Abstract
The aim of this study was to describe a new strategy, consisting of the use of cone-beam computed tomography (CBCT) in the planning and intraoperative stages of root canal treatment (RCT), associated with the use of radiopaque gutta-percha markers, as an auxiliary tool in the location of severely calcified root canals. Three cases involving anterior and posterior teeth with severe calcification of the root canal were submitted to initial periapical radiographic and CBCT evaluations for diagnosis and planning of the operative steps. In a first intervention, when the location of the canal orifice was not successful, radiopaque markers were inserted in the suggested position of canal orifice with the aid of magnification and the use of ultrasonic devices, in order to perform an intraoperative CBCT analysis that allowed dynamic navigation through the static position of markers. The association of intraoperative CBCT with radiopaque markers allowed the location of the canal orifice and the following RCT execution. The use of CBCT in two different moments of RCT allowed the diagnosis of three-dimensional anatomical variations of root canal. Add, when associated with the use of radiopaque gutta-percha markers, acted as an auxiliary tool in the location of the canal orifice of calcified canals. Therefore, the presented strategy provides the clinician the precision that cases with calcification require and give an important contribution to treatment predictability.
Key Words: Cone-Beam Computed Tomography, Dental Pulp Calcification, Intraoperative, Root Canal Treatment
Introduction
Dental pulp calcifications result from accelerated deposition of mineralized tissue into the pulp chamber and root canal system (RCS) in response to external aggressors, as a result of trauma, orthodontic movements, caries lesions and previous restorative interventions with the use of materials that induce the formation of this mineralized tissue [1]. This reactive dentin deposition can lead to partial or complete obliteration of the root canal [2]. Clinically, teeth with calcifications may be discolored and yellowish, opaque, and have a higher degree of chromaticity, as well as diminished response to pulp vitality tests, making it difficult to diagnose pulpal disorders [3]. Not all cases of dental pulp calcifications require intervention; however, the presence of an inflammatory process of the pulp tissue, microbial contamination of the RCS or development of periapical pathology, makes it necessary to perform root canal treatment [4].
The American Association of Endodontics considers that the procedure involved in root canal treatment of calcified canals has a high level of difficulty and complexity [5], since location of the canal orifices and their biomechanical preparation represent a clinical challenge. Moreover, these procedures are often associated with excessive wear of the tooth structure, as well as a higher risk of canal deviation and root perforation, even when performed with the aid of magnification tools [6, 7].
Radiographic exams initially used as diagnostic imaging can increase the ability to diagnose pulpal calcifications, but two-dimensional images do not provide conclusive information relative to the direction and details of the internal anatomy of the RSC. Thus, with the aim of allowing three-dimensional analysis, imaging exams such as cone-beam computed tomography (CBCT) are important tools for accurate diagnosis and planning of more complex cases, such as dental pulp calcifications [8, 9]. Therefore, it is necessary to plan the ideal time to perform the CBCT scan, whether it is for diagnostic, intraoperative or follow-up purposes, in addition to defining accurate parameters for use to capture the images. The literature highlights the use of CBCT in endodontics, especially in the initial treatment time, for the purposes of diagnostic imaging and follow-up of treatment [5, 8]. However, in recent years an increase has also been observed in the intraoperative use of CBCT for the location of the second mesiobuccal (MB2) canal, diagnosis of resorptions, fractures and location of calcified canals [10].
In this scenario, Floratos and Miltiadous [11] proposed a new technique, in which gutta-percha points are used as markers of the suggested position of the root canal orifice that is evaluated in all planes of the CBCT images. However, up to now, there has been no complete and detailed description of this methodology, or assessment of when it would be the ideal time to insert the gutta-percha points, and a critical analysis of the technique.
Therefore, the present study aimed to report a series of cases in which the radiopaque gutta-percha marker technique was used as an auxiliary tool in the location of calcified canals, associated with the use of intraoperative CBCT, ultrasonic devices and image magnification tools.
Case Reports
Case 1
A 58-year-old woman was referred to the private dental office (endodontic referral clinical in Lisbon, Portugal) for endodontic evaluation, due to complaints associated with teeth in the first quadrant. No relevant medical history, and no extra-oral changes were detected. The patient complained of sporadic discomfort imprecisely localized in the right maxillary region, which worsened when chewing, and had been present for several months.
During clinical evaluation, tooth #16 showed an extensive composite resin restoration on the mesial and occlusal surfaces, with grade 1 tooth mobility, and periodontal probing scores were within healthy limits. A vestibular sinus tract was observed, with positive complaints in response to percussion and palpation tests, and no response to the cold pulp test (Endo Cold Spray; Henry Schein, Langen, Germany). The initial periapical radiograph revealed three independent roots, with alterations at the level of the periapical bone trabeculae and apparent reduction in volume of the pulp chamber, especially in the area of the mesial pulp horn (Figure 1A and 1B). For this reason, a preoperative CBCT scan was performed (Veraview 800; J Morita MFG, Kyoto, Japan), with 90 kV, 2mA, 4040 mm field of view (FOV) and 0.2 mm voxel (Figures 1C-1E), as a complementary tool for use in diagnosis and planning. In this examination, severe calcification of the first mesiobuccal (MB1) canal was evident, more pronounced than that found in the MB2 canal (Figures. 1D and 1E). The diagnosis of chronic apical periodontitis was then established, and non-surgical root canal treatment was chosen as the treatment plan. The treatment process was explained to the patient and informed consent was obtained from her.
