Abstract
Background
Mental health problems are frequent in the postpartum period, but accessible treatment options are lacking. The MPOWER study investigated whether the use of trained lay coaches could increase the uptake and effectiveness of a web-based intervention (WBI) for women with postpartum depression and/or anxiety.
Objectives
First, to compare the feasibility and acceptability of a WBI for women with postpartum depression and anxiety, with and without the addition of telephone coaching calls. Second, to estimate the effectiveness of the WBI at decreasing symptoms of depression and anxiety at 6 months, with and without coaching calls.
Methods
We conducted a pilot randomized controlled trial (RCT) that enrolled women who had recently given birth and had mild to moderate postpartum depression and/or anxiety. Study participants were provided access to the WBI. Women randomized to the intervention group also received up to 7 telephone coaching calls during the 6 months of follow up. We evaluated the feasibility of the intervention through participants' usage of the WBI, as well as the completion and fidelity of planned coach calls. We measured acceptability via two questionnaires on the usability of the WBI and participant satisfaction with the intervention. To determine the potential effectiveness of the intervention, the primary outcomes were defined as symptoms of depression and anxiety at 6 months and adjusted mean differences between groups for these outcomes were estimated using linear regression models.
Results
We recruited 52 participants (25 intervention; 27 control). At 6 months, 88 % (22/25) of participants randomized to the intervention arm and 59 % (16/27) of participants randomized to the control arm remained in the study. The intervention group had an average of 11 (95 % CI: [5, 18]) more website logins than the control group. Intervention group participants completed a mean of 6.2 coaching calls with high fidelity. The estimates of the effect of the intervention on mental health outcomes at 6-months were imprecise but point estimates and confidence intervals were consistent with a moderate beneficial effect of the intervention on both symptoms of depression and anxiety (fully adjusted effects sizes: 0.51 (95 % CI: [−0.14, 1.17]) and 0.56 (95 % CI: [−0.09, 1.22]), respectively).
Conclusions
WBIs with coaching are feasible, acceptable, and potentially effective treatment options for women with mild to moderate postpartum depression and/or anxiety. The addition of coaching calls markedly increased engagement with the WBI, but a larger RCT is needed to determine the effectiveness of such an intervention.
Keywords: Postpartum depression, Postpartum anxiety, Perinatal anxiety, Perinatal depression, Web-based intervention, Telephone coaching
Highlights
-
•
Web-based interventions are promising for the treatment of post-partum depression and/or anxiety.
-
•
We compared interventions with and without coaching on 6-month outcomes.
-
•
Both interventions were feasible and acceptable for postpartum depression/anxiety.
-
•
Coach calls increased engagement and were potentially effective at 6 months.
-
•
A larger trial is needed to determine if the coached intervention is effective.
1. Introduction
1.1. Background information
Perinatal mood and anxiety disorders affect at least 1 in 5 women during the perinatal period from pregnancy until 1 year postpartum (Dennis et al., 2017). These disorders negatively affect the woman's ability to function, care for her newborn, and form a secure attachment with her baby (Martins and Gaffan, 2000; Field, 2010; Fairbrother et al., 2016).
Current treatment options for perinatal depression and anxiety have limitations. Pharmacological treatment is difficult to implement in the context of pregnancy and breastfeeding (National Institute for Clinical Excellence, 2007), and women often prefer a non-pharmacological treatment (Ride and Lancsar, 2016). Cognitive behavioral therapy (CBT) is considered the most effective psychotherapy for treating pregnant and postpartum women; mindfulness-based techniques and are also increasingly popular and are effective at reducing stress and anxiety (Williams, 2014; Branquinho et al., 2021). However, there are many barriers to accessing psychotherapy in Canada including high out-of-pocket costs, long wait times, and a lack of knowledge about available services (Moroz et al., 2020).
1.2. Prior work
Web-based interventions (WBIs) are increasingly popular treatment options for mental health disorders. Participant engagement with WBIs is generally high at the start of an intervention, but often decreases over time (de Graaf et al., 2009; Eysenbach, 2005), which limits potential therapeutic benefits (Donkin et al., 2013; Enrique et al., 2019). For this reason, human support is increasingly used to augment WBIs (Mohr et al., 2011). Guidance by coaches, therapists, or general practitioners may increase participants' accountability or motivation to complete the intervention and could also encourage them to adhere to the intervention through specific prompts, potentially increasing the effectiveness of such interventions(Renfrew et al., 2021; Mohr et al., 2011; Alkhaldi et al., 2016; Baumeister et al., 2014; Ryan et al., 2018; McCusker et al., 2022).
In the context of perinatal depression and anxiety, two recent reviews of WBIs suggested that they were effective in preventing maternal depression and anxiety (Loughnan et al., 2019; Lee et al., 2016). Of the RCTs that investigated the use of WBIs for maternal depression, few have included an element of telephone support (O'Mahen et al., 2014; Milgrom et al., 2016; Pugh et al., 2016), and none investigated the incremental effect of telephone coaching when coupled with a WBI for postpartum depression and anxiety. Further, these trials all used mental health professionals as coaches, while we used trained lay coaches, which potentially decreases the cost and increases the scalability of this intervention.
