 1.5 SD above the general study population mean (i.e., at or above 20) on the Anxiety Sensitivity Index (Reiss, Peterson, 1986). These criteria ensured the inclusion of only those with elevated levels of AS, and are in line with procedures used by Schmidt, Eggleston (2007b). Following eligibility determination, participants were randomly assigned to either an active computer-assisted AS reduction protocol (n=52) or a computer-assisted control condition (n=52) using a random numbers table. Both conditions are described in detail below. All study therapists were doctoral-level students in a clinical psychology program who were trained in the intervention procedures to ensure understanding of and adherence to the protocol. The intervention component of both conditions was completed during a single laboratory session that lasted approximately 50 minutes. Outcome data was collected at post-treatment, one week follow-up, and one month follow-up. Participants received research familiarization credit; all study procedures were in accordance with American Psychological Association standard ethical guidelines and approved by the Institutional Review Board. Data were collected across three semesters from February 2009 to March 2010.
Anxiety sensitivity education and reduction training (ASERT)
The ASERT condition (Keough and Schmidt, 2012) was derived from an intervention originally developed by Schmidt, Eggleston (2007b). Participants first received psychoeducation about the nature of stress and myths about the dangers of anxiety symptoms via a guided 50 minute PowerPoint presentation. Therapists then assessed participant’s fear of various arousal sensations via a series of interoceptive exposures (IE). Participants were exposed to a range of exercises (e.g., straw breathing; chair spinning) that elicit a strong physiological response (e.g., tightness in the chest; dizziness), after which they were asked how distressing each sensation was. Participants were then instructed to continue the top fear-producing IE exercise until distress ratings reached minimal levels. Participants were also provided with monitoring forms to use for daily IE homework for the month following the intervention.
Physical health education training (PHET)
The PHET condition was designed to control for the effects of general education and therapist time (Keough and Schmidt, 2012). Participants were provided with psychoeducation about general health-related topics such as diet, exercise, and sleep using a PowerPoint presentation. Therapists subsequently discussed how to monitor daily health habits, and provided daily monitoring forms for the month following the intervention.
Data analytic plan
All analyses were conducted using the SPSS 20.0 software package. A 2-tailed significance level of .05 was chosen a priori. Listwise deletion was used for all analyses, given that there was very little missing data across measures and time points. Demographic variables and baseline scores between groups were compared using t-tests and chi-square tests. To examine the effects of group on outcome variables (OCIR-NH and SIR) we analyzed between-group differences using repeated measures analysis of variance (ANOVA). We also used analysis of covariance (ANCOVA) to control for baseline depression symptoms. Simple effects analyses were conducted using between-group ANCOVAs (controlling for pretreatment scores), as well as paired-sample t-tests for within-group comparisons between assessments.
Mediation models were first tested using a series of linear regression analyses. Direct effects of the intervention (1=PHET; 2=ASERT) on the mediator variable (post-treatment ASI-3) and outcome variable (post-treatment symptom measures) were examined, controlling for pretreatment levels. Analyses were repeated for one-week and one-month follow-up assessments. Next, the PRODCLIN program was used to calculate indirect effect estimates (MacKinnon et al., 2007). PRODCLIN assesses the product of the unstandardized path coefficients divided by the pooled standard error of the path coefficients (αβ/σαβ). A confidence interval is generated, whereby the inclusion of zero between the upper and lower limits suggests the absence of a statistically significant mediation effect. Product of coefficients methods have been associated with higher power than the more traditional approaches to testing mediation (MacKinnon et al., 2002).
Results
Descriptive Statistics
Of the 104 participants who were randomized, 101 completed the post-treatment assessment, 104 completed the one week follow-up, and 103 completed the one month follow-up (for the CONSORT diagram see Keough and Schmidt, 2012). Comparison of completers and non-completers revealed no significant differences (all p’s > .10) on any demographic or baseline variables. The sample was divided equally between individuals assigned to the ASERT (treatment) condition (n = 52, 50%) and individuals assigned to the PHET (control) condition (n = 52, 50%). Means of study variables and demographic variables by treatment condition at baseline are summarized in Table 1. Participants in the two conditions did not differ from one another on any demographic variables considered, including age, ethnicity, gender, and psychiatric medication usage (all p’s > .10). OCIR-NH and SIR scores were also not associated with differences in any of these demographic variables. Participants in the ASERT condition did not differ from those in the PHET condition for OCIR-NH, ASI-3, and BDI scores; however, the PHET condition did endorse significantly greater SIR scores at pretreatment than the ASERT condition.
Table 1.