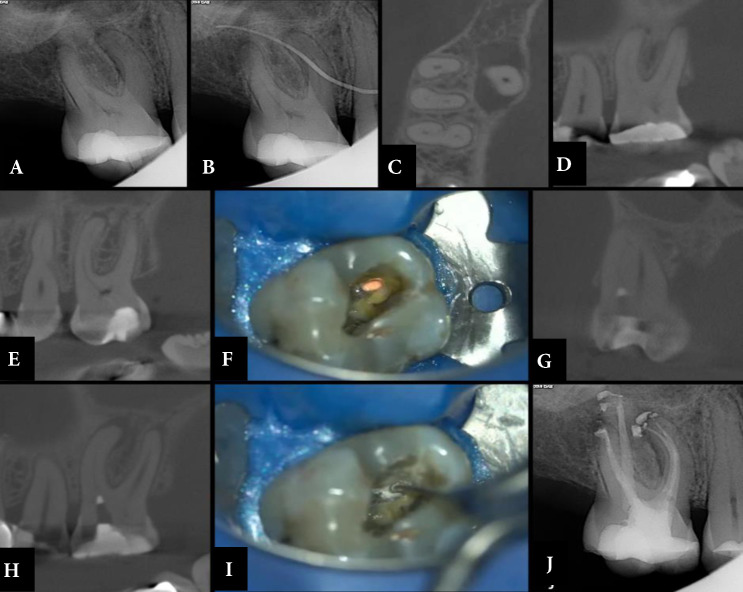
Figure 1.
A) Initial periapical radiography; B) Radiography of fistulous path, revealing the origin of chronic apical periodontitis; C) Axial plane of initial CBCT, where presence of two canals (MB1 and MB2) in mesio-buccal root is observed; D) Sagittal plane of initial CBCT scan performed at level of canal MB1, highlighting severe calcification presented and drawing attention to probable difficulty in locating it; E) Sagittal plane of initial CBCT scan performed at level of canal MB2, highlighting its permeability and continuation with pulp chamber, which facilitated its localization; F) Gutta-percha radiopaque point applied at MB end of pulp chamber floor; G) Coronal plane of intraoperative CBCT with radiopaque gutta-percha point showing palatal location of canal in relation to radiopaque marker; H) Intraoperative CBCT axial plane showing no deviation in various planes; I) Intraoperative CBCT sagittal plane with radiopaque gutta-percha marker showing no excessive wear mesially or distally and apical location to radiopaque marker. J) Selective grinding in region marked by intraoperative CBCT, with ultrasonic insert Finder (Helse, Brazil). K) Final radiograph, highlighting obturation of Vertucci type IV canals MB1 and MB2
In the first appointment, after infiltrative buccal anesthesia with 1.8 mL of 4% articaine with epinephrine 1:200.000 (Artinibsa; Inibsa Dental, Llia de Vall, Barcelona, Spain), tooth was isolated using a rubber dam, and access to the pulp chamber was obtained with a spherical diamond bur rotating at high-speed. This was refined with an ultrasonic insert (US) Start-X 1 (Dentsply Maillefer, Ballaigues, Switzerland), under magnification by using an operating microscope (Flexion Advanced; CJ-Optik, Germany). Three root canals were located: distobuccal (DB), palatal (P) and the second mesiobuccal (MB2). Unexpectedly, contrary to findings usually expected by CBCT observation, it was possible to locate the MB2 canal before the MB1 canal. The glide-path was then established with a #10 and #15 K-file (Dentsply Maillefer, Switzerland) and the working lenghts were determined with the aid of the electronic apical locator (Root-ZX; Morita, Tokyo, Japan), and the canals were instrumented under irrigation with 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Spain), with the WaveOne Gold reciprocating file system (Dentsply Maillefer, Ballaigues, Switzerland) coupled to a Smart-X Plus motor (Dentsply Maillefer, Ballaigues, Switzerland), according to the manufacturer's instructions. The RCS was irrigated with 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Spain) throughout the entire instrumentation procedure. After complete instrumentation of MB2 canal, a search for MB1 canal began with the aid of US Start-X 2 (Dentsply Maillefer, Ballaigues, Switzerland) inserts in the region situated vestibular to MB2 canal, which corresponded to the probable location of the MB1 canal orifice.