2. Methods
2.1. Study design
This pilot RCT in women with mild to moderate postpartum depression and/or anxiety compared a telephone coaching intervention coupled with a WBI to a WBI alone. The primary outcomes were symptoms of anxiety and depression at 6 months of follow up. Secondary outcomes were parental stress and maternal functioning at 3 and 6 months (methods and results of these analyses are in Appendix C). We also measured the feasibility and acceptability of both interventions. Due to the nature of the interventions, blinding of participants and the coaches was not possible. Participants provided written, informed consent to participate in the study through an online form. The study was approved by the Ethics Review Board at the primary research site. The trial was registered at the United States National Institutes of Health (ClinicalTrials.gov) #NCT04073043 in April 2019, and followed CONSORT criteria for RCTs (Moher et al., 2012).
2.2. Study population
Participants were recruited in Montreal, Canada through a large university-affiliated community hospital and the nearby healthcare network. We contacted a sample of mothers soon after birth who had delivered at the primary study hospital or at a facility within the community healthcare network between August 12th, 2019 and October 18th, 2020, to screen them for study eligibility. Because of the COVID-19 pandemic, in-person recruitment stopped from mid-March 2020 for 4.5 months. Inclusion criteria were: age 18 years or older, live birth delivery, Canadian residency, communication in English or French, and access to internet and email. In the community healthcare network, women who met these initial eligibility criteria were referred to the study by nurses from obstetric and postpartum clinics or self-referred in response to recruitment flyers. The study coordinator (SB) provided all interested eligible participants with a link to complete an online screening and eligibility form. Eligible participants were contacted by the study coordinator between 5 and 12 weeks postpartum and were subsequently screened online for symptoms of depression and anxiety.
Inclusion criteria at the mental health screening stage were an Edinburgh Postnatal Depression Scale (EPDS) score between 10 and 19 and/or a Generalized Anxiety Disorder-7 scale (GAD-7) score above 10. Participants were ineligible if they were in active psychological treatment. Women who endorsed any response other than ‘never’ on the self-harm question on the EPDS were offered a telephone follow-up with a mental health nurse and received a comprehensive list of resources by email.
If the potential participant met these criteria, we obtained their informed consent electronically and subsequently took baseline measures via an online survey platform, SimpleSurvey. Women who did not meet eligibility criteria for the RCT were sent a list of community resources by email. We offered participants nominal gift cards for completion of the follow-up questionnaires.
2.3. Randomization
Participants were randomized to receive either the WBI accompanied by coaching (intervention group) or the WBI alone (control group) by a computer-generated randomization schedule that used random block sizes of 2 or 4 with an allocation ratio of 1:1 in SAS University edition. A participant identifier number from the original screening was entered into the randomization schedule to ensure allocation concealment.
2.4. Study interventions
2.4.1. Website
HealthyMoms is a secure psychoeducational e-health platform consisting of four self-guided sections including emotional health, healthy living, mental fitness tools, and parenting with 19 learning modules embedded in these sections. Modules were grounded in cognitive-behavioral therapy (CBT) and mindfulness-based practices (Beck and Beck, 1995; Badker and Misri, 2017) and were informed by our Phase I needs assessment with women during the perinatal period (Da Costa et al., 2015). The modules include evidence-based strategies to promote maternal health behaviours (Stremler et al., 2013, Lee and Gay, 2011, Gaston et al., 2012, Chasan-Taber et al., 2011, Health Canada, 2010, Health Canada, 2007) and to enhance women's engagement with their antenatal care providers (Alegria et al., 2014; Griffin et al., 2004). The intervention and control group participants were emailed an access link to the website on the date of randomization and subsequently had access to HealthyMoms for 200 days after they were randomized. There were no time limitations or recommended pace for the participants to move through the modules. Rather, the website served as a bank of resources that participants could navigate based on their unique needs and priorities.
2.4.2. Coaching
The coaching protocol for the intervention group was adapted from one that a study investigator (JM) used in previous trials (McCusker et al., 2022). Coaches were non-professional women, with bachelor's degrees in psychology and experience in community organizations providing resources to clientele. The coach supervisor had a master's degree in counseling psychology.
The coach trainer led two one-day sessions with the coaches, which included practice coaching calls. Coaches called participants weekly during the first month, biweekly during the second month and once during the third month of the intervention period, for a maximum total of 7 calls, regardless of how many modules of the WBI a participant had consulted. Each call had a specific agenda. The main goal of the coaching calls was for the coach to guide and encourage the participant's use of the WBI and in the development of “SMART” (specific, measurable, achievable, realistic, time-limited) goals (University of California, 2016), but not to provide psychotherapy. Coaches were trained to provide information on the WBI, encourage and reinforce their use of the WBI, listen reflectively, and convey empathy to participants and to structure the calls. Coaches were trained to avoid giving personal advice or directives, interpreting behaviours, talking about their own experience, or taking on an expert role by providing information on anything beyond the WBI and its content. The recommended length of each call was 10–15 minutes.
