Abstract
Objectives
The current study explores the level of perceived social stigma and associated psychological challenges among healthcare workers during the second wave of the COVID-19 pandemic in Egypt.
Methods
This was a cross-sectional study of 150 healthcare workers at Cairo University hospitals that were confirmed positive for COVID-19 infection. Participants were interviewed for assessment of perceived COVID-19-related stigma and associated psychological symptoms using the Patient Health Questionnaire for depression, the Generalized Anxiety Disorder Assessment for anxiety, and the Post-Traumatic Stress Disorder Checklist for post-traumatic stress symptoms.
Results
Two-thirds of participants perceived moderate-to-severe COVID-19-related stigma. Depression, anxiety, and post-traumatic stress symptoms were observed at varying levels in 58.0%, 38.0%, and 11.3% of participants, respectively. Female sex and occupation as a nurse were significantly associated with the total perceived COVID-19-related stigma score. COVID-19-related stigma perception significantly correlated with depression, anxiety, and post-traumatic stress.
Conclusion
Perceived social stigma prevails among healthcare workers and is associated with numerous psychological disturbances.
Keywords: Healthcare workers, stigma perception, COVID-19, Cairo University hospital, psychological symptoms, depression, anxiety, post-traumatic stress disorder.
Introduction
On 11 March 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) a global pandemic. Since then, the world has been witnessing the pandemic’s detrimental impact on various psychological and social aspects.1 Although the pandemic’s effects on social and mental health are still under research, the link between viral epidemics and the development of psycho-social derangement has been described repeatedly in the literature.2,3 Reports during and after the severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome outbreaks have documented significant levels of anxiety, depression, and post-traumatic stress symptoms in survivors at 1 month and up to 50 months of follow-up.4 The global social stigma pandemic that started early—when COVID-19 infection was still confined to China—was an associated observation. At the time, the virus was often stereotypically referred to as the “Chinese virus” by many international newspapers and political authorities, as though a virus could have a nationality.5
The COVID-19-related stigma spread globally in concert with the disease itself. Although this ripple stigma effect impacts all community members through various pathways, certain groups are more vulnerable than others, notably those working in the healthcare system.6
Social avoidance, public harassment, physical violence, and restrictions in the use of public transport were reported forms of social stigmatization experienced by healthcare workers (HCWs) globally7 not only in developing countries such as Mexico, Malawi, Bangladesh, and India but also in the United Kingdom and the United States. More than 200 global incidents of COVID-19-related assaults on HCWs and medical facilities were recorded during the current pandemic.8
The spreading COVID-19-related social stigma against HCWs is a burden to their psychological well-being, which is already endangered by the uncertainty of the new disease, the long and high-pressure work hours, and the continuous fear of potentially exposing families and their loved ones to infection.9 The psychologically traumatizing effects of stigma on HCWs—especially those who were in direct contact with patients—were previously reported during the Middle East respiratory syndrome outbreak.10 During the current pandemic and especially during the first wave, Egyptian HCWs were often labeled as a source of infection and repeatedly ostracized by society.11 For example, a physician who died of severe COVID-19 illness was denied burial by the people of her village whereas many others were forced to abandon their homes after being accused of bringing the disease to their neighborhoods.12 These incidents alerted local Egyptian authorities to the importance of increasing public awareness of infection transmission and effective self-protection and shed light on the considerable role of HCWs in the fierce battle against the COVID-19 pandemic.
Our study aimed to detect whether social stigmatization remains an obstacle faced by Egyptian HCWs and explore the mental health-related factors that may be associated with high levels of stigma perception. Our results can guide the development by responsible authorities of national interventions that support the mental health of HCWs who desire a better lifestyle. Furthermore, findings can assist the design of public health education programs aimed at improving the level of community awareness and acceptance. This will pave the way for considerable improvement in the national management of future health-related catastrophes.
Methodology
This cross-sectional study was conducted from February 2021 to April 2021 on workers at Cairo University hospitals who showed symptoms suggesting COVID-19 infection during the second wave of the pandemic. Workers were then assessed for symptom severity through the Al Kasr-AlAiny Hospital phone triage service and were referred for reverse transcriptase-polymerase chain reaction testing of nasopharyngeal swabs for severe acute respiratory syndrome coronavirus 2. Only those who tested positive for COVID-19 infection between December 2020 to the end of February 2021 were contacted by phone 2 months after infection for assessment of post-COVID-19 psychological sequelae and stigma perception. Those with a history of psychological disease at any time before COVID-19 infection (as detected by medical history taken early in the phone interview) were excluded from the study. Study participants included not only physicians and nurses but also technicians, janitors, pharmacists, and those in administrative positions at Cairo University hospitals.
The calculated sample size of 150 participants, based on previous studies that assessed stigma perception among HCWs during the COVID-19 pandemic,13 was determined with OpenEpi 6 software using a confidence interval of 95% and a power of 80%. One hundred sixty participants were contacted 2 months after infection and interviewed by phone to complete the questionnaires. Ten respondents were excluded because of refusal to participate or a previous history of psychological disease and all patient details were de-identified.