After unsuccessfully seeking this location, in spite of a significant period of ultrasonic insert wear, it was decided to apply a radiopaque marker, in order to avoid the increased risk of excessive wear and eventual root perforation, end the session, and perform an intraoperative CBCT exam. This would provide three-dimensional guidance in the search and location of the MB1 canal in the following session. A small portion of injectable gutta-percha was used as a radiopaque marker, which was applied with Obtura II Gutta-percha gun (Obtura Spartan, Fenton, MO, USA) at the furthest MB end of the floor of the access cavity (Figure 1F). The tooth was provisionally restored (Teflon and Cavit, 3M, Germany) and immediately before the second session, a new intraoperative CBCT scan was performed (Veraview 800, Morita, Japan) with settings of 90 kV, 2mA, FOV 4040 mm and voxel 0.2 mm. Observation of these CBCT images enabled visualization of the MB1 canal orifice and the radiopaque gutta-percha points, and allowed three-dimensional correlation, making it possible to conclude that the MB1 canal entrance was in a more apical and more palatal location to the point indicated by the radiopaque gutta-percha point (Figure 1G-1I). This detailed information made it possible to locate the MB1 canal quickly and without procedural error, with the aid of Finder ultrasonic insert (Helse, Santa Rosa de Viterbo, SP, Brazil) (Figure 1J) and ISO #10 C-Pilot hand file (VDW, Munich, Germany), under microscopic magnification.
Instrumentation was performed according to the same protocol described previously. The final irrigation protocol performed consisted of 17% EDTA (Laboratorios Clarben S.A., Spain), irrigation for 1 min, followed by 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Spain). The canals were dried with paper cones and obturation was performed with epoxy resin-based cement (AH-Plus, Dentsply Maillefer, Ballaigues, Switzerland) and gutta-percha, by using the continuous wave vertical condensation technique with System B (Sybron Endo, Orange, CA, USA) and Obtura II (Obtura Spartan, Fenton, MO, USA). After cleaning the pulp chamber with alcohol, intra-coronal sealing was performed with glass ionomer (Ionoseal, Voco GmbH, Cuxhaven, Germany) cement, and provisional restoration (Cavit, 3M, Seefeld, Germany), followed by occlusal adjustment (Figure 1K).
Case 2
A 32-year-old woman patient was referred to the private dental office (endodontic referral clinical in Lisbon, Portugal) for endodontic evaluation, after radiographic detection of possible internal resorption in tooth 41 during an orthodontic control visit. No relevant medical history and no extra-oral changes were observed. Patient mentioned no pain present at the time of examination, but reported a history of increased pain on cold thermal stimuli, and occasional spontaneous pain. Tooth #41 showed grade 1 tooth mobility and periodontal probing scores within healthy limits; negative percussion tests, with no associated pain; increased pain response to cold sensitivity testing (Endo Cold Spray, Henry Schein, Germany), with slow remission.
The initial periapical radiograph revealed severe root canal calcification, presence of internal resorption located in the region of the coronal third of the root and thickening of the periodontal ligament (Figure 2A). As a complementary means of diagnosis and planning, a preoperative CBCT scan was performed (Veraview 800, Morita, Japan), with 90 kV, 2 mA, 4040 mm FOV and 0.2 mm voxel. This examination confirmed severe calcification of the root canal and the presence of internal resorption, with irregular peripheral expansion in the region of the coronal third of the root, without root perforation (Figures 2B and 2C). The diagnosis of internal resorption with irreversible inflammation of the pulp was then established, and non-surgical root canal treatment was indicated. The treatment process was explained to the patient and informed consent was obtained from her.
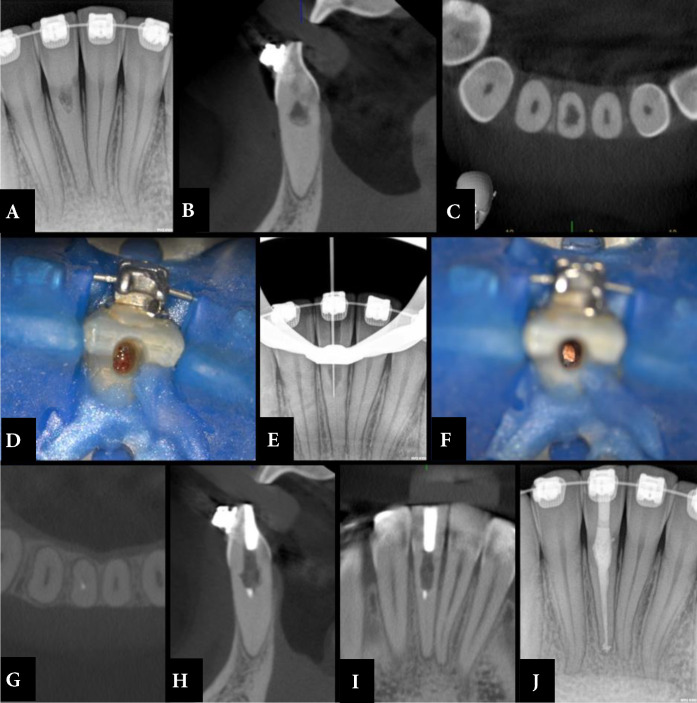
Figure 2.
