Abstract
Although studies have investigated the factors associated with psychological post-COVID-19 symptoms, the impact of marital status on symptom development has not been fully determined. This study conducts a questionnaire survey to investigate the association between marital status and the proportion of patients with post-COVID-19 symptoms in 749 cases as valid responses. Depressive state and memory impairment were more frequently seen in the no-spouse group when each symptom was compared according to marital status. Particularly in individuals in the 40s who had minor COVID-19 illness, this trend was noted. Single patients with mild COVID-19 illness may need proactive psychological support.
Keywords: COVID-19, Depression, Post-COVID-19, Long COVID-19
Abbreviations: COVID-19, coronavirus disease of 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
1. Main text
The sequelae of COVID-19 are known as “post-COVID-19” or “long COVID,” which include physical and psychological symptoms. The psychological symptoms have been reported to have associations with the female sex, the severity of the COVID-19 illness, and socioeconomic status [1]. Along with these risk factors, it can be indicated that the presence or absence of a spouse influences the development of psychological conditions as is the case with other types of diseases [2]. However, it has not yet been adequately determined how marital status affects psychological post-COVID-19 symptoms.
In this study, we used a questionnaire survey to examine the relationship between marital status and the percentage of patients with post-COVID-19 symptoms who were diagnosed between the ages of 20 and 80 in Oita Prefecture, Japan. We administered anonymous questionnaires to 2116 people who had been previously confirmed to have severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, in collaboration with the Oita Prefectural Government. The targeted sample included people who were diagnosed with COVID-19 as mild illness on January 2022, moderate illness from January to March 2022, and severe illness from July 2021 to March 2022, as defined by the World Health Organization [3]. A long inclusion period was adopted for moderate and severe COVID-19 illness to involve a certain number of these patients. Patients who were hospitalized upon the patient's request but had no oxygen required were classified into mild illness cases.
Along with the existence or absence of each symptom and its duration, we also inquired about marital status. In this study, participants living apart were categorized as belonging to the spouse group. There were a number of symptoms, including fatigue, cough, sputum, joint discomfort, dyspnea, loss of concentration, depression, taste disorder, diarrhea, asomnia, smell disorder, hair loss, and memory defect. As we wanted to focus on not only “chronic” but also “prolonged” conditions, the data on whether these symptoms existed at approximately one month after the infection has been documented. Statistical Package for the Social Sciences version 22 was used to perform chi-square tests for between-group comparisons (IBM Japan, Tokyo, Japan). The institutional ethics committee of our institution gave its approval to the study protocol (approval number 2372; approval date 30 August 2022). Before they were enrolled in the study, all subjects provided their written, informed permission. The responses of 791 (37%) out of the 2116 eligible patients were obtained. After excluding 39 cases with entirely blank responses, no consent obtained, and inconsistent infection dates including multiple infections answered, 752 (36%) cases were considered valid responses. In addition, 749 (35%) cases were eventually evaluated after 3 instances were removed for having blank responses to the marital status question. Four hundred (53%) of the genuine cases' respondents were female, and 540 (72%) said that they had a spouse. In 611 (82%), 100 (13%), and 38 (5% of instances), the COVID-19 disease was mild, moderate, or severe. When each symptom was compared by marital status, depressive state and memory defect showed a significant difference between the spouse and no-spouse group.
The depressive state was significantly more commonly observed in the no-spouse group (54/209, 26%) than in the spouse group (98/540, 18%), as shown in Fig. 1 . This significance was found only in patients with mild COVID-19 illness but not in those with moderate and severe COVID-19 illness (Fig. 2 A). Additionally, despite having little statistical significance, people in 40s displayed a greater difference when compared by age group (Fig. 3 A). Additionally, the no-spouse group (19/209, 9%) had considerably higher instances of memory impairment than the spouse group (28/540, 5%). This tendency was likely to be seen in patients with mild COVID-19 illness (Fig. 2B). When comparing by age group, significant difference was observed in 40s (Fig. 3B).
