Abstract
Objectives:
To examine age-related trajectories of cardiovascular risk and use of aspirin and statin among US adults aged 50 or older.
Design:
Repeated cross-sectional study using data from 2011–2018 National Health and Nutrition Examination Surveys.
Setting:
Nationally representative health interview survey in the United States
Participants:
Non-institutionalized adults aged 50 years and older (n=11,392 unweighted).
Measurements:
Primary prevention was defined as the prevention of a first cardiovascular event including coronary heart disease, angina/angina pectoris, heart attack, or stroke, whereas secondary prevention was defined as those with a history of these clinical conditions. Medication use was determined by self-report; aspirin use included dose and frequency, and statin use included generic names, days of prescription fills, and indications. We examined linear trends between age and each medication use, after controlling for period, sex, and race/ethnicity.
Results:
Prevalence of those eligible for primary prevention treatment increased with age from 31.8% in ages 50–54 to 52.0% in ages ≥75 (p<0.001). Similarly, those eligible for secondary prevention treatment increased with age from 2.7% in ages 50–54 to 21.1% in ages ≥75 (p<0.001). Low-dose daily aspirin use increased with age (p<0.001), and 45.3% of adults aged ≥75 took low-dose aspirin daily for primary prevention. Statin use also increased with age (p<0.001), and 56.4% of adults aged ≥75 had long-term statin use for secondary prevention.
Conclusion:
While adults aged ≥75 do not benefit from the use of aspirin to prevent the first CVD, many continue to take aspirin on a regular basis. In spite of the clear benefit of statin use to prevent a subsequent CVD event, many older adults in this risk category are not taking a statin. Further education and guidance for both healthcare providers and older adults regarding the appropriate use of aspirin and statins to prevent CVD is needed.
Keywords: Cardiovascular, aspirin, statin, pharmaco-epidemiology
Introduction
Cardiovascular disease (CVD) is a broad term that includes atherosclerosis, heart failure, cerebrovascular disease, peripheral vascular disease and other cardiac abnormalities (e.g., arrhythmias, cardiomyopathy, endocarditis, myocarditis, pericarditis, and valvular heart disease),1 and is the number 1 cause of mortality globally, resulting in 17.9 million deaths each year.2 In the US, about 655,000 Americans die from CVD each year (i.e., one in every 4 deaths),3 and the CVD-related economic burden is estimated to be about $219 billion annually.3 Age is an important risk factor for CVDs, and older adults are particularly at greater risk of CVDs.4 While the prevention of CVD in older adults is a public health priority, the appropriate use of medications is also important.
The prevention of CVD can be broadly divided into preventing a first CVD event (primary prevention), and preventing subsequent CVD events (secondary prevention).4,5 While healthy lifestyle habits (e.g., healthy diet, regular physical activity, and not smoking) can improve cardiovascular health in later life,6 pharmacological interventions, such as the use of aspirin and statin, may also be helpful. The American College of Cardiology (ACC), American Heart Association (AHA), and US Preventive Services Task Force (USPSTF) all recommend the use of aspirin and/or a statin for the primary and secondary prevention of CVD in different age groups, based on the available data and associated risks and benefits.7–9 These guidelines have focused on the risk of atherosclerotic CVD (ASCVD), which is caused by plaque buildup in arterial walls and refers to the following conditions: acute coronary syndromes, coronary heart disease, cerebrovascular disease, and other peripheral arterial diseases.10,11
The USPSTF recommends initiating low-dose aspirin use for the primary prevention of CVD in adults, who (1) have a ≥10% risk of 10-year ASCVD, (2) are not at increased risk for bleeding, (3) have a life expectancy of at least 10 years, and (4) are willing to take low-dose aspirin daily for at least 10 years. The USPSTF gives a grade of B (i.e., recommended to provide this service) for adults aged 50 to 59, a grade of C (i.e., provide this service only if considerations support the providing the service in an individual patient) for adults aged 60 to 69, and a grade of I (i.e., insufficient evidence to make a recommendation) to those aged ≥70 and younger than 50 years.
The USPSTF recommends that adults without a history of CVD use a low- or moderate-dose statin for the prevention of CVD with the following three criteria: (1) ages between 40 and 75 years, (2) one or more CVD risk factors (e.g., dyslipidemia, diabetes, hypertension, or smoking), and (3) ≥10% risk of 10-year ASCVD, with an overall recommendation grade of B.9 Grade of C was given to those with the first two criteria and a 7.5% to 10% of 10-year ASCVD risk, and grade of I was given otherwise.9
The appropriate use of pharmaco-therapeutic interventions to prevent CVD in older adults is complicated by the under-representation of older adults in clinical trials and a resulting lack of high-quality evidence. Though multiple randomized controlled trials (RCTs) have shown the beneficial effects of aspirin and statin use in secondary prevention of CVD in older adults, there is insufficient high-quality evidence to support the use of aspirin and/or a statin for the primary prevention of CVD in adults aged ≥75,8,9
We aim to examine prevalence, national trends, and use patterns in older adults who are taking aspirin or statins for primary and secondary prevention of CVD. Using nationally representative data, we sought to answer the following questions: 1) Is aspirin being overused for the primary prevention of CVD in adults aged ≥50? 2) Are statins under-used for the secondary prevention of CVD in adults aged ≥50? 3) What are the patterns of aspirin and statin use (e.g., doses) in older adults? While our analyses focus on adults aged ≥50, our primary focus is among adults aged ≥75.
