Abstract
Female sex workers (FSWs) in sub-Saharan Africa are a marginalized group with an increased morbidity risk. Psychoactive substance use among this group is common and increases the risk of adverse health consequences. The type of substance used, extent, and nature of use varies with different settings and regions. We examine the use of specific psychoactive substances among FSWs residing in an urban informal settlement in Nairobi. This cross-sectional study was conducted between April and August 2017. Structured questionnaires were administered in face-to-face interviews. Descriptive statistics and logistic regression were undertaken to examine prevalence, patterns, and factors associated with use of specific substances. Out of 301 FSWs, 98% reported current psychoactive substance use. The most used substance was alcohol with 95.6% of the study population reporting use in the past year. Of these, 151 (50.2%) met criteria for very high-risk drinkers. Reported current use was 61.5% for cannabis, 47.2% for khat, and 30.9% for tobacco. Factors independently associated with hazardous and harmful alcohol use included earning a higher monthly income (>USD50) and disclosure of sex work to close family and friends. There is an urgent need for preventive and curative interventions to address the high prevalence of substance use among FSW residing in high-risk urban informal settlements in Kenya.
Keywords: Female sex workers, informal settlements, sub–Saharan Africa, Substance us, Kenya
Introduction
Female sex workers (FSWs) register among the highest population risk groups for psychoactive substance use with prevalence as high as 92% in low- and middle- income countries (Semple et al. 2015). The high prevalence of psychoactive substance use among female sex workers is a well-recognized public health concern. Of key importance is the direct and indirect role substance use plays in contributing to subsequent higher rates of Human Immunodeficiency Virus (HIV) and other sexually transmitted infections among the workers (Chersich et al. 2014; Panda et al. 2001; Strathdee et al. 2015), directly through needle sharing practices and indirectly through sexual risk taking. In addition, rates of violence (Moret et al. 2016; “Violence and Exposure to HIV Among Sex Workers in Phnom Penh, Cambodia” 2006) and serious psychiatric morbidity are also higher among female sex workers who use drugs (Roberts, Mathers, and Degenhardt 2010).
This high burden of substance use among FSWs has been largely explained by the unique characteristics of the sex work setting (Strathdee et al. 2015). The availability, accessibility, and acceptability of drug use are key contributors to the high levels of drug consumption among this group (Harcourt, Donovan, and Harcourt 2005; Roshanfekr et al. 2015). Qualitative studies suggest that some FSWs may use psychoactive substances as a way of escaping stigma and hopelessness related to the sex work industry, while others believe that drugs are useful for relaxation and gaining confidence in order to face clients (Chen et al. 2015; Roberts, Mathers, and Degenhardt, 2010; Ross et al. 2013). Though this forms a small percentage of FSWs, drug dependence itself can lead to initiation of sex work in order to obtain money to purchase drugs, or to directly acquire drugs in exchange for sex (Devine et al. 2010).
Previous studies that have addressed sex work in Kenya have focused on its relationship with HIV and sexual behavior (Chersich et al. 2007; Othieno, Obondo, and Mathai 2012; Tegang et al. 2010). However, little is known about the type of substance used, extent, and nature of use, as well as factors related to this use. Identifying the factors that increase the risk for substance use among FSW and characterizing the prevalence of substance use is critical in order to develop effective contextualized interventions for prevention and care in Kenya. To this end, we conducted a cross-sectional survey to determine the prevalence of use of specific types of substances and to examine factors associated with their use among FSWs residing in the informal urban settlement of Kibera in Nairobi, Kenya.
Methods
Study design and setting
This cross-sectional study design involved administering semi-structured, face-to-face interviews with enrolled participants. The study was conducted in Kibera informal settlement located in Nairobi, the capital of Kenya. We partnered with a community-based organization located in Kibera that works with FSWs to support their HIV care and treatment. Data were collected by trained nurses from April to June 2017.
Participants
Detailed recruitment procedures have been described elsewhere (Denckla et al. 2019). Briefly, consenting women who self-identified as current FSWs, which were defined as consensual sex involving transaction of commercial value, either monetary or anything in kind, who were residents in one of the Kibera villages, and were at least 14 years of age, were eligible for enrollment into the study. The emancipated minors included in the study were those aged below 18 years and were either pregnant or a mother or a household head. Participants were recruited by Community Health Volunteers (CHVs) who were residents of Kibera and maintained direct contact with FSWs in this setting. The CHVs identified women who were in leadership roles for distinct FSW cohorts across several villages in Kibera to provide initial information about the study and identify female sex workers. A total of 10 cohort leaders were identified, each with a cohort membership of approximately 50 women. The CHVs then provided cohort leaders with referral information, including date, time, and place, to pass on to cohort members to present themselves to the study office for screening and enrollment.
The study procedures were approved by the Kenya Medical Research Institute Scientific and Ethics Review Unit (SSC No: 2903). The Nairobi County government and the area chief granted jurisdictional permissions to carry out the study. Enrollment of emancipated minors following informed consent follows national guidelines for conducting adolescents, sexual and reproductive health research in Kenya (NASCOP & KEMRI 2015).
