Highlights
-
•
There is little guidance for physical therapists on how best to provide first line care for people with low back pain.
-
•
Providing validation to patients seems important.
-
•
The AxEL-Q is a valid and reliable tool that could help to guide physical therapy consultations.
-
•
Physical therapists could consider focusing patient education and advice on messages about cause, severity, and imaging, and in doing so remove barriers to physical activity.
Keywords: Attitude, Behavioural change, First-line care, Self-management, Validation
Abstract
Background
The first-line treatment consistently recommended for people with low back pain is patient education and advice. Regardless of the duration of low back pain, clinicians should provide education on the benign nature of low back pain, reassurance about the absence of a serious medical condition, and advice to remain active. There is little guidance on how best to provide this care.
Objective
This Masterclass will draw on recent evidence to explore how physical therapy clinicians could deliver person-centred education and advice to people with low back pain to refine their clinical consultation.
Discussion
First, we highlight the potential value of providing validation to acknowledge the distressing experience and consequences of low back pain. Second, we describe a tool to open channels of communication to provide education and advice in a patient-centred and efficient way. Clinicians could consider using the Attitude toward Education and advice for Low back pain Questionnaire to gain an insight into patient attitudes toward education and advice at the outset of a clinical encounter. Finally, we provide options for tailoring patient education and advice to promote self-management of low back pain based on patient attitudes. We present evidence that a positive attitude toward messages about causes rather than messages about physical activity predicts intention to self-manage low back pain. We combine this evidence to suggest a pathway for clinicians to provide education and advice to people with low back pain within the time constraints of a clinical consultation.
Introduction
Low back pain is common and burdensome. The point prevalence of activity-limiting low back pain lasting more than one day is 7.8%, meaning that approximately 577 million people experience low back pain at any one time across the world.1 Many people with low back pain seek care to manage their problem; a systematic review of 14 studies found that 47 to 67% of people with low back pain seek care annually, and 30% have sought care within the past month.2 Although spending on health services has increased, outcomes for people with low back pain are not improving.3
Clinical practice guidelines aim to assist clinicians in providing high-value care to people presenting with low back pain. High-value care is providing care with the optimal outcome for the person's circumstance delivered at the right price.4 After screening for clinical features of serious pathology and conducting a physical and psychological assessment, regardless of the duration of low back pain, the first-line treatment consistently recommended is patient education and advice.5,6 However, systematic reviews have highlighted a gap between clinical practice guideline recommendations for care and the care that is actually provided in practice.7,8 For example, people presenting for care with low back pain commonly receive unnecessary diagnostic imaging9 or a high number of treatments known to provide little or no benefit and cause harm such as opioids,10 antidepressants,11,12 muscle relaxants,13 and spinal fusion surgery.14 These services provide minimal or no benefit, considering the harms, the costs, alternatives, and the preferences of the patient, and are classified as ‘low-value’ care.15
Clinicians commonly report that a desire to maintain a harmonious relationship with patients and the time constraints of clinical practice are important barriers to providing high-value care, such as education and advice to people presenting with low back pain.16 In this Masterclass, we will introduce new evidence on strategies to help physical therapists overcome these barriers to providing high-value care. First, we highlight the potential value of providing validation to nurture a harmonious relationship. Second, we will describe a tool to open channels of communication to provide education and advice in a patient-centred and efficient way. Finally, we provide options for tailoring patient education and advice to promote self-management of low back pain based on patient attitudes to maximise the time available in clinical consultations.
Nurturing person-centred care
Shared decision making is at the heart of person-centred care
A cornerstone of modern healthcare is to include people in their care decisions.17 For effective shared decision making, clinicians should share information on treatment options and their potential outcomes including risks and benefits, based on the best research evidence. In turn, the person is encouraged to provide an insight into the personal burden of low back pain and express their treatment preferences and values.18 However, too often, the person's voice is left out of the decision-making process, and patients feel dismissed and invalidated by their health care professional.19,20 Ethnographic observations and face-to-face interviews with patients in a complex care management program observed that patients with chronic musculoskeletal pain required a long period of relationship- and trust-building before they were willing to engage with health care professionals’ recommendations.21 During interviews, the patients admitted that they felt marginalised and mistrusted the clinicians, which affected their willingness to engage with the intervention.21 A phenomenological analysis of patients admitted to hospital with acute low back pain provided an insight into patients’ experience of severe pain, disability, and helplessness, feelings that manifested in a desire for validation and cynicism toward health professionals who were perceived as attempting to minimise the severity of their condition.22 Together, these findings suggest that patients may not feel supported to discuss their preferences and values with health care professionals in a clinical consultation, which may disrupt the shared decision-making process.
Experience of back pain expressed on social media
Exploring social media interactions could provide valuable clinical information not otherwise disclosed in consultation with a health care provider. We conducted a content analysis to understand what people post on social media relative to low back pain to enhance our understanding of the personal burden of low back pain and peoples’ expectations for managing their problem.23 Social media is a contemporary forum for computer-based disclosure,24 that provides the advantage of access and perceived anonymity,25 allowing people to communicate their views and experiences about low back pain independent of health care professionals.26,27 We identified two main themes; the first theme, from the status broadcasts, "Hear my pain", suggests that people with low back pain seem to use social media to seek validation and share their experiences. The second theme, from the responses, "I feel for you", suggests that social media is used to share support for people with low back pain. A third main finding related to what was not said, there were no public responses to over three-quarters of the status broadcasts about low back pain.
