Abstract
Aim:
To quantify the association between the duration of the pediatric-to-adult care transfer with glycemic control among patients with type 1 diabetes (T1D).
Methods:
This retrospective cohort study included patients with T1D who completed transfer between pediatric and adult diabetes clinics at a single academic medical center between 2004 and 2020. The primary exposure was time from the last pediatric to first adult diabetes care encounter. The primary outcome was the average HbA1c in the first year after entry into adult care.
Results:
A total of 449 patients (mean age at transfer 19.8yrs, 51.7 % male) were included for analysis. Transfer required a median of nearly 5 months (196 days; IQR:93–251) and in adjusted and unadjusted models was strongly associated with increased HbA1c within 1 year of transfer (0.19 %, 2 mmol/mol; 95 %CI:0.04 %–0.33 %) for each 6 months of latency. In secondary analyses, transfer latency also exhibited a significant association with days spent hospitalized (IRR 1.23 per 6 months; 95 %CI:1.08–1.33).
Conclusions:
Our findings isolate and quantify the impact of prolonged lapses in care associated with the pediatric-to-adult care transfer. These findings underscore the need for providers and healthcare systems to improve this care transition in order to improve outcomes for this vulnerable patient population.
Keywords: Type 1 Diabetes, Transition, Transfer, Young Adult, Care Utilization
1. Introduction
Adolescents and emerging adults with type 1 diabetes are particularly vulnerable to acute and chronic complications associated with this chronic disease. [1,2] Cross-sectional studies have consistently shown that among all age groups, average HbA1c is the highest among late adolescents and early young adults. [3,4] Notably, when compared to the general population, 20–29 year old males with type 1 diabetes face a threefold increase in mortality, while females in this age group have a six-fold increase in mortality. [5] Among many potential personal, social, and health system factors, difficulty in transferring care between pediatric and adult care models has been identified as a modifiable factor contributing to worsening disease control. [1,6,7].
Care transition – the planned purposeful process of moving from a pediatric-to-adult model of care – ideally involves years of planning and ongoing follow-up for patients, providers and their social support systems. [8–11] Transition is highlighted by the transfer between pediatric and adult care, which, for patients with type 1 diabetes, is a high-risk event for loss to follow-up, rising HbA1c, hospitalization, and mortality. [2,12–16] Previous work quantifying this impact has largely relied either on age-based cut-offs (e.g., age 18 years) to define care transfer, included only pediatric or adult patients, or did not define a particular time of transfer due to inherent challenges of tracking longitudinal outcomes between distinct health care systems. [3,11–15,17] Thus, while clinical experience and qualitative data strongly suggest prolonged transfer as a risk factor for worsened outcomes among these patients, quantitative data to isolate its impact on changes in important diabetes-related outcomes are limited. [13,15,18,19].
In this study, we used detailed electronic health record (EHR) data including pediatric and adult clinic, laboratory, and hospital admission data to identify a subset of patients who transferred care within a single academic medical center. This rich dataset allowed us to analyze trends in HbA1c and healthcare utilization with respect to age and relative to key events in the transfer of care. We sought to isolate the association of prolonged transfer from pediatric-to-adult care on both short and long-term measures of disease control as well as changes in healthcare utilization within this cohort.
1.1. Subjects, Materials, and Methods
1.1.1. Pediatric type 1 diabetes clinical environment and cohort identification
The current study is a retrospective cohort study of patients with type 1 diabetes from a single medical center in the Southeast United States. Pediatric and adult patients received outpatient care within a single outpatient clinic floor in adjacent offices. Pediatric and adult providers also provided outpatient care to a small proportion of patients at outlying satellite clinics, all of which were included for analysis. The decision for transfer to adult care occurred at the discretion of the pediatric provider with no established or mandated age of transfer to adult care. For the duration of the study period, there were no formal transition preparation or receivership programs implemented within either the pediatric or adult clinics. Eligible patients were identified using an automated search of EHR data including the records from these pediatric and adult diabetes practices. In order to identify patients with established care in the pediatric clinic, patient records were included if they had three consecutive years with at least one clinic visit per year in the pediatric diabetes clinic prior to 3/15/2020. Patients were identified as having type 1 diabetes by an ICD diagnosis code of type 1 diabetes mellitus (ICD10: E10.*) submitted by the billing provider at the time of the visit. Previous work suggests that provider-assigned diagnosis of type 1 diabetes is a highly specific indicator of diabetes diagnosis. [20] Diagnosis was further confirmed by manual chart review of those patients taking non-insulin medications, and those with clinic visits in the pediatric pulmonary clinic to exclude those with type 2 diabetes and cystic fibrosis-related diabetes. After validation, a total of 4,128 patients met our criteria for being engaged in pediatric diabetes care and were eligible for further analysis.
