Abstract
Patients with an acute subdural hematoma (aSDH) usually have a history of head trauma, but some patients may present with spontaneous aSDH due to a ruptured aneurysm. Spontaneous aSDH is a rare manifestation of aneurysmal rupture. However, aneurysmal rupture remains a major cause of spontaneous aSDH. A 42-year-old man was brought to the emergency room because of a sudden loss of consciousness during sexual intercourse. The patient has seizures and weakness on the right side of his body. The patient has no history of trauma and has never taken anticoagulant or antiplatelet drugs, sexual aphrodisiacs, or other drugs. Physical examination revealed the Glasgow Coma Scale of E2V1M3, ptosis on the left eye, left pupil mydriasis, right central facial palsy, and right hemiparesis. Laboratory results showed hypercoagulopathy. Noncontrast head computed tomography scan revealed subdural hematoma with no subarachnoid or intraparenchymal hemorrhage. The patient underwent an emergency craniotomy, and the hematoma was evacuated. Cerebral angiography was performed 1 week later, revealing a saccular aneurysm in the left posterior communicating artery. The patient has successfully undergone endovascular coiling and was discharged from the hospital in good condition, fully conscious, with no weakness in half side of the body, but there is still third nerve palsy. Patients with pure aSDH without a history of trauma should consider the possibility of aneurysm rupture and perform an angiographic examination to rule out vascular malformations so that the patient can receive appropriate treatment.
Keywords: Acute subdural hematoma, Ruptured aneurysm, Cerebral angiography
Introduction
Patients with an acute subdural hematoma (aSDH) usually have a history of head trauma [1]. However, some patients may present with spontaneous aSDH due to a ruptured aneurysm [2]. The incidence of aSDH due to a ruptured intracranial aneurysm is approximately 8% [3]. Manifestations of ruptured intracranial aneurysms are often associated with subarachnoid or intraparenchymal hemorrhage [3]. The prevalence of isolated aSDHs without intraparenchymal or subarachnoid hemorrhage is very low [3,4]. Pure aSDH due to an aneurysm is often caused by a rupture of the posterior communicating artery [1]. Several conditions have been reported causing spontaneous aSDH arteriovenous malformation [5], cerebral venous sinus thrombosis [6], Moyamoya disease [7], coagulopathy [8,9], leukemia [10], meningiomas [11], metastatic lesions [12].
In this case report, we report a ruptured posterior communicating artery aneurysm that manifests as pure aSDH.
Case report
A 42-year-old male patient presented to the emergency room because of a sudden loss of consciousness 3 hours before admission during sexual intercourse. The patient also vomited once and got weakness on the right side of the body. The patient has status focal to bilateral tonic-clonic seizures on the way to the hospital. There were no previous headaches.
The patient's wife disregarded that the patient's left eyelid had closed slightly 2 months ago. The patient has no history of trauma and has never taken anticoagulant or antiplatelet drugs, sexual aphrodisiacs, or other drugs.
Physical examination revealed his blood pressure was 183/105 mm Hg. He had a Glasgow Coma Scale of E2V1M3, ptosis on the left eye, left pupil mydriasis, right central facial palsy, and right hemiparesis.
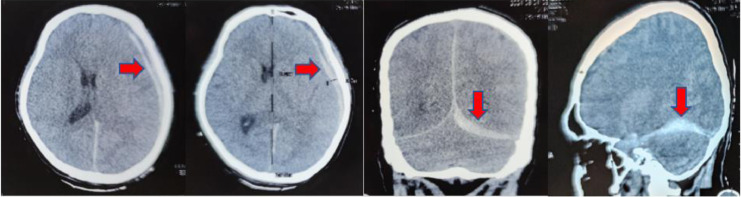
Laboratory results showed hypercoagulopathy with a D-dimer value of 4020. Noncontrast head computed tomography (CT) scan revealed subdural hematoma in the left hemisphere region, cerebral falx, and left cerebellar tentorium. The maximum hematomal thickness of 1 cm, causing a 0.4 cm midline shift, brain edema. No fracture line was seen, subarachnoid or intraparenchymal hemorrhage (Fig. 1).
Fig. 1.
A left-sided acute subdural hematoma (arrow) with midline shift is visible on computed tomography scans, but there is no subarachnoid hemorrhage.
The patient received antiseizure medication phenytoin and an urgent craniotomy hematoma evacuation. Due to the patient having an aSDH spontaneously, he underwent cerebral angiography 1 week later. Cerebral angiography revealed a saccular aneurysm on the left posterior communicating artery with neck size 0.8 mm, dome 9.7 × 9.6 mm pointing true posterior (Fig. 2A). According to 3-dimensional angiography, the aneurysm had an uneven shape and had extra minor outpouchings that indicated where it had ruptured (Fig. 2B). The man has successfully undergone endovascular coiling (Fig. 3). After treatment, the patient was well conscious, with no weakness in the right side of the body, but only paralysis of the third nerve in the left eye.