Descriptive statistics and correlations for pre-treatment measures across treatment condition.
| 1. | 2. | 3. | 4. | Age | % Female | % Caucasian | |
|---|---|---|---|---|---|---|---|
| 1. ASI-3 | - | - | - | - | |||
| 2. OCIR-NH | .43*** | - | - | - | - | ||
| 3. SIR | .30*** | .46*** | - | - | - | - | |
| 4. BDI | .63*** | .58*** | .47*** | - | - | - | - |
| PHET Mean | 27.96 | 14.44 | 23.48 | 12.00 | 18.73 | 82.7% | 78.8% |
| PHET SD | 12.26 | 11.69 | 15.91 | 9.69 | 1.50 | - | - |
| ASERT Mean | 27.88 | 13.00 | 14.80 | 11.08 | 19.00 | 82.7% | 84.6% |
| ASERT SD | 12.37 | 9.85 | 8.66 | 9.17 | 1.34 | - | - |
| F statistic | < .01 | 0.46 | 11.75*** | 0.25 | 0.92 | - | - |
| Χ2 statistic | .07 | .75 |
p < .01,
p < .001
Note. ASERT = anxiety sensitivity; PHET = physical health education training; OCIR-NH = Obsessive Compulsive Inventory Revised – non-hoarding modified total score; SIR = Saving Inventory Revised; ASI-3 = Anxiety Sensitivity Index-3; BDI = Beck Depression Inventory.
Effects of treatment condition on OC symptoms
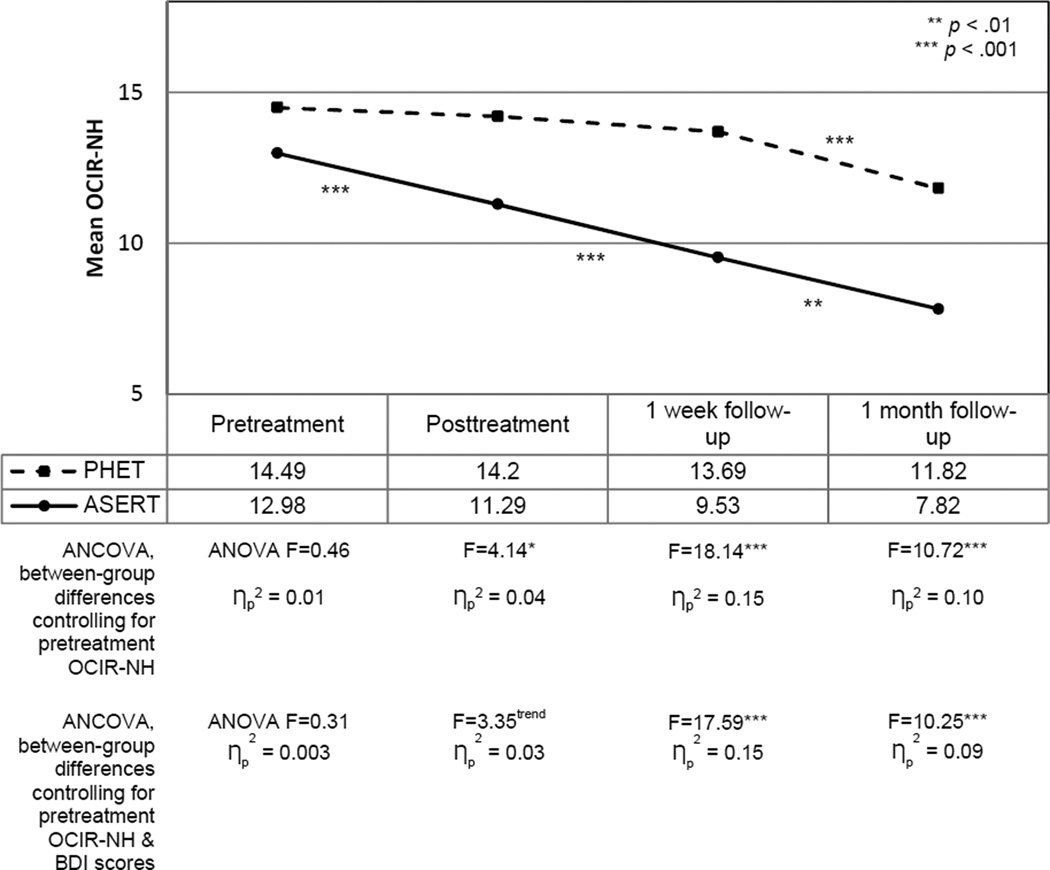
A 2 (condition: ASERT, PHET) × 4 (time: pre-treatment, post-treatment, one week follow-up, one month follow-up) mixed model ANOVA was used to examine changes in OC symptom severity from baseline across the follow-up period. Findings revealed a significant main effect of time F (3, 100) = 29.95, p < .001, as well as a significant time by condition interaction F (3, 100) = 4.55, p < .01. Simple effect analyses were conducted to examine the form of this interaction (see Figure 1). A series of between-group ANCOVAs, controlling for pretreatment OCIR-NH scores, revealed that the ASERT and PHET conditions differed meaningfully from one another at each post-treatment assessment. The size of these effects was in the medium range. Within-group analyses revealed that the PHET condition did not demonstrate a significant change in scores at any point, with one notable exception. Specifically, a paired-samples t-test revealed that OCIR-NH scores were significantly lower at the one month follow-up assessment compared to the one week follow-up assessment (t (1, 50) = 3.78, p < .001). In contrast, the ASERT condition demonstrated significant reductions in OCIR-NH scores between pre- and post-treatment (t (1, 50) = 4.04, p < .001), between post-treatment and one week follow-up (t (1, 50) = 4.68, p < .001), and between one week follow-up and one month follow-up (t (1, 51) = 2.67, p < .01).