Methods
Data source and study sample
We used 2011–2018 data from the National Health and Nutrition Examination Survey (NHANES), which is administered by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention (CDC).12 NHANES, a nationally representative cross-sectional survey, collects systematic information about socio-demographic and health-related inquiries of about 5,000 non-institutionalized US civilians in each wave of two years. The NCHS of CDC use collected information to report vital and health statistics of the US reguarly.12 In this study, we limited our sample to adults aged ≥50 with complete covariate data (n=11,392 unweighted), which was equivalent to 106,795,630 adults when data were extrapolated to the US population (See Supplementary Table 1 for details). The overall survey response rate of NHANES ranged from 48.8% to 69.5%, depending the survey year.13 Our study was exempted from review by the Institutional Review Board at the University of Connecticut School of Medicine as we used publicly available, de-identified data. Study procedures followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.14,15 Further details of the survey, including study descriptions, questionnaires, sampling methodology, and other technical reports are available on the NHANES website.16
Measures
Primary and secondary prevention for CVD.
To identify individuals eligible for treatment represented by primary or secondary prevention for CVD,5,7–9 we used the following validated measures: Primary prevention was defined as those with 10% or greater of 10-year ASCVD risk, but with no prior history of coronary heart disease, angina/angina pectoris, heart attack, or stroke. The secondary prevention was defined as those with a prior history of these clinical conditions.
Use of aspirin and statins.
Since 2011, the NHANES collects data regarding the preventive aspirin use among adults aged ≥40.17 Aspirin use was ascertained using the following three survey questionnaires: “Do doctors or other health care providers recommend that you take a low-dose aspirin each day to prevent health attacks, strokes, or cancer? Have you ever been told to do this?”, “Are you now following this advice?”, and “On your own, are you taking a low-dose aspirin each day to prevent heart attacks, strokes, or cancer?” Using these dichotomous questionnaires, we created a binary variable (yes or no), indicating current aspirin use. Among aspirin users, two additional questions were asked: “How often do you take an aspirin?” (every day, every other day, or other), and “What is the size or dose that you take?” (in milligrams (mg)).
For statin use, survey participants were asked if they have taken any medications in the past 30 days for which they needed a prescription. Those who responded, “yes,” were then asked to show the interviewer the medication containers of all the products used. We identified statin use based on the following generic names: atorvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin, simvastatin, and combined products. For statin use, we have also identified the days of prescription fills and categorized the use as: short-term (≤180 days), mid-term (181–720 days), and long-term (≥721 days). Among statin users, clinical indications using International Classification of Diseases, 10th edition (ICD-10) were also provided, although about 25% of survey participants with statin use had missing values for such clinical indications.
Covariates.
In this study, we controlled for key demographic factors, which are age, sex, and race/ethnicity.18,19 We used a number of clinical conditions (e.g., systolic blood pressure, diastolic blood pressure, HDL, LDL, and total cholesterol, diabetes, history of hypertension treatment, and current smoking status) to construct a 10-year ASCVD risk scale.7,20 We used a 10% or greater of this scale as an indicator for eligibility of preventive treatment.
Analytical plan
First, we estimated prevalence and national trends of aspirin use among adults aged ≥50 from 2011–2012 to 2017–2018. We stratified by reason for use, prevention type, and key demographic factors (i.e., age, sex, and race/ethnicity). We examined linear trends across years and estimated the period association.21,22 We reported adjusted odds ratio (AOR) and corresponding 95% confidence intervals (CI), after controlling for key demographic factors. We repeated the same analyses in use of statin.
After assessing national trends and period effects (i.e., changes in prevalence of aspirin or statin use over time), we estimated prevalence of individuals who were eligible for primary prevention, secondary prevention, or both by age group (i.e., 50–54, 55–59, 60–64, 65–69, 70–74, or ≥75). We tested linear trends if each prevention type increased with 5-year increments in age, after controlling for period, sex, and race/ethnicity. We then estimated aspirin and statin use by age in each prevention type. In each prevention type, we tested linear trends if each medication use increased with 5-year increments in age, after adjusting for period, sex, and race/ethnicity.
Finally, we examined patterns of aspirin and statin use by age and prevention type. We tested whether frequency of aspirin use (i.e., every day, every other day, or other) increased with 5-year increments in age and by prevention type. For statin use, we tested whether term use (i.e., short-term, mid-term, or long-term) increased with 5-year increments in age and by prevention type.
We also reported any use and co-use of aspirin and statins for preventing CVD-related events, and whether these medication uses increased with age. We also reported dosing information (in milligrams) among aspirin users and clinical indications for statin users. All analyses were conducted using Stata (version 16.1 MP/6-Core)23 and accounted for the complex survey sampling design (i.e., unequal probability of selection, clustering and stratification) in NHAMES using svy commands.24 We set p<0.05 as the test of statistical significance in this study.
Results
Socio-demographic characteristics of the study sample
The mean age of survey participants was 63.6 (standard deviation=9.3), and 53.3% were female. Of the survey participants, 72.6% were non-Hispanic white, 10.1% were non-Hispanic black, 9.9% were Hispanic, and 7.5% were other racial/ethnic minorities. In addition, 60.5% were married, 6.5% were never married, and 33.0% were either widowed, divorced, separated or other. While 84.8% were born in the US, 15.2% were born outside the US. Finally, 30.6% of them had a bachelor’s degree or higher, and 50.3% had a household income of $55,000 or greater. More detailed information can also be found elsewhere.18
Prevalence and national trends of use of aspirin and statin
Of the survey participants, 37.0% (95% CI, 35.5–38.6%) used aspirin, and the aspirin use remained stable across years, ranging from 38.8% in 2011–2012 to 36.0% in 2017–2018 (Table 1). The majority of aspirin users had a recommendation by a doctor, ranging from 33.8% in 2011–2012 to 32.2% in 2017–2018, whereas less than 6% of the users took an aspirin on their own. Among adults eligible for primary prevention, 38.0% (95% CI, 35.8–40.2%) used aspirin, and 68.1% (95% CI, 64.3–71.7%) of adults eligible for secondary prevention took aspirin. The prevalence rates were stable and no significant national trends were found. When stratified by age, sex, and race/ethnicity, adults aged between 55 and 59 (AOR, 0.59; 95% CI, 0.40–0.86 for linear time trends) and non-Hispanic blacks (AOR, 0.67; 95% CI, 0.49–0.91) for linear time trends) had decreasing trends of aspirin use over time.
