Abstract
External cervical resorption is a type of pathological root resorption that is often asymptomatic. It leads to progressive loss of dental hard tissues while the pulp usually remains vital. The first symptom reported by a patient may be a pink shadow at an esthetic zone. This case report describes the treatment of external cervical resorption of a first upper incisor according to the new classification, treatment and management methods introduced in 2018. After 30 months the endodontic treatment was performed due to pulp necrosis and symptomatic apical periodontitis.
Key Words: Central Maxillary Incisor, Cone-Beam Computed Tomography, External Cervical Resorption, Tooth Resorption
Introduction
External cervical resorption (ECR) is a type of pathological root resorption that initially develops in the cervical aspect of the tooth. It affects the connective tissue attachment region below the epithelial attachment and above the alveolar bone [1, 2]. Damage to the periodontal ligament and cementum initiate the resorption process. It leads to dentine exposure in cervical area of the tooth, making it sensitive to osteoclast activity [3, 4]. Orthodontic treatment and traumatic injury are considered the main predisposing factors for ECR. Additional risk factors such as internal bleaching of tooth, periodontal or surgical treatment and bruxism have also been reported in the literature. In some cases, the cause of resorption is unknown and the process is then called idiopathic invasive cervical resorption [5-7]. Generally, ECR does not reach the pulp because the predentin is resistant to resorption process [8]. Patel et al. [9] introduced a new classification for the ECR based on a cone beam computed tomography (CBCT) image. Three features of the ECR were assessed: height of the ECR, circumferential spread and the proximity to the root canal (Table 1). In the same year, the European Society of Endodontology proposed a treatment and management methods of ECR using classification of Patel et al. [10]. The proposed treatment methods include [9, 10]:
Table 1.
A three-dimensional classification for ECR according to Patel et al. [9]
| Height | Circumferential spread | Proximity to the root canal |
|---|---|---|
| 1. At cemento-enamel junction level (supracrestal ) | A⩽90° | d Lesion confined to dentine |
| 2. Extends into coronal third of root (subcrestal) | B>90°⩽180° | |
| 3. Extends into mid-third of the root | C>180°⩽270° | p Probable pulpal involvement |
| 4. Extends into apical-third of the root | D>270° |
1. Removal of resorptive tissue and restoration of the defect with a direct restoration-1Ad, 2Ad, 2Bd and endodontic treatment in case of probable pulp involvement-1Ap, 2Ap, 2Bp.
2. Removal of resorptive tissue from the root canal access during endodontic treatment-2Cp, 2Dp, 3Cp, 3Dp.
3. Extraction of an endodontically treated tooth to allow restoration and/or recontouring of an otherwise inaccessible resorption defect, followed by replantation-3Ad, 3Bd.
4. Periodic reviewed of untreatable teeth-2-4Dd, 2-4Dp.
5. Extraction of untreatable teeth.
This case report describes the treatment of external cervical resorption in accordance with the latest European Society of Endodontology guidelines.
Case Report
In April 2018, a 56-year-old male patient was referred to the Department of Conservate Dentistry and Endodontics, University Dental Clinic In Szczecin, Poland by a general dental practitioner for treatment of tooth 21 (first left upper incisor) due to suspected external cervical resorption. The non-smoking, healthy patient, without known allergies, did not report any toothache. During anamnesis the patient denied trauma, orthodontic treatment and bleaching of teeth. Clinical examination revealed a characteristic sign of ECR - a pink shadow in the cervical aspect of the tooth 21 with loss of hard tissue (Figure 1A). The sensitivity tests including thermal and electric pulp tests (Vitality Scanner 2006, KerrHawe, Bioggio, Switzerland) were positive and the percussion test was negative. During periodontal examination (WHO-62 periodontal probe) probing depth was approximately 5 mm on labial side. Tooth was not mobile, and no caries or previous filling was present. The hygiene was optimal (Approximal Plaque Index-API Indexindex 20%) and significant wear of the incisal edges of the upper incisors and canines was observed [11].
Figure 1.