Measures
Our primary outcome of interest was reported use of psychoactive substance. This was assessed using the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) (WHO ASSIST Working Group 2002). The ASSIST is a validated World Health Organization (WHO) screening instrument used to obtain information on lifetime as well as current and frequency of use of psychoactive substances, such as tobacco products, alcohol, cannabis, cocaine, khat, and other amphetamine-type stimulants (ATS), sedatives and sleeping pills (benzodiazepines), hallucinogens, inhalants, and opioids. Some of the substances may have been prescribed by a medical provider, however we focused on non-prescription use of these substances. Current use is defined as use of substance in the last 3 months. The ASSIST instrument, though not validated in Kenya, has been validated in Zambia for sub-Saharan Africa settings and found to have strong internal reliability and discriminant validity between low and moderate risk for most substance types (Kane et al. 2016). Alcohol consumption, drinking behaviors, and alcohol-related problems in the past one year were assessed using the clinician administered version of the Alcohol Use Disorders Identification Test (AUDIT) developed by the WHO, whereby Kenya was included in the foundation validity study for AUDIT (Saunders et al. 1993). A cutoff of 8 was used to indicate hazardous and harmful alcohol use (Babor et al. 2001). All questionnaires and consent forms were translated into Kiswahili, the local language, and back translated to English. Participants were given an option of selecting their most preferred language. Prior to data collection, pretesting of all study questionnaires was undertaken and few edits were done on the structure and form to improve understanding and data quality. Some edits included providing the street name terminologies for the substance type as examples in the ASSIST questionnaire.
Independent variables included age, marital status, monthly income, level of education, and number of years the FSW had resided in Kibera. We also examined behavioral factors such as condom use, place of sex work, years of conducting sex work and disclosure of sex work to close family and friends. Variables selected for assessment were based on previous literature.
Data analysis
The primary outcome was defined as use of any psychoactive substance. Polysubstance use was defined as concurrent use of more than one type of substance. Based on the scoring cut off on the AUDIT tool, we categorized alcohol use for descriptive purpose into four categories: 0–7 = non-drinker or low-level problem drinker; 8–15 = hazardous or moderate-level problem drinker; 16–19 harmful or high-level problem drinker; and ≥20 = very high risk or alcohol dependent (Luchters et al. 2011; Saunders et al. 1993). When testing associations between substance use and social and behavioral variables, we included only hazardous alcohol users and high-risk drinkers (score of 8 and above) because this aligns with problematic use of alcohol.
Descriptive statistics were used to characterize participant demographic characteristics, socioeconomic status, and psychosocial and clinical history parameters. Descriptive statistics involved the use of frequencies, reported as proportions of categorical variables and mean, standard deviation, and range of continuous variables. To gain an understanding of socio-demographic and clinical factors associated with the use of psychoactive substances, bivariable logistic regression models were fitted. Socio-demographic, psychosocial, and clinical history factors that were significantly (p < .05) associated with use of psychoactive substances for each outcome variable in the bivariate logistic regression models were entered as covariates in multivariable logistic regression models to examine the association of socio-demographic variable independent of other covarying factors assessed in the present study. Multiple regression approach allowed us to control for possible interactions between covariates. The risk of psychoactive substance use was computed as an odds ratio with a confidence level of 95%. Hosmer–Lemeshow test was used to evaluate the goodness of fit of the multivariable logistic regression models with higher p-values indicating a better fit of the model.
Results
Sociodemographic and behavioral characteristics
A total of 301 participants were enrolled in the study. The mean age of the participants was 26 years with nearly half (46.5%) reporting a secondary or higher level of education (see Supplementary Table 1). None of the participants reported being married at the time of interview. The average monthly income obtained from sex work was USD142. Many (98.3%) reported hotel lodgings as the primary location for sex work. These are often small, affordable bed and breakfast type of accommodation (Supplementary Table 1).
Substance use pattern
Alcohol was the most commonly used substance. Specifically, more than half (52.8%) of the respondents met criteria for very high-risk drinkers or alcohol dependent, defined as ≥20 on AUDIT (see Table 1). Alcohol use was followed by cannabis use at 61.5%, khat1 47.2%, and tobacco use 30.9% of the full sample. The prevalence of current psychoactive substance use was very similar to lifetime use, with only a slight decrease in the number for currently used study samples. Nearly 80% of participants reported current concurrent use of two or more substances (Table 1). Cannabis, tobacco, and amphetamine/khat had the highest frequency of use, with many reporting daily use (Figure 1).
Table 1.
Frequency of lifetime and current substance use among study participants.
| Substance type | Lifetime use N = 287 (%) | Current use (past 1 year) N = 301 (%) |
|---|---|---|
| Any alcohol use | 287 (95.3) | 286 (95.1) |
| Risky drinking (AUDIT score ≥8) | 244 (85.0) | 244 (81.1) |
| Nondrinker or low-level problem drinker (AUDIT Score 0–7) | 42 (14.6) | 42 (14.0) |
| Hazardous or moderate-level problem drinker (AUDIT score 8–15) | 60 (20.9) | 60 (21.0) |
| Harmful or high-level problem drinker (AUDIT score 16–19) | 33 (11.5) | 33 (11.5) |
| Very high risk or probably dependent drinker (AUDIT score ≥20) | 151 (52.6) | 151 (50.2) |
| Current use (past 3 months) | ||
| Tobacco | 102 (33.9) | 93 (30.9) |
| Cannabis | 189 (62.8) | 185 (61.5) |
| Khat and other Amphetamine Type Stimulants (ATS) | 144 (47.8) | 142 (47.2) |
| Cocaine | 18 (6.0) | 14 (4.6) |
| Opioids (heroin) | 3 (1.0) | 2 (0.7) |
| Inhalation | 11 (3.7) | 8 (2.66) |
| Sedatives | 18 (6.0) | 14 (4.65) |
| Hallucinogen | 19 (6.3) | 15 (5.0) |
| Others | 2 (0.7) | 2 (0.7) |
| Polysubstance use | ||
| 2 Substances used | 97 (32.8) | 96 (32.0) |
| 3 Substances used | 97 (32.8) | 96 (32.0) |
| >3 Substances used | 85 (28.2) | 80 (26.6) |
Figure 1.