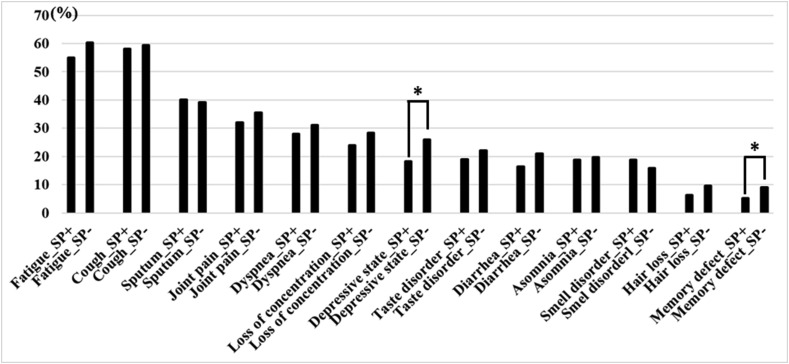
Fig. 1.
The proportion of patients with post-COVID-19 symptoms in accordance with marital status. The proportion of patients with a depressive state was significantly higher in the no-spouse group than in the spouse group (54/209, 26% in the no-spouse group vs. 98/540, 18% in the spouse group, p = 0.019)∗. Similarly, that of patients with memory defects was significantly higher in the no-spouse group than in the spouse group (19/209, 9% in the no-spouse group vs. 28/540, 5% in the spouse group, p = 0.048). SP, spouse.
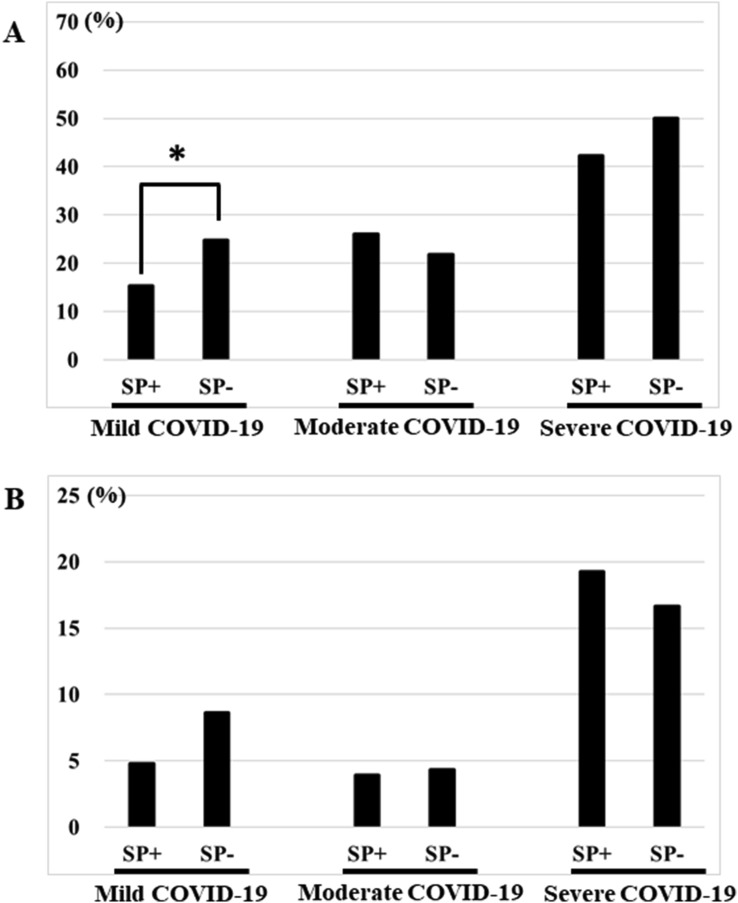
Fig. 2.
The proportion of patients with depressive state and memory defect in accordance with the severity of COVID-19 illness. (A) Depressive state was observed in 67 of 437 (15%) patients in the spouse group vs. 43 of 174 (25%) in the no-spouse group (p = 0.006) in mild COVID-19 cases∗, 20 of 77 (26%) in the spouse group vs. 5 of 23 (22%) in the no-spouse group (p = 0.681) in moderate COVID-19 cases, and 11 of 26 (42%) in the spouse group vs. 6 of 12 (50%) in the no-spouse group (p = 0.658) in severe COVID-19 cases. (B) Memory defect was observed in 21 of 437 (5%) patients in the spouse group vs. 15 of 174 (9%) in the no-spouse group (p = 0.071) in mild COVID-19 cases, 3 of 77 (4%) in the spouse group vs. 1 of 23 (4%) in the no-spouse group (p = 0.655) in moderate COVID-19 cases, and 5 of 26 (19%) in the spouse group vs. 2 of 12 (17%) in the no-spouse group (p = 0.615) in severe COVID-19 cases. SP, spouse.