A) Initial periapical radiograph demonstrating severe internal calcification of root canal; B, C) Sagittal and axial planes, respectively, of initial CBCT, where presence of resorption and its exact three-dimensional location can be observed, with no associated root perforation; D) Photograph taken after access surgery, showing presence of granulation tissue in area of resorption; E) Intraoperative periapical radiograph, where slight deviation in distal direction was detected; F) Picture after placing gutta-percha radiopaque point, in deepest area of abrasion performed with ultrasound; G, H and I) Axial, sagittal and coronal planes, respectively, of intraoperative CBCT, in which radiopaque gutta-percha marker can be seen and correlated with center of root, where canal is located; J) Final radiograph, with three-dimensional obturation of root canal and internal resorption
In the first visit, after infiltrative buccal anesthesia with 1.8 mL of articaine 4% with epinephrine 1:200,000 (Artinibsa, Inibsa, Spain) and absolute isolation , access to the resorption site was obtained with a spherical diamond bur rotating at high-speed, under microscopic magnification (Flexion Advanced, CJ-Optik, Germany), enabling the presence of granulation tissue to be observed (Figure 2D). Irrigation with 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Spain) and mechanical cleaning of the resorption area with a Clearsonic ultrasonic insert (Helse, Brazil) were performed. Subsequently, ISO steel hand files #10 K and #15 K (Dentsply Maillefer, Ballaigues, Switzerland) were used to seek the location of the root canal orifice, in the region apical to the internal resorption, while advancing in the apical direction by means of controlled grinding performed with the Finder ultrasonic insert (Helse, Santa Rosa do Viterbo, SP, Brazil).
As the canal orifice had not yet located after some apical advancement, a periapical radiograph was taken with a digital spacer size A (Dentsply Maillefer, Switzerland), placed in the deepest zone of the grinding performed. This radiograph revealed a slight distal deviation in the mesial-distal direction that made it impossible to evaluate any possible deviation in the vestibular-lingual direction (Figure 2E). Therefore, it was decided to apply a radiopaque marker at that point, end the session and have an intraoperative CBCT scan performed to provide three-dimensional guidance in finding and locating the canal orifice in the next session. The radiopaque marker chosen was a small portion of injectable gutta-percha, applied with Obtura II gutta-percha gun (Obtura Spartan, USA) at the deepest site of wear (Figure 2F). The tooth was provisionally restored (Teflon and Cavit, 3M, Germany) and immediately before the second session a new intraoperative CBCT scan was performed (Veraview X800, Morita, Kyoto, Japan) with settings of 90 kV, 2 mA, FOV 4040 mm and voxel 0.2 mm.
Observation of these CBCT images allowed visualization of the radiopaque gutta-percha markers and their three-dimensional correlation with the possible location of the canal orifice. As it was not possible to visualize the canal in CBCT images, it was decided to correlate the radiopaque marker with the root center, where the canal would usually be located. Therefore, these CBCT images made it possible to conclude that there was an effective deviation in the distal and buccal direction (Figures 2G-2I). With this information, it was possible to redirect the wear with the Finder ultrasonic insert (Helse, Brazil), and finally locate the canal quickly and without procedural errors, by using an ISO #10 C-Pilot hand file.
Instrumentation was performed with the WaveOne Gold reciprocating system (Dentsply Maillefer, Switzerland) coupled to the Smart-X Plus motor (Dentsply Maillefer, Switzerland) according to the manufacturer's instructions. The canal was irrigated with 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Spain) throughout the entire instrumentation procedure. The final irrigation protocol performed consisted of 17% EDTA (Laboratorios Clarben S.A., Spain), irrigation for 1 minute, followed by 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Murcia, Spain). The canal was dried with paper cones and obturation was performed with epoxy resin-based cement (AH-Plus; Dentsply Maillefer, Ballaigues, Switzerland) and gutta-percha by using the continuous wave vertical condensation technique with System B (Sybron Endo, USA) and Obtura II (Obtura Spartan, Fenton, MO, USA). After cleaning the pulp chamber with alcohol, glass ionomer (Ionoseal; Voco GmbH, Cuxhaven, Germany) was used for intracoronal sealing, and provisional restoration was performed (Cavit, 3M, Seefeld, Germany) (Figure 2J).
Case 3
A 26-year-old man patient was referred to the private dental office (endodontic referral clinical in Lisbon, Portugal) for endodontic evaluation, due to complaints associated with teeth in the first quadrant. No relevant medical history and no extra-oral changes were observed. Patient complained of sporadic discomfort with precise location in tooth 11, with a history of trauma; however, the patient did not know the specific date of occurrence, as he only remembered the fact because the tooth color changed (Figure 3A). Tooth #11 had grade I tooth mobility and periodontal probing scores within healthy limits. The patient reported a positive complaint to percussion and palpation tests, with no response to the cold pulp test (Endo Cold Spray; Henry Schein, Langen, Germany). The initial periapical radiograph revealed reduction in the volume of pulp chamber and root canal up to the middle third (Figure 3B). For this reason, a preoperative CBCT scan (Veraview R100, Morita, Japan), with settings of 80 kV, 3 mA, FOV 40 mm40 mm and voxel 0.2 mm was performed as a complementary tool for use in diagnosis and planning (Figures 3C and 3D).