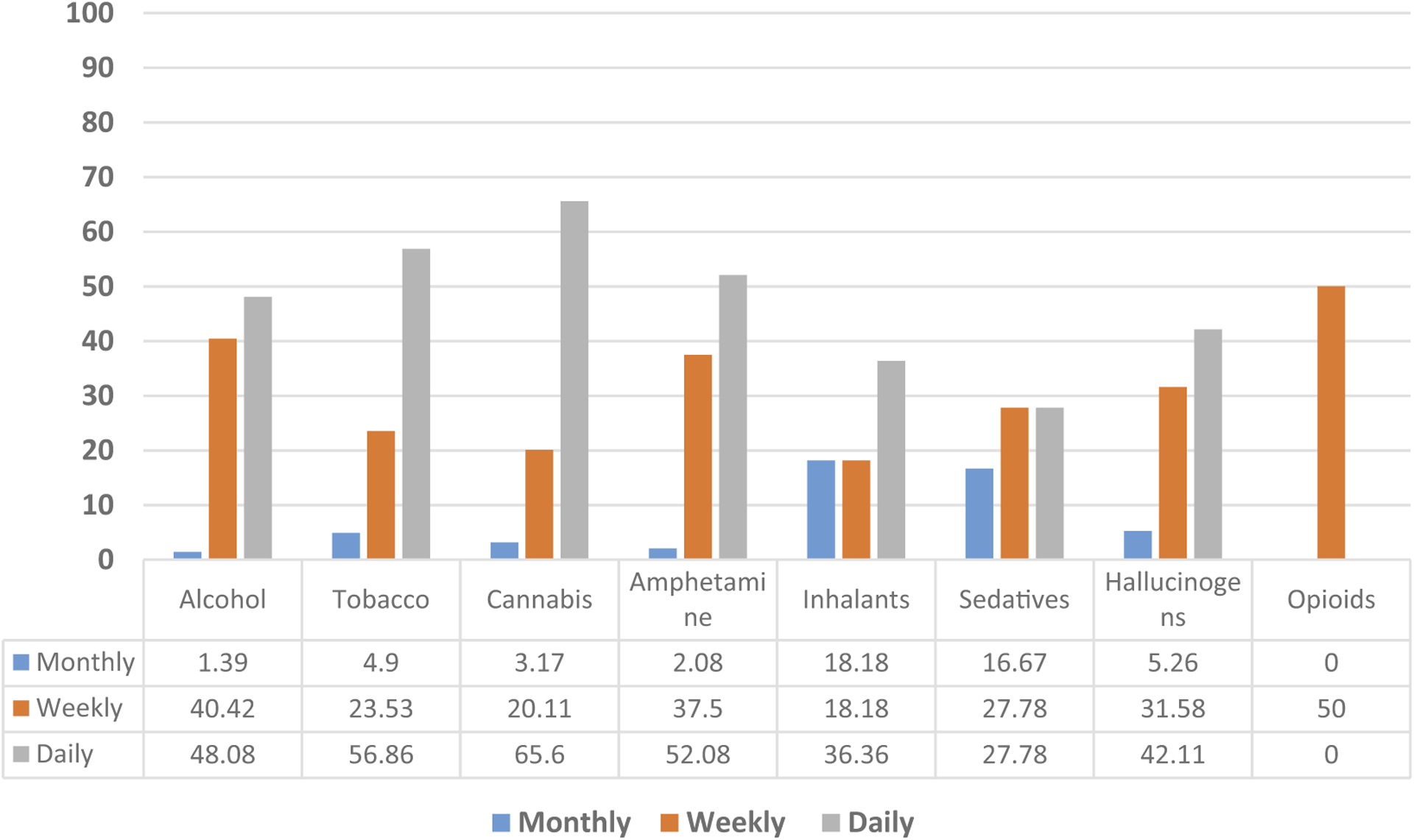
Percentage of sample endorsing substance use displayed separately for daily, weekly, and monthly use among those using each substance.
Factors associated with substance use
Disclosure of sex work to close relatives and friends (adjusted odds ratio [AOR] = 5.53, 95% CI 2.30–13.30), and earning a monthly income of between USD150 and USD250 (AOR 3.97, 95% CI 1.28–12.35), adjusted for age was more likely to contribute to hazardous and harmful alcohol use in the past year, this association became null when income increased over USD250 AOR of 3.18, 95% CI 0.71–14.33 (Table 3). Location of sex work identified as the client’s home was only significant in the bivariate analysis in increasing odds of hazardous and harmful alcohol use (OR 2.67, 95% CI 1.31–5.46) (Table 2).
Table 3.
Adjusted odds ratio for factors associated with substance use among FSWs.