Table 1.
Trends of aspirin use among US adults aged 50 or older, 2011–2018
| 2011–2012 | 2013–2014 | 2015–2016 | 2017–2018 | Period association, AOR (95% CI, p) | |
|---|---|---|---|---|---|
|
| |||||
| Sample size | |||||
| Unweighted sample | 2,706 | 2,783 | 2,827 | 3,076 | |
| Weighted population | 25,213,630 | 25,902,862 | 27,188,841 | 28,490,297 | |
|
| |||||
| Total | 38.8% | 36.7% | 36.7% | 36.0% | 0.88 (0.71–1.08, 0.214) |
| Reason for use | |||||
| Recommended by a doctor | 33.8% | 32.7% | 31.3% | 32.2% | 0.89 (0.73–1.09, 0.245) |
| On your own | 5.0% | 4.0% | 5.4% | 3.9% | 0.92 (0.58–1.47, 0.720) |
| CVD-risk | |||||
| Any | 45.2% | 45.0% | 42.6% | 42.1% | 0.88 (0.71–1.08, 0.216) |
| Primary prevention | 39.7% | 40.1% | 36.8% | 35.7% | 0.82 (0.64–1.06, 0.130) |
| Secondary prevention | 71.0% | 66.2% | 66.9% | 68.6% | 0.93 (0.58–1.50, 0.771) |
| Age, years | |||||
| 50–54 | 19.7% | 20.3% | 20.5% | 20.0% | 1.05 (0.62–1.77, 0.856) |
| 55–59 | 40.6% | 25.4% | 27.4% | 26.5% | 0.59 (0.40–0.86, 0.007) |
| 60–64 | 41.1% | 37.5% | 39.6% | 33.8% | 0.80 (0.54–1.20, 0.266) |
| 65–69 | 38.9% | 45.7% | 43.2% | 40.3% | 0.97 (0.53–1.78, 0.922) |
| 70–74 | 49.0% | 50.1% | 49.0% | 49.6% | 1.02 (0.66–1.57, 0.943) |
| >75 | 52.6% | 53.5% | 49.6% | 53.7% | 1.01 (0.79–1.27, 0.978) |
| Sex | |||||
| Male | 41.9% | 40.2% | 40.4% | 41.2% | 0.96 (0.76–1.21, 0.731) |
| Female | 36.2% | 33.6% | 33.4% | 31.6% | 0.81 (0.60–1.08, 0.145) |
| Race/ethnicity | |||||
| White, non-Hispanic | 41.1% | 39.0% | 38.2% | 38.9% | 0.85 (0.67–1.11, 0.237) |
| Black, non-Hispanic | 38.6% | 36.3% | 35.9% | 30.8% | 0.67 (0.49–0.91, 0.013) |
| Hispanic | 28.5% | 25.6% | 31.5% | 29.8% | 1.15 (0.86–1.55, 0.338) |
| Other, non-Hispanic | 27.1% | 25.3% | 30.8% | 28.2% | 1.17 (0.80–1.72, 0.411) |
Note: Data are from National Health and Nutrition Examination Survey (NHANES). Analyses were adjusted for age, sex, and race/ethnicity. AOR stands for adjusted odds ratio. CI stands for confidence intervals.
Similarly, about 34.8% (95% CI, 33.5–36.2%) of all adults aged ≥50 took statins, and such use remained stable across years, ranging from 33.6% in 2011–2012 to 33.4% in 2017–2018 (Table 2). Of adults eligible for primary prevention, the prevalence of statin use remained stable, ranging from 30.6% (95% CI, 27.7–33.7%) in 2011 to 2012 to 30.4% (95% CI, 26.4–34.7%) in 2017–2018. Of adults eligible for secondary prevention, the prevalence of statin use increased slightly from 66.9% (95% CI, 59.1–73.9%) in 2011–2012 to 70.0% (95% CI, 64.8–74.8%) in 2017–2018, but these trends were not significant. When stratified by age, sex, and race/ethnicity, adults aged between 55 and 59 presented a decreasing trend of statin use over time (AOR, 0.56; 95% CI, 0.35–0.91).
Table 2.
