Abstract
Introduction:
This study aimed to determine the success rate of the combination of buccal infiltration (BI) and inferior alveolar nerve block (IANB) injections in irreversible pulpitis in mandibular molars after premedication with ibuprofen.
Materials and Methods:
From 132 patients participated in the study, 120 patients were included. One hour before root canal treatment, patients with mandibular molars with symptomatic irreversible pulpitis received either a 600 mg ibuprofen capsule or a placebo. All patients received 2% lidocaine with 1:80000 epinephrine and 4% articaine with 1:100000 epinephrine for IANB and BI, respectively. Patients’ pain was evaluated using the Heft-Parker visual analog scale during the preparation of access cavity, exposure of pulp, and instrumentation of root canal. The success of anesthesia was defined as the absence of pain or mild pain. The Chi-square and t-test were employed for data analysis.
Results:
The difference between patient age and gender in the two groups was not significant (P>0.05). The anesthesia success rate was 85% in the premedicated and 70% in the placebo group, with statistically significant results (P=0.049).
Conclusion:
Based on this triple-blinded randomized clinical study, mandibular molars with irreversible pulpitis were not thoroughly anesthetized by a combination of IANB+BI after premedication with ibuprofen (600 mg), even though anesthesia success was improved significantly by ibuprofen premedication.
Key Words: Anesthesia, Buccal Infiltration, Inferior Alveolar Nerve Block, Ibuprofen, Placebo, Premedication
Introduction
Since patient comfort is of great importance to all patients and dental practitioners, numerous investigations have focused on improving anesthesia success rates during and after endodontic treatment [1-5]. Mandibular posterior teeth are commonly known to be extremely challenging to anesthetize, especially if they have irreversible pulpitis [6-9].
Systematic reviews and meta-analyses have reported that mandibular posterior tooth anesthesia is improved significantly by employing inferior alveolar nerve block (IANB) with lidocaine and 1:100000 epinephrine in combination with a 4% articaine and 1:100000 epinephrine buccal injection [10-12].
In addition to using different techniques and anesthetic solutions to improve anesthetic success, premedication with nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen has also been extensively evaluated [13-16] .
Administering local anesthesia after the use of an NSAID has been reported to have no significant effect on anesthetic success by some studies [14, 17-19], while others have shown significantly higher success rates for IAN blocks following premedication [13, 20-24]. Premedication with NSAIDs has been found to increase the efficacy of IANB in a systematic review and meta-analysis on 19 articles [25]. Also, a recent systematic review examined 35 studies on how IANB success in treatment of irreversible pulpitis is affected by premedication. This study expressed the need for further supporting research to clarify the finding that some medications are relatively effective in this regard [15].
Premedication with ibuprofen has been more widely studied than premedication with other NSAIDs. Recently, Karapinar-Kazandag et al. [15] have found a preference for this drug, administered alone or compared with other drugs, in their systematic review.
Despite the greater attention ibuprofen has received, the effect on IANB block has been studied in other NSAIDs as well. Ketorolac is one of these drugs [15]. Two earlier investigations have pointed to meaningful improvement in anesthesia success rates of oral or parenteral ketorolac premedication in mandibular teeth with irreversible pulpitis in combination with anesthesia by IANB and articaine lingual and buccal infiltrations [13, 24]. However, several studies have found no meaningful difference between ketorolac and placebo [14, 26, 27].
The anesthetic technique used in previous investigations on NSAID premedication was mostly IANB [20, 28].
Therefore, the present study assessed the anesthetic efficacy of IANB with 2% lidocaine and 1:80000 epinephrine accompanied by a buccal injection of 4% articaine with 1: 100000 epinephrine in mandibular molars with irreversible pulpitis with and without premedication with 600 mg ibuprofen.
Materials and Methods
This study was approved by the Ethics Committee of Kerman University of Medical Sciences in Iran (IR.KMU.REC.1395.13) and registered in the Iranian Registry of Clinical Trials (ID No. IRCT201611242016N7). The inclusion and exclusion criteria in this study are as follows:
Inclusion criteria: Patients in need of root canal treatment for mandibular molars with symptomatic irreversible pulpitis (history of spontaneous pain or lingering pain) due to caries, aged 18 years or more, with no contraindications to taking either ibuprofen (no record of an allergic reaction to aspirin, NSAIDs, lidocaine, or articaine with epinephrine and those with nasal polyp, or a history of peptic ulcers, gastrointestinal (GI) bleeding, pregnancy, lactation, or renal or hepatic disease), with no history of GI disorders or ulcer and no severe systemic illness.