2.5. Measures
2.5.1. Feasibility
Participants' logins to the WBI and the pages that they viewed on the website were tracked using Slimstat. We assessed the feasibility of coaching from coach logs that recorded the number and length of calls completed and from the fidelity monitoring of recorded calls. (Appendix D). The fidelity checklist comprised 8 items on procedure (e.g., adherence to call agenda, appropriate length of each call) and 9 items on content (e.g., behavior including avoidance of therapeutic role, including points on whether the coach correctly introduced themselves and helped participants with their goals) (Appendix D). Supervision meetings took place once per week between coaches and the coach supervisor where difficulties and questions were resolved.
2.5.2. Acceptability
Perceived usability of the WBI was assessed with a 21-item questionnaire administered at 6 months, adapted from previous health website usability measures (Barrera et al., 2015; Haga et al., 2013) and recommendations of the Science Panel on Interactive Communications and Health (Robinson et al., 1998). The items assessed the users' experience with the website in terms of its usability (layout, navigation, functionality) and acceptability (overall usefulness, usefulness of specific topics, utility of the site for improving mood and engaging in healthy behaviours). Participants rated their level of agreement with each item on a scale from 1 (strongly disagree) to 5 (strongly agree). An overall usability score was computed as a mean of the 21 items, with negatively phrased items reverse scored.
We used the Client Satisfaction Questionnaire (CSQ-8) to measure participants' satisfaction with the interventions at 6 months. We defined a high satisfaction score as a composite score of 24 or higher out of 32.
2.5.3. Potential effectiveness
Participants self-reported depression symptoms at baseline, 3 months, and 6 months via the EPDS, a 10-item self-report measure with a four-point response scale designed to screen for depressive symptoms in the previous seven days (Cox et al., 1987). Sum scores for the 10 items generate a total score. We ascertained anxiety symptoms at baseline, 3 months, and 6 months using the GAD-7, a seven-item self-report questionnaire that measures anxiety symptoms during the last 2 weeks.
2.6. Baseline covariates
We collected data on participants' age, education, household income, language spoken at home, immigration to Canada, total number of pregnancies, and use of professional mental health services during the previous 12 months at baseline using online questionnaires (Canadian Community Health Survey (CHS), 2012).
2.7. Statistical analyses
We determined that a minimum sample size of 20 participants in each study arm would yield an accurate estimate of the standard deviation of the outcome measure to detect a small effect size (0.2) in a full study (Whitehead et al., 2016). All analyses were conducted using STATA version 15.1 or SAS University edition. Analysis was by intention-to-treat. We assessed baseline imbalance for the outcome measures and seven other variables. We considered a difference of at least 10 % across study groups for categorical variables or a standardized mean difference of >0.2 for continuous variables to be clinically significant differences. To estimate the effect of the intervention on EPDS and GAD-7 scores, we fit four linear regression models. The first model was unadjusted; the coefficients from this model are crude estimates of the standardized mean differences (Cohen's d) for EPDS and GAD-7 scores between groups.
The second model controlled for baseline imbalances in EPDS and GAD-7 scores, and the third model adjusted for those baseline imbalances and immigration status, since this was a potential confounder and was also imbalanced between groups at baseline. The last model included baseline EPDS and GAD-7 scores, but was adjusted for income rather than immigration status because income was a potential confounder that was imbalanced between groups at baseline but was expected to be collinear with immigration status. Cohens d and 95 % confidence intervals were computed from each of these regression models for the two primary outcomes (Hedges, 2009; Borenstein et al., 2009). For Cohen's d, 0.2 is considered a small effect, 0.5 is moderate, and anything above 0.8 is considered a large effect (Lachenbruch and Cohen, 1989).
All the analyses conducted were for the completers of the questionnaires at all time points. Methods for handling sensitivity analyses to account for missing data are described in Appendix B.
3. Results
3.1. Recruitment and retention
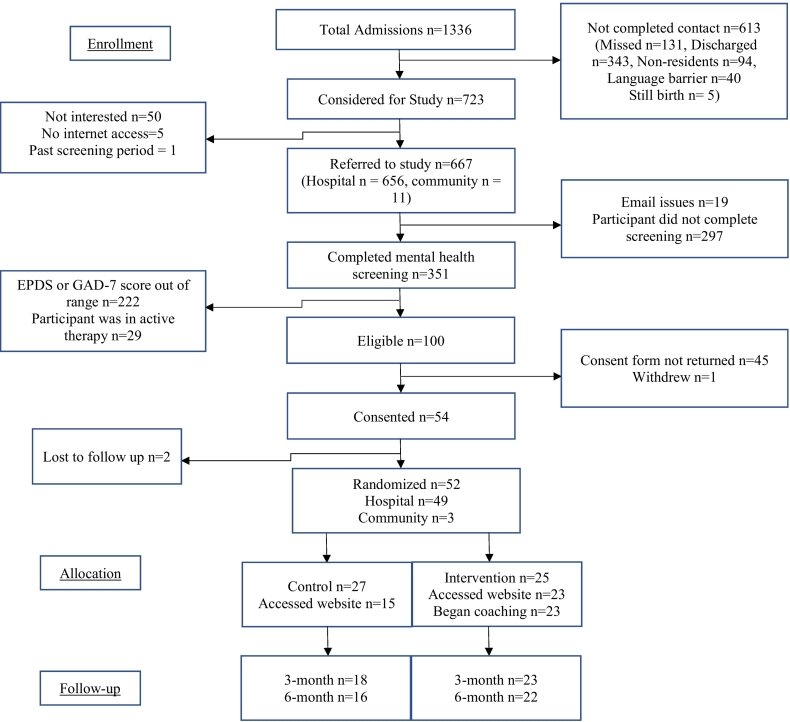
Fig. 1 describes the flow of participants through the study. Prior to the mental health screening, participants were excluded because they were not interested, had no internet access, gave birth past the screening period, because we could not contact them, or because they did not complete screening or were lost between the two screening phases. Participants with a GAD-7 score above 14 and/or an EPDS score of 20 or higher at the initial screening were offered a referral to a mental health nurse (n = 11, of whom 5 accepted). An additional 9 participants that had high GAD-7 or EPDS scores during the 3- and 6-month follow-up were also referred to the mental health nurse (n = 9, of whom 2 accepted).