Trends of statin use among US adults aged 50 or older, 2011–2018
| 2011–2012 | 2013–2014 | 2015–2016 | 2017–2018 | Period association, AOR (95% CI, p) | |
|---|---|---|---|---|---|
|
| |||||
| Sample size | |||||
| Unweighted sample | 2,706 | 2,783 | 2,827 | 3,076 | |
| Weighted population | 25,213,630 | 25,902,862 | 27,188,841 | 28,490,297 | |
|
| |||||
| Total | 33.6% | 37.9% | 34.5% | 33.4% | 0.90 (0.76–1.07, 0.246) |
| CVD-risk | |||||
| Any | 37.0% | 43.3% | 41.5% | 38.2% | 1.01 (0.83–1.23; 0.929) |
| Primary prevention | 30.6% | 36.6% | 35.2% | 30.4% | 0.95 (0.77–1.19; 0.665) |
| Secondary prevention | 66.9% | 72.3% | 67.9% | 70.1% | 1.06 (0.70–1.60; 0.787) |
| Age, years | |||||
| 50–54 | 19.9% | 20.0% | 15.4% | 17.8% | 0.80 (0.43–1.48; 0.464) |
| 55–59 | 28.4% | 31.2% | 24.0% | 18.9% | 0.56 (0.35–0.91; 0.019) |
| 60–64 | 32.7% | 36.5% | 34.3% | 33.5% | 1.00 (0.72–1.40; 0.988) |
| 65–69 | 41.6% | 44.9% | 45.9% | 39.7% | 0.90 (0.54–1.48; 0.664) |
| 70–74 | 48.2% | 53.1% | 50.2% | 47.7% | 0.93 (0.65–1.32; 0.664) |
| ≥75 | 43.9% | 53.6% | 48.6% | 52.3% | 1.27 (0.99–1.64; 0.065) |
| Sex | |||||
| Male | 35.8% | 41.6% | 40.5% | 37.0% | 0.98 (0.81–1.20; 0.876) |
| Female | 31.7% | 34.6% | 29.2% | 30.3% | 0.83 (0.65–1.06; 0.138) |
| Race/ethnicity | |||||
| White, non-Hispanic | 34.5% | 39.6% | 35.2% | 34.0% | 0.86 (0.70–1.07; 0.176) |
| Black, non-Hispanic | 32.2% | 36.3% | 32.1% | 31.7% | 0.87 (0.68–1.11; 0.250) |
| Hispanic | 26.7% | 25.6% | 29.2% | 30.4% | 1.26 (0.97–1.63; 0.077) |
| Other, non-Hispanic | 35.8% | 36.9% | 38.6% | 34.4% | 1.00 (0.61–1.66; 0.993) |
Note: Data are from National Health and Nutrition Examination Survey (NHANES). Analyses were adjusted for age, sex, and race/ethnicity. AOR, adjusted odds ratio. CI, confidence intervals.
Prevalence of cardiovascular risk and use of aspirin and statin by age and prevention type
