Abstract
Background:
Little is known about injuries to the adductor magnus (AM) muscle and how to manage them.
Purpose:
To describe the injury mechanisms of the AM and its histoarchitecture, clinical characteristics, and imaging features in elite athletes.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 11 competitive athletes with an AM injury were included in the study. Each case was clinically assessed, and the diagnosis and classification were made by magnetic resonance imaging (MRI) according to the British Athletics Muscle Injury Classification (BAMIC) and mechanism, location, grade, and reinjury (MLG-R) classification. A 1-year follow-up was performed, and return-to-play (RTP) time was recorded.
Results:
Different mechanisms of injury were found; most of the athletes (10/11) had flexion and internal rotation of the hip with extension or slight flexion of the knee. Symptoms consisted of pain in the posteromedial (7/11) or medial (4/11) thigh during adduction and flexion of the knee. Clinically, there was a suspicion of an injury to the AM in only 3 athletes. According to MRI, 5 lesions were located in the ischiocondylar portion (3 in the proximal and 2 in the distal myoconnective junction) and 6 in the pubofemoral portion (4 in the distal and 2 in the proximal myoconnective junction). Most of the ischiocondylar lesions were myotendinous (3/5), and most of the pubofemoral lesions were myofascial (5/6). The BAMIC and MLG-R classification coincided in distinguishing injuries of moderate and mild severity. The management was nonoperative in all cases. The mean RTP time was 14 days (range, 0-35 days) and was longer in the ischiocondylar cases than in the pubofemoral cases (21 vs 8 days, respectively). Only 1 recurrence, at <10 months, was recorded.
Conclusion:
Posteromedial thigh pain after an eccentric contraction during forced adduction of the thigh from hip internal rotation should raise a suspicion of AM lesions. The identification of the affected portion was possible on MRI. An injury in the ischiocondylar portion entailed a longer RTP time than an injury in the pubofemoral portion.
Keywords: adductor magnus injury, BAMIC and MLG-R classification, hip, MRI, pelvis, thigh
Adductor complex injuries account for 10% to 16% of injuries in sports with frequent eccentric loads, particularly soccer. 7,18,24 This muscle group is the second group most likely to be injured in these sports, accounting for 20% to 25% of all muscle injuries. 7
After the Doha agreement, 35 lesions to the adductor muscle group were included in the category of causes of groin pain, specifically adductor-related groin pain (ARGP). 11 With ARGP, the most commonly injured muscle is the adductor longus (AL) at the level of the proximal or distal musculotendinous junction (MTJ). 30 However, the literature focuses more frequently on lesions that affect the AL insertion because of their controversial and optional surgical treatment. 4,6,28,29 References to injuries to other adductor muscles are practically anecdotal in the literature. 1,26,37 Indeed, there are very few published studies that refer to isolated injuries of the adductor magnus (AM) muscle. 12,17,21,23,30
Anatomy and Function of the AM
The AM is a complex muscle with a triangular appearance that is located in the medial and posterior compartments of the thigh and is part of the adductor muscles of the hip. It is located next to the adductor brevis in a plane deep to the muscular wall formed by the pectineus, the AL, and the gracilis. After the gluteus maximus, it is the heaviest muscle with the largest cross-sectional area of the lower extremity. 14,33
The AM is divided into an adductor (pubofemoral) portion and an ischiocondylar portion 15,25 (Figure 1). The former is innervated by the obturator nerve, whereas the latter is innervated by the sciatic nerve. The pubofemoral portion originates proximally from the inferior pubic ramus and ischial ramus, while the ischiocondylar portion has its origin lateral to the pubofemoral portion and inferior and medial to the conjoint and semimembranosus tendons of the hamstring 25 (Figure 2).
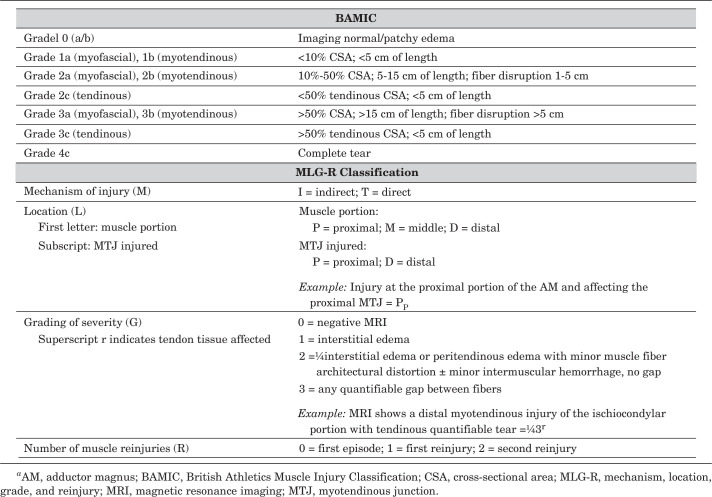
Figure 1.
Diagrams of (A) anterior and (B) posterior views of the adductor magnus, showing the pubofemoral (a) and ischiocondylar (b) portions.