The reporting of this study conforms to STROBE guidelines.14
Research tools
Section 1: Sociodemographic and clinical characteristics
A questionnaire including the following items was developed to detect sociodemographic characteristics, medical history, and COVID-19-related clinical data:
Age, sex, residency, marital status, occupation (e.g., doctor, technician, administrative job), and specialty
History of psychiatric disorders before COVID-19 infection (for exclusion)
History of chronic disease (e.g., diabetes mellitus, hypertension)
Smoking history
Whether direct involvement in the care of COVID-19 patients and specification of the care pathway (e.g., clinic, isolation room, or ICU)
Place of treatment when infected with COVID-19 (e.g., home, hospital ward, or ICU)
The need for mechanical ventilation when infected with COVID-19
The need for corticosteroids in the COVID-19 treatment regimen.
Section 2: Perceived COVID-19-related stigmatization
A thorough review of the literature until the study date yielded no specific tools for the detection of COVID-19-related stigma. Based on research that evaluated stigma perception among HCWs during similar epidemics, we used the tool developed by Verma et al.,15 who adapted the HIV Berger scale16 to assess stigma perception among HCWs in Singapore during the 2004 SARS epidemic.
Our scale consisted of 17 items that are classified into four subscales—disclosure concerns, personalized stigma, concern with public attitudes, and negative self-image—and each item can be assigned to more than one subscale. Using a 4-point Likert scale, the 17 items were scored 1, 2, 3, and 4 corresponding to the answers “strongly disagree,” “disagree,” “agree,” and “strongly agree,” respectively. The total score ranged from 17 to 68, with high scores indicating high levels of perceived stigmatization. Each subscale was scored by adding the scores of its constituent items. The 17-item scale had a Cronbach’s alpha of 0.906, suggesting high internal consistency.7 Because of the lack of a universally accepted cutoff point for scores, we adopted Charles et al.’s categorization, in which the overall scores are captured into three stigma categories—no-mild, moderate, and severe—using the 33rd and the 66th percentile cutoff values from the distribution of scores.17
The questionnaire was translated into Arabic by the Cairo University Centre for Foreign Languages and Specialized Translation to fit our study population, which included healthcare workers who were not necessarily familiar with the English language. The Arabic version was tested for the suitability and clarity of questions before being used in the study on a separate diversified sample of HCWs whose answers were not included in the study results. The pilot testing revealed no need for modifying or rephrasing the translated questionnaire items. Face validation of the questionnaire was performed by two family medicine experts.
Section 3: Post-COVID-19 psychological sequelae
Depression, anxiety, and symptoms of post-traumatic stress disorder (PTSD) were evaluated using Arabic versions of the following validated tools:
The 9-item Patient Health Questionnaire (PHQ-9; range: 0–27):18–20 This tool was used for the assessment of depression symptom severity. The PHQ-9 score was calculated by allocating scores of 0, 1, 2, and 3 corresponding to the responses “not at all,” “several days,” “on more than half of the days,” and “nearly every day,” respectively. The total score was categorized as follows: no depression (0–4), mild depression (5–9), moderate depression (10–14), and severe depression (15–27). The Cronbach’s alpha of the Arabic version of the questionnaire was 0.857.19
The Generalized Anxiety Disorder Questionnaire (GAD-7; range: 0–21):20,21 This tool assessed the severity of anxiety symptoms. The GAD-7 is calculated by giving scores of 0, 1, 2, and 3 corresponding to the responses “not at all,” ”several days,” “on more than half of the days,” and “nearly every day,” respectively. Total scores of 5, 10, and 15 were the cutoff points for mild, moderate, and severe anxiety, respectively. The Cronbach’s alpha of the Arabic version of the questionnaire was 0.763.19
The 20-item Post Traumatic Stress Disorder Checklist for DSM-5 (PCL-5; range: 0–80):22,23 This tool assessed PTSD symptoms by asking participants to report their emotions toward a specific traumatic experience. In this study, participants were asked to respond about their experience with the COVID-19 pandemic as HCWs and COVID-19 survivors. The PCL-5 items were rated on a 5-point Likert-type scale with scores ranging from “not at all” (0) to “extremely” (4). A score of 33 was used as a cutoff for the diagnosis of PTSD based on previous research.23,24 The Cronbach’s alpha of the Arabic version of the questionnaire was 0.85.23
Ethics approval and consent to participate
Approval was obtained from the Research Ethics Committee of the Faculty of Medicine, Cairo University (Institutional review board: MD-78-2021; date of approval: 8-4-2021). After oral consent was obtained from participants at the beginning of the phone interview, a clarification of study objectives was provided, followed by a statement disclosing that responding is voluntary and a rationale for refusing to participate is not required.
Statistical analysis
Data were coded and entered into Microsoft Excel.® IBM SPSS Statistical Package for Social Sciences version 24 (IBM Corp., Armonk, NY, USA) was used for data management and statistical analysis.
Means and standard deviations or medians and ranges were used to summarize numerical data while percentages were used to summarize categorical data. A t-test and the Mann–Whitney test were used to compare normally distributed and non-normally distributed numerical variables, respectively. For categorical variables, the chi-square test or Fisher’s exact test was used as appropriate for various analyses.
Adjusted odds ratios were determined using stepwise logistic regression to measure the magnitude of the effect of various factors on COVID-19-related stigma grades. All P-values were two-sided. P-values ≤0.05 were considered significant.
Results
A total of 150 HCWs with a mean age of 36.9 ± 10.6 years participated. More than half of the participants were female (54.0%), married (71.3%), and living in Cairo (50.7%) and the majority were doctors (38.6%) and nurses (30.0%). The majority were nonsmokers (90.7%) and only 28.7% had chronic disease, which predominantly included hypertension (34.9%) and diabetes (23.3%).