Figure 1.
Mean levels of OC symptom severity (OCIR-NH) across assessment time-points, including within- and between-group comparisons.
We next sought to determine whether the time by condition interaction would remain significant if we only considered those participants with elevated OC symptoms. First, individuals who scored above 14 on the OCIR-NH were identified as representing a high OC sample (n=49). The cut-score of 14 was selected because it represents the mean OCIR-NH score in the current sample, and also coincides with the score for the original OCIR that is 1 SD below the clinical mean (Foa, Huppert, 2002). Next, we repeated the 2 (condition: ASERT (n=25), PHET (n=24)) × 4 (time: pre-treatment, post-treatment, one week follow-up, one month follow-up) mixed model ANOVA. A similar pattern of results emerged: there was a significant main effect of time F (3, 49) = 28.45, p < .001, as well as a significant time by condition interaction F (3, 49) = 4.30, p < .01.
A final set of follow-up analyses considered whether controlling for relevant covariates. First we considered depressive symptoms as the primary covariate, which was identified as an important covariate given that OCD is commonly comorbid with depression (LaSalle et al., 2004) and elevated levels of AS have also been linked with depression (Otto et al., 1995). The same pattern of results held with a significant time by condition interaction F (3,100) = 3.67, p < .02. Despite controlling for levels of depression, the ASERT condition was associated with significant reductions in OC symptoms, in contrast to the PHET condition. We also considered generalized anxiety symptoms as an additional covariate, given the relevance of worry to both AS and OC symptoms (Calleo et al., 2010, Floyd et al., 2005, van Rijsoort et al., 2001). Again, the same pattern of results held with a significant time by condition interaction F (3,100) = 3.08, p < .05, controlling for both BDI and PSWQ scores.
Mediation effects of changes in anxiety sensitivity on changes in OC symptoms
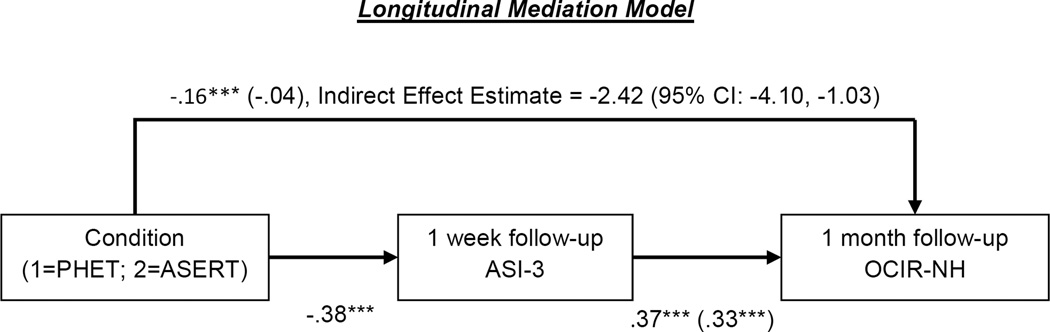
To determine whether changes in AS mediated the effect of treatment condition on reduction of OC symptoms, we conducted a series of hierarchical linear regression analyses. Figure 2 summarizes the model tested. This model used lagged longitudinal data to examine whether changes in AS at 1 week follow-up mediated changes in OC symptoms at 1 month follow-up. Pre-treatment ASI-3 and OCIR-NH scores were included as covariates to allow us to consider change from baseline for AS and OC symptoms, respectively. Results from the full regression analyses conducted with the mediator and outcome variable are summarized in Table 2. A direct effect was found for condition on the mediator variable at 1 week follow-up. For the outcome variable analysis, condition was not significantly associated with one month follow-up OCIR-NH scores, after controlling for baseline levels and the mediator variable (i.e., ASI-3 scores). Examining the indirect effect estimate (see Figure 2), mediation between condition and change in OCIR-NH via change in ASI-3 was supported.
Figure 2.
Mediational model for association between condition (PHET vs ASERT) and OC symptoms (OCIR-NH) as mediated by AS (ASI-3), controlling for pretreatment AS and OC symptoms. Values on paths are path coefficients (standardized βs). Path coefficients in parentheses are standardized partial regression coefficients from equations that include the other variable with a direct effect on the criterion (standardized βs). The indirect effect estimate is derived from the PRODCLIN procedure. *p < .05, **p < .01, ***p < .001
Table 2.
