Abstract
As a common belief, most viruses can egress from the host cells as single particles and transmit to uninfected cells. Emerging data have revealed en bloc viral transmission as lipid bilayer-cloaked particles via extracellular vesicles especially exosomes (Exo). The supporting membrane can be originated from multivesicular bodies during intra-luminal vesicle formation and autophagic response. Exo are nano-sized particles, ranging from 40–200 nm, with the ability to harbor several types of signaling molecules from donor to acceptor cells in a paracrine manner, resulting in the modulation of specific signaling reactions in target cells. The phenomenon of Exo biogenesis consists of multiple and complex biological steps with the participation of diverse constituents and molecular pathways. Due to similarities between Exo biogenesis and virus replication and the existence of shared pathways, it is thought that viruses can hijack the Exo biogenesis machinery to spread and evade immune cells. To this end, Exo can transmit complete virions (as single units or aggregates), separate viral components, and naked genetic materials. The current review article aims to scrutinize challenges and opportunities related to the exosomal delivery of viruses in terms of viral infections and public health.
Video Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s12964-022-01037-5.
Keywords: Viruses, Exosomes, Shared signaling pathways, Transmission, Infection
Introduction
Each cell can release different types of extracellular vesicles (EV) into the extracellular matrix (ECM) under physiological and pathological conditions [1]. Among EVs, exosomes (Exo) have been considered significant biological tools in cell-to-cell paracrine activity [1]. The existence of diverse biological factors inside the Exo highlights their critical role of them in the transport of signaling biomolecules [2]. Various lipids, nucleic acids (miRNAs, lncRNA and circRNA, mitochondrial DNA, and single and double-strand DNA), and growth factors can be found in the lumen of Exo [2]. Because Exo biogenesis and abscission are tightly regulated by varied effectors from different pathways [3], it is logical to hypothesize that Exo production can affect other cellular activities or vice versa [4]. In support of this claim, molecular investigations have shown similarities between the Exo biogenesis and assembly and egress system of several viruses [5]. During the last decades, this phenomenon has led to the rise of the Trojan Exo hypothesis demonstrating that different viruses can hijack the Exo trafficking system to spread between the cells without the direct interaction between viral ligands and host cell receptors [6]. The identification and presence of viral particles inside the releasing Exo supports the integration of the viral and Exo assembly systems [7]. Whether and how viruses can hijack the Exo trafficking system is the subject of debate. Here, we aimed to highlight the possible interaction between viral assembly machinery with the Exo trafficking system. Beidses, different mechanisms viruses can use for propagation and infection via Exo will be discussed.
Exosome biogenesis and abscission
Exo are originated from intracellular vesicles namely intraluminal vesicles (ILVs) (Fig. 1). The concept of ILVs implies the invagination of the endosomal membrane into the lumen that promotes the formation of numerous nano-sized vesicles [8, 9]. Further fusion of the endosomal compartments with plasma membrane triggers the release of ILVs into the ECM where they are, hereafter, known as Exo with an average size of 30–150 nm [8–10]. The physiological significance of Exo is related to the transfer of different biomolecules between the cells during different contexts, suggesting that Exo act as natural bio-shuttles inside the body [11]. The procedure of Exo biogenesis is summarized in three steps as follows; formation, transfer, and release (abscission) [12]. The formation of Exo ancestors is triggered by inward budding and de novo formation of early endosomes through the endosomal pathway [13, 14]. As an alternative pathway, early endosomes are derived from the Trans-Golgi network and can fuse with the pre-existing early endosomes [13, 14]. In later phases, early endosomes mature into late endosomes. During endosomal maturation, Rab 5 is replaced with Rab 7 via a guanosine exchange factor namely Mon1–Ccz1 complex [15]. It was suggested that Rab 7 is a regular protein in several processes related to endosomal maturation, degradation, and secretion [15]. Inside late endosomes, the membrane is actively invaginated into the luminal surface to constitute numerous ILVs resulting in the formation of multi-vesicular appearance namely multivesicular bodies (MVBs) [16]. There are multiple MVB biogenesis mechanisms as follows; ESCRT-dependent and ESCRT-independent mechanisms [17]. It was suggested that the ESCRT-dependent pathway is classified into canonical and non-canonical signaling cascades [18]. In the canonical ESCRT-dependent pathway, ESCRT-0, its HRS domain with tyrosine kinase activity is recruited to the endosomal membrane via phosphatidylinositol-3-Phosphate binding (Fig. 2A) [19]. This complex can recognize ubiquitinated proteins and sequestrate into the luminal surface of vesicles [19]. In the latter steps, ESCRT-0, as a member of the sorting machinery system, is recalled followed by the addition of ESCRT-I, -II, and –III [20]. Among them, the collaboration of the collection of ESCRT-0, -I, and II facilitates the invagination of endosomal membranes and enhances the sorting efficiency of ubiquitinated proteins within the buds [20]. Upon the recruitment of ESCRT-III, ESCRT-III components are dynamically assembled to promote ILV formation and abscission from the MVB membrane [20]. After the completion of this step, ESCRT-III is disassociated via the activation of AAA-ATPase Vps4 [21].
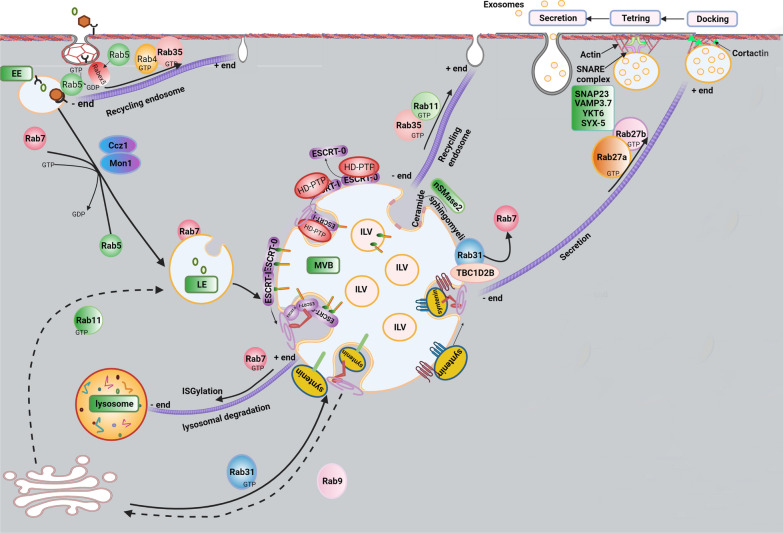
Fig. 1.
The generation of Exo is regulated by multiple intracellular pathways. Cargoes are sequestrated into early endosomes which are originated from endocytosis (Rab4, Rab5, Rab7, and Rab35) or Trans-Golgi network (Rab11). Exo fusion and recycling back pathways are regulated by the activity of Rab proteins (Rab 27a and Rab27b), SNARE complex (SYX-5, YKT6, VAMP3.7, SNAP23). The formation of ILVs inside the MVBs is mediated by inward invagination endosomal membrane via multiple pathways: ESCRT-dependent (ESCRT-0, I, II, II and syndecan-syntenin-ALIX axis), and ESCRT-independent pathways (ceramide-enriched microdomains and tetraspanin-enriched microdomains). Multiple pathways can distinguish the orientation of MVBs toward lysosomal depredation or fusion with the plasma membrane. ISGylation process can induce lysosomal degradation. The lysosomal degradation pathway is regulated by interaction Rab7 with Dynein and induction mobility toward microtubule minus ends. To fuse the MVBs with the membrane, various Rab-GTPases control the transport of MVBs on microtubules. Rab27 stabilizes the rearrangement of the actin cytoskeleton by improving the attachment of Cortactin, leading to MVBs docking. Docking, tethering, and releasing are three steps. The activity of SNAREs mediates the fusion of the MVB membrane with the plasma membrane
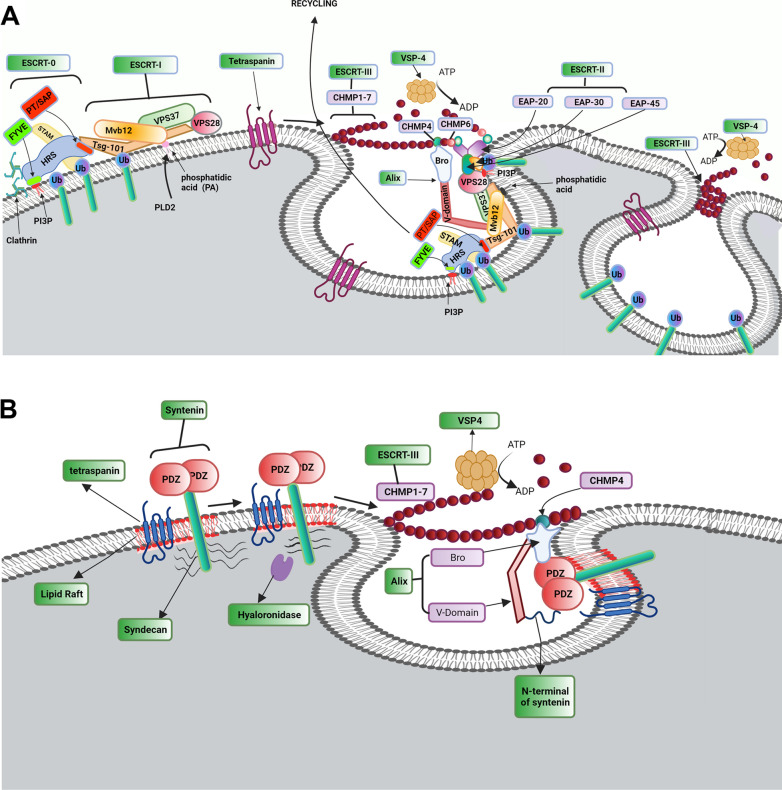
Fig. 2.
Exo biogenesis via conventional ESCRT-dependent pathway (A). Conventional ESCRT-dependent strategy can lead sorting of four ubiquitinated cargos into ILVs. ESCRT machinery is composed of ESCRT-0, -I, -II, and -III. The recruitment of ESCRT-0 occurs on the cytoplasmic side of the endosomal membrane. ESCRT-0 complex consists of HRS and STAM subunits to recognize the ubiquitinated cargoes. The recruitment of ESCRT-0 is triggered via the interaction of the ESCRT-0 HRS subunit with PIP3 on the endosomal membrane. The interaction of ESCRT-0 HRS with clathrin proteins enhances the clustering of ESCRT-0 to endosomal membrane microdomains. To select exosomal cargo, ESCRT-0 provides a platform for the attachment of ESCRT-I. ESCRT-I consists of four subunits: TSG-101, Mvb12, VPS37, and VPS28. Interaction between ESCRT-0 HRS subunit with ESCRT-1 TSG-101 subunit leads to physical attachment of ESCRT-0 and ESCRT-1 on endosome membrane. ESCRT-0 and -I proteins provide a binding site for of ESRT-II complex (EAP45, EAP30, and two EAP20). The physical connection is done via the ESCRT-I VPS28 subunit and ESCRT-II EAP45 subunit. Interaction of ESCRT-I with ESCRT-II can induce invagination of the endosomal membrane. The complex of ESCRT-0, -I, and -II can induce the assembly and polymerization of ESCRT-III subunits (CHMP-1, -2, -3, -4, -5, -6, and -7). Interaction of EAP20 of ESCRT-II with CHMP6 of ESCRT-III promotes the recruitment of ESCRT-III subunits. The activation of ESCRT-III promotes a chain around the neck of intraluminal vesicles. Endosomal membrane curvature is stimulated by the interaction of Alix with Mvb12 and CHMP4 subunits of ESCRT-I and ESCRT-III, respectively. Upon ILV scission, Vps4-ATPase induces ESCRT-II subunits disassociation. Role of Syndecan-Syntenin-Alix in Exo biogenesis (B). Syndecan-Syntenin-Alix stimulates Alix-ESCRT-mediated sorting in Exo. Heparanase induces Syndecans clustering and facilitates its attachment to adaptor protein Syntenin via PDZ domains. Syntenin N-terminus connects to Alix via the direct interaction with V-domain. In the end, VSP4 is recruited by the ESCRT-III complex and leads a session of ILVs into MVB
The non-canonical ESCRT-dependent mechanisms can participate in the formation of ILVs in yeasts, and some species of mammals [22]. For this purpose, the Histidine domain protein tyrosine phosphatase (HD-PTP) acts as a scaffold protein and binds the ESCRT complex in the absence of ESCRT-II [18]. It has been shown that there are other non-canonical ESCRT-dependent mechanisms activated by the syndecan-syntenin-ALIX axis (Fig. 2B) [23]. Of note, syndecan, as a transmembrane protein, interacts with syntenin to recall ALIX [23]. The final complex is not involved in the ubiquitination of proteins. To be specific, in the syndecan-syntenin-ALIX axis, both ESCRT-III and VPS4 actively regulate membrane budding and cargo sorting [24]. A plethora of documents has shown that ESCRT-independent mechanisms are also involved in ILV biogenesis [25]. Noteworthy, sphingomyelin located on the endosomal membrane is further cleaved to ceramide and phosphorylcholine by the activity of neutral sphingomyelinase 2 (nSMase 2) [26]. The collaboration of Ceramide with the ESCRT-independent pathway forms lipid raft microdomains at the surface of the endosomal membrane [27]. As a correlate, this complex induces negative curvature of the ceramide-enriched membrane and enforces ILV into the MVB lumen [27]. Molecular investigations have revealed that other effectors such as Rabs can also orchestrate the process of ILV formation via ESCRT-independent mechanisms [28]. For instance, RAB31 controls ceramide-dependent ILV budding procedure [28]. Like RAB31, some tetraspanin subsets such as CD63 play an important role in the ESCRT-independent pathway of ILV biogenesis [25]. This protein can stimulate the formation of tetraspanin-enriched microdomains, participating in ILVs biogenesis [29]. Based on the numerous findings, three destinations have been proposed for second endosomes inside each cell as follows; abscission, enzymatic digestion, and recycling [25]. First, these particles are directly guided to lysosomes where they undergo enzymatic degradation [25]. In the latter scenario, MVBs can fuse with the plasma membrane and shed their contents (hereafter known as Exo) into the neighboring ECM [8, 30]. Some fraction of released Exo can return to the host cells through the recycling mechanisms. This action is done by back-fusion with the plasma membrane and the participation of specific elements related to secretion pathways [31]. To orientate MVBs toward enzymatic digestion or abscission procedure, effectors from the Rab-GTPase family such as Rab7, 11, 35, and 27 are involved [3]. For example, Rab7 mediates MVB trafficking to lysosomal degradation. Rab11, 27, and 35 in collaboration with the SNARE complex control the secretion of ILVs out of the cells [31]. Molecular identification of Exo has shown complex cargo sorting and selective genomic, proteomic, and lipidomic contents [32]. This would occur in the parent cells where all steps correlated with Exo formation, transfer, and release happen. Therefore, it is logical to mention that the metabolic status of host cells contributes to the diversity of Exo cargo type [32]. Based on recent studies, it has been proposed that the final composition of EVs is relatively different from the parental cells [33]. This apparent difference may relate to the engagement of specific cargo sorting machinery with highly regulated activities that increase the density of certain factors inside the ILVs [33]. Noteworthy, some of the sorted biomolecules are common among all Exo like antigen-presentation proteins, adhesion molecules, motility factors, heat shock proteins (HSPs) and chaperones, MVB biogenesis associated factors, tetraspanins, trafficking and membrane fusion proteins, LAMP (lysosome-associated membrane glycoprotein), GTPases and metabolic enzymes [34–36]. Exo can harbor genomic content such as DNA, RNA, coding, and non-coding RNAs. Other genomic components such as mRNA, miRNA, rRNA, tRNA, vault RNA, Y-RNA, and circular RNA have been previously determined inside the Exo [33, 37]. A quantitative genomic analysis has revealed that the nucleotide content of Exo cargo differs, if not completely but in part, from the donor cell profile [38]. Data suggest the participation of specific sequence motifs in the loading of certain RNAs into the Exo lumen. Like RNAs, several types of DNA such as ssDNA, dsDNA, and mtDNA are sorted into the Exo. Of note, the manipulation of host cells to deliver DNA horizontally into the other cells is limited [38]. Variable levels of lipids including Cholesterol, Ceramides, Sphingomyelin, Phosphatidylserine, Gangliosides, and saturated fatty acids exist inside the Exo [39]. A piece of evidence points to the fact that lipid composition can affect Exo stability, trafficking, recognition, and internalization rate [40]. The existence of a significant difference in the lipid content of Exos isolated from plasma suggests that plasma harbors several arrays of Exos that originated from different cell sources. Alternatively, certain molecular pathways are engaged to sort specific lipids into the Exo [41]. Like lipid profile, genomic and proteomic profiles, results showed a mild to moderate increase of carbohydrates inside the Exo compared to the cytosol. For instance, Mannose, complex N-linked glycans, poly-lactosamine, and sialic acid are enriched into the Exo during the synthesis procedure [33, 42]. It is believed that the type and content of carbohydrates can change the exosomal protein content. Among carbohydrates, glycans act as a sorting device of proteins [42]. Concerning sorting activity, recent experiments have shown the crucial role of the ubiquitination process in the direction of different proteins into the Exo.
Of several intracellular mechanisms, the ESCRT accelerates the sorting of ubiquitinated proteins into the ILVs, furthermore, it is involved in the formation of ILVs [37], cytokinesis, and the invagination of some of the viruses. This complex is a modular super complex and consists of four components ESCRT-0, -I, -II, and -III, and accessory complexes Vps4 and Alix. Endosomal sorting is closely associated with the activity of the ESCRT system for the regulation of specific cargoes into ILVs inside MVBs [43, 44].
In the early stages, the factor ESRT0 initiates the formation of MVBs [45]. This factor is a heterodimer protein with two subunits, HRS (HGF-regulated tyrosine kinase substrate) and STAM (signal transducing adaptor molecule) [46]. It is believed that the promotion of HRS correlates with the formation of ILVs [47]. To this end, HRS attaches to phosphatidylinositol-3- phosphate (PI3P) on the endosomal membrane by the FYVE zinc finger domain, and the carboxy-terminal clathrin box of HRS contributes to HRS clustering into clathrin endosomal microdomains [48, 49]. Following the clathrin removal by V-ATPase HSC70, the formation of ILVs continues [32, 50]. The complex of HRS and STAM can bind to the clusters of ubiquitinated proteins by ubiquitin-binding domains, and ubiquitinated cargoes are directed to efficient sorting and degradation [51]. In later steps, HRS of ESCRT-0 binds to the amine terminal of the TSG101 subunit of ESCRT-I via P (T/S) A P motif in the carboxy-terminal [52–56].
ESCRT-I is a soluble hetero-tetramer protein complex consisting of four subunits: TSG101, Vps28, Vps37, and Mvb12 [57–61]. Protein–protein interaction between HRS of ESCRT-0 and TGS101 of ESCRT-I results in the recruitment of ESCRT-I from the cytoplasm to endosomal microdomains [60]. Furthermore, a recently conducted study has shown that produced phosphatidic acid by phospholipase-D2 interacts with Mvb12, an ESCRT-I subunit. As a correlate, phospholipase D2 activity supports the recruitment of ESCRT-I on the endosomal membrane and in the end, directs ESCRT-dependent endosomal maturation [62]. It has been proposed that ESCRT-I is a rod-shaped complex and is a bridge adapter to connect TSG101 with HRS while VPS28 simultaneously is attached to the specific residue of EAP45 belonging to the ESCRT-II complex [63–65]. Besides, TSG 101 can directly interact with ubiquitinated proteins through the UEV domain [66]. The collaboration of ESCRT-I with -II, triggers the invagination of the endosomal membrane into the lumen [67, 68].
Like ESRT-I, ESCRT-II plays an important role in membrane budding, MVB biogenesis, bridging ESCRT complexes to each other [69], and probably communicating between MVBs and microtubules via RILP, Rab7, and dynein [70–72]. ESCRT-II is a hetero-tetramer complex with a Y-shaped structure, composed of EP45, EP30 attaching section, and two EP20 as branch structures. The complex v binds to PI3P via the Glue domain of the EAP45 subunit preferentially, ubiquitinated cargos, and VPS28 of ESCRT-I [54, 56, 57]. In addition, ESCRT-II interacts with two ESCRT-III complexes via engaging two EAP20 subunits [73, 74].
Unlike ESCRT-0, -I, and -II, the ESCRT-III complex is vulnerable to cytosol niche due to a lack of pre-assembled structure [69, 75]. The formation of the ESCRT-0, -I, -II complex recalls the ESCRT-III components and stimulates the transient polymerization of helical filaments on the endosomal membrane [69, 75]. Molecular investigation revealed that the interaction between C-N units initiates ESCRT assembly. It is thought that ESCRT-III is composed of seven different subsets including CHMP 1, 2, 3, 4,5,6, and 7. Among them, the factor CHMP6 recalls the EAP20 in the structure of ESCRT-II. By the progression of these steps, the ESCRT-III complex facilities the budding vesicles into the endosome lumen via collaboration with a specific complex consisting of two hexameric or heptameric rings namely the AAA-ATPase Vps4 complex. The ATPase activity of Vps4 is regulated by the stimulation of an adaptor protein Vta1[69, 76]. The recruitment of other effectors such as Alix and TSG101 support molecular bridges for the attachment of ESCRT-I and -III [77, 78]. In addition, the formation of syndecan-syntenin-Alix can provide a niche to attach this complex to the ESCRT machinery system involved in the cargo sorting of protein inside the ILVs independent of ubiquitination [79, 80]. During the ILV formation, the importance of other components such as lipids has been proved. Ceramides form specific membrane microdomains at the surface of the endosomal membrane and induce negative curvature of the ceramide-enriched membrane. In addition to ILV formation, Ceramides are subsequently converted to sphingosine 1 phosphate and sphingosine via metabolic reactions, acting as lipid mediators [32, 81, 82]. For example, sphingosine 1 phosphate binds to the sphingosine 1 phosphate receptor coupled with inhibitory G protein involved in the cargo sorting into ILVs and the exosomal maturation inside the MVBs [32, 81]. Cholesterol-rich lipid rafts act as a platform for signaling coordination through receptors such as GPI-binding proteins, tyrosine kinases of the Src family, and Ca2+ channels [32, 83, 84].