Fig. 1.
Flow chart.
After the mental health screening, 100 potential participants were eligible and 52 consented (52 %): 27 were randomized to the control arm and 25 to the intervention arm. At 6 months, 22 participants (88 %) in the intervention arm and 16 participants (67 %) in the control arm remained in the study.
There were baseline differences between the intervention and control arms for depression and anxiety scores (Table 1). Participants in the intervention group were, on average, more likely to speak English or French at home, less likely to be an immigrant to Canada, and were more likely to have an income of $60,000 or more compared to the control group (Table 1).
Table 1.
Baseline characteristics by study group.
| Variablesa | Control (n = 27) |
Intervention (n = 25) |
Difference in % or standardized mean differenceb | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Edinburgh Postnatal Depression Scale (EPDS: 0 to 30) | |||||
| <12 (depression possible/not likely) | 10 | 37.0 | 14 | 56.0 | 19.0 |
| 12–19 (fairly high possibility of depression or probable depression) | 17 | 63.0 | 11 | 44.0 | 19.0 |
| Mean (SD) | 12.5 (2.5) | 12.2 (2.4) | 0.12 | ||
| Generalized Anxiety Disorder (GAD-7: 0 to 21) | |||||
| 0–4 (minimal anxiety) | 10 | 37.0 | 4 | 16.7 | 20.3 |
| 5–9 (mild anxiety) | 12 | 44.4 | 15 | 62.5 | 18.1 |
| 10+ (moderate or severe anxiety) | 5 | 18.6 | 5 | 20.8 | 2.2 |
| N missing | 0 | 1 | |||
| Mean (SD) | 6.5 (4.2) | 7.3 (3.7) | 0.20 | ||
| Age, mean (SD) | 32.7 (4.3) | 32.9 (4.7) | 0.04 | ||
| N missing | 2 | 1 | |||
| Language spoken at home | |||||
| English/French | 14 | 51.8 | 19 | 76.0 | 24.2 |
| Other | 13 | 48.2 | 6 | 24.0 | |
| Immigrant to Canada | 19 | 70.4 | 13 | 52.0 | 18.4 |
| Education | |||||
| Bachelor degree or less | 14 | 51.9 | 16 | 64.0 | 12.1 |
| Master/doctorate | 13 | 48.1 | 9 | 36.0 | |
| Annual household income (Canadian $) | |||||
| <$60,000 | 14 | 51.8 | 8 | 32.0 | 19.8 |
| $60,000 + | 13 | 48.2 | 17 | 68.0 | |
| Number of pregnancies including current pregnancy | |||||
| 1 | 11 | 40.7 | 12 | 48.0 | 7.3 |
| 2+ | 16 | 59.3 | 13 | 52.0 | 7.3 |
| Use of professional mental health services in the past 12 months | 4 | 14.8 | 2 | 8.0 | 6.8 |
Baseline variables that were selected a priori were EPDS and GAD-7 scores. Age, language, immigration status, education, household income, number of pregnancies, and use of mental health services were variables that were selected to verify baseline imbalances between study groups after the study began.
Baseline imbalances between the two study groups, defined as either a difference of 10 % or more between groups for categorical variables or a standardized mean difference of at least 0.2 for continuous variables, are in bold.
3.2. Feasibility
Average fidelity scores for the sample of 42 monitored calls were 93.9 % (7.5/8) for procedure and 100 % (9/9) for content. For the intervention group, 2 participants mentioned “a lack of time” as a reason for dropping out of the study. These 2 early dropouts did not receive any coach calls and did not access the website during the intervention period. Among those with at least one completed call, the average length of the call was 12.1 min and the average total call time with each participant over the entire intervention period was 74.9 min (Table 2). The intervention greatly increased the uptake of the website: 92 % of the coached group ever accessed the website compared to 56 % of the control group, and among users, the coached group logged in to the website almost 3 times more often (Table 2). On average, over the 200-day period over which participants had access to the website, participants who received coaching calls logged onto the site more often, viewed more of its webpages, and accessed more modules than controls (Table 2).
Table 2.
