Abstract
We reported that in a 29-year-old male patient with hyperthyroidism, bilateral breast swelling appeared in three days after starting methimazole and gradually aggravated. Several days later, a small amount of transparent liquid could be squeezed out from bilateral mammary glands. Breast ultrasound confirmed gynaecomastia. The level of testosterone, estradiol and luteinizing hormone increased. After the patient continued taking methimazole for a while, gynaecomastia relieved. Testosterone, luteinizing hormone and thyroid functions restored to normal. The possible mechanisms included increased levels of serum total cholesterol and relatively decreased T3 after initiating methimazole.
Keywords: hyperthyroidism, gynaecomastia, methimazole, testosterone
INTRODUCTION
Gynaecomastia is benign hyperplasia of breast tissue in men, characterized by enlargement of one or two breasts and palpable solid tenderness masses under the areola. Most patients with gynaecomastia have no obvious syndromes, but it has a great effect on the psychology of the patients (1). The pathological basis of gynaecomastia is the imbalance of estrogen/androgen levels. Thyroid hormones can enhance the estrogen/androgen ratio (2). An association between gynaecomastia and thyroid dysfunction has been well-documented, especially in hyperthyroidism (1). Gynaecomastia is one of the clinical manifestations of hyperthyroidism, with a prevalence of 2-40%. When thyroid function returned to a euthyroid state, gynaecomastia was relieved (3). It was reported that gynaecomastia also happened in the course of treating hyperthyroidism, about 50 to 103 days after antithyroid drugs (4). Our paper reported a case that gynaecomastia appeared three days after the initial treatment of methimazole in a patient with hyperthyroidism.
CASE REPORT
A 29-year-old man was presented to a local hospital on October 9th, 2019 because of paroxysmal panic, tremor, and weight loss for 3 months. He didn’t complain of any breast discomfort. His laboratory investigations revealed that thyroid Stimulating Hormone (TSH) was 0.0003uIU/mL, total triiodothyronine (TT3) 6.19nmol/L, total tetraiodothyronine (TT4) 190.4nmol/L, free triiodothyronine (FT3) 22.71pmol/L and free tetraiodothyronine (FT4) 22.68pmol/L (Table 1). White blood cell count, alanine transaminase, and aspartate aminotransferase were normal. Thyroid ultrasound showed diffuse enlargement and thickening of bilateral thyroid with uneven parenchymal echoes and rich blood flow signal. He was diagnosed with hyperthyroidism and 10mg of methimazole (Merck Serono) and 10mg of propranolol were prescribed 3 times daily.
Table 1.
The change of thyroid hormones and sex hormones
| Thyroidfunction | Sex hormones | Breast ultrasound(cm) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TT3 (nmol/L) |
TT4 (nmol/L) |
FT3 (pmol/L) |
FT4 (pmol/L) |
TSH (mIU/L) | FSH (U/L) | LH (1.2-8.6 IU/L) |
P(ng/mL) | T (6.07-27.1 nmol/L) |
E2(0.07-0.17 nmol/L) |
PRL (56.0-278.3 mIU/L) |
Left | Right | |
| 2019- 10-09 |
6.19 (0.89-2.44) |
190.4 (62.68-150.83) |
22.71 ⬆ (2.63-5.7) |
22.68 ⬆ (9.00-19.05) |
0.0003 ⬇ (0.35-5) |
||||||||
| 2019- 11-14 |
4.65 ⬆ (1.01-2.95) |
203.2 ⬆ (55.34-160.88) |
10.92 ⬆ (2.76-6.3) |
24.92 ⬆ (10.42- 24.32) |
0 ⬇ (0.55- 4.78) |
4.39 | 11.33 ⬆ | 0.84 | 37.29 ⬆ | 0.39 ⬆ | 227.96 | 1.0 | 1.6 |
| 2020- 01-09 |
1.78 | 50.6 | 4.05 | 10.63 | 5.7 ⬆ | 4.68 | 17.81 | 0.23 ⬆ | 0.7 | 0.8 | |||
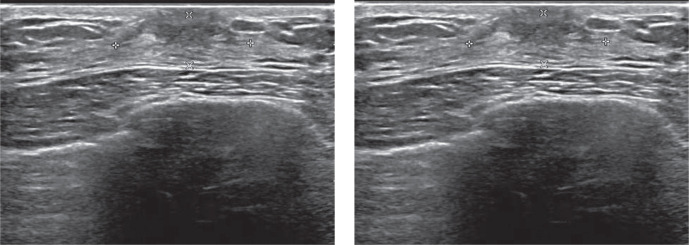
Three days after starting treatment, bilateral breast swelling appeared and gradually aggravated, followed by nipple tenderness. Later, a small amount of transparent liquid could be squeezed out from bilateral mammary glands. Sexual function and libido did not change. On November 13th, he was admitted to a local hospital. Breast ultrasound examination showed that there were echoes of mammary tissue around bilateral papillae, and the glandular layer was thickened, with 1.0cm on the left and 1.6cm on the right (Fig. 1), respectively. The ductus of bilateral mammary glands were dilated and structurally disordered. The patient denied any other drugs or diseases.