Previous studies support the role of Tetraspanins respectively CD63, CD9, and CD81 in the ESCRT-independent pathway of Exo biogenesis [85–87]. These proteins can modulate cell adhesion, signaling, invasion, membrane fusion, trafficking, and membrane abscission [88, 89]. Tetraspanins with conserved transmembrane structures are organized in the membrane microdomains-rich cholesterol; Tetraspanins, as adaptors for other proteins, through interaction with Tetraspanins and other transmembrane and cytosolic proteins are involved in the formation of specialized membrane platforms called Tetraspanin membrane microdomains (TEM) [90, 91]. Of note, CD63, as a transmembrane protein can interact with Syntenin to form the CD63-Syntenin-ALIX complex which is involved in the MVB biogenesis [92]. Other Tetraspanin members such as CD81 and CD9 can attach to cytoskeletal actin and endosomal membrane microdomains via G proteins [88, 93]. However, a direct association between the CD81 and Rac GTPase in TEM is proved [94, 95]. On the other side, the interaction of CD9 with exosomal integrin is involved in targeting Exo to the specific tissue.
Upon the formation of ILVs, they are directed to lysosomal degradation or exosomal release [25]. Technically, the exosomal abscission process is summarized in three-step tethering, docking, and fusion [96]. Membrane tethering, the initial interaction between the MVB membrane and plasma membranes, is mediated by the interaction of Rab GTPases on the plasma membrane with tethering proteins on the MVB membrane [96]. Tethering machinery directs the formation of t-SNARE complexes on the plasma membrane, so triggers the assembly t-SNAREs with v-SNAREs on the surface of MVB and at the end leads to the partial formation of SNARE complex at the site of docking [96]. The balance between lysosomal degradation and exosomal release is controlled by different regulators. Based on studies, the level of Tetraspanin-6 (TSPN6) in the cells plays determining role in the fate of specific cargoes to the degradation of secretory pathways to preserve this balance [97]. Also, the role of TSPN6 has been proved in the exosomal release of (amyloid precursor protein) APP into the HEK293 cells [98]. High cellular levels of TSPN6 via inhibition of Syntenin/Syndecan and Syntenin/CD63 complexes formation prevents exosomal release and promotes lysosomal degradation of cargoes. On the other side low levels of TSPN6 direct the secretory pathway. The diverse effects of TSPN6 on the fate of ILVs possibly are depending on cell types and contexts [99]. The additional transfer of ubiquitinated cargo into ILVs via ESCRT-dependent mechanisms guides ILVs to the lysosomal pathway while the participation of Tetraspanin-dependent mechanisms targets ILVs to the secretory pathway. Noteworthy, ISGylation of peptides along with ubiquitin-like modification orients MVBs to the lysosomal pathway [100]. Unlike this pathway, further activation of RAB31 and interaction with Flotillin belonging to lipid raft microdomains, or TBC1D2B-derived activation of RAB31 (an activator of GTPase) directs MVBs to the secretion pathway rather than lysosomal degradation (Fig. 3A–B) [28].
Fig. 3.
RAB31 inhibits the lysosomal degradation of MVBs (A). The existence of a tyrosine kinase receptor namely EGFR on the late endosomal surface activates Rab31 via tyrosine phosphorylation. The phosphorylated Rab31 interacts with flotillin proteins. Rab31-flotillin acts as a scaffold heterodimer protein and forms a budding platform for sorting EGFR and other proteins into MVB lumen in collaboration with lipid rafts. On the other hand, Rab31 recruits TBC1D2B, and the Rab31-TBC1D2B complex inactivates Rab7, preventing the lysosomal degradation of MVBs. Besides the Syntenin-Alix-ESCRT-III, Rab31-flotillin complex acts as parallel sorting machinery that drives different cargoes such as CD63, CD81, and CD9 into exosomal pathways. CD63 is a membrane protein that can interact with PDZ domains of Syntenin. Interaction N-terminal of Syntenin with the V-domain of Alix induces the recruitment of ESCRT-III by the Bro domain of Alix and the formation of ILVs. HD-PTP acts as a scaffold for the binding of ESCRT subsets during the trafficking of ubiquitinated cargo into the MVB lumen (B). HRS and STAM are subunits of ESCRT-0 and can bind to the ubiquitinated cargos on the endosomal membrane. STAM is composed of STAM (GAT) and SH3 domains. STAM domain interacts with the Bro1 domain of HD-PTP and the SH3 domain is linked to the PPRPTAPKP motif in the PTP domain of HD-PTP. ESCRT-0 is dissociated from HD-PTP by the interaction of ESCRT-I TSG-101 with the PTAP motif of the PTP domain. Then, the ESCRT-I UBAP1 subunit can interact with the FYX2L motif in the CC region of the PTP domain. In the later phase, the interaction of ESCRT-III CHMP4 subunit with the Bro domain of HD-PTP enhances the dissociation of ESCRT-0 from HD-PTP, facilitates polymerization of ESCRT-III, and drives the ubiquitinated cargo into the MVB pathway
To promote exosomal abscission, the physical contact of Exo and plasma membrane is mandatory. The promotion of certain factors like actin and actin-regulating proteins, SNAREs, tethering factors, Rabs, and other types of RAS is important [14]. In this regard, cytoskeletal proteins such as actin and actin regulatory proteins (non-muscle myosin II/ROCK1/MLC/actin signaling pathway), microtubules as well as motor molecules (dyneins and kinesins) are involved in the secretion of Exo [101]. Of known proteins involved in docking and loading of MVBs into the inner surface of the plasma membrane, Cortactin and collaboration with Rab27A and coronin 1b promote the fusion of MVBs to membranes [102]. One of the important determinants in the fusion of MVBs to the membrane is associated with P4-ATPase ATP9A located at the inner surface of the plasma membrane and the MVB external surface. The lipid flippase activity of P4-ATPase ATP9A can regulate the recycling/secretion of MVBs [103]. Importantly, the activation of the SNARE complex leads to the fusion of MVBs with the target membrane. These proteins are categorized to v-SNAREs (attached to the vesicles) and t-SNAREs (attached to the target membrane). This complex is composed of syntaxin1 and SNAP25 (t-SNAREs), synaptobrevin (v-SNARE), and regulatory protein synaptotagmin. Depending on the type of organism, cell type, and MVB cargo, different proteins participate in the regulation of Exo secretion [8]. On the other side, oligomerization of the Synaptotagmin regulates the assembly of the SNARE complex at the docking site [104]. These features result in fusion of the MVB membrane with the plasma membrane and at the end release Exo [104]. The homologs of Synaptobrevin/Vesicle-associated membrane proteins (VAMP) participate in the Exo secretion process depending on kind of cells. For example, Vamp7 is involved in the exosomal secretion in the K562 cell line from leukemia cells [105] and YKT6 is involved in the exosomal secretion in the HEK293 cell line from the human embryonic kidney and in the A549 cell line of the human lung cancer cells [104].
Due to the complexity of Exo trafficking and the incorporation of numerous effectors from multiple signaling pathways, it is logical to hypothesize that these types of machinery could be used by numerous transduction cascades [18]. Due to similarities between viruses and the Exo biogenesis system, the replication, and intracellular transfer of viruses could be hijacked by viruses in favor of viral replication and propagation to the other cells [106]. In support of this claim, some reports are demonstrating that viruses use Exos or their intracellular machinery system to spread the infection out of the host cells [107].
Entry pathway of viruses
Understanding the mechanisms involved in viral entry seems the first step to answering how the dynamic growth of each virus is associated with the Exo trafficking system [107]. Molecular investigations have revealed that the entry of viral particles into the cells closely depends on overcoming several natural barriers including the plasma membrane, cytoskeletal dam, and intracellular membranes [108]. To circumvent these barriers, viruses commonly exploit direct fusion using endocytic mechanisms [109]. Noteworthy, the internalization strategy of viruses depends on the pH of target cells and several viral properties such as ligands and size [110]. It was suggested that viruses with fusion proteins and certain ligands can enter the host cell using several mechanisms as below (Fig. 4) [111];
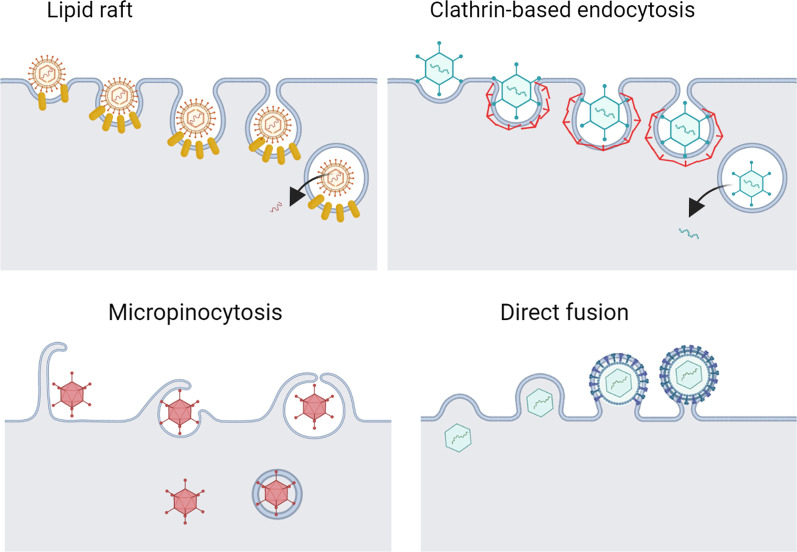
Fig. 4.
Several mechanisms used by viruses to internalize the host cells
Direct fusion pathway
At physiological pH, some of the enveloped viruses such as human immunodeficiency virus (HIV), and Herpes simplex viruses (HSV) like Epstein Barr Virus (EBV) are transferred into the cytosol using direct fusion [112]. Direct fusion includes three distinct steps as follows; tethering, docking, and further fusion. The latter step can be orchestrated via direct or indirect fusion [113]. Under physiological conditions, viral tethering is initiated by the non-permanent and non-specific attachment of viral ligands to proteoglycans and glycolipids [114]. After that, the docking step is triggered which is followed by the exposure of modules to maintain specific interaction and in the next phase, the fusion of viral particles and cell membrane occurs due to conformational remodeling of ligands and receptors [115]. It has been shown that the involvement of certain signaling pathways can facilitate the procedure of viral entry into the cytosol. For instance, HIV attaches to the cell surface after the interaction of viral fusion glycoprotein namely gp41/120 to the cognate receptor CD4 [116]. In next steps, other receptors like CXCR4 or CCR5 are promoted on the cell surface to perform specific binding and changes in viral glycoprotein for accelerating viral entry [117].
Endocytic pathways
Endocytic uptake is the collection of biological changes in the host cell membrane which are associated with the formation of curvature endocytic vesicles to carry viral particles into the deeper part of cytosol [118, 119]. It is believed that the integration and involvement of certain signaling cascades are essential to promoting the formation of endocytic vesicles [120]. Of note, lumen acidification in early or late endosomes can speed up virus penetration into the cytosol [121]. The active role of endocytic signaling pathways such as clathrin-dependent endocytosis, micropinocytosis, and lipid raft-dependent mechanisms are integral to the formation of viral endocytic vesicles [122, 123]. Among lipid raft-dependent endocytosis, pathways based on caveolae, flotillin, and GTPase regulators associated with focal adhesion kinase1 (GRAF1) can be exemplified [124].
For the entry of viruses via clathrin-based endocytosis, certain viruses such as Hepatitis B Virus (HBV), SARS-CoV-2, and type 1 HSV can attach to growth factor receptors such as epithelial growth factor receptor (EGFR) [125–127]. Upon viral and receptor interaction, tyrosine residues are phosphorylated in participant receptors followed by ubiquitination via the activity of ubiquitin ligase (Fig. 5A). Ubiquitylated receptors provoke other membrane-associated components such as FCH domain only 1/2 (FCHO1/2); epidermal growth factor receptor substrate 15 (EPS15); and intersectin [128]. The direct interaction of FCHO1/2 and intersection to EGFR recruits adaptor protein-2 (AP-2). In the next step, the activation of phosphatidylinositol phosphate kinase increases local levels of PIP2, leading to the assembly of membrane clathrin [128]. Of note, the polymerization of actin fibers accelerates membrane invagination and localization of clathrin molecules on the surface of vesicles [129]. The procedure of vesicle fission is done by involving dynamin and BAR domain proteins like endophilins and amphiphysins [130]. From the structural view of point, dynamin has GTPase activity that can support dynamin polymerized into the helical structure at the neck of endocytic vesicles, resulting in the disassociation of vesicles from the plasma membrane. Owing to the ATPase activity of head shock cognate protein 70 (HSC70) and hydrolysis phosphate bands in phosphatidylinositol 4, 5-biphosphate [PI (4, 5) P2] by the activity of phospholipase C, clathrin coat is removed from the surface of vesicles [131].
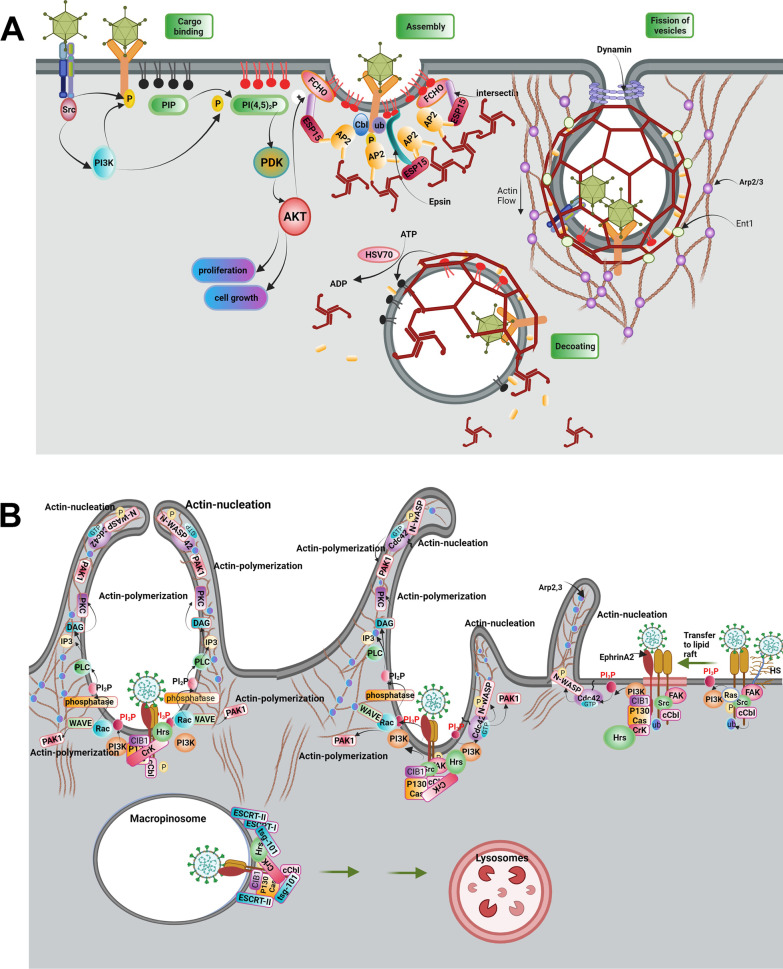
Fig. 5.
Internalization of the virus using Clathrin-dependent endocytosis (A). Virus attachment to a wide variety of cell receptors can induce activation and autophosphorylation of Src. Interaction of Src with cell surface receptors drives phosphorylation of receptors and activation of the PI3K/Akt/mTOR signaling pathway. PI3-K via activation of cCbl (E3ubiquitin ligase) multi-ubiquitylates EGFR, which drives phosphorylation and ubiquitination of receptor, then translocates virus bonded receptors into lipid raft. Ubiquitinated receptor drives phosphorylation and monoubiquitylation of EPS15 and monoubiquitylation of epsin. Epsin is a scaffold protein and binds to PI(4,5)2P in lipid rafts, cargo receptors, Esp15, AP2 protein, and clathrin molecules. Furthermore, the interaction of ESP15 with FCHO and intersectin proteins forms a trimeric FCHo/Eps15/ intersectin complex that can interact with AP2. Thus, AP2 is recruited for attachment to the membrane receptors and Clathrin molecules via interaction with FCHo/Eps15/ intersectin complex and Epsin proteins. Nucleation of AP2 can increase the local concentration of PIP2 by incrementing the activity of PIP kinase. Membrane fission of clathrin-coated vesicles is followed by the formation of dynamin helical oligomers at the neck of vesicles. After scission, vesicles are uncoated by the activity of the HSC70 chaperone, which dephosphorylates PI(4,5)P2 to PI4P, at the results clathrin coat is disassembled. Internalization mechanism of the virus by micropinocytosis (B). entry of the virus into cells is mediated by the initial attachment of the virus to the heparan sulfate and subsequently, integrins molecules, which is followed by induction of FAK, Src, Ras, and PI3K, signaling molecules. Activation of PI3-K recruits Ub-ligase cCbl which, both monoubiquitinates integrins molecules and leads them into the lipid raft on PM. In lipid rafts virus attached to the ubiquitinated integrins interacts with Ephrin A2 receptor; which results in the recruitment of CIB1 (adaptor protein)-p130Cas (scaffold protein)-Crk (effector protein) molecules to Ephrin A2-integrin -virus complex. CIB1-p130Cas-Crk complex recruits Hrs of ESCRT-0 to the site of macropinocytosis on the PM. Besides activated signaling of Ras and PI3-K induce actin nucleation and polymerization via activation of Cdc42-WASP, Rac1-WAVE complexes, and PAK1. Besides, PIP3 on the PM recruits phospholipase C (PLC), which leads producing of IP3 and diacylglycerol (DAG). DAG, in turn, recruits protein kinase C (PKC) to further promote actin polymerization. After the scission of macropinosomes by CtBP1and/or dynamin (is not shown here) recruitment of Tsg101 by Ephrin A2, c-Cbl, and associated signal molecules, and sequential recruitment of ESCRT I-III complex proteins on the endosome directs macropinosomes to the lysosomal degradation
Micropinocytosis
Micropinocytosis is involved in the entry of certain viruses from different families such as Cytomegaloviridae, Adenoviridae (adenoviruses type 3 and 35), Paramyxoviridae (Nipah virus), Orthomyxoviridae (influenza virus type A), Poxviridae (Vaccinia virus), Togaviridae (Chikungunya virus), and Reoviridae [132, 133]. This process is stimulated following the attachment of the virus to the EGFR co-receptor (Fig. 5B). The activation of tyrosine/serine kinase in receptors provokes and triggers specific downstream effectors such as PI3K, PKC, and Rac1 GTPase. Along with these changes, cytoskeletal remodeling is promoted to the invaginated plasma membrane [132]. Like clathrin-based endocytosis, the GTPase activity of dynamin and kinase activity of CtBP1 help the fission of macropinocytic vesicles [134].
Lipid raft-dependent endocytosis
Caveolae-mediated endocytosis
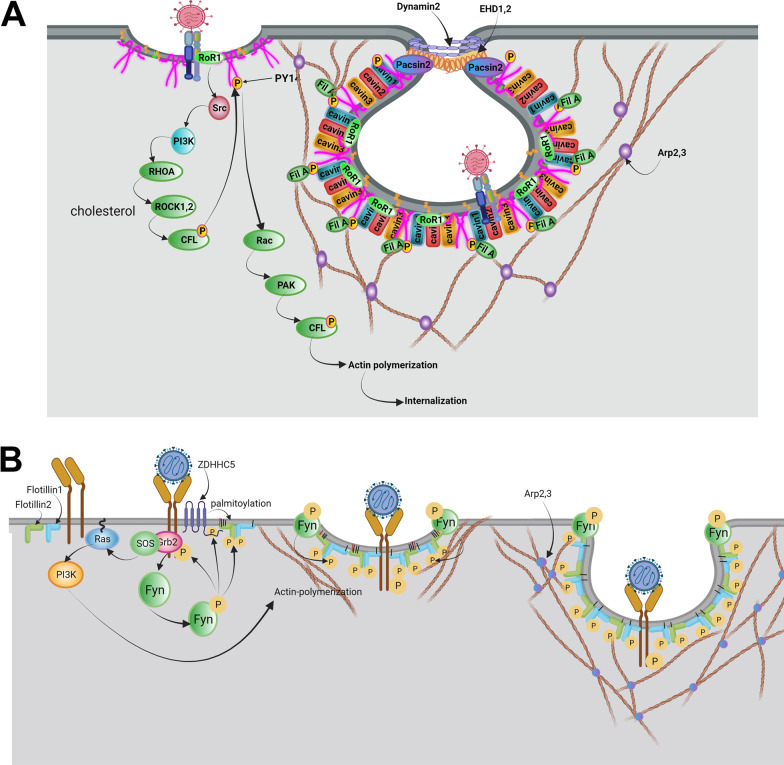
Some viruses like Simian virus 40 (SV40) exploit caveolae vesicles for cellular entry [135]. From an ultrastructural viewpoint, caveolae are multiple membrane pits that contain high contents of cholesterol and phosphatidylserine [136]. Several factors such as Caveolin1 to 3, Cavin1 to 4, and EHD2, Pacsin2, and receptor tyrosine kinase-like orphan receptor 1 (Rob1) mediate the formation of caveolae (Fig. 6A) [137]. Tyrosine residue 14 of Caveolin-1 is phosphorylated by Src kinase immediately after the attachment of the virus to the plasma membrane [138]. To be specific, Rob1 acts as a docking protein and provides a platform to make complexes by the collaboration of phosphorylated caveolin-1 with cavin [139]. These features in turn lead to the generation of caveolae-coated vesicles. Also, phosphorylated caveolin-1 can interact with cell cytoskeleton via engaging filamin A [140]. By the progression of the signaling pathway, type 2 dynamin accelerates the fission of caveolae-coated vesicles via GTPase activity in an actin-dependent manner [141].