One interpretation of these findings is that there may be gaps in our understanding of the personal burden of low back pain and its impact. These results suggest that people want to feel validated; one potential reason for using social media is due to feeling dismissed or invalidated by clinicians, which is incongruent with person-centred care.
The role of validation
Providing validation seems important for people presenting with low back pain, but potentially absent from clinical consultations.28 A meta-ethnography of 38 qualitative studies exploring the experience of low back pain found that seeking validation is common.29 Validation seems particularly relevant for people with low back pain as they feel that others question the legitimacy of their 'invisible' pain.30 Health professionals who manage patients with pain admit to treating patients differently depending on whether or not they have a biomedical diagnosis.31 Validation is a process in which the listener communicates an understanding and legitimacy of a patient's experiences, feelings, actions, and worries.32 The effect of communicating validation or invalidation on worry, treatment adherence, and pain intensity was investigated in a randomised controlled experiment. Those authors report that trust and engagement were nurtured in the validating encounter, positively impacting treatment adherence and patient satisfaction.33 A second randomised controlled experiment (n = 28) where participants were interviewed about pain found that participants in the validated group reported greater satisfaction with the interview than the invalidated group.34 Validation was also the focus of two topical reviews: The first highlighted the potential value of providing validation to reduce the incidence of pain behaviours, leading to reductions in physical disability and psychological distress.35 The second review reported that when patients do not feel validated, it can lead to greater disability as patients increase their efforts to convince the other person that their pain symptoms are real.36 Cross-sectional studies that used questionnaires to measure stigma in people with low back pain reported that patients often feel dismissed and invalidated by health care professionals,19 findings echoed in qualitative data from interviews of people attending primary care with low back pain.20 There are no trials that investigate the effect of providing validation on pain and disability in people with low back pain. However, the above evidence suggests that providing validation could improve patient satisfaction and engagement, and support shared decision making.
Physical therapists clinical implication: validation
Physical therapists should attempt to validate their patients, it is important to people with low back pain. Validating communication does not prolong the length of the consultation.37 Recent early evidence suggests that health professionals can be trained to provide validation within the time frame of a clinical consultation.38 To support validation, physical therapists could begin a clinical consultation by allowing the patient time to tell their story while acknowledging the distressing experiences and consequences of low back pain. Examples of validating communication are active listening, including summaries and reflections on what the person has said, including empathic statements like “that must have been hard”, “I can see you are experiencing a lot of pain”, posing follow-up questions, and using appropriate body language (such as leaning forward, looking at the person, nodding when agreeing and smiling).34
Enhancing clinical communication
Communication of patient education and advice
Providing patient education and advice relies on effective communication. Effective communication uses a mix of open and closed questions, seeks permission, explains rationales for approaches, uses the persons own narrative and lived experience to reflect back to them, and is at the heart of person-centred care.39 However, effective communication is undervalued by clinicians and perceived as time inefficient.40 A qualitative synthesis of thirty studies reported barriers and facilitators to physician-patient communication. Lack of time and resources were explicitly identified as barriers to effective communication along with tensions between physician–patient understandings of medical concerns and social stressors.40 Time constraints may prevent the clinician from attempting to provide education and advice or may manifest as a consultation feeling rushed and the patient not feeling validated.41 Feeling rushed could contribute to people with low back pain perceiving clinicians as insufficient at expressing empathy,42 even uncaring.31,43 This perception is incongruent with person centred-care.
Components of patient education and advice
Some guidance on the information that could be prioritised in a patient education and advice intervention for low back pain was provided in a recent Delphi study.44 In this study a panel of expert researchers, clinicians, and consumers with low back pain reached consensus on a set of evidence-based key messages for people with low back pain. These key messages were related to; staying active, identifying the rare, serious causes of low back pain, reassurance, unnecessary interventions, principles of management, and disease knowledge.44 Examples of the key messages include "Hurt does not necessarily mean harm", and "Take ownership of your own wellbeing".
The role of attitudes
Social psychologists have studied attitude as a "behavioural disposition" for decades.45 A behavioural disposition is a tendency toward a particular act.45 Ajzen's theory of planned behaviour proposed that attitude towards a behaviour is the best predictor of a behavioural intention, which is in turn the proximal determinant of actual behaviour.46 In a systematic review, researchers investigated whether changing attitudes, norms, or self-efficacy led to changes in intentions and behaviour by synthesising findings from 204 experimental studies. In the included studies, participants were randomly assigned to a treatment that increased the respective cognition compared to a control condition and differences in later intentions or behaviour were measured. The authors reported that interventions that experimentally induced changes in attitudes, norms, and self-efficacy led to moderately-sized changes in intention and small to moderately-sized changes in health behaviour.47 Attitudes towards health educational messages have been shown to predict behaviours such as condom use48 and breast cancer screening.49 For people with low back pain, adherence to first-line care is influenced by their expectations for treatment and attitudes towards the specific health care behaviour.50,51
A tool to enhance the clinical utility of patient education and advice
A questionnaire to understand patient attitudes toward messages of patient education and advice such as those identified in the Delphi study, could enable clinicians to provide more efficient consultations within the time constraints of clinical practice. Questionnaires are available to evaluate attitudes or beliefs related to the experience of having low back pain, for example, the Pain and Impairment Relationship Scale (PAIRS),52 the Survey of Pain Attitudes (SOPA), and the Back Pain Attitude Questionnaire.53 Evaluation of the measurement properties suggests that each questionnaire demonstrates adequate internal consistency, test re-test stability, and hypothesis testing supports convergent and discriminant validity.52, 53, 54 However, there is currently no reliable questionnaire to understand patient attitudes toward education and advice for managing low back pain. As a result, valuable clinician time and resources may be underutilised or misdirected when providing education and advice.