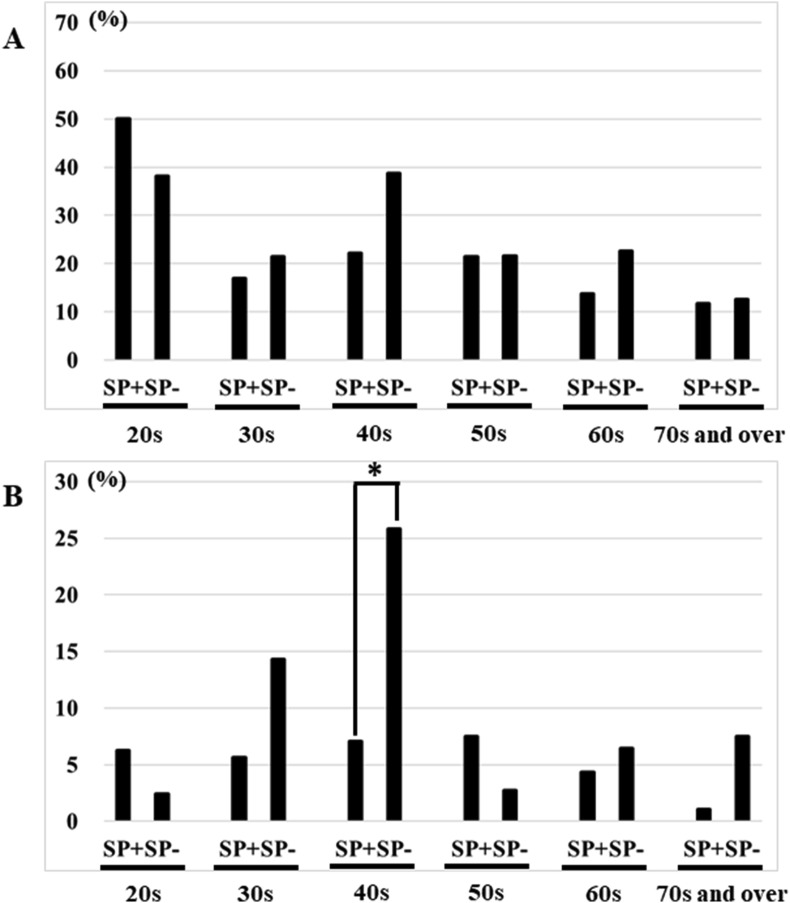
Fig. 3.
The proportion of patients with depressive states and memory defects in accordance to age group. (A) Depressive state was observed in 8 of 16 (50%) patients in the spouse group vs. 16 of 42 (38%) in the no-spouse group (p = 0.411) in 20s, 12 of 71 (17%) in the spouse group vs. 6 of 28 (21%) in the no-spouse group (p = 0.599) in 30s, 25 of 113 (22%) in the spouse group vs. 12 of 31 (39%) in the no-spouse group (p = 0.061) in 40s, 23 of 107 (22%) in the spouse group vs. 8 of 37 (22%) in the no-spouse group (p = 0.987) in 50s, 19 of 139 (14%) in the spouse group vs. 7 of 31 (23%) in the no-spouse group (p = 0.165) in 60s, and 11 of 94 (12%) in the spouse group vs. 5 of 40 (13%) in the no-spouse group (p = 0.552) in 70s and over. (B) Memory defect was observed in 1 of 16 (6%) patients in the spouse group vs. 1 of 42 (2%) in the no-spouse group (p = 0.479) in 20s, 4 of 71 (6%) in the spouse group vs. 4 of 28 (14%) in the no-spouse group (p = 0.155) in 30s, 8 of 113 (7%) in the spouse group vs. 8 of 31 (26%) in the no-spouse group (p = 0.007) in 40s∗, 8 of 107 (8%) in the spouse group vs. 1 of 37 (3%) in the no-spouse group (p = 0.275) in 50s, 6 of 139 (4%) in the spouse group vs. 2 of 31 (7%) in the no-spouse group (p = 0.446) in 60s, and 1 of 94 (1%) in the spouse group vs. 3 of 40 (8%) in the no-spouse group (p = 0.079) in 70s and over. SP, spouse.