Feasibility and acceptability of the intervention by study group (n = 52).
| Variables | Control |
Intervention |
Differencea [95 % confidence interval] | ||
|---|---|---|---|---|---|
| (n = 27) |
(n = 25) |
||||
| n | % | n | % | ||
| Website useb | |||||
| Any login | 15 | 55.6 | 23 | 92.0 | 36.4 [14.9; 58.0] |
| Number of logins, mean (SD) (among users) | 6.7 (6.2) | 18.1 (12.4) | 11.4 [5.2; 17.6] | ||
| Coaching | |||||
| Number of coach calls per participant, n (%) | |||||
| 0 | 2 | 8.0 | |||
| 1–4 | 2 | 8.0 | |||
| 5–6 | 6 | 24.0 | |||
| 7 | 15 | 60.0 | |||
| Mean (SD)c | 6.2 (1.6) | ||||
| Length of a call in minutesd, mean (SD) | 12.1 (5.5) | ||||
| Cumulative length of callsd, mean (SD) | 74.9 (28.8) | ||||
| Website usability questionnaire completede: | (n = 11) | (n = 19) | |||
| Website usability score (1 to 5), mean (SD)e | 4.0 (0.7) | 3.9 (0.7) | −0.0 [−0.5; 0.5] | ||
| Program satisfaction questionnaire completed: | (n = 16) | (n = 22) | |||
| High satisfaction (24+) | 8 | 50.0 | 17 | 77.3 | 27.3 [−2.8; 57.4] |
Difference in proportion of the 2 groups for binary variables and mean difference between the 2 groups for continuous variables; statistically significant differences at a type I error rate of 0.05 are in bold font.
From baseline until the end of follow up at 6 months.
Among participants with 1+ coach call, n = 23.
For all coach calls, n = 142.
Among 6-month completers, n = 38.
3.3. Acceptability
Among those who had accessed the website and completed the 6-month questionnaire, intervention and control groups had similar responses to the usability questionnaire (Table 2; detailed results in Appendix A). Participants in the intervention group were more likely to have a high satisfaction composite score on the Client Satisfaction Questionnaire (17/22, 77.3 %) compared to the control group (8/16, 50.0 %) (Table 2).
3.4. Potential effectiveness
3.4.1. Primary outcomes
Crude estimates of the observed mean scores for depression and anxiety symptoms at baseline, 3 months, and 6 months are presented in Table 3. Overall, symptom score averages were relatively low, similar between groups, and responses were not very variable over time (Table 3).
Table 3.
Crude depression and anxiety symptom scores at baseline, 3 months, and 6 months, by study group.a
| Edinburgh Postnatal Depression Scale (EPDS: 0 to 30), mean (SD) |
Generalized Anxiety Disorder (GAD-7: 0 to 21), mean (SD) |
|||
|---|---|---|---|---|
| Control (n = 15) | Intervention (n = 21) | Control (n = 15) | Intervention (n = 21) | |
| Baseline | 12.40 (2.32) | 12.19 (2.5) | 6.80 (4.26) | 7.05 (3.61) |
| 3 months | 8.67 (4.62) | 9.01 (4.15) | 4.73 (4.67) | 4.50 (4.04) |
| 6 months | 10.00 (4.34) | 7.81 (3.53) | 7.00 (4.52) | 4.33 (4.25) |
Results are for completers of all three time points (n = 36); SD: standard deviation.
In both the unadjusted and adjusted models, there were moderate differences between groups suggesting that the intervention was beneficial (Table 4). The adjusted models had higher differences between groups compared to the unadjusted models (Table 4). Because of the small sample size, the confidence intervals for the effect estimates are wide, but the majority of the values in the 95 % confidence intervals suggest a small to moderate positive effect of the intervention (Table 4). Sensitivity analyses that checked the robustness of these estimates to differential losses to follow-up found similar effect sizes, and thus there is no evidence in our data that the results were meaningfully impacted by selection bias (Appendix B).
Table 4.
Effect sizes of the intervention on symptoms of depression and anxiety at 6 months by study group.a
| Variables | Effect size [95 % confidence interval] |
|
|---|---|---|
| Edinburgh Perinatal/Postnatal Depression Scale EPDS | Generalized Anxiety Disorder GAD-7 | |
| Unadjusted | 0.45 [−0.21; 1.10] | 0.44 [−0.21; 1.10] |
| Adjusted for EPDS (<12/12+) and GAD-7 score | 0.54 [−0.11; 1.20] | 0.58 [−0.08; 1.23] |
| Adjusted for EPDS (<12/12+), GAD-7 score and immigrant | 0.51 [−0.14; 1.17] | 0.56 [−0.09; 1.22] |
| Adjusted for EPDS (<12/12+), GAD-7 score and income | 0.56 [−0.10; 1.21] | 0.54 [−0.12; 1.19] |
Results are for 6 month completers (n = 38).
4. Discussion
In this pilot RCT, a WBI accompanied by up to 7 short telephone calls by a trained lay coach was a feasible, acceptable, and potentially effective intervention for women with mild to moderate postpartum depression and/or anxiety. The coaching intervention greatly increased engagement with the website. Our results also show that trained lay coaches can deliver the coaching intervention with high fidelity, as found previously (McCusker et al., 2022).
The study sample had a high level of education (almost 90 % had university level education) and 62 % were immigrants to Canada; these characteristics limit the generalizability of the results to the target population of the community served by the hospital that we recruited from and to the greater Montreal population. Recruiting participants from the post-partum unit in the hospital did not pose difficulties. However, having participants consent online once they were discharged resulted in a low consent rate. Further research is needed on how best to recruit participants to a larger study.