The Attitude toward Education and advice for Low back pain Questionnaire (AxEL-Q) provides clinicians with a valid and reliable tool to understand attitude toward education and advice for low back pain55 (Appendix). It was developed using guidance from the COSMIN consortium and evaluated in a sample of 313 participants with low back pain. The questionnaire draft was reduced to a 3-Factor questionnaire through exploratory factor analysis; Factor 1, attitude toward staying active, consists of 9 items with a score range from 0 to 54 with higher scores indicating a more positive attitude; Factor 2, attitude toward low back pain being rarely caused by a serious health problem, consists of 4 items, with a score range from 0 to 24 with higher scores indicating a more positive attitude; Factor 3; Attitude toward not needing to know the cause of back pain to manage it effectively, consists of 4 items, with a score range from 0 to 24 with higher scores indicating a more positive attitude. There was a strong inverse association between each factor and the Back Beliefs Questionnaire (BBQ) and a moderate positive association with the modified Pain Self-Efficacy Questionnaire (PSEQ). The strength of the relationship with the BBQ suggests that unhelpful beliefs underpin unhelpful attitudes and the relationship with the modified PSEQ suggests that the AxEL-Q has promise at predicting future behaviour. Each independent factor demonstrated acceptable internal consistency; Cronbach α Factor 1 = 0.92, Factor 2 = 0.91, Factor 3 = 0.90 and adequate intraclass correlation coefficients; Factor 1 = 0.71, Factor 2 = 0.73, Factor 3 = 0.79. Each subscale could be used independently to understand attitudes toward aspects of education and advice for people with low back pain. This would allow clinicians who have time restraints, for example GPs, to use only the relevant subscale when necessary.
We used Factor 1, attitude toward staying active, of the AxEL-Q as a secondary outcome in an online randomised controlled trial, that investigated the effect of two video interventions designed to reassure people about low back pain in comparison with no intervention.56 Future randomized controlled trials to investigate if using the tool to guide treatment in a clinical setting is more helpful at improving patient outcomes compared to not using it are necessary.
Physical therapy clinical implication: communication
The AxEL-Q could be integrated into physical therapy clinical practice as a tool that patients complete prior to or during their appointment and used as a starting point to enhance communication in consultations. For example, a negative attitude toward a message of education that low back pain is rarely caused by a serious health problem could lead a physical therapist to target that message, and begin a conversation with questions such as, “Why did you answer that way?” or “What does this statement mean to you?”. Conversely, a positive attitude toward a message about advice to stay active might suggest that the physical therapist should not focus on re-enforcing that message. This might allow effective communication of the education and advice most relevant to each patient. To broaden the clinical utility, the AxEL-Q is being translated into German, Turkish. and Arabic. We added a hypothetical clinical scenario (using the PICKUP tool57) to demonstrate how these strategies might be used in physical therapy clinical practice (Table 1).
Table 1.
A hypothetical scenario to demonstrate how these communication strategies might be applied in physical therapy clinical practice.