Fig. 6.
Internalization of the virus using Caveolae-dependent endocytosis (A). Attachment of virions to the membrane receptors in membrane microdomains enriched in cholesterol and PtdSer activates receptor tyrosine kinase-like orphan receptor 1 (ROR1) and subsequently directs activation of Src, PI3K, RhoA, ROCK, CFL1 signaling pathway, at the end leads phosphorylation of Caveolin1. ROR1, as a scaffold protein, facilitates the interaction of cavin-1 and phosphorylated Caveolin1 at the PM. Also, Caveolin1 recruits EHD1,2 and Dynamin2 via binding to the Pacsin2, thus leading to the formation of the caveolae neck and session of caveolae vesicles. On the other hand, phosphorylated Caveolin1 leads to actin polymerization via the activation of Rac1, PAK1, and CFL1 signaling pathways. Caveolin1 through binding to Filamin A is associated with actin proteins and regulates caveolae vesicle trafficking. Possible mechanism of virus entry mediated by flotillin-dependent endocytosis (B). Initial attachment of the virus to the cell receptor is followed by activation of PI3K, which phosphorylates Fyn kinase, activated Fyn kinase regulates both activation of zDHHC5 and phosphorylation of Flotillins. zDHHC5 via palmitoylation of flotillin1, 2 facilitates their binding to PM. Also, phosphorylated Flotillins induce homo or heterodimerization of flotillins and the formation of invagination vesicles. Besides, activated PI3K leads to actin polymerization and changes the dynamic of the actin cytoskeleton, thus the formation of endocytic vesicles
Flotillin-dependent endocytosis
Flotillin-dependent endocytosis is involved in the internalization of some viruses such as SARS-COV-2 [142, 143]. The phosphorylation of flotillin by tyrosine kinase activity (Fyn kinase) is touted to be the most important mechanism in flotillin-dependent endocytosis (Fig. 6B). In contrast to different endocytic pathways, the fission and detachment of vesicles from an inner surface of the plasma membrane is done in the absence of dynamin [142, 143].
GRAF1-dependent endocytosis
The last mechanism that participates in the viral entry is GRAF1-dependent endocytosis which is exploited by some viral particles such as SARS-COV2, Adeno-associated virus-2 (AAV2), and SV40 [144]. The GTPase activity of GRAF1 and Cdc42 and the presence of GTP binding proteins such as ADP-ribosylation factor 1 (Arf1) help to the formation of tubular invaginations after the stimulation of actin-related proteins-2/3 (ARP2/3) in the absence of dynamin [145, 146].
Shared types of machinery between Exo biogenesis and viral replication
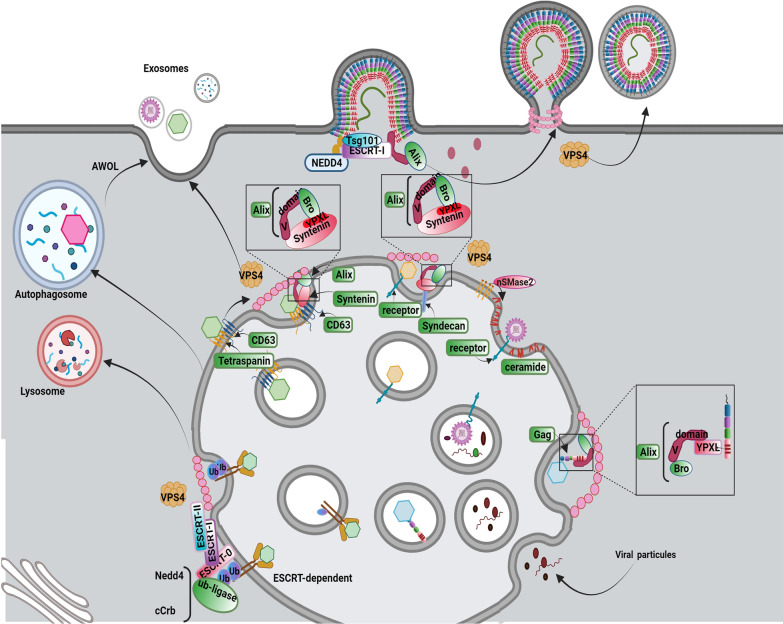
Exo can reflect instant intracellular changes and pathological conditions like viral infections and anaplastic modification after release into the ECM [11]. Whether the virions have been educated to intentionally exploit Exo trafficking machinery for transmission or the existence of different shared biogenesis systems between Exo machinery and viral replication pathway leads to accidental Exo-based delivery of viruses needs further explanation. To date, the possible positive and negative effects of viral entry on Exo biogenesis and abscission rate have not been completely addressed yet. Based on some evidence, viruses have the potential to incorporate several effectors within Exo biogenesis [147]. It is thought that common pathway between virus replication with Exo biogenesis can accelerate viral replication and abscission [147, 148]. Additionally, the decoration of viruses with host cell lipid layer helps them to enter the other cells using Exo ligands and escape from the direct and indirect activity of immune cells. On the other hand, the uptake of Exo containing viral particles by antigen presenting cells can facilitate antigen-presenting procedures [147, 148]. Therefore, the exosomal delivery of certain viruses by Exo can act as a two-edged sword in the dynamic activity of viral infections (Fig. 7).
Fig. 7.
Hijacking mechanisms Cellular adaptor proteins and complexes for promoting viral infection. There are several budding systems for the release of virions. Different enveloped viruses are driven toward PM and hijack the ESCRT pathway via mimic of interactions between cellular adaptors and ESCRT factors. Furthermore, virions invaginate into the MVB and are led to lysosomal degradation or hijack exosomal and autophagosomal pathways. Budding into the MVB is mediated by the hijacking of the ESCRT pathway via attachment to the ubiquitinated viral receptors and finally lysosomal degradation. Also, the entry of virions into the secretion pathway is mediated by the attachment of virions to CD63 and recruitment of the CD63-Syntenin-Alix pathway. In addition to the binding of the virus to the host endosomal receptors and lead formation of ILV by Syndecan-Syntenin-Alix, and formation of ceramide by nSMnase induce. Besides, capsid proteins of virion recruit Alix to the PM and lead assembly of ESCRT-III and formation of virion vesicles. Hijacking Alix protein can promote viral ILV budding and exosomal pathway. ILVs containing LC3 form autophagosome-like vesicles which mediate the exit of the virus through autophagosomal vesicles or AWOL
Contrary to the release of lytic viruses (non-permissive viruses), the exploitation of Exo biogenesis machinery by non-lytic viruses is mighty in the assembly and release steps using two distinct approaches. As above-mentioned, certain viruses mainly enveloped like enveloped virions can hijack numerous effectors related to plasma membrane fission for internalization and packaging. Regarding the existence of reverse-topology plasma membrane fission and the inevitable role of ESCRT machinery in this procedure, it is thought that ESCRT machinery can mediate, in part but not completely, the release of enveloped viruses from host cells. From a molecular structure view of point, the outward fission of the plasma membrane is done by the activity of ESCRT machinery subsets such as TSG101 of ESCRT-I, ALIX, and NEDD4L [149]. Of course, this mechanism is not the only pathway for the exosomal efflux of viruses. It is suggested that some viruses can enter MVBs in the stage of ILVs formation. This strategy can lead to two separate destinies. On one hand, some fraction of MVBs and late endosomes are directed toward enzymatic digestion by lysosomes which can confine further propagation of viruses. On the other hand, the fusion of MVBs and late endosomes to the plasma membrane can facilitate viral efflux and reach remote sites [147]. It is possible that specific components of viruses such as proteins, and nucleic acids are sorted into Exo lumen or entire viral particles (such as virions) can be transmitted to the other cells. Therefore, it is noteworthy to mention that Exo signaling pathway provides several machinery systems which are critical for viral infection and propagation. In support of this notion, the existence of some viruses such as HIV, HSV-1, rotaviruses, Langat virus, and noroviruses have been identified inside the lumen of released Exo [150]. Along with this statement, viral components of other virus types such as HIV, EBV, CMV, HSV-1, Kaposi's sarcoma-associated herpes virus (KSHV), and coronaviruses can be detected inside the Exo particles.
Invagination of viral particles using ESCRT complex
Viruses can hijack factors related to the ESCRT pathway by providing viral structural proteins that mimic natural ligand activity. To this end, virus-associated structural proteins can recruit the ESCRT complex components using certain motifs that can interact with cell surface receptors. P (T/S) AP, YPXL, and PPXY are such motifs within the viral structure that bind with surface receptors [151]. It has been indicated that the activation of P (T/S)AP motifs in the HRS subunit of ESCRT-0 can recruit ESCRT-1 TSG101 via binding of the P(T/S) AP motif with the UEV domain of TSG101 [152]. The similar structure of the P (T/S) AP motif has been indicated within viral Gag protein from Retroviridiae (such as HIV and murine leukemia virus), Z proteins of Arenaviridae (Lassa virus and lymphocytic choriomeningitis virus), VP40 proteins of Filoviridae (Ebola virus and Marburg virus), and M (Matrix) proteins of Rhabdoviridae (vesicular stomatitis virus and rabies virus) [153–157]. These factors can activate TGG101, leading to the participation of the ESCRT complex at the site of virus entry [149]. Within the cells, the YPXnL motif of syntenin can interact with the V-domain of Alix. It is believed that Alix actively is involved in the MVB pathway [158]. Many viruses belong to different families like Retroviridiae, Arenaviridae, Hepadnavirideae, Herpesviridae, Flaviviridae, Filoviridae, Paramyxoviridae, and Tombusviridae are potent to activate such mechanisms for viral particle entry [156, 159, 160]. The interaction of the viral YPnXL, motif with the V-domain of Alix can be exploited in favor of viral entry [161]. PPXY is another motif with the ability to interact with WW and HECT domains of the NEDD4 family and E3 ubiquitin ligases. The interaction promotes the ubiquitylation using NEDD4, as an ESCRT auxiliary protein, leading to the sorting of proteins into the MVBs [162]. Of note, a PPXY-like motif exists in several viruses from different families such as Retroviridiae, Rhabdoviridae [157], Arenaviridae [153], Filoviridae [156], Reoviridae [149], Hepadnavirideae [149], and Paramyxoviridae [159]. Similarly, the interaction of PPXY-NEDD4 increases the budding of the virus into the MVBs. Notably, in specific virus types such as HIV, the existence of several motifs in Gag can recall different adaptor proteins of the ESCRT system for the promotion of the budding procedure [163].
Viral efflux via ESCRT-dependent exosomal system
It is thought that both enveloped and non-enveloped viruses can be internalized into the releasing Exo via the recruitment of ESRT components or associated proteins [164, 165]. Experiments have revealed that hepatitis A virus (HAV) can be detected in the circulation in two distinct forms; naked non-enveloped capsid and quasi–enveloped virion (eHAV) [166]. The second form is resistant to host immune system activity. The release of eHAV can be done via the ESCRT subsets such as HRS and TSG101 and ESCRT-associated proteins such as Alix and VPS4. In support of this declaration, the suppression of HRS and TSG101 did not completely affect eHAV efflux while the inhibition of VPS4B and Alix led to the accumulation of eHAV inside the host cells [166]. In contrast to the eHAV, suppression of HRS significantly diminishes the exit of hepatitis C virus (HCV) release and the number of viral particles increased inside the cytosol [167]. Molecular analyses have revealed that ubiquitination of HCV core protein by E6AP (E3 ubiquitin ligase) leads to the interaction of the virus with HRS and subsequent cloaking after entrance into the endosomal membranes. According to the data, it is suggested that HCV virions can be sorted into the releasing MVBs [168]. The inhibition of MVB formation using certain chemicals such as U18666A aborts HCV release without any modification in the intracellular assembly of viral particles [167].
Viruses efflux via ESCRT-independent exosomal system
Viruses can also exploit ESCRT-independent pathways to assemble and enter into the MVBs [169]. This approach is not affected after the suppression of ATPase activity in Vps4. Whether and how different viruses can use different exosomal pathways for releasing efflux has not been fully addressed. It has been shown that several viruses belonging to the Picornaviridae family such as enteroviruses can use plasma membrane-derived and endosomal vesicles for assembly and propagation (Table 1) [169]. Among different types of enteroviruses, poliovirus can spread using autophagosome-like vesicles. This phenomenon is also known as autophagosome-mediated exit without lysis (AWOL). Other enteroviruses such as Coxsackievirus B3 (CVB3) use an AWOL-like mechanism for virion release. Besides, the efflux of CVB3 particles via microvesicles has also been proved using fluorescent timers [170]. Images provided by transmission electron microscopy have indicated the release of CVB3 virions from the host cells via engaging microvesicles. Enterovirus 71 (EV71) is another enterovirus disseminated using EVs [171]. Molecular investigations have supported the sorting of VP1 protein and RNA of EV71 virion into the EVs. Upon the completion of the efflux procedure using EVs, viruses can infect the acceptor cells. For instance, it has been shown that HPV-containing Exo can affect human neuroblastoma cell lines [171]. Data suggest the participation of different exosomal pathways for the assembly and propagation of certain virus types [172]. For example, the dissemination of the human herpes virus (HHV-6) is done by Exo. During the maturation and assembly of the HHV-6, both, Trans-Golgi network vesicular and tubular structures can be discriminated. Proteomic investigations have shown that these particles express both tetraspanins such as CD63 and HHV-6 virion proteins. Interestingly, co-localization of HHV-6 envelope protein (gB) and CD63 has been indicated in late endosomes juxtaposed to the nucleus [172]. As above-mentioned, the decoration of viral particles such as rotavirus and norovirus inside secretory vesicles can increase the possibility of infection rate [173]. Like different viruses, entrap of norovirus inside CD9+, CD81+, and CD63+ Exo has been indicated [174]. The suppression of ceramide synthesis after inhibition of sphingomyelinases via GW4869 reduces the exosomal efflux of noroviruses [169]. Based on microfluidic tracking analysis, it has been shown that the amount of rotavirus-containing vesicles and the number of vesicle proteins increased after rotavirus infection. Both microvesicles and Exo are involved in the transmission of rotavirus particles [150]. A load of viral particles can be done in terms of Exo surface or lumen. Of note, the attachment virion to the surface of EVs is not ordinary and was seen in some types of viruses like rotaviruses, polyomaviruses, HSV-1, and adenoviruses. The existence of VP4 and VP8 is suitable evidence for exosomal delivery of rotavirus [150]. Within the cells, the physical interaction of viral factor NSP4 with endoplasmic reticulum DLP provides a platform to increase the interaction of viral VP4 with lipid raft domains, resulting in the penetration of viral particles into the Exo and microvesicles [175]. In some circumstances, the completion of viral assembly is associated with the activity of Exo. For example, the transmission of the Ebola virus (EBOV) glycoprotein (GP), VP40, and nucleoprotein (NP) depend on Exo and microvesicle activity [176]. It is thought that three mechanisms exist inside Exo for the internalization of EBOV proteins [177]. First, EBO virion can enter the cell after the formation of early endosomes. Upon the release of viral genetic elements from endosomes, proteins such as VP40 and GP do not fully exist and are stable during Exo biogenesis [177]. In the second mechanism, EBOV proteins are transferred into the ILV lumen inside the MVBs. The ubiquitination of VP40 promotes its entry into the Exo via the collaboration of the ESCRT complex. Along with these activities, GP can be guided into Trans-Golgi vesicles and viral RNA (NP) is directed into Exo via unknown mechanisms. In the latter mechanism, viral particles can be released into the ECM after outward budding from plasma membrane. Noteworthy, viral protein VP40 is attached to the vesicle surface while both NP and RNA are located at inner surface of vesicle membrane [177].
Table 1.
Mechanisms used by several virus types to release from the host cells
| Type of virus | Family | Intracellular transfer | Hijacking mechanism | Releasing mechanisms | Reference |
|---|---|---|---|---|---|
| Enveloped DNA viruses | |||||
| Epstein-Barr Virus | Herpesviridae | ESCRT-dependent and ESCRT-independent pathways | TSG101, CD63, Syntenin‑1, Alix, and lipid rafts | Late endosomes | [195, 196, 238] |
| Kaposi's sarcoma-associated herpesvirus | Herpesviridae | ESCRT-dependent and ESCRT-independent pathways | Viral LMP1 | Late endosomes | [182, 239] |
| Human Herpes virus-6 | Herpesviridae | ESCRT-independent pathway | CD63 and viral gB | Late endosomes | [172] |
| Human Cytomegalovirus | Herpesviridae | ESCRT-independent, Vamp3-dependent pathways | VAMP3, viral pUL71 and UL99 | Late endosomes | [197, 240] |
| Herpes simplex virus 1 | Herpesviridae | ESCRT-dependent pathway | ESCRT-III |
Microvesicular budding, Autophagosome-mediated exit without lysis, Late endosomes |
[241, 242] |
| Non-enveloped DNA viruses | |||||
| Adenoviruses 2 and 5 | Adenoviridae | ESCRT-independent pathway | Exosomal CD46, Lamp2c | Late endosomes, Microvesicular budding | [181, 243, 244] |
| Hepatitis B virus | Hepadnavirideae | ESCRT-dependent pathway | α-taxilin, viral LHBs, TSG101, 2-adaptin, Nedd4 | Late endosomes, Microvesicular budding | [245] |
| Enveloped RNA viruses | |||||
| Japanese encephalitis virus | Flaviviridae | ESCRT-dependent pathway | viral NS3, TSG101 | Late endosomes | [246, 247] |
| Yellow fever virus | Flaviviridae | ESCRT-dependent pathway | Viral NS3 protein, Alix | Late endosomes | [248, 249] |
| Dengue virus | Flaviviridae | ESCRT-dependent pathway | Viral NS3, Alix, viral protein E, Tsp29Fb | Late endosomes | [186, 187, 249, 250] |
| West Nile virus | Flaviviridae | ESCRT-dependent pathway | Viral NS3, Alix and ESCRT | Late endosomes | [249] |
| Zika virus | Flaviviridae | ESCRT-dependent pathway | Viral NS3 protein interacts with Alix | Late endosomes | [249, 251] |
| Tick-borne encephalitis | Flaviviridae | ESCRT-dependent pathway | ND | Late endosomes | [249] |
| Hepatitis C Virus | Flaviviridae | ESCRT-dependent pathway | Viral NS2 and NS5A proteins, Ago2, HSP90, and CD81 | Late endosomes | [252–254] |
| Human immunodeficiency virus-1 | Retroviridiae | ESCRT-dependent pathway | Viral Nef, Alix, viral Gag, and Syntenin | Late endosomes | [161, 191, 255, 256] |
| Equine Infectious Anemia Virus | Retroviridiae | ESCRT-dependent pathway | Viral Gag, Alix |
Late endosomes TGN is the assembly site |
[257] |
|
Feline immunodeficiency virus |
Retroviridiae | ESCRT-dependent pathway | Viral Gag, and Alix | Microvesicular budding | [258, 259] |
| Human immunodeficiency virus-2 | Retroviridiae | ESCRT-dependent pathway | Viral Nef, Alix and viral Gag, and TSG-101 | Late endosomes, Microvesicular budding | [260, 261] |
| Mouse Mammary Tumor Virus | Retroviridiae | ESCRT-dependent pathway | Viral Gag and NEDD4 | ND | [262] |
| Murine Leukemia Virus | Retroviridiae | ESCRT-dependent pathway | Viral Gag and WWP1 | Late endosomes, Microvesicular budding | [260, 263, 264] |
|
Porcine endogenous retrovirus |
Retroviridiae | ESCRT-dependent pathway | Viral Gag, and WWP2 | Late endosomes | [265] |
| Prototypic foamy viruses | Retroviridiae | ESCRT-dependent pathway | Viral Gag, TSG-101, and PPPI | Late endosomes, Microvesicular budding, trans-Golgi network | [266, 267] |
| Mason–Pfizer monkey virus | Retroviridiae | ESCRT-dependent pathway | Viral Gag, TSG-101 and NEDD4 | Microvesicular budding | [268, 269] |
|
Human T cell leukemia virus type 1 |
Retroviridiae | ESCRT-dependent pathway | Viral Gag, TSG-101 and NEDD4 | Late endosomes | [260, 270] |
| Human endogenous retrovirus-K | Retroviridiae | ESCRT-dependent pathway | Viral Gag, TSG-101 | Late endosomes | [271, 272] |
| Rous sarcoma virus | Retroviridiae | ESCRT-dependent pathway | Gag, NEDD4 and Alix | Late endosomes | [273, 274] |
| Respiratory syncytial virus | Pneumoviridae | ESCRT-independent pathway | ND | Late endosomes | [46] |
| Human Pegivirus, GB virus C | Flaviviridae | ESCRT-dependent pathway | hnRNPA2B1 protein | Late endosomes | [275, 276] |
| Ebola virus | Flaviviridae | ESCRT-dependent pathway | Viral VP40, TSG-101, NEDD4, and VP24 | Late endosomes, Microvesicular budding | [277, 278] |
| Marburg virus | Flaviviridae | ESCRT-dependent pathway | TSG-101, Viral VP40 and NEDD4 | Microvesicular budding | [279–281] |
| Lassa fever virus | Arenaviridae | ESCRT-dependent pathway | Z protein and TSG-101 | Microvesicular budding | [282, 283] |
| Rabies Virus | Rhabdoviridae | ESCRT-dependent pathway | Viral M protein, ESCRTI, Alix, ESCRT III and VPS4 | Microvesicular budding | [284, 285] |
| Vesicular stomatitis virus | Rhabdoviridae | ESCRT-dependent pathway | Viral M protein, TSG-101, and NEDD4 | Microvesicular budding | [286] |
| Parainfluenza virus 5 | Paramyxoviridae | ESCRT-dependent pathway | Viral M protein, and VPS4 ATPase | Microvesicular budding | [287] |
| Parainfluenza virus 3 | Paramyxoviridae | ESCRT-dependent pathway | Viral M protein | Microvesicular budding | [288] |
| Newcastle disease | Paramyxoviridae | ESCRT-dependent pathway | Viral M protein and VPS4 ATPase | Microvesicular budding | [289] |
| Mumps virus | Paramyxoviridae | ESCRT-dependent pathway | Viral M protein and VPS4 ATPase | Microvesicular budding | [290] |
| Hepatitis E virus | Hepeviridae | ESCRT-dependent pathway | Viral pORF3, and TSG-101 | Late endosomes | [291, 292] |
| Non-enveloped RNA viruses | |||||
| Hepatitis A virus | Picornaviridae | ESCRT-dependent pathway | Viral VP2, Alix and VPS4B | Late endosomes | [166, 293] |
| Coxsackievirus B | Picornaviridae | ESCRT-dependent pathway | LC3 | Microvesicular budding, Autophagosome-mediated exit without lysis and | [294] |
| Poliovirus | Picornaviridae | ESCRT-dependent and independent pathways | Alix | Microvesicular budding, Autophagosome-mediated exit without lysis and | [165] |
| Enterovirus 71 | Picornaviridae | ESCRT-dependent pathway | ND | Late endosomes | [295–297] |
| Reovirus | Reoviridae | ESCRT-dependent pathway | Rab5, Viral capsid protein P2 | Late endosomes, modified lysosomal organelle act as transporter virions to the plasma membrane | [184, 298] |
| Rotavirus | Reoviridae | Probably ESCRT-dependent pathway | Probably VP4 interacts with lipid Rafts | Microvesicular budding | [150] |
| Norovirus | Caliciviridae | Probably ESCRT-dependent pathway | Viral VP1, Phosphatidylserine lipid | Late endosomes | [174] |
It should not be forgotten that the Trojan activity of each virus can be used for several therapeutic purposes [178]. For instance, oncolytic adenovirus-loaded EVs can be used for successful transfection and genetic manipulation of cancer cells [179]. Further propagation and viral spread are done by different proposed mechanisms. Viral bodies can be externalized from host cells after the formation of membrane-associated microvesicles. The attachment of viral components inside the lumen and surface of MVBs has touted another underlying mechanism for the efflux of adenoviral infection out of the host cells [180]. Finally, the invagination of ILVs inside the MVB lumen can also help viral propagation. As described in Exo signaling pathway, some of MVBs may be directed toward the lysosomal degradation procedure [181]. Similarly, the transfer of KSHV genetic materials from cell to cell has been documented using Exo [182]. Even though, the transfer of Exo-containing KSHV RNA can dictate specific metabolic conditions in recipient cells. For example, upon the entry of KSHV-loaded Exo, the respiration capacity of mitochondria is diminished coinciding with the induction hypoxic condition. One reason would be that KSHV-infected cells produce Exo which contains a large amount of lactate dehydrogenase, resulting in the shift of oxidative phosphorylation toward glycolysis [182]. Because of the diversity in viral activity and the existence of different pathogenic molecules in the structure of viruses, it is logical to hypothesize that viruses can, in part, exploit different parts of the Exo signaling pathway. Previous studies confirmed the critical role of Exo in the dissemination of non-lytic human reoviruses from host cells to neighbor cells. This virus is transferred as virion bodies by complete incorporation into an exosomal system [183]. Considering the phylogenetic association of the Exo-related pathway, the mechanism of viral hijack has some similarities between the species. Reoviruses can maintain specific interaction between the nucleocapsid domain and intracellular Rab5, participating in virus packaging via releasing Exo [184]. Concerning transport activity, reoviruses can also bind to specific motifs RGD and KGE, and NPXY of λ2 nucleocapsid to the carboxylic domain of β1 integrin and enter the endosomes [183, 185]. In another study, it was shown that the entry and release of Dengue virus (DENV), belonging to Flaviviridae and transmitted by mosquitoes, can be done by Exo. Analyses have confirmed the entry of DENV into the Exo can increase exosomal diameter compared to intact Exo. Interestingly, these Exo can fit complete and fragmented viral components [186]. It is believed that human CD63 ortholog namely Tsp29Fb, a member of the tetraspanin complex, is responsible for viral loading into the Exo lumen via direct interaction of viral E protein with Tsp29Fb [187]. Within the pulmonary niche, the influenza virus can be easily transmitted between epithelial cells via Exo. These Exo can harbor viral antigens, proteins, and genetic materials in addition to inflammatory factors [188, 189]. Evidence points to the fact under specific conditions the dynamic viral infection and Exo biogenesis are closely interconnected [190]. For example, the infection of cells with the rabies virus can reduce the transit time of Exo inside the cytosol, leading to an accelerated Exo release. The inhibition of Exo secretory mechanism using certain chemical s and GW4869 and si-Rab27a leads to apparent reduction of Exo biogenesis and elimination of viral RNA [190].