1.1.2. Transfer cohort identification
Pediatric patients engaged in care for type 1 diabetes were included in our transfer cohort if they had undergone a transfer to the adult diabetes clinic – defined as having at least two clinic visits in the adult diabetes clinic prior to 3/15/2020. Furthermore, to identify only those patients who transferred their care directly to our adult diabetes clinic – without significant follow up by an external provider – we included only those patients who completed transfer to the adult clinic within 2 years of their last pediatric clinic visit. Additionally, due to the small number of patients with only primary care follow up for their diabetes care in our center (n = 2), these patients were excluded from our analysis. Among the 4,128 patients identified as being followed in our pediatric clinic within this timeframe, 449 met our definition of an observed, internal care transfer and were included in our primary analysis.
1.1.3. Visit identification and lab data extraction
We analyzed lab values and health system encounters by study subjects to the pediatric diabetes clinic, emergency department and pediatric inpatient units as well as any adult outpatient, inpatient or emergency department visits within the medical center’s facilities during the study period. Data prior to 1/1/2004 are not complete in the EHR and were excluded. Furthermore, visits completed after 3/15/2020 were also excluded due to disruptions in clinical care associated with the COVID-19 pandemic and documented elsewhere. [21].
1.1.4. Transfer date determination and transfer ‘Epoch’ designation
Using visit dates to the pediatric and adult diabetes clinics, a timeline of care was determined for each patient (Fig. 1). The first visit date to the pediatric diabetes clinic was assigned as the date of diagnosis, and the date of the last pediatric diabetes clinic visit was used as the end date for pediatric diabetes care. Thus, any clinical encounter within this interval was coded as occurring in the pediatric care epoch. Similarly, visits falling between the first adult diabetes clinic visit to the end of the study period were identified as occurring in the adult care epoch. Finally, visits falling after the last pediatric and before the first adult visits were coded as being in the transition epoch regardless of the care site (adult or pediatric associated) where the visit occurred. All subsequent analyses used these care epochs to determine if an encounter or laboratory value was pediatric, transition or adult.
Fig. 1.
Diagram of Analytic Approach to Each Patient’s Care Encounter Timeline. Above diagram represents the analytic approach taken for visits for each patient. Visits and laboratory values that occurred/were obtained before the last pediatric diabetes clinic visit were analyzed as pediatric while those occurring after the first adult visit were similarly deemed to be belonging to the adult care epoch.
1.1.5. Exposure
The primary exposure for the study was transfer latency, defined as the time (in days) from the last pediatric to the first adult diabetes visit. Subsequent analysis scaled transfer latency by six months (180 days) for ease of interpretation on a clinically relevant time scale. [22].
1.1.6. Outcomes
The primary outcome was the mean HbA1c measured at all visits in the first year of the adult care epoch with pre-planned sensitivity analysis to evaluate HbA1c time-horizons at 2 years and all visits. A priori secondary outcomes were ED visits and days admitted in the first year after transition. These visits were determined by simple counts of patients encounters meeting these criteria during the transition epoch for each patient standardized to the duration of the transition epoch for these patients.
1.1.7. Ethics statement
This project was determined to be exempt research by the Vanderbilt Institutional Review Board [VUMC IRB# 182241]. In accordance with the ethical framework previously described for Research Derivative studies, [23] all investigators must have IRB determination prior to accessing the resource, and also signed a standard data use agreement.