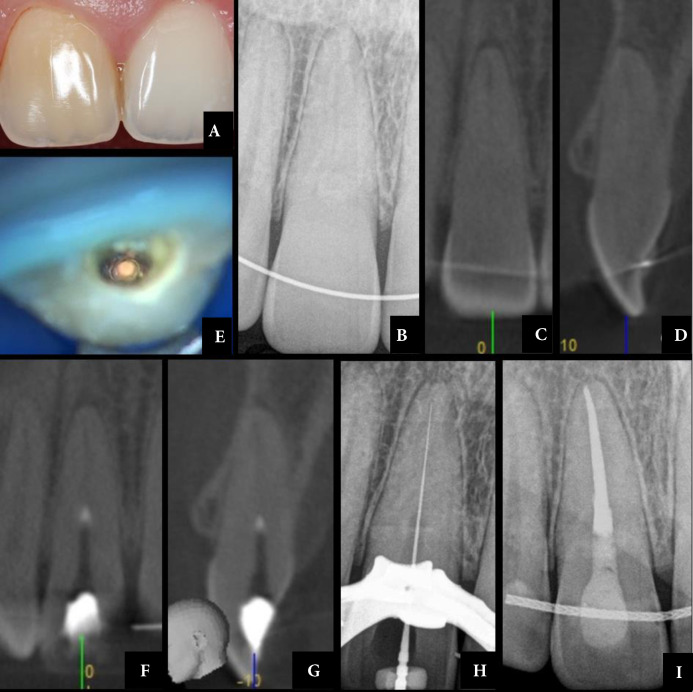
Figure 3.
A) Initial photograph showing difference in coloration due to dentin deposition; B) Initial periapical radiograph demonstrating severe calcification of root canal; C and D) Coronal and sagittal planes, respectively, of initial CBCT; E) Photograph after placement of radiopaque gutta-percha point in deepest zone of ultrasound-guided abrasion; F and G) Coronal and sagittal planes, respectively, of intraoperative CBCT, in which radiopaque gutta-percha marker is observed and correlated with root center; H) Intraoperative periapical radiograph, after canal location; I) Intraoperative periapical radiograph, after main cone positioning; J) Final radiograph, with three-dimensional root canal obturation
After diagnosis of pulp necrosis, the treatment plan proposed and accepted was non-surgical root canal treatment. The treatment process was explained to the patient and informed consent was obtained. In the first appointment, after infiltrative buccal anesthesia with 1.8 mL of 4% articaine with epinephrine 1:200,000 (Artinibsa, Inibsa, Spain) and absolute isolation, with the aid of magnification under an operating microscope (DF Vasconcelos, So Paulo, SP, Brazil) access to the pulp chamber was obtained with a spherical diamond bur rotating at high-speed, and the access was refined with an ultrasonic insert Start-X 1 (Dentsply Maillefer, Ballaigues, Switzerland).
Due to obliteration, wear was performed with US Start-X 2 (Dentsply Maillefer, Ballaigues, Switzerland) insert in the central region of the pulp chamber. After this, in order to avoid excessive wear that could increase the risk of perforation, a three-dimensional search was proposed in an area corresponding to the probable location of the canal orifice, specifically for location of the canal orifice. For this purpose, a small portion of injectable gutta-percha was applied with gutta-percha gun EQ-V (Metabiomed, Cheongju, South Korea) (Figure 3E) to act as a three-dimensional guide. The tooth was provisionally restored (Cavit, 3M, Germany) and immediately before the second session, a new intraoperative CBCT scan was performed (Veraview R100, Morita, Japan), with settings of 80 kV, 3 mA, FOV 40 mm40 mm and voxel 0.2 mm. From the place where the radiopaque marker was observed, it was possible to visualize the location of the canal orifice and the distance to the wear point marked by the gutta-percha (Figure 3F) and (Figure 3G). Thus, the canal was located with the aid of US Start-X 3 tip (Dentsply Maillefer, Ballaigues, Switzerland) and hand file ISO #10 C-Pilot (VDW, Munich, Germany). The glide path was obtained using a steel hand file ISO #10 K C-Pilot and #15 K (Dentsply Maillefer, Ballaigues, Switzerland) with the aid of an electronic apical locator (Root-ZX, Morita, Kyoto, Japan) (Figure 3H). The canal was instrumented with the ProTaper Next NiTi file system (ProTaper Next, Dentsply Maillefer, Switzerland), coupled to the Smart-X Plus motor (Dentsply Maillefer, Switzerland), according to the manufacturer's instructions. The canal was irrigated with 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Spain) throughout the entire instrumentation procedure. The final irrigation protocol performed consisted of 17% EDTA (Laboratorios Clarben S.A., Spain) irrigation for 1-minute followed by 5.25% sodium hypochlorite (Denta Flux, J. Ripoll SL, Spain). The canal was dried with paper cones and obturation was performed with epoxy resin-based cement (AH-plus, Dentsply Maillefer, Ballaigues, Switzerland) and gutta-percha using the vertical continuous wave condensation technique with EQ-V (Metabiomed, Cheongju, South Korea). After cleaning the pulp chamber with alcohol, Tetric Evo Flow (Ivoclar Vivadent, Amherst, NY, USA) was used for intra-coronal sealing, and restoration was performed with composite resin (3M, ESPE Germany) (Figure 3I).
