Abstract
We demonstrate the power of a data-informed medicines-based approach in discovering the indirect effect of the COVID-19 pandemic on cardiovascular events using 1.32 billion records of dispensed medications in England, Scotland and Wales. We estimate that interruption of preventive care could result in more than 13,000 extra cardiovascular events.
Subject terms: Epidemiology, Preventive medicine
The project
Cardiovascular disease (CVD) is the leading cause of mortality worldwide. Strategies to prevent CVD are therefore of critical importance and, in the UK, they currently include screening for drug-modifiable risk factors, such as type 2 diabetes, hypertension and high lipids.
The COVID-19 pandemic disrupted healthcare systems via multiple mechanisms, although how the pandemic affected the screening and treatment of common risk factors for CVD remains under-studied at a national level1,2. Moreover, the downstream impact of missed detection or treatment of risk factors for CVD outcomes, such as myocardial infarction and stroke, is poorly understood. We investigated changes in prescribed and dispensed medicines that are used to treat CVD risk factors over the course of the COVID-19 pandemic, and assessed the impact of not treating these risk factors on future CVD events.
The discovery
The UK’s comprehensive national medical records track health over the life course for >60 million people in England, Scotland and Wales3–5. Using these records, we investigated the impact of the COVID-19 pandemic on mediation usage. Specifically, eleven sub-groups of people were analysed, defined by their use of medicines used to treat CVD and its risk factors, such as high blood pressure, high cholesterol and diabetes. Medication records were matched via non-identifying unique pseudo-identifiers to individual-level socio-demographic characteristics. We analysed trends in first (incident) medication use across 1.32 billion records of community-dispensed CVD medications from England, Scotland and Wales between April 2018 and July 2021. By highlighting monthly trends in incident medication use, we aimed to understand the changes in the number of new starters on drugs that are used to control CVD risk factors of diabetes, hypertension and high lipids.
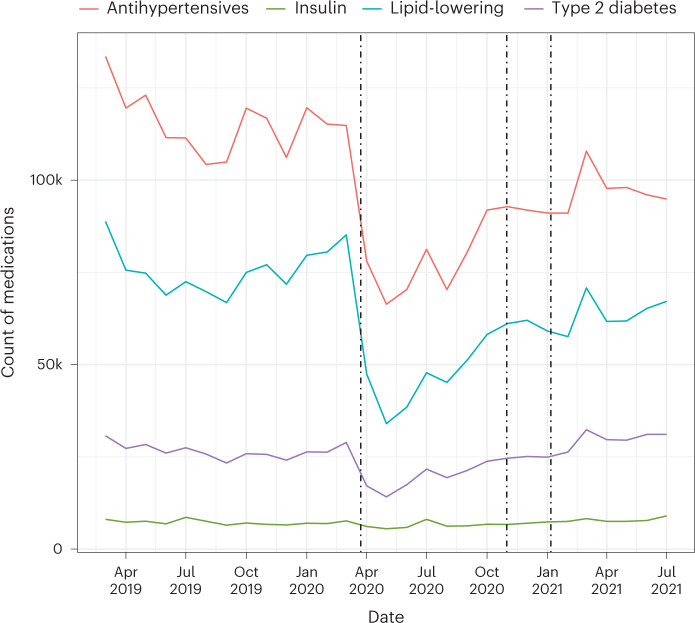
There was a marked decline in the number of CVD preventive medicines dispensed at the start of the COVID-19 pandemic. Specifically, 491,306 fewer individuals initiated antihypertensive treatment than expected based on 2019 levels (Fig. 1). Further analysis revealed that this reduction could result in 13,662 additional CVD events, including 2,281 myocardial infarctions and 3,474 strokes, should individuals remain untreated over their life-course. Incident use of lipid-lowering medicines also decreased by 16,744 patients per month compared with 2019. By contrast, incident use of medicines to treat type 2 diabetes increased by approximately 623 patients per month, although the dispensing of insulin medication remained steady.
Fig. 1. Trends in the count of incident medications dispensed for England, Scotland and Wales.
Counts by month for incident medications dispensed for four different subgroups of CVD medication are shown. Vertical dotted lines indicate the timing of the first, second and third national lockdowns on 26 March 2020, 5 November 2020 and 6 January 2021, respectively. © 2022, Dale, C. E. et al.