Regression analyses of mediator and outcome variables.
| DV | B | SE | b |
|---|---|---|---|
| 1 week follow-up ASI-3 (mediator) | |||
| Covariate: Pretreatment ASI-3 | 0.82 | 0.06 | 0.75*** |
| Predictor: Condition | −10.02 | 1.43 | −0.38*** |
| 1 month follow-up OCIR-NH (outcome) | |||
| Covariate: Pretreatment OCIR-NH | 0.73 | 0.05 | 0.81*** |
| Covariate: Pretreatment ASI-3 | −0.19 | 0.06 | −0.24** |
| Mediator: 1 week follow-up ASI-3 | 0.24 | 0.06 | 0.33*** |
| Predictor: Condition | −0.74 | 1.08 | −0.04 |
Note. Condition = intervention condition (i.e., 1=PHET, 2=ASERT); OCIR-NH = Obsessive Compulsive Inventory Revised – non-hoarding modified total score; ASI-3 = Anxiety Sensitivity Index-3.
p < .01,
p < .001
We additionally examined an alternative mediation model, in an attempt to consider the specificity of changes in AS contributing to the effect of treatment condition on changes in OC symptoms. Specifically, we tested a model wherein changes in depression were hypothesized to mediate the effect of treatment condition on OC symptoms. This model was not supported; condition did not predict 1 week follow-up BDI scores, controlling for pre-treatment BDI scores.
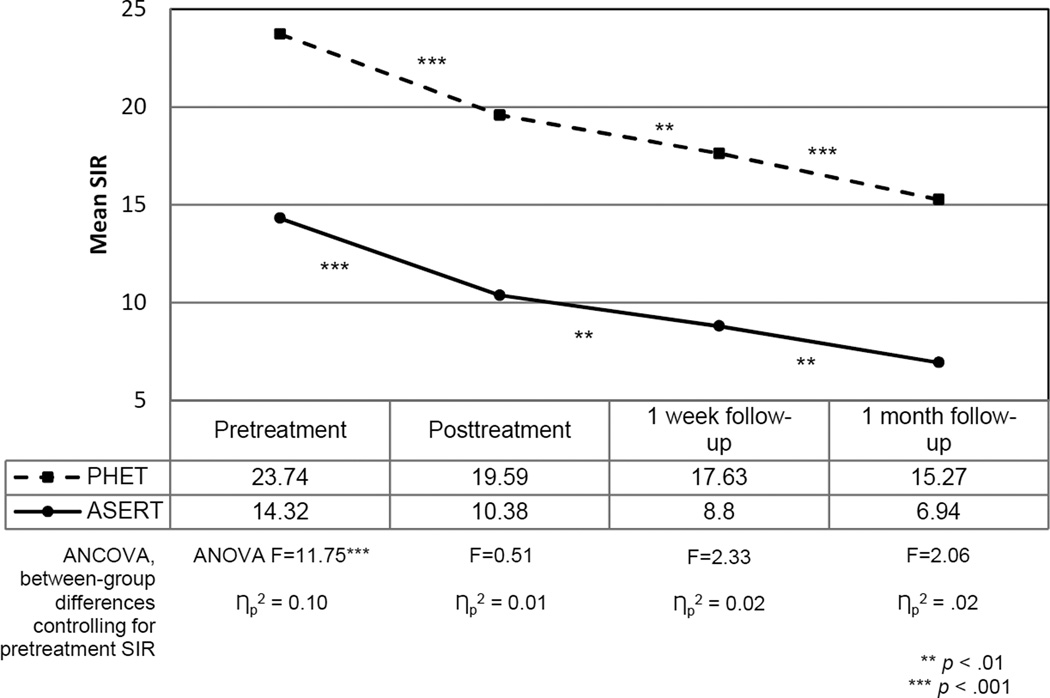
Effects of treatment condition on post-treatment hoarding symptoms
The same pattern of results as noted for OC symptoms did not hold when we examined hoarding symptoms (see Figure 3). A 2 (condition) × 4 (time) mixed model ANOVA revealed a significant effect of time F (3, 99) = 74.39, p < .001; however, there was no significant time by condition interaction F (3, 100) = 0.38, p =.67. Between-group analyses, taking into account baseline differences on the SIR, revealed that the two conditions did not significantly differ from one another at any time point (see Figure 3). Within-group analyses demonstrated that hoarding symptoms across both conditions evidenced significant reductions across the follow-up period. More specifically, both groups demonstrated significant reductions in SIR scores between pre- and post-treatment (ASERT t (1, 50) = 7.44, p < .001; PHET t (1, 50) = 5.86, p < .001), between post-treatment and one week follow-up (ASERT t (1, 50) = 3.28, p < .01; PHET t (1, 50) = 2.66, p < .01), and between one week follow-up and one month follow-up (ASERT t (1, 50) = 3.35, p < .001; PHET t (1, 50) = 4.02, p < .001). Given that condition did not have a significant effect on SIR reductions, we did not examine the AS mediation model for hoarding symptoms.
Figure 3.
Mean levels of hoarding symptom severity (SIR) across assessment time-points, including within- and between-group comparisons.