HIV is another virus that uses several dissemination mechanisms. This virus provides motifs Gag protein which is actively involved in the formation of budding from the plasma membrane. Besides, the invagination of early endosomes and formation of ILVs are integral to the transport of HIV Nef protein and vmiRTAR, and finally, the release of viral Tat protein via budding and direct diffusion can help viral particle dissemination [191]. Using an Exo-based delivery system, HIV can be resistant to the host immune system for a long time. The replication of HIV has not been shown. Interestingly, HIV-loaded Exo have significant fusion capacity due to the fusogenic activity of the Tat factor. It seems that the internalization of HIV-loaded Exo can be promoted via ESCRT-dependent and associated proteins. In Nef containing Exo, ALIX is provoked to internalize the Exo cargo. It has been shown that Nef can regulate the sorting of RNAs into the Exo lumen. For example, the activity of RNA-TAR (miRTAR) is regulated by Nef, leading to rapid viral propagation inside the host cells [192, 193]. Epstein–Barr virus (EBV) belongs to the oncovirus with tumorigenic activity [194]. Notably, the existence of specific microenvironment conditions such as hypoxia and low-pH rates increase Exo and propagation of EBV [195]. The procedure of EBV-encoded RNA (EBER) and LMP-1 loading into the Exo lumen is associated with ESCRT complex activity. Other associated factors such as HRS, TSG101, CD63, Syntenin-1, and Alix facilitate sorting into Exo [196]. To be specific, the direct interaction of LMP-1 with CD63 and/or physical attachment of LMP-1 to lipid rafts promotes cargo sorting into Exo and spread viral particles in immune cells [196]. Proteomic analysis of Exo released from cells infected with HCMV showed the common membrane origin between the virions and Exo. Data indicated that viruses use Exo ESCRT machinery for assembly and transmission with the collaboration of VMP3 [197].
Angiotensin-converting enzyme 2 (ACE2) is a membrane-bound receptor that can attach to spike ligands belonging to the Coronaviridae family. It is thought that the participation of CD9, a tetraspanin component, can facilitate the entry of certain coronaviruses into the cells. CD9 and dipeptidyl peptidase 4 (DPP4) in collaboration with transmembrane protease serine subtype 2 (TMPRSS2) act as linkers for the physical attachment of spike proteins to the host cell membrane, leading to the fusion of the virus with the host cells [198]. Regarding the critical role of CD9 in the sorting into Exo, the existence of CD9 in released Exo is a common feature of virus-infected cells which use the Exo signaling pathway [88]. As mentioned before, rotaviruses can exploit the Trans-Golgi apparatus for propagation and dissemination. On this basis, the close interaction of GBF1 with NSP4 induces trimerization of VP7, and the association of assembly protein VP7 and spike protein VP4 [175]. In the next steps, VP4 is localized to lipid raft microdomains Trans-Golgi apparatus, leading to rotavirus capsid assembly. Simultaneously, the formation of NSP4/VP7/VP4 in the lipid raft microdomains or ERGIC compartments is initiated [199]. It seems that ERGIC35 can promote the entry of VP4 (spike protein) and VP7 (assembly protein) into the vesicles [200]. The critical role of lipid rafts domains with high levels of cholesterol and sphingolipids is integral to cargo sorting [201, 202].
It is believed that Tetraspanin microdomains of CD9, CD63, CD81, and/or CD82 can provide large fusion areas or budding platforms [203]. Previously, the accumulation of components of the ESCRT complex for the efflux of viral particles has been indicated at the site of budding after infection with HIV and HAV [204–206]. In line with this claim, the application of anti-Tetraspanin antibodies can significantly alter viral internalization or fusion [207]. As such, these antibodies are potent enough to inhibit the coronavirus and low-pathogen influenza virus infection [208].
Within the host cells, several signaling cascades can be exploited by viruses. For example, viruses like influenza, HSV1, HIV1, etc. can hijack PI3K/Akt axis for effective viral entry [209]. Unlike these viruses, certain viruses infecting epithelial cells such as porcine sapovirus, SARS COV-2, and other viruses use can tight junctions (TJs) and relevant downstream RhoA/ROCK/pMLC signaling pathways to access co-receptors required for viral entry [210–212]. In this line, the interaction of viral particles with cell surface receptors activates Src kinases and induces downstream signaling pathways. It was suggested that Src associates with cell surface receptors directly, G-protein-coupled receptors (GPCRs), and receptors of tyrosine kinases (RTKs), and indirectly, integrin-mediated by focal adhesion kinase (FAK), leading to the phosphorylation of Rho GTPases and PI3K [209, 213]. As a correlate, the inhibition of EGFR and PI3K phosphorylation plus PIP2 can reduce viral uptake [214]. Src can associate lipid rafts and interfere in the biogenesis and secretion of Exos. This activity is done by the phosphorylation of the cytosolic domain of syndecan and syntenin tyrosine 46 via Src [215]. Besides, the close interaction of Src with Alix induces ILV formation [216].
Challenges and opportunities associated with exosomal delivery of viruses
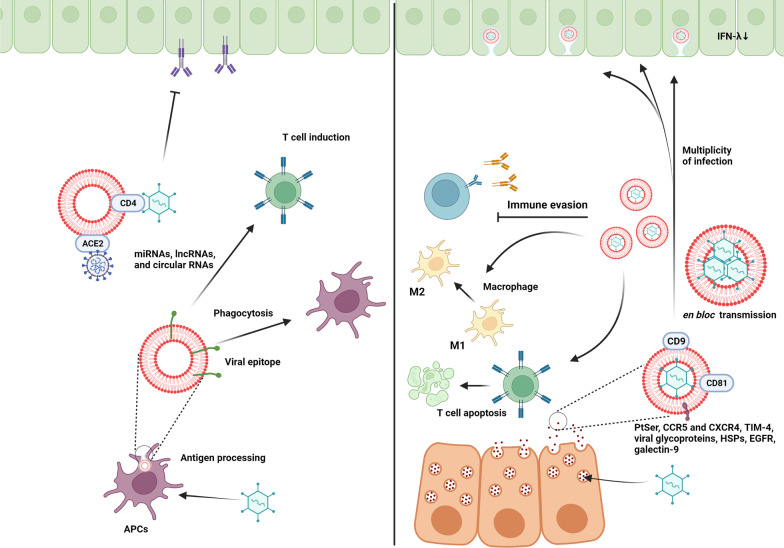
As previously mentioned, viruses can replicate following the entry into the host cells, leading to cytopathic effects and tissue damage. Within the body, the activation of the host immune system control virus replication and transmission of infectious particles at early steps [217]. According to some data, specific types of viruses can hijack multiple secretion pathways of the host cells such as Exo biogenesis machinery. Thus, one could hypothesize that the formation of an exosomal lipid membrane around viral particles can act as a natural barrier and prevent direct contact of immune cells with viral components [218]. Given the fact that Exo can distribute within the whole body, it is thought that viruses can easily spread to remote sites using Exo as a biological transport system. To be specific, the increase of Exo secretion accelerates the propagation of viral bodies from the secreting cells to acceptor cells (Fig. 8; Table 2) [219]. In support of this notion, it has been shown that EVs can release CCR5 and CXCR4 which act as receptors and co-receptors for the entry of HIV into the target cells. The lack of these factors limits the transmission of this virus into non-talent cells. Like the HIV envelope, the existence of phosphatidylserine receptor TIM-4 on the Exo surface can increase the HIV transfection rate [220]. Logically, the simultaneous transmission of the viral body with signaling molecules increases the possibility of infection in non-talent receptor-negative cells, leading to accidental viral infection via the Exo machinery. In non-envelop viruses such as HAV and hepatitis E virus (HEV), Exo can constitute a pseudo-envelope around these particles and act as a Trojan horse for massive propagation [218]. Therefore, it seems that the close interaction of viral components with an exosomal delivery system can lead to a multiplicity of infections. In an experiment, the production of engineered Exo containing high levels of 29-mer peptide, rabies virus glycoprotein, increased the interaction of these Exo with acetylcholine receptors in neural cells [7]. Interestingly, EVs transmit viruses as single particles or clustered aggregates linked tightly via spatiotemporal coupling such as enteroviruses, leading to en bloc transmission of viruses [221]. Ultrastructural imaging and molecular investigations have revealed that Exo are eligible bioshuttles to carry infectious virion-free naked genomes or proteins into the uninfected cells. For example, exosomal transfer of HCV replicon in in vitro conditions has led to cell infection with less efficiency [222]. Despite these possibilities, communications and interaction between the cells via Exo is more complicated rather than a simple transfer procedure.
Fig. 8.
Opposing effects of Exo on viral infectivity and immunity
Table 2.
Mechanisms related to Exo-based viral immunity and tolerance
| Virus type | Immunity mechanisms | Outcome |
|---|---|---|
| Various viruses | Exosomal miR-146a↑ and miR-148a↑ | Inflammatory response ↑ |
| Rabies virus | Exosomal miR-423-5p↑ | IFNβ-related signaling pathway↑, Early-stage viral immunity↑ |
| HCV | Exosomal miR-21↑, miR-29a↑, miR-19a↑, and miR-192 | Immune system regulation↑ |
| HBV | Exosomal miR-192↑, miR-21↑, miR-215↑, miR-221↑, and miR-222↑, miR-29a↑, HBx↑, HBV pre-genomic RNA↑ | Immune system regulation↑, Il-12↓, Il-6↓, PDL-1↓ |
| EBV | Exosomal miR-21↑, miR-29a↑, miR-BART3↑, miR-BHRF1-1↑, LMP1 ↑ | Macrophage IL-12↓, NK cells activity ↓, modulation of the immune response, T cell proliferation↓ |
| Dengue virus-2 | Viral NS3 protein↑ and several special miRNAs↑ | Early defense program↑ |
| HSV-1 | Exosomal miR-H28↑ and miR-H29↑, glycoprotein B↑ | Regulation of immune function |
| Enterovirus 71 | Exosomal miR-146a↑ | IFN-related pathway in immune cells↓ |
| Ebola virus | Exosomal VP40 NP↑, Glycoprotein↑ | Apoptosis of T, B cells, and monocytes↑ |
| Japanese encephalitis virus | Exosomal miR-let-7a/b↑ | Apoptotic pathways↑ |
| HIV | Exosomal miR-16↓, miR-125b↓, miR-146a↑, miR-21↑, Nef↑ | Immune response↑, pro-inflammatory cytokines↑, activation of monocytes and macrophages↑ |
| Polyomavirus 2 | Exosomal jcv-miR-J1-5p↑, jcv-miR-J1-3p↑ | large T antigen↓, UL16-binding protein 3↓, NK cell activity↓, viral infection ↑ |
| Rhinovirus | Exosomal miR-155↑, Tenascin-c↑ | Pro-inflammatory cytokines↑ |
| Influenza A virus | Exosomal miR-17-5p↑, miR-483-3p, 5p↑, mir-374-5p↑, and miR-446i↑, miR-451a↑, miR-5100↑ and miR-7704↑ |
miR-17-5p leads to antiviral factor Mx1↓, and viral infection↑ The induction of miR-483-3p, 5p↑, mir-374-5p↑, and miR-446i↑, miR-451a↑, miR-5100↑ and miR-7704↑ can contribute to reduction of viral infection via IFN-β↑, IL-6↑, TNF-α↑, C–C motif chemokine ligand 2 (CCL2)↑, SP100↑ |
Although explored to a lesser extent, Exo can protect viruses against several immune cell reactions via distinct mechanisms. Membrane-cloaked viruses can efficiently evade neutralizing antibodies [223]. Besides non-lytic spread of viruses from the host cells reduce pro-inflammatory responses and the possibility of necrotic changes and decoration of the Exo surface with certain factors reduces immune cell reactivity [221]. It is thought that the existence of MHC molecules on the exosomal surface diminishes the presentation of viral antigens to the APCs [224]. In addition to the critical role of Exo in hiding viral antigens from the immune system, the existence of distinct biomolecules in the exosomal lumen and membrane can in turn weaken immune cell response. The molecular identity of Exo exhibits certain factors such as HSPs (HSP72) with the ability to activate STAT-3, leading to immunosuppression via reduced M1 to M2 macrophage polarization [225, 226]. Besides, the existence of several growth factors and receptors such as EGFR can lead to the desensitization of macrophages against particles via engaging MEKK2 and IRF3 [227]. Likewise, EBV-infected cells release Exo which are enriched in galectin-9. This factor can promote apoptotic changes in type 1 T helper lymphocytes [228]. Other viral genetic pools transferred via Exo can modulate apoptosis in immune cells. SARS-CoV-2 infected cells can shed Exo with certain viral RNA and high content of Orf2, 3a, 4, 5, 6, 7a, and 9 proteins and ACE2+ [229, 230]. It has been shown that SARS-CoV-2 Orf6 can neutralize the nuclear translocation of STAT1 and 2 and suppress the expression of IFN-stimulated genes, leading to impaired cellular immunity against viruses [231]. The transfer of viral particles inside circulating Exo is related to the lack of direct physical interaction of viral antigens with antibody-producing lymphocytes as seen in COVID-19 patients. It is noteworthy to mention that most contents of Exo RNAs remain intact during viral infection, indicating that the immune-modulatory properties of Exo are still stable [232]. As such, it can be concluded that the exosomal delivery of viruses can contribute to the distribution of infectious particles using either viral or Exo equipment.
In addition to supporting the role of Exo in the propagation of viral infections, virus-carrying Exo can also act as a decoy for immune cells. For example, the production of Exo with a specific proteomic signature containing high levels of ACE2, also known as defensosomes, has been indicated. The Exo can prohibit the entry of SARS-CoV-2 to other cells via direct binding spike protein on the virus surface [230]. Besides, recently it was suggested that circulatory Exo isolated from COVID-19 patients contained higher proteins associated with inflammation, coagulation, and immune response [229]. To this end, Barberis and co-workers found a significant increase in levels of certain factors such as alpha-1-acid glycoprotein 1, C-reactive protein, lysozyme C, titin, and zinc-alpha-2-glycoprotein in Exo isolated from COVID-19 patients. They also showed the increase of IL-12, NO, ROS, and elevation of factors associated with coagulation, prothrombin activation, and clathrin-mediated endocytosis [229]. Unlike non-immune cells, effector APCs can introduce viral epitopes inside EVs during antigen processing. EVs containing viral epitopes can be easily reached by neighboring APCs at proximity or remote sites and frustrate them in the absence of complete virion or necessary elements, resulting in provoking acquired immunity (Fig. 8). Along with these statements, the entry of APC-associated EVs into the uninfected non-APCs can trigger specific signaling pathways that limit viral replication and transmission [233]. Exo-carrying viral genetic materials such as miRNAs, lncRNAs, and circular RNAs can induce anti-viral immunity inside the target cells [234]. The elevated miR-423-5p contents in Exo-isolated from rabies virus infection can limit viral infection via the induction of the interferon signaling pathway [235]. In an experiment, the incubation of human macrophages with IFN-α produces Exo that are rich in DNA cytidine deaminase APOBEC3G, leading to the protection of hepatocytes against HBV [236]. The existence of receptors on the Exo surface can also limit virus infection. For example, it was shown that T cell-derived Exo can carry CD4 with the potential to bind and neutralize HIV virus. On the other hand, the infection of host cells with HIV and production viral Nef can per se reduce the levels of CD4 on Exo surface and promote viral infectivity [237].
Conclusion
Despite recent advances in the understanding of the intersection between viral replication and Exo biogenesis, the exact underlying mechanisms remain to be understood. It seems that Exo can act as natural bioshuttles to cover the viral particles in direct contact with immune cells and increase the entry of viruses due to surface ligands which are more important for envelope viruses. On the other hand, the existence of other signaling molecules can limit the virus’s propagation to non-infected cells. These features show the opposing effects of Exo on viral infections and more investigations are highly recommended to address these issues.
Acknowledgements
Authors wish to thank the personnel of the Faculty of Advance Medical Sciences for guidance and help.
Abbreviations
- AP-2
Adaptor protein-2
- AAV2
Adeno-associated virus-2
- ACE2
Angiotensin-converting enzyme 2
- AWOL
Autophagosome-mediated exit without lysis
- CVB3
Coxsackievirus B3
- DPP4
Dipeptidyl peptidase 4
- dsDNA
Double-stranded DNA
- ESCRT
Endosomal sorting complexes required for transport machinery
- EV71
Enterovirus 71
- EBV
Epstein–Barr virus
- Exo
Exosomes
- ECM
Extracellular matrix
- EV
Extracellular vesicles
- FAK
Focal adhesion kinase
- GPCRs
G-protein-coupled receptors
- HSC70
Head shock cognate protein 70
- HSPs
Heat shock proteins
- HAV
Hepatitis A virus
- HCV
Hepatitis C Virus
- HEV
Hepatitis E virus
- HRS
HGF-regulated tyrosine kinase substrate
- HD-PTP
Histidine domain protein tyrosine phosphatase
- HHV-6
Human herpes virus
- ILVs
Intraluminal vesicles
- MVs
Microvesicles
- mtDNA
Mitochondrial DNA
- MVBs
Multivesicular bodies
- nSMase 2
Neutral sphingomyelinase 2
- PI3K
Phosphatidylinositol 3-kinase
- PI3P
Phosphatidylinositol-3-phosphate
- PKC
Protein kinase C
- eHAV
Quasi–enveloped virion
- Rob1
Receptor tyrosine kinase-like orphan receptor 1
- RTKs
Receptors of tyrosine kinases
- STAM
Signal transducing adaptor molecule
- SV40
Simian virus 40
- ssDNA
Single-stranded DNA
- SNAREs
Soluble N-ethylmaleimide-sensitive factor attachment protein receptors
- TEM
Tetraspanin membrane microdomains
- TMPRSS2
Transmembrane protease serine subtype 2
- VAMP
Vesicle-associated membrane proteins
Author contributions
NM, SH, HM, ES, and AZ collected data and prepared the manuscript. RR, MN and MM supervised the study. All authors read and approved the final manuscript.