While our estimates of effectiveness of the coaching intervention are imprecise, they indicated a trend towards a moderate positive effect of the lay coaching and WBI intervention on symptoms of depression and anxiety. This suggests that coaching calls can not only augment the use of WBIs among participants with postpartum depression and/or anxiety but may also increase their effectiveness.
4.1. Comparison with prior work
This is the first RCT to our knowledge to examine the incremental effectiveness of coaching calls when paired with a WBI to support people with postpartum depression and/or anxiety. This study is also important in its focus on people with mild to moderate symptoms who may not be recognized by clinicians, as systematic screening is not currently done. People that have recently given birth but have less severe symptoms may have more difficulty accessing appropriate services that are more readily available to patients with severe symptoms. Prior self-guided WBIs targeting perinatal depression and anxiety have been challenged by suboptimal user engagement (Loughnan et al., 2019). Our results on potential effectiveness are also consistent with previous studies on WBIs coupled with human support for postnatal depression, which indicated clinically significant effects of such interventions compared to treatment as usual (that is, where the control group did not have access to the WBI) (Milgrom et al., 2016; Pugh et al., 2016).
4.2. Limitations
At least four study limitations should be considered. First, effect estimates for the intervention's effect on EPDS and GAD-7 were imprecise due to the small sample size and limit conclusions about the comparative effectiveness of the two methods of delivering the WBI. Further, the small sample size led to a baseline imbalance on important covariates between groups, which could potentially confound our results, although we adjusted for these covariates and the differences between effect estimates in our adjusted and unadjusted models were small. Still, the small sample size increases the chance of imbalances between groups on unmeasured confounders. Second, losses to follow up were significant and differed between intervention and control groups. Although our sensitivity analyses confirmed the robustness of our estimates to this potential selection bias based on measured predictors of loss to follow-up, these methods cannot account for unmeasured variables that may predict censoring. Third, the nature of the intervention made it impossible for participants to be blinded. Finally, the study sample is likely not representative of the target population as mentioned above, and thus our results may not be generalizable to the population served by the hospital that we recruited in, nor the broader Montreal community.
4.3. Relevance to clinical practice
Telephone coaching with a WBI could fill a service gap for parents with mild to moderate postpartum depression and/or anxiety, whose conditions may not be recognized by clinicians, and who may have difficulty accessing appropriate services. We designed the intervention to facilitate access to treatment, considering barriers such as lack of time and transportation, based on the results of our previous needs assessment (Schwartz et al., 2021). If found effective in a subsequent larger scale RCT, this intervention may be a safe and cost-effective treatment option to augment existing mental health services for postpartum populations. For example, it can also be used as a low intensity first step in a stepped-care approach to mental health treatment (van Straten et al., 2015). This study augments the evidence base on use of lay telephone coaching to treat mental health disorders (McCusker et al., 2022; Lambert et al., 2021).
4.4. Conclusions
Our results show that brief telephone coaching by trained lay coaches coupled with a WBI is a feasible and acceptable intervention for postpartum depression and/or anxiety. Compared to a WBI alone, this intervention is potentially effective in reducing symptoms of depression and anxiety at 6 months. Lay coaching and WBIs are scalable and relatively inexpensive interventions that offer an alternative to often more expensive and less accessible mental health treatment services. A larger trial which is adequately powered to investigate the effectiveness of such an intervention is warranted.
Abbreviations
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We would like to acknowledge the support of Jocelyne Paul B.SC.N, as well as the Obstetrics Team on the post-partum unit at St. Mary's Hospital Center.
Funding
This work was supported by the Royal Bank of Canada.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2022.100597.
