Abstract
Endodontic-periodontal lesions have always been a challenge for treatment due to the reduced success rate in comparison to endodontic or periodontal lesions alone. This case report describes surgical/endodontic management of supra-erupted non-vital maxillary incisor with primary periodontal and secondary endodontic lesions with mobility grade III and severe horizontal and vertical loss of attachment apparatus in a 55 years old woman with aggressive periodontitis. The successful results at one-year follow-up revealed that with an appropriate case selection strategy, proper regeneration method and soft tissue enhancement, severe combined endo-perio lesions may treat.
Key Words: Chronic Periodontitis, Periodontal Endodontic Lesion, Periodontal Regeneration
Introduction
Periodontal involvement with subsequent endodontic lesion is a complicated situation because it usually comes with massive periodontal destruction that could compromise tooth vitality. In this situation, reductive periodontal surgery with the aim of pocket elimination cannot be achieved and the only option is to do guided tissue regeneration (GTR). Success of GTR process depends on various factors, including stage of destruction and remaining bony walls, as in cases with higher levels of destruction, less successful outcome is expected.
A principal reason for periodontal regenerative therapy is to achieve healthy tooth supporting structure that could meet patients functional needs and also satisfies his/her aesthetic demands [1]. Reduced probing depth (PD) and clinical attachment level (CAL) gain are the most common criteria for evaluating the result of periodontal treatment [2, 3]. Although these goals could be obtained by conventional periodontal surgery, today there is a tremendous interest to regenerative treatments, named GTR with rational of recreating tooth supporting structures, i.e. cementum, periodontal ligament and alveolar bone [4]. Since the introduction of GTR by Gotllow et al. [5], there was a lot of clinical trials comparing open flap debridement and GTR in cases which both treatment modalities could be considered to be beneficial for the patient [6]. But in cases with severe loss of attachment apparatus, the only treatment option could be to save the tooth with regenerative therapy if possible, or to do tooth extraction. There is limited reports of using GTR for treatment of tooth with extreme peripheral loss of attachment. In this article, we describe surgical procedure of saving a maxillary incisor with sever bone loss and grade III mobility and puss secretion.
Case Report
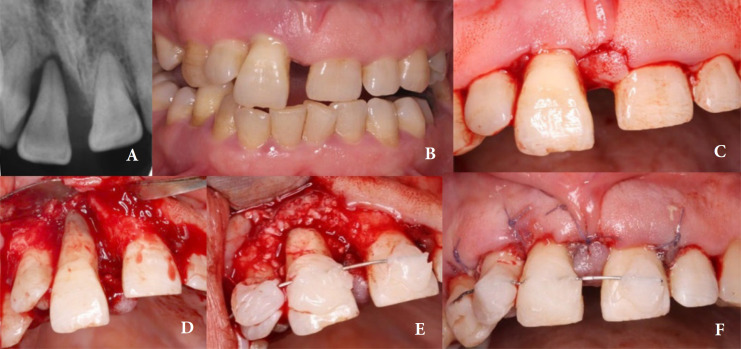
A 55 years old woman, with none contributory medical statement and chief complaint of hypermobility of right maxillary incisor, referred to the department of periodontology of Mashhad University of Medical Sciences. In clinical examination, the tooth was 3 mm supra-erupted compared to adjacent central incisor and showed sever mobility in both horizontal and vertical dimensions (grade III mobility, Miller classification [7]; Figures1A and 1B). Probing depth varied from 12 mm in mid buccal and mid palatal to 6-8 mm in interproximal areas. Puss secretion was observed due to probing. Plaque index was 85%. Periodontal condition of the patient diagnosed as periodontitis stage IV grade C based on the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions [8]. The tooth did not respond to any cold sensibility, or electric pulp tester and was only sensitive for percussion test. The diagnosis for pulp and periapical conditions were pulp necrosis associated with symptomatic apical periodontitis.
Figure 1.
A) Preoperative radiograph, vertical bone loss extended to the apex mesially and distally; B) Clinical photograph, extruded right central incisor and pathologic migration; C) Flap design with modified papilla preservation method; D) Flap reflected and defect debrided thoroughly; E) GTR procedure performed around right central incisors and teeth splinted; F) Flap adaptation and suturing
Supra and subgingival scaling and root planning were performed in two sessions with 1 week interval; amoxicillin 500 mg and metronidazole 250 mg were prescribed for 1 week. After 1 month, clinical parameters was reevaluated. Plaque index decrease to 20% and bleeding on probing (BOP) showed significant decrease in comparison with baseline. But the probing depths and mobility of tooth #11 was remained unchanged. Tooth prognosis considered questionable to hopeless according to McGuire and Nunn classification [9].