Funding
This is a report of the database from a Ph.D. thesis registered in Tabriz University of Medical Sciences under the supervision of Dr. Mohammad Nori with the number 66627 and Ethical code IR.TBZMED.VCR.REC.1399.055.
Availability of data and materials
All data generated or analyzed in the manuscript are included in this article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Authors declare there is no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reza Rahbarghazi, Morteza Milani, and Mohammad Nouri have contributed equally to this work
Contributor Information
Reza Rahbarghazi, Email: Rezarahbardvm@gmail.com, Email: rahbarghazir@tbzmed.ac.ir.
Morteza Milani, Email: milanimo@tbzmed.ac.ir.
Mohammad Nouri, Email: Nourimd@yahoo.com.
References
- 1.Rezabakhsh A, Sokullu E, Rahbarghazi R. Applications, challenges and prospects of mesenchymal stem cell exosomes in regenerative medicine. Stem Cell Res Ther. 2021;12(1):1–8. doi: 10.1186/s13287-021-02596-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan M-H, Chang Z-X, Huang C-YF, Lee LJ, Liu R-S, Hsiao M. Integrated therapy platform of exosomal system: hybrid inorganic/organic nanoparticles with exosomes for cancer treatment. Nanoscale Horizons; 2022. [DOI] [PubMed]
- 3.Amini H, Rezabakhsh A, Heidarzadeh M, Hassanpour M, Hashemzadeh S, Ghaderi S, Sokullu E, Rahbarghazi R, Reiter RJ. An examination of the putative role of melatonin in exosome biogenesis. Front Cell Dev Biol. 2021;9:686551. doi: 10.3389/fcell.2021.686551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gurunathan S, Kang M-H, Kim J-H. A comprehensive review on factors influences biogenesis, functions, therapeutic and clinical implications of exosomes. Int J Nanomed. 2021;16:1281. doi: 10.2147/IJN.S291956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaudhari P, Ghate V, Nampoothiri M, Lewis S. Multifunctional role of exosomes in viral diseases: From transmission to diagnosis and therapy. Cell Signal. 2022;110325. [DOI] [PMC free article] [PubMed]
- 6.Izquierdo-Useros N, Naranjo-Gómez M, Erkizia I, Puertas MC, Borràs FE, Blanco J, Martinez-Picado J. HIV and mature dendritic cells: Trojan exosomes riding the Trojan horse? PLoS Pathog. 2010;6(3):e1000740. doi: 10.1371/journal.ppat.1000740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saad MH, Badierah R, Redwan EM, El-Fakharany EM. A comprehensive insight into the role of exosomes in viral infection: dual faces bearing different functions. Pharmaceutics. 2021;13(9):1405. doi: 10.3390/pharmaceutics13091405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Niel G, d'Angelo G, Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat Rev Mol Cell Biol. 2018;19(4):213. doi: 10.1038/nrm.2017.125. [DOI] [PubMed] [Google Scholar]
- 9.Xu R, Rai A, Chen M, Suwakulsiri W, Greening DW, Simpson RJ. Extracellular vesicles in cancer—implications for future improvements in cancer care. Nat Rev Clin Oncol. 2018;15(10):617–638. doi: 10.1038/s41571-018-0036-9. [DOI] [PubMed] [Google Scholar]
- 10.Van der Pol E, Böing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol Rev. 2012;64(3):676–705. doi: 10.1124/pr.112.005983. [DOI] [PubMed] [Google Scholar]
- 11.Rajabi H, Konyalilar N, Erkan S, Mortazavi D, Korkunc SK, Kayalar O, Bayram H, Rahbarghazi R. Emerging role of exosomes in the pathology of chronic obstructive pulmonary diseases; destructive and therapeutic properties. Stem Cell Res Ther. 2022;13(1):144. doi: 10.1186/s13287-022-02820-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teng F, Fussenegger M. Shedding Light on Extracellular Vesicle Biogenesis and Bioengineering. Advanced Science. 2020;2003505. [DOI] [PMC free article] [PubMed]
- 13.Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science.2020; 367 (6478). [DOI] [PMC free article] [PubMed]
- 14.Hessvik NP, Llorente A. Current knowledge on exosome biogenesis and release. Cell Mol Life Sci. 2018;75(2):193–208. doi: 10.1007/s00018-017-2595-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagano M, Toshima JY, Siekhaus DE, Toshima J. Rab5-mediated endosome formation is regulated at the trans-Golgi network. Commun Biol. 2019;2(1):1–12. doi: 10.1038/s42003-019-0670-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rezabakhsh A, Sokullu E, Rahbarghazi R. Applications, challenges and prospects of mesenchymal stem cell exosomes in regenerative medicine. Stem Cell Res Ther. 2021;12(1):521. doi: 10.1186/s13287-021-02596-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kenific CM, Zhang H, Lyden D. An exosome pathway without an ESCRT. Cell Res. 2021;31(2):105–106. doi: 10.1038/s41422-020-00418-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parkinson MD, Piper SC, Bright NA, Evans JL, Boname JM, Bowers K, Lehner PJ, Luzio JP. A non-canonical ESCRT pathway, including histidine domain phosphotyrosine phosphatase (HD-PTP), is used for down-regulation of virally ubiquitinated MHC class I. Biochem J. 2015;471(1):79–88. doi: 10.1042/bj20150336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coudert L, Osseni A, Gangloff YG, Schaeffer L, Leblanc P. The ESCRT-0 subcomplex component Hrs/Hgs is a master regulator of myogenesis via modulation of signaling and degradation pathways. BMC Biol. 2021;19(1):153. doi: 10.1186/s12915-021-01091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heidarzadeh M, Gürsoy-Özdemir Y, Kaya M, Eslami Abriz A, Zarebkohan A, Rahbarghazi R, Sokullu E. Exosomal delivery of therapeutic modulators through the blood–brain barrier; promise and pitfalls. Cell Biosci. 2021;11(1):142. doi: 10.1186/s13578-021-00650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tan J, Davies BA, Payne JA, Benson LM, Katzmann DJ. Conformational changes in the endosomal sorting complex required for the transport III subunit Ist1 lead to distinct modes of ATPase Vps4 regulation *. J Biol Chem. 2015;290(50):30053–30065. doi: 10.1074/jbc.M115.665604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stoten CL, Carlton JG. ESCRT-dependent control of membrane remodelling during cell division. Semin Cell Dev Biol. 2018;74:50–65. doi: 10.1016/j.semcdb.2017.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leblanc R, Kashyap R, Barral K, Egea-Jimenez AL, Kovalskyy D, Feracci M, Garcia M, Derviaux C, Betzi S, Ghossoub R, Platonov M, Roche P, Morelli X, Hoffer L, Zimmermann P. Pharmacological inhibition of syntenin PDZ2 domain impairs breast cancer cell activities and exosome loading with syndecan and EpCAM cargo. J Extracell Vesicles. 2020;10(2):e12039. doi: 10.1002/jev2.12039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Larios J, Mercier V, Roux A, Gruenberg J. ALIX- and ESCRT-III-dependent sorting of tetraspanins to exosomes. J Cell Biol. 2020 doi: 10.1083/jcb.201904113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heidarzadeh M, Gürsoy-Özdemir Y, Kaya M, Eslami Abriz A, Zarebkohan A, Rahbarghazi R, Sokullu E. Exosomal delivery of therapeutic modulators through the blood–brain barrier; promise and pitfalls. Cell Biosci. 2021;11(1):1–28. doi: 10.1186/s13578-021-00650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Börtlein C, Schumacher F, Kleuser B, Dölken L, Avota E. Role of neutral sphingomyelinase-2 (NSM 2) in the control of t cell plasma membrane lipid composition and cholesterol homeostasis. Front Cell Dev Biol. 2019;7:226. doi: 10.3389/fcell.2019.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teng F, Fussenegger M. Shedding Light on Extracellular Vesicle Biogenesis and Bioengineering. Adv Sci. 2020;8(1):2003505. doi: 10.1002/advs.202003505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wei D, Zhan W, Gao Y, Huang L, Gong R, Wang W, Zhang R, Wu Y, Gao S, Kang T. RAB31 marks and controls an ESCRT-independent exosome pathway. Cell Res. 2021;31(2):157–177. doi: 10.1038/s41422-020-00409-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nydegger S, Khurana S, Krementsov DN, Foti M, Thali M. Mapping of tetraspanin-enriched microdomains that can function as gateways for HIV-1. J Cell Biol. 2006;173(5):795–807. doi: 10.1083/jcb.200508165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meldolesi J. Exosomes and ectosomes in intercellular communication. Curr Biol. 2018;28(8):R435–R444. doi: 10.1016/j.cub.2018.01.059. [DOI] [PubMed] [Google Scholar]
- 31.Yang L, Peng X, Li Y, Zhang X, Ma Y, Wu C, Fan Q, Wei S, Li H, Liu J. Long non-coding RNA HOTAIR promotes exosome secretion by regulating RAB35 and SNAP23 in hepatocellular carcinoma. Mol Cancer. 2019;18(1):1–12. doi: 10.1186/s12943-019-0990-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palmulli R, van Niel G. To be or not to be… secreted as exosomes, a balance finely tuned by the mechanisms of biogenesis. Essays Biochem. 2018;62(2):177–191. doi: 10.1042/EBC20170076. [DOI] [PubMed] [Google Scholar]
- 33.Anand S, Samuel M, Kumar S. Mathivanan S (2019) Ticket to a bubble ride: Cargo sorting into exosomes and extracellular vesicles. Biochim Biophys Acta BBA Proteins Proteom. 1867;12:140203. doi: 10.1016/j.bbapap.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 34.Wei H, Chen Q, Lin L, Sha C, Li T, Liu Y, Yin X, Xu Y, Chen L, Gao W. Regulation of exosome production and cargo sorting. Int J Biol Sci. 2021;17(1):163. doi: 10.7150/ijbs.53671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu C, Su C. Design strategies and application progress of therapeutic exosomes. Theranostics. 2019;9(4):1015. doi: 10.7150/thno.30853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conde-Vancells J, Rodriguez-Suarez E, Embade N, Gil D, Matthiesen R, Valle M, Elortza F, Lu SC, Mato JM, Falcon-Perez JM. Characterization and comprehensive proteome profiling of exosomes secreted by hepatocytes. J Proteome Res. 2008;7(12):5157–5166. doi: 10.1021/pr8004887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McAndrews KM, Kalluri R. Mechanisms associated with biogenesis of exosomes in cancer. Mol Cancer. 2019;18(1):52. doi: 10.1186/s12943-019-0963-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee TH, Chennakrishnaiah S, Meehan B, Montermini L, Garnier D, D'Asti E, Hou W, Magnus N, Gayden T, Jabado N. Barriers to horizontal cell transformation by extracellular vesicles containing oncogenic H-ras. Oncotarget. 2016;7(32):51991. doi: 10.18632/oncotarget.10627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Llorente A, Skotland T, Sylvänne T, Kauhanen D, Róg T, Orłowski A, Vattulainen I, Ekroos K. Sandvig K (2013) Molecular lipidomics of exosomes released by PC-3 prostate cancer cells. Biochim Biophys Acta BBA Mol Cell Biol Lipids. 1831;7:1302–1309. doi: 10.1016/j.bbalip.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 40.Subra C, Grand D, Laulagnier K, Stella A, Lambeau G, Paillasse M, De Medina P, Monsarrat B, Perret B, Silvente-Poirot S. Exosomes account for vesicle-mediated transcellular transport of activatable phospholipases and prostaglandins. J Lipid Res. 2010;51(8):2105–2120. doi: 10.1194/jlr.M003657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peterka O, Jirásko R, Chocholoušková M, Kuchař L, Wolrab D, Hájek R, Vrána D, Strouhal O, Melichar B. Holčapek M (2020) Lipidomic characterization of exosomes isolated from human plasma using various mass spectrometry techniques. Biochim Biophys Acta BBA Mol Cell Biol Lipids. 1865;5:158634. doi: 10.1016/j.bbalip.2020.158634. [DOI] [PubMed] [Google Scholar]
- 42.Batista BS, Eng WS, Pilobello KT, Hendricks-Muñoz KD, Mahal LK. Identification of a conserved glycan signature for microvesicles. J Proteome Res. 2011;10(10):4624–4633. doi: 10.1021/pr200434y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hurley JH, Hanson PI. Membrane budding and scission by the ESCRT machinery: it's all in the neck. Nat Rev Mol Cell Biol. 2010;11(8):556–566. doi: 10.1038/nrm2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shao H, Im H, Castro CM, Breakefield X, Weissleder R, Lee H. New technologies for analysis of extracellular vesicles. Chem Rev. 2018;118(4):1917–1950. doi: 10.1021/acs.chemrev.7b00534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Teis D, Saksena S, Emr SD. SnapShot: the ESCRT machinery. Cell. 2009;137(1):182–182. doi: 10.1016/j.cell.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 46.Tamai K, Tanaka N, Nakano T, Kakazu E, Kondo Y, Inoue J, Shiina M, Fukushima K, Hoshino T, Sano K. Exosome secretion of dendritic cells is regulated by Hrs, an ESCRT-0 protein. Biochem Biophys Res Commun. 2010;399(3):384–390. doi: 10.1016/j.bbrc.2010.07.083. [DOI] [PubMed] [Google Scholar]
- 47.Janvier K, Pelchen-Matthews A, Renaud J-B, Caillet M, Marsh M, Berlioz-Torrent C. The ESCRT-0 component HRS is required for HIV-1 Vpu-mediated BST-2/tetherin down-regulation. PLoS Pathog. 2011;7(2):e1001265. doi: 10.1371/journal.ppat.1001265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schink KO, Raiborg C, Stenmark H. Phosphatidylinositol 3-phosphate, a lipid that regulates membrane dynamics, protein sorting and cell signalling. BioEssays. 2013;35(10):900–912. doi: 10.1002/bies.201300064. [DOI] [PubMed] [Google Scholar]
- 49.Raiborg C, Bache KG, Mehlum A, Stang E, Stenmark H. Hrs recruits clathrin to early endosomes. EMBO J. 2001;20(17):5008–5021. doi: 10.1093/emboj/20.17.5008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schlossman DM, Schmid SL, Braell WA, Rothman JE. An enzyme that removes clathrin coats: purification of an uncoating ATPase. J Cell Biol. 1984;99(2):723–733. doi: 10.1083/jcb.99.2.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Raiborg C, Wesche J, Malerød L, Stenmark H. Flat clathrin coats on endosomes mediate degradative protein sorting by scaffolding Hrs in dynamic microdomains. J Cell Sci. 2006;119(12):2414–2424. doi: 10.1242/jcs.02978. [DOI] [PubMed] [Google Scholar]
- 52.Lu Q, Hope LW, Brasch M, Reinhard C, Cohen SN. TSG101 interaction with HRS mediates endosomal trafficking and receptor down-regulation. Proc Natl Acad Sci. 2003;100(13):7626–7631. doi: 10.1073/pnas.0932599100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bache KG, Brech A, Mehlum A, Stenmark H. Hrs regulates multivesicular body formation via ESCRT recruitment to endosomes. J Cell Biol. 2003;162(3):435–442. doi: 10.1083/jcb.200302131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pornillos O, Alam SL, Davis DR, Sundquist WI. Structure of the Tsg101 UEV domain in complex with the PTAP motif of the HIV-1 p6 protein. Nat Struct Biol. 2002;9(11):812–817. doi: 10.1038/nsb856. [DOI] [PubMed] [Google Scholar]
- 55.Pornillos O, Alam SL, Rich RL, Myszka DG, Davis DR, Sundquist WI. Structure and functional interactions of the Tsg101 UEV domain. EMBO J. 2002;21(10):2397–2406. doi: 10.1093/emboj/21.10.2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pornillos O, Higginson DS, Stray KM, Fisher RD, Garrus JE, Payne M, He G-P, Wang HE, Morham SG, Sundquist WI. HIV Gag mimics the Tsg101-recruiting activity of the human Hrs protein. J Cell Biol. 2003;162(3):425–434. doi: 10.1083/jcb.200302138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gill DJ, Teo H, Sun J, Perisic O, Veprintsev DB, Emr SD, Williams RL. Structural insight into the ESCRT-I/-II link and its role in MVB trafficking. EMBO J. 2007;26(2):600–612. doi: 10.1038/sj.emboj.7601501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bache KG, Slagsvold T, Cabezas A, Rosendal KR, Raiborg C, Stenmark H. The growth-regulatory protein HCRP1/hVps37A is a subunit of mammalian ESCRT-I and mediates receptor down-regulation. Mol Biol Cell. 2004;15(9):4337–4346. doi: 10.1091/mbc.e04-03-0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bishop N, Woodman P. TSG101/mammalian VPS23 and mammalian VPS28 interact directly and are recruited to VPS4-induced endosomes. J Biol Chem. 2001;276(15):11735–11742. doi: 10.1074/jbc.M009863200. [DOI] [PubMed] [Google Scholar]
- 60.Eastman SW, Martin-Serrano J, Chung W, Zang T, Bieniasz PD. Identification of human VPS37C, a component of endosomal sorting complex required for transport-I important for viral budding. J Biol Chem. 2005;280(1):628–636. doi: 10.1074/jbc.M410384200. [DOI] [PubMed] [Google Scholar]
- 61.Morita E, Sandrin V, Alam SL, Eckert DM, Gygi SP, Sundquist WI. Identification of human MVB12 proteins as ESCRT-I subunits that function in HIV budding. Cell Host Microbe. 2007;2(1):41–53. doi: 10.1016/j.chom.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Egea-Jimenez AL, Audebert S, Castro-Cruz M, Borg J-P, David G, Camoin L, Zimmermann. PLD2-phosphatidic acid recruit ESCRT-I to late endosomes for exosome biogenesis. bioRxiv; 2020.