| Maria recently developed low back pain. She booked a physical therapy appointment. The physical therapist began the consultation by taking a focused clinical history. The physical therapist screened for features of serious pathology, explored the events associated with the onset of the pain, and assessed Maria's prognosis using the PICKUP tool. Throughout the history intake the physical therapist listened actively, asked open ended questions, and reflected some aspects of Maria's experience back to her. The physical therapist expressed empathy, acknowledging the distressing nature of low back pain. This validated Maria's experience and engaged her in the consultation. |
| Maria requested information on how best to manage the pain. At this point the physical therapist asked Maria to complete the AxEL-Q questionnaire which took 5 minutes. Once completed, Maria and the physical therapist reviewed her responses. This prompted a discussion around Maria's attitude toward recommended care for low back pain. She had a negative attitude towards Factor 3 related to causes of back pain but a positive attitude towards Factor 1 related to staying active. |
| The physical therapist used Maria's responses on the AxEL-Q to focus the consultation on addressing her attitude toward needing to know the cause of low back pain. They did this by discussing what is known and unknown about causes of low back pain. The physical therapist used statements such as; |
| “Your pain may not necessarily be related to the extent of damage in your back. Hurt does not necessarily mean harm” and “It is not necessary to know the specific cause of your back pain in order to manage the pain effectively” to guide the conversation. |
Tailoring patient education to promote self-management
Self-management
One objective of patient education and advice is to promote self-management. Self-management is defined by behavioural scientists as a 'practice of activities that individuals initiate and perform on their own behalf in maintaining life, health, and wellbeing'.58 Self-management for low back pain is an active process that should involve exercise, supported by clinical education and advice.59,60 From a clinician perspective, self-management is not just about providing information but teaching the patient skills that can be generalised to manage their health conditions independently.61 This requires the patient to have, or develop, emotional, behavioural, and technical skills.58 Self-management skills include problem-solving, decision making, action planning, self-tailoring, and self-monitoring.62
It is usually difficult for most patients to follow self-management recommendations without feedback or reinforcement.63 Further, current self-management interventions only provide small or unimportant reductions in pain related disability.64 A randomised controlled trial (n = 461) compared the effectiveness of tailored self-management support delivered using a smartphone application compared to usual care. Participants were provided with self-management recommendations which were guided by a type of artificial intelligence using case-based reasoning.64 Case-based reasoning uses knowledge of earlier successful cases and data from the current case including ratings of pain intensity, self-efficacy, fear-avoidance, and perceived barriers to provide individually tailored self-management advice. The authors reported an effect that was small and of uncertain clinical significance. Despite these results, developing strategies to optimise self-management remains a priority for people with low back pain.65,66
Roadmaps to promote self-management
Measuring attitudes towards education and advice could provide an insight into what messages of education and advice are important to promote self-management and for whom they should be prioritised. This is a novel method to facilitate person-centred care.
We conducted an observational study that identified key messages that were positively viewed by individuals with and without low back pain and found that some could predict intention to self-manage low back pain.67 We identified a hierarchical list of educational statements that could facilitate self-management in people with low back pain of different durations. Clinicians could refer to this list when a patient presents with low back pain and prioritise the patient education and advice they provide. For example, for people with acute or subacute low back pain, clinicians could prioritise discussion about cause with messages such as “Your pain may not necessarily be related to the extent of damage in your back. Hurt does not necessarily mean harm” and “It is not necessary to know the specific cause of your back pain in order to manage the pain effectively”. For people with chronic low back pain clinicians could prioritise discussion related to severity and imaging with messages such as “It is rare for low back pain to be caused by a more serious health problem” and “Imaging e.g., x-ray, CT scan or MRI is usually not needed in the majority of cases of low back pain”.
Information related to low back pain online is often inaccurate.68 However, a mixed-methods study highlighted that participants with low back pain valued learning about causes and influences on pain.69 Those authors reported that for the participants to engage in activities that were meaningful to them, such as physical activity, learning that "pain does not mean my body is damaged" was essential. A second qualitative analysis found that people with chronic low back pain who have received multiple clinical diagnosis for their pain were less likely to engage in activities of daily life.70 Recently, people with low back pain (n = 419) presenting for care completed a survey to understand what they perceived as important for their care, and patient results were compared to what physicians (n = 198) perceived as important to their patients.71 The authors reported that patients placed more importance on an “explanation of what is causing the pain” compared to physicians, and patients wanted to understand the cause of pain more than surgery, medication, and diagnostic tests.71
Physical therapy clinical implication: tailored education and advice
Not only do people want to know about cause of low back pain, specific messages of reassurance about cause and severity of low back pain were consistently more predictive of intention to self-manage than statements encouraging physical activity. Physical therapists could consider focusing patient education and advice on messages about cause, severity, and imaging, and in doing so remove barriers to physical activity and support self-management.
Summary
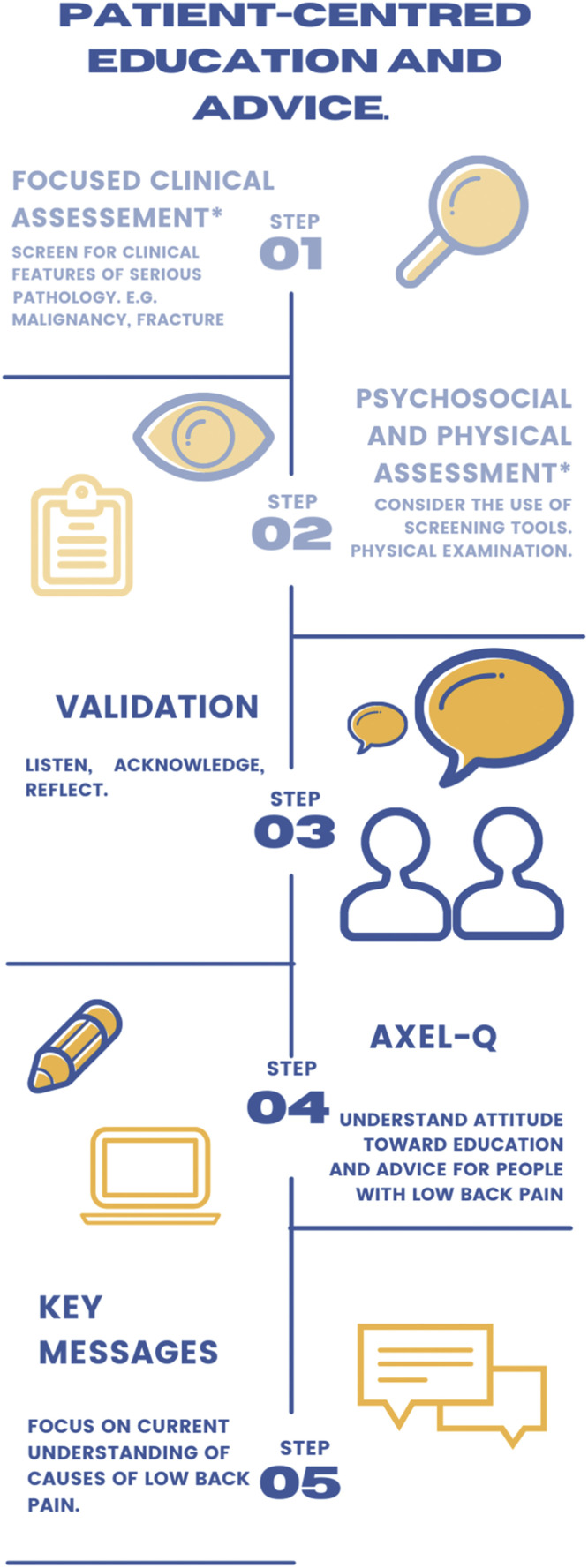
In this Masterclass, we have provided suggestions for a person-centred education and advice that should enable physical therapists to confidently deliver high value care within the time constraints of clinical practice. We outline these suggested steps in Fig. 1.