The implications
Our analysis suggests that the number of first initiation of medicines to prevent CVD greatly declined during the COVID-19 pandemic and has not returned to pre-pandemic levels. This is despite recovery in the dispensing of medications after the initial declines following the first UK lockdown. Our results highlight the urgent need for methods to identify and treat individuals who have missed treatment and remain untreated. Without this, large numbers of excess future CVD events will add to the indirect impacts of the pandemic. We believe our work has relevance for many countries, given that some of the medicines investigated in our analysis are inexpensive and the mainstay of atherosclerotic CVD prevention worldwide.
Our work is not without limitations. Importantly, we analysed ‘real world’ medication data that were not collected for research purposes. It is possible that artefacts may exist within the data owing to differences in data collection, processing or transfer, and these may vary over time and by source. Estimates of the impact of a reduction in medicine use on CVD events rely on assumptions that may change over time and in direct response to the pandemic. The final impact of the pandemic on CVD events in the UK is highly dynamic and will be influenced by many factors that could not be captured by our model.
We have shown that using medicines as a proxy for disease can complement investigations using electronic health records and disease diagnostic codes. Such analyses can be incorporated into methods to identify individuals who have missed treatment, which is urgently required to avoid additional future CVD events. This medicines approach provides policy makers with an additional lens to monitor healthcare pathways, providing a rapid response tool in the event of a future pandemic or other similar disruption event.
Caroline Dale, Rohan Takhar & Reecha Sofat
University of Liverpool, Liverpool, UK.
Expert opinion
“Overall, this is a comprehensive and fascinating study of practice changes during the pandemic.” Amanda K Verma, Washington University School of Medicine, St. Louis, Missouri
Behind the paper
The idea behind this research sprang from trying to understand the way disasters impact the delivery of regular clinical care for chronic disease. Often the way a clinical pathway is actioned is through the use of medicines. We were therefore interested to see if medicines could tell us how clinical pathways were disrupted as an indirect result of the COVID-19 pandemic, as this also represented a sudden interruption to normality and shock to the healthcare system. Our ‘eureka’ moment came with the analysis of the incident data, which suddenly revealed patterns that were masked in routinely reported medications data. Using medicines in this way could be applied to surveillance of healthcare in general as well as understanding when clinical pathways are disrupted, which could build additional resilience in healthcare planning. R.S., R.T. & C.D.
From the editor
“This study of the impact of the COVID-19 pandemic on cardiovascular disease prevention stands out as a truly large-scale analysis, based on analysis of a drug prescription database from Great Britain containing more than 1 billion records. The findings show greatly reduced use of anti-hypertensive and lipid-lowering medicines, leading the authors to call for the identification and treatment of individuals who may have missed treatment during the pandemic.” Editorial Team, Nature Medicine.
Footnotes
This is a summary of: Dale, C. E. et al. The impact of the COVID-19 pandemic on cardiovascular disease prevention and management. Nat. Med. 10.1038/s41591-022-02158-7 (2022).
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Watt, T., Kelly, E. & Fisher, R. Use of primary care during the COVID-19 pandemic: May 2021 update: Patient-level data analysis of the impact of COVID-19 on primary care activity in England. (ed. The Health Foundation) (2021). This webpage describes the impact of the COVID-19 pandemic on primary care in England.
- 2.Carr MJ, et al. Impact of COVID-19 on diagnoses, monitoring, and mortality in people with type 2 diabetes in the UK. Lancet Diabetes Endocrinol. 2021;9:413–415. doi: 10.1016/S2213-8587(21)00116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wood A, et al. Linked electronic health records for research on a nationwide cohort of more than 54 million people in England: data resource. BMJ. 2021;373:n826. doi: 10.1136/bmj.n826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bennie M, Malcolm W, McTaggart S, Mueller T. Improving prescribing through big data approaches-Ten years of the Scottish Prescribing Information System. Br. J. Clin. Pharmacol. 2020;86:250–257. doi: 10.1111/bcp.14184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lyons RA, et al. The SAIL databank: linking multiple health and social care datasets. BMC Med. Inform. Decis. Mak. 2009;9:3. doi: 10.1186/1472-6947-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]