- 63.Teo H, Gill DJ, Sun J, Perisic O, Veprintsev DB, Vallis Y, Emr SD, Williams RL. ESCRT-I core and ESCRT-II GLUE domain structures reveal role for GLUE in linking to ESCRT-I and membranes. Cell. 2006;125(1):99–111. doi: 10.1016/j.cell.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 64.Hirano S, Suzuki N, Slagsvold T, Kawasaki M, Trambaiolo D, Kato R, Stenmark H, Wakatsuki S. Structural basis of ubiquitin recognition by mammalian Eap45 GLUE domain. Nat Struct Mol Biol. 2006;13(11):1031–1032. doi: 10.1038/nsmb1163. [DOI] [PubMed] [Google Scholar]
- 65.Alam SL, Langelier C, Whitby FG, Koirala S, Robinson H, Hill CP, Sundquist WI. Structural basis for ubiquitin recognition by the human ESCRT-II EAP45 GLUE domain. Nat Struct Mol Biol. 2006;13(11):1029–1030. doi: 10.1038/nsmb1160. [DOI] [PubMed] [Google Scholar]
- 66.Bilodeau PS, Winistorfer SC, Kearney WR, Robertson AD, Piper RC. Vps27-Hse1 and ESCRT-I complexes cooperate to increase efficiency of sorting ubiquitinated proteins at the endosome. J Cell Biol. 2003;163(2):237–243. doi: 10.1083/jcb.200305007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schmidt O, Teis D. The ESCRT machinery. Curr Biol. 2012;22(4):R116–R120. doi: 10.1016/j.cub.2012.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Williams RL, Urbé S. The emerging shape of the ESCRT machinery. Nat Rev Mol Cell Biol. 2007;8(5):355–368. doi: 10.1038/nrm2162. [DOI] [PubMed] [Google Scholar]
- 69.Babst M, Katzmann DJ, Snyder WB, Wendland B, Emr SD. Endosome-associated complex, ESCRT-II, recruits transport machinery for protein sorting at the multivesicular body. Dev Cell. 2002;3(2):283–289. doi: 10.1016/S1534-5807(02)00219-8. [DOI] [PubMed] [Google Scholar]
- 70.Progida C, Malerød L, Stuffers S, Brech A, Bucci C, Stenmark H. RILP is required for the proper morphology and function of late endosomes. J Cell Sci. 2007;120(21):3729–3737. doi: 10.1242/jcs.017301. [DOI] [PubMed] [Google Scholar]
- 71.Tschuschke M, Kocherova I, Bryja A, Mozdziak P, Angelova Volponi A, Janowicz K, Sibiak R, Piotrowska-Kempisty H, Iżycki D, Bukowska D. Inclusion biogenesis, methods of isolation and clinical application of human cellular exosomes. J Clin Med. 2020;9(2):436. doi: 10.3390/jcm9020436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Inoue J, Krueger EW, Chen J, Cao H, Ninomiya M, McNiven MA. HBV secretion is regulated through the activation of endocytic and autophagic compartments mediated by Rab7 stimulation. J Cell Sci. 2015;128(9):1696–1706. doi: 10.1242/jcs.158097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Teo H, Perisic O, González B, Williams RL. ESCRT-II, an endosome-associated complex required for protein sorting: crystal structure and interactions with ESCRT-III and membranes. Dev Cell. 2004;7(4):559–569. doi: 10.1016/j.devcel.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 74.Yorikawa C, Shibata H, Waguri S, Hatta K, Horii M, Katoh K, Kobayashi T, Uchiyama Y, Maki M. Human CHMP6, a myristoylated ESCRT-III protein, interacts directly with an ESCRT-II component EAP20 and regulates endosomal cargo sorting. Biochem J. 2005;387(1):17–26. doi: 10.1042/BJ20041227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Maity S, Caillat C, Miguet N, Sulbaran G, Effantin G, Schoehn G, Roos WH, Weissenhorn W. VPS4 triggers constriction and cleavage of ESCRT-III helical filaments. Sci Adv. 2019;5(4):eaau7198. doi: 10.1126/sciadv.aau7198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Huber ST, Mostafavi S, Mortensen SA, Sachse C. Structure and assembly of ESCRT-III helical Vps24 filaments. Sci Adv. 2020;6(34):eaba4897. doi: 10.1126/sciadv.aba4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Martin-Serrano J, Yaravoy A, Perez-Caballero D, Bieniasz PD. Divergent retroviral late-budding domains recruit vacuolar protein sorting factors by using alternative adaptor proteins. Proc Natl Acad Sci. 2003;100(21):12414–12419. doi: 10.1073/pnas.2133846100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Von Schwedler UK, Stuchell M, Müller B, Ward DM, Chung H-Y, Morita E, Wang HE, Davis T, He G-P, Cimbora DM. The protein network of HIV budding. Cell. 2003;114(6):701–713. doi: 10.1016/S0092-8674(03)00714-1. [DOI] [PubMed] [Google Scholar]
- 79.Baietti MF, Zhang Z, Mortier E, Melchior A, Degeest G, Geeraerts A, Ivarsson Y, Depoortere F, Coomans C, Vermeiren E. Syndecan–syntenin–ALIX regulates the biogenesis of exosomes. Nat Cell Biol. 2012;14(7):677–685. doi: 10.1038/ncb2502. [DOI] [PubMed] [Google Scholar]
- 80.Friand V, David G, Zimmermann P. Syntenin and syndecan in the biogenesis of exosomes. Biol Cell. 2015;107(10):331–341. doi: 10.1111/boc.201500010. [DOI] [PubMed] [Google Scholar]
- 81.Kajimoto T, Okada T, Miya S, Zhang L, Nakamura S-i. Ongoing activation of sphingosine 1-phosphate receptors mediates maturation of exosomal multivesicular endosomes. Nat Commun. 2013;4(1):1–13. doi: 10.1038/ncomms3712. [DOI] [PubMed] [Google Scholar]
- 82.Wang G, Dinkins M, He Q, Zhu G, Poirier C, Campbell A, Mayer-Proschel M, Bieberich E. Astrocytes secrete exosomes enriched with proapoptotic ceramide and prostate apoptosis response 4 (PAR-4): potential mechanism of apoptosis induction in Alzheimer disease (AD) J Biol Chem. 2012;287(25):21384–21395. doi: 10.1074/jbc.M112.340513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.de Gassart A, Géminard C, Février B, Raposo G, Vidal M. Lipid raft-associated protein sorting in exosomes. Blood. 2003;102(13):4336–4344. doi: 10.1182/blood-2003-03-0871. [DOI] [PubMed] [Google Scholar]
- 84.Wei H, Malcor J-DM, Harper MT. Lipid rafts are essential for release of phosphatidylserine-exposing extracellular vesicles from platelets. Sci Rep. 2018;8(1):1–11. doi: 10.1038/s41598-018-28363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.van Niel G, Charrin S, Simoes S, Romao M, Rochin L, Saftig P, Marks MS, Rubinstein E, Raposo G. The tetraspanin CD63 regulates ESCRT-independent and -dependent endosomal sorting during melanogenesis. Dev Cell. 2011;21(4):708–721. doi: 10.1016/j.devcel.2011.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chairoungdua A, Smith DL, Pochard P, Hull M, Caplan MJ. Exosome release of β-catenin: a novel mechanism that antagonizes Wnt signaling. J Cell Biol. 2010;190(6):1079–1091. doi: 10.1083/jcb.201002049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Luga V, Zhang L, Viloria-Petit AM, Ogunjimi AA, Inanlou MR, Chiu E, Buchanan M, Hosein AN, Basik M, Wrana JL. Exosomes mediate stromal mobilization of autocrine Wnt-PCP signaling in breast cancer cell migration. Cell. 2012;151(7):1542–1556. doi: 10.1016/j.cell.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 88.Andreu Z, Yáñez-Mó M. Tetraspanins in extracellular vesicle formation and function. Front Immunol. 2014;5:442. doi: 10.3389/fimmu.2014.00442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hemler ME. Targeting of tetraspanin proteins—potential benefits and strategies. Nat Rev Drug Discov. 2008;7(9):747–758. doi: 10.1038/nrd2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zimmerman B, Kelly B, McMillan BJ, Seegar TC, Dror RO, Kruse AC, Blacklow SC. Crystal structure of a full-length human tetraspanin reveals a cholesterol-binding pocket. Cell. 2016;167(4):1041–1051. e1011. doi: 10.1016/j.cell.2016.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Charrin S, Manié S, Thiele C, Billard M, Gerlier D, Boucheix C, Rubinstein E. A physical and functional link between cholesterol and tetraspanins. Eur J Immunol. 2003;33(9):2479–2489. doi: 10.1002/eji.200323884. [DOI] [PubMed] [Google Scholar]
- 92.Stoorvogel W. Resolving sorting mechanisms into exosomes. Cell Res. 2015;25(5):531–532. doi: 10.1038/cr.2015.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sala-Valdés M, Ursa Á, Charrin S, Rubinstein E, Hemler ME, Sánchez-Madrid F, Yáñez-Mó M. EWI-2 and EWI-F link the tetraspanin web to the actin cytoskeleton through their direct association with ezrin-radixin-moesin proteins. J Biol Chem. 2006;281(28):19665–19675. doi: 10.1074/jbc.M602116200. [DOI] [PubMed] [Google Scholar]
- 94.Tejera E, Rocha-Perugini V, López-Martín S, Pérez-Hernández D, Bachir AI, Horwitz AR, Vázquez J, Sánchez-Madrid F, Yáñez-Mo M. CD81 regulates cell migration through its association with Rac GTPase. Mol Biol Cell. 2013;24(3):261–273. doi: 10.1091/mbc.e12-09-0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Perez-Hernandez D, Gutiérrez-Vázquez C, Jorge I, López-Martín S, Ursa A, Sánchez-Madrid F, Vázquez J, Yáñez-Mó M. The intracellular interactome of tetraspanin-enriched microdomains reveals their function as sorting machineries toward exosomes. J Biol Chem. 2013;288(17):11649–11661. doi: 10.1074/jbc.M112.445304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xie S, Zhang Q, Jiang L. Current knowledge on exosome biogenesis cargo-sorting mechanism and therapeutic implications. Membranes. 2022 doi: 10.3390/membranes12050498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ghossoub R, Chéry M, Audebert S, Leblanc R, Egea-Jimenez AL, Lembo F, Mammar S, Le Dez F, Camoin L, Borg JP, Rubinstein E, David G, Zimmermann P. Tetraspanin-6 negatively regulates exosome production. Proc Natl Acad Sci USA. 2020;117(11):5913–5922. doi: 10.1073/pnas.1922447117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Guix FX, Sannerud R, Berditchevski F, Arranz AM, Horré K, Snellinx A, Thathiah A, Saido T, Saito T, Rajesh S, Overduin M, Kumar-Singh S, Radaelli E, Corthout N, Colombelli J, Tosi S, Munck S, Salas IH, Annaert W, De Strooper B. Tetraspanin 6: a pivotal protein of the multiple vesicular body determining exosome release and lysosomal degradation of amyloid precursor protein fragments. Mol Neurodegener. 2017;12(1):25. doi: 10.1186/s13024-017-0165-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Guix FX, Sannerud R, Berditchevski F, Arranz AM, Horré K, Snellinx A, Thathiah A, Saido T, Saito T, Rajesh S. Tetraspanin 6: a pivotal protein of the multiple vesicular body determining exosome release and lysosomal degradation of amyloid precursor protein fragments. Mol Neurodegener. 2017;12(1):1–21. doi: 10.1186/s13024-017-0165-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Villarroya-Beltri C, Baixauli F, Mittelbrunn M, Fernández-Delgado I, Torralba D, Moreno-Gonzalo O, Baldanta S, Enrich C, Guerra S, Sánchez-Madrid F. ISGylation controls exosome secretion by promoting lysosomal degradation of MVB proteins. Nat Commun. 2016;7(1):1–11. doi: 10.1038/ncomms13588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lv Y, Chen J, Hu J, Qian Y, Kong Y, Fu L. Nonmuscle myosin heavy chain IIa-mediated exosome release via regulation of the rho-associated Kinase 1/Myosin light chains/actin pathway. Front Pharmacol.2020;11 [DOI] [PMC free article] [PubMed]
- 102.Sinha S, Hoshino D, Hong NH, Kirkbride KC, Grega-Larson NE, Seiki M, Tyska MJ, Weaver AM. Cortactin promotes exosome secretion by controlling branched actin dynamics. J Cell Biol. 2016;214(2):197–213. doi: 10.1083/jcb.201601025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Naik J, Hau CM, Ten Bloemendaal L, Mok KS, Hajji N, Wehman AM, Meisner S, Muncan V, Paauw NJ, de Vries H. The P4-ATPase ATP9A is a novel determinant of exosome release. PLoS ONE. 2019;14(4):e0213069. doi: 10.1371/journal.pone.0213069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gross JC, Chaudhary V, Bartscherer K, Boutros M. Active Wnt proteins are secreted on exosomes. Nat Cell Biol. 2012;14(10):1036–1045. doi: 10.1038/ncb2574. [DOI] [PubMed] [Google Scholar]
- 105.Fader CM, Sánchez DG, Mestre MB, Colombo MI. TI-VAMP/VAMP7 and VAMP3/cellubrevin: two v-SNARE proteins involved in specific steps of the autophagy/multivesicular body pathways. Biochim Biophys Acta BBA Mol Cell Res. 2009;1793(12):1901–1916. doi: 10.1016/j.bbamcr.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 106.Reyes-Ruiz JM, Osuna-Ramos JF, De Jesús-González LA, Palacios-Rápalo SN, Cordero-Rivera CD, Farfan-Morales CN, Hurtado-Monzón AM, Gallardo-Flores CE, Alcaraz-Estrada SL, Salas-Benito JS, Del Ángel RM. The regulation of flavivirus infection by hijacking exosome-Mediated cell-cell communication: new insights on virus-host interactions. Viruses. 2020 doi: 10.3390/v12070765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dogrammatzis C, Waisner H, Kalamvoki M. Cloaked viruses and viral factors in cutting edge exosome-based therapies. Front Cell Dev Biol. 2020 doi: 10.3389/fcell.2020.00376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jackson CB, Farzan M, Chen B, Choe H. Mechanisms of SARS-CoV-2 entry into cells. Nat Rev Mol Cell Biol. 2022;23(1):3–20. doi: 10.1038/s41580-021-00418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lakadamyali M, Rust MJ, Zhuang X. Endocytosis of influenza viruses. Microbes Infect. 2004;6(10):929–936. doi: 10.1016/j.micinf.2004.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liu H, Maruyama H, Masuda T, Honda A, Arai F. The influence of virus infection on the extracellular ph of the host cell detected on cell membrane. Front Microbiol. 2016 doi: 10.3389/fmicb.2016.01127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sun X, Roth SL, Bialecki MA, Whittaker GR. Internalization and fusion mechanism of vesicular stomatitis virus and related rhabdoviruses. Futur Virol. 2010;5(1):85–96. doi: 10.2217/fvl.09.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yamamoto M, Shindo M, Funayama T, Sumi C, Saito T, Toki Y, Hatayama M, Imadome K-I, Mizukami Y, Okumura T. Late-onset posttransplant Epstein-Barr virusrelated lymphoproliferative disease after cord blood transplantation for chronic active Epstein Barr virus infection: a case report. Medicine. 2022;101(12):e29055–e29055. doi: 10.1097/MD.0000000000029055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Harrison SC. Viral membrane fusion. Nat Struct Mol Biol. 2008;15(7):690–698. doi: 10.1038/nsmb.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Banerjee N, Mukhopadhyay S. Viral glycoproteins: biological role and application in diagnosis. Virusdisease. 2016;27(1):1–11. doi: 10.1007/s13337-015-0293-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Maginnis MS. Virus-receptor interactions: the key to cellular invasion. J Mol Biol. 2018;430(17):2590–2611. doi: 10.1016/j.jmb.2018.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Finzi A, Xiang S-H, Pacheco B, Wang L, Haight J, Kassa A, Danek B, Pancera M, Kwong PD, Sodroski J. Topological layers in the HIV-1 gp120 inner domain regulate gp41 interaction and CD4-triggered conformational transitions. Mol Cell. 2010;37(5):656–667. doi: 10.1016/j.molcel.2010.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bleul CC, Wu L, Hoxie JA, Springer TA, Mackay CR. The HIV coreceptors CXCR4 and CCR5 are differentially expressed and regulated on human T lymphocytes. Proc Natl Acad Sci. 1997;94(5):1925–1930. doi: 10.1073/pnas.94.5.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Francia V, Reker-Smit C, Salvati A. Mechanisms of Uptake and Membrane Curvature Generation for the Internalization of Silica Nanoparticles by Cells. Nano Lett. 2022;22(7):3118–3124. doi: 10.1021/acs.nanolett.2c00537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.He K, Wei Y, Zhang Z, Chen H, Yuan B, Pang H-B, Yang K. Membrane-curvature-mediated co-endocytosis of bystander and functional nanoparticles. Nanoscale. 2021;13(21):9626–9633. doi: 10.1039/d1nr01443a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.von Zastrow M, Sorkin A. Signaling on the endocytic pathway. Curr Opin Cell Biol. 2007;19(4):436–445. doi: 10.1016/j.ceb.2007.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lagache T, Sieben C, Meyer T, Herrmann A, Holcman D. Stochastic model of acidification, activation of hemagglutinin and escape of influenza viruses from an endosome. Front Phys. 2017 doi: 10.3389/fphy.2017.00025. [DOI] [Google Scholar]
- 122.Hansen CG, Nichols BJ. Molecular mechanisms of clathrin-independent endocytosis. J Cell Sci. 2009;122(Pt 11):1713–1721. doi: 10.1242/jcs.033951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLOS Pathog. 2010;6(9):e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.El-Sayed A, Harashima H. Endocytosis of gene delivery vectors: from clathrin-dependent to lipid raft-mediated endocytosis. Mol Ther J Am Soc Gene Ther. 2013;21(6):1118–1130. doi: 10.1038/mt.2013.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Iwamoto M, Saso W, Nishioka K, Ohashi H, Sugiyama R, Ryo A, Ohki M, Yun J-H, Park S-Y, Ohshima T. The machinery for endocytosis of epidermal growth factor receptor coordinates the transport of incoming hepatitis B virus to the endosomal network. J Biol Chem. 2020;295(3):800–807. doi: 10.1016/S0021-9258(17)49936-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hondermarck H, Bartlett NW, Nurcombe V. The role of growth factor receptors in viral infections: an opportunity for drug repurposing against emerging viral diseases such as COVID-19? FASEB BioAdv. 2020;2(5):296–303. doi: 10.1096/fba.2020-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zheng K, Xiang Y, Wang X, Wang Q, Zhong M, Wang S, Wang X, Fan J, Kitazato K, Wang Y. Epidermal growth factor receptor-PI3K signaling controls cofilin activity to facilitate herpes simplex virus 1 entry into neuronal cells. MBio. 2014;5(1):e00958–e1913. doi: 10.1128/mBio.00958-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Łyszkiewicz M, Ziętara N, Frey L, Pannicke U, Stern M, Liu Y, Fan Y, Puchałka J, Hollizeck S, Somekh I. Human FCHO1 deficiency reveals role for clathrin-mediated endocytosis in development and function of T cells. Nat Commun. 2020;11(1):1–15. doi: 10.1038/s41467-020-14809-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yang C, Colosi P, Hugelier S, Zabezhinsky D, Lakadamyali M, Svitkina T. Actin polymerization promotes invagination of flat clathrin-coated lattices in mammalian cells by pushing at lattice edges. Nat Commun. 2022;13(1):6127. doi: 10.1038/s41467-022-33852-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ren G, Vajjhala P, Lee JS, Winsor B, Munn AL. The BAR domain proteins: molding membranes in fission, fusion, and phagy. Microbiol Mol Biol Rev. 2006;70(1):37–120. doi: 10.1128/MMBR.70.1.37-120.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kaksonen M, Roux A. Mechanisms of clathrin-mediated endocytosis. Nat Rev Mol Cell Biol. 2018;19(5):313–326. doi: 10.1038/nrm.2017.132. [DOI] [PubMed] [Google Scholar]
- 132.Lee CHR, Mohamed Hussain K, Chu JJH. Macropinocytosis dependent entry of Chikungunya virus into human muscle cells. PLoS Negl Trop Dis. 2019;13(8):e0007610–e0007610. doi: 10.1371/journal.pntd.0007610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Aravamudhan P, Raghunathan K, Konopka-Anstadt J, Pathak A, Sutherland DM, Carter BD, Dermody TS. Reovirus uses macropinocytosis-mediated entry and fast axonal transport to infect neurons. PLoS Pathog. 2020;16(2):e1008380–e1008380. doi: 10.1371/journal.ppat.1008380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Liberali P, Kakkonen E, Turacchio G, Valente C, Spaar A, Perinetti G, Böckmann RA, Corda D, Colanzi A, Marjomaki V. The closure of Pak1-dependent macropinosomes requires the phosphorylation of CtBP1/BARS. EMBO J. 2008;27(7):970–981. doi: 10.1038/emboj.2008.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cossart P, Helenius A. Endocytosis of viruses and bacteria. Cold Spring Harb Perspect Biol. 2014;6(8):a016972. doi: 10.1101/cshperspect.a016972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Stoeber M, Schellenberger P, Siebert CA, Leyrat C, Helenius A, Grünewald K. Model for the architecture of caveolae based on a flexible, net-like assembly of Cavin1 and Caveolin discs. Proc Natl Acad Sci. 2016;113(50):E8069–E8078. doi: 10.1073/pnas.1616838113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Nishimura T, Suetsugu S. Super-resolution analysis of PACSIN2 and EHD2 at caveolae. PLoS ONE. 2022;17(7):e0271003. doi: 10.1371/journal.pone.0271003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Shajahan AN, Dobbin ZC, Hickman FE, Dakshanamurthy S, Clarke R. Tyrosine-phosphorylated caveolin-1 (Tyr-14) increases sensitivity to paclitaxel by inhibiting BCL2 and BCLxL proteins via c-Jun N-terminal kinase (JNK) J Biol Chem. 2012;287(21):17682–17692. doi: 10.1074/jbc.M111.304022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chettimada S, Yang J, Moon HG, Jin Y. Caveolae, caveolin-1 and cavin-1: Emerging roles in pulmonary hypertension. World J Respirol. 2015;5(2):126–134. doi: 10.5320/wjr.v5.i2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Boettcher JP, Kirchner M, Churin Y, Kaushansky A, Pompaiah M, Thorn H, Brinkmann V, MacBeath G, Meyer TF. Tyrosine-phosphorylated caveolin-1 blocks bacterial uptake by inducing Vav2-RhoA-mediated cytoskeletal rearrangements. PLOS Biol. 2010;8(8):e1000457. doi: 10.1371/journal.pbio.1000457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Moskovich O, Herzog L-O, Ehrlich M, Fishelson Z. Caveolin-1 and dynamin-2 are essential for removal of the complement C5b–9 complex via endocytosis*. J Biol Chem. 2012;287(24):19904–19915. doi: 10.1074/jbc.M111.333039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Glebov OO. Understanding SARS-CoV-2 endocytosis for COVID-19 drug repurposing. FEBS J. 2020;287(17):3664–3671. doi: 10.1111/febs.15369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Babina IS, Donatello S, Nabi IR, Hopkins AM. Lipid rafts as master regulators of breast cancer cell function. Breast Cancer Carcinogen Cell Growth Signal Pathw. 2011;401:428. [Google Scholar]
- 144.Ripa I, Andreu S, López-Guerrero JA, Bello-Morales R. Membrane rafts: portals for viral entry. Front Microbiol. 2021;12:120. doi: 10.3389/fmicb.2021.631274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sathe M, Muthukrishnan G, Rae J, Disanza A, Thattai M, Scita G, Parton RG, Mayor S. Small GTPases and BAR domain proteins regulate branched actin polymerisation for clathrin and dynamin-independent endocytosis. Nat Commun. 2018;9(1):1–16. doi: 10.1038/s41467-018-03955-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Shafaq-Zadah M, Dransart E, Johannes L. Clathrin-independent endocytosis, retrograde trafficking, and cell polarity. Curr Opin Cell Biol. 2020;65:112–121. doi: 10.1016/j.ceb.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Badierah RA, Uversky VN, Redwan EM. Dancing with Trojan horses: an interplay between the extracellular vesicles and viruses. J Biomol Struct Dyn. 2021;39(8):3034–3060. doi: 10.1080/07391102.2020.1756409. [DOI] [PubMed] [Google Scholar]
- 148.Cremer T, Gallo RC, Margolis LB. Extracellular vesicles and viruses: are they close relatives? Proc Natl Acad Sci USA. 2016;113(33):9155–9161. doi: 10.1073/pnas.1605146113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Votteler J, Sundquist WI. Virus budding and the ESCRT pathway. Cell Host Microbe. 2013;14(3):232–241. doi: 10.1016/j.chom.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Iša P, Pérez-Delgado A, Quevedo IR, López S, Arias CF. Rotaviruses associate with distinct types of extracellular vesicles. Viruses. 2020;12(7):763. doi: 10.3390/v12070763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Barnes J, Wilson DW. Seeking closure: how do herpesviruses recruit the cellular ESCRT apparatus? J Virol. 2019;93(13):e00392–e1319. doi: 10.1128/JVI.00392-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Rheinemann L, Sundquist WI. Virus budding. Encyclopedia Virol. 2021;519.