1.1.8. Statistical Methods
Transfer latency was summarized by demographic and clinical characteristics using standard descriptive statistics. HbA1c was summarized by age and by time since last pediatric visit using smoothing splines. Multivariable regression models with different levels of adjustment quantified associations between transfer latency (per 6-month increase) and outcomes: linear regression for HbA1c, which exhibited a symmetric distribution, and Poisson regression for annualized ED visit and days admitted. Adjustment covariates included demographic characteristics and care-related factors. Demographic characteristics included gender, race/ethnicity as recorded in the EHR (non-Hispanic White, non-Hispanic Black, Hispanic), insurance type (public, private), and age at diagnosis, and care-related factors were HbA1c in the year prior to transition, pediatric visit frequency, and occurrence of the last pediatric visit before or after 1/1/2010 (to account for temporal trends arising from implementation of the Affordable Care Act). For ED visit and hospitalization outcomes, the number of these visits in the year prior to transfer was also included in adjusted models. In sensitivity analyses, models were rerun with increasing HbA1c time-horizons – 2 years after transfer completion and all visits after transfer as well as by requiring 1 or 2 years to pediatric and adult follow up. All analyses were completed using Stata v16.1 (StataCorp, College Station, Texas). We followed standardized guidance for reporting observational studies. [24].
1.2. Results:
1.2.1. Cohort Demographics
Among 4,128 patients followed in our pediatric diabetes clinic, we identified 449 patients who met inclusion criteria for our transfer cohort with an observed transfer of care to our adult diabetes clinic between 1/1/2004 and 3/15/2020. Demographics of the total pediatric clinic cohort as well as the transfer cohort are presented in Table 1. Overall, the cohort that completed transfer to an adult provider within two years of their last pediatric visit was more likely to be non-Hispanic White (86.7 % vs 80.7 %), have a similar HbA1c in the last year prior to transfer to adult care (8.8 % vs 8.9 %) and have a later age at diagnosis (11.5yrs. vs 9.5yrs) as compared to the population of pediatric clinic patients who did not meet our inclusion criteria for the transfer cohort. We also noted a striking difference in insurance providers, with only 8.0 % of those completing transition within our clinic having Medicaid as their primary insurance, whereas Medicaid covered nearly 30 % of patients in the total pediatric population.
Table 1.
Demographic and Clinical Characteristics of Transfer and Non-Transfer Pediatric Patients.
| Characteristic | Transfer Patients | Non-Transfer Patients |
|---|---|---|
|
| ||
| Total Number | 449 | 3,679 |
| Male Gender (%) | 232 (51.7 %) | 1940 (52.7 %) |
| Race/Ethnicity | ||
| Non-Hispanic, White (%) | 390 (86.7 %) | 2968 (80.7 %) |
| Non-Hispanic, Black (%) | 36 (8.0 %) | 360 (9.8 %) |
| Hispanic (%) | 10 (2.2 %) | 106 (2.9 %) |
| Medicaid insurance at last pediatric visit (%) | 36 (8.0 %) | 1088 (29.6 %) |
| Age (in years) at Diagnosis (Mean, SD) | 11.5 (3.5) | 9.5 (4.1) |
| Mean A1c while in pediatric care (SD) | 8.8 % (1.4) | 8.9 % (1.5) |
| Mean A1c while in the last year of pediatric care (SD) | 9.0 % (2.0) | N/A |
| Average pediatric visits per year (SD) | 3.6 (1.9) | 4.1 (1.8) |
| Average pediatric hospital inpatient days per year (SD) | 0.15 (0.37) | 0.24 (0.59) |
| Median duration (in months) of pediatric follow up (IQR) | 95.7 (60.5 – 129.1) | N/A |
| Median duration (in months) of adult follow up (IQR) | 46.2 (19.4 – 75.6) | N/A |
All patients were seen in 3 consecutive years in the pediatric diabetes clinic with a primary diagnosis at each of these visits of Type 1 Diabetes. Patients included in the transfer cohort completed at least two clinic visits in the adult diabetes clinic at the same medical center.
1.2.2. Trends in HbA1c and transition timing
As with previous cross-sectional and longitudinal studies, our cohort exhibited a gradual rise in mean HbA1c beginning in late adolescence with a peak at age 18 years 6 months and a subsequent decline in mean HbA1c across the early to mid 20 s (Supplementary Figure S1). [3] Within our cohort, the mean age patients completed their last pediatric clinic visit was 19.3 years (SD 1.3) while the mean age at the first adult clinic visit was 19.8 years (SD 1.3). Overall, the mean HbA1c within the first year before transfer and the first year after transfer, were nearly equal: 9.0 % (75 mmol/mol; SD 1.9 %) and 8.9 % (74 mmol/mol; SD 2.0 %), respectively.