| Alcohol use (AUDIT score ≥8) n = 286 AOR (95% CI) | Cannabis n = 301 AOR (95% CI) | Khat n = 301 AOR (95% CI) | Polysubstance Use (>2) n = 301 AOR (95% CI) | |
|---|---|---|---|---|
| Age, mean | ||||
| 14–19 | 0.60 (0.21, 1.71) | 2.87 (1.20, 6.83)* | 1.53 (0.62, 3.78) | 0.74 (0.29, 1.88) |
| 20–24 | 1.93 (0.72, 5.18) | 2.46 (1.21, 4.98)* | 2.08 (0.95, 4.53) | 1.96 (0.83, 4.62) |
| 25–29 | 1.34 (0.45, 3.93) | 1.56 (0.75, 3.24) | 2.75 (1.28, 5.91)** | 1.67 (0.74, 3.77) |
| 30+ | 1.0 | 1.0 | 1.0 | 1.0 |
| Marital status | ||||
| Single | 1.49 (0.80, 2.77) | 1.96 (0.98, 3.94) | ||
| Widowed | 5.73 (1.73, 19.04)** | 4.39 (0.92, 20.89) | ||
| Divorced/Separated | 1.0 | 1.0 | ||
| Single-parent home | ||||
| Yes | 1.97 (1.00, 3.89) | 3.47 (1.82, 6.58)*** | 2.71 (1.15, 6.39)* | |
| No | 1.0 | 1.0 | 1.0 | |
| Monthly income from sex work (USD) | ||||
| <50. 00 | 1.0 | 1.0 | ||
| 50.00–149.99 | 3.11 (1.20, 8.05)* | 2.68 (1.19, 6.01)* | ||
| 150.00–250.00 | 3.97 (1.28, 12.35)* | 3.33 (1.38, 8.01)** | ||
| >250.00 | 3.18 (0.71, 14.33) | 2.96 (0.98, 8.99) | ||
| Duration of sex work | ||||
| <2 yrs | 1.0 | |||
| 2–4 yrs | 2.67 (1.14, 6.24)* | |||
| 5–9 yrs | 3.72 (1.47, 9.43)** | |||
| 10+ yrs | 3.40 (1.03, 11.18)* | |||
| Location of sex work | ||||
| Vehicle | 1.80 (0.75, 4.34) | 1.91 (0.86, 4.22) | ||
| Client house | 1.93 (0.88, 4.23) | 1.35 (0.81, 2.25) | ||
| Disclosure of sex work | ||||
| Yes | 5.53 (2.30, 13.30)*** | |||
| No | 1.0 |
p < .001;
p < .01;
p < .05
NB: The Hosmer–Lemeshow goodness-of-fit test was not significant for all our fitted models (χ2 = 13.06, p = .2896; χ2 = 3.63, p = .9795; χ2 = 2.39, p = .9665; and χ2 = 2.24, p = .9726), indicating the models fit the data well.
Table 2.
Univariate analysis (unadjusted odds ratio) of factors associated with substance use.
| Alcohol use (AUDIT score ≥8) n = 286† OR (95% CI) | Cannabis n = 301 OR (95% CI) | Khat n = 301 OR (95% CI) | Polysubstance use (≥2) n = 301 OR (95% CI) | |
|---|---|---|---|---|
| Age, mean | ||||
| 14–19 | 0.72 (0.28, 1.85) | 1.69 (0.81, 3.51) | 1.55 (0.74, 3.24) | 1.01 (0.47, 2.19) |
| 20–24 | 1.62 (0.68, 3.85) | 2.03 (1.10, 3.73)* | 2.22 (1.20, 4.12)* | 2.67 (1.28, 5.53)** |
| 25–29 | 1.47 (0.56, 3.87) | 1.53 (0.78, 3.02) | 2.27 (1.14, 4.52)* | 1.70 (0.78, 3.69) |
| 30+ | 1.0 | 1.0 | 1.0 | 1.0 |
| Duration in Kibera | ||||
| <5 yrs | 1.0 | 1.0 | 1.0 | 1.0 |
| 5–10 yrs | 0.75 (0.26, 2.23) | 1.01 (0.50, 2.06) | 0.82 (0.41, 1.67) | 1.27 (0.57, 2.83) |
| 11+ yrs | 0.72 (0.25, 2.03) | 1.46 (0.74, 2.90) | 1.10 (0.56, 2.14) | 1.41 (0.65, 3.04) |
| Marital status | ||||
| Single | 0.76 (0.37, 1.56) | 1.62 (1.00, 2.65) | 1.61 (0.99, 2.62) | 2.03 (1.16, 3.54)* |
| Widowed | 1.00 (0.20, 4.91) | 1.86 (0.61, 5.73) | 3.51 (1.14, 10.81)* | 3.17 (0.68, 14.74) |
| Divorced/Separated | 1.0 | 1.0 | 1.0 | 1.0 |
| Education | ||||
| Primary or below | 1.02 (0.52, 1.98) | 0.79 (0.50, 1.26) | 0.82 (0.52, 1.29) | 0.88 (0.51, 1.51) |
| Secondary or higher | 1.0 | 1.0 | 1.0 | 1.0 |
| Single-parent home | ||||
| Yes | 2.15 (0.81, 5.74) | 2.01 (1.07, 3.76)* | 3.40 (1.85, 6.24)*** | 2.63 (1.14, 6.08)* |
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Monthly income from sex work (USD) | ||||
| <50.00 | 1.0 | 1.0 | 1.0 | 1.0 |
| 50.00–149.99 | 4.11 (1.76, 9.60)** | 2.41 (1.14, 5.09)* | 1.25 (0.59, 2.62) | 1.26 (0.57, 2.81) |
| 150.00–250.00 | 7.15 (2.52, 20.27)*** | 3.49 (1.55, 7.85)** | 1.76 (0.80, 3.89) | 2.29 (0.92, 5.71) |
| >250.00 | 5.85 (1.47, 23.30)* | 3.67 (1.31, 10.26)* | 1.80 (0.67, 4.79) | 2.20 (0.67, 7.26) |
| Duration of sex work | ||||
| <2 yrs | 1.0 | 1.0 | 1.0 | 1.0 |
| 2–4 yrs | 1.08 (0.33, 3.49) | 2.36 (1.06, 5.25)* | 1.32 (0.59, 2.95) | 1.43 (0.60, 3.42) |
| 5–9 yrs | 0.86 (0.26, 2.83) | 2.30 (1.00, 5.25)* | 1.39 (0.61, 3.17) | 1.87 (0.74, 4.73) |
| 10+ yrs | 0.83 (0.18, 3.76) | 1.66 (0.57, 4.85) | 1.63 (0.56, 4.75) | 1.10 (0.34, 3.56) |
| Location of sex work | ||||
| Brothel | 1.59 (0.20, 12.89) | 1.47 (0.37, 5.81) | 4.76 (0.99, 22.82) | 1.17 (0.24, 5.65) |
| Lodging | 1.96 (0.20, 19.30) | 1.61 (0.22, 11.56) | 2.71 (0.28, 26.37) | - |
| Massage parlor | 2.34 (0.30, 18.36) | 0.82 (0.28, 2.44) | 0.62 (0.20, 1.89) | 0.72 (0.22, 2.36) |
| Vehicle | 2.50 (1.10, 5.67)* | 2.69 (1.29, 5.54)** | 2.00 (0.75, 5.37) | |
| Client house | 2.67 (1.31, 5.46)** | 1.75 (1.09, 2.82)* | 1.28 (0.81, 2.01) | 1.68 (0.96, 2.94) |
| Own house | 2.18 (0.74, 6.42) | 1.26 (0.66, 2.38) | 1.06 (0.58, 1.95) | 1.20 (0.56, 2.55) |
| Disclosure of sex work | ||||
| Yes | 6.21 (2.90, 13.30)*** | 1.73 (0.90, 3.33) | 1.37 (0.71, 2.66) | 1.26 (0.60, 2.66) |