Patient informed about condition and prognosis of the tooth. Treatment modalities and esthetic challenges of implant treatment due to lack of sufficient vertical bone height was described to the patient. Regarding all considered factors, rescue of the tooth was attempted. Informed consent was obtained before surgery.
Surgical protocol
The patient obtained 2g amoxicillin 1h before surgery as a prophylactic regimen before any GTR and was advised to wash her mouth with 0.2% chlorhexidine for 1 min [10]. Under local infiltration anesthesia with 2% lidocaine containing 1:80000 epinephrine (Darupakhsh, Tehran, Iran), a modified papilla preservation flap was performed (Figure 1C) and the buccal and palatal flap was elevated thoroughly to have a good vision of bony defect (Figure 1D). After degranulation and debridement of the root surface, the tooth was relocated apically with hand pressure and then a semi-rigid splint with wire and composite resin fixed the tooth to the adjacent teeth. Freeze-dried bone allograft (500-1000 micrometer; Regen Allograft, Tehran, Iran) placed all over the apical third of the root (Figure 1E), and collagenic membrane (0.3-0.6 mm precordium membrane; Regen Allograft, Tehran, Iran) was used to stabilize the bone material. The flap was repositioned and secured with vicryl 5-0 (Supa, Tehran, Iran; Figure 1F). Amoxicillin and 0.2 % chlorhexidine mouthwash were prescribed for the patient for 1 week.
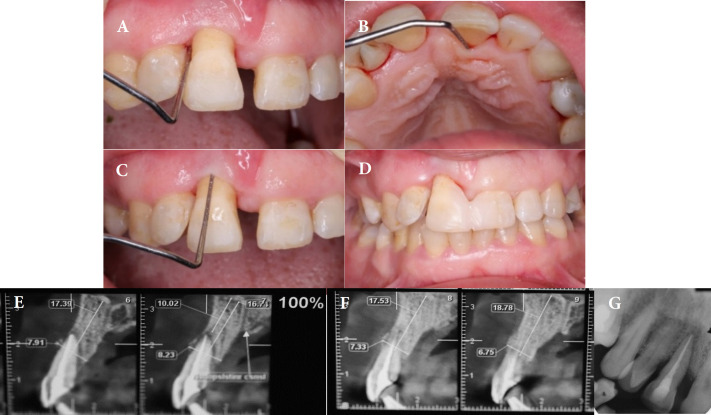
Sutures were removed after 2 weeks. Healing was uneventful and no membrane exposure was observed. The patient was referred to the endodontist for root canal treatment 2 weeks postoperative. The reason that root canal treatment didn’t perform sooner, was severe mobility and need to splint the tooth after relocation during surgery. The patient recalled monthly for 6 months. The splint was removed at this time. Clinical evaluation showed a significant decrease in probing depth (the uppermost PD was 3 mm in mid-palatal) without BOP (Figures 2A to 2C). One month later, a slight upward movement of the tooth was noticed. So the tooth was splinted to the adjacent incisor with composite resin (Figure 2D) and the patient asked to use an interdental brush. Eight months post-operative, a cone-beam computed tomography (CBCT) scan was taken (Figures 2E and 2F). Twelve-month follow-up showed stable results, no BOP, and PD was 1-2 mm (Figure 2G).
Figure 2.
A) Six months follow-up with reduced pocket depth mesially; B) Follow up photograph with reduced pocket depth to 3 mm palatally; C) Follow-up and pocket depth 3 mm labially; D) Composite splinting and central incisor reshaping; E & F) CBCT radiograph 8 months after GTR procedure; note alveolar bone formed labially and mesio-distally; G) Periapical radiographs after 12 months, notable bone formation apico-coronally
Discussion
Evidence regarding the treatment of primary periodontal and subsequent endodontic lesions is rare in the literature [11]. Most of the articles refer to teeth with primary endodontic and secondary periodontal involvement or combined endo-perio lesions [12-15]. In this article, successful management of a maxillary incisor has presented which had a primary periodontal lesion with secondary endodontic involvement. The baseline prognosis was classified as questionable to hopeless according to McGuire and Nunn's classification [9]. But the prognosis improved after periodontal surgery and endodontic treatment. The importance of pre-surgical splinting has been proven in such cases and is associated with better outcomes [16, 17]. In this case, the tooth was 3 mm supra-erupted and was in a traumatic position with the apposed tooth. Therefore, after debridement and granulation tissue removal, relocation to the original position was done and a semi-rigid splint was placed. Despite previous articles, endodontic treatment was performed after periodontal surgery. Since the tooth was highly mobile (more than 4 mm in the horizontal direction and 1 mm in the vertical direction), it had to be repositioned and splinted in the correct position prior to the root canal treatment. The impact of strict maintenance following the GTR procedure, to achieve favorable outcomes, is undeniable, so the patient was instructed about weekly follow-ups for the first 2 months post-surgery; then it was changed to monthly follow-ups.