1.2.3. Association between transfer latency and HbA1c after transfer to adult care
Median transfer latency – the time from the last pediatric diabetes visit to the first adult diabetes visit – was approximately 5 months (144 days; IQR 93 – 251). Notably, 38.9 % (175) of patients had latencies of more than 6 months and 13.5 % (61) were observed to have more than a year between their last pediatric and first adult visits. Transfer latency was observed to substantially differ across levels of multiple social and clinical factors, including race/ethnicity, insurance status, age of diagnosis, pediatric HbA1c, and frequency of both admissions and clinic visits while in pediatric care (Table 2). In particular, median transfer latency was greater among non-Hispanic Black patients compared to non-Hispanic White and Hispanic patients, and among patients insured by Medicaid compared to those with private insurance.
Table 2.
Transfer Latency by Demographic and Clinical Characteristics.
| Days of Transfer “Latency” (Median, IQR) | |
|---|---|
|
| |
| All Patients | 146 (94 – 265) |
| Gender | |
| Female | 145 (93 – 257) |
| Male | 143.5 (92.5 – 248.5) |
| Race/Ethnicity | |
| Non-Hispanic White | 142 (93 – 249) |
| Non-Hispanic Black | 194 (96 – 312) |
| Hispanic | 129.5 (70 – 177) |
| Last pediatric insurance coverage | |
| Private Insurance | 138 (92 – 237) |
| Medicaid | 244.5 (144 – 391) |
| Age at Diagnosis | |
| < 8 years | 177 (96 – 326) |
| 8 – 14 years | 146.5 (95 – 252) |
| >=14 years | 119.5 (91 – 213) |
| Average HbA1c 1 year prior to transition to adult care | |
| < 7 %(<53 mmol/mol) | 112.5 (92.5 – 233) |
| 7 – 8.5 % (53–69 mmol/mol) | 145 (93 – 232) |
| 8.5 – 10 % (69–86 mmol/mol) | 158 (96 – 257) |
| >= 10 % (greater than86 mmol/mol) | 146 (91 – 264) |
| Average visits to the pediatric clinic per year | |
| < 2 | 181.5 (99 – 348) |
| 2–4 | 156 (95 – 257) |
| >= 4 | 116.5 (89 – 182.5) |
| Ever Admitted for T1D? | |
| No | 145 (95 – 252) |
| Yes | 138.5 (90.5 – 248.5) |
| Last Peds year | |
| Before 2010 | 146 (93 – 300) |
| 2010 or later | 142.5 (92.5 – 236) |
In our primary analyses, we observed an increase in average HbA1c of 0.31 % (3 mmol/mol; 95 %CI 0.09 %–0.53 %) for every 6 months of delay between the last pediatric and first adult visits (Table 3). This difference was attenuated but remained statistically significant after covariate adjustment: 0.19 % (2 mmol/mol; 95 %CI 0.04 % – 0.33 %). These findings were robust in pre-specified sensitivity analyses extending HbA1c values to include those 2 years after transfer as well as including all adult HbA1c values (Supplementary Table S1). Fig. 2 shows trends in HbA1c relative to the last pediatric clinic visit. Those with the shortest transfer latency (<3 months) saw a modest decrease in mean HbA1c from their last pediatric to first adult clinic visits (9.1 % vs 8.8 %) while those that took more than 6 months between pediatric and adult visits saw a rise in HbA1c across this period (9.2 % vs 9.5 %). Those completing transfer between 3 and 6 months had no significant change in their HbA1c during their latent period (8.7 % vs 8.7 %). Notably, while those with transfer latencies shorter than 6 months saw overall trends toward lower HbA1cs over the first 36 months after transfer to adult care, those who took more than 6 months to transfer saw no such decline in HbA1c over this period with HbA1c remaining roughly unchanged over this period.
Table 3.