After controlling for period effects and key demographic factors, prevalence of those eligible for primary prevention treatment increased with 5-year increments in age from 31.8% (95% CI, 28.7–35.1%) in ages 50–54 to 52.0% (95% CI, 49.4–54.6%) in ages ≥75 (p<0.001) (Figure 1, Panel A1). Similarly, those eligible for secondary prevention treatment increased with age from 2.7% (95% CI, 1.9–3.9%) in ages 50–54 to 21.1% (95% CI, 19.1–23.2%) in ages ≥75 (p<0.001) (Figure 1, Panel B1).
Figure 1.
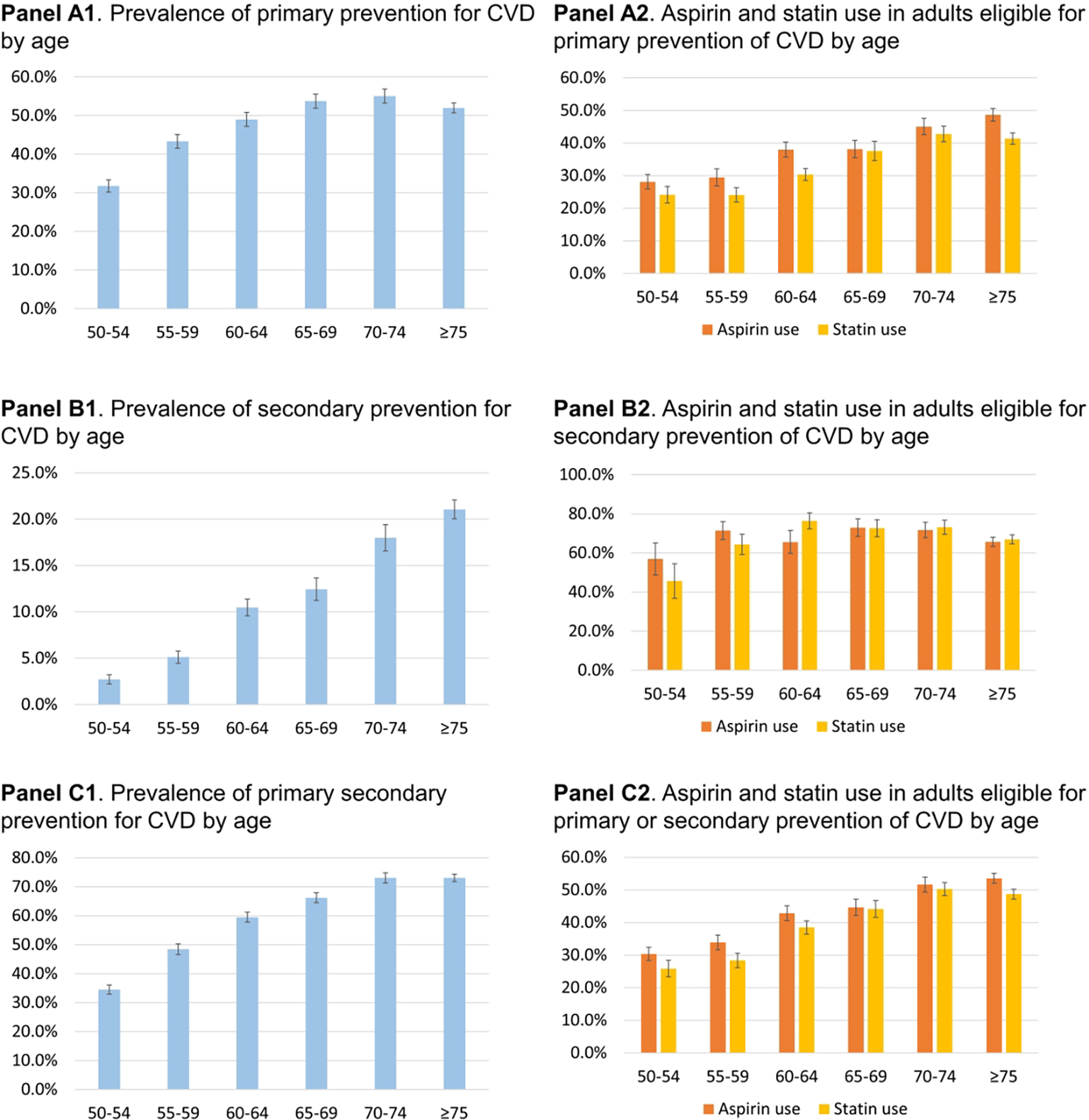
Prevalence of aspirin and statin use by age and prevention type among US adults aged 50 and older, 2011–2018
Note: Data are from National Health and Nutrition Examination Survey (NHANES). Whiskers represent 95% confidence intervals
Among adults eligible for primary prevention, 38.0% used aspirin, and the use increased with age from 28.1% (95% CI, 23.9–32.7%) in ages 50–54 to 48.7% (95 CI, 44.8–52.5%) in ages ≥75 (p<0.001); and 33.2% used a statin and its use increased with age from 24.2% (95% CI, 19.5–29.6%) in ages 50–54 to 41.4% (95% CI, 38.0–44.8%) in ages ≥75 (p<0.001) (Figure 1, Panel A2). Among adults eligible for secondary prevention, 68.1% used aspirin and its use increased with age from 56.9% (95% CI, 40.4–72.0%) in ages 50–54 to 65.7% (95% CI, 60.8–70.2%) in ages ≥75 (p<0.001); and 69.3% used a statin and its use increased with age from 45.6% (95% CI, 29.1–63.2%) in ages 50–54 to 66.9% (95% CI, 62.1–71.4%) in ages ≥75 (p<0.001) (Figure 1, Panel B2).
Patterns of aspirin and statin use by age and prevention type
Among those eligible for primary prevention, 33.9% (95% CI, 31.7–36.2%) used aspirin daily and this everyday use increased with age from 23.9% (95% CI, 19.5–29.0%) in ages 50–54 to 45.3% (95 CI, 41.36–49.4%) in ages ≥75 (p<0.001) (Figure 2, Panel A1). In addition, 26.7% (95% CI, 25.1–28.5%) used statins for a long-term (i.e., ≥721 days) and this pattern increased with age from 18.5% (95% CI, 14.1–23.9%) in ages 50–54 to 35.3% (95% CI, 32.2–38.5%) in ages ≥75 (p<0.001) (Figure 2, Panel B1).
Figure 2.
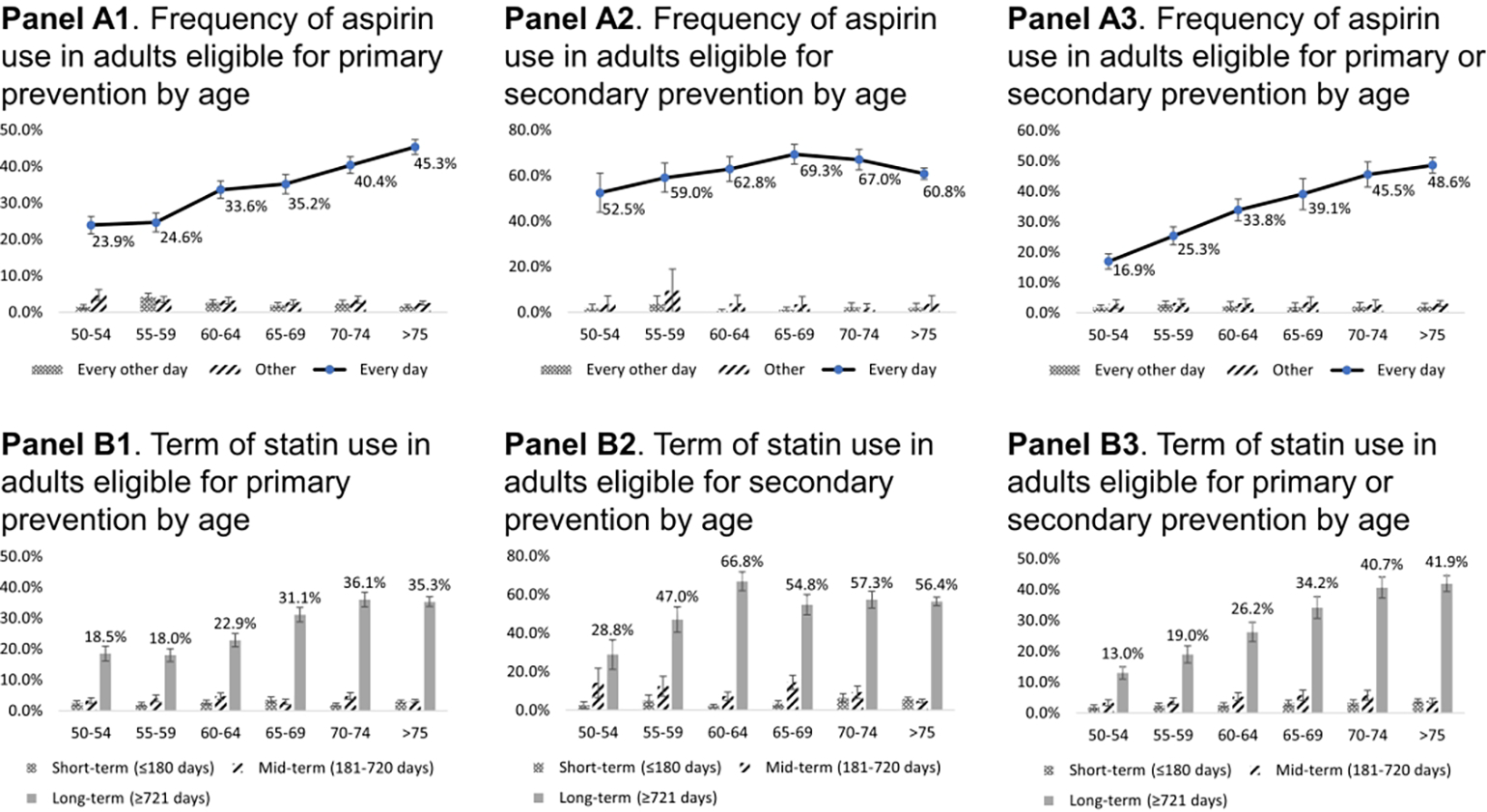
Patterns of aspirin and statin use by age and prevention type among US adults aged 50 and older, 2011–2018
Note: Data are from National Health and Nutrition Examination Survey (NHANES). Whiskers represent 95% confidence intervals.