Discussion
Severe or total calcification of dental root canals can be a consequence of caries lesions, abfraction, abrasion, pulp capping, occlusal imbalance, parafunctional habits, aging, trauma and orthodontic movements [9]. With regard to dental trauma, considering that evidence in the literature has shown that up to 24% of traumatized teeth develop different degrees of pulp obliteration [2] and that up to a quarter of post-traumatic calcification cases can develop periapical pathology, cases such as these make it necessary to perform the root canal treatment. Thus, proper planning of the case and the choice of imaging resources, instruments and tools for execution of the operative procedures are important factors, in order to achieve treatment success. Moreover, this must be achieved without excessive dentin wear and weakening of remaining coronal structure, as well as reduced risk of root perforation.
Therefore, several techniques have been proposed to make the operative procedure related to root canal treatment of calcified teeth predictable and with less risk. Noteworthy are procedures used to gain access through the incisal border in anterior teeth [12], analysis and observation of different dentin colors, since the calcified pulp chamber consists of a darker-colored dentin as a result of sclerotic dentin formation [13]. Other helpful techniques include the use of magnification tools [14], dyes such as methylene blue, bubble test or "champagne effect" observed under microscope magnification [15], multiple radiographic incidences performed at different angulations [16], periapical endodontic surgery [2] and use of specific ultrasonic devices [17]. Furthermore, in the last decade the use of CBCT has emerged as a complementary planning mechanism through dynamic 3D navigation [8, 18], and is, therefore, capable of being applied to cases of dental pulp calcification, either at the time of diagnosis for initial evaluation of the case and knowledge of the internal anatomy [8, 18, 19], or during the intraoperative procedure, as reported by Ball et al. [10] in a review article. Notably, the use of CBCT has enabled the development of endodontic guides for access to and glide paths of calcified canals [3, 20].
Therefore, this report on a case series described the use of CBCT in detail, in two moments of root canal treatment of calcified teeth, firstly for clinical planning, and then as an intraoperative resource associated with the technique of using radiopaque gutta-percha points, in order to facilitate the endodontic approach to treatment of teeth with severe dental pulp calcification. Since identification and location of calcified canals orifice, such as those in the cases described, represent a highly complex challenge and level of difficulty, to even the most experienced clinicians. Both the American Association of Endodontics and the American Academy of Oral and Maxillofacial Radiology have listed the above-mentioned procedure as being one of the 12 clinical applications for the use of CBCT [5]. This indication also forms part of the guidelines suggested by the European Society of Endodontics [21].
Therefore, when considering the initial planning of the three cases presented, the use of CBCT allowed not only the complexity of the SCR and root geometry to be evaluated, but also the level and extent of dental pulp calcification, position of the root canal orifice. This was especially relevant in the Case 1, in which the localization of the canal MB2 was oriented towards the positions of MB1 and P. Thus, the first CBCT images enabled the professional, to begin the operative procedure in order to locate canal orifices, with the aid of magnification tools and ultrasonic devices. After treatment began, difficulty in locating the canal orifice continued, even after a significant period of ultrasonic insert wear, associated with the use of magnification tools, observation of clinical signs, inspection with a straight explorer and analysis of changes in dentin coloring. In order to avoid the increasing risk of excessive wear and possible perforation, it was decided to apply a radiopaque marker, interrupt the session, and perform an intraoperative CBCT exam. This provided three-dimensional guidance to continue with the search and location of the canal orifice in a subsequent session.
The intraoperative CBCT, associated with use of the technique with radiopaque gutta-percha points provided static positions of the markers, irrespective of the horizontal and vertical angles used. This enabled spatial reorientation and redirection of the access to reach the root canals, by three-dimensional observation of axial, coronal and sagittal reconstructions, differently from images observed in the two-dimensional analysis of periapical radiographs [19]. The 3D visualization favored more accurate evaluation of anatomical variations and location of adjacent structures, when compared with conventional radiographic techniques obtained by using the parallax principle [22]. This enabled treatment of the cases described.
Furthermore, the use of intraoperative CBCT associated with use of radiopaque gutta-percha points, in the simple technique described in the present report, are procedures particularly indicated for cases of dental pulp calcification [11]. The placement of guides consisting of a sufficient amount of radiopaque gutta-percha points was facilitated by using of an injectable gun, and allowed their visualization in the intraoperative CBCT scan. This promoted detailed analysis of the access maneuvers performed so far, as well as a three-dimensional study of the areas where additional dentin wear should be performed. Less wear is important, especially in the case of treatment of posterior teeth, as observed in the Case 1, describing the treatment of a maxillary first molar with calcified mesial canals. In this case, excessive wear could have led to deviations and perforations; therefore, the use of intraoperative CBCT was essential for locating the canal and performing the treatment with safety.
It is worth mentioning that the technique of endodontic guides for preparing access and glide path of calcified canals has limitations to application in molars, due to patients limited mouth opening, laboratory intervention and additional cost involved [23], even when such guides are made in reduced dimensions [24]. Thus, although the indications of the use of guided endodontics in complex scenarios of calcified molars [25, 26], there is no consensus about the application of endodontic guides in posterior teeth, and despite the number of publications on the topic, there is still a low level of scientific evidence supporting their use[1, 7, 9, 13, 20]. Nevertheless, the technique presented in the present report may be an alternative for use in endodontic treatment of calcified canals in posterior teeth.