Fig. 2.
(A) Digital subtraction angiography on day 7th after craniotomy. Angiography represents a saccular aneurysm on the left posterior communicating artery with neck size 0.8 mm, dome 9.7 × 9.6 mm pointing true posterior. (B) Three-dimensional angiography showed the aneurysm had an uneven shape and had extra minor outpouchings that indicated where it had ruptured.
Fig. 3.
Left carotid angiography after coiling on day 7th after craniotomy shows that the aneurysm has been occluded.
Discussion
Spontaneous aSDH is a rare manifestation of aneurysmal rupture. However, aneurysmal rupture remains a major cause of spontaneous aSDH [13]. Therefore, it is necessary to consider the possibility of aneurysm rupture in people with aSDH who do not have a history of trauma, as in this case.
There are differences in the appearance of a brain CT scan of a subdural hematoma due to trauma compared to a ruptured aneurysm. In traumatic aSDH, the hematoma could appear in lentiform, iso or hypodense, or crescent-shaped. The aneurysm-related subdural hematoma appeared as hyperdense, one-sided, and triangular or curved over the Sylvian fissure [14]. A subdural hematoma caused by aneurysmal rupture is usually followed by subarachnoid hemorrhage (SAH), intracerebral hemorrhage (ICH), or intraventricular hemorrhage (IVH) extension [14]. However, in this case, pure aSDH was obtained.
Several mechanisms explain the occurrence of pure aSDH, including (1) aneurysm rupture attached to the tentorium or falx, (2) cortical aneurysm rupture, (3) aneurysm rupture caused by a bleeding spot in the petroclinoid fold, (4) rupture of a cortical artery aneurysm that protrudes through the arachnoid, (5) aneurysm rupture that extends into the subdural space [4]. Whereas the mechanism of aSDH accompanied by subarachnoid hemorrhage or intraparenchymal hemorrhage includes: (1) Massive cerebral bleeding tears the arachnoid membrane and ruptures through the cortex, allowing blood to flow into the subdural area; (2) The final rupture happens into the subdural area when the sentinel hemorrhage creates adhesions between the aneurysm and arachnoid; (3) A weak spot deep within the arachnoid can allow high-pressure blood flow from a leaky aneurysm to enter the subdural region [4].
The posterior communicating artery was the site of the aneurysm most frequently presenting pure aSDH (58.3%), followed by the distal anterior cerebral artery (16.7%), and the middle cerebral artery (12.5%) [15]. Patients with aSDH with suspected aneurysm rupture usually require imaging, including digital subtraction angiography, magnetic resonance angiography, or computed tomographic angiography [2].
Initial preoperative angiographic examination for nontraumatic aSDH is debatable [1]. The decision was made depending on the patient's neurologic status, history of trauma, coagulopathy, and ICH and SAH in brain CT scan [1]. If the patient presents with a stable neurologic condition, computed tomographic angiography should be done before surgery [1]. However, immediate decompression surgery will be performed if the patient presents with rapid clinical deterioration (as in this case) [1]. Postoperative angiography is necessary to rule out vascular abnormalities if no source of bleeding can be found after surgery [1]. In our case, cerebral angiography and endovascular coiling were performed 1 week after surgery. aSDH due to aneurysmal bleeding accompanied by SAH has a poor prognosis on discharge or within 3 months [16]. In this case, the patient had aSDH without SAH, so with prompt and appropriate treatment, the patient had a better prognosis and was discharged from the hospital with GCS 15, with no hemiparesis and only left paralysis of the third nerve of the left eye.
Conclusion
It is uncommon to have a spontaneous aSDH without intraparenchymal or subarachnoid hemorrhage. Individuals with pure aSDH with no prior history of trauma should consider aneurysm rupture and perform an angiographic examination to rule out vascular malformations. The angiographic examination could rule out other aSDH causes, and the patient can receive appropriate treatment.
Patient consent
Written informed consent for the publication of this case report was obtained from a relative of the patient.
Footnotes
Acknowledgments: The authors would like to thank all lecturers, family, and friends who have taught and supported us. The authors declared that no grants were involved in supporting this work.
Competing Interests: All authors declare no conflicts of interest.
Provenance and peer review: Not commissioned, externally peer-reviewed.