Among those eligible for secondary prevention, 63.1% (95% CI, 59.2–66.8%) used aspirin daily; this pattern increased with age from 52.5% (95% CI, 35.7–68.7%) in ages 50–54 to 60.8% (95 CI, 55.8–65.6) in ages ≥75, but linear trends were not significant (Figure 2, Panel A2). Long-term statin use, however, significantly increased with age from 28.8% (95% CI, 16.0–46.2%) in ages 50–54 to 56.4% (95% CI, 52.0–60.8%) in ages ≥75 (p<0.001) (Figure 2, Panel B2).
Of adults eligible for either primary or secondary prevention, 58.8% (95% CI, 56.9–60.7%) used either an aspirin or a statin, and 24.8% (95% CI, 23.3–26.4%) used both. The co-use also increases significantly with age, ranging from 13.0% (95% CI, 8.9–18.6%) in ages 50–54 to 31.3% (95% CI, 28.8–33.9%) in ages ≥75 (p<0.001). Finally, 98.6% of aspirin users reported 325 milligrams or lower in dose among aspirin users. About 25% of statin users had missing values in clinical indications, but 74.2% of statin users reported that they have CVD-related clinical indications (e.g., E78.1 (pure hyperglyceridemia), I21.P (to prevent heart attack/myocardial infarction), and I63.P (to prevent stroke)).
Discussion
This study presents the most recent trends of cardiovascular risk and use of low-dose aspirin and statin in adults aged ≥50 using nationally representative survey data. Between 2011 and 2018, more than half of adults aged ≥50 years took aspirin or a statin. Use of these medications significantly increased with age. We did not find period or cohort effects in the survey participants.
Aspirin use
Aspirin use increased significantly with 5-year increments in the age, regardless of prevention type. Our findings are consistent with a previous study, which reported that the aspirin use increases with age from 18.4% in adults aged 50–59 years to 44.6% in adults aged 70–79 years and 46.2% in adults aged ≥80 in 2017.25 We were not able to compare our findings with another study, which reported a lower prevalence rate (22.1% in 2012–2015 for primary prevention),26 because this previous study did not use the ASCVD algorithms to identify primary prevention and included those who are 40–49 years old. Our findings extend these two previous studies by examining aspirin use by prevention type and pattern of use. For example, daily use of aspirin increases with age; it appears that aspirin users are generally adherent to instructions for aspirin use. Furthermore, more than 98% of aspirin users reported 325 milligrams or lower in dose, which is consistent with the clinical guidelines.5,7
Based on multiple RCTs27–30 and a meta-analysis31 that have shown no significant benefit of aspirin for the primary prevention of CVD in older adults, our findings indicate that aspirin may have been inappropriately used in many older adults. It is worth noting, however, that some of earlier studies27–31 are likely to have an increased Type II error due to poor adherence or losses to follow-up. Further steps are needed to decrease the use of aspirin by older adults who do not have a history of CVD. This should include educating both healthcare providers and their patients regarding the lack of benefits and potential risks of aspirin use, and an increased focus on lifestyle modification and blood pressure control as the best means of preventing the first CVD in older adults.32
Though the efficacy of aspirin for the secondary prevention of CVD is well established in older adults,33 many older adults in this study with a history of CVD did not take aspirin. This finding may be reasonable since many of these older adults may have had contraindication to the use aspirin, such as taking anticoagulants for atrial fibrillation. Future research is needed to assess safer use of aspirin for the secondary prevention of CVD.
Statin use
Similar to the aspirin use, use of statins also increased significantly with age. One previous study reported that the prevalence of statin use among US older adults increased from 33.8% in 2005–2006 to 46.2% in 2010–2011.34 Another study reported in 2016 showed that about 32.2% of older adults were taking a statin.35 Our findings are generally consistent with these studies, although we did not make direct comparisons due to differences in calendar periods, inclusion criteria, study settings (e.g., outside the US).
There continues to be uncertain regarding the use of statins for the primary prevention of CVD for older adults in their 70s and above. However, there are several large RCTs underway that will hopefully clarify this issue. In addition, there are compelling epidemiologic data (e.g., US veterans aged ≥7536) indicating that adults aged ≥70 with elevated low-density lipoproteins (LDL) cholesterol and no previous history of CVD can have beneficial effects of statin use for the primary prevention of CVD in older adults.37,38
Despite the evidence from both RCTs and meta-analyses that statins are effective and safe for the secondary prevention of CVD in older adults,39–41 our data show that statins are underutilized in many adults aged ≥75 with a history of CVD. Other studies have demonstrated a similar under-utilization of stains for the secondary prevention of CVD in older adults.42 Further steps are required to increase the use of statins in older adults with existing CVD. The education of both healthcare providers and their older patients regarding the compelling benefits of using statins for the secondary prevention of CVD is important.