Discussion
The current investigation represents the first examination of the effectiveness of a brief, AS-focused intervention on reducing symptoms for two OC spectrum conditions. In line with our hypotheses, the ASERT group demonstrated greater reductions in OC symptoms immediately following treatment, and continued to make gains across the follow-up period. In contrast, our hypothesis regarding similar effects of the intervention on the reduction of hoarding symptoms was not supported.
The findings regarding OC symptom reduction are consistent with previous work demonstrating similar effectiveness of single-session AS interventions for decreasing symptoms of anxiety, PTSD, worry, and depression (Mitchell et al., 2014, Norr et al., 2014, Schmidt et al., 2014). Results also support conclusions drawn from clinical case reports that AS may represent a key treatment target that, unless addressed, may interfere with successful completion of exposures for OCD (Pence et al., 2010). Our findings therefore open up the possibility of including a brief, one-session AS intervention into existing treatments for OCD. Such an addition may render cognitive behavioral therapy for OCD more effective by reducing avoidance behaviors and anxious responding during exposures. Given the heterogenous nature of OCD (Mataix-Cols et al., 2005), future research with clinical samples should consider whether reducing levels of AS would have differential impact across the OC symptom dimensions. In the same vein, research should consider whether focusing on different facets of AS (e.g., cognitive concerns; Schmidt, Capron, 2014) would be more or less effective in reducing facets of OCD.
The fact that reducing an anxiety-related cognitive factor would result in reduction of OC symptoms may speak indirectly to the more general relationship between OCD and anxiety. Historically, OCD was classified as an anxiety disorder (Abramowitz and Deacon, 2005) and hierarchical models of emotional distress disorders supported categorizing OCD as a fundamental fear disorder (Lahey et al., 2004, Miller et al., 2008, Slade and Watson, 2006). This changed when the recent DSM-5 (American Psychiatric Association, 2013) removed OCD from the anxiety disorders classification, placing it instead in a separate OCD and Related Disorders spectrum (Stein et al., 2014). Regardless of whether OCD represents a core anxiety disorder or not, our findings provide additional evidence that at least some of the underlying etiological and/or maintaining factors of OCD are closely related to the anxiety and fear network.
The null findings regarding the association between the intervention and reductions in hoarding symptoms were surprising, particularly in light of the growing body of research indicating a strong relationship between hoarding and various facets of emotional tolerance (Medley, Capron, 2013, Shaw et al., 2015, Timpano, Buckner, 2009, Timpano et al., 2014). Emotional tolerance is a term used to describe a higher order factor that captures AS, distress tolerance, tolerance of uncertainty, and frustration tolerance (Leyro et al., 2010). One explanation for our findings may be that the ASERT intervention, which was focused on interoceptive exposure for physical symptoms of anxiety, did not adequately capture the facet of emotional tolerance that acts as a causal risk factor for hoarding. Research examining the association between hoarding and the emotional tolerance sub-factors has been constrained by cross-sectional designs, which do not allow for the differentiation between correlates, risk factors, and causally-relevant risk factors that may be modified (Kraemer et al., 2001).
An additional, interesting consideration is that both the active and control conditions demonstrated significant decreases in hoarding symptoms across the assessment time points. It is certainly possible that this reduction is simply reflecting regression to the mean. However, a second potential explanation is that the PHET condition may have included elements that captured an active intervention pertinent to hoarding. It may be that the nature of the educational material included in the PHET group presentation was as relevant for hoarding symptoms, as the ASERT condition materials (i.e., interoceptive exposure and related homework). Individuals in the PHET group were provided with health-relevant psychoeducation focused on diet, alcohol consumption, exercise, and sleep. Therapists also discussed monitoring daily health habits, and participants were encouraged at post-treatment to complete daily habit monitoring forms (Keough and Schmidt, 2012). A separate line of research has found that hoarding is associated with low self-control (Timpano and Schmidt, 2013), a general risk factor that captures one’s inability to resist urges and follow through with behavioral goals. Preliminary work has attempted to modulate this risk factor using an intervention that aims to increase levels of self-control in hoarding patients by having them monitor daily health behaviors (Timpano and Schmidt, 2010), very similar in nature to what was described in the PHET condition.