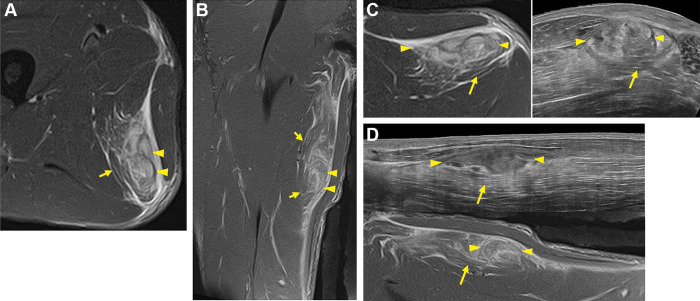
Figure 2.
(A) Diagram of the insertions of the pubofemoral portion (blue) and ischiocondylar portion (red) of the adductor magnus (AM) in the ischiopubic ramus and ischial tuberosity as well as the hamstring (green) in the ischial tuberosity. (B) Diagram of the lateral view of the AM, demonstrating the pubofemoral (a) and ischiocondylar (b) portions.
The most proximal pubofemoral fibers follow a more horizontal direction and can be defined as the smaller and anterior portion of the muscle called the adductor minimus. 15 The distal attachment of the adductor portion reaches the linea aspera and blends with the proximal attachment of the short head of the biceps femoris muscle. This combination of the adductor portion and the short head of the biceps femoris allows the 2 muscles to work in a coordinated manner as stabilizers of the femur and pelvis. 15
The ischiocondylar or hamstring portion of the AM is so named because of its similarity in structure, proximal insertion, and common innervation to the hamstring muscles. 15,32 It is nearly vertical in orientation, extending from the ischial tuberosity to the adductor tubercle on the medial femoral condyle and through fibrous attachments to the supracondylar line of the femur.
This complex structure allows us to identify, in the AM, a proximal MTJ and a distal MTJ of the adductor portion as well as a proximal MTJ and a distal MTJ of the ischiocondylar portion. Both portions of the AM are adductors of the thigh; however, the pubofemoral portion is also a hip flexor (mainly at the expense of more proximal fibers), and the ischiocondylar portion is also a hip extensor (when the hip is in maximum flexion). These functions diminish as the hip approaches neutral positions. 19 These 2 portions of the muscle also work synergistically during the gait cycle and control the pelvis for postural stabilization.
According to Jeno and Schindler, 15 the AM can be compared with the deltoid muscle: although its function as a whole is to adduct the thigh, a part flexes it and functions as a medial rotator, while the other extends it and acts as a side rotator. Thus, on one hand, the most superior segment of the pubofemoral portion (along with the fibers from the short head of the biceps femoris) focuses its main activity on pelvic stabilization 15 ; on the other hand, the rest of the muscle, with longer fibers, performs thigh mobilization activities through its lever arm. 32
In this work, we wanted to examine our experience of AM injuries and their different locations in a group of athletes without ruling out causal relationships with other factors. Therefore, the purpose of our study was to present our series of isolated tears of the AM in high-level athletes. We hypothesized that an AM injury presents with pain not only in the medial aspect of the thigh but also in the posteromedial aspect; by using magnetic resonance imaging (MRI), we can define which portion of the AM (pubofemoral or ischiocondylar) is injured and which injuries in the ischiocondylar portion portend a longer return-to-play (RTP) time.
Methods
Participants
Included were high-level athletes who were diagnosed with an AM injury between October 2011 and February 2021. The protocol for this study was approved by the ethics committee for clinical research of the Catalan Sports Council, and written informed consent was obtained from all included participants.
The study athletes were aged 18 to 36 years and participated in competitive sports. We included athletes who presented with pain in the medial or posteromedial aspect of the thigh during their sports activity (training or matches) and had MRI scans that confirmed an AM injury within 4 days of the injury. We excluded all injuries to the AM caused by direct trauma (eg, racket contusion, kick, hit by a pitch).
Characteristics recorded included athlete age, weight, height, sport, laterality, affected limb, limb dominance, thigh aspect affected and mechanism of injury. Limb dominance was indicated by the hand or foot body segment that performs the function of support or impulse in movement in which force, dexterity, or precision is required. 2
Clinical Examination
A clinical examination was performed by 3 physicians (R.B., X.V., Á.R-C.), each with more than 20 years of experience in sports medicine. The examination consisted of palpation of the affected area to localize the pain and identify its level (proximal, middle, or distal third of the thigh) and the affected part of the thigh (medial, posterior, or posteromedial). In all cases, we performed assisted passive stretching of both the adductor and the hamstring muscles. Stretching was led fully by the physician so that the patient was able to relax his or her body in the position. We performed hip flexion for the hamstring and hip adduction for the adductors to allow the weight of gravity to release the explored muscles in each stretch.
Each assisted stretch was compared with that of the contralateral limb to assess the limitations of the injured limb’s range of motion. We also performed isometric, concentric, and eccentric maneuvers of the main muscle groups, especially the hamstring and adductors (adductor squeeze test). For the squeeze test, the hip joint was maintained at 45° of flexion, and the knee joint was at 90° of flexion. In this position, assisted by a clinician, the patient performed an isometric contraction and reported the area of pain. 5 In all cases, a diagnosis of an AM injury was made and included in our analysis.