Our findings have several clinical implications. First, both aspirin and statins are increasingly common with increments in age regardless of primary or secondary prevention types. Clinicians should continue to carefully weigh potential benefits and harms of these medications or consider deprescribing, and actively communicate with their patients to minimize potential side effects. Secondly, some of the clinical guidelines are to be updated in the near future. For example, the USPSTF guidelines for both aspirin and statin use will be updated soon, and there is a growing consensus that aspirin should not be used for the primary prevention of CVD-related events. In fact, in 2019, the ACC and AHA revised their recommendation about aspirin use for the primary prevention of ASCVD (i.e., “Aspirin should be used infrequently in the routine primary prevention of ASCVD because of lack of net benefit.”7). Healthcare providers should inform their older patients about the appropriate aspirin use, so that they can avoid misuse of aspirin, which can be easily purchased over the counter.
Limitations of this study include limited generalizability among adults who are institutionalized (e.g., nursing homes), and lack of CVD-related health outcomes. Another limitation is that although ASCVD risk calculators were used to identify high-risk patients who are most likely to benefit from primary prevention, these algorithms have not been validated among those aged ≥75. Another limitation is the cross-sectional nature of the data, which limited us to derive any causal interpretation of the findings.
Despite these limitations, our study highlights that between 2011 and 2018, 35.8 million older adults took either aspirin or statins for preventing CVD-related events and use of these medications increased significantly with age. Our findings suggest that aspirin seems to be overused for the primary prevention of CVD whereas statins are underused for the secondary prevention of CVD in adults aged ≥75. Because the majority of aspirin users had a recommendation by a doctor, provider and patient education is needed to reduce potentially unnecessary aspirin use for the primary prevention of CVD. Given the efficacy of statin use for secondary prevention of CVD, increased statin use should also be supported for the secondary prevention of CVD. Safer prescribing practice, patient education, and patient-oriented effectiveness research should be continually encouraged to reduce potential harms and improve CVD-related patient outcomes.
Supplementary Material
Impact statement:
Using nationwide survey data, this is the first study to examine age-related trajectories of cardiovascular risk and use of aspirin and statin among US adults aged 50 or older between 2011 and 2018.
Acknowledgments and disclosures
Concept and design: Rhee, Ross, and Coll
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Rhee
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Rhee
Footnotes
Conflicts of interest: In the past 36 months, Dr. Rhee was supported in part by the National Institute on Aging (#T32AG019134) through Yale School of Medicine. Rhee is currently funded by the National Institute of Mental Health (#R21MH117438) and the Institute for Collaboration on Health, Intervention, and Policy (InCHIP) at the University of Connecticut. Dr. Ross received research support through Yale from Johnson and Johnson to develop methods of clinical trial data sharing, from Medtronic, Inc. and the Food and Drug Administration (FDA) to develop methods for post-market surveillance of medical devices (U01FD004585), from the Centers of Medicare and Medicaid Services (CMS) to develop and maintain performance measures that are used for public reporting, from the FDA to establish a Center for Excellence in Regulatory Science and Innovation (CERSI) at Yale University and the Mayo Clinic (U01FD005938), from the Blue Cross Blue Shield Association to better understand medical technology evaluation, and from the Agency for Healthcare Research and Quality (R01HS022882).
References
- 1.Semb AG, Ikdahl E, Wibetoe G, Crowson C, Rollefstad S. Atherosclerotic cardiovascular disease prevention in rheumatoid arthritis. Nat Rev Rheumatol. 2020;16(7):361–379. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Cardiovascular dieases. 2020; https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1. Accessed November 5, 2020.
- 3.Centers for Disease Control and Prevention. Heart disease. 2020; https://www.cdc.gov/heartdisease/facts.htm. Accessed November 5, 2020.
- 4.Coll PP, Roche V, Olsen JS, Voit JH, Bowen E, Kumar M. The Prevention of Cardiovascular Disease in Older Adults. J Am Geriatr Soc. 2020;68(5):1098–1106. [DOI] [PubMed] [Google Scholar]
- 5.Peters AT, Mutharasan RK. Aspirin for Prevention of Cardiovascular Disease. JAMA. 2020;323(7):676–676. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Prevent heart disease. 2020; https://www.cdc.gov/heartdisease/prevention.htm. Accessed November 5, 2020.
- 7.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e563–e595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Preventive Services Task Force. Aspirin use to prevent cardiovascular disease and colorectal cancer: Preventive medication. 2016; https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/aspirin-to-prevent-cardiovascular-disease-and-cancer. Accessed September 10, 2020.
- 9.US Preventive Services Task Force. Statin use for the primary prevention of cardiovascular disease in adults: Preventive medication. 2016; https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/statin-use-in-adults-preventive-medication. Accessed September 10, 2020.
- 10.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082–e1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chamberlain JJ, Johnson EL, Leal S, Rhinehart AS, Shubrook JH, Peterson L.Cardiovascular Disease and Risk Management: Review of the American Diabetes Association Standards of Medical Care in Diabetes 2018. Ann Intern Med. 2018;168(9):640–650. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. About the National Health and Nutrition Examination Survey. 2017; https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed June 5, 2020.
- 13.Centers for Disease Control and Prevention. NHANES response rates and population totals.2020; https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx#response-rates. Accessed November 9, 2020.
- 14.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800–804. [DOI] [PubMed] [Google Scholar]
- 15.Enhancing the QUAlity and Transparency Of health Research (EQUATOR) Network. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. 2019; http://www.equator-network.org/reporting-guidelines/strobe/. Accessed September 25, 2019.