Appendix A. Supplementary data
Supplementary material
References
- Alegria M., Carson N., Flores M., Li X., Shi P., Lessios A.S., Polo A., Allen M., Fierro M., Interian A., Jimenez A., La Roche M., Lee C., Lewis-Fernandez R., Livas-Stein G., Safar L., Schuman C., Storey J., Shrout P.E. Activation, self-management, engagement, and retention in behavioral health care: a randomized clinical trial of the DECIDE intervention. JAMA Psychiatry. 2014;71:557–565. doi: 10.1001/jamapsychiatry.2013.4519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhaldi G., Hamilton F.L., Lau R., Webster R., Michie S., Murray E. The effectiveness of prompts to promote engagement with digital interventions: a systematic review. J. Med. Internet Res. 2016;18 doi: 10.2196/jmir.4790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badker R., Misri S. Mindfulness-based therapy in the perinatal period: a review of the literature. B. C. Med. J. 2017;59:18–21. [Google Scholar]
- Barrera A.Z., Wickham R.E., Munoz R.F. Online prevention of postpartum depression for spanish- and english-speaking pregnant women: a pilot randomized controlled trial. Internet Interv. 2015;2:257–265. doi: 10.1016/j.invent.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister H., Reichler L., Munzinger M., Lin J. The impact of guidance on internet-based mental health interventions : a systematic review. Internet Interv. 2014;1:205–215. [Google Scholar]
- Beck J., Beck A. Guilford Press; New York NY: 1995. Cognitive Therapy : Basics and Beyond. [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J., Rothstein H. John Wiley & Sons Ltd.; 2009. Introduction to Meta-analysis. [Google Scholar]
- Branquinho M., Rodriguez-Munoz M.F., Maia B.R., Marques M., Matos M., Osma J., Moreno-Peral P., Conejo-Ceron S., Fonseca A., Vousoura E. Effectiveness of psychological interventions in the treatment of perinatal depression: a systematic review of systematic reviews and meta-analyses. J. Affect. Disord. 2021;291:294–306. doi: 10.1016/j.jad.2021.05.010. [DOI] [PubMed] [Google Scholar]
- Canadian Community Health Survey (Chs) Statistics Canada; 2012. Mental Health: Questionnaire. [Database on the Internet] [Online] 2012. November 26, 2021. [Accessed] [Google Scholar]
- Chasan-Taber L., Silveira M., Marcus B.H., Braun B., Stanek E., Markenson G. Feasibility and efficacy of a physical activity intervention among pregnant women: the behaviors affecting baby and you (B.A.B.Y.) study. J. Phys. Act. Health. 2011;8(Suppl. 2):S228–S238. doi: 10.1123/jpah.8.s2.s228. [DOI] [PubMed] [Google Scholar]
- Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Da Costa D., Zelkowitz P., Bailey K., Cruz R., Bernard J.C., Dasgupta K., Lowensteyn I., Khalife S. Results of a needs assessment to guide the development of a website to enhance emotional wellness and healthy behaviors during pregnancy. J. Perinat. Educ. 2015;24:213–224. doi: 10.1891/1058-1243.24.4.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Graaf L.E., Huibers M.J., Riper H., Gerhards S.A., Arntz A. Use and acceptability of unsupported online computerized cognitive behavioral therapy for depression and associations with clinical outcome. J. Affect. Disord. 2009;116:227–231. doi: 10.1016/j.jad.2008.12.009. [DOI] [PubMed] [Google Scholar]
- Dennis C.L., Falah-Hassani K., Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br. J. Psychiatry. 2017;210:315–323. doi: 10.1192/bjp.bp.116.187179. [DOI] [PubMed] [Google Scholar]
- Donkin L., Hickie I.B., Christensen H., Naismith S.L., Neal B., Cockayne N.L., Glozier N. Rethinking the dose-response relationship between usage and outcome in an online intervention for depression: randomized controlled trial. J. Med. Internet Res. 2013;15 doi: 10.2196/jmir.2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enrique A., Palacios J.E., Ryan H., Richards D. Exploring the relationship between usage and outcomes of an internet-based intervention for individuals with depressive symptoms: secondary analysis of data from a randomized controlled trial. J. Med. Internet Res. 2019;21 doi: 10.2196/12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. The law of attrition. J. Med. Internet Res. 2005;7 doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbrother N., Janssen P., Antony M.M., Tucker E., Young A.H. Perinatal anxiety disorder prevalence and incidence. J. Affect. Disord. 2016;200:148–155. doi: 10.1016/j.jad.2015.12.082. [DOI] [PubMed] [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev. 2010;33:1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaston A., Cramp A., Prapavessis H. Enhancing self-efficacy and exercise readiness in pregnant women. Psychol. Sport Exerc. 2012;13:550–557. [Google Scholar]
- Griffin S.J., Kinmonth A.L., Veltman M.W., Gillard S., Grant J., Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann. Fam. Med. 2004;2:595–608. doi: 10.1370/afm.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haga S.M., Drozd F., Brendryen H., Slinning K. Mamma mia: a feasibility study of a web-based intervention to reduce the risk of postpartum depression and enhance subjective well-being. JMIR Res. Protoc. 2013;2 doi: 10.2196/resprot.2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Canada . Government of Canada; Ontawa ON: 2007. Eating Well with Canada's Food Guide: A Resource for Educators and Communicators. [Google Scholar]
- Health Canada . 2010. Prenatal Nutrition Guidelines for Health Professionals: Gestational Weight Gain, Ottawa ON. [Google Scholar]
- Hedges L. In: The Handbook of Research Synthesis and Meta-Analysis. 2nded. Cooper H., Hedges L., Valentine J., editors. Russell Sage Foundation; 2009. Effect sizes in nested designs. [Google Scholar]
- Lachenbruch P., Cohen J. Statistical power analysis for the behavioral sciences. J. Am. Stat. Assoc. 1989;84:1096. [Google Scholar]