Figure 1.
Ultrasound images of right breast on November 13th , 2019.
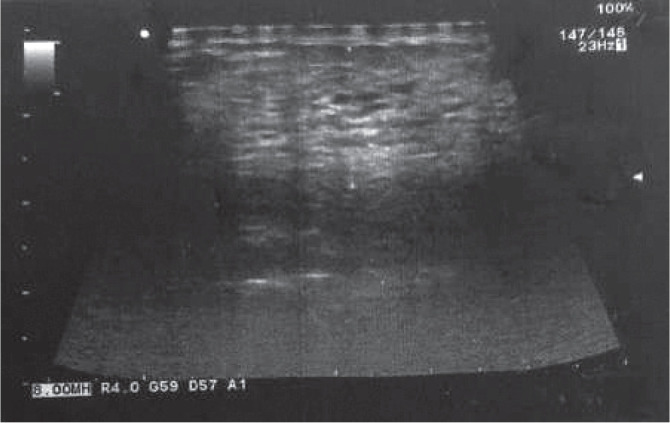
On November 14th, he came to our hospital and laboratory investigations showed that TSH 0.003 mIU/L, FT3 10.92pmol/L, FT4 24.92pmol/L, TT3 4.65nmol/L, TT4 203.2nmol/L, TSH receptor antibody 8.79IU/L, Follicle-stimulating hormone (FSH) 4.39IU/L, prolactin (PRL) 227.96mIU/L, testosterone (T) 37.29nmol/L, estradiol (E2) 0.39nmol/L, and luteinizing hormone (LH) 11.33IU/L. (Table 1) Bilateral breast swelling and tenderness were relieved significantly about 4 days after continuing methimazole. On January 9th, 2020, when he came back to our hospital, there was no discomfort in bilateral breasts, and transparent liquid could not be extruded. FT3, FT4, TT3, TT4, Testosterone, and LH were normal, E2 17.81nmol/L and TSH 5.7mIU/L. Breast ultrasound showed that the thickness of the left gland was 0.7cm, and the right 0.8cm (Fig. 2), much better than on November 13th, 2019.
Figure 2.
Ultrasound images of left and right breasts on January 9th 2020.
DISCUSSION
In our case, hyperthyroidism was diagnosed and methimazole (10mg 3/d) was started. After 3 days of treatment, both his breasts became swollen, progressively worsened, and tenderness appeared. LH, T, and E2 increased obviously and PRL was normal. After he continued taking methimazole for a while, sex hormones significantly decreased and gynaecomastia was gradually relieved.
According to previous reports, gynaecomastia can occur in male thyrotoxic patients and resolve after returning to a euthyroid state. Its mechanism is not fully understood. It was supposed to be related to the increase of sex hormone- binding globulin and increased conversion of T to E2, which may increase the ratio of free estradiol/testosterone in the blood (2).
In our case, gynaecomastia did not appear before antithyroid treatment, suggesting that gynaecomastia was not caused by thyrotoxicosis. After the initial treatment of methimazole, he developed gynaecomastia. This was not an adverse drug reaction of methimazole or propranolol, because gynaecomastia was relieved as the patient continued taking the same dose of methimazole and propranolol. The patient denied a history of other diseases. Therefore, we speculated that gynaecomastia was related to the initiation of anti-thyroid treatment.
In 1951, Bauer FK and Goodwin WE first reported that three patients exhibited bilateral breast tenderness and swelling 14 to 23 days after receiving a therapeutic dose of 131I, and they resolved spontaneously after 2 to 4 weeks. It was speculated that the change in thyroid function brought by 131I therapy resulted in enhanced stimulation of the adrenal cortex by the pituitary gland. Gynaecomastia occurred in the case of adrenal cortical hyperfunction (5) Berson and Schreiber reported that two patients with hyperthyroidism had slight pain and swelling in the breast around 50 and 103 days after methimazole treatment, respectively. The symptoms were relieved as thyroid function was recovered (4). The authors did not analyze possible mechanisms. In the above papers, sex hormones were not measured when gynaecomastia appeared. It was also reported in 2018 that a thyrotoxic patient developed gynaecomastia after euthyroidism restoration and sex hormones were normal, but free T and free E2 were not measured. It was speculated that both thyroid function and autoantibodies might play a role in gynaecomastia (6).