Fig. 1.
Steps for providing person-centred education and advice for people with low back pain. Screening for clinical features of serious pathology and conducting a physical and psychological assessment are the initial steps in the care pathway for people presenting with low back pain. This Masterclass focuses on the next steps to help physical therapists provide high-value patient education and advice to their patients, starting with step 3; providing validation, step 4; opening channels of communication and step 5; tailoring education and advice.
Conflicts of interest
ETO, AGC, JHM have no conflicts of interest to declare. ACT has received funding from the Australian National Health and Medical Research Council (NHMRC) including an NHMRC Early Career Fellowship (APP1144026) and funds from an NHMRC Program Grant (APP1113532) entitled ‘Using healthcare wisely: reducing inappropriate use of tests and treatments.’
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.bjpt.2022.100478.
Appendix. Supplementary materials
References
- 1.Kyu H., Abate D., Abate K., et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990 –2017 : a systematic analysis for the Global Burden of Disease Study 201. Lancet. 2018;392(10159):1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beyera G.K., O'Brien J., Campbell S. Health-care utilisation for low back pain: a systematic review and meta-analysis of population-based observational studies. Rheumatol Int. 2019;39(10):1663–1679. doi: 10.1007/s00296-019-04430-5. [DOI] [PubMed] [Google Scholar]
- 3.Deyo R.A., Mirza S.K., Turner J.A., Martin B.I. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22(1):62–68. doi: 10.3122/jabfm.2009.01.080102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gardner C., Moseley G.L., Karran E.L., Wiles L.K., Hibbert P. Implementing high value back pain care in private physiotherapy in Australia: a qualitative evaluation of physiotherapists who participated in an “implementation to innovation” system. Can J Pain. 2020;4(1):86–102. doi: 10.1080/24740527.2020.1732808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koes B.W., van Tulder M., Lin C.-.W.C., Macedo L.G., McAuley J., Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19(12):2075–2094. doi: 10.1007/s00586-010-1502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qaseem A., Wilt T.J., McLean R.M., Forciea M.A. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 7.Foster N.E., Anema J.R., Cherkin D., et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2384. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 8.Kamper S.J., Logan G., Copsey B., et al. What is usual care for low back pain? A systematic review of health care provided to patients with low back pain in family practice and emergency departments. Pain. 2020;161(4):694–702. doi: 10.1097/j.pain.0000000000001751. [DOI] [PubMed] [Google Scholar]
- 9.Jarvik J.G., Gold L.S., Comstock B.A., et al. Association of early imaging for back pain with clinical outcomes in older adults. JAMA - J Am Med Assoc. 2015;313(11):1143–1153. doi: 10.1001/jama.2015.1871. [DOI] [PubMed] [Google Scholar]
- 10.Shaheed C.A., Maher C.G., Williams K.A., Day R., McLachlan A.J. Efficacy, tolerability, and dose-dependent effects of opioid analgesics for low back pain a systematic review and meta-analysis. JAMA Intern Med. 2016;176(7):958–968. doi: 10.1001/jamainternmed.2016.1251. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira G.E., McLachlan A.J., Lin C.W.C., et al. Efficacy and safety of antidepressants for the treatment of back pain and osteoarthritis: systematic review and meta-analysis. BMJ. 2021;372:1–13. doi: 10.1136/bmj.m4825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferraro M.C., Bagg M.K., Wewege M.A., et al. Efficacy, acceptability, and safety of antidepressants for low back pain: a systematic review and meta-analysis. Syst Rev. 2021;10(1):1–13. doi: 10.1186/s13643-021-01599-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cashin A.G., Folly T., Bagg M.K., et al. Efficacy, acceptability, and safety of muscle relaxants for adults with non-specific low back pain: systematic review and meta-analysis. BMJ. 2021;374(table 1):1–12. doi: 10.1136/bmj.n1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris I.A., Traeger A., Stanford R., Maher C.G., Buchbinder R. Lumbar spine fusion: what is the evidence? Intern Med J. 2018;48(12):1430–1434. doi: 10.1111/imj.14120. [DOI] [PubMed] [Google Scholar]