One-third (33.3%) of participants were directly involved in the care of COVID-19 patients, mainly through working in isolation wards (15.3%). Most of those who were infected were treated at home (91.3%) and did not require mechanical ventilation (99.3%); only 29.3% received corticosteroids as a part of their treatment regimen (Table 1).
Table 1.
Sociodemographic and COVID-19-related characteristics of the study sample (n = 150).
| Count | % | |
|---|---|---|
| Age (years) | ||
| Mean ± SD | 36.9 ± 10.6 | |
| Range | 22–60 | |
| Sex | ||
| Female | 81 | 54.0 |
| Male | 69 | 46.0 |
| Smoking | ||
| No | 136 | 90.7 |
| Yes | 14 | 9.3 |
| Marital status | ||
| Married | 107 | 71.3 |
| Single | 38 | 25.3 |
| Divorced | 4 | 2.7 |
| Widow | 1 | 0.7 |
| Residency | ||
| Cairo | 76 | 50.7 |
| Giza | 64 | 42.7 |
| Other governorates | 10 | 6.7 |
| Occupation | ||
| Doctors | 58 | 38.6 |
| Nurses | 45 | 30.0 |
| Administrative job in faculty/hospital | 20 | 13.3 |
| Others* | 14 | 9.3 |
| Technicians | 13 | 8.7 |
| Chronic diseases | ||
| No | 107 | 71.3 |
| Yes | 43 | 28.7 |
| Type of chronic disease (n = 43)** | ||
| Hypertension | 15 | 34.9 |
| Diabetes mellitus | 10 | 23.3 |
| Hypothyroidism | 7 | 16.3 |
| Cardiac disease | 6 | 14.0 |
| Asthma | 6 | 14.0 |
| Dyslipidemia | 6 | 14.0 |
| Other*** | 6 | 14.0 |
| Rheumatoid arthritis | 3 | 7.0 |
| Directly involved in the care of COVID-19 patients | ||
| No | 100 | 66.7 |
| Yes | 50 | 33.3 |
| COVID-19 patient care pathway (n = 50) | ||
| Isolation ward | 23 | 15.3 |
| ICU | 13 | 8.7 |
| Outpatient clinic | 8 | 5.3 |
| Radiology services | 6 | 4.0 |
| Place of treatment when infected with COVID-19 | ||
| Home | 137 | 91.3 |
| Hospital ward | 11 | 7.3 |
| ICU | 2 | 1.3 |
| Need for mechanical ventilation | ||
| No | 149 | 99.3 |
| Yes | 1 | 0.7 |
| Need for corticosteroids in treatment regimen | ||
| No | 106 | 70.7 |
| Yes | 44 | 29.3 |
SD: standard deviation, ICU: intensive care unit.
*Other occupations included janitors, pharmacists, nutritionists, and laboratory specialists.
**Some participants had more than one chronic disease at the same time.
***Other chronic diseases included glucose-6-phosphate dehydrogenase deficiency, gastroesophageal reflux disease, epilepsy, chronic hepatitis B, and sinusitis.
The study sample included HCWs across various specialties. Some respondents, such as ICU staff, anesthesiologists, and the staff of laboratory and radiology departments, were frontliners caring for COVID-19 patients; the remaining participants were academic staff and those in administrative posts in the faculty or hospital who were not directly involved in the care of COVID-19 patients. No statistically significant relationships were observed between the various specialties and the total COVID-19-related stigma score (Table 2).
Table 2.
Total COVID-19-related stigma scores within specialties and departments (n = 150).
| Specialty | N (%) | Mean | SD | P-value |
|---|---|---|---|---|
| Total COVID-19 related stigma score | ||||
| Medical specialties | 49 (32.7) | 28.1 | 8.8 | 0.278 |
| Surgical specialties | 40 (26.7) | 30.9 | 11.6 | |
| Administrative jobs | 20 (13.3) | 27.9 | 7.8 | |
| Diagnostic (laboratory and radiology) staff | 19 (12.7) | 31.5 | 12.9 | |
| Academic jobs and house officers | 12 (8.0) | 24.8 | 4.0 | |
| ICU-anesthesia | 10 (6.7) | 32.1 | 9.0 |
SD: standard deviation, ICU: intensive care unit.
Nearly 70% of participants perceived moderate-to-severe COVID-19-related stigma, with varying response rates across the four stigma subscales (Table 3). With regard to the post-COVID-19 psychological impact, 58.0%, 38.0%, and 11.3% of respondents experienced varying levels of depression, anxiety, and PTSD symptoms, respectively (Table 4). Fifty-eight participants (38.7%) did not report any post-COVID-19 psychological symptoms.
Table 3.