Exclusion criteria: Patients with physical status according to The American Society of Anesthesiologists (ASA) ≥ 2, presence of periodontal ligament widening or radiolucency, no response to pulp sensibility tests, tenderness to percussion, or palpation, use of medications and analgesics within 24 h before the treatment, teeth with full crowns, and teeth that could not be retained due to restorative or periodontal reasons.
To confirm the diagnosis of irreversible pulpitis, in addition to having a history of spontaneous pain, the mandibular molars were tested with a cold pulp test (Cool Spray, Aeronova GmbH & CO., Dresden, Germany). Irreversible pulpitis was confirmed by a prolonged response to the cold test.
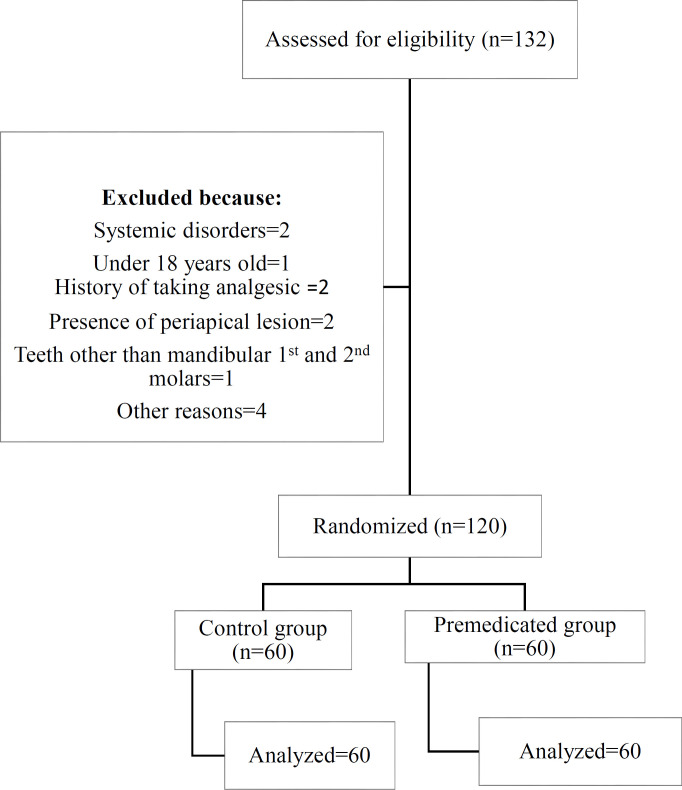
The sample size was calculated using data from a previous study [29]. It was calculated that a sample size of 50 patients in each group is required to detect a difference of 25% in the success rate of anesthesia between the two groups with a power of 80% and ɑ= 0.05. Considering a 20% dropout rate, 60 patients were the minimum sample size for each group. Of the total of 132 patients enrolled initially, 120 individuals were included in this prospective, randomized triple-blinded study (Figure 1). The patients were treated in Kerman Dental School Endodontic Department postgraduate clinic in Iran from September 2016 to April 2017. After a complete description of the nature of the study, the risks, and the possibility of discomfort, an informed consent was obtained from the each patient who agreed to participate in the study. Although the patients reported no spontaneous pain at the time of treatment, their response to the cold test was assessed using the Heft-Parker visual analog scale (VAS). Each patient received either a placebo or 600 mg of ibuprofen, provided in capsules of the same color and size. These were taken orally by the patients 1 h before commencing the access cavity preparation. The tablets were placed in two separate jars with different codes of 1 and 2. Only the pharmacist (AP) knew the content of the capsules with each code. Therefore, the capsules’ contents were known by neither the practitioner nor the patients. The patients were randomly assigned to two groups including 60 patients each, through the use of random digits. After deciding which number belonged to each capsule code, each number was written on opaque white paper. All pieces of paper were then folded and placed in a jar and were randomly selected by patients at the start of the treatment visit. The appropriate capsule was given to the patient based on the number.
Figure 1.