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Condom use with clients | ||||
| Yes | 1.0 | 1.0 | 1.0 | 1.0 |
| Sometimes/No | 1.43 (0.68, 2.98) | 1.19 (0.72, 1.96) | 1.14 (0.70, 1.86) | 0.95 (0.53, 1.70) |
p < .001;
p < .01;
p < .05
Fifteen respondents did not provide AUDIT tool response. Fourteen of them had reported to have never taken alcohol in their lifetime while one though stated that they had taken alcohol in the last 3 months, failed to respond to AUDIT tool section.
For cannabis use in the past 3 months, four variables remained significant in the multivariable analysis. Younger mean age of between 14 and 24 years (AOR 2.87, 95% CI 1.20–6.83) and 20–24 years (AOR 2.46, 95% CI 1.21–4.98) relative to older age ≥25 years, being raised in a single-parent home (AOR 1.97, 95% CI 1.00–3.89) compared to ones raised in a family with both parents, monthly income of between USD50–149 USD (AOR 2.68, 95% CI 1.19–6.01) and $USD150–250 (AOR 3.33, 95% CI 1.38–8.01) relative to monthly income <USD50 and sex work duration of 2–4 years (AOR 2.67, 95% CI 1.14–6.24), 5–9 years (AOR 3.72, 95% CI 1.47–9.43) and ≥10 years (AOR 3.40, 95% CI 1.03–11.18) relative to <2-year sex duration showed significant association to cannabis use in the past 3 months (Table 3).
Similar to cannabis use, for khat use, significance in the multivariable analysis was seen for FSWs reporting being raised in single parent with an AOR of 3.47, 95% CI 1.82–6.58. However, unlike cannabis use, an older age group of between 25 and 29 years remained significant in the multivariable analysis with an AOR of 2.75, 95% CI 1.28–5.91 (Table 3).
For polysubstance use, only being raised in a single-parent home remained significant in the multivariable analysis (AOR 2.71, 95% CI 1.15–6.39). Other variables, such as mean age of 20–24 and single marital status, were only significant in the bivariate analysis with an OR 2.67, 95% CI 1.28–5.53, and OR 2.03, 95% CI 1.16–3.54, respectively (Table 2).
Being raised in a single-parent home increased the odds of reporting current cannabis, khat, and polysubstance use among women in this study relative to ones raised in a family with both parents (Table 3).
Discussion
We found a high prevalence of substance use in this study sample. Our findings are consistent with other studies reporting similarly high prevalence of substance use among FSWs (Odukoya et al. 2013; Scorgie et al. 2012; Yadav et al. 2013). Prior work has suggested that this high prevalence can be attributed to the stressful living and work environment of these women, as well as the acceptability and accessibility of psychoactive substances (Chen et al. 2015; Lancaster et al. 2018; Syvertsen et al. 2019).
Alcohol, tobacco, cannabis, and khat had the highest prevalence of use. However, cannabis, tobacco, and khat, in that order, had the highest frequency of daily use. This finding is consistent with prior work reporting that the stimulating property of these substances is preferred in an attempt to improve energy and motivation for sex work rather than the depressant effect of other substances like alcohol (Katie et al. 2016). Differences in patterns of daily use may also be due to cost. Cannabis, tobacco, and khat are more affordable relative to other substances, and this may contribute to ease of access and subsequent use. Nevertheless, although fewer reported daily use of alcohol, compared to cannabis, tobacco, and khat, nearly all (95%) of participants reported use of alcohol in the past 3 months with a majority of those (85%) being classified as hazardous or harmful drinkers. More than half of all participants (52.8%) were very high-risk drinkers based on the AUDIT cut off score of 20 or more. Prior work has suggested that the prevalence of high-risk drinking among FSWs may be attributed to cultural acceptance and promotion of alcohol in the FSW line of work (Li, Li, and Stanton, n.d.; Sudhinaraset, Wigglesworth, and Takeuchi 2016). In our study, the majority of participants reported conducting sex work within lodgings, which are local settings in Kibera that promote the sale and consumption of alcohol. It may be that conducting sex work in lodgings increases the risk for substance use, a possibility that warrants further investigation
The prevalence of injection drug use (IDU) was low (1%) in our sample. Studies in other settings have found higher rates (Strathdee et al. 2008). The baseline prevalence of IDU in Kenya is lower (0.3%) relative to other locations (Okal et al. 2013), possibly explaining the lower prevalence among IDUs in this sample.