MRI Assessment
MRI was performed after the injury. Except for the first 3 patients, MRI was conducted on a 3-T Vantage Titan (Canon Medical Systems) using various sequences: axial, sagittal, and coronal T2-weighted fat-saturated images (repetition time, 5200, 5000, and 3700 ms; echo time, 44-60 ms; slice thickness, 2.5-3.5 mm; field of view, 256 × 256, 192 × 272, and 288 × 320 mm) and axial and coronal T1-weighted turbo spin echo images (repetition time, 900-980 ms; echo time, 11 ms; slice thickness, 2.5-3.5 mm; field of view, 352 × 352 and 288 × 320 mm). For muscle MRI, it is recommended to perform fluid-sensitive sequences (T2-weighted in our case) with an intermediate TE (eg, <65 ms) to obtain adequate contrast and spatial resolution of connective tissue. 8,13
A radiologist with 12 years of experience in musculoskeletal MRI (S.M.) and a physician with 6 years of experience in musculoskeletal MRI (M.B.) independently reviewed and evaluated the MRI scans and categorized the lesions in relation to their histoarchitecture and the affected MTJ. 31 They also recorded the existence of previous scars in the AM, the loss of tension and loss of pennation angle, and the presence of a hematoma. Each lesion was classified according to 2 systems: the British Athletics Muscle Injury Classification (BAMIC) 27 and the mechanism, location, grade, and reinjury (MLG-R) classification developed by the Football Club Barcelona–Aspetar–Duke University 34 (Figure 3). In cases of a discrepancy between the 2 observers, the images were reviewed by the observers and 2 physicians with more than 30 years of experience in muscle injury imaging (R.B., G.R.) until a consensus was reached.
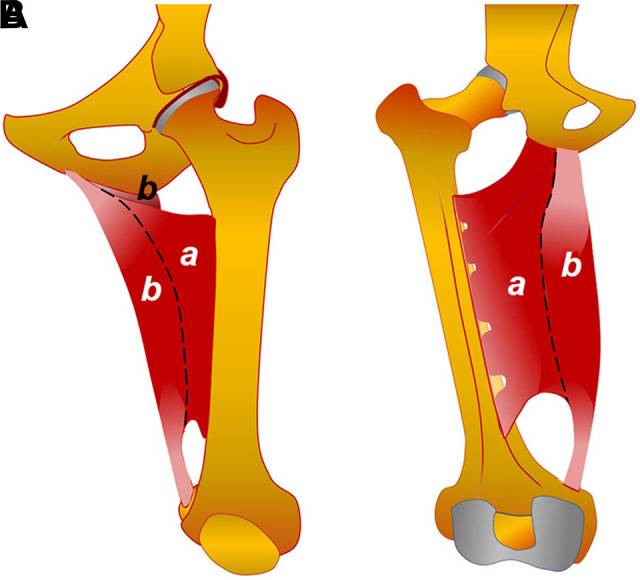
Figure 3.
Treatment, RTP Time, and Reinjury Evaluation
Gradual RTP was instituted under the supervision of 3 physicians (R.B., X.V., Á.R-C.). All injured athletes underwent a standardized rehabilitation program inspired by the rehabilitation protocol of hamstring injuries. 9,20 The rehabilitation program was divided into 4 phases:
Acute phase: gait normalization and rest-ice-compression-elevation.
Range of motion and strength phase: painless recovery of range of motion, starting with concentric training and progressing to eccentric training.
Functional phase: controlled lower extremity loading and return to running activities, sport-specific training and agility exercises (service games for tennis players and explosive runs and jumps for the rest of the athletes), and plyometric training.
RTP phase: When the patient completed the rehabilitation process, he or she began training on the playing surface (individual sports) or with the team. The decision of RTP was made when there was little chance of a reinjury. Objective criteria were used such as a clinical and physical examination without any limitations and functional criteria such as an isokinetic strength test.
Athletes needed to be pain-free before they could progress to the next phase. Treatment with nonsteroidal anti-inflammatory drugs was not performed in any patient, and treatment with local injections was not necessary in any patient. The duration of each phase varied according to the severity of the injury and the response of the athlete. Furthermore, care was taken to avoid detraining during the rehabilitation period by engaging in cardiovascular fitness, maintaining motor control skills when possible, and ensuring good hydration and nutrition of the athlete. The RTP time was recorded, and an update on reinjuries was performed through a telephone interview (November to December 2021).
Results
Participants
A total of 11 athletes with a diagnosed AM injury were included in the study. Patient data are provided in Table 1. Overall, 6 athletes were high-level tennis players (all ranked within the top 100 players of the Association of Tennis Professionals or the Women’s Tennis Association), 3 were professional soccer players, 1 was a professional shot putter, and 1 was a professional fencer. Most athletes were right-handed (82%); however, the more affected limb was the left (73%). The nondominant leg was involved in 6 of the 11 patients.
Table 1.
Characteristics of Study Athletes (N = 11) a
| Value | |
|---|---|
| Age, y | 24 ± 5 (18-31) |
| Height, cm | 1.8 ± 0.1 (162-194) |
| Weight, kg | 74.0 ± 7.8 (58-85) |
| Body mass index | 22.7 ± 0.8 (21.6-24.7) |
| Sex | |
| Female | 4 (36.4) |
| Male | 7 (63.6) |
| Sport | |
| Tennis | 6 (54.5) |
| Soccer | 3 (27.3) |
| Shot put | 1 (9.1) |
| Fencing | 1 (9.1) |
| Limb dominance | |
| Right | 9 (81.8) |
| Left | 2 (18.2) |
| Affected limb | |
| Right | 3 (27.3) |
| Left | 8 (72.7) |
| Affected aspect of thigh | |
| Medial | 4 (36.4) |
| Posteromedial | 7 (63.6) |
| Injury mechanism | |
| Slide on playing surface | 4 (36.4) |
| Loading | 3 (27.3) |
| Tennis serve | 3 (27.3) |
| Progressive pain | 1 (9.1) |
a Data are reported as mean ± SD (range) or n (%).