A) Preoperative intraoral photograph shows a pink shadow in the cervical aspect of the tooth 21 with loss of hard tissue; B) Preoperative CBCT frontal, sagittal and axial views of maxillary first left incisor shows external cervical resorption
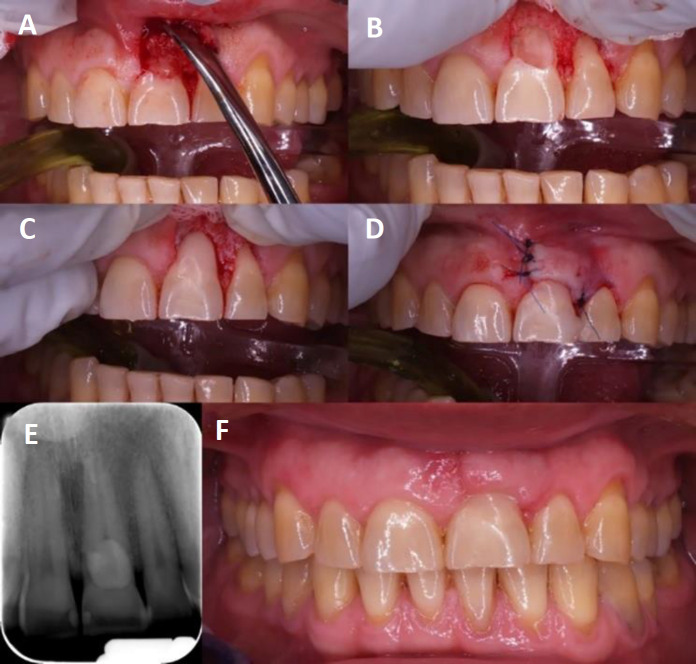
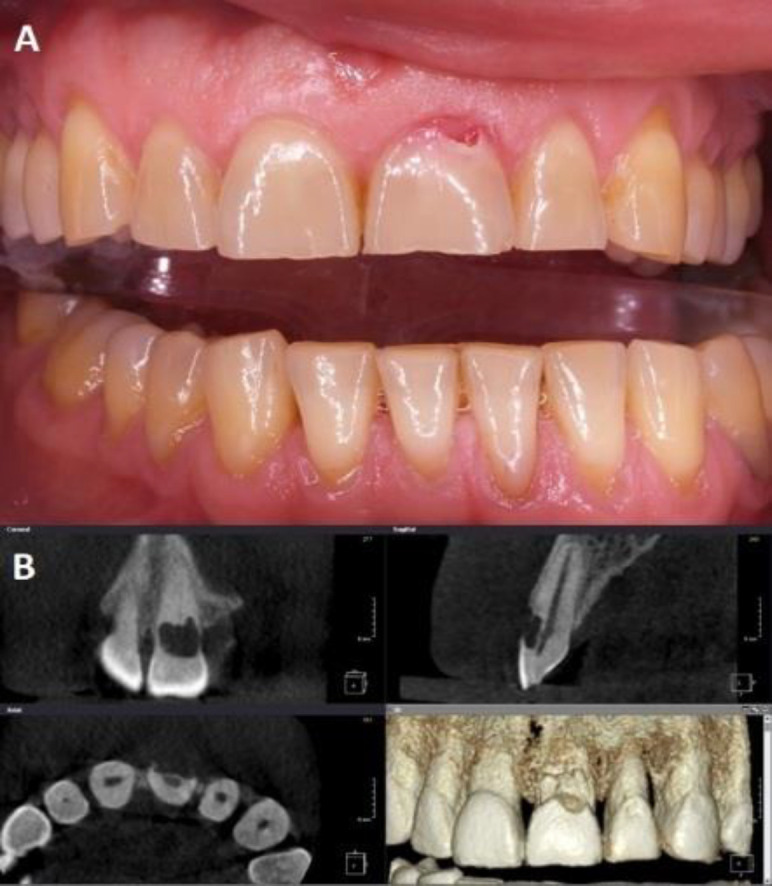
A CBCT (Cranex 3Dx, Soredex, KaVo Imaging, PA, USA) with a small field of view (FOV) 40×40 mm and voxel size 0.125 mm was performed to assess an extent of the resorption (Figure 1A). Class 2Bd external cervical resorption according to Patel et al. [8] was diagnosed. The patient was offered a treatment plan consistent with the European Society of Endodontology recommendations for class 2Bd external resorption, which included reflecting a flap, removal of the resorptive tissue and then direct filling of the defect [9]. Due to the normal condition of the pulp (confirmed by the cold sensitivity test) and normal periapical tissues, as well as the lack of direct contact between the resorptive defect and the pulp cavity, no indications for endodontic treatment of the tooth 21 were found. After explaining the procedure to the patient, written informed consent was obtained from the patient. Under local anesthesia of 2% lidocaine with epinephrine (Xylodont 1:50000, Molteni Stomat, Kraków, Poland) intrasulcular incision from tooth 21 to 22 with vertical release was performed to expose the resorption cavity (Figure 2A). In the next step, the resorptive tissue was removed using an excavator (Figure 2B). The cavity was filled using Single Bond Universal adhesive (3M ESPE, MN, USA) and Estelite Sigma Quick A3 (Tokuyama, Tokyo, Japan) (Figure 2C). Finally, the flap was repositioned and sutured with 4.0 monofilament suture (Figure 2D) and postoperative RVG image was taken (Figure 2E). The sutures were removed seven days after the surgery-normal tissue healing was found (Figure 2F). After 30 days, during next control visit, no abnormalities were found. Unfortunately, the patient did not attend a follow-up appointment 6 months after the procedure. In November 2020 the patient presented to the Department of Conservate Dentistry and Endodontics, University Dental Clinic because of pain in the area of the upper left front teeth experienced when biting down. Clinical examination of tooth 21 revealed negative pulp response to sensitivity tests, 7 mm probing depth at the labial surface, no gingival inflammation or pathological mobility. The esthetic effect was satisfactory (Figure 3A). A CBCT with FOV 40×40 mm and voxel size 0.125 mm revealed 2 mm vertical defect of the alveolar bone from the labial side under a composite filling and periapical radiolucency (Figure 3B). Based on the symptoms a diagnosis of pulp necrosis with symptomatic apical periodontitis was made. Written informed consent was obtained and rubber dam was placed, and