However, in this case, breast swelling progressively developed after 3 days of methimazole treatment, and a small amount of transparent liquid could be squeezed. T, LH, and E2 were significantly higher than normal. Breast ultrasound confirmed breast development. The possible mechanisms were as follows: 1) the levels of serum total cholesterol, LDL cholesterol, and phospholipid were decreased in hyperthyroidism, and the levels of serum lipids were significantly and transiently increased after antithyroid therapy (7). Cholesterol is the raw material to synthesize sex hormones. The increase in the raw material and dyslipidemia would cause an increase in T and E2. Unfortunately, we did not track dynamic changes in total cholesterol. 2) It was reported that male rats had elevated serum LH levels during hypothyroidism and decreased serum LH levels during thyrotoxicosis, suggesting that T3 can act on gonadotropin cells and has a direct effect on the synthesis and secretion of LH and FSH (8). In our case, during the initial treatment of hyperthyroidism, the decrease in T3 caused a transient disorder similar to hypothyroidism, which lead to an increase in LH secretion, in turn secreting more T.
Due to the physical defects, male patients with gynecomastia faced greater psychological pressure and a heavier mental burden, often accompanied by anxiety and depression. But according to previous reports and our case, gynaecomastia during hyperthyroidism treatment can gradually improve with returning to normal thyroid function even without any special treatment. Thus, doctors should explain the condition in detail to patients, soothe the patients’ tension, and alleviate the patients’ anxiety.
In conclusion, this case reminded us that gynaecomastia can occur at the initial stage of methimazole treatment and recover without special treatment. It is speculated that it may be related to the rise in serum total cholesterol and LDL-cholesterol levels and the effect of T3 on LH.
Conflict of interest
The authors declare that they have no conflict of interest.
Author Contributions
All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
References
- 1.Sansone A, Romanelli F, Sansone M, Lenzi A, Di Luigi L. Gynecomastia and hormones. Endocrine. 2017;55:37–44. doi: 10.1007/s12020-016-0975-9. [DOI] [PubMed] [Google Scholar]
- 2.Ismail AAA, Barth JH. Endocrinology of gynaecomastia. Ann Clin Biochem. 2001;38:596–607. doi: 10.1258/0004563011900993. [DOI] [PubMed] [Google Scholar]
- 3.Sanyal T, Dutta D, Shivprasad K, Ghosh S, Mukhopadhyay S, Chowdhury S. Gynaecomastia as the initial presentation of thyrotoxicosis. Indian J Endocrinol Metab. 2012;16:S352–S353. doi: 10.4103/2230-8210.104089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berson SA, Schreiber SS. Gynaecomastia and hyperthyroidism. J Clin Endocrinol Metab. 1953;13(9):1126–1128. doi: 10.1210/jcem-13-9-1126. [DOI] [PubMed] [Google Scholar]
- 5.Bauer FK,Goodwin WE. Acne and Gynaecomastia following I131 therapy for hyperthyroidism. J Clin Endocrinol Metab. 1951;11(12):1574–1576. doi: 10.1210/jcem-11-12-1574. [DOI] [PubMed] [Google Scholar]
- 6.Calcaterra V, Clerici E, Ceolin V, Regalbuto C, Larizza D. Gynecomastia after euthyroidism restoration in a patient with type 1 diabetes and Graves’ disease. Clin Case Rep. 2018;6(8):1481–1484. doi: 10.1002/ccr3.1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nishitani H, Okamura K, Noguchi S, Inoue K, Morotomi Y, Fujishima M. Serum lipid levels in thyroid dysfunction with special reference to transient elevation during treatment in hyperthyroid Grave’s disease. Horm Metab Res. 1990;22(9):490–493. doi: 10.1055/s-2007-1004953. [DOI] [PubMed] [Google Scholar]
- 8.Romano RM, Bargi-Souza P, Brunetto EL, Goulart-Silva F, Salgado RM, Zorn TMT, Nunes MT. Triiodothyronine differentially modulates the LH and FSH synthesis and secretion in male rats. Endocrine. 2018;59(1):191–202. doi: 10.1007/s12020-017-1487-y. [DOI] [PubMed] [Google Scholar]