Various mechanisms of injury were recorded. In most patients, the injury occurred acutely during an opening of the limbs, either under loading (patients 1, 2, and 10) or during a slide on the playing surface (patients 6, 7, 9, and 11). In 3 tennis players (patients 4, 5, and 8), the mechanism of injury was the end of the service motion, just at the moment of placing the ipsilateral limb on the ground. In the case of sliding, it was affected the contralateral limb. Finally, patient 3 had progressive tenderness of the medial aspect of the thigh during training sessions and soccer matches for 1 week.
Clinical Examination
In 7 patients, pain was located at the posteromedial aspect of the thigh, while in 4 patients, it was located at the medial aspect. In 5 patients, pain was located in the middle third; in 4 patients, it was proximal; and in 2 patients, the location was broader, affecting the proximal and middle areas. Most athletes presented with pain in both adduction and flexion of the knee. The squeeze test findings at full knee extension (180°) and at 90° of knee flexion were positive for the entire sample. With this exploration, the clinician guided the diagnosis toward a hamstring strain in 5 patients, an AL injury in 3 patients, and an AM rupture in the remaining 3 patients. With these suspected diagnoses, MRI was requested.
MRI Assessment
The main MRI findings are presented in Table 2. AM injuries were diagnosed via MRI in all athletes: 5 were located in the ischiocondylar portion, of which 3 affected the proximal myoconnective junction (Figure 4) and 2 affected the distal myoconnective junction (Figures 5 and 6), and 6 were located in the pubofemoral portion, of which 2 affected the proximal myoconnective junction (Figure 7) and 4 affected the distal myoconnective junction (Figure 8). The ischiocondylar lesions had greater involvement of the myotendinous connective structure, while the pubofemoral lesions mainly had myofascial involvement. In 3 patients with ischiocondylar lesions, there was an alteration in tendon tension, which never occurred with pubofemoral injuries. In all except patient 3, there was an alteration in the pennation angle. Of the 5 instances in which a clear hematoma was observed, 3 injuries were localized in the ischiocondylar portion and 2 in the pubofemoral portion.
Table 2.
MRI Findings and RTP Times a
| Anatomic and Histoarchitecture Findings | Injury Classification | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Sport | Anatomic Portion Affected | MTJ Involved | Loss of Tension | Loss of Pennation Angle | Hematoma | Fibrosis/Scar | BAMIC | MLG-R | RTP Time, d |
| 1 | Soccer | Pubofemoral | Distal | No | Yes | No | No | 1a | I Pd 3 0 | 8 |
| 2 | Shot put | Ischiocondylar | Distal | Yes | Yes | No | No | 2b | I Dd 3r 0 | 6 |
| 3 | Soccer | Pubofemoral | Proximal | No | No | No | No | 1a | I Pp 2 0 | 0 |
| 4 | Tennis | Ischiocondylar | Proximal | Yes | Yes | No | Yes | 2c | I Pp 3r 0 | 17 |
| 5 | Tennis | Ischiocondylar | Distal | No | Yes | Yes | No | 3a | I Md 3 0 | 25 |
| 6 | Tennis | Pubofemoral | Distal | No | Yes | Yes | No | 2a | I Pd 3 0 | 19 |
| 7 | Tennis | Pubofemoral | Distal | No | Yes | Yes | No | 2b | I Pd 3 0 | 10 |
| 8 | Tennis | Ischiocondylar | Proximal | Yes | Yes | Yes | No | 2c | I Pp 3r 0 | 35 |
| 9 | Tennis | Pubofemoral | Proximal | No | Yes | No | No | 2a | I Mp 3 0 | 10 |
| 10 | Soccer | Pubofemoral | Distal | No | Yes | No | No | 1a | I Pd 3 0 | 3 |
| 11 | Fencing | Ischiocondylar | Proximal | No | Yes | Yes | No | 2b | I Pp 3 0 | 21 |
a BAMIC, British Athletics Muscle Injury Classification; MLG-R, mechanism, location, grade, and reinjury; MRI, magnetic resonance imaging; MTJ, myotendinous junction; RTP, return to play.
Figure 4.
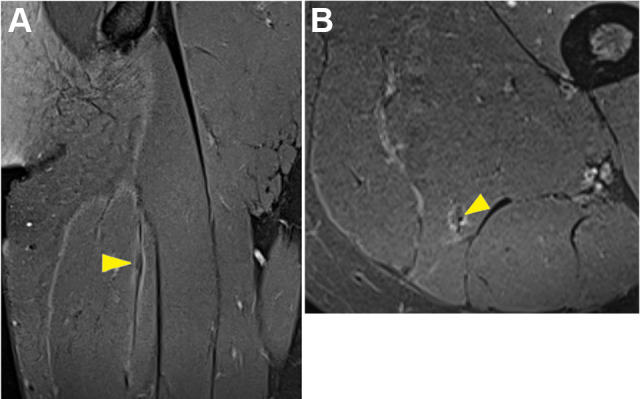
Tennis player (patient 4) with a proximal tendinous injury of the ischiocondylar portion. (A) Coronal and (B) axial T2-weighted fat-saturated magnetic resonance imaging of scarring on the proximal tendon of the ischiocondylar portion (arrowheads). Injury rating: I Pp 3r 0 (according to MLG-R classification) and 2c (according to British Athletics Muscle Injury Classification).