endodontic treatment was performed. Working length was established to 24 mm, cleaning and shaping of root canal was performed using MTwo (VDW, Munich, Germany) rotary file system to size 40/0.04. Passive ultrasonic irrigation with 5.25% NaOCl and 15% EDTA was performed. Root canal was temporary filled with non-setting calcium hydroxide and the access cavity was then sealed with glass-ionomer cement Riva Self Cure (SDI, Victoria, Australia) for one week. At second visit the canal was obturated using lateral condensation of gutta-percha and AH Plus (Dentsply Sirona, NC, USA) sealer. The tooth was reconstructed using Glassix (Nordin, Chailly, Switzerland) fiberglass and NexCore cement (Meta Biomed, Chungcheongbuk, Republic of Korea). The access cavity was restored with adhesive Single Bond Universal and resin composite Estelite Sigma Quick A3. The postoperative radiographic image was taken (Figure 3C).
Figure 2.
Steps of treatment performed: A) External cervical resorption defect after flap reflection; B) Cavity after resorption tissue removal; C) Resorption cavity restored with adhesive and resin composite; D) Intraoral photograph after flap reposition and suture; E) Postoperative radiograph; F) Intraoral photograph after seven days
Figure 3.
Status after 30 months: A) Intraoral photography showing good esthetic effect, B) CBCT frontal, sagittal and axial views of treated tooth show periapical lesion and defect of bone; C) Radiograph after endodontic treatment and fiber post cementation
Discussion
In 1999 Heithersay [2] has proposed a clinical classification of ECR according to its size and proximity to the root canal. The classification was based on conventional radiographs: Class 1-Denotes a small invasive resorptive lesion near the cervical area with shallow penetration into dentine; Class 2–Denotes a well-defined invasive resorptive lesion that has penetrated close to the coronal pulp chamber but shows little or no extension into the radicular dentine; Class 3–Denotes a deeper invasion of dentine by resorbing tissue, not only involving the coronal dentine but also extending into the coronal third of the root; Class 4–Denotes a large invasive resorptive process that has extended beyond the coronal third of the root [2]. Heithersay [2] in the article described radiologic, clinical, and histopathologic features of ECR [2]. In the European Society of Endodontology position statement and in the joint statement of the American Association of Endodontists & American Academy of Oral & Maxillofacial Radiology the use of CBCT to assess and manage root resorption has been recommended [12, 13]. In 2018 Patel et al. [10] created new classification for ECR based on the CBCT which was used in this study. This new classification was accepted by European Society of Endodontology and on its basis, treatment options were presented [10].