In the adjusted analysis, we found that women in their early 20s were twice as likely to use cannabis and khat, as compared to women 30 years and older. Other studies have similarly found illicit drug use among women to be higher among 18–25 year age-group compared to an older demographic (McHugh, Wigderson, and Greenfield 2014). Younger age may be associated with greater vulnerability to social influences, for example, through peer pressure to use substances, relative to older adults (Gardner and Steinberg 2005; Jaccard, Blanton, and Dodge 2005).
FSWs who were widowed were 6 times more likely to report khat use compared to divorced or separated women, while single women were twice as likely to report polysubstance use. An unmarried marital status has been associated with higher rates of substance use in some studies (Sharma, Singh, and Talukdar 2016), while others have found the reverse (Medhi et al. 2012). In our sample, only one participant reported as cohabiting and none were married. Therefore, it is likely that we were underpowered to detect a reliable association.
A single-parent household upbringing tripled the likelihood of women reporting use of khat. Family structure has been shown to have a significant impact on substance use patterns in later life (Barrett and Jay Turner 2006; Lander, Howsare, and Byrne 2013; Vanessa and Crano 2009). For example, the absence of a biological parent was associated with increased cannabis use among adolescents in a multi-country analysis, a finding consistent with our results (Hoffmann 2017; Lander, Howsare, and Byrne 2013).
Earning a monthly income greater than USD50 was associated with reporting harmful or hazardous alcohol intake and cannabis use. Higher income may increase capacity to purchase and use alcohol and cannabis. However, higher-income participants may also experience increased demands for transactional sex or engage in riskier, higher-paying transactional sex, which in turn increases reliance on psychoactive substances as a coping strategy. Previous research has shown that income from sex work is linked to the number of clients being served as well as the riskiness of sex work involved (Harcourt and Donovan 2005; Surratt 2007).
Participants who had disclosed their sex work status to close relatives and friends were 6 times more likely to report hazardous or harmful use of alcohol. Disclosure of highly stigmatized sex work might be expected to lower distress given increase in social support and could potentially protect against harmful drinking. However, sex work-related stigma and discrimination is prevalent globally (Benoit et al. 2018; Benoit, McCarthy, and Jansson 2015; Dourado et al. 2019).
Disclosure of sex status may further increase distress if stigma and discrimination increase as a result. It is possible that women in turn attempt to cope with stigma and discrimination with alcohol use. It is also possible that women likely to disclose alcohol use in the context of this study are also more likely to disclose sex-work status to friends and family, thereby reflecting individual differences in comfort with reporting, rather than a pathway for potential alcohol use risk.
The stigmatized and illegal nature of sex work results in many barriers to carrying out research in this setting. To address this, studies of sex workers often rely on respondent-driven sampling (RDS). We employed a modified RDS (Denckla et al. 2019) procedure to ensure that the FSWs in the study were actually earning income from transactional sex. In this setting of extreme poverty, there was some risk that participants may have sought enrollment simply for income regardless of employment status. Though necessary, this modification may have introduced a sampling bias such that only those FSWs known to group leaders were recruited for the study. A second limitation is that although the translated ASSIST and AUDIT were piloted, a full validation study in this setting prior to administration was not undertaken. However, both the original ASSIST and AUDIT were designed and validated in populations within Sub Saharan Africa and have shown strong validity and reliability (Kane et al. 2016; Saunders et al. 1993). Third, all data were based on self-report and could be prone to retrospective bias. Finally, this was a cross-sectional study; hence, temporality and causality cannot be established.
In conclusion, there is a high rate of substance use and high-risk drinking in this sample of female sex workers, further compounding social and physical health risks. Prevention, health promotive and curative strategies targeted at alcohol and substance use disorders are warranted.
Supplementary Material
Acknowledgments
The authors would like to thank i) the Kibera community health volunteers (Edwina Achieng and Pamella Owino) for their consultative and sensitization role in the study. and ii) acknowledge posthumously Julia Amayo, the director of our partner community-based organization in Kibera for her consultative role in this project.