Figure 5.
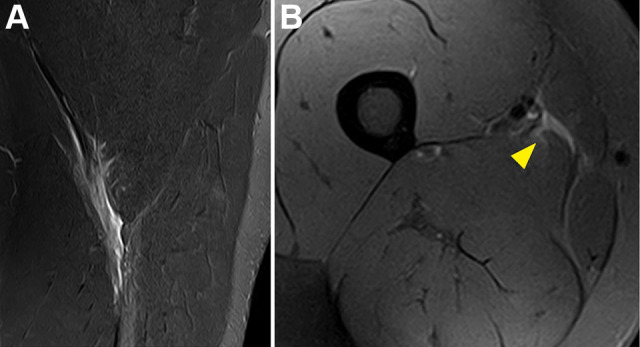
Shot putter (patient 2) with a distal myotendinous injury of the ischiocondylar portion. (A) Sagittal and (B) axial T2-weighted fat-saturated magnetic resonance imaging of tearing of the distal musculotendinous junction (arrowhead), with the loss of pennation angle and interstitial and intermuscular edema. Injury rating: I Dd 3r 0 (according to MLG-R classification) and 2b (according to British Athletics Muscle Injury Classification).
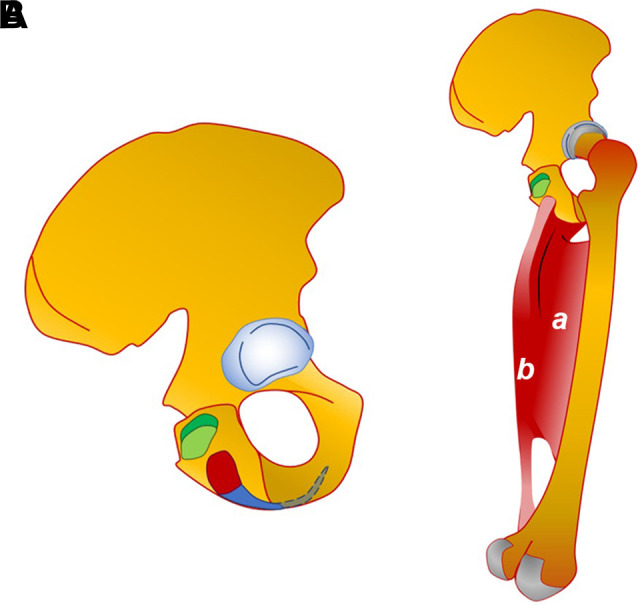
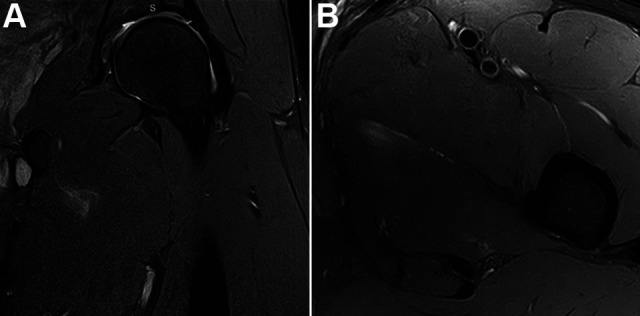
Figure 6.
Tennis player (patient 5) with a distal myofascial injury of the ischiocondylar portion. (A) Coronal and (B) axial T2-weighted fat-saturated magnetic resonance imaging (MRI) of an extensive hematoma (arrowheads), with the surrounding fibers displaced and interstitial edema (arrows). (C) Short-axis view of ultrasound with the corresponding MRI section and (D) panoramic view of ultrasound. Injury rating: I Md 3 0 (according to MLG-R classification) and 3a (according to British Athletics Muscle Injury Classification).
Figure 7.
Soccer player (patient 3) with a proximal myofascial injury of the pubofemoral portion. (A) Coronal and (B) axial T2-weighted fat-saturated magnetic resonance imaging of blurred muscle fibers and mild intermuscular edema. Injury rating: I Pp 2 0 (according to MLG-R classification) and 1a (according to British Athletics Muscle Injury Classification).
Figure 8.
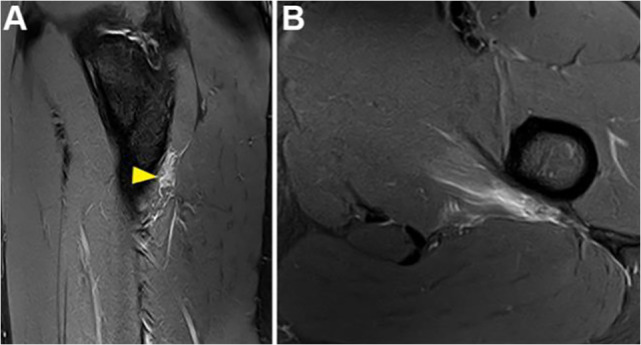
Soccer player (patient 1) with a distal myofascial injury of the pubofemoral portion. (A) Sagittal and (B) axial T2-weighted fat-saturated magnetic resonance imaging of tearing of the distal musculotendinous junction (arrowhead), with the loss of pennation angle and interstitial and intermuscular edema. Injury rating: I Pd 3 0 (according to MLG-R classification) and 1a (according to British Athletics Muscle Injury Classification).