Regression Models for Transfer Latency association with Primary and Secondary Outcomes.
| Difference in HbAlc (%) in the first year in adult carea | p value | IRR for ED visits in the first year in adult carea | p value | IRR for inpatient days in the first year in adult carea | p value | |
|---|---|---|---|---|---|---|
|
| ||||||
| Model 1 (Unadjusted) | 0.31 (0.09 to 0.53) | 0.005 | 1.25 (1.04 to 1.51) | 0.018 | 1.41 (1.27 to 1.58) | <0.001 |
| Model 2 (Demographic Adjusted)b | 0.28 (0.06 to 0.50) | 0.014 | 1.04 (0.86 to 1.27) | 0.67 | 1.21 (1.03 to 1.28) | 0.001 |
| Model 3 (Fully Adjusted)c | 0.19 (0.04 to 0.33) | 0.011 | 1.09 (0.90 to 1.44) | 0.39 | 1.23 (1.11 to 1.38) | <0.001 |
Contrasts (i.e., mean difference in HbA1c, incidence rate ratios) are for every additional 6 months of transfer latency.
Demographic factors: gender, race, insurance type (public vs private) and age at diagnosis.
Fully adjusted model factors: demographic factors and A1c in the year prior to transition, pediatric visit frequency, last pediatric visit before or after 2010. For ED visit and hospitalization outcomes the number of these visits in the year prior to transfer was also included in the fully adjusted model.
Fig. 2.
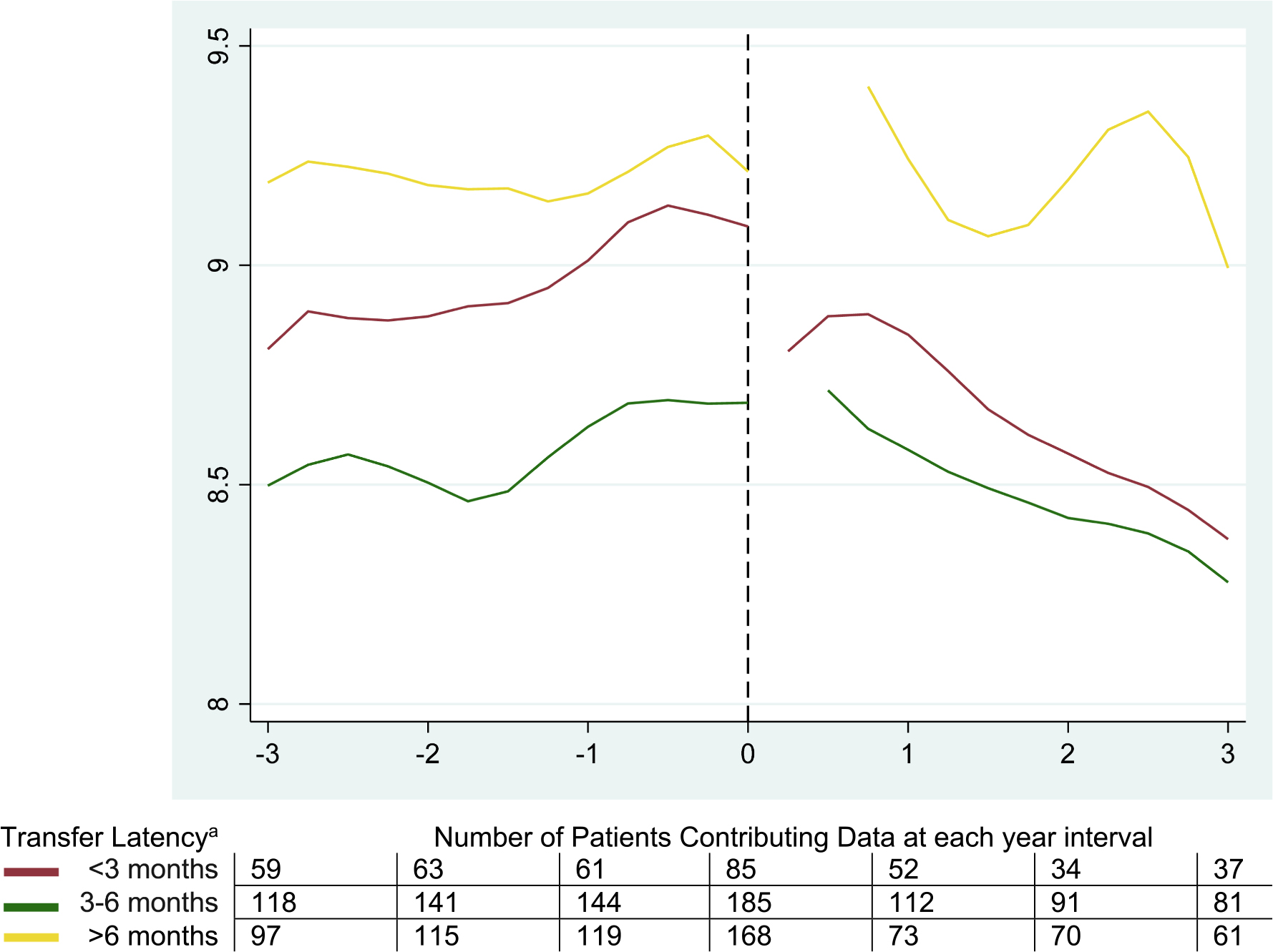
HbA1c (%) Relative to Time of Last Pediatric Clinic Visit Across Transfer Latency Cohorts a Transfer Latency strata chosen based on standard care recommendations for clinical monitoring for patients with type 1 diabetes. [22].