- 15.Buchbinder R., Underwood M., Hartvigsen J., Maher C.G. The Lancet Series call to action to reduce low value care for low back pain: an update. Pain. 2020;161(Supplement 1):S57–S64. doi: 10.1097/j.pain.0000000000001869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slade S.C., Kent P., Patel S., Bucknall T., Buchbinder R. Barriers to primary care clinician adherence to clinical guidelines for the management of low back pain: a systematic review and metasynthesis of qualitative studies. Clin J Pain. 2016;32(9):800–816. doi: 10.1097/AJP.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 17.Hoffmann T., Bakhit M., Michaleff Z. Shared decision making and physical therapy: what, when, how, and why? Brazilian J Phys Ther. 2022;26(1) doi: 10.1016/j.bjpt.2021.100382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barry M.J., Edgman-Levitan S. Shared decision making — the pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–781. doi: 10.1056/nejmp1109283. [DOI] [PubMed] [Google Scholar]
- 19.Toye F., Barker K. Persistent non-specific low back pain and patients’ experience of general practice: a qualitative study. Prim Health Care Res Dev. 2012;13(1):72–84. doi: 10.1017/S1463423611000387. [DOI] [PubMed] [Google Scholar]
- 20.Penn T.M., Overstreet D.S., Aroke E.N., et al. Perceived injustice helps explain the association between chronic pain stigma and movement-evoked pain in adults with nonspecific chronic low back pain. Pain Med (United States) 2020;21(11):3161–3171. doi: 10.1093/PM/PNAA095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fleming M.D., Shim J.K., Yen I., et al. Patient engagement at the margins: health care providers’ assessments of engagement and the structural determinants of health in the safety-net. Soc Sci Med. 2017;183:11–18. doi: 10.1016/j.socscimed.2017.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.El-Haddad C., Damodaran A., Patrick Mcneil H., Hu W. The experience of patients admitted to hospital with acute low back pain: a qualitative study. Int J Rheum Dis. 2018;21(4):796–803. doi: 10.1111/1756-185X.12870. [DOI] [PubMed] [Google Scholar]
- 23.O'Hagan E.T., Traeger A.C., Bunzli S., et al. What do people post on social media relative to low back pain? A content analysis of Australian data. Musculoskelet Sci Pract. 2021;54(January) doi: 10.1016/j.msksp.2021.102402. [DOI] [PubMed] [Google Scholar]
- 24.Moorhead S.A., Hazlett D.E., Harrison L., Carroll J.K., Irwin A., Hoving C. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15(4):1–17. doi: 10.2196/jmir.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cline R.J.W., Haynes K.M. Consumer health information seeking on the Internet: the state of the art. Health Educ Res. 2001;16(6):671–692. doi: 10.1093/her/16.6.671. [DOI] [PubMed] [Google Scholar]
- 26.Naslund J.A., Aschbrenner K.A., Marsch L.A., et al. The future of mental health care: peer-to-peer support and social media. Epidemiol Psychiatr Sci. 2016;25(2):113–122. doi: 10.1017/S2045796015001067.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hefler M., Kerrigan V., Henryks J., Freeman B., Thomas D.P. Social media and health information sharing among Australian Indigenous people. Health Promot Int. 2019;34(4):706–715. doi: 10.1093/heapro/day018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Toye F., Seers K., Hannink E., Barker K. A mega-ethnography of eleven qualitative evidence syntheses exploring the experience of living with chronic non-malignant pain. BMC Med Res Methodol. 2017;17(1):1–11. doi: 10.1186/s12874-017-0392-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacNeela P., Doyle C., O'Gorman D., Ruane N., McGuire B.E. Experiences of chronic low back pain: a meta-ethnography of qualitative research. Health Psychol Rev. 2015;9(1):63–82. doi: 10.1080/17437199.2013.840951. [DOI] [PubMed] [Google Scholar]
- 30.Bunzli S., Watkins R., Smith A., Schutze R., O'Sullivan P.B. Lives on hold a qualitative synthesis exploring the experience of chronic low-back pain. Clin J Pain. 2013;29(10) doi: 10.1097/AJP.0b013e31827a6dd8. www.clinicalpain.com%7C907 Accessed April 12, 2019. [DOI] [PubMed] [Google Scholar]
- 31.Buchman D.Z., Ho A., Illes J. You present like a drug addict: patient and clinician perspectives on trust and trustworthiness in chronic pain management. Pain Med (United States) 2016;17(8):1394–1406. doi: 10.1093/pm/pnv083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Linehan M. In: Empathy Reconisdered: New Directions in Psychotherapy. Bohart A, Greenber L, editors. American Psychological Association Inc.; Washington DC: 1997. Validation and psychotherapy. [Google Scholar]