In the case of anterior teeth, the use of intraoperative CBCT associated with the technique of using radiopaque gutta-percha points allowed the professional to interrupt the treatment safely, minimizing the risk of excessive dentin wear, deviations and root perforations [11]. Moreover, it favored successful treatment of teeth #41 and #11, reported in the Cases 2 and 3, respectively. Although there is greater acceptance of the technique of using endodontic guides for preparation of access and glide path in calcified canals for root canal treatment of anterior teeth [6, 27, 28]; nevertheless, it is a technique that results in large loss of hard tissue. This arises from wear due to the need for direct access to the root canal, and can lead to the occurrence of deviations and perforations, as was observed in clinical Case 2, in which the beginning of deviation in the original path of the root canal was observed, prior to the use of intraoperative CBCT. Not only is the diameter of drills available at present to perform preparation for the use of guides capable of making the teeth more susceptible to fracture [29], but they also hinder location of the second root canal, present in up to 45.3% of cases of mandibular incisors [30]. Thus, the importance of using of intraoperative CBCT is evident: to analyze the anatomy of RCS, three-dimensional reorientation of biomechanical preparation, adjustment of the wear performed, and for safety in performing the treatment of cases.
Therefore, from the description of the cases in this report, the combination of factors associated with preoperative planning exams, magnification tools, use of ultrasonic devices, as well as professional abilities and clinical diagnostic resources are emphasized. The technique proposed for locating the calcified canal orifice with the use of intraoperative CBCT and guide with radiopaque marker, allowed non-surgical endodontic treatment of anterior and posterior teeth to be performed. Moreover, these procedures allowed less wear of dentin structure, reduced costs, facilitated resources, and avoided errors and accidents during access.
Conclusion
It could be noted that the use of CBCT in two moments of root canal treatment allowed three-dimensional localization of the anatomical variations, and location of the canal orifice. The clinician was provided with precise information required in cases with calcification, and an important contribution was made to treatment predictability.
Acknowledgment
We gratefully acknowledge financial support by the Coordination for the Improvement of Higher Education Personnel (CAPES, Brazil). The authors deny any conflicts of interest. We affirm that we have no financial affiliation (e.g., employment, direct payment, stock holdings, retainers, consultant ships, patent licensing arrangements or honoraria), or involvement with any commercial organization with direct financial interest in the subject or materials discussed in this manuscript, nor have any such arrangements existed in the past three years.
Conflict of Interest:
None declared.
References
- 1.Lara-Mendes STO, Barbosa CFM, Santa-Rosa CC, Machado VC. Guided Endodontic Access in Maxillary Molars Using Cone-beam Computed Tomography and Computer-aided Design/Computer-aided Manufacturing System: A Case Report. J Endod. 2018;44(5):875–9. doi: 10.1016/j.joen.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 2.McCabe PS, Dummer PM. Pulp canal obliteration: an endodontic diagnosis and treatment challenge. Int Endod J. 2012;45(2):177–97. doi: 10.1111/j.1365-2591.2011.01963.x. [DOI] [PubMed] [Google Scholar]
- 3.Torres A, Shaheen E, Lambrechts P, Politis C, Jacobs R. Microguided Endodontics: a case report of a maxillary lateral incisor with pulp canal obliteration and apical periodontitis. Int Endod J. 2019;52(4):540–9. doi: 10.1111/iej.13031. [DOI] [PubMed] [Google Scholar]
- 4.Siqueira JF Jr, Ras IN. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod. 2008;34(11):1291–301. doi: 10.1016/j.joen.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 5.AAE. and AAOMR Joint Position Statement. Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):508–12. doi: 10.1016/j.oooo.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 6.Zehnder MS, Connert T, Weiger R, Krastl G, Khl S. Guided endodontics: accuracy of a novel method for guided access cavity preparation and root canal location. Int Endod J. 2016;49(10):966–72. doi: 10.1111/iej.12544. [DOI] [PubMed] [Google Scholar]
- 7.Buchgreitz J, Buchgreitz M, Bjrndal L. Guided root canal preparation using cone beam computed tomography and optical surface scans - an observational study of pulp space obliteration and drill path depth in 50 patients. Int Endod J. 2019;52(5):559–68. doi: 10.1111/iej.13038. [DOI] [PubMed] [Google Scholar]
- 8.Patel S, Durack C, Abella F, Shemesh H, Roig M, Lemberg K. Cone beam computed tomography in Endodontics - a review. Int Endod J. 2015;48(1):3–15. doi: 10.1111/iej.12270. [DOI] [PubMed] [Google Scholar]