The MRI reviewers only presented a discrepancy in 1 patient (patient 5; see Figure 6). The large hematoma made it difficult to rule out the loss of tension in the distal tendon of the ischiocondylar portion. After a discussion with the most experienced physicians, it was ruled out.
Treatment, RTP Time, and Reinjury Evaluation
In all athletes, the management was nonsurgical. Except in 2 patients (patients 3 and 10), an initial rest from sports of 48 hours and the application of ice were prescribed. All the athletes passed the rehabilitation phases without difficulty. In patient 5, during the acute phase, crutches were used. The mean RTP time was 14 days (range, 0-35 days), as shown in Table 3. Specifically, a mean RTP time of 21 days (range, 6-35 days) was reported for ischiocondylar injuries, whereas pubofemoral injuries had a mean RTP time of 8 days (range, 0-19 days). Through a telephone survey of the athletes, we identified a single case of recurrence in a year (patient 8). This reinjury required an RTP time of 3 weeks .
Discussion
The major finding of this series of 11 AM lesions was that there are 2 types of strain injuries of the AM: in the ischiocondylar portion or the pubofemoral portion. The mechanism of injury was flexion and internal rotation of the hip with extension of the knee. Symptoms consisted of pain in the posteromedial or medial aspect of the thigh. The athletes returned to sports at 2 to 3 weeks after the injury, but an ischiocondylar injury had a longer RTP time than a pubofemoral one.
The AM has an important role in stabilizing the hip and pelvis in hip flexion positions. 19 This occurs during sports-specific actions such as lateral sliding on the playing surface with the extremities open in flexion and internal rotation of the hip or opening of the thigh under loading. In all but 1 patient (patient 3), injuries occurred when the hip was in flexion and the knee was in internal rotation with extension or slight flexion. These situations occurred at the end of a tennis serve (3 patients), during a lateral slide on the playing surface (3 in tennis and 1 in fencing), or while load bearing with the thighs open (2 in soccer and 1 in shot put).
Of the 11 patients, 6 were tennis players of a very high level who were injured during the service motion or while sliding on the playing surface. In the case of serving, the affected limb was ipsilateral, whereas in the case of sliding, it was contralateral. The sliding injuries mainly occurred on a clay tennis court, where this type of movement is common. Injuries that occurred during serves were ischiocondylar, while the ones that occurred while sliding were pubofemoral. The injuries during serves occurred in the ipsilateral extremity at the end of the gesture, when the hip was flexed and internally rotated and the player initiated extension. In this position, the hip extensor moment of the AM is more effective than that of the hamstring or gluteus maximus, 19 and most likely, this is the specific position responsible for isolated AM injuries during the tennis service motion.
AM lesions should not be considered solely in the case of groin pain, but they may have more distal involvement, with pain in the posteromedial or medial aspect of the thigh. In a study of 111 adductor injuries, Serner et al 30 identified the following distribution: 62 were in the AL, 18 in the adductor brevis, 17 in the pectineus, 9 in the obturator externus, 4 in the gracilis, and only 1 in the AM. The study by Serner et al only counted adductor injuries with groin pain; therefore, they only found 1 patient with an AM injury.
In 5 patients, the injury affected the ischiocondylar portion; in 4 of them, the initial diagnosis (after a clinical evaluation) was a hamstring strain. Because the AM shares common innervation and actions with the major hamstring tendons, this structure is considered to be part of the hamstring muscle complex 16,22,25 ; therefore, Broski et al 3 called it the “mini-hamstring.” Moreover, it has been described that in 6% of the cases of complete avulsion of the hamstring, there is an associated detachment of the ischiocondylar portion of the AM. 3 Probably because of this, it is relatively easy to confuse an AM injury with a hamstring injury. In addition, as AM lesions do not generally present with severe symptoms, MRI is not performed, and they are erroneously classified as hamstring injuries. In the series presented, as athletes were professional, MRI was quickly performed. A diagnosis of this type of injury is more frequently made initially by MRI, which is an imaging technique that is not usually the first diagnostic step in cases of recreational athletes. In recreational athletes, this injury is probably underdiagnosed. In our opinion, ultrasound has become an essential tool in sports medicine care. In most consultations for muscle injuries, ultrasound is performed as the first diagnostic method. In the future, better knowledge of the anatomy may lead to the better utilization of ultrasound and, with it, a better diagnosis of this injury, even in recreational athletes.
As was mentioned previously, AM injuries could be observed and localized in the pubofemoral or ischiocondylar portion. In 6 patients, the lesion was located in the pubofemoral portion. In previous literature, only Kuhlmann et al 17 described an AM rupture with involvement of the pubofemoral portion. Once the injury was identified by location in the correct muscle and portion, it was assessed with the BAMIC 27 : 7 of 11 patients had grade 2 (moderate) injuries, and 3 of 11 had grade 1 (small) injuries. Regarding the location (site), 3 of 11 were myotendinous (“b”), and 6 of 11 were myofascial (“a”). Similar observations were made by using the MLG-R classification. 34 In this case, most injuries (8/11) were located in the proximal third of the muscle, being easily confused for injuries that affect the proximal third of the hamstring. Although they were located in the proximal third, the subscript “d,” corresponding to the distal MTJ, was recorded in 6 of 11 cases. In 4 of these cases, the subscript “d” involved the pubofemoral portion. Anatomically, these injuries were located further away from the proximal origin of the muscle and in the thickness of the muscular body. In 10 of 11 patients, injuries were classified as grade 3, which suggests structural lesions with a distortion of the architecture of 11% to 25% of the cross-sectional area and thus considered moderate or small lesions according to the BAMIC.