Results of the current study should be interpreted in light of several limitations. First and foremost, participants were selected based on elevated AS levels, not diagnostic status (Keough and Schmidt, 2012). Although 45% of the participants met criteria for a current Axis-I diagnosis, only three individuals were diagnosed with full OCD1. Conclusions regarding the possible effectiveness of the intervention for OCD, as well as conclusions regarding the non-effectiveness of the intervention for hoarding, should therefore remain provisional until results have been replicated with clinical samples. Both OC and hoarding symptoms have been found to be dimensional constructs (Olatunji et al., 2008, Timpano et al., 2013), and as a result, findings from non-clinical studies often replicate with clinical samples. Nevertheless, further research will be necessary with clearly characterized OCD and Hoarding Disorder populations. A related note is that our sample was also fairly homogenous, and included a small age range, as well as higher proportions of females and Caucasians. Findings may therefore not be generalizable to the population as a whole. A third limitation is that we only relied on self-report measures. Using a multi-modal assessment battery, including behavioral avoidance tests (e.g., Najmi et al., 2012) or behavioral discarding tasks (e.g., Preston et al., 2009, Timpano and Schmidt, 2013), would represent an interesting extension of the current study, and would likely provide a more complete understanding of the overall impact an AS intervention. The follow-up assessment period was relatively short, only extending one month past the intervention. A fourth limitation is the large difference in baseline hoarding symptoms between the two intervention groups. Although we controlled for SIR scores in our analyses and there was a significant time effect in both conditions, these group differences nevertheless may have contributed to our findings. Finally, the current research only focused on hoarding and OC symptoms; subsequent studies should consider the relationship between AS and other types of OC spectrum conditions, including body dysmorphic disorder, chronic tic disorders, and trichotillomania. Both OCD and Hoarding Disorder have been recognized as extremely severe and disabling syndromes that represent key public health burdens (Lopez and Murray, 1998, Tolin et al., 2008). Unfortunately, and despite the availability of empirically supported treatments, both conditions also represent challenging treatment targets (Jenike, 2004, Tolin et al., 2015). There continues to be a need to identify new avenues through which to develop additional interventions and/or improve existing clinical approaches. The current findings therefore provide important clinical implications for the amelioration of these OC spectrum conditions. Future research is warranted that will investigate the effectiveness of an AS-focused intervention with respect to the prevention of OC spectrum symptoms, as well as an adjunctive intervention that could be combined with existing cognitive behavioral treatments.
Acknowledgments
Role of Funding Source.
This investigation was supported in part by a National Institutes of Mental Health Award (1F31 MH086174-01, PI: M. Keough)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
At the time that this study was conducted, the Hoarding Disorder module had not yet been incorporated into the Structured Clinical Interview for DSM-IV. We therefore do not have estimates of the number of individuals who may have met for Hoarding Disorder.
Contributors.
Authors Keough, Timpano, and Schmidt designed the study, while authors Keough and Raines executed data collection. Authors Timpano, Raines, and Shaw wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
we have no potential conflicts of interests to report.
References
- Abramowitz JS, Deacon BJ. Obsessive-compulsive disorder: essential phenomenology and overlap with other anxiety disorders. Concepts and controversies in obsessive-compulsive disorder: Springer. 2005:119–149. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Anestis MD, Holm-Denoma J, Gordon KH, Schmidt NB, Joiner TE. The Role of Anxiety Sensitivity in Eating Pathology. Cognitive Therapy and Research. 2008;32:370–385. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Boswell JF, Farchione TJ, Sauer-Zavala S, Murray HW, Fortune MR, Barlow DH. Anxiety Sensitivity and Interoceptive Exposure: A Transdiagnostic Construct and Change Strategy. Behavior Therapy. 2013;44:417–431. doi: 10.1016/j.beth.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calleo JS, Hart J, Björgvinsson T, Stanley MA. Obsessions and worry beliefs in an inpatient OCD population. Journal of Anxiety Disorders. 2010;24:903–908. doi: 10.1016/j.janxdis.2010.06.015. [DOI] [PubMed] [Google Scholar]
- Capron DW, Fitch KE, Medley A, Blagg C, Mallott M, Joiner TE. Role of anxiety sensitivity subfactors in suicidal ideation and suicide attempt history. Depression and Anxiety. 2012;29:195–201. doi: 10.1002/da.20871. [DOI] [PubMed] [Google Scholar]
- Coles ME, Frost RO, Heimberg RG, Steketee G. Hoarding behaviors in a large college sample. Behaviour Research and Therapy. 2003;41:179–194. doi: 10.1016/s0005-7967(01)00136-x. [DOI] [PubMed] [Google Scholar]