- 33.Linton S.J., Boersma K., Vangronsveld K., Fruzzetti A. Painfully reassuring? The effects of validation on emotions and adherence in a pain test. Eur J Pain (United Kingdom) 2012;16(4):592–599. doi: 10.1016/j.ejpain.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 34.Vangronsveld K.L., Linton S.J. The effect of validating and invalidating communication on satisfaction, pain and affect in nurses suffering from low back pain during a semi-structured interview. Eur J Pain (United Kingdom) 2012;16(2):239–246. doi: 10.1016/j.ejpain.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 35.Edmond S.N., Keefe F.J. Validating pain communication: current state of the science. Pain. 2015;156(2):215–291. doi: 10.1097/01.j.pain.0000460301.18207.c2.Validating. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Linton S.J., McCracken L.M., Vlaeyen J.W.S. Reassurance: help or hinder in the treatment of pain. Pain. 2008;134(1–2):5–8. doi: 10.1016/j.pain.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 37.Holopainen R., Simpson P., Piirainen A., et al. Physiotherapists’ perceptions of learning and implementing a biopsychosocial intervention to treat musculoskeletal pain conditions: a systematic review and metasynthesis of qualitative studies. Pain. 2020;161(6):1150–1168. doi: 10.1097/j.pain.0000000000001809. [DOI] [PubMed] [Google Scholar]
- 38.Holopainen R., Lausmaa M., Edlund S., et al. Physiotherapists’ validating and invalidating communication before and after participating in brief cognitive functional therapy training. Test of concept study. Eur J Physiother. 2021;0(0):1–7. doi: 10.1080/21679169.2021.1967446. [DOI] [Google Scholar]
- 39.Lin I., Wiles L., Waller R., et al. Patient-centred care: the cornerstone for high-value musculoskeletal pain management. Br J Sports Med. 2020;54(21):1240–1242. doi: 10.1136/bjsports-2019-101918. [DOI] [PubMed] [Google Scholar]
- 40.Parker D., Byng R., Dickens C., Kinsey D., McCabe R. Barriers and facilitators to GP–patient communication about emotional concerns in UK primary care: a systematic review. Fam Pract. 2020;37(4):434–444. doi: 10.1093/FAMPRA/CMAA002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Toye F., Belton J., Hannink E., Seers K., Barker K. A healing journey with chronic pain: a meta-ethnography synthesizing 195 qualitative studies. Pain Med. 2020;00(0):1–12. doi: 10.1093/pm/pnaa373. [DOI] [PubMed] [Google Scholar]
- 42.Hasenbring M.I., Pincus T. Effective reassurance in primary care of low back pain: what messages from clinicians are most beneficial at early stages? Clin J Pain. 2015;31(2):133–136. doi: 10.1097/AJP.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 43.Evers S. Patient perspectives on communication with primary care physicians about chronic low back pain. Perm J. 2017:1–5. doi: 10.7812/tpp/16-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.French S.D., Nielsen M., Hall L., et al. Essential key messages about diagnosis, imaging, and self-care for people with low back pain: a modified Delphi study of consumer and expert opinions. Pain. 2019;160(12):2787–2797. doi: 10.1097/j.pain.0000000000001663. [DOI] [PubMed] [Google Scholar]
- 45.Bergman M.M. A theoretical note on the differences between attitudes, opinions, and values. Swiss Polit Sci Rev. 1998;4(2):81–93. doi: 10.1002/j.1662-6370.1998.tb00239.x. [DOI] [Google Scholar]
- 46.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 47.Sheeran P., Maki A., Montanaro E., et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Heal Psychol. 2016;35(11):1178–1188. doi: 10.1037/hea0000387. [DOI] [PubMed] [Google Scholar]
- 48.Asare M. Using the theory of planned behavior to determine the condom use behaviour among college students. Am J Health Stud. 2015;30(1):43–50. [PMC free article] [PubMed] [Google Scholar]
- 49.Griva F., Anagnostopoulos F., Madoglou S. Mammography screening and the theory of planned behavior: suggestions toward an extended model of prediction. Women Heal. 2009;49(8):662–681. doi: 10.1080/03630240903496010. [DOI] [PubMed] [Google Scholar]
- 50.Bishop F.L., Dima A., Ngui J., et al. Lovely pie in the sky plans”: a qualitative study of clinicians’ perspectives on guidelines for managing low back pain in primary care in England. Spine (Phila Pa 1976) 2015;40(23):1842. doi: 10.1097/BRS.0000000000001215. [DOI] [PubMed] [Google Scholar]
- 51.Slade S.C., Kent P., Patel S., Bucknall T., Buchbinder R. Barriers to primary care clinician adherence to clinical guidelines for the management of low back pain: a systematic review and metasynthesis of qualitative studies. Clin J Pain. 2016;32(9):800–816. doi: 10.1097/AJP.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 52.Rainville J., Bagnall D., Phalen L. Health care providers’ attitudes and beliefs about functional impairments and chronic back pain. Clin J Pain. 1995;11(4):287–295. doi: 10.1097/00002508-199512000-00006. [DOI] [PubMed] [Google Scholar]
- 53.Darlow B., Perry M., Mathieson F., et al. The development and exploratory analysis of the Back Pain Attitudes Questionnaire (Back-PAQ) BMJ Open. 2014;4(5) doi: 10.1136/bmjopen-2014-005251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Slater M.A., Hall H.F., Atkinson J.H., Garfin S.R. Pain and impairment beliefs in chronic low back pain: validation of the Pain and Impairment Relationship Scale (PAIRS) Pain. 1991;44(1):51–56. doi: 10.1016/0304-3959(91)90146-O. [DOI] [PubMed] [Google Scholar]