Endodontic-periodontal (endo-perio) dilemma has always been a challenge of treatment. The number of successfully treated cases is significantly lower in comparison with isolated endodontic lesions [18]. The decision-making process to save the tooth based on initial prognosis is another challenge, since most of the teeth with massive endo-perio lesions, specifically those with primary periodontal and secondary endodontic involvement, are classified with questionable or hopeless prognoses. It should be considered as Kwok & Caton said [19]: “because the periodontium is highly dynamic, the timing of prognostication is extremely important, so the periodontal prognosis is a dynamic entity”.
In cases with isolated endodontic involvement, the size of the lesion doesn’t seem to affect the outcome [18]. Analysis of the of root canal treatments’ outcome, revealed high survival rate [20] and proved that the number of teeth extracted due to the endodontic failure, is less than 10% [21]. In contrary, there is not a consensus upon whether the lesion size is important in the treatment outcome of combined endo-perio lesions [18]; in such lesions, the prognosis of periodontal lesion is the main determinant of overall prognosis. New designs in surgical procedures, including papilla preservation flaps, magnification, and the introduction of enamel matrix derivative (Emdogain) has led to improvements in successful treatment of cases that seemed impossible to treat before [22].
A 6-8 mm probing clinical attachment level gain and reducing mobility to grade I post-splint removal, are highly optimal results for this case. These results demonstrate the potential of regenerative therapy, more than previously expected, and further reconfirms that saving the tooth in such complicated situations could be a logical decision, considering that extraction of a single tooth in aggressive periodontitis cases may lead to unstoppable serial extractions.
Conclusion
This case report explained that with an appropriate case selection strategy and proper regeneration method, as well as soft tissue enhancement we may treat severe combined endo-perio lesions. The final outcome of this procedure depends on a thorough assessment of the periodontal condition of the tooth and its prognosis, stringent regeneration modality, importance of splinting, and successful endodontic treatment.
Conflict of Interest:
‘None declared’.
References
- 1.Zander HA, Polson AM, Heijl LC. Goals of periodontal therapy. J Periodontol. 1976;47(5):261–6. doi: 10.1902/jop.1976.47.5.261. [DOI] [PubMed] [Google Scholar]
- 2.Hujoel PP, Löe H, Anerud A, Boysen H, Leroux BG. The informativeness of attachment loss on tooth mortality. J Periodontol. 1999;70(1):44–8. doi: 10.1902/jop.1999.70.1.44. [DOI] [PubMed] [Google Scholar]
- 3.Hujoel PP, Leroux BG, DeRouen TA, Powell LV, Kiyak HA. Evaluating the validity of probing attachment loss as a surrogate for tooth mortality in a clinical trial on the elderly. J Dent Res. 1997;76(4):858–66. doi: 10.1177/00220345970760040701. [DOI] [PubMed] [Google Scholar]
- 4.Garrett S. Periodontal regeneration around natural teeth. Ann Periodontol. 1996;1(1):621–66. doi: 10.1902/annals.1996.1.1.621. [DOI] [PubMed] [Google Scholar]
- 5.Gottlow J, Nyman S, Karring T, Lindhe J. New attachment formation as the result of controlled tissue regeneration. J Clin Periodontol. 1984;11(8):494–503. doi: 10.1111/j.1600-051x.1984.tb00901.x. [DOI] [PubMed] [Google Scholar]
- 6.Petsos H, Ratka-Krüger P, Neukranz E, Raetzke P, Eickholz P, Nickles K. Infrabony defects 20 years after open flap debridement and guided tissue regeneration. J Clin Periodontol. 2019;46(5):552–63. doi: 10.1111/jcpe.13110. [DOI] [PubMed] [Google Scholar]
- 7.SC M. Textbook of periodontia. 3 ed. Blackston; 1950. [Google Scholar]