In the case presented, patient did not report any predisposing factors that could be related with ECR, but the significant tooth wear is worth noting. Parafunctional habits (e.g., bruxism, nail biting, etc.) causes 2.4% to 23.2% of the ECR [6, 13, 14]. Interestingly, bruxism can be a sole cause of ECR [6]. The teeth most commonly affected by ECR are maxillary anterior teeth-maxillary incisors: 27% to 29 % and maxillary canines: 14% to 21% [5, 15].
Espona et al. [16] conducted a treatment of ECR in lateral maxillary incisor. They used a nanohybrid composite resin with 2-bottle self-etching adhesive to fill the resorption defect. At the 7-year follow-up, tooth remained asymptomatic with a normal response to cold testing [16]. According to Elias et al. [17] universal adhesive systems are not more toxic than self-etching adhesives [17]. In the presented case universal adhesive system (Single Bond Universal) and nanofilled composite Estelite Sigma Quick were used to fill the resorption cavity. After 30 months, a pulp necrosis was diagnosed, probably caused by the universal adhesive system, which have cytotoxic and genotoxic effect on viable cells [18, 19]. The procedure presented by Kqiku et al. [20] seems to be safer for the pulp. The researchers used white MTA (Pro Root, Dentsply, Konstanz, Germany), glass ionomer cement (Fuji IX, Fuji, Tokyo, Japan) and light-cured composite (bonding: Excite; composite: Artemis Enamel A2, both by Vivadent, Schaan, Liechtenstein) to fill the resorption cavity. After a four-year follow-up, the pulp responded positively to sensibility tests [20]. Other materials, that are used successfully to fill the cavity in the treatment of external cervical resorption include Biodentine [21] or glass ionomer cement [22]."
Conclusion
External cervical resorption lesions that can be treated conservatively have a good prognosis. However, patients should be informed of the limited evidence of treatment, possibility of late complications and the need for control visits.
Conflict of Interest:
‘None declared’.
References
- 1.Tronstad L. Root resorption--etiology, terminology and clinical manifestations. Endod Dent Traumatol. 1988;4(6):241–52. doi: 10.1111/j.1600-9657.1988.tb00642.x. [DOI] [PubMed] [Google Scholar]
- 2.Heithersay GS. Clinical, radiologic, and histopathologic features of invasive cervical resorption. Quintessence Int. 1999;30(1):27–37. [PubMed] [Google Scholar]
- 3.Neuvald L, Consolaro A. Cementoenamel junction: microscopic analysis and external cervical resorption. J Endod. 2000;26(9):503–8. doi: 10.1097/00004770-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Patel S, Mavridou AM, Lambrechts P, Saberi N. External cervical resorption-part 1: histopathology, distribution and presentation. Int Endod J. 2018;51(11):1205–23. doi: 10.1111/iej.12942. [DOI] [PubMed] [Google Scholar]
- 5.Mavridou AM, Bergmans L, Barendregt D, Lambrechts P. Descriptive Analysis of Factors Associated with External Cervical Resorption. J Endod. 2017;43(10):1602–10. doi: 10.1016/j.joen.2017.05.026. [DOI] [PubMed] [Google Scholar]
- 6.Heithersay GS. Invasive cervical resorption: an analysis of potential predisposing factors. Quintessence Int. 1999;30(2):83–95. [PubMed] [Google Scholar]
- 7.Patel S, Kanagasingam S, Pitt Ford T. External cervical resorption: a review. J Endod. 2009;35(5):616–25. doi: 10.1016/j.joen.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Patel J, Beddis HP. How to assess and manage external cervical resorption. Br Dent J. 2019;227(8):695–701. doi: 10.1038/s41415-019-0781-x. [DOI] [PubMed] [Google Scholar]