References
- 1.Mrfka M, Pistracher K, Augustin M, Kurschel-Lackner S, Mokry M. Acute subdural hematoma without subarachnoid hemorrhage or intraparenchymal hematoma caused by rupture of a posterior communicating artery aneurysm: case report and review of the literature. J Emerg Med. 2013;44:e369–e373. doi: 10.1016/j.jemermed.2012.11.073. [DOI] [PubMed] [Google Scholar]
- 2.Abecassis ZA, Nistal DA, Abecassis IJ, Sen RD, Levitt MR. Ghost aneurysms in acute subdural hematomas: a report of two cases. World Neurosurg. 2020;139:e159–e165. doi: 10.1016/j.wneu.2020.03.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Abdulwahhab AH, Al-Sharydah AM, Al-Suhibani SS, Almulhim AS, Al-Dhafeeri OM, Al-Jubran SA. A ruptured posterior communicating artery aneurysm presenting as tentorial and spinal isolated subdural hemorrhage: a case report and literature review. BMC Neurol. 2020;20:1–7. doi: 10.1186/s12883-020-01682-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marbacher S, Fandino J, Lukes A. Acute subdural hematoma from ruptured cerebral aneurysm. Acta Neurochir (Wien) 2010;152:501–506. doi: 10.1007/s00701-009-0521-0. [DOI] [PubMed] [Google Scholar]
- 5.Choi HJ, Lee Il J, Nam KH, Ko JK. Acute spontaneous subdural hematoma due to rupture of a tiny cortical arteriovenous malformation. J Korean Neurosurg Soc. 2015;58:547–549. doi: 10.3340/jkns.2015.58.6.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bansal H, Chaudhary A, Mahajan A, Paul B. Acute subdural hematoma secondary to cerebral venous sinus thrombosis: case report and review of literature. Asian J Neurosurg. 2016;11:177. doi: 10.4103/1793-5482.175632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vijayasaradhi M, Prasad V. Moyamoya disease presenting as bilateral acute subdural hematomas without deficits. Asian J Neurosurg. 2017;12:228–231. doi: 10.4103/1793-5482.149997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Depreitere B, Van Calenbergh F, Van Loon J, Mendelow AD. A clinical comparison of non-traumatic acute subdural haematomas either related to coagulopathy or of arterial origin without coagulopathy. Acta Neurochir (Wien) 2003;145:541–546. doi: 10.1007/s00701-003-0020-7. [DOI] [PubMed] [Google Scholar]
- 9.Garbossa D, Altieri R, Calamo Specchia F, Agnoletti A, Pilloni G, Lanotte M, et al. Are acute subdural hematomas possible without head trauma? Asian J Neurosurg. 2014;9:218–222. doi: 10.4103/1793-5482.146612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiong X, Li Q, Yang WS, Wei X, Hu X, Wang XC, et al. Comparison of swirl sign and black hole sign in predicting early hematoma growth in patients with spontaneous intracerebral hemorrhage. Med Sci Monit. 2018;24:567–573. doi: 10.12659/MSM.906708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alghabban FA, Alhamss YJ, Farag AA, Alfahmi JA, SA Al-saiari, Alghamdi F, et al. Incidental intraoperative finding of meningioma in spontaneous acute subdural hematoma: a case report from Saudi Arabia and review of literature. Int J Surg Case Rep. 2020;77:314–317. doi: 10.1016/j.ijscr.2020.10.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chye CL, Lin KH, Ou CH, Sun CK, Chang IW, Liang CL. Acute spontaneous subdural hematoma caused by skull metastasis of hepatocellular carcinoma: case report. BMC Surg. 2015;15:1–4. doi: 10.1186/s12893-015-0045-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beucler N, Haikal C, Hibbert D, Sellier A, Joubert C, Desse N, et al. Spontaneous acute subdural hematoma: beware of the aneurysm. J Neurosci Rural Pract. 2019;10:537–541. doi: 10.1055/s-0039-1697770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmad S, Rashid U, Akhtar S, Churojana A, Yasin Mansour O, Akmal M. Spontaneous acute subdural haemorrhage with rupture of distal anterior cerebral artery aneurysm: a case report and review of literature. Interdiscip Neurosurg Adv Tech Case Manag. 2021;25 doi: 10.1016/j.inat.2021.101142. [DOI] [Google Scholar]
- 15.Koerbel A, Ernemann U, Freudenstein D. Acute subdural haematoma without subarachnoid haemorrhage caused by rupture of an internal carotid artery bifurcation aneurysm: case report and review of literature. Br J Radiol. 2005;78:646–650. doi: 10.1259/bjr/60601877. [DOI] [PubMed] [Google Scholar]
- 16.Biesbroek JM, Van Der Sprenkel JWB, Algra A, Rinkel GJE. Prognosis of acute subdural haematoma from intracranial aneurysm rupture. J Neurol Neurosurg Psychiatry. 2013;84:254–257. doi: 10.1136/jnnp-2011-302139. [DOI] [PubMed] [Google Scholar]