Consort flowchart
A topical anesthetic (20% Benzocaine; Premier, Philadelphia, PA, USA) was applied to the IANB injection site one h after the capsule was taken. One min later, the injection was administered using a side-loading cartridge syringe (Dena Instruments, Forgeman Instruments Co., Sialkot, Pakistan). The syringe was fitted with a 27-gauge 38-mm needle (Nik Rahnama Kar Co., Tehran, Iran). Based on the standard IANB method, to ensure negative blood aspiration, following needle insertion and bone contact, the needle was withdrawn 1–2 mm and aspiration was performed. For all patients, 1.8 mL of 2% lidocaine with 1:80000 epinephrine (Darupakhsh, Tehran, Iran) was used for the IANB. The patients were asked about numbness of their lip 5 min post-injection. Failure of the IANB was confirmed if the patient did not report numbness in the lip, and these patients were removed from the study. In case of positive response, after application of topical gel to the molar tooth’s buccal vestibule, 1.8 mL of 4% articaine with 1:100000 epinephrine (Artinibsa, Inibsa, Barcelona, Spain) was injected as a BI injection. Access cavity preparation for endodontic treatment started after tooth isolation with a rubber dam 15 min after the IANB injection[29, 30].
The patients used a VAS to rate their pain before the treatment, after the cold test before taking the premedication capsule, 1 h after taking the pill and following the second cold test, 15 min following IANB injection, during dentin cutting, after pulp exposure, and during root canal instrumentation. The pain ratings of no pain, mild pain, moderate pain, and severe pain were defined as 0 mm, between 0 mm and 54 mm, between 54 mm and 114 mm, and above114 mm, respectively [29]. If the patients felt pain (more than 54 mm), it was assumed as the failure of anesthesia [29, 30].
The supplementary anesthetic techniques of intra-pulpal and intra-ligamental injections were used in case of anesthesia failure. The patients were followed up for one week to ensure the absence of adverse effects.
The student t and chi-square tests were utilized to analyze data. P<0.05 was considered significant. As the statistician was unaware of the groups’ premedication status, the study was a triple-blinded clinical trial.
Results
From the total of 132 patients initially enrolled, twelve patients were excluded due to being younger than 18 years (1 patient), third molar teeth (1 patient), a history of taking analgesics in the past 24 h (2 patients), detection of periapical radiolucency (2 patients), systemic disease (2 patients), and other reasons (4 patients). Overall, a total of 120 patients were included in this study.
Up to one week following the treatment visit, no adverse events attributed to the anesthetic solutions or premedication with ibuprofen were reported. The difference between the groups was not significant in patients’ response to the cold test before taking either medication or placebo (P=0.86).
Table 1 presents the mean age of the patients and their gender. The two groups showed no significant difference in age and gender (P=0.14, P=1.00, respectively). There was no significant difference between the reported baseline pain levels before taking the premedication capsules (P=0.37).
Table 1.
Baseline information regarding the two study groups (n=60)
| Characteristic | Placebo | Premedication | P -value |
|---|---|---|---|
| Age | 29.3 (±7.68) | 31.56 (±9.18) | 0.14 |
| Gender | |||
| Male | 24(40%) | 24 (40%) | 1.00 |
| Female | 36(60%) | 36(60%) | |
| Mandibular Molars | |||
| First | 29 | 27 | 0.71 |
| Second | 31 | 33 | |
The difference between the overall anesthesia success rates in the placebo and ibuprofen groups was statistically significant (70% and 85%, respectively) (P=0.049) (Table 2).
Table 2.
Percent success rate at various stages during access cavity preparation and root canal instrumentation.
|
Stage of
treatment Significance |
Cold test
(n) |
15 min
(n) % |
Dentin cutting
(n) % |
Pulp exposure
(n)% |
Instrumentation
(n) |
Final Success
(n) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PM* | PL** | PM | PL | PM | PL | PM | PL | PM | PL | PM | PL | |||
| <54 | >54 | <54 | >54 | 100 (60) | 100 (60) | 90.00 (54) |
91.66 (55) |
85.00 (51) | 75.00 (45) |
85.00 (51) |
70.00 (42) |
85 (51) |
70.00 (42) | |
| 5 | 55 | 8 | 52 | |||||||||||
| P -value | 0.86 | 1.00 | 0.752 | 0.031 | 0.029 | 0.049 | ||||||||
PM: Premedicated group; PL: Placebo group
None of the patients in either group had sensitivity to the cold test 15 min following IANB injection. There was no significant difference between the number of first and second mandibular molars in the groups (P=0.71).
In a placebo group, a significantly higher number of failures to achieve adequate anesthesia were recorded in the pulp exposure stage of treatment (P=0.031) (Table 2).
Discussion
In this research, ibuprofen premedication significantly impacted the anesthesia success rate for mandibular molars with irreversible pulpitis when an IANB was administered using 2% lidocaine with 1:80000 epinephrine plus a buccal infiltration injection with 4% articaine and 1:100000 epinephrine.