- 153.Mpingabo PI, Urata S, Yasuda J. Analysis of the cell type-dependence on the arenavirus Z-mediated virus-like particle production. Front Microbiol. 2020;11:2301. doi: 10.3389/fmicb.2020.562814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Wang J, Danzy S, Kumar N, Ly H, Liang Y. Biological roles and functional mechanisms of arenavirus Z protein in viral replication. J Virol. 2012;86(18):9794–9801. doi: 10.1128/JVI.00385-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Demirov DG, Ono A, Orenstein JM, Freed EO. Overexpression of the N-terminal domain of TSG101 inhibits HIV-1 budding by blocking late domain function. Proc Natl Acad Sci. 2002;99(2):955–960. doi: 10.1073/pnas.032511899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wendt L, Kämper L, Schmidt ML, Mettenleiter TC, Hoenen T. Analysis of a putative late domain using an Ebola virus transcription and replication-competent virus-like particle system. J Infect Dis. 2018;218(suppl_5):S355–S359. doi: 10.1093/infdis/jiy247. [DOI] [PubMed] [Google Scholar]
- 157.Irie T, Harty RN. L-domain flanking sequences are important for host interactions and efficient budding of vesicular stomatitis virus recombinants. J Virol. 2005;79(20):12617–12622. doi: 10.1128/JVI.79.20.12617-12622.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Dores MR, Chen B, Lin H, Soh UJ, Paing MM, Montagne WA, Meerloo T, Trejo J. ALIX binds a YPX3L motif of the GPCR PAR1 and mediates ubiquitin-independent ESCRT-III/MVB sorting. J Cell Biol. 2012;197(3):407–419. doi: 10.1083/jcb.201110031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Ray G, Schmitt PT, Schmitt AP. Angiomotin-like 1 links paramyxovirus M proteins to NEDD4 family ubiquitin ligases. Viruses. 2019;11(2):128. doi: 10.3390/v11020128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kovalev N, de Castro Martín IF, Pogany J, Barajas D, Pathak K, Risco C, Nagy PD. Role of viral RNA and co-opted cellular ESCRT-I and ESCRT-III factors in formation of tombusvirus spherules harboring the tombusvirus replicase. J Virol. 2016;90(7):3611–3626. doi: 10.1128/JVI.02775-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Sette P, O’Connor SK, Yerramilli VS, Dussupt V, Nagashima K, Chutiraka K, Lingappa J, Scarlata S, Bouamr F. HIV-1 nucleocapsid mimics the membrane adaptor syntenin PDZ to gain access to ESCRTs and promote virus budding. Cell Host Microbe. 2016;19(3):336–348. doi: 10.1016/j.chom.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Qian H, Zhang Y, Wu B, Wu S, You S, Zhang N, Sun Y. Structure and function of HECT E3 ubiquitin ligases and their role in oxidative stress. J Transl Intern Med. 2020;8(2):71. doi: 10.2478/jtim-2020-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Koshizuka T, Kondo H, Kato H, Takahashi K. Human cytomegalovirus UL42 protein inhibits the degradation of glycoprotein B through inhibition of Nedd4 family ubiquitin E3 ligases. Microbiol Immunol; 2021. [DOI] [PubMed]
- 164.Ju Y, Bai H, Ren L, Zhang L. The role of exosome and the ESCRT pathway on enveloped virus infection. Int J Mol Sci. 2021 doi: 10.3390/ijms22169060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Yang JE, Rossignol ED, Chang D, Zaia J, Forrester I, Raja K, Winbigler H, Nicastro D, Jackson WT, Bullitt E. Complexity and ultrastructure of infectious extracellular vesicles from cells infected by non-enveloped virus. Sci Rep. 2020;10(1):7939. doi: 10.1038/s41598-020-64531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Feng Z, Hensley L, McKnight KL, Hu F, Madden V, Ping L, Jeong S-H, Walker C, Lanford RE, Lemon SM. A pathogenic picornavirus acquires an envelope by hijacking cellular membranes. Nature. 2013;496(7445):367–371. doi: 10.1038/nature12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ramakrishnaiah V, Thumann C, Fofana I, Habersetzer F, Pan Q, de Ruiter PE, Willemsen R, Demmers JA, Raj VS, Jenster G. Exosome-mediated transmission of hepatitis C virus between human hepatoma Huh7.5 cells. Proc Nat Acad Sci. 2013;110(32):13109–13113. doi: 10.1073/pnas.1221899110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Elgner F, Ren H, Medvedev R, Ploen D, Himmelsbach K, Boller K, Hildt E. The intracellular cholesterol transport inhibitor U18666A inhibits the exosome-dependent release of mature hepatitis C virus. J Virol. 2016;90(24):11181–11196. doi: 10.1128/JVI.01053-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Santiana M, Ghosh S, Ho BA, Rajasekaran V, Du W-L, Mutsafi Y, De Jésus-Diaz DA, Sosnovtsev SV, Levenson EA, Parra GI. Vesicle-cloaked virus clusters are optimal units for inter-organismal viral transmission. Cell Host Microbe. 2018;24(2):208–220. e208. doi: 10.1016/j.chom.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Robinson SM, Tsueng G, Sin J, Mangale V, Rahawi S, McIntyre LL, Williams W, Kha N, Cruz C, Hancock BM. Coxsackievirus B exits the host cell in shed microvesicles displaying autophagosomal markers. PLoS Pathog. 2014;10(4):e1004045. doi: 10.1371/journal.ppat.1004045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Mao L, Wu J, Shen L, Yang J, Chen J, Xu H. Enterovirus 71 transmission by exosomes establishes a productive infection in human neuroblastoma cells. Virus Genes. 2016;52(2):189–194. doi: 10.1007/s11262-016-1292-3. [DOI] [PubMed] [Google Scholar]
- 172.Mori Y, Koike M, Moriishi E, Kawabata A, Tang H, Oyaizu H, Uchiyama Y, Yamanishi K. Human herpesvirus-6 induces MVB formation, and virus egress occurs by an exosomal release pathway. Traffic. 2008;9(10):1728–1742. doi: 10.1111/j.1600-0854.2008.00796.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Todd KV, Tripp RA. Exosome-mediated human norovirus infection. PLoS ONE. 2020;15(8):0237044. doi: 10.1371/journal.pone.0237044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Santiana M, Ghosh S, Ho BA, Rajasekaran V, Du W-L, Mutsafi Y, De Jésus-Diaz DA, Sosnovtsev SV, Levenson EA, Parra GI, Takvorian PM, Cali A, Bleck C, Vlasova AN, Saif LJ, Patton JT, Lopalco P, Corcelli A, Green KY, Altan-Bonnet N. Vesicle-cloaked virus clusters are optimal units for inter-organismal viral transmission. Cell Host Microbe. 2018;24(2):208–220.e208. doi: 10.1016/j.chom.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Martínez JL, Arnoldi F, Schraner EM, Eichwald C, Silva-Ayala D, Lee E, Sztul E, Burrone ÓR, López S, Arias CF. The guanine nucleotide exchange factor GBF1 participates in rotavirus replication. J Virol. 2019;93(19):e01062–e11019. doi: 10.1128/JVI.01062-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Pleet ML, Erickson J, DeMarino C, Barclay RA, Cowen M, Lepene B, Liang J, Kuhn JH, Prugar L, Stonier SW, Dye JM, Zhou W, Liotta LA, Aman MJ, Kashanchi F. Ebola virus VP40 modulates cell cycle and biogenesis of extracellular vesicles. J Infect Dis. 2018;218(suppl5):S365–S387. doi: 10.1093/infdis/jiy472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Pleet ML, DeMarino C, Stonier SW, Dye JM, Jacobson S, Aman MJ, Kashanchi F. Extracellular vesicles and Ebola virus: a new mechanism of immune evasion. Viruses. 2019;11(5):410. doi: 10.3390/v11050410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wirchnianski AS, Wec AZ, Nyakatura EK, Herbert AS, Slough MM, Kuehne AI, Mittler E, Jangra RK, Teruya J, Dye JM, Lai JR, Chandran K. Two distinct lysosomal targeting strategies afford Trojan horse antibodies with pan-filovirus activity. Front Immunol. 2021;12:729851. doi: 10.3389/fimmu.2021.729851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Garofalo M, Villa A, Rizzi N, Kuryk L, Mazzaferro V, Ciana P. Systemic administration and targeted delivery of immunogenic oncolytic adenovirus encapsulated in extracellular vesicles for cancer therapies. Viruses. 2018 doi: 10.3390/v10100558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Perrin P, Janssen L, Janssen H, van den Broek B, Voortman LM, van Elsland D, Berlin I, Neefjes J. Retrofusion of intralumenal MVB membranes parallels viral infection and coexists with exosome release. Curr Biol. 2021;31(17):3884–3893.e3884. doi: 10.1016/j.cub.2021.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Saari H, Turunen T, Lõhmus A, Turunen M, Jalasvuori M, Butcher SJ, Ylä-Herttuala S, Viitala T, Cerullo V, Siljander PR. Extracellular vesicles provide a capsid-free vector for oncolytic adenoviral DNA delivery. J Extracell Vesicles. 2020;9(1):1747206. doi: 10.1080/20013078.2020.1747206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Yogev O, Henderson S, Hayes MJ, Marelli SS, Ofir-Birin Y, Regev-Rudzki N, Herrero J, Enver T. Herpesviruses shape tumour microenvironment through exosomal transfer of viral microRNAs. PLoS Pathog. 2017;13(8):e1006524. doi: 10.1371/journal.ppat.1006524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Roth AN, Aravamudhan P, de Castro IF, Tenorio R, Risco C, Dermody TS. Ins and outs of reovirus: vesicular trafficking in viral entry and egress. Trends Microbiol. 2021;29(4):363–375. doi: 10.1016/j.tim.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Chen Q, Liu Y, Ren J, Zhong P, Chen M, Jia D, Chen H, Wei T. Exosomes mediate horizontal transmission of viral pathogens from insect vectors to plant phloem. Elife. 2021;10:e64603. doi: 10.7554/eLife.64603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Koehler M, Petitjean SJ, Yang J, Aravamudhan P, Somoulay X, Giudice CL, Poncin MA, Dumitru AC, Dermody TS, Alsteens D. Reovirus directly engages integrin to recruit clathrin for entry into host cells. Nat Commun. 2021;12(1):1–15. doi: 10.1038/s41467-021-22380-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Reyes-Ruiz JM, Osuna-Ramos JF, De Jesús-González LA, Hurtado-Monzón AM, Farfan-Morales CN, Cervantes-Salazar M, Bolaños J, Cigarroa-Mayorga OE, San Martín-Martínez E, Medina F. Isolation and characterization of exosomes released from mosquito cells infected with dengue virus. Virus Res. 2019;266:1–14. doi: 10.1016/j.virusres.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 187.Vora A, Zhou W, Londono-Renteria B, Woodson M, Sherman MB, Colpitts TM, Neelakanta G, Sultana H. Arthropod EVs mediate dengue virus transmission through interaction with a tetraspanin domain containing glycoprotein Tsp29Fb. Proc Natl Acad Sci. 2018;115(28):E6604–E6613. doi: 10.1073/pnas.1720125115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bedford JG, Infusini G, Dagley LF, Villalon-Letelier F, Zheng MZ, Bennett-Wood V, Reading PC, Wakim LM. Airway exosomes released during influenza virus infection serve as a key component of the antiviral innate immune response. Front Immunol. 2020;11:887. doi: 10.3389/fimmu.2020.00887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Zheng B, Zhou J, Wang H. Host microRNAs and exosomes that modulate influenza virus infection. Virus Res. 2020;279:197885. doi: 10.1016/j.virusres.2020.197885. [DOI] [PubMed] [Google Scholar]
- 190.Wang J, Wu F, Liu C, Dai W, Teng Y, Su W, Kong W, Gao F, Cai L, Hou A. Exosomes released from rabies virus-infected cells may be involved in the infection process. Virol Sin. 2019;34(1):59–65. doi: 10.1007/s12250-019-00087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Madison MN, Okeoma CM. Exosomes: implications in HIV-1 pathogenesis. Viruses. 2015;7(7):4093–4118. doi: 10.3390/v7072810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Raab-Traub N, Dittmer DP. Viral effects on the content and function of extracellular vesicles. Nat Rev Microbiol. 2017;15(9):559–572. doi: 10.1038/nrmicro.2017.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Giannessi F, Aiello A, Franchi F, Percario ZA, Affabris E. The role of extracellular vesicles as allies of HIV HCV and SARS viruses. Viruses. 2020;12(5):571. doi: 10.3390/v12050571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Teow S-Y, Liew K, Khoo AS-B, Peh S-C. Pathogenic role of exosomes in Epstein-Barr Virus (EBV)-associated cancers. Int J Biol Sci. 2017;13(10):1276. doi: 10.7150/ijbs.19531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Hinata M, Kunita A, Abe H, Morishita Y, Sakuma K, Yamashita H, Seto Y, Ushiku T, Fukayama M. Exosomes of Epstein-Barr virus-associated gastric carcinoma suppress dendritic cell maturation. Microorganisms. 2020;8(11):1776. doi: 10.3390/microorganisms8111776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Chen W, Xie Y, Wang T, Wang L. New insights into Epstein-Barr virus-associated tumors: exosomes. Oncol Rep. 2022;47(1):1–12. doi: 10.3892/or.2021.8224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Turner DL, Korneev DV, Purdy JG, de Marco A, Mathias RA. The host exosome pathway underpins biogenesis of the human cytomegalovirus virion. Elife. 2020;9:e58288. doi: 10.7554/eLife.58288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Earnest JT, Hantak MP, Li K, McCray PB, Jr, Perlman S, Gallagher T. The tetraspanin CD9 facilitates MERS-coronavirus entry by scaffolding host cell receptors and proteases. PLoS Pathog. 2017;13(7):e1006546. doi: 10.1371/journal.ppat.1006546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Patra U, Mukhopadhyay U, Mukherjee A, Dutta S, Chawla-Sarkar M. Treading a HOSTile path: Mapping the dynamic landscape of host cell–rotavirus interactions to explore novel host-directed curative dimensions. Virulence. 2021;12(1):1022–1062. doi: 10.1080/21505594.2021.1903198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Cuadras MA, Bordier BB, Zambrano JL, Ludert JE, Greenberg HB. Dissecting rotavirus particle-raft interaction with small interfering RNAs: insights into rotavirus transit through the secretory pathway. J Virol. 2006;80(8):3935–3946. doi: 10.1128/JVI.80.8.3935-3946.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Mohan KV, Muller J, Atreya CD. Defective rotavirus particle assembly in lovastatin-treated MA104 cells. Adv Virol. 2008;153(12):2283–2290. doi: 10.1007/s00705-008-0261-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Cuadras MA, Greenberg HB. Rotavirus infectious particles use lipid rafts during replication for transport to the cell surface in vitro and in vivo. Virology. 2003;313(1):308–321. doi: 10.1016/S0042-6822(03)00326-X. [DOI] [PubMed] [Google Scholar]
- 203.New C, Lee Z-Y, Tan KS, Wong AH-P, Wang DY, Tran T. Tetraspanins: host factors in viral infections. Int J Mol Sci. 2021;22(21):11609. doi: 10.3390/ijms222111609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Sundquist WI, Kräusslich H-G. HIV-1 assembly, budding, and maturation. Cold Spring Harb Perspect Med. 2012;2(7):a006924. doi: 10.1101/cshperspect.a006924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.McKnight KL, Xie L, González-López O, Rivera-Serrano EE, Chen X, Lemon SM. Protein composition of the hepatitis a virus quasi-envelope. Proc Natl Acad Sci. 2017;114(25):6587–6592. doi: 10.1073/pnas.1619519114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Florin L, Lang T. Tetraspanin assemblies in virus infection. Front Immunol. 2018;9:1140. doi: 10.3389/fimmu.2018.01140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Sato K, Aoki J, Misawa N, Daikoku E, Sano K, Tanaka Y, Koyanagi Y. Modulation of human immunodeficiency virus type 1 infectivity through incorporation of tetraspanin proteins. J Virol. 2008;82(2):1021–1033. doi: 10.1128/JVI.01044-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Earnest JT, Hantak MP, Park J-E, Gallagher T. Coronavirus and influenza virus proteolytic priming takes place in tetraspanin-enriched membrane microdomains. J Virol. 2015;89(11):6093–6104. doi: 10.1128/JVI.00543-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Diehl N, Schaal H. Make yourself at home: viral hijacking of the PI3K/Akt signaling pathway. Viruses. 2013;5(12):3192–3212. doi: 10.3390/v5123192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Soliman M, Cho E-H, Park J-G, Kim J-Y, Alfajaro MM, Baek Y-B, Kim D-S, Kang M-I, Park S-I, Cho K-O. Rotavirus-induced early activation of the RhoA/ROCK/MLC signaling pathway mediates the disruption of tight junctions in polarized MDCK cells. Sci Rep. 2018;8(1):1–13. doi: 10.1038/s41598-018-32352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Sharif M, Baek Y-B, Naveed A, Stalin N, Kang M-I, Park S-I, Soliman M, Cho K-O. Porcine sapovirus-induced tight junction dissociation via activation of the RhoA/ROCK/MLC signaling pathway. J Virol. 2021;95(11):e00051–e121. doi: 10.1128/JVI.00051-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Linfield DT, Raduka A, Aghapour M, Rezaee F. Airway tight junctions as targets of viral infections: tight junctions and viral infections. Tissue Barriers. 2021;9(2):1883965. doi: 10.1080/21688370.2021.1883965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Van Huizen E, McInerney GM. Activation of the PI3K-AKT pathway by old world alphaviruses. Cells. 2020;9(4):970. doi: 10.3390/cells9040970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Sánchez EG, Quintas A, Pérez-Núñez D, Nogal M, Barroso S, Carrascosa ÁL, Revilla Y. African swine fever virus uses macropinocytosis to enter host cells. PLoS Pathog. 2012;8(6):e1002754. doi: 10.1371/journal.ppat.1002754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Imjeti NS, Menck K, Egea-Jimenez AL, Lecointre C, Lembo F, Bouguenina H, Badache A, Ghossoub R, David G, Roche S. Syntenin mediates SRC function in exosomal cell-to-cell communication. Proc Natl Acad Sci. 2017;114(47):12495–12500. doi: 10.1073/pnas.1713433114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Hikita T, Kuwahara A, Watanabe R, Miyata M, Oneyama C. Src in endosomal membranes promotes exosome secretion and tumor progression. Sci Rep. 2019;9(1):1–14. doi: 10.1038/s41598-019-39882-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Chowdhury MA, Hossain N, Kashem MA, Shahid MA, Alam A. Immune response in COVID-19: a review. J Infect Public Health. 2020;13(11):1619–1629. doi: 10.1016/j.jiph.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Gould SJ, Booth AM, Hildreth JE. The Trojan exosome hypothesis. Proc Natl Acad Sci. 2003;100(19):10592–10597. doi: 10.1073/pnas.1831413100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Gurunathan S, Kang MH, Kim J-H. Diverse effects of exosomes on Covid-19: a perspective of progress from transmission to therapeutic developments. Front Immunol. 2021 doi: 10.3389/fimmu.2021.716407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Sims B, Farrow AL, Williams SD, Bansal A, Krendelchtchikov A, Gu L, Matthews QL. Role of TIM-4 in exosome-dependent entry of HIV-1 into human immune cells. Int J Nanomed. 2017;12:4823. doi: 10.2147/IJN.S132762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Kerviel A, Zhang M, Altan-Bonnet N. A new infectious unit: extracellular vesicles carrying virus populations. Annu Rev Cell Dev Biol. 2021;37:171–197. doi: 10.1146/annurev-cellbio-040621-032416. [DOI] [PubMed] [Google Scholar]
- 222.Longatti A, Boyd B, Chisari FV. Virion-independent transfer of replication-competent hepatitis C virus RNA between permissive cells. J Virol. 2015;89(5):2956–2961. doi: 10.1128/JVI.02721-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Cheng M, Dietz L, Gong Y, Eichler F, Nammour J, Ng C, Grimm D, Maguire CA. Neutralizing antibody evasion and transduction with purified extracellular vesicle-enveloped adeno-associated virus vectors. Hum Gene Ther. 2021;32(23–24):1457–1470. doi: 10.1089/hum.2021.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Hong S, Ruan S, Greenberg Z, He M, McGill JL. Development of surface engineered antigenic exosomes as vaccines for respiratory syncytial virus. Sci Rep. 2021;11(1):1–13. doi: 10.1038/s41598-021-00765-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Wyciszkiewicz A, Kalinowska-Łyszczarz A, Nowakowski B, Kaźmierczak K, Osztynowicz K, Michalak S. Expression of small heat shock proteins in exosomes from patients with gynecologic cancers. Sci Rep. 2019;9(1):1–9. doi: 10.1038/s41598-019-46221-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ham S, Lima LG, Chai EPZ, Muller A, Lobb RJ, Krumeich S, Wen SW, Wiegmans AP, Möller A. Breast cancer-derived exosomes alter macrophage polarization via gp130/STAT3 signaling. Front Immunol. 2018;871. [DOI] [PMC free article] [PubMed]
- 227.Fan C-S, Chen C-C, Chen L-L, Chua KV, Hung H-C, Hsu JT-A, Huang T-S. Extracellular HSP90α Induces MyD88− IRAK Complex-Associated IKKα/β− NF-κB/IRF3 and JAK2/TYK2− STAT-3 Signaling in Macrophages for Tumor-Promoting M2-Polarization. Cells. 2022;11(2):229. doi: 10.3390/cells11020229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Klibi J, Niki T, Riedel A, Pioche-Durieu C, Souquere S, Rubinstein E, Le Moulec S, Guigay J, Hirashima M, Guemira F. Blood diffusion and Th1-suppressive effects of galectin-9–containing exosomes released by Epstein-Barr virus–infected nasopharyngeal carcinoma cells Blood. J Am Soc Hematol. 2009;113(9):1957–1966. doi: 10.1182/blood-2008-02-142596. [DOI] [PubMed] [Google Scholar]