- 55.O'Hagan E.T., Skinner I.W., Jones M.D., et al. Development and measurement properties of the AxEL (attitude toward education and advice for low-back-pain) questionnaire. Health Qual Life Outcomes. 2022;20(1):4. doi: 10.1186/s12955-021-01908-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.O'Hagan E.T., Traeger A.C., Schabrun S.M., et al. It ’s safe to move! A protocol for a randomised controlled trial investigating the effect of a video designed to increase people ’s confidence becoming more active despite back pain. BMJ Open. 2022;12(e063250):1–6. doi: 10.1136/bmjopen-2022-063250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Traeger A.C., Henschke N., Hübscher M., et al. Estimating the risk of chronic pain: development and validation of a prognostic model (PICKUP) for patients with acute low back pain. PLoS Med. 2016;13(5) doi: 10.1371/journal.pmed.1002019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Corbin J., Strauss A. Jossey-Bass; San Francisco: 1988. Unending Work and Care: Managing Chronic Illness at Home. ed. [Google Scholar]
- 59.Davies F., Wood F., Bullock A., Wallace C., Edwards A. Interventions to improve the self-management support health professionals provide for people with progressive neurological conditions: protocol for a realist synthesis. doi:10.1136/bmjopen-2016-014575 [DOI] [PMC free article] [PubMed]
- 60.May S. Self-management of chronic low back pain and osteoarthritis. Nat Rev Rheumatol. 2010;6(4):199–209. doi: 10.1038/nrrheum.2010.26. [DOI] [PubMed] [Google Scholar]
- 61.Hutting N., Johnston V., Staal J.B., Heerkens Y.F. Promoting the use of self-management strategies for people with persistent musculoskeletal disorders: the role of physical therapists. J Orthop Sports Phys Ther. 2019;49(4):212–215. doi: 10.2519/jospt.2019.0605. [DOI] [PubMed] [Google Scholar]
- 62.Hutting N., Caneiro J.P., Ong'wen O.M., Miciak M., Roberts L. Patient-centered care in musculoskeletal practice: key elements to support clinicians to focus on the person. Musculoskelet Sci Pract. 2021;(August) doi: 10.1016/j.msksp.2021.102434. [DOI] [PubMed] [Google Scholar]
- 63.Seid M.A., Abdela O.A., Zeleke E.G. Adherence to self-care recommendations and associated factors among adult heart failure patients. From the patients’ point of view. PLoS One. 2019;14(2):1–13. doi: 10.1371/journal.pone.0211768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sandal L.F., Bach K., Øverås C.K., et al. Effectiveness of app-delivered, tailored self-management support for adults with lower back pain–related disability. JAMA Intern Med. 2021:1–9. doi: 10.1001/jamainternmed.2021.4097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kongsted A., Ris I., Kjaer P., Hartvigsen J. Self-management at the core of back pain care: 10 key points for clinicians: self-management support in back pain. Brazilian J Phys Ther. 2021;25(4):396–406. doi: 10.1016/j.bjpt.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lim Y.Z., Chou L., Au R.T., et al. People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: a systematic review. J Physiother. 2019;65(3):124–135. doi: 10.1016/j.jphys.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 67.O'Hagan E.T., Di Pietro F., Traeger A.C., et al. What messages predict intention to self-manage low back pain? A study of attitudes towards patient education. Pain. 2022 doi: 10.1097/j.pain.0000000000002530. [DOI] [PubMed] [Google Scholar]
- 68.Santos R.P., Alonso T.P., Correia I.M.T., Nogueira L.C., Meziat-Filho N., Reis F.J.J. Patients should not rely on low back pain information from Brazilian official websites: a mixed-methods review. Brazilian J Phys Ther. 2022;26(1) doi: 10.1016/j.bjpt.2022.100389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Leake H.B., Moseley G.L., Stanton T.R., O'Hagan E.T., Heathcote L.C. What do patients value learning about pain? A mixed methods survey on the relevance of target concepts following pain science education. Pain. 2021;162(10):2558–2568. doi: 10.1097/j.pain.0000000000002244. [DOI] [PubMed] [Google Scholar]
- 70.Bonfim I da S., Corrêa L.A., Nogueira L.A.C., Meziat-Filho N., Reis F.J.J., de Almeida R.S. Your spine is so worn out’ – the influence of clinical diagnosis on beliefs in patients with non-specific chronic low back pain – a qualitative study. Brazilian J Phys Ther. 2021;25(6):811–818. doi: 10.1016/j.bjpt.2021.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Smuck M., Barrette K., Martinez-Ith A., Sultana G., Zheng P. What does the patient with back pain want? A comparison of patient preferences and physician assumptions. Spine J. 2021;22 doi: 10.1016/j.spinee.2021.09.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.