It has been claimed that asymptomatic irreversible pulpitis may have higher anesthesia success rate when a NSAID prescribed prior to the endodontic treatment because the medication may prevent formation of TTx-resistance sodium channels. However, in the symptomatic irreversible pulpitis the TTx-resistance sodium channels have already been formed and for that reason prescribing a NSAID has no significant impact on improving anesthesia success rate [31]. However, in this study, despite including teeth with symptomatic irreversible pulpitis, premedication with ibuprofen could significantly improve anesthesia success rate. Several variables may have the potential to influence the success rates of IANB. These include the anesthetic solution volume, the administered anesthetic drug, the state of the pulp, and taking an NSAID before administering the anesthetic [7, 16, 21, 24, 32-36].
Despite some arguments regarding the efficacy of premedication with an NSAID, results of two systematic reviews and meta-analyses revealed that premedication with an NSAID had a significant impact on anesthesia success for mandibular posterior teeth [20, 25, 37, 38].
The present study results also showed that when lidocaine was used for IANB plus a buccal injection of articaine, premedication with 600 mg ibuprofen significantly improved anesthesia success in mandibular molars with irreversible pulpitis.
In a recent systematic review and meta-analysis, the infiltration technique, both as a primary and supplementary injection given after primary IANB failure, has been found to increase the overall anesthesia efficacy [6]. Also, the results of another systematic review and meta-analysis by Corbella et al. [25] showed that administration of a supplementary buccal injection was marginally significant in improving the success rate of IANB. However, four other systematic reviews and meta-analyses have reported the significantly higher efficacy of using articaine as a supplementary buccal injection [10-12, 39].
The rationale of using an NSAID as a premedication is to decrease the level of inflammatory mediators and therefore increase anesthesia success [7, 15]. Two investigations conducted by Yadav et al. [24] and Akhlaghi et al. [13] reported that ketorolac premedication combined with buccal or lingual articaine infiltrations, respectively, yielded significantly higher success rates. However, the present study results showed a significant difference when ibuprofen was used for premedication (P<0.05). Ibuprofen is known to be a safer medication compared to ketorolac [40].
Therefore, it would be more reasonable to prescribe it as an NSAID for premedication to improve anesthesia success. It should be mentioned that not all NSAIDs will have the same effect on anesthesia success; for instance, ketorolac was significantly more effective in improving anesthesia success compared to diclofenac potassium when used as a premedication for teeth with irreversible pulpitis [22, 41].
There are some concerns regarding the possible adverse effects of articaine versus lidocaine when used as anesthetic agents in dentistry [42, 43]. However, no significant difference in adverse effects has been reported between the two anesthetics in two systematic reviews and meta-analyses [12, 39]. None of the patients reported adverse effects from the anesthetic agent or technique up to one week after the treatment in the present study.
It has been reported that the gender of patients may have a significant impact on the anesthetic efficacy of articaine infiltration injections for first mandibular molars [30]. However, the present research found no significant difference between the numbers of female patients in the two groups.
In previous studies, the use of the anesthetic solution for buccal infiltration in combination with IANB for anesthetizing mandibular molars has been performed either immediately following the IANB injection [13, 44] or as supplemental anesthesia in case adequate anesthesia was not achieved by the IANB [45-48]. Traditionally, lip numbness has been considered an indicator of a successful IANB injection. However, injecting an anesthetic solution as a buccal infiltration immediately following the IANB may make it difficult for the operator to confirm the success of the first injection, i.e., the IANB. A method to overcome this shortcoming is to wait for 5 min between the two injections to ensure the success of the IANB by asking the patients regarding their lip numbness and providing the second injection, i.e., the BI, after that [49]. In the present study, this method was used. Those patients who did not report numbness of the lip 5 min post- IANB were excluded from the study.
Various doses of ibuprofen have been used as premedication, ranging between 300 to 800 mg [14, 16, 17, 19, 21, 23, 50]. A systematic review and meta-analysis reported that 600–800 mg ibuprofen dosage significantly impacted IANB [51]. Therefore, 600 mg ibuprofen was used in the present study. The anesthesia success rate in mandibular molar with irreversible pulpitis has been found to be in the range of 14.8–88% [44, 52]. The ketorolac premedicated group in the studies reported by Akhlaghi et al. [13] and Yadav et al. [24] showed an 85% lower anesthesia rate of success than the premedication group in our study. The difference in anesthetic solutions used for the IANB and the inclusion criteria may be reasons for this difference.