Injuries that comprise ARGP have a mean RTP time of about 14 days, which represents approximately half the recovery time of pubic-related groin pain or inguinal-related groin pain. 10,36 In our series, the mean RTP time was 14 days, similar to the RTP time of ARGP. Although the number of patients was small and reliable statistical analysis could not be performed, the mean RTP time of ischiocondylar injuries was clearly longer than the mean RTP time of pubofemoral injuries: 21 versus 8 days, respectively. One explanation for this difference is that injuries of the ischiocondylar portion had more myotendinous connective structures affected than those of the pubofemoral portion, which affected myofascial structures.
Lesions involving the AM are usually well tolerated in our experience, and perhaps for this reason, they are underdiagnosed. In our series, patient 4 showed a scar in the proximal tendon of the ischiocondylar portion (Figure 4). This athlete reported discomfort during the service motion a few weeks before the medical consultation, but the symptoms were well tolerated. We assumed that the scar was from an injury that had occurred during the period of discomfort. Moreover, the telephone interview only registered 1 case of a reinjury (patient 8) that was resolved in 3 weeks and without any sequelae.
Limitations
The main limitations of this study are the small number of patients and its retrospective design. Nevertheless, this is the first study presenting a series of AM injuries in athletes and describing 2 types of them—ischiocondylar and pubofemoral—on the basis of the complex anatomic structure of this muscle.
Conclusion
Sports medicine specialists and team physicians should be more aware of AM injuries. Posteromedial thigh pain after an eccentric contraction during forced adduction of the thigh from hip internal rotation should raise a suspicion of AM lesions. Using MRI, we can identify properly the portion affected. An injury in the ischiocondylar portion entailed a longer RTP time than an injury in the pubofemoral portion.
Footnotes
Final revision submitted September 10, 2022; accepted September 13, 2022.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Catalan Sports Council (No. 042/CEICGC/2021).
References
- 1. Attarian DE. Isolated acute hip adductor brevis strain. J South Orthop Assoc. 2000;9(3):213–215. [PubMed] [Google Scholar]
- 2. Ballestero E, Duran C, Planas A, López Bedoya J, Vernetta M. Fuerza y dominancia lateral. Apunts Sports Med. 1997;1(47):74–80. [Google Scholar]
- 3. Broski SM, Murthy NS, Krych AJ, Obey MR, Collins MS. The adductor magnus “mini-hamstring”: MRI appearance and potential pitfalls. Skeletal Radiol. 2016;45(2):213–219. [DOI] [PubMed] [Google Scholar]
- 4. Chopra A, Robinson P. Imaging athletic groin pain. Radiol Clin North Am. 2016;54(5):865–873. [DOI] [PubMed] [Google Scholar]
- 5. Delahunt E, Kennelly C, McEntee BL, Coughlan GF, Green BS. The thigh adductor squeeze test: 45° of hip flexion as the optimal test position for eliciting adductor muscle activity and maximum pressure values. Man Ther. 2011;16(5):476–480. [DOI] [PubMed] [Google Scholar]
- 6. Dimitrakopoulou A, Schilders EM, Talbot JC, Bismil Q. Acute avulsion of the fibrocartilage origin of the adductor longus in professional soccer players: a report of two cases. Clin J Sport Med. 2008;18:167–169. [DOI] [PubMed] [Google Scholar]
- 7. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–1232. [DOI] [PubMed] [Google Scholar]
- 8. Ekstrand J, Healy JC, Waldén M, Lee JC, English B, Hägglund M. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br J Sports Med. 2012;46:112–117. [DOI] [PubMed] [Google Scholar]
- 9. Futbol Club Barcelona Medical Services. Clinical practice guide for muscle injuries: epidemiology, diagnosis, treatment and prevention. Version 4.5. Apunts Sports Med. 2009;164:179–203. [Google Scholar]
- 10. Hallén A, Ekstrand J. Return to play following muscle injuries in professional footballers. J Sports Sci. 2014;32(13):1229–1236. [DOI] [PubMed] [Google Scholar]
- 11. Heijboer WMP, Weir A, Delahunt E, et al. A Delphi survey and international e-survey evaluating the Doha agreement meeting classification system in groin pain: where are we 5 years later? J Sci Med Sport. 2022;25(1):3–8. [DOI] [PubMed] [Google Scholar]
- 12. Iqbal A, Kalia S, Beale D, James SL, Botchu R. Isolated distal adductor magnus tendon avulsion as a rare cause of medial knee pain: a case report. Indian J Radiol Imaging. 2020;30(4):507–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Isern-Kebschull J, Mechó S, Pruna R, et al. Sports-related lower limb muscle injuries: pattern recognition approach and MRI review. Insights Imaging. 2020;11:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ito J, Moriyama H, Inokuchi S, Goto N. Human lower limb muscles: an evaluation of weight and fiber size. Okajimas Folia Anat Jpn. 2003;80(2-3):47–55. [DOI] [PubMed] [Google Scholar]