- Creamer M, Foran J, Bell R. The Beck Anxiety Inventory in a non-clinical sample. Behaviour Research and Therapy. 1995;33:477–485. doi: 10.1016/0005-7967(94)00082-u. [DOI] [PubMed] [Google Scholar]
- Deacon B, Abramowitz J. Anxiety sensitivity and its dimensions across the anxiety disorders. Journal of Anxiety Disorders. 2006;20:837–857. doi: 10.1016/j.janxdis.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky MJ, Babson K, Leen-Feldner EW, Schmidt NB. An integrated approach to panic prevention targeting the empirically supported risk factors of smoking and anxiety sensitivity: Theoretical basis and evidence from a pilot project evaluating feasibility and short-term efficacy. Journal of Anxiety Disorders. 2008;22:1227–1243. doi: 10.1016/j.janxdis.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd M, Garfield A, LaSota MT. Anxiety sensitivity and worry. Personality and Individual Differences. 2005;38:1223–1229. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychological Assessment. 2002;14:485–496. [PubMed] [Google Scholar]
- Frost RO, Steketee G, Grisham JR. Measurement of compulsive hoarding: Saving Inventory-Revised. Behaviour Research and Therapy. 2004;42:1163–1182. doi: 10.1016/j.brat.2003.07.006. [DOI] [PubMed] [Google Scholar]
- Gardenswartz CA, Craske MG. Prevention of panic disorder. Behavior Therapy. 2001;32:725–737. [Google Scholar]
- Jenike MA. Obsessive–compulsive disorder. New England Journal of Medicine. 2004;350:259–265. doi: 10.1056/NEJMcp031002. [DOI] [PubMed] [Google Scholar]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, Schmidt NB. Anxiety symptomatology: The association with distress tolerance and anxiety sensitivity. Behavior Therapy. 2010;41:567–574. doi: 10.1016/j.beth.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keough ME, Schmidt NB. Refinement of a brief anxiety sensitivity reduction intervention. Journal of Consulting And Clinical Psychology. 2012;80:766–772. doi: 10.1037/a0027961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- LaSalle VH, Cromer KR, Nelson KN, Kazuba D, Justement L, Murphy DL. Diagnostic interview assessed neuropsychiatric disorder comorbidity in 334 individuals with obsessive-compulsive disorder. Depression and Anxiety. 2004;19:163–173. doi: 10.1002/da.20009. [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010;136:576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez AD, Murray CC. The global burden of disease, 1990–2020. Nature Medicine. 1998;4:1241–1243. doi: 10.1038/3218. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams JB, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODLIN. Behavior Research Methods. 2007;39:384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mataix-Cols D, Frost RO, Pertusa A, Clark LA, Saxena S, Leckman JF, et al. Hoarding disorder: a new diagnosis for DSM-V? Depression and Anxiety. 2010;27:556–572. doi: 10.1002/da.20693. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Rosario-Campos MC, Leckman JF. A multidimensional model of obsessive-compulsive disorder. American Journal of Psychiatry. 2005;162:228–238. doi: 10.1176/appi.ajp.162.2.228. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Medley A, Capron DW, Korte KJ, Schmidt NB. Anxiety Sensitivity: A Potential Vulnerability Factor For Compulisve Hoarding. Cognitive Behaviour Therapy. 2013;42:45–55. doi: 10.1080/16506073.2012.738242. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State worry questionnaire. Behaviour research and therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Miller MW, Fogler JM, Wolf EJ, Kaloupek DG, Keane TM. The internalizing and externalizing structure of psychiatric comorbidity in combat veterans. Journal of traumatic stress. 2008;21:58–65. doi: 10.1002/jts.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell MA, Capron DW, Raines AM, Schmidt NB. Reduction of cognitive concerns of anxiety sensitivity is uniquely associated with reduction of PTSD and depressive symptoms: a comparison of civilians and veterans. Journal of psychiatric research. 2014;48:25–31. doi: 10.1016/j.jpsychires.2013.10.013. [DOI] [PubMed] [Google Scholar]
- Najmi S, Tobin AC, Amir N. Psychometric properties of a behavioral test of contamination-related obsessive–compulsive symptoms. Cognitive Therapy And Research. 2012;36:228–233. [Google Scholar]
- Norr AM, Allan NP, Macatee RJ, Keough ME, Schmidt NB. The effects of an anxiety sensitivity intervention on anxiety, depression, and worry: Mediation through affect tolerances. Behaviour Research and Therapy. 2014;59:12–19. doi: 10.1016/j.brat.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Williams BJ, Haslam N, Abramowitz JS, Tolin DF. The latent structure of obsessive-compulsive symptoms: A taxometric study. Depression and Anxiety. 2008;25:956–968. doi: 10.1002/da.20387. [DOI] [PubMed] [Google Scholar]
- Otto MW, Pollack MH, Fava M, Uccello R, Rosenbaum JF. Elevated anxieyt sensitivity index scores in patients with major depression: Correlates and changes with antidepressant treatment. Journal of Anxiety Disorders. 1995;9:117–123. [Google Scholar]
- Pence SL, Jr, Sulkowski ML, Jordan C, Storch EA. When exposures go wrong: troubleshooting guidelines for managing difficult scenarios that arise in exposure-based treatment for obsessive-compulsive disorder. American journal of psychotherapy. 2010;64:39–53. doi: 10.1176/appi.psychotherapy.2010.64.1.39. [DOI] [PubMed] [Google Scholar]