1.2.4. Association between transfer latency and care utilization
In addition to the association between latency and HbA1c observed in our primary analysis, unadjusted and adjusted analyses of measures of care utilization – ED visits and admission days within 1 year of the last pediatric visit – showed statistically significant and clinically meaningful increases in hospitalization days with prolonged transfer latency. We observed a 23 % increase in inpatient days for every 6 months of transfer latency (Incidence Rate Ratio, IRR 1.23; 95 %CI 1.11–1.38) after covariate adjustment. In our unadjusted analysis, we observed a statistically significant 25 % increase in ED visits for every 6 months of transfer latency (IRR 1.25 (95 %CI 1.04–1.51), an association which reduced in magnitude and below the threshold for statistical significance in adjusted analyses (IRR 1.09 (95 %CI 0.90–1.44)).
2. Discussion
This retrospective cohort study used a novel study design to isolate the impact of pediatric-to-adult care transition on disease control among patients with type 1 diabetes. Our innovative approach – analyzing data based on time rather than age relative to important events in the transfer of care from pediatric-to-adult providers–provides unique insight into trends in HbA1c across these milestone events in care. We were able to quantify the impact of prolonged transfer latency on markers of disease control and care utilization. We observed a clinically and statistically significant association of transfer latency with both glycemia and inpatient hospital days. While not statistically significant, we also observed clinically significant increases in ED utilization with prolonged transfer, which was likely due to the relatively low frequency of these events, limiting our power to detect statistically significant differences.
It is important to note, as highlighted in Table 1, that the cohort included in our primary analysis is not representative of the underlying population of patients with type 1 diabetes in our clinic or according to population studies. Patients in our transfer cohort were significantly more likely to be non-Hispanic White, have private insurance, and lower average HbA1c levels in the pediatric period than those in the general population of pediatric type 1 diabetes. While these differences limit the generalizability of our estimate of the effect of latency on HbA1c, the persistence of this association, even in a cohort of young adults likely to have greater resources than the overall clinic population, strongly suggests that our findings underestimate the negative impact transfer latency has on disease control and care utilization among all patients with type 1 diabetes.
Among those patients with public insurance and from underrepresented groups who were included in our cohort had marked increases in transfer latency. Therefore, our data suggest that the pediatric-to-adult transfer appears to exacerbate existing health disparities within our system both in fewer patients completing this transfer, and with poorer outcomes among those who do successfully transfer. While this dataset provides little additional context for these findings, the concordance of our observations with other recent studies adds further support to these conclusions and suggest that social determinants of health such as access to time off for medical care and transportation may play a role in these findings. [15,25] The disparate outcomes based on income and race in this study merit further investigation both to confirm and explore these findings as well as to assess the impact of potential interventions to address these issues such as increased use of telehealth or more comprehensive approaches to care which address the additional barriers faced by these groups.