- 16.Centers for Disease Control and Prevention. NAMES 2013–2014: Data, documentation,codebooks, SAS code. 2018; https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2013. Accessed November 27, 2019.
- 17.Centers for Disease Control and Prevention. National Health and Nutrition Examination Suruvey: Preventive aspirin use. 2020; https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/RXQASA_J.htm. Accessed November 15, 2020.
- 18.Rhee TG, Marottoli RA, Cooney LM Jr, Fortinsky RH. Associations of Social and Behavioral Determinants of Health Index with Self-Rated Health, Functional Limitations, and Health Services Use in Older Adults. J Am Geriatr Soc. 2020;68(8):1731–1738. [DOI] [PubMed] [Google Scholar]
- 19.Rhee TG, Lee K, Schensul JJ. Black-white Disparities in Social and Behavioral Determinants of Health Index and Their Associations with Self-rated Health and Functional Limitations in Older Adults. J Gerontol A Biol Sci Med Sci. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carey RM, Whelton PK, Committee AAHGW. Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann Intern Med. 2018;168(5):351–358. [DOI] [PubMed] [Google Scholar]
- 21.Rhee TG, Olfson M, Nierenberg AA, Wilkinson ST. 20-Year Trends in the Pharmacologic Treatment of Bipolar Disorder by Psychiatrists in Outpatient Care Settings. Am J Psychiatry. 2020;177(8):706–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rhee TG, Wilkinson ST, Steffens DC, Rosenheck RA, Olfson M. Prevalence of teatment for depression among US adults who screen positive for depression, 2007–2016. JAMA Psychiatry. 2020:E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stata Statistical Software: Release 16 [computer program]. College Station, TX: StataCorp LP.2020. [Google Scholar]
- 24.Centers for Disease Control and Prevention. NHANES 2013–2014: Data documentation, Codebook, and Frequencies: Demographic Variables and Sample Weights. 2015; https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/DEMO_H.htm. Accessed March 2, 2020.
- 25.O’Brien CW, Juraschek SP, Wee CC. Prevalence of Aspirin Use for Primary Prevention of Cardiovascular Disease in the United States: Results From the 2017 National Health Interview Survey. Ann Intern Med. 2019;171(8):596–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stuntz M, Bernstein B. Recent trends in the prevalence of low-dose aspirin use for primary and secondary prevention of cardiovascular disease in the United States, 2012–2015. Prev Med Rep. 2017;5:183–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gaziano JM, Brotons C, Coppolecchia R, et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet. 2018;392(10152):1036–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McNeil JJ, Woods RL, Nelson MR, et al. Effect of Aspirin on Disability-free Survival in the Healthy Elderly. N Engl J Med. 2018;379(16):1499–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Capodanno D, Angiolillo DJ. Aspirin for Primary Cardiovascular Risk Prevention and Beyond in Diabetes Mellitus. Circulation. 2016;134(20):1579–1594. [DOI] [PubMed] [Google Scholar]
- 30.McNeil JJ, Wolfe R, Woods RL, et al. Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly. N Engl J Med. 2018;379(16):1509–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zheng SL, Roddick AJ. Association of Aspirin Use for Primary Prevention With Cardiovascular Events and Bleeding Events: A Systematic Review and Meta-analysis. JAMA. 2019;321(3):277–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chiang KF, Shah SJ, Stafford RS. A Practical Approach to Low-Dose Aspirin for Primary Prevention. JAMA. 2019. [DOI] [PubMed] [Google Scholar]
- 33.Antithrombotic Trialists C, Baigent C, Blackwell L, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373(9678):1849–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qato DM, Wilder J, Schumm LP, Gillet V, Alexander GC. Changes in Prescription and Over-the-Counter Medication and Dietary Supplement Use Among Older Adults in the United States, 2005 vs 2011. JAMA Intern Med. 2016;176(4):473–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ofori-Asenso R, Ilomaki J, Tacey M, et al. Predictors of statin use among older adults: A nationwide cross-sectional study. J Clin Lipidol. 2019;13(1):156–162 e151. [DOI] [PubMed] [Google Scholar]
- 36.Orkaby AR, Driver JA, Ho YL, et al. Association of Statin Use With All-Cause and Cardiovascular Mortality in US Veterans 75 Years and Older. JAMA. 2020;324(1):68–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mortensen MB, Nordestgaard BG. Elevated LDL cholesterol and increased risk of myocardial infarction and atherosclerotic cardiovascular disease in individuals aged 70–100 years: a contemporary primary prevention cohort. Lancet. 2020;396(10263):1644–1652. [DOI] [PubMed] [Google Scholar]
- 38.Strandberg TE. Role of Statin Therapy in Primary Prevention of Cardiovascular Disease in Elderly Patients. Curr Atheroscler Rep. 2019;21(8):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Afilalo J, Duque G, Steele R, Jukema JW, de Craen AJ, Eisenberg MJ. Statins for secondary prevention in elderly patients: a hierarchical bayesian meta-analysis. J Am Coll Cardiol. 2008;51(1):37–45. [DOI] [PubMed] [Google Scholar]
- 40.Nilsson SF, Laursen TM, Hjorthoj C, Thorup A, Nordentoft M. Risk of psychiatric disordersin offspring of parents with a history of homelessness during childhood and adolescence in Denmark: a nationwide, register-based, cohort study. Lancet Public Health. 2017;2(12):e541–e550. [DOI] [PubMed] [Google Scholar]
- 41.Cholesterol Treatment Trialists C Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Allen Maycock CA, Muhlestein JB, Horne BD, et al. Statin therapy is associated with reduced mortality across all age groups of individuals with significant coronary disease, including very elderly patients. J Am Coll Cardiol. 2002;40(10):1777–1785. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