- Preston SD, Muroff JR, Wengrovitz SM. Investigating the mechanisms of hoarding from an experimental perspective. Depression and Anxiety. 2009;26:425–437. doi: 10.1002/da.20417. [DOI] [PubMed] [Google Scholar]
- Raines AM, Oglesby ME, Capron DW, Schmidt NB. Obsessive compulsive disorder and anxiety sensitivity: Identification of specific relations among symptom dimensions. Journal of Obsessive-Compulsive and Related Disorders. 2014;3:71–76. [Google Scholar]
- Reiss S. Expectancy Model of Fear, Anxiety and Panic. Clinical Psychology Review. 1991;11:141–153. [Google Scholar]
- Reiss S, McNally R. Expectancy Model of Fear. In: Reiss S, Bootzin R, editors. Theoretical issues in behavior therapy. San Diego, CA: Academic Press; 1985. [Google Scholar]
- Reiss S, Peterson R, Gursky D, McNally R. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Robinson LJ, Freeston MH. Emotion and internal experience in obsessive compulsive disorder: reviewing the role of alexithymia, anxiety sensitivity and distress tolerance. Clinical Psychology Review. 2014;34:256–271. doi: 10.1016/j.cpr.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Rodriguez BF, Bruce SE, Pagano ME, Spencer MA, Keller MB. Factor structure and stability of the Anxiety Sensitivity Index in a longitudinal study of anxiety disorder patients. Behaviour Research and Therapy. 2004;42:79–91. doi: 10.1016/s0005-7967(03)00074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Buckner JD, Keough ME. Anxiety sensitivity as a prospective predictor of alcohol use disorders. Behavior Modification. 2007a;31:202–219. doi: 10.1177/0145445506297019. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, Allan NP. Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. Journal of Consulting and Clinical Psychology. 2014;82:1023–1033. doi: 10.1037/a0036651. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey JA. Anxiety sensitivity amelioration training (ASAT): A longitudinal primary prevention program targeting cognitive vulnerability. Journal of Anxiety Disorders. 2007b;21:302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Woolaway-Bickel K, Trakowski J, Santiago HT, Storey J, Koselka M, et al. Dismantling cognitive–behavioral treatment for panic disorder: Questioning the utility of breathing retraining. Journal of Consulting and Clinical Psychology. 2000;68:417. doi: 10.1037//0022-006x.68.3.417. [DOI] [PubMed] [Google Scholar]
- Shaw AM, Llabre MM, Timpano KR. Affect Intolerance and Hoarding Symptoms: A Structural Equation Modeling Approach. International Journal of Cognitive Therapy. 2015 in press. [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Stein DJ, Craske MA, Friedman MJ, Phillips KA. Anxiety disorders, obsessive-compulsive and related disorders, trauma- and stressor-related disorders, and dissociative disorders in DSM-5. American Journal of Psychiatry. 2014;171:611–613. doi: 10.1176/appi.ajp.2014.14010003. [DOI] [PubMed] [Google Scholar]
- Taylor S. Anxiety Sensitivity: Theory, Research, and Treatment of the Fear of Anxiety. Mahwah, New Jersey: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- Taylor S, Koch WJ, McNally RJ. How does anxiety sensitivity vary across the anxiety disorders? Journal of Anxiety Disorders. 1992;6:249–259. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: Development and initial validation of the anxiety sensitivity index-3. Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Timpano KR, Broman-Fulks JJ, Glaesmer H, Exner C, Rief W, Olatunji BO, et al. A taxometric exploration of the latent structure of hoarding. Psychological Assessment. 2013;25:194–203. doi: 10.1037/a0029966. [DOI] [PubMed] [Google Scholar]
- Timpano KR, Buckner JD, Richey JA, Murphy DL, Schmidt NB. Exploration of Anxiety Sensitivity and Distress Tolerance as Vulnerability Factors for Hoarding Behaviors. Depression and Anxiety. 2009;26:343–353. doi: 10.1002/da.20469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timpano KR, Schmidt NB. The Association Between Self-Control and Hoarding: A Case Report. Cogn Behav Pract. 2010;17:439–448. [Google Scholar]
- Timpano KR, Schmidt NB. The relationship between self-control deficits and hoarding: a multimethod investigation across three samples. Journal of Abnormal Psychology. 2013;122:13–25. doi: 10.1037/a0029760. [DOI] [PubMed] [Google Scholar]
- Timpano KR, Shaw AM, Cougle JR, Fitch KE. A multifaceted assessment of emotional tolerance and intensity in hoarding. Behavior Therapy. 2014;45:690–699. doi: 10.1016/j.beth.2014.04.002. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, Gray KD, Fitch KE. The economic and social burden of compulsive hoarding. Psychiatry Research. 2008;160:200–211. doi: 10.1016/j.psychres.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, Muroff JR. Cognitive Behavioral Therapy for Hoarding Disorder: A Meta-Analysis. Depression and Anxiety. 2015 doi: 10.1002/da.22327. [DOI] [PubMed] [Google Scholar]
- van Rijsoort S, Emmelkamp P, Vervaeke G. Assessment of worry and OCD: how are they related? Personality and Individual Differences. 2001;31:247–258. [Google Scholar]
- Westling BE, Öst L-G. Brief cognitive behaviour therapy of panic disorder. Scandinavian Journal of Behaviour Therapy. 1999;28:49–57. [Google Scholar]
- Zinbarg RE, Barlow DH, Brown TA. Hierarchical structure and general factor saturation of the anxiety sensitivity index: Evidence and implications. Psychological Assessment. 1997;9:277–284. [Google Scholar]