Total COVID-19-related stigma level and subscale distribution (n = 150).
| Questionnaire | Cutoff score | Level | Count | % |
|---|---|---|---|---|
| Total COVID-19-related stigma scale | 0–33% | No-mild | 50 | 33.3 |
| >33–<66% | Moderate | 88 | 58.7 | |
| ≥66% | Severe | 12 | 8.0 | |
| Total COVID-19-related stigma scale Mean ± SD | 43.01 ± 14.53 | |||
| Personalized stigma subscale | 0–33% | No-mild | 88 | 58.7 |
| >33–<66% | Moderate | 48 | 32.0 | |
| ≥66% | Severe | 14 | 9.3 | |
| Personalized stigma subscaleMean ± SD | 37.7 ± 16.53 | |||
| Disclosure concern subscale | >33–<66% | Moderate | 142 | 94.7 |
| ≥66% | Severe | 8 | 5.3 | |
| Disclosure concern subscaleMean ± SD | 47.67 ± 7.92 | |||
| Negative self-image subscale | 0–33% | No-mild | 73 | 48.7 |
| >33–<66% | Moderate | 66 | 44.0 | |
| ≥66% | Severe | 11 | 7.3 | |
| Negative self-image subscaleMean ± SD | 36.28 ± 14.71 | |||
| Concern with public attitude subscale | 0–33% | No-mild | 63 | 42.0 |
| >33–<66% | Moderate | 68 | 45.3 | |
| ≥66% | Severe | 19 | 12.7 | |
| Concern with public attitude subscale Mean ± SD | 42.57 ± 17.16 | |||
SD: standard deviation.
Table 4.
Post-COVID psychological sequelae (n = 92).
| Questionnaire | Cutoff score | Level | Count | % |
|---|---|---|---|---|
| Depression (PHQ-9) | 0–4 | No Depression | 63 | 42.0 |
| 5–9 | Mild | 35 | 23.3 | |
| 10–14 | Moderate | 35 | 23.3 | |
| 15–19 | Moderately Severe | 15 | 10.0 | |
| ≥20 | Severe | 2 | 1.3 | |
| PHQ-9 Mean ± SD | 7 ± 6 | |||
| Anxiety (GAD-7) | 0–4 | No Anxiety | 93 | 62.0 |
| 5–9 | Mild | 16 | 10.7 | |
| 10–14 | Moderate | 12 | 8.0 | |
| ≥15 | Severe | 29 | 19.3 | |
| GAD-7 Mean ± SD | 5 ± 7 | |||
| PCL-5 | <33 | No PTSD | 133 | 88.7 |
| ≥33 | PTSD | 17 | 11.3 | |
| PCL-5 Mean ± SD | 10 ± 13 | |||
SD: standard deviation, ICU: intensive care unit, PHQ-9: Patient Health Questionnaire, GAD-7: Generalized Anxiety Disorder Questionnaire, PCL-5: Post Traumatic Stress Disorder Checklist for DSM-5.
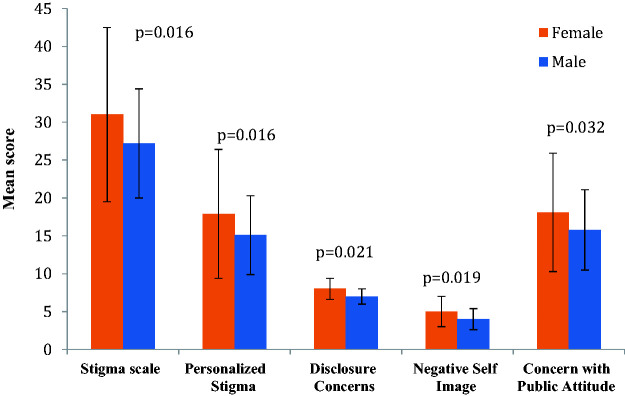
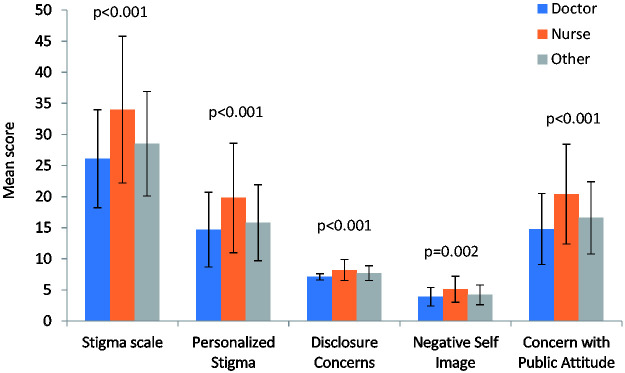
The total COVID-19-related stigma score was not significantly associated with sociodemographic or clinical characteristics other than female sex (31 ± 11.5, P = 0.016) and occupation as a nurse (26.1 ± 7.9, P < 0.001; Figures 1 and 2). A significant positive correlation was observed between the total COVID-19-related stigma score and the three psychological factors examined: the PHQ-9 score for depression, the GAD-7 score for anxiety, and the PCL-5 score for PTSD (r = 0.379, 0.361, and 0.374, respectively, P < 0.001).
Figure 1.
Perceived COVID-19-related stigma among HCWs in relation to sex.
Figure 2.
Perceived COVID-19-related stigma among HCWs in relation to occupation.
P ≤ 0.05 is considered statistically significant. Analysis using one-way ANOVA followed by pairwise comparisons; nurses were significantly different from the other groups.
Other occupations included technicians, administrative employees in faculty or hospital, pharmacists, nutritionists, laboratory specialists, and janitors.
Moderate-severe COVID-19-related stigma perception was significantly associated with occupation (P = 0.004) and place of treatment (P = 0.028; Table 5). Furthermore, moderate-severe COVID-19-related stigma perception was significantly associated with all psychological factors examined (P ≤ 0.001; Table 6).
Table 5.