- 8.Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF. Periodontitis: consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and peri-Implant Diseases and Conditions. J Periodontol. 2018:89 Suppl 1:S173–s82. doi: 10.1002/JPER.17-0721. [DOI] [PubMed] [Google Scholar]
- 9.McGuire MK, Nunn ME. Prognosis versus actual outcome The effectiveness of clinical parameters in developing an accurate prognosis. J Periodontol. 1996;67(7):658–65. doi: 10.1902/jop.1996.67.7.658. [DOI] [PubMed] [Google Scholar]
- 10.Hai JH, Lee C, Kapila YL, Chaffee BW, Armitage GC. Antibiotic prescribing practices in periodontal surgeries with and without bone grafting. J Periodontol. 2020;91(4):508–15. doi: 10.1002/JPER.19-0195. [DOI] [PubMed] [Google Scholar]
- 11.Blank BS, Levy AR. Combined treatment of a large periodontal defect using GTR and DFDBA. Int J Periodontics Restorative Dent. 1999;19(5):481–7. [PubMed] [Google Scholar]
- 12.Pompa DG. Guided tissue repair of complete buccal dehiscences associated with periapical defects: a clinical retrospective study. J Am Dent Assoc. 1997;128(7):989–97. doi: 10.14219/jada.archive.1997.0340. [DOI] [PubMed] [Google Scholar]
- 13.Sooratgar A, Tabrizizade M, Nourelahi M, Asadi Y, Sooratgar H. Management of an endodontic-periodontal lesion in a maxillary lateral incisor with palatal radicular groove: a case report. Iran Endod J. 2016;11(2):142–5. doi: 10.7508/iej.2016.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fonseca FO, Vasconcellos BC, Costa MM, Sobrinho APR, Tavares WLF. Combined endodontic and surgical therapy for resolution of type III dens invaginatus. Iran Endod J. 2020;15(2):117–23. doi: 10.22037/iej.v15i2.26882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qing L, Hong Z, Xu S, Ning Y, Ma X, Yang M, Chen L. Periodontal regeneration of teeth with radicular developmental groove after intentional replantation: two case reports. Iran Endod J . 16(4):254–60. doi: 10.22037/iej.v16i4.33432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cortellini P, Tonetti MS, Lang NP, Suvan JE, Zucchelli G, Vangsted T, Silvestri M, Rossi R, McClain P, Fonzar A, Dubravec D, Adriaens P. The simplified papilla preservation flap in the regenerative treatment of deep intrabony defects: clinical outcomes and postoperative morbidity. J Periodontol. 2001;72(12):1702–12. doi: 10.1902/jop.2001.72.12.1702. [DOI] [PubMed] [Google Scholar]
- 17.Schulz A, Hilgers RD, Niedermeier W. The effect of splinting of teeth in combination with reconstructive periodontal surgery in humans. Clin Oral Investig. 2000;4(2):98–105. doi: 10.1007/s007840050123. [DOI] [PubMed] [Google Scholar]
- 18.Kim E, Song JS, Jung IY, Lee SJ, Kim S. Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J Endod. 2008;34(5):546–51. doi: 10.1016/j.joen.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 19.Kwok V, Caton JG. Commentary: prognosis revisited: a system for assigning periodontal prognosis. J Periodontol. 2007;78(11):2063–71. doi: 10.1902/jop.2007.070210. [DOI] [PubMed] [Google Scholar]
- 20.Paolantonio M, Femminella B, Coppolino E, Sammartino G, D'Arcangelo C, Perfetti G, Perinetti G. Autogenous periosteal barrier membranes and bone grafts in the treatment of periodontal intrabony defects of single-rooted teeth: a 12-month reentry randomized controlled clinical trial. J Periodontol. 2010;81(11):1587–95. doi: 10.1902/jop.2010.100094. [DOI] [PubMed] [Google Scholar]
- 21.Vire DE. Failure of endodontically treated teeth: classification and evaluation. J Endod. 1991;17(7):338–42. doi: 10.1016/S0099-2399(06)81702-4. [DOI] [PubMed] [Google Scholar]
- 22.Pico-Blanco A, Castelo-Baz P, Caneiro-Queija L, Liñares-González A, Martin-Lancharro P, Blanco-Carrión J. Saving single-rooted teeth with combined endodontic-periodontal lesions. J Endod. 2016;42(12):1859–64. doi: 10.1016/j.joen.2016.08.015. [DOI] [PubMed] [Google Scholar]