- 9.Lara-Mendes STO, Barbosa CFM, Machado VC, Santa-Rosa CC. A New Approach for Minimally Invasive Access to Severely Calcified Anterior Teeth Using the Guided Endodontics Technique. J Endod. 2018;44(10):1578–82. doi: 10.1016/j.joen.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 10.Ball RL, Barbizam JV, Cohenca N. Intraoperative endodontic applications of cone-beam computed tomography. J Endod. 2013;39(4):548–57. doi: 10.1016/j.joen.2012.11.038. [DOI] [PubMed] [Google Scholar]
- 11.Floratos S, Miltiadous ME. Intraoperative Use of CBCT for Identification and Localization of Calcified Canals: A Clinical Technique. Case Rep Dent. 2017;2017:1265701. doi: 10.1155/2017/1265701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCabe PS. Avoiding perforations in endodontics. J Ir Dent Assoc. 2006;52(3):139–48. [PubMed] [Google Scholar]
- 13.Shi X, Zhao S, Wang W, Jiang Q, Yang X. Novel navigation technique for the endodontic treatment of a molar with pulp canal calcification and apical pathology. Aust Endod J. 2018;44(1):66–70. doi: 10.1111/aej.12207. [DOI] [PubMed] [Google Scholar]
- 14.de Cunha F, de Souza IM, Monnerat J. Pulp canal obliteration subsequent to trauma: perforation management with MTA followed by canal localization and obturation. Braz J Dent Traumatol. 2009;1(2):64–8. [Google Scholar]
- 15.Johnson BR. Endodontic access. Gen Dent. 2009;57(6):570–7; quiz 8-9, 95, 679. [PubMed] [Google Scholar]
- 16.O'Connor RP, De Mayo TJ, Roahen JO. The lateral radiograph: an aid to labiolingual position during treatment of calcified anterior teeth. J Endod. 1994;20(4):183–4. doi: 10.1016/s0099-2399(06)80332-8. [DOI] [PubMed] [Google Scholar]
- 17.Falcon PA, Falcon CY, Abbasi F, Hirschberg CS. Chamberless Endodontic Access for Treatment of Calcified Anterior Central Incisors. J Endod. 2021;47(2):322–6. doi: 10.1016/j.joen.2020.10.017. [DOI] [PubMed] [Google Scholar]
- 18.van der Meer WJ, Vissink A, Ng YL, Gulabivala K. 3D Computer aided treatment planning in endodontics. J Dent. 2016;45:67–72. doi: 10.1016/j.jdent.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Patel S, Brown J, Semper M, Abella F, Mannocci F. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. Int Endod J. 2019;52(12):1675–8. doi: 10.1111/iej.13187. [DOI] [PubMed] [Google Scholar]
- 20.Llaquet Pujol M, Vidal C, Mercad M, Muoz M, Ortolani-Seltenerich S. Guided Endodontics for Managing Severely Calcified Canals. J Endod. 2021;47(2):315–21. doi: 10.1016/j.joen.2020.11.026. [DOI] [PubMed] [Google Scholar]
- 21.Patel S, Brown J, Pimentel T, Kelly RD, Abella F, Durack C. Cone beam computed tomography in Endodontics - a review of the literature. Int Endod J. 2019;52(8):1138–52. doi: 10.1111/iej.13115. [DOI] [PubMed] [Google Scholar]
- 22.Davies A, Mannocci F, Mitchell P, Andiappan M, Patel S. The detection of periapical pathoses in root filled teeth using single and parallax periapical radiographs versus cone beam computed tomography - a clinical study. Int Endod J. 2015;48(6):582–92. doi: 10.1111/iej.12352. [DOI] [PubMed] [Google Scholar]
- 23.Maia LM, de Carvalho Machado V, da Silva N, Brito Jnior M, da Silveira RR, Moreira Jnior G, Ribeiro Sobrinho AP. Case Reports in Maxillary Posterior Teeth by Guided Endodontic Access. J Endod. 2019;45(2):214–8. doi: 10.1016/j.joen.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 24.Buchgreitz J, Buchgreitz M, Bjrndal L. Guided Endodontics Modified for Treating Molars by Using an Intracoronal Guide Technique. J Endod. 2019;45(6):818–23. doi: 10.1016/j.joen.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 25.Tavares WLF, de Carvalho Machado V, Fonseca FO, Vasconcellos BC, Magalhes LC, Viana ACD, Henriques LCF. Guided endodontics in complex scenarios of calcified molars. Iran Endod J. 2020;15(1):50–6. doi: 10.22037/iej.v15i1.26709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moreira ML, Toubes KM, Jnior GM, Tonelli SQ, Carvalho MVd, Silveira FF, Nunes E. Guided endodontics in nonsurgical retreatment of a mandibular first molar: a new approach and case report. Iran Endod J. 2020 doi: 10.22037/iej.v15i2.27183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freire BB, Vianna S, Nascimento EHL, Freire M, Chilvarquer I. Guided Endodontic Access in a Calcified Central Incisor: A Conservative Alternative for Endodontic Therapy. Iran Endod J. 2021;16(1):56–9. doi: 10.22037/iej.v16i1.27427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fonseca Tavares WL, Diniz Viana AC, de Carvalho Machado V, Feitosa Henriques LC, Ribeiro Sobrinho AP. Guided Endodontic Access of Calcified Anterior Teeth. J Endod. 2018;44(7):1195–9. doi: 10.1016/j.joen.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 29.Kishen A, Kumar GV, Chen NN. Stress-strain response in human dentine: rethinking fracture predilection in postcore restored teeth. Dent Traumatol. 2004;20(2):90–100. doi: 10.1111/j.1600-4469.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- 30.Leoni GB, Versiani MA, Pcora JD, Damio de Sousa-Neto M. Micro-computed tomographic analysis of the root canal morphology of mandibular incisors. J Endod. 2014;40(5):710–6. doi: 10.1016/j.joen.2013.09.003. [DOI] [PubMed] [Google Scholar]