Relationship between COVID-19-related stigma perception severity and basic sociodemographic and clinical data (n = 150).
| COVID-19-related stigma perception severity |
|||
|---|---|---|---|
| No-mild(n = 50) |
Moderate-severe(n = 100) |
||
| N (%) | N (%) | P-value | |
| Marital status | |||
| Without partner | 18 (41.9) | 25 (58.1) | 0.160 |
| With Partner | 32 (29.9) | 75 (70.1) | |
| Residency | |||
| Cairo | 27 (35.5) | 49 (64.5) | 0.615 |
| Giza | 21 (32.8) | 43 (67.2) | |
| Other | 2 (20.0) | 8 (80.0) | |
| Occupation | |||
| Doctor | 28 (48.3) | 30 (51.7) | 0.004 |
| Nurse | 8 (17.8) | 37 (82.2) | |
| Other* | 14 (29.8) | 33 (70.2) | |
| Chronic disease | |||
| No | 36 (33.6) | 71 (66.4) | 0.989 |
| Yes | 14 (32.6) | 29 (67.4) | |
| Smoking | |||
| No | 43 (31.6) | 93 (68.4) | 0.165 |
| Yes | 7 (50.0) | 7 (50.0) | |
| Directly involved in the care of COVID patients | |||
| No | 36 (36.0) | 64 (64.0) | 0.327 |
| Yes | 14 (28.0) | 36 (72.0) | |
| Place of treatment when infected with COVID | |||
| Home | 50 (36.5) | 87 (63.5) | 0.028 |
| Hospital ward | 0 | 11 (100.0) | |
| ICU | 0 | 2 (100.0) | |
| Need for mechanical ventilation | |||
| No | 50 (33.6) | 99 (66.4) | 1.000 |
| Yes | 0 (0.0) | 1 (100.0) | |
| Need for corticosteroids | |||
| No | 39 (36.8) | 67 (63.2) | 0.163 |
| Yes | 11 (25.0) | 33 (75.0) | |
*Other occupations included janitors, pharmacists, nutritionists, and laboratory specialists.
Table 6.
Relationship between COVID-19-related stigma perception severity and psychological findings.
| No-mild perceived stigma |
Moderate-severe perceived stigma |
||
|---|---|---|---|
| Median (range) | Median (range) | P-value* | |
| Depression (PHQ-9) | 4 (0–14) | 7 (0–21) | <0.001 |
| Anxiety (GAD-7) | 0 (0–15) | 4 (0–21) | 0.001 |
| PTSD (PCL-5) | 2 (0–19) | 6 (0–48) | <0.001 |
*P ≤ 0.05 was deemed a statistically significant analysis using the Mann–Whitney test.
Multiple linear regression using a multivariate analysis model showed that depression, anxiety, and female sex were the most significant predictors of COVID-19-related stigma perception (Table 7).
Table 7.
Multivariate linear regression for factors associated with COVID-19-related stigma perception.
| Unstandardized coefficients |
Standardized coefficients |
95.0% confidence interval for B |
|||||
|---|---|---|---|---|---|---|---|
| B | SE | Beta | T | P-value | Lower bound | Upper bound | |
| Constant | 24.55 | 1.17 | 20.94 | <0.001 | 22.2 | 26.9 | |
| Depression (PHQ-9) | 0.69 | 0.13 | 0.39 | 5.19 | <0.001 | 0.4 | 1.0 |
| Anxiety (GAD-7) | 0.53 | 0.11 | 0.37 | 4.79 | <0.001 | 0.3 | 0.8 |
| Sex (male/female) | −3.45 | 1.54 | −0.17 | −2.24 | 0.026 | −6.5 | −0.4 |
PHQ-9: Patient Health Questionnaire, GAD-7: Generalized Anxiety Disorder Questionnaire, SE: standard error.
Logistic regression indicated that occupation as a nurse (OR:3.56, CI: 1.30–9.74) and being diagnosed with PTSD symptoms (OR:1.07, CI: 1.03–1.12) carried more risk for developing moderate-severe COVID-19-related stigma perception.
Discussion
The current study investigated the level of COVID-19-related stigma perception and associated psychological challenges among a diverse sample of HCWs who were diagnosed positive for COVID-19 infection with reverse transcriptase-polymerase chain reaction testing at Cairo University hospitals during the second wave of the COVID-19 pandemic in Egypt.
Social stigmatization has always been an obstacle faced by HCWs during epidemics, especially those with the ambiguous nature and vast life-changing impact of the current COVID-19 pandemic. For example, during the SARS pandemic in Taiwan, feeling stigmatized and rejected by others was the most commonly reported finding among a sample of 338 HCWs.25
In our study, nearly 70% of HCWs reported moderate-to-severe COVID-19-related stigma perception despite, by the time of data collection, almost a year having passed since COVID-19 was declared a global pandemic by the World Health Organization and notwithstanding considerable national and international efforts to fight social stigma against HCWs.
These findings are consistent with another study of 424 healthcare professionals in New Delhi, India conducted from May to July 2020. Overall, 70% of participants perceived some form of stigma and a noticeable change in their community members’ behavior when HCWs were seen wearing their white coats or medical uniforms; more than 30% felt endangered and were hesitant to disclose their COVID-19 test results to others.26 Higher levels of stigmatization than in the New Delhi study were found in another study that explored perceived COVID-19-related stigma among Egyptian physicians between 7 to 21 June 2020.; 31.2% of 509 physicians reported severe levels and 64.2% reported moderate levels of perceived COVID-19-related stigma.7 The higher levels of perceived stigmatization documented in this study may be attributable to a difference in the timeline (the study was conducted during the first wave of the pandemic in Egypt) and may further be due to the undiversified study sample, which included only physicians.