During the COVID-19 pandemic, it was reported that single people are more prone to feel loneliness than those who do not live alone [4], and this feeling might lead to the development of a depressive state. Similarly, external stress may induce memory impairment increasing serum cortisol levels [5]. Although the association between marital status and psychological status in relation to post-COVID-19 has not widely been investigated, a report from China demonstrated that insomnia after COVID-19 was related to marital status [6]. Another study [7] also revealed a link between marital status in the general population and the severity of psychiatric symptoms during COVID-19. The current study in Japan revealed a similar pattern, suggesting that the idea that marital status affects psychological symptoms may be widespread. Interestingly, in our analyses, the significant association between marital status and depressive state or memory defect was observed mainly among the mild cases, suggesting that they are more likely to feel mental stress due to social isolation even though their physical condition was asymptomatic or mild. The sub-analysis by age group detected a significant difference in 40s. The elevated incidence of depression among members of this generation is undoubtedly related to their higher social standing, more obligations, and propensity to be severely influenced by social isolation. A population-based study published even before the COVID-19 pandemic showed that persons living alone, especially in 40s, had a higher prevalence of anxiety or depression than persons living with a partner [8].
SARS-CoV-2 itself may directly influence the nervous system [9]. Such direct influence is more frequently observed in severe than mild COVID-19 cases [10]. In the present analyses, a depressive state was surely more frequently observed in moderate and severe COVID-19 cases (Fig. 2), but a significant difference was found only in mild cases. For single patients with mild COVID-19 illness, social isolation rather than viral virulence itself might affect their psychological conditions, which could explain the gap in marital status to COVID-19 severity. Only married status is not directly linked to the difference in the prevalence of depressive mood and memory deficit, despite the fact that psychiatric symptoms are associated with a variety of socioeconomic factors [2]. The prevention and early improvement of these mental symptoms, particularly in moderate COVID-19 instances, may be facilitated by proactive psychological assistance for single individuals. Additionally, exercise combining low- and moderate-intensity strength muscle training may improve the depressive state after COVID-19 [11]. Moreover, the combination of these approaches would be beneficial to reduce the development of mental stress in patients with mild COVID-19 illness. In light of the scientific facts regarding the virulence of the pandemic strain, we do need to flexible re-consider whether the social isolation of COVID-19 patients with asymptomatic or mild symptoms is necessary.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgement
This research was supported by the Oita Prefectural Platform Program.
References
- 1.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gutiérrez-Rojas L., Porras-Segovia A., Dunne H., Andrade-González N., Cervilla J.A. Prevalence and correlates of major depressive disorder: a systematic review. Br J Psychiatry. 2020;42:657–672. doi: 10.1590/1516-4446-2019-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . 27 May 2020. Clinical management of COVID-19: interim guidance.https://wwwwhoint/publications/i/item/clinical-management-of-covid-19 2020. [Google Scholar]
- 4.Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., et al. The trajectory of loneliness in response to COVID-19. Am Psychol. 2020;75:897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klier C., Buratto L.G. Stress and long-term memory retrieval: a systematic review. Trends Psychiatry Psychother. 2020;42:284–291. doi: 10.1590/2237-6089-2019-0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X., Yu H., Bian G., Hu Z., Liu X., Zhou Q., et al. Prevalence, risk factors, and clinical correlates of insomnia in volunteer and at home medical staff during the COVID-19. Brain Behav Immun. 2020;87:140–141. doi: 10.1016/j.bbi.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L., et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Molarius A., Berglund K., Eriksson C., Eriksson H.G., Lindén-Boström M., Nordström E., et al. Mental health symptoms in relation to socio-economic conditions and lifestyle factors-a population-based study in Sweden. BMC Publ Health. 2009;9:302. doi: 10.1186/1471-2458-9-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aghagoli G., Gallo Marin B., Katchur N.J., Chaves-Sell F., Asaad W.F., Murphy S.A. Neurological involvement in COVID-19 and potential mechanisms: a review. Neurocritical Care. 2021;34:1062–1071. doi: 10.1007/s12028-020-01049-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in wuhan, China. Jama Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jimeno-Almazán A., Franco-López F., Buendía-Romero Á., Martínez-Cava A., Sánchez-Agar J.A., Sánchez-Alcaraz Martínez B.J., et al. Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: a randomized controlled trial. Scand J Med Sci Sports. 2022;32:1791–1801. doi: 10.1111/sms.14240. [DOI] [PMC free article] [PubMed] [Google Scholar]