As discussed above, current methods of local anesthesia lead to much anesthesia failure in mandibular posterior teeth with irreversible pulpitis. The significant effect of the tooth type was reported by a study with a large sample size using articaine as a supplementary buccal injection in mandibular posterior teeth [46]. Therefore, to avoid bias, only the first and second mandibular molar were included in the present study.
In summary, the present study results indicate that 100% anesthesia could not be achieved by premedication with ibuprofen and using a combination of IANB+buccal infiltration injections with 4% articaine and 1: 100000 epinephrine. However, premedication before these injections with 600 mg ibuprofen resulted in significant improvement in anesthesia success.
Conclusion
Mandibular molars with symptomatic irreversible pulpitis were not thoroughly anesthetized by a combination of IANB+BI after premedication with ibuprofen (600 mg), even though anesthesia success was improved significantly by ibuprofen premedication.
Acknowledgment
Authors wish to thank Endodontology Research Center of Kerman University of Medical Sciences for the financial support.
Conflict of Interest:
‘None declared’.
References
- 1.Parirokh M, Rekabi AR, Ashouri R, Nakhaee N, Abbott PV, Gorjestani H. Effect of occlusal reduction on postoperative pain in teeth with irreversible pulpitis and mild tenderness to percussion. J Endod. 2013;39(1):1–5. doi: 10.1016/j.joen.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Moradi Askari E, Parirokh M, Nakhaee N, Hosseini HR, Abbott PV. The effect of maxillary first molar root length on the success rate of buccal infiltration anesthesia. J Endod. 2016;42(10):1462–6. doi: 10.1016/j.joen.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Maljaei E, Pourkazemi M, Ghanizadeh M, Ranjbar R. The efficacy of buccal infiltration of 4% articaine and psa injection of 2% lidocaine on anesthesia of maxillary second molars. Iran Endod J. 2017;12(3):276–81. doi: 10.22037/iej.v12i3.16464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sakhaeimanesh V, Khazaei S, Kaviani N, Saatchi M, Shafiei M, Khademi A. Anesthetic efficacy of articaine and ketamine for inferior alveolar nerve block in symptomatic irreversible pulpitis: a prospective randomized double-blind study. Iran Endod J. 2017;12(4):449–53. doi: 10.22037/iej.v12i4.16224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghoddusi J, Zarrabi MH, Daneshvar F, Naghavi N. Efficacy of ianb and gow-gates techniques in mandibular molars with symptomatic irreversible pulpitis: a prospective randomized double blind clinical study. Iran Endod J. 2018;13(2):143–8. doi: 10.22037/iej.v13i2.18625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta A, Sahai A, Aggarwal V, Mehta N, Abraham D, Jala S, Singh A. Anesthetic efficacy of primary and supplemental buccal/lingual infiltration in patients with irreversible pulpitis in human mandibular molars: a systematic review and meta-analysis. J Dent Anesth Pain Med. 2021;21(4):283. doi: 10.17245/jdapm.2021.21.4.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parirokh M, Abbott PV. Various strategies for pain-free root canal treatment. Iran Endod J. 2014;9(1):1. [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y-H, Wang D-R, Liu J-Y, Pan J. Local anesthesia in oral and maxillofacial surgery: A review of current opinion. J Dent Sci. 2020 doi: 10.1016/j.jds.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parirokh M, Yosefi MH, Nakhaee N, Manochehrifar H, Abbott PV, Reza Forghani F. Effect of bupivacaine on postoperative pain for inferior alveolar nerve block anesthesia after single-visit root canal treatment in teeth with irreversible pulpitis. J Endod. 2012;38(8):1035–9. doi: 10.1016/j.joen.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 10.Brandt RG, Anderson PF, McDonald NJ, Sohn W, Peters MC. The pulpal anesthetic efficacy of articaine versus lidocaine in dentistry: a meta-analysis. J Am Dent Assoc. 2011;142(5):493–504. doi: 10.14219/jada.archive.2011.0219. [DOI] [PubMed] [Google Scholar]