In our study, the total COVID-19-related stigma score was significantly related to the female sex (31 ± 11.5, P = 0.016) and to nurses’ occupation (26.1 ± 7.9, P < 0.001) despite the inclusion of doctors and other healthcare professionals in the study. Similar results were documented by Zandifar et al., who reported that COVID-19-related stigma was more prevalent among females in an examination of a varied sample of 894 HCWs in Iran from March to April 2020.27 Moreover, Radhakrishnan et al. reported a significantly higher prevalence of stigmatizing experiences among nurses compared with doctors (P < 0.01).28 These findings are consistent with the results of Yufika et al., who observed that doctors reported considerably lower perception of COVID-19-related stigma compared with nurses in a sample of 288 HCWs.29 These higher levels of stigma perception repeatedly observed among nurses compared with levels in other HCWs can be attributed to the social misbehavior toward the nursing profession that is associated with higher internalized stigma.30 Furthermore, because of the nature of their work, nurses are always in closer contact with patients compared with other medical personnel; this results in nurses being labelled as potential carriers of infection.31
No significant association was observed in our study between the total COVID-19-related stigma score and other sociodemographic or COVID-19-related characteristics of the study sample. Contrary to our study, other studies have reported that high COVID-19-related stigma perception is associated with younger age, being married,32 and direct involvement in the care of COVID-19-positive patients.33
With regard to post-COVID-19 psychological impact, 58.0%, 38.0%, and 11.3% of participants experienced varying levels of depression, anxiety, and PTSD symptoms. The combination of being an HCW during the pandemic and a COVID-19 survivor—with its scientifically proven psychological sequalae34—may have produced these findings.
Studies investigating the psychological impact of the COVID-19 pandemic on HCWs have documented similar or even higher occurrences of psychological sequelae. For instance, a global study conducted from 20 April to 21 May 2020 with 2097 HCWs, most of whom belonged to low- and middle-income countries in the Eastern Mediterranean Region, reported prevalences of anxiety and depression of 60% and 53%, respectively.35 In addition, PTSD symptoms were documented among HCWs directly serving COVID-19 patients in more than a quarter (26.2%) of the study sample.36 Another study of a diverse sample of 262 HCWs from various Egyptian governorates reported that 98.5% of participants experienced moderate-to-severe stress, 90.5% experienced various degrees of anxiety, and 94% reported mild-to-severe depression.37 Becoming infected with COVID-19 was found to amplify the risk of developing negative mental health consequences among HCWs given that a higher prevalence of anxiety and depressive symptoms were detected in those previously infected than those who were not infected.38
In the present study, we observed that HCWs who experienced high levels of depression, anxiety, or post-traumatic stress symptoms were more likely to develop moderate-to-severe perceptions of COVID-19-related stigma because significant associations were found between high scores of all the psychological factors assessed—depression (P ≤ 0.001), anxiety (P = 0.001), and PTSD (P < 0.001)—and moderate-to-severely perceived COVID-19-related stigma.
Consistent with these findings, psychological ill-being and stress were associated with high stigma perception levels among HCWs in many other studies. For example, Teksin et al. evaluated mood disorders and their association with COVID-19 stigmatization among a sample of 452 HCWs. The authors reported a significant association between the perception of stigma and depression and anxiety scores.33 Moreover, Adhikari et al. investigated mental health outcomes and determinants of stigma among 213 HCWs during the same period as our study. The level of perceived social stigma was 57% and anxiety and depression were associated with positive stigma perception among respondents.39 Another study of Indian physicians serving in COVID-19-assigned hospitals reported a significant association between stigma and perceived stress scores.40
In the present study, having post-traumatic stress symptoms was the most significant predictor of moderate-to-severe COVID-19-related stigma perception, as detected by logistic regression models (P = 0.003, OR: 1.07, CI: 1.03–1.12). This finding was similar to the results of Zandifar et al., who documented a significant positive association between stigma and post-traumatic stress symptoms among a sample of 894 HCWs.27
Our findings provide strong evidence that despite continuous government efforts—including broad campaigns on local television channels and social media—to support Egyptian HCWs in their battle against the current pandemic through, social stigmatization and psychological challenges hinder Egyptian HCWs from doing their jobs.
Stigmatization against HCWs results in lower job satisfaction and increased occupational stress41, both of which negatively impact the medical task force's productivity.42 However, enhancing job satisfaction can help protect HCWs from mental stressors and buffer the substantial psychological burden of being a healthcare provider during the current pandemic.43 Because medical service providers across specialties represent the frontline defense against the COVID-19 pandemic, providing these workers with a healthy and supportive environment is important.44
To the best of our knowledge, most published studies have assessed the level of stigma perception among HCWs during only the first wave of the pandemic in Egypt. However, no study has continued to track this variable and the possible associated psychological challenges during the second pandemic wave and later.
Recommendations
Reported almost a year after the first COVID-19 case was discovered in Egypt, our findings should alert national authorities to provide better psychological care for HCWs and guide new strategies to improve the psychological resilience of the medical task force during the current and any future pandemic. Short- and long-term psychological care strategies should be applied in all medical care facilities; strategies must include regular psychological screening for all medical personnel and appropriate care for those who screen positive for any psychological issue both at the time of detection and at long-term follow-up. In addition, broad awareness campaigns are required to neutralize the stigma of psychological disease among the public and the HCW community and spread the concept of seeking psychological help when needed without shame or fear of judgment.