This study has implications for multiple stakeholders within health care systems. First, for pediatric providers, our findings emphasize the importance of transition planning to ensuring close follow up with an adult provider after transfer from pediatric-to-adult care. Recent work has shown improved outcomes for pediatric-based transition programs using care navigators to assist patients in establishing care with adult providers. [1] The current study provides data to quantify this impact and provides further insight into one potential mechanism for these gains. Second, for adult providers, these findings emphasize the importance of developing systems to accept pediatric patients into adult practice. Maintaining and reinforcing positive health behaviors is a key goal of frequent clinic visits which is demonstrated in our data and will help to avoid short- and long-term diabetes-related complications. Third, ensuring a smooth transfer of care also may have significant benefits to hospitals and payors as demonstrated by the association between increased transfer latency and high-cost care utilization such as hospitalizations and ED visits.
The current study has several strengths: to our knowledge, it is the largest US cohort with complete longitudinal data across the pediatric-to-adult transition among patients with T1D for which the exact timing of the pediatric-to-adult care transfer is known. [26] The rich clinical and laboratory data in our dataset allowed us to demonstrate the heterogeneity of transfer initiation and duration across this population and how this correlated with important clinical outcomes. Compared to other similar studies, our ability to isolate the exact timing of transition independent of age provides the opportunity to better understand the effect of this event independent of co-occurring biological and social changes within this age group [4,12,27].
Among the limitations to our data are concerns about generalizability and completeness of our dataset. Given the fragmented nature of medical record data systems, follow up information including the granular visit-level data needed to conduct these analyses were not available for all patients in our pediatric clinic, as noted above. Thus, even within this narrow cohort, our estimates of the association of transfer latency with ED utilization and hospitalized days are likely underestimates of overall utilization by these patients.
Overall, our findings support that prolonged time between the last pediatric visit and first adult visit in patients with T1D is a significant risk factor for worsened disease control and healthcare utilization – as measured by HbA1c and hospital days – after transfer to adult care. This emphasizes the importance of optimizing care at this care transition on disease control. Future work is needed to replicate these results in diverse populations within the US healthcare context and to quantify the impact of prolonged transfer latency on rates of future complications.
Supplementary Material
Acknowledgements
Funding:
The publication was supported by National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number T32 DK007061 (DRT), the Vanderbilt Diabetes Research and Training Center (P30 DK20593) and the Vanderbilt Institute for Clinical and Translational Research CTSA award (UL1 TR002243) from the NCATS.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary material
Supplementary data to this article can be found online at https://doi.org/10.1016/j.diabres.2022.110113.
References
- [1].Peters A, Laffel L, American Diabetes Association Transitions Working G. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society). Diabetes Care 2011;34(11):2477–85. DOI: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lyons SK, Libman IM, Sperling MA. Clinical review: Diabetes in the adolescent: transitional issues. J Clin Endocrinol Metab 2013;98(12):4639–45. 10.1210/jc.2013-2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio LA, et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care 2015;38(6):971–8. [DOI] [PubMed] [Google Scholar]
- [4].Petitti DB, Klingensmith GJ, Bell RA, Andrews JS, Dabelea D, Imperatore G, et al. Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr 2009;155(5):668–672.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Laing SP, Swerdlow AJ, Slater SD, Botha JL, Burden AC, Waugh NR, et al. The british diabetic association cohort study, I: all-cause mortality in patients with insulin-treated diabetes mellitus. Diabet Med 1999;16(6):459–65. [DOI] [PubMed] [Google Scholar]
- [6].Sandler CN, Garvey KC. A practice in maturation: current perspectives on the transition from pediatric to adult care for young adults with diabetes. Curr Diab Rep 2019;19(11):126. 10.1007/s11892-019-1247-x. [DOI] [PubMed] [Google Scholar]