Funding
This research was funded by the Kenya Medical Research Internal Research Grants SP/IRG/01013. The funding body, however, did not participate in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Footnotes
Supplemental data for this article can be accessed on the publisher’s website
A psychoactive substance chewed for its amphetamine like properties. Khat formed the largest contribution of amphetamine like substances reported and hence used interchangeably in the text.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Babor TF, Higgins-Biddle JC, Saunders JB, and Monteiro MG; World Health Organization. 2001. AUDIT : The alcohol use disorders identification test : Guidelines for use in primary health care. 2nd ed. Geneva: World Health Organization. [Google Scholar]
- Barrett AE, and Jay Turner R. 2006. Family structure and substance use problems in adolescence and early adulthood: Examining explanations for the relationship. Addiction 101 (1):109–20. doi: 10.1111/j.1360-0443.2005.01296.x. [DOI] [PubMed] [Google Scholar]
- Benoit C, Jansson SM, Smith M, and Flagg J. 2018. Prostitution stigma and its effect on the working conditions, personal lives, and health of sex workers. The Journal of Sex Research 55 (4–5):457–71. doi: 10.1080/00224499.2017.1393652. [DOI] [PubMed] [Google Scholar]
- Benoit C, McCarthy B, and Jansson M. 2015. Stigma, sex work, and substance use: A comparative analysis. Sociology of Health & Illness 37 (3):437–51. doi: 10.1111/1467-9566.12201. [DOI] [PubMed] [Google Scholar]
- Chen Y, Li X, Shen Z, Zhou Y, and Tang Z. 2015. Drinking reasons and alcohol problems by work venue among female sex workers in Guangxi, China. Substance Use & Misuse 50 (5):642–52. doi: 10.3109/10826084.2014.997827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chersich MF, Bosire W, King’ola N, Temmerman M, and Luchters S. 2014. Effects of hazardous and harmful alcohol use on HIV incidence and sexual behaviour: A cohort study of Kenyan female sex workers. Globalization and Health 10 (January):22. doi: 10.1186/1744-8603-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chersich MF, Luchters SMF, Malonza IM, Mwarogo P, King’ola N, and Temmerman M. 2007. Heavy episodic drinking among Kenyan female sex workers is associated with unsafe sex, sexual violence and sexually transmitted infections. International Journal of STD & AIDS 18 (11):764–69. doi: 10.1258/095646207782212342. [DOI] [PubMed] [Google Scholar]
- Denckla CA, Ongeri L, Ouma L, Singa B, Maingi C, Bosire R, Otieno P, et al. 2019. Prevalence of parental bereavement among female sex workers (FSW) in Kibera, Kenya. Journal of Loss and Trauma 24 (2). doi: 10.1080/15325024.2018.1560692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine A, Bowen K, Dzuvichu B, Rungsung R, and Kermode M. 2010. Pathways to sex-work in Nagaland, India: Implications for HIV prevention and community mobilisation. AIDS Care 22 (2):228–37. doi: 10.1080/09540120903039869. [DOI] [PubMed] [Google Scholar]
- Dourado I, Guimarães MDC, Damacena GN, Magno L, de Souza Júnior PRB, and Szwarcwald CL. 2019. Sex work stigma and non-disclosure to health care providers: Data from a large RDS study among FSW in Brazil. BMC International Health and Human Rights 19 (1):8. doi: 10.1186/s12914-019-0193-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enkins C 2006. Violence and exposure to HIV among sex workers in Phnom Penh, Cambodia. https://www.hivpolicy.org/Library/HPP001702.pdf
- Gardner M, and Steinberg L. 2005. Peer influence on risk taking, risk preference, and risky decision making in adolescence and adulthood: An experimental study. Developmental Psychology 41 (4):625–35. doi: 10.1037/0012-1649.41.4.625. [DOI] [PubMed] [Google Scholar]
- Harcourt C, and Donovan B. 2005. The many faces of sex work. Sexually Transmitted Infections 81 (3):201–06. doi: 10.1136/sti.2004.012468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcourt C, Donovan B, and Harcourt C. 2005. The many faces of sex work. Sex Transm Infect 81 (3):201–06. doi: 10.1136/sti.2004.012468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann JP 2017. Family structure and adolescent substance use: An international perspective. Substance Use and Misuse 52 (13):1667–83. doi: 10.1080/10826084.2017.1305413. [DOI] [PubMed] [Google Scholar]
- Jaccard J, Blanton H, and Dodge T. 2005. Peer influences on risk behavior: An analysis of the effects of a close friend. Developmental Psychology 41 (1):135–47. doi: 10.1037/0012-1649.41.1.135. [DOI] [PubMed] [Google Scholar]
- Kane JC, Murray LK, Bass JK, Johnson RM, and Bolton P. 2016. Validation of a substance and alcohol use assessment instrument among orphans and vulnerable children in Zambia using audio computer assisted self-interviewing (ACASI). Drug and Alcohol Dependence 166 (September):85–92. doi: 10.1016/j.drugalcdep.2016.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katie H-J, Choi S, Duo L, Luo Z, and Jennifer Huang Z. 2016. Occupational and demographic factors associated with drug use among female sex workers at the China–Myanmar border. Drug and Alcohol Dependence 161 (April):42–49. doi: 10.1016/j.drugalcdep.2016.01.026. [DOI] [PubMed] [Google Scholar]
- Lancaster KE, MacLean SA, Lungu T, Mmodzi P, Hosseinipour MC, Hershow RB, Powers KA, et al. 2018. Socioecological factors related to hazardous alcohol use among female sex workers in Lilongwe, Malawi: A mixed methods study. Substance Use & Misuse 53 (5):782–91. doi: 10.1080/10826084.2017.1365088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lander L, Howsare J, and Byrne M. 2013. The impact of substance use disorders on families and children: From theory to practice. Social Work in Public Health 28 (3–4):194–205. doi: 10.1080/19371918.2013.759005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Li X, and Stanton B. n.d. Alcohol use among female sex workers and male clients: An integrative review of global literature. Alcohol and Alcoholism (Oxford, Oxfordshire) 45 (2):188–99. doi: 10.1093/alcalc/agp095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchters S, Geibel S, Syengo M, Lango D, King’ola N, Temmerman M, and Chersich MF. 2011. Use of AUDIT, and measures of drinking frequency and patterns to detect associations between alcohol and sexual behaviour in male sex workers in Kenya. BMC Public Health 11 (May):384. doi: 10.1186/1471-2458-11-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Wigderson S, and Greenfield SF. 2014. Epidemiology of substance use in reproductive-age women. Obstetrics and gynecology clinics of North America 41 (2): 117. doi: 10.1016/j.ogc.