The main limitation of the study was that all participants were HCWs who were previously infected with COVID-19. Therefore, we were unable to determine whether these findings were entirely attributable to participants’ role as HCWs during the stressful period of the pandemic or whether findings were partially a psychological sequela for COVID-19 infection. Furthermore, contrary to the characteristics of other studies, the smaller sample size and the limited participation of other healthcare professionals in this study did not permit the generalization of results.
Conclusion
Despite governmental efforts, perceived social stigma among Egyptian healthcare workers still prevails and is associated with high levels of depression, anxiety, and post-traumatic stress symptoms.
Footnotes
The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Dalia Mohamed Gaber https://orcid.org/0000-0002-7847-8886
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Authors' contributions
DM analyzed and interpreted data collected from participants and was a major contributor to writing the manuscript. MM was responsible for writing the background section of the manuscript. AM was responsible for writing the methodology section. YS wrote the results section and MD was responsible for writing the discussion and conclusion sections. All authors read and approved the final manuscript.
Consent for publication
All data obtained were confidential and used only for research purposes. Approval for publication was obtained as a part of the consent to participate.
References
- 1.Zhou X, Li Y, Li T, et al. Follow-up of asymptomatic patients with SARS-CoV-2 infection. Clin Microbiol Infect 2020; 26: 957–959. Available from:/pmc/articles/PMC7271011/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020; 7: 611–627. Available from: www.thelancet.com/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luo Y, Chua CR, Xiong Z, et al. A Systematic Review of the Impact of Viral Respiratory Epidemics on Mental Health: An Implication on the Coronavirus Disease 2019 Pandemic. Front Psychiatry 2020; 11: 565098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses [Internet]. Brain Behav Immun 2020; 87: 18–22. Available from: https://pubmed.ncbi.nlm.nih.gov/32240762/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Villa S, Jaramillo E, Mangioni D, et al. Stigma at the time of the COVID-19 pandemic [Internet]. Clin Microbiol Infect 2020; 26: 1450–1452. Available from:/pmc/articles/PMC7411378/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdelhafiz AS, Alorabi M. Social Stigma: The Hidden Threat of COVID-19. Front Public Health 2020; 8: 429. Available from:/pmc/articles/PMC7484807/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mostafa A, Sabry W, Mostafa NS. COVID-19-related stigmatization among a sample of Egyptian healthcare workers. PLoS One 2020; 15: e0244172. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0244172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis 2020; 20: 782. Available from: http://www.thelancet.com/article/S1473309920304989/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramaci T, Barattucci M, Ledda C, et al. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustain [Internet] 2020; 12: 3834. Available from: https://www.mdpi.com/2071-1050/12/9/3834/htm. [Google Scholar]
- 10.Park JS, Lee EH, Park NR, et al. Mental Health of Nurses Working at a Government-designated Hospital During a MERS-CoV Outbreak: A Cross-sectional Study. Arch Psychiatr Nurs 2018; 32: 2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stigma spreads alongside COVID-19 in Egypt – Al-Monitor: the Pulse of the Middle East [Internet]. [cited 2021. Sep 15]. Available from: https://www.al-monitor.com/originals/2020/04/egypt-stigma-coronavirus-patients-recover-burial.html.
- 12.Virus turns health workers in Egypt into “outcasts” – World – The Jakarta Post [Internet]. [cited 2021. Sep 15]. Available from: https://www.thejakartapost.com/news/2020/04/21/virus-turns-health-workers-in-egypt-into-outcasts.html.
- 13.Do Duy C, Nong VM, Van AN, et al. COVID-19-related stigma and its association with mental health of health-care workers after quarantine in Vietnam [Internet]. Psychiatry Clin Neurosci 2020; 74: 566–568. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7404653/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573–577. [DOI] [PubMed] [Google Scholar]
- 15.Verma S, Mythily S, Chan YH, et al. Post-SARS psychological morbidity and stigma among general practitioners and traditional Chinese medicine practitioners in Singapore. Ann Acad Med Singapore 2004; 33: 743–748. [PubMed] [Google Scholar]
- 16.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Res Nurs Heal 2001; 24: 518–529. Available from: https://pubmed.ncbi.nlm.nih.gov/11746080/ [DOI] [PubMed] [Google Scholar]
- 17.Charles B, Jeyaseelan L, Pandian AK, et al. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India - a community based cross sectional study. BMC Public Health 2012; 12: 463. Available from: https://pubmed.ncbi.nlm.nih.gov/22720691/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–613. Available from: https://pubmed.ncbi.nlm.nih.gov/11556941/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.AlHadi AN, AlAteeq DA, Al-Sharif E, et al. An arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann Gen Psychiatry 2017; 16: 32. Available from: https://pubmed.ncbi.nlm.nih.gov/28878812/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sawaya H, Atoui M, Hamadeh A, et al. Adaptation and initial validation of the Patient Health Questionnaire – 9 (PHQ-9) and the Generalized Anxiety Disorder – 7 Questionnaire (GAD-7) in an Arabic speaking Lebanese psychiatric outpatient sample. Psychiatry Res 2016; 239: 245–252. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006; 166: 1092–1097. Available from: https://pubmed.ncbi.nlm.nih.gov/16717171/. [DOI] [PubMed] [Google Scholar]