- 11.Kung J, McDonagh M, Sedgley CM. Does articaine provide an advantage over lidocaine in patients with symptomatic irreversible pulpitis? A systematic review and meta-analysis. J Endod. 2015;41(11):1784–94. doi: 10.1016/j.joen.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Su N, Li C, Wang H, Shen J, Liu W, Kou L. Efficacy and safety of articaine versus lidocaine for irreversible pulpitis treatment: a systematic review and meta‐analysis of randomised controlled trials. Aust Endod J. 2016;42(1):4–15. doi: 10.1111/aej.12125. [DOI] [PubMed] [Google Scholar]
- 13.Akhlaghi NM, Hormozi B, Abbott PV, Khalilak Z. Efficacy of ketorolac buccal infiltrations and inferior alveolar nerve blocks in patients with irreversible pulpitis: a prospective, double-blind, randomized clinical trial. J Endod. 2016;42(5):691–5. doi: 10.1016/j.joen.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Aggarwal V, Singla M, Kabi D. Comparative evaluation of effect of preoperative oral medication of ibuprofen and ketorolac on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis: a prospective, double-blind, randomized clinical trial. J Endod. 2010;36(3):375–8. doi: 10.1016/j.joen.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 15.Karapinar-Kazandag M, Tanalp J, Ersev H. Effect of premedication on the success of inferior alveolar nerve block in patients with irreversible pulpitis: a systematic review of the literature. Biomed Res Int. 2019:2019. doi: 10.1155/2019/6587429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar M, Singla R, Gill GS, Kalra T, Jain N. Evaluating combined effect of oral premedication with ibuprofen and dexamethasone on success of inferior alveolar nerve block in mandibular molars with symptomatic irreversible pulpitis: a prospective, double-blind, randomized clinical trial. J Endod. 2021;47(5):705–10. doi: 10.1016/j.joen.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Oleson M, Drum M, Reader A, Nusstein J, Beck M. Effect of preoperative ibuprofen on the success of the inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2010;36(3):379–82. doi: 10.1016/j.joen.2009.12.030. [DOI] [PubMed] [Google Scholar]
- 18.Ramazani M, Hamidi MR, Moghaddamnia AA, Ramazani N, Zarenejad N. The prophylactic effects of zintoma and ibuprofen on post-endodontic pain of molars with irreversible pulpitis: a randomized clinical trial. Iran Endod J. 2013;8(3):129. [PMC free article] [PubMed] [Google Scholar]
- 19.Shahi S, Mokhtari H, Rahimi S, Yavari HR, Narimani S, Abdolrahimi M, Nezafati S. Effect of premedication with ibuprofen and dexamethasone on success rate of inferior alveolar nerve block for teeth with asymptomatic irreversible pulpitis: a randomized clinical trial. J Endod. 2013;39(2):160–2. doi: 10.1016/j.joen.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 20.Nagendrababu V, Pulikkotil SJ, Veettil SK, Teerawattanapong N, Setzer FC. Effect of nonsteroidal anti-inflammatory drug as an oral premedication on the anesthetic success of inferior alveolar nerve block in treatment of irreversible pulpitis: a systematic review with meta-analysis and trial sequential analysis. J Endod. 2018;44(6):914–22. doi: 10.1016/j.joen.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 21.Parirokh M, Ashouri R, Rekabi AR, Nakhaee N, Pardakhti A, Askarifard S, Abbott PV. The effect of premedication with ibuprofen and indomethacin on the success of inferior alveolar nerve block for teeth with irreversible pulpitis. J Endod. 2010;36(9):1450–4. doi: 10.1016/j.joen.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 22.Saha SG, Jain S, Dubey S, Kala S, Misuriya A, Kataria D. Effect of oral premedication on the efficacy of inferior alveolar nerve block in patients with symptomatic irreversible pulpitis: a prospective, double-blind, randomized controlled clinical trial. J Clin Diagn Res. 2016;10(2):ZC25. doi: 10.7860/JCDR/2016/16873.7195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shantiaee Y, Javaheri S, Movahhedian A, Eslami S, Dianat O. Efficacy of preoperative ibuprofen and meloxicam on the success rate of inferior alveolar nerve block for teeth with irreversible pulpitis. Int Endod J. 2017;67(2):85–90. doi: 10.1111/idj.12272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yadav M, Grewal MS, Grewal S, Deshwal P. Comparison of preoperative oral ketorolac on anesthetic efficacy of inferior alveolar nerve block and buccal and lingual infiltration with articaine and lidocaine in patients with irreversible pulpitis: a prospective, randomized, controlled, double-blind study. J Endod. 2015;41(11):1773–7. doi: 10.1016/j.joen.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Corbella S, Taschieri S, Mannocci F, Rosen E, Tsesis I, Del Fabbro M. Inferior alveolar nerve block for the treatment of teeth presenting with irreversible pulpitis: A systematic review of the literature and meta-analysis. Quintessence Int. 2017;48:1. doi: 10.3290/j.qi.a37131. [DOI] [PubMed] [Google Scholar]