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medhi GK, Mahanta J, Kermode M, Paranjape RS, Adhikary R, Kumar Phukan S, and Ngully P. 2012. Factors associated with history of drug use among female sex workers (FSW) in a high HIV prevalence state of India. BMC Public Health 12 (January):273. doi: 10.1186/1471-2458-12-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moret JED, Carrico AW, Evans JL, Stein ES, Couture M-C, Maher L, and Page K; Young Women’s Health Study Collaborative. 2016. The impact of violence on sex risk and drug use behaviors among women engaged in sex work in Phnom Penh, Cambodia. Drug and Alcohol Dependence 161 (April):171–77. doi: 10.1016/j.drugalcdep.2016.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NASCOP & KEMRI. 2015. Guidelines for conducting adolescent HIV sexual and reproductive health research in Kenya. Government of Kenya. http://icop.or.ke/wp-content/uploads/2016/10/Adolescents-Guidance-on-HIV-SRH-Research.pdf. [Google Scholar]
- Odukoya OO, Sekoni AO, Onajole AT, and Upadhyay RP. 2013. Alcohol consumption and cigarette smoking pattern among brothel-based female sex workers in two local government areas in Lagos State, Nigeria. African Health Sciences 13 (2):490–97. doi: 10.4314/ahs.v13i2.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okal J, Geibel S, Muraguri N, Musyoki H, Tun W, Broz D, Kuria D, Kim A, Oluoch T, and Fisher Raymond H. 2013. Estimates of the size of key populations at risk for HIV infection: Men who have sex with men, female sex workers and injecting drug users in Nairobi, Kenya. Sexually Transmitted Infections 89 (5):366–71. doi: 10.1136/sex-trans-2013-051071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Othieno CJ, Obondo A, and Mathai M. 2012. Improving adherence to ante-retroviral treatment for people with harmful alcohol use in Kariobangi, Kenya through participatory research and action. BMC Public Health 12 (January):677. doi: 10.1186/1471-2458-12-677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda S, Bijaya L, Sadhana Devi N, Foley E, Chatterjee A, Banerjee D, Naik TN, Saha MK, and Bhattacharya SK. 2001. Interface between drug use and sex work in Manipur. The National Medical Journal of India 14 (4):209–11. [PubMed] [Google Scholar]
- Roberts A, Mathers B, and Degenhardt L. 2010. Women who inject drugs: A review of their risks, experiences and needs. https://www.unodc.org/documents/hiv-aids/Women_who_inject_drugs.pdf.
- Roshanfekr P, Noori R, Dejman M, Fathi Geshnigani Z, and Rafiey H. 2015. Drug use and sex work among at-risk women: A qualitative study of initial factors. Iranian Journal of Psychiatry and Behavioral Sciences 9 (2):e953. doi: 10.17795/ijpbs953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross R, Simon C, Stimson G, Tanguay P, Verster A, Clay C, Derozier S, et al. 2013. When sex work and drug use overlap: Considerations for advocacy and practice. Www.Ihra.Net
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, and Grant M. 1993. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 88 (6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Scorgie F, Chersich MF, Ntaganira I, Gerbase A, Lule F, and Lo Y-R. 2012. Socio-demographic characteristics and behavioral risk factors of female sex workers in Sub-Saharan Africa: A systematic review. AIDS and Behavior 16 (4):920–33. doi: 10.1007/s10461-011-9985-z. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Stockman JK, Pitpitan EV, Strathdee SA, Chavarin CV, Mendoza DV, Aarons GA, and Patterson TL. 2015. Prevalence and correlates of client-perpetrated violence against female sex workers in 13 Mexican Cities. Edited by Jesse Lawton Clark. PloS One 10 (11):e0143317. doi: 10.1371/journal.pone.0143317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma SK, Singh SK, and Talukdar B. 2016. Understanding the factors associated with alcohol use among female sex workers in a high HIV Prevalence Northeast State of India. Journal of Infectious Diseases and Treatment 2 (1). doi: 10.21767/2472-1093.100017. [DOI] [Google Scholar]
- Strathdee SA, Philbin MM, Semple SJ, Minya P, Orozovich P, Martinez G, Lozada R, et al. 2008. Correlates of injection drug use among female sex workers in two Mexico-U.S. Border Cities. Drug and Alcohol Dependence 92 (1–3):132. doi: 10.1016/J.DRUGALCDEP.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, West BS, Reed E, Moazen B, Moazan B, Azim T, and Dolan K. 2015. Substance use and HIV among female sex workers and female prisoners: Risk environments and implications for prevention, treatment, and policies. Journal of Acquired Immune Deficiency Syndromes (1999) 69 Suppl 2 (1):S110–7. doi: 10.1097/QAI.0000000000000624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudhinaraset M, Wigglesworth C, and Takeuchi DT. 2016. Social and cultural contexts of alcohol use: Influences in a social–ecological framework. Alcohol Research : Current Reviews 38 (1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surratt H 2007. Sex work in the Caribbean basin: patterns of substance use and HIV risk among migrant sex workers in the US Virgin Islands. AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV 19 (10):1274–82. doi: 10.1080/09540120701426490. [DOI] [PubMed] [Google Scholar]
- Syvertsen JL, Agot K, Ohaga S, and Robertson Bazzi A. 2019. You can’t do this job when you are sober: Heroin use among female sex workers and the need for comprehensive drug treatment programming in Kenya. Drug and Alcohol Dependence 194 (January):495–99. doi: 10.1016/j.drugalcdep.2018.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tegang SP, Abdallah S, Emukule G, Luchters S, Kingola N, Baras M, Mucheke S, and Mwarogo P. 2010. Concurrent