- 229.Barberis E, Vanella VV, Falasca M, Caneapero V, Cappellano G, Raineri D, Ghirimoldi M, De Giorgis V, Puricelli C, Vaschetto R, Sainaghi PP, Bruno S, Sica A, Dianzani U, Rolla R, Chiocchetti A, Cantaluppi V, Baldanzi G, Marengo E, Manfredi M. Circulating exosomes are strongly involved in SARS-CoV-2 infection. Front Mol Biosci. 2021 doi: 10.3389/fmolb.2021.632290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Ching KL, de Vries M, Gago J, Dancel-Manning K, Sall J, Rice WJ, Barnett C, Liang F-X, Thorpe LE, Shopsin B. ACE2-containing defensosomes serve as decoys to inhibit SARS-CoV-2 infection. bioRxiv; 2021. [DOI] [PMC free article] [PubMed]
- 231.Miorin L, Kehrer T, Sanchez-Aparicio MT, Zhang K, Cohen P, Patel RS, Cupic A, Makio T, Mei M, Moreno E, Danziger O, White KM, Rathnasinghe R, Uccellini M, Gao S, Aydillo T, Mena I, Yin X, Martin-Sancho L, Krogan NJ, Chanda SK, Schotsaert M, Wozniak RW, Ren Y, Rosenberg BR, Fontoura BMA, García-Sastre A. SARS-CoV-2 Orf6 hijacks Nup98 to block STAT nuclear import and antagonize interferon signaling. Proc Natl Acad Sci. 2020;117(45):28344. doi: 10.1073/pnas.2016650117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Tenoever BR. RNA viruses and the host microRNA machinery. Nat Rev Microbiol. 2013;11 (3). [DOI] [PubMed]
- 233.Torralba D, Baixauli F, Villarroya-Beltri C, Fernández-Delgado I, Latorre-Pellicer A, Acín-Pérez R, Martín-Cófreces NB, Jaso-Tamame ÁL, Iborra S, Jorge I. Priming of dendritic cells by DNA-containing extracellular vesicles from activated T cells through antigen-driven contacts. Nat Commun. 2018;9(1):1–17. doi: 10.1038/s41467-018-05077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Kudr J, Michalek P, Ilieva L, Adam V, Zitka O. COVID-19: A challenge for electrochemical biosensors. TrAC, Trends Anal Chem. 2021;136:116192. doi: 10.1016/j.trac.2021.116192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Wang J, Teng Y, Zhao G, Li F, Hou A, Sun B, Kong W, Gao F, Cai L, Jiang C. Exosome-mediated delivery of inducible miR-423-5p enhances resistance of MRC-5 cells to rabies virus infection. Int J Mol Sci. 2019;20(7):1537. doi: 10.3390/ijms20071537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Li J, Liu K, Liu Y, Xu Y, Zhang F, Yang H, Liu J, Pan T, Chen J, Wu M. Exosomes mediate the cell-to-cell transmission of IFN-α-induced antiviral activity. Nat Immunol. 2013;14(8):793–803. doi: 10.1038/ni.2647. [DOI] [PubMed] [Google Scholar]
- 237.de Carvalho JV, de Castro RO, da Silva EZ, Silveira PP, da Silva-Januário ME, Arruda E, Jamur MC, Oliver C, Aguiar RS, daSilva LL. Nef neutralizes the ability of exosomes from CD4+ T cells to act as decoys during HIV-1 infection. PLoS ONE. 2014;9(11):e113691. doi: 10.1371/journal.pone.0113691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Zuo L, Xie Y, Tang J, Xin S, Liu L, Zhang S, Yan Q, Zhu F, Lu J. Targeting exosomal EBV-LMP1 transfer and miR-203 expression via the NF-κB pathway: the therapeutic role of aspirin in NPC. Mol Ther Nucleic Acids. 2019;17:175–184. doi: 10.1016/j.omtn.2019.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Meckes DG, Gunawardena HP, Dekroon RM, Heaton PR, Edwards RH, Ozgur S, Griffith JD, Damania B, Raab-Traub N. Modulation of B-cell exosome proteins by gamma herpesvirus infection. Proc Natl Acad Sci. 2013;110(31):E2925–E2933. doi: 10.1073/pnas.1303906110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Schauflinger M, Fischer D, Schreiber A, Chevillotte M, Walther P, Mertens T, von Einem J. The tegument protein UL71 of human cytomegalovirus is involved in late envelopment and affects multivesicular bodies. J Virol. 2011;85(8):3821–3832. doi: 10.1128/JVI.01540-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Arii J, Watanabe M, Maeda F, Tokai-Nishizumi N, Chihara T, Miura M, Maruzuru Y, Koyanagi N, Kato A, Kawaguchi Y. ESCRT-III mediates budding across the inner nuclear membrane and regulates its integrity. Nat Commun. 2018;9(1):1–15. doi: 10.1038/s41467-018-05889-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Kalamvoki M, Deschamps T. Extracellular vesicles during Herpes Simplex Virus type 1 infection: an inquire. Virol J. 2016;13(1):1–12. doi: 10.1186/s12985-016-0518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Persson BD, John L, Rafie K, Strebl M, Frängsmyr L, Ballmann MZ, Mindler K, Havenga M, Lemckert A, Stehle T. Human species D adenovirus hexon capsid protein mediates cell entry through a direct interaction with CD46. Proc Nat Acad Sci. 2021;118 (3). [DOI] [PMC free article] [PubMed]
- 244.Lan B, Zeng S, Grützmann R, Pilarsky C. The role of exosomes in pancreatic cancer. Int J Mol Sci. 2019;20(18):4332. doi: 10.3390/ijms20184332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Jiang B, Himmelsbach K, Ren H, Boller K, Hildt E. Subviral hepatitis B virus filaments, like infectious viral particles, are released via multivesicular bodies. J Virol. 2015;90(7):3330–3341. doi: 10.1128/JVI.03109-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Chiou C-T, Hu C-CA, Chen P-H, Liao C-L, Lin Y-L, Wang J-J. Association of Japanese encephalitis virus NS3 protein with microtubules and tumour susceptibility gene 101 (TSG101) protein. J Gen Virol. 2003;84(10):2795–2805. doi: 10.1099/vir.0.19201-0. [DOI] [PubMed] [Google Scholar]
- 247.Mukherjee S, Akbar I, Kumari B, Vrati S, Basu A, Banerjee A. Japanese Encephalitis Virus-induced let-7a/b interacted with the NOTCH-TLR 7 pathway in microglia and facilitated neuronal death via caspase activation. J Neurochem. 2019;149(4):518–534. doi: 10.1111/jnc.14645. [DOI] [PubMed] [Google Scholar]
- 248.Carpp LN, Galler R, Bonaldo MC. Interaction between the yellow fever virus nonstructural protein NS3 and the host protein Alix contributes to the release of infectious particles. Microbes Infect. 2011;13(1):85–95. doi: 10.1016/j.micinf.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 249.Reyes-Ruiz JM, Osuna-Ramos JF, Jesús-González D, Adrián L, Palacios-Rápalo SN, Cordero-Rivera CD, Farfan-Morales CN, Hurtado-Monzón AM, Gallardo-Flores CE, Alcaraz-Estrada SL. The regulation of flavivirus infection by hijacking exosome-mediated cell–cell communication: new insights on virus–host interactions. Viruses. 2020;12(7):765. doi: 10.3390/v12070765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Thepparit C, Khongwichit S, Ketsuwan K, Libsittikul S, Auewarakul P, Smith DR. Dengue virus requires apoptosis linked gene-2-interacting protein X (ALIX) for viral propagation. Virus Res. 2019;261:65–71. doi: 10.1016/j.virusres.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 251.York SB, Sun L, Cone AS, Duke LC, Cheerathodi MR, Meckes DG., Jr Zika virus hijacks extracellular vesicle tetraspanin pathways for cell-to-cell transmission. Msphere. 2021;6(3):e00192–e1121. doi: 10.1128/mSphere.00192-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Umar M, Manzoor S. CD81+ exosomes play a pivotal role in the establishment of hepatitis C persistent infection and contribute toward the progression of hepatocellular carcinoma. Viral Immunol. 2019;32(10):453–462. doi: 10.1089/vim.2019.0077. [DOI] [PubMed] [Google Scholar]
- 253.Barouch-Bentov R, Neveu G, Xiao F, Beer M, Bekerman E, Schor S, Campbell J, Boonyaratanakornkit J, Lindenbach B, Lu A. Hepatitis C virus proteins interact with the endosomal sorting complex required for transport (ESCRT) machinery via ubiquitination to facilitate viral envelopment. MBio. 2016;7(6):e01456–e11416. doi: 10.1128/mBio.01456-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Devhare PB, Sasaki R, Shrivastava S, Di Bisceglie AM, Ray R, Ray RB. Exosome-mediated intercellular communication between hepatitis C virus-infected hepatocytes and hepatic stellate cells. J Virol. 2017;91(6):e02225–e12216. doi: 10.1128/JVI.02225-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Buffalo CZ, Iwamoto Y, Hurley JH, Ren X. How HIV Nef proteins hijack membrane traffic to promote infection. J Virol. 2019;93(24):e01322–e11319. doi: 10.1128/JVI.01322-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Sadri Nahand J, Bokharaei-Salim F, Karimzadeh M, Moghoofei M, Karampoor S, Mirzaei HR, Tabibzadeh A, Jafari A, Ghaderi A, Asemi Z. MicroRNAs and exosomes: key players in HIV pathogenesis. HIV Med. 2020;21(4):246–278. doi: 10.1111/hiv.12822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Zhang Z, Ma J, Zhang X, Su C, Yao Q-C, Wang X. Equine infectious anemia virus Gag assembly and export are directed by matrix protein through trans-Golgi networks and cellular vesicles. J Virol. 2016;90(4):1824–1838. doi: 10.1128/JVI.02814-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Del Vecchio C, Celestino M, Celegato M, Palù G, Parolin C, Bouamr F, Calistri A. Alix-mediated rescue of feline immunodeficiency virus budding differs from that observed with human immunodeficiency virus. J Virol. 2020;94(11):e02019–02019. doi: 10.1128/JVI.02019-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.González SA, Affranchino JL. Properties and functions of feline immunodeficiency virus Gag domains in virion assembly and budding. Viruses. 2018;10(5):261. doi: 10.3390/v10050261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Welker L, Paillart J-C, Bernacchi S. Importance of viral late domains in budding and release of enveloped RNA viruses. Viruses. 2021;13(8):1559. doi: 10.3390/v13081559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Zhai Q, Fisher RD, Chung H-Y, Myszka DG, Sundquist WI, Hill CP. Structural and functional studies of ALIX interactions with YPXnL late domains of HIV-1 and EIAV. Nat Struct Mol Biol. 2008;15(1):43–49. doi: 10.1038/nsmb1319. [DOI] [PubMed] [Google Scholar]
- 262.Coren LV, Nagashima K, Ott DE. A PLPPV sequence in the p8 region of Gag provides late domain function for mouse mammary tumor virus. Virology. 2019;535:272–278. doi: 10.1016/j.virol.2019.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Sherer NM, Lehmann MJ, Jimenez-Soto LF, Ingmundson A, Horner SM, Cicchetti G, Allen PG, Pypaert M, Cunningham JM, Mothes W. Visualization of retroviral replication in living cells reveals budding into multivesicular bodies. Traffic. 2003;4(11):785–801. doi: 10.1034/j.1600-0854.2003.00135.x. [DOI] [PubMed] [Google Scholar]
- 264.Martin-Serrano J, Eastman SW, Chung W, Bieniasz PD. HECT ubiquitin ligases link viral and cellular PPXY motifs to the vacuolar protein-sorting pathway. J Cell Biol. 2005;168(1):89–101. doi: 10.1083/jcb.200408155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Abe M, Fukuma A, Yoshikawa R, Miyazawa T, Yasuda J. Inhibition of budding/release of porcine endogenous retrovirus. Microbiol Immunol. 2014;58(8):432–438. doi: 10.1111/1348-0421.12166. [DOI] [PubMed] [Google Scholar]
- 266.Dupont A, Glück IM, Ponti D, Stirnnagel K, Hütter S, Perrotton F, Stanke N, Richter S, Lindemann D, Lamb DC. Identification of an intermediate step in foamy virus fusion. Viruses. 2020;12(12):1472. doi: 10.3390/v12121472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Hütter S, Zurnic I, Lindemann D. Foamy virus budding and release. Viruses. 2013;5(4):1075–1098. doi: 10.3390/v5041075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Buckmaster MV, Zadrozny KK, Ganser-Pornillos BK, Pornillos O, Goff SP. Structural determinants of virion assembly and release in the C terminus of the Mason-Pfizer monkey virus capsid protein. J Virol. 2021;95(19):e00615–00621. doi: 10.1128/JVI.00615-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Gottwein E, Bodem J, Müller B, Schmechel A, Zentgraf H, Kräusslich H-G. The Mason-Pfizer monkey virus PPPY and PSAP motifs both contribute to virus release. J Virol. 2003;77(17):9474–9485. doi: 10.1128/jvi.77.17.9474-9485.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Blot V, Perugi F, Gay B, Prévost M-C, Briant L, Tangy F, Abriel H, Staub O, Dokhélar M-C, Pique C. Nedd4. 1-mediated ubiquitination and subsequent recruitment of Tsg101 ensure HTLV-1 Gag trafficking towards the multivesicular body pathway prior to virus budding. J Cell Sci. 2004;117(11):2357–2367. doi: 10.1242/jcs.01095. [DOI] [PubMed] [Google Scholar]
- 271.Li Y, Chen Y, Zhang N, Fan D. Human endogenous retrovirus K (HERV-K) env in neuronal extracellular vesicles: a new biomarker of motor neuron disease. Amyotroph Lateral Scler Frontotemporal Degener. 2021;1–8 [DOI] [PubMed]
- 272.Chudak C, Beimforde N, George M, Zimmermann A, Lausch V, Hanke K, Bannert N. Identification of late assembly domains of the human endogenous retrovirus-K (HML-2) Retrovirology. 2013;10(1):1–14. doi: 10.1186/1742-4690-10-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Chahar HS, Corsello T, Kudlicki AS, Komaravelli N, Casola A. Respiratory syncytial virus infection changes cargo composition of exosome released from airway epithelial cells. Sci Rep. 2018;8(1):1–18. doi: 10.1038/s41598-017-18672-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Kikonyogo A, Bouamr F, Vana ML, Xiang Y, Aiyar A, Carter C, Leis J. Proteins related to the Nedd4 family of ubiquitin protein ligases interact with the L domain of Rous sarcoma virus and are required for gag budding from cells. Proc Natl Acad Sci. 2001;98(20):11199–11204. doi: 10.1073/pnas.201268998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Villarroya-Beltri C, Gutiérrez-Vázquez C, Sánchez-Cabo F, Pérez-Hernández D, Vázquez J, Martin-Cofreces N, Martinez-Herrera DJ, Pascual-Montano A, Mittelbrunn M, Sánchez-Madrid F. Sumoylated hnRNPA2B1 controls the sorting of miRNAs into exosomes through binding to specific motifs. Nat Commun. 2013;4:2980–2980. doi: 10.1038/ncomms3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Chivero ET, Bhattarai N, McLinden JH, Xiang J, Stapleton JT. Human Pegivirus (HPgV; formerly known as GBV-C) inhibits IL-12 dependent natural killer cell function. Virology. 2015;485:116–127. doi: 10.1016/j.virol.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Han Z, Ruthel G, Dash S, Berry CT, Freedman BD, Harty RN, Shtanko O. Angiomotin regulates budding and spread of Ebola virus. J Biol Chem. 2020;295(25):8596–8601. doi: 10.1074/jbc.AC120.013171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Takamatsu Y, Kolesnikova L, Schauflinger M, Noda T, Becker S. The Integrity of the YxxL Motif of Ebola Virus VP24 Is Important for the Transport of Nucleocapsid-Like Structures and for the Regulation of Viral RNA Synthesis. J Virol. 2020;94(9):e02170–e12119. doi: 10.1128/JVI.02170-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Han Z, Ye H, Liang J, Shepley-McTaggart A, Wrobel JE, Reitz AB, Whigham A, Kavelish KN, Saporito MS, Freedman BD, Shtanko O, Harty RN. Compound FC-10696 inhibits egress of marburg virus. Antimicrob Agents Chemother. 2021;65(7):e0008621–e0008621. doi: 10.1128/AAC.00086-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Loughran HM, Han Z, Wrobel JE, Decker SE, Ruthel G, Freedman BD, Harty RN, Reitz AB. Quinoxaline-based inhibitors of Ebola and Marburg VP40 egress. Bioorg Med Chem Lett. 2016;26(15):3429–3435. doi: 10.1016/j.bmcl.2016.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Dolnik O, Kolesnikova L, Stevermann L, Becker S. Tsg101 Is recruited by a late domain of the nucleocapsid protein to support budding of marburg virus-like particles. J Virol. 2010;84(15):7847–7856. doi: 10.1128/JVI.00476-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Baillet N, Krieger S, Carnec X, Mateo M, Journeaux A, Merabet O, Caro V, Tangy F, Vidalain P-O, Baize S. E3 ligase ITCH interacts with the Z matrix protein of lassa and mopeia viruses and is required for the release of infectious particles. Viruses. 2020;12(1):49. doi: 10.3390/v12010049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Eichler R, Strecker T, Kolesnikova L, ter Meulen J, Weissenhorn W, Becker S, Klenk HD, Garten W, Lenz O. Characterization of the Lassa virus matrix protein Z: electron microscopic study of virus-like particles and interaction with the nucleoprotein (NP) Virus Res. 2004;100(2):249–255. doi: 10.1016/j.virusres.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 284.Zhang Y, Wang Y, Feng Y, Tu Z, Lou Z, Tu C. Proteomic profiling of purified rabies virus particles. Virol Sin. 2020;35(2):143–155. doi: 10.1007/s12250-019-00157-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Wirblich C, Tan GS, Papaneri A, Godlewski PJ, Orenstein JM, Harty RN, Schnell MJ. PPEY motif within the rabies virus (RV) matrix protein is essential for efficient virion release and RV pathogenicity. J Virol. 2008;82(19):9730–9738. doi: 10.1128/JVI.00889-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Havranek KE, Reyes Ballista JM, Hines KM, Brindley MA. Untargeted lipidomics of vesicular stomatitis virus-infected cells and viral particles. Viruses. 2021;14(1):3. doi: 10.3390/v14010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Harrison MS, Schmitt PT, Pei Z, Schmitt AP. Role of ubiquitin in parainfluenza virus 5 particle formation. J Virol. 2012;86(7):3474–3485. doi: 10.1128/JVI.06021-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Ueda H, Yamakawa N, Takeuchi K. Amino- and carboxyl-terminal ends of the bovine parainfluenza virus type 3 matrix protein are important for virion and virus-like particle release. Virology. 2021;561:17–27. doi: 10.1016/j.virol.2021.05.014. [DOI] [PubMed] [Google Scholar]
- 289.Duan Z, Hu Z, Zhu J, Xu H, Chen J, Liu H, Hu S, Liu X. Mutations in the FPIV motif of Newcastle disease virus matrix protein attenuate virus replication and reduce virus budding. Adv Virol. 2014;159(7):1813–1819. doi: 10.1007/s00705-014-1998-2. [DOI] [PubMed] [Google Scholar]
- 290.Li M, Schmitt PT, Li Z, McCrory TS, He B, Schmitt AP. Mumps virus matrix, fusion, and nucleocapsid proteins cooperate for efficient production of virus-like particles. J Virol. 2009;83(14):7261–7272. doi: 10.1128/JVI.00421-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Primadharsini PP, Nagashima S, Takahashi M, Kobayashi T, Nishiyama T, Nishizawa T, Yasuda J, Mulyanto OH. Multivesicular body sorting and the exosomal pathway are required for the release of rat hepatitis E virus from infected cells. Virus Res. 2020;278:197868. doi: 10.1016/j.virusres.2020.197868. [DOI] [PubMed] [Google Scholar]
- 292.Nagashima S, Takahashi M, Jirintai S, Tanggis KT, Nishizawa T, Okamoto H. The membrane on the surface of hepatitis E virus particles is derived from the intracellular membrane and contains trans-Golgi network protein 2. Adv Virol. 2014;159(5):979–991. doi: 10.1007/s00705-013-1912-3. [DOI] [PubMed] [Google Scholar]
- 293.Jiang W, Ma P, Deng L, Liu Z, Wang X, Liu X, Long G. Hepatitis A virus structural protein pX interacts with ALIX and promotes the secretion of virions and foreign proteins through exosome-like vesicles. J Extracell Vesicles. 2020;9(1):1716513–1716513. doi: 10.1080/20013078.2020.1716513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Robinson SM, Tsueng G, Sin J, Mangale V, Rahawi S, McIntyre LL, Williams W, Kha N, Cruz C, Hancock BM, Nguyen DP, Sayen MR, Hilton BJ, Doran KS, Segall AM, Wolkowicz R, Cornell CT, Whitton JL, Gottlieb RA, Feuer R. Coxsackievirus B exits the host cell in shed microvesicles displaying autophagosomal markers. PLoS Pathog. 2014;10(4):e1004045–e1004045. doi: 10.1371/journal.ppat.1004045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Gu J, Wu J, Fang D, Qiu Y, Zou X, Jia X, Yin Y, Shen L, Mao L. Exosomes cloak the virion to transmit enterovirus 71 non-lytically. Virulence. 2020;11(1):32–38. doi: 10.1080/21505594.2019.1705022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Huang H-I, Lin J-Y, Chiang H-C, Huang P-N, Lin Q-D, Shih S-R. Exosomes facilitate transmission of enterovirus A71 from human intestinal epithelial cells. J Infect Dis. 2020;222(3):456–469. doi: 10.1093/infdis/jiaa174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Fu Y, Zhang L, Zhang F, Tang T, Zhou Q, Feng C, Jin Y, Wu Z. Exosome-mediated miR-146a transfer suppresses type I interferon response and facilitates EV71 infection. PLoS Pathog. 2017;13(9):e1006611–e1006611. doi: 10.1371/journal.ppat.1006611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Fernández de Castro I, Tenorio R, Ortega-González P, Knowlton JJ, Zamora PF, Lee CH, Fernández JJ, Dermody TS, Risco C. A modified lysosomal organelle mediates nonlytic egress of reovirus. J Cell Biol. 2020;219(7):e201910131. doi: 10.1083/jcb.201910131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed in the manuscript are included in this article.