- 26.Jena A, Shashirekha G. Effect of preoperative medications on the efficacy of inferior alveolar nerve block in patients with irreversible pulpitis: A placebo-controlled clinical study. J Conserv Dent. 2013;16(2):171. doi: 10.4103/0972-0707.108209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nivedha V, Sherwood IA, Abbott PV, Ramaprabha B, Bhargavi P. Pre‐operative ketorolac efficacy with different anesthetics, irrigants during single visit root canal treatment of mandibular molars with acute irreversible pulpitis. Aust Endod J. 2020;46(3):343–50. doi: 10.1111/aej.12407. [DOI] [PubMed] [Google Scholar]
- 28.Zanjir M, Lighvan NL, Yarascavitch C, Beyene J, Shah PS, Azarpazhooh A. Efficacy and safety of pulpal anesthesia strategies during endodontic treatment of permanent mandibular molars with symptomatic irreversible pulpitis: a systematic review and network meta-analysis. J Endod. 2019;45(12):1435–64. doi: 10.1016/j.joen.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Heft MW, Parker SR. An experimental basis for revising the graphic rating scale for pain. Pain. 1984;19(2):153–61. doi: 10.1016/0304-3959(84)90835-2. [DOI] [PubMed] [Google Scholar]
- 30.Kwon H, Shin Y, Cho SY, Park SH, Jung IY. Factors affecting the success rate of buccal infiltration anaesthesia in the mandibular molar region. Int Endod J. 2014;47(12):1117–22. doi: 10.1111/iej.12259. [DOI] [PubMed] [Google Scholar]
- 31.Parirokh M, Abbott PV. Present status and future directions-mechanisms and management of local anaesthetic failures. Int Endod J. 2022 doi: 10.1111/iej.13697. [DOI] [PubMed] [Google Scholar]
- 32.Abazarpoor R, Parirokh M, Nakhaee N, Abbott PV. A comparison of different volumes of articaine for inferior alveolar nerve block for molar teeth with symptomatic irreversible pulpitis. J Endod. 2015;41(9):1408–11. doi: 10.1016/j.joen.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 33.Hosseini HR, Parirokh M, Nakhaee N, Abbott PV, Samani S. Efficacy of articaine and lidocaine for buccal infiltration of first maxillary molars with symptomatic irreversible pulpitis: a randomized double-blinded clinical trial. Iran Endod J. 2016;11(2):79. doi: 10.7508/iej.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kanaa M, Whitworth J, Corbett I, Meechan J. Articaine buccal infiltration enhances the effectiveness of lidocaine inferior alveolar nerve block. Int Endod J. 2009;42(3):238–46. doi: 10.1111/j.1365-2591.2008.01507.x. [DOI] [PubMed] [Google Scholar]
- 35.Parirokh M, Yosefi MH, Nakhaee N, Abbott PV, Manochehrifar H. The success rate of bupivacaine and lidocaine as anesthetic agents in inferior alveolar nerve block in teeth with irreversible pulpitis without spontaneous pain. Restor Dent Endod. 2015;40(2):155–60. doi: 10.5395/rde.2015.40.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parirokh M, Sadr S, Nakhaee N, Abbott P, Askarifard S. Efficacy of supplementary buccal infiltrations and intraligamentary injections to inferior alveolar nerve blocks in mandibular first molars with asymptomatic irreversible pulpitis: a randomized controlled trial. Int Endod J. 2014;47(10):926–33. doi: 10.1111/iej.12236. [DOI] [PubMed] [Google Scholar]
- 37.Shirvani A, Shamszadeh S, Eghbal MJ, Marvasti LA, Asgary S. Effect of preoperative oral analgesics on pulpal anesthesia in patients with irreversible pulpitis-a systematic review and meta-analysis. Clin Oral Investig. 2017;21(1):43–52. doi: 10.1007/s00784-016-1974-1. [DOI] [PubMed] [Google Scholar]
- 38.Pulikkotil S, Nagendrababu V, Veettil S, Jinatongthai P, Setzer F. Effect of oral premedication on the anaesthetic efficacy of inferior alveolar nerve block in patients with irreversible pulpitis–A systematic review and network meta‐analysis of randomized controlled trials. Int Endod J. 2018;51(9):989–1004. doi: 10.1111/iej.12912. [DOI] [PubMed] [Google Scholar]