- 22.Weathers FW, Litz BT, Keane TM, et al. The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. Vol. 5, National Center for PTSD. 2013. p. 3. [Google Scholar]
- 23.Ibrahim H, Ertl V, Catani C, et al. The validity of Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry 2018; 18: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng P, Xu LZ, Zheng WH, et al. Psychometric property study of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) in Chinese healthcare workers during the outbreak of corona virus disease 2019. J Affect Disord 2020; 277: 368–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bai YM, Lin CC, Lin CY, et al. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv 2004; 55: 1055–1057. [DOI] [PubMed] [Google Scholar]
- 26.Yadav K, Laskar AR, Rasania SK. A study on stigma and apprehensions related to COVID-19 among healthcare professionals in Delhi. Int J Community Med Public Heal 2020; 7: 4547. [Google Scholar]
- 27.Zandifar A, Badrfam R, Khonsari NM, et al. Prevalence and associated factors of posttraumatic stress symptoms and stigma among health care workers in contact with COVID-19 patients. Iran J Psychiatry 2020; 15: 340–350. Available from:/pmc/articles/PMC7610075/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Radhakrishnan RV, Jain M, Mohanty CR, et al. The perceived social stigma, self-esteem, and its determinants among the health care professionals working in India during COVID 19 pandemic. Med J Armed Forces India 2021; 77: S450–S458. Available from: 10.1016/j.mjafi.2021.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yufika A, Pratama R, Anwar S, et al. Stigma Associated with COVID-19 Among Health Care Workers in Indonesia. Disaster Med Public Health Prep 2020; 16: 1942–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hossain MB, Kippax S. HIV-related discriminatory attitudes of healthcare workers in Bangladesh. J Heal Popul Nutr 2010; 28: 199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhagavathula AS, Aldhaleei WA, Rahmani J, et al. Knowledge and perceptions of COVID-19 among health care workers: Cross-sectional study. JMIR Public Heal Surveill 2020; 6: e19160. Available from: https://pubmed.ncbi.nlm.nih.gov/32320381/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yuan Y, Zhao YJ, Zhang QE, et al. COVID-19-related stigma and its sociodemographic correlates: a comparative study. Global Health 2021; 17: 54. Available from: https://pubmed.ncbi.nlm.nih.gov/33962651/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teksin G, Uluyol OB, Onur OS, et al. Stigma-related Factors and their Effects on Health-care Workers during COVID-19 Pandemics in Turkey: A Multicenter Study. Sisli Etfal Hastan Tip Bul 2020; 54: 281–290. Available from:/pmc/articles/PMC7729714/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo Q, Zheng Y, Shi J, et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: A mixed-method study. Brain Behav Immun 2020; 88: 17–27. Available from: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Htay MNN, Marzo RR, AlRifai A, et al. Immediate impact of COVID-19 on mental health and its associated factors among healthcare workers: A global perspective across 31 countries. J Glob Health 2020; 10: 020381. Available from:/pmc/articles/PMC7649521/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Di Tella M, Romeo A, Benfante A, et al. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract 2020; 26: 1583–1587. Available from: https://pubmed.ncbi.nlm.nih.gov/32710481/. [DOI] [PubMed] [Google Scholar]
- 37.Aly HM, Nemr NA, Kishk RM, et al. Stress, anxiety and depression among healthcare workers facing COVID-19 pandemic in Egypt: A cross-sectional online-based study. BMJ Open 2021; 11: e045281. Available from: https://bmjopen.bmj.com/content/11/4/e045281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Braquehais MD, Vargas-Cáceres S, Gómez-Durán E, et al. The impact of the COVID-19 pandemic on the mental health of healthcare professionals [Internet]. QJM 2020; 113: 613–617. Available from: https://academic.oup.com/qjmed/article/113/9/613/5860843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Adhikari SP, Rawal N, Shrestha DB, et al. Prevalence of Anxiety, Depression, and Perceived Stigma in Healthcare Workers in Nepal During Later Phase of First Wave of COVID-19 Pandemic: A Web-Based Cross-Sectional Survey. Cureus 2021; 13: e16037. Available from:/pmc/articles/PMC8321677/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Uvais NA, Shihabudheen P, Hafi NAB. Perceived Stress and Stigma Among Doctors Working in COVID-19-Designated Hospitals in India. Prim Care Companion CNS Disord 2020; 22: 20br02724. Available from: https://www.psychiatrist.com/pcc/covid-19/covid-perceived-stress-and-stigma-among-doctors-in-india. [DOI] [PubMed] [Google Scholar]
- 41.Hernandez SHA, Morgan BJ, Parshall MB. Resilience, stress, stigma, and barriers to mental healthcare in U.S. Air Force Nursing Personnel. Nurs Res 2016; 65: 481–486. Available from:/pmc/articles/PMC5091011/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Said RM, El-Shafei DA. Occupational stress, job satisfaction, and intent to leave: nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ Sci Pollut Res Int 2020; 28: 8791–801. Available from: https://link.springer.com/article/10.1007/s11356-020-11235-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hoboubi N, Choobineh A, Kamari Ghanavati F, et al. The Impact of Job Stress and Job Satisfaction on Workforce Productivity in an Iranian Petrochemical Industry. Saf Health Work 2017; 8: 67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hennein R, Mew EJ, Lowe SR. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS One 2021; 16: e0246602. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0246602. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.