- Lambert S., Grover S., Laizner A.M., McCusker J., Belzile E., Moodie E.E.M., Kayser J.W., Lowensteyn I., Vallis M., Walker M., Da Costa D., Pilote L., Ibberson C., De Raad M. Adaptive web-based stress management programs among adults with a cardiovascular disease: a pilot sequential multiple assignment randomized trial (SMART) Patient Educ. Couns. 2021;105:1587–1597. doi: 10.1016/j.pec.2021.10.020. [DOI] [PubMed] [Google Scholar]
- Lee K.A., Gay C.L. Can modifications to the bedroom environment improve the sleep of new parents? Two randomized controlled trials. Res. Nurs. Health. 2011;34:7–19. doi: 10.1002/nur.20413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E.W., Denison F.C., Hor K., Reynolds R.M. Web-based interventions for prevention and treatment of perinatal mood disorders: a systematic review. BMC Pregnancy Childbirth. 2016;16:38. doi: 10.1186/s12884-016-0831-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loughnan S.A., Joubert A.E., Grierson A., Andrews G., Newby J.M. Internet-delivered psychological interventions for clinical anxiety and depression in perinatal women: a systematic review and meta-analysis. Arch. Womens Ment. Health. 2019;22:737–750. doi: 10.1007/s00737-019-00961-9. [DOI] [PubMed] [Google Scholar]
- Martins C., Gaffan E.A. Effects of early maternal depression on patterns of infant-mother attachment: a meta-analytic investigation. J. Child Psychol. Psychiatry. 2000;41:737–746. [PubMed] [Google Scholar]
- McCusker J., Lambert S.D., Ciampi A., Jones J.M., Li M., Yaffe M.J., Pelland M.E., Belzile E., De Raad M. Trained lay coaches and self-care cognitive-behavioral tools improve depression outcomes. Patient Educ. Couns. 2022;105:2747–2756. doi: 10.1016/j.pec.2022.03.021. [DOI] [PubMed] [Google Scholar]
- Milgrom J., Danaher B.G., Gemmill A.W., Holt C., Holt C.J., Seeley J.R., Tyler M.S., Ross J., Ericksen J. Internet cognitive behavioral therapy for women with postnatal depression: a randomized controlled trial of MumMoodBooster. J. Med. Internet Res. 2016;18 doi: 10.2196/jmir.4993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Hopewell S., Schulz K.F., Montori V., Gotzsche P.C., Devereaux P.J., Elbourne D., Egger M., Altman D.G. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012;10:28–55. doi: 10.1016/j.ijsu.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Mohr D.C., Cuijpers P., Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J. Med. Internet Res. 2011;13 doi: 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moroz N., Moroz I., D'angelo M.S. Mental health services in Canada: barriers and cost-effective solutions to increase access. Healthc. Manage. Forum. 2020;33:282–287. doi: 10.1177/0840470420933911. [DOI] [PubMed] [Google Scholar]
- National Institute for Clinical Excellence . 2007. Antenatal and Postnatal Health: Clinical Management and Service Guidelines, London UK. [Google Scholar]
- O'Mahen H.A., Richards D.A., Woodford J., Wilkinson E., Mcginley J., Taylor R.S., Warren F.C. Netmums: a phase II randomized controlled trial of a guided internet behavioural activation treatment for postpartum depression. Psychol. Med. 2014;44:1675–1689. doi: 10.1017/S0033291713002092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugh N.E., Hadjistavropoulos H.D., Dirkse D. A randomised controlled trial of therapist-assisted, Internet-delivered cognitive behavior therapy for women with maternal depression. Plos One. 2016:11. doi: 10.1371/journal.pone.0149186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renfrew M.E., Morton D.P., Morton J.K., Przybylko G. The influence of human support on the effectiveness of digital mental health promotion interventions for the general population. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.716106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ride J., Lancsar E. Women's preferences for treatment of perinatal depression and anxiety: a discrete choice experiment. PLoS One. 2016;11 doi: 10.1371/journal.pone.0156629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson T.N., Patrick K., Eng T.R., Gustafson D. An evidence-based approach to interactive health communication: a challenge to medicine in the information age. Science panel on interactive communication and health. JAMA. 1998;280:1264–1269. doi: 10.1001/jama.280.14.1264. [DOI] [PubMed] [Google Scholar]
- Ryan C., Bergin M., Wells J.S. Theoretical perspectives of adherence to web-based interventions: a scoping review. Int. J. Behav. Med. 2018;25:17–29. doi: 10.1007/s12529-017-9678-8. [DOI] [PubMed] [Google Scholar]
- Schwartz H., McCusker J., Law S., Zelkowitz P., Somera J., Singh S. Perinatal mental healthcare needs among women at a community hospital. J. Obstet. Gynaecol. Can. 2021;43(322–328) doi: 10.1016/j.jogc.2020.08.015. [DOI] [PubMed] [Google Scholar]
- Stremler R., Hodnett E., Kenton L., Lee K., Weiss S., Weston J., Willan A. Effect of behavioural-educational intervention on sleep for primiparous women and their infants in early postpartum: multisite randomised controlled trial. BMJ. 2013;346 doi: 10.1136/bmj.f1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of California . 2016. SMART Goals: A How to Guide. [Google Scholar]
- Van Straten A., Hill J., Richards D.A., Cuijpers P. Stepped care treatment delivery for depression: a systematic review and meta-analysis. Psychol. Med. 2015;45:231–246. doi: 10.1017/S0033291714000701. [DOI] [PubMed] [Google Scholar]
- Whitehead A.L., Julious S.A., Cooper C.L., Campbell M.J. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat. Methods Med. Res. 2016;25:1057–1073. doi: 10.1177/0962280215588241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J. BC Reproductive Mental Health; Vancouver, BC: 2014. Best Practice Guidelines for Mental Health Disorders in the Perinatal Period. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material