- [7].Garvey KC, Wolpert HA, Laffel LM, Rhodes ET, Wolfsdorf JI, Finkelstein JA. Health care transition in young adults with type 1 diabetes: barriers to timely establishment of adult diabetes care. Endocr Pract 2013;19(6):946–52. 10.4158/EP13109.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chu PY, Maslow GR, von Isenburg M, Chung RJ. Systematic review of the impact of transition interventions for adolescents with chronic Illness on transfer from pediatric to adult healthcare. J Pediatr Nurs 2015;30(5):e19–27. 10.1016/j.pedn.2015.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Blum RWM, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. a position paper of the society for adolescent medicine. J Adolesc Health 1993;14(7):570–6. [DOI] [PubMed] [Google Scholar]
- [10].Sheehan AM, While AE, Coyne I. The experiences and impact of transition from child to adult healthcare services for young people with Type 1 diabetes: a systematic review. Diabet Med 2015;32(4):440–58. 10.1111/dme.12639. [DOI] [PubMed] [Google Scholar]
- [11].Lotstein DS, Seid M, Klingensmith G, Case D, Lawrence JM, Pihoker C, et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics 2013;131(4):e1062–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Clements MA, Foster NC, Maahs DM, Schatz DA, Olson BA, Tsalikian E, et al. Hemoglobin A1c (HbA1c) changes over time among adolescent and young adult participants in the T1D exchange clinic registry. Pediatr Diabetes 2016;17(5):327–36. [DOI] [PubMed] [Google Scholar]
- [13].Bryden KS, Dunger DB, Mayou RA, Peveler RC, Neil HA. Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care 2003;26(4):1052–7. (https://www.ncbi.nlm.nih.gov/pubmed/12663572). [DOI] [PubMed] [Google Scholar]
- [14].Pinhas-Hamiel O, Hamiel U, Boyko V, Graph-Barel C, Reichman B, Lerner-Geva L. Trajectories of HbA1c levels in children and youth with type 1 diabetes. PLoS One 2014;9(10):e109109. DOI: 10.1371/journal.pone.0109109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Nip ASY, Lodish M. Trend of diabetes-related hospital admissions during the transition period from adolescence to adulthood in the state of california. Diabetes Care 2021;44(12):2723–8. [DOI] [PubMed] [Google Scholar]
- [16].Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A. Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality - united states, 2000–2014. MMWR Morb Mortal Wkly Rep 2018;67(12):362–5. 10.15585/mmwr.mm6712a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of Type 1 diabetes management and outcomes from the T1D Exchange in 2016–2018. Diabetes Technol Ther 2019;21(2):66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Garvey KC, Foster NC, Agarwal S, DiMeglio LA, Anderson BJ, Corathers SD, et al. Health care transition preparation and experiences in a U.S. national sample of young adults with type 1 diabetes. Diabetes Care 2017;40(3):317–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hilliard ME, Perlus JG, Clark LM, Haynie DL, Plotnick LP, Guttmann-Bauman I, et al. Perspectives from before and after the pediatric to adult care transition: a mixed-methods study in type 1 diabetes. Diabetes Care 2014;37(2):346–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Crume TL, Hamman RF, Isom S, et al. The accuracy of provider diagnosed diabetes type in youth compared to an etiologic criteria in the SEARCH for Diabetes in Youth Study. Pediatr Diabetes 2020. 10.1111/pedi.13126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Tilden DR, Datye KA, Moore DJ, French B, Jaser SS. The rapid transition to telemedicine and its effect on access to care for patients with type 1 diabetes during the COVID-19 Pandemic. Diabetes Care 2021;44(6):1447–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].American DA. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of medical care in diabetes-2021. Diabetes Care 2021;44 (Suppl 1):S40–52. 10.2337/dc21-S004. [DOI] [PubMed] [Google Scholar]
- [23].Roden DM, Pulley JM, Basford MA, Bernard GR, Clayton EW, Balser JR, et al. Development of a large-scale de-identified DNA biobank to enable personalized medicine. Clin Pharmacol Ther 2008;84(3):362–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61 (4):344–9. [DOI] [PubMed] [Google Scholar]
- [25].Agarwal S, Kanapka LG, Raymond JK, et al. Racial-Ethnic Inequity in Young Adults With Type 1 Diabetes. J Clin Endocrinol Metab 2020;105(8). DOI: 10.1210/clinem/dgaa236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shulman R, Cohen E, Benchimol EI, Nakhla M. Methods for Measuring the time of transfer from pediatric to adult care for chronic conditions using administrative data: a scoping review. Clin Epidemiol 2020;12:691–8. 10.2147/CLEP.S256846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Toschi E, Bailey RJ, Miller KM, Calhoun PM. Improvement in A1c levels in early adulthood in the T1D Exchange: impact of racial, socioeconomic, and clinical factors. J Clin Endocrinol Metab 2021;106(5):1294–302. 10.1210/clinem/dgab077. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