- 15. Jeno SH, Schindler GS. Anatomy, bony pelvis and lower limb, thigh adductor magnus muscles. In: StatPearls. NCBI Bookshelf. StatPearls Publishing; 2020:1-4. [PubMed] [Google Scholar]
- 16. Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics. 2005;25(3):571–586. [DOI] [PubMed] [Google Scholar]
- 17. Kuhlmann JN, Kirsch JM, Mimoun M, Baux S. Traumatic rupture of the great adductor (adductor magnus): apropos of a case. Article in French. Rev Chir Orthop Reparatrice Appar Mot. 1986;72:317–319. [PubMed] [Google Scholar]
- 18. Lynch SA, Renstrom PA. Groin injuries in sport: treatment strategies. Sports Med. 1999;28:137–144. [DOI] [PubMed] [Google Scholar]
- 19. Mallac C. Adductor magnus: tales of tightness. Sports Injury Bulletin. Accessed February 20, 2021. https://www.sportsinjurybulletin.com/anatomy/anatomy/adductor-magnus-tales-of-tightness
- 20. Malliaropoulos N, Papalexandris S, Papalada A, Papacostas E. The role of stretching in rehabilitation of hamstring injuries: 80 athletes follow-up. Med Sci Sports Exerc. 2004;36(5):756–759. [DOI] [PubMed] [Google Scholar]
- 21. Martin T, Louis R, Corinne B, Antoine L, Nathan D. Spontaneous hip adductor haematoma. J Pediatr Surg Case Rep. 2020;60:101568. [Google Scholar]
- 22. Martini F, Timmons MJ, Tallitsch RB. Human Anatomy. Pearson Benjamin Cummings; 2012. [Google Scholar]
- 23. McNeilan RJ, Rose M, Mei-Dan O, Genuario J. Open repair of acute proximal adductor magnus avulsion. Arthrosc Tech. 2018;8(1):e75–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nielsen AB, Yde J. Epidemiology and traumatology of injuries in soccer. Am J Sports Med. 1989;17:803–807. [DOI] [PubMed] [Google Scholar]
- 25. Obey MR, Broski SM, Spinner RJ, Collins MS, Krych AJ. Anatomy of the adductor magnus origin: implications for proximal hamstring injuries. Orthop J Sports Med. 2016;4(1):2325967115625055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pedret C, Balius R, Barceló P, et al. Isolated tears of the gracilis muscle. Am J Sports Med. 2011;39(5):1077–1080. [DOI] [PubMed] [Google Scholar]
- 27. Pollock N, James SL, Lee JC, Chakraverty R. British Athletics Muscle Injury Classification: a new grading system. Br J Sports Med. 2014;48(18):1347–1351. [DOI] [PubMed] [Google Scholar]
- 28. Schilders E, Bismil Q, Robinson P, O’Connor PJ, Gibbon WW, Talbot JC. Adductor-related groin pain in competitive athletes: role of adductor enthesis, magnetic resonance imaging, and entheseal pubic cleft injections. J Bone Joint Surg Am. 2007;89(10):2173–2178. [DOI] [PubMed] [Google Scholar]
- 29. Schlegel TF, Bushnell BD, Godfrey J, Boublik M. Success of nonoperative management of adductor longus tendon ruptures in National Football League athletes. Am J Sports Med. 2009;37:1394–1399. [DOI] [PubMed] [Google Scholar]
- 30. Serner A, Weir A, Tol JL, et al. Characteristics of acute groin injuries in the hip flexor muscles: a detailed MRI study in athletes. Scand J Med Sci Sports. 2018;28(2):677–685. [DOI] [PubMed] [Google Scholar]
- 31. Study Group of the Muscle and Tendon System from the Spanish Society of Sports Traumatology; Balius R, Blasi M, Pedret C, et al. A histoarchitectural approach to skeletal muscle injury: searching for a common nomenclature. Orthop J Sports Med. 2020;8(3):2325967120909090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Takizawa M, Suzuki D, Ito H, Fujimiya M, Uchiyama E. The adductor part of the adductor magnus is innervated by both obturator and sciatic nerves. Clin Anat. 2014;27:778–782. [DOI] [PubMed] [Google Scholar]
- 33. Takizawa M, Suzuki D, Ito H, Fujimiya M, Uchiyama E. Why adductor magnus muscle is large: the function based on muscle morphology in cadavers. Scand J Med Sci Sports. 2012;24(1):197–203. [DOI] [PubMed] [Google Scholar]
- 34. Valle X, Alentorn-Geli E, Tol JL, et al. Muscle injuries in sports: a new evidence-informed and expert consensus-based classification with clinical application. Sports Med. 2017;47(7):1241–1253. [DOI] [PubMed] [Google Scholar]
- 35. Weir A, Brukner P, Delahunt E, et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med. 2015;48:768–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Werner J, Hägglund M, Ekstrand J, Waldén M. Hip and groin time-loss injuries decreased slightly but injury burden remained constant in men’s professional football: the 15-year prospective UEFA Elite Club Injury Study. Br J Sports Med. 2019;53(9):539–546. [DOI] [PubMed] [Google Scholar]
- 37. Wong-On M, Turmo-Garuz A, Arriaza R, et al. Injuries of the obturator muscles in professional soccer players. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1936–1942. [DOI] [PubMed] [Google Scholar]