- 39.Katyal V. The efficacy and safety of articaine versus lignocaine in dental treatments: a meta-analysis. J Dent. 2010;38(4):307–17. doi: 10.1016/j.jdent.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 40.Rodríguez LAG, Cattaruzzi C, Troncon MG, Agostinis L. Risk of hospitalization for upper gastrointestinal tract bleeding associated with ketorolac, other nonsteroidal anti-inflammatory drugs, calcium antagonists, and other antihypertensive drugs. Arch Intern Med. 1998;158(1):33–9. doi: 10.1001/archinte.158.1.33. [DOI] [PubMed] [Google Scholar]
- 41.Stentz D, Drum M, Reader A, Nusstein J, Fowler S, Beck M. Effect of a combination of intranasal ketorolac and nitrous oxide on the success of the inferior alveolar nerve block in patients with symptomatic irreversible pulpitis: a prospective, randomized, double-blind study. J Endod. 2018;44(1):9–13. doi: 10.1016/j.joen.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 42.Becker DE, Reed KL. Local anesthetics: review of pharmacological considerations. Anesth Prog. 2012;59(2):90–102. doi: 10.2344/0003-3006-59.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sambrook P, Smith W, Elijah J, Goss A. Severe adverse reactions to dental local anaesthetics: systemic reactions. Aust Endod J. 2011;56(2):148–53. doi: 10.1111/j.1834-7819.2011.01316.x. [DOI] [PubMed] [Google Scholar]
- 44.Parirokh M, Satvati SA, Sharifi R, Rekabi AR, Gorjestani H, Nakhaee N, Abbott PV. Efficacy of combining a buccal infiltration with an inferior alveolar nerve block for mandibular molars with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(3):468–73. doi: 10.1016/j.tripleo.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 45.Ashraf H, Kazem M, Dianat O, Noghrehkar F. Efficacy of articaine versus lidocaine in block and infiltration anesthesia administered in teeth with irreversible pulpitis: a prospective, randomized, double-blind study. J Endod. 2013;39(1):6–10. doi: 10.1016/j.joen.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 46.Fowler S, Drum M, Reader A, Beck M. Anesthetic success of an inferior alveolar nerve block and supplemental articaine buccal infiltration for molars and premolars in patients with symptomatic irreversible pulpitis. J Endod. 2016;42(3):390–2. doi: 10.1016/j.joen.2015.12.025. [DOI] [PubMed] [Google Scholar]
- 47.Kanaa MD, Whitworth JM, Meechan JG. A prospective randomized trial of different supplementary local anesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in mandibular teeth. J Endod. 2012;38(4):421–5. doi: 10.1016/j.joen.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 48.Matthews R, Drum M, Reader A, Nusstein J, Beck M. Articaine for supplemental buccal mandibular infiltration anesthesia in patients with irreversible pulpitis when the inferior alveolar nerve block fails. J Endod. 2009;35(3):343–6. doi: 10.1016/j.joen.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 49.Fan S, Chen W-l, Pan C-b, Huang Z-q, Xian M-q, Yang Z-h, Dias-Ribeiro E, Liang Y-c, Jiao J-y, Ye Y-s. Anesthetic efficacy of inferior alveolar nerve block plus buccal infiltration or periodontal ligament injections with articaine in patients with irreversible pulpitis in the mandibular first molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(5):e89–e93. doi: 10.1016/j.tripleo.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 50.Lapidus D, Goldberg J, Hobbs EH, Ram S, Clark GT, Enciso R. Effect of premedication to provide analgesia as a supplement to inferior alveolar nerve block in patients with irreversible pulpitis. J Am Dent Assoc. 2016;147(6):427–37. doi: 10.1016/j.adaj.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 51.Li C, Yang X, Ma X, Li L, Shi Z. Preoperative oral nonsteroidal anti-inflammatory drugs for the success of the inferior alveolar nerve block in irreversible pulpitis treatment: a systematic review and meta-analysis based on randomized controlled trials. Quintessence Int. 2012;43(3):209–19. [PubMed] [Google Scholar]
- 52.Sood R, Hans M-K, Shetty S. Comparison of anesthetic efficacy of 4% articaine with 1: 100,000 epinephrine and 2% lidocaine with 1: 80,000 epinephrine for inferior alveolar nerve block in patients with irreversible pulpitis. J Clin Exp Dent. 2014;6(5):e520. doi: 10.4317/jced.51617. [DOI] [PMC free article] [PubMed] [Google Scholar]