- 9.Patel S, Foschi F, Mannocci F, Patel K. External cervical resorption: a three-dimensional classification. Int Endod J. 2018;51(2):206–14. doi: 10.1111/iej.12824. [DOI] [PubMed] [Google Scholar]
- 10.Patel S, Lambrechts P, Shemesh H, Mavridou A. European Society of Endodontology position statement: External Cervical Resorption. Int Endod J. 2018;51(12):1323–6. doi: 10.1111/iej.13008. [DOI] [PubMed] [Google Scholar]
- 11.Lange DE, Plagmann HC, Eenboom A, Promesberger A. [Clinical methods for the objective evaluation of oral hygiene] Dtsch Zahnarztl Z. 1977;32(1):44–7. [PubMed] [Google Scholar]
- 12.Patel S, Durack C, Abella F, Roig M, Shemesh H, Lambrechts P, Lemberg K. European Society of Endodontology position statement: the use of CBCT in endodontics. Int Endod J. 2014;47(6):502–4. doi: 10.1111/iej.12267. [DOI] [PubMed] [Google Scholar]
- 13.AAE and AAOMR Joint Position Statement. Use of Cone Beam Computed Tomography in Endodontics 2015 Update. J Endod. 2015;41(9):1393–6. doi: 10.1016/j.joen.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 14.Irinakis E, Aleksejuniene J, Shen Y, Haapasalo M. External Cervical Resorption: A Retrospective Case-Control Study. J Endod. 2020;46(10):1420–7. doi: 10.1016/j.joen.2020.05.021. [DOI] [PubMed] [Google Scholar]
- 15.Jeng PY, Lin LD, Chang SH, Lee YL, Wang CY, Jeng JH, Tsai YL. Invasive Cervical Resorption-Distribution, Potential Predisposing Factors, and Clinical Characteristics. J Endod. 2020;46(4):475–82. doi: 10.1016/j.joen.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 16.Espona J, Roig E, Durán-Sindreu F, Abella F, Machado M, Roig M. Invasive Cervical Resorption: Clinical Management in the Anterior Zone. J Endod. 2018;44(11):1749–54. doi: 10.1016/j.joen.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 17.Elias ST, Santos AF, Garcia FC, Pereira PN, Hilgert LA, Fonseca-Bazzo YM, Guerra EN, Ribeiro AP. Cytotoxicity of universal, self-etching and etch-and-rinse adhesive systems according to the polymerization time. Braz Dent J. 2015;26(2):160–8. doi: 10.1590/0103-6440201300294. [DOI] [PubMed] [Google Scholar]
- 18.Sürmelioğlu D, Hepokur C, Yavuz SA, Aydın U. Evaluation of the cytotoxic and genotoxic effects of different universal adhesive systems. J Conserv Dent. 2020;23(4):384–9. doi: 10.4103/JCD.JCD_376_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leite M, Costa CAS, Duarte RM, Andrade AKM, Soares DG. Bond Strength and Cytotoxicity of a Universal Adhesive According to the Hybridization Strategies to Dentin. Braz Dent J. 2018;29(1):68–75. doi: 10.1590/0103-6440201801698. [DOI] [PubMed] [Google Scholar]
- 20.Kqiku L, Ebeleseder KA, Glockner K. Treatment of invasive cervical resorption with sandwich technique using mineral trioxide aggregate: a case report. Oper Dent. 2012;37(1):98–106. doi: 10.2341/11-143-S. [DOI] [PubMed] [Google Scholar]
- 21.Eftekhar L, Ashraf H, Jabbari S. Management of Invasive Cervical Root Resorption in a Mandibular Canine Using Biodentine as a Restorative Material: A Case Report. Iran Endod J. 2017;12(3):386–9. doi: 10.22037/iej.v12i3.16668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bachesk AB, Queiroz AF, Bin LR, Bachesk AB, Pavan AJ. Clinical Approach to External Cervical Resorption in the Anterior Teeth: A Case Report Study. Iran Endod J. 16(2):118–22. doi: 10.22037/iej.v16i2.32373. [DOI] [PMC free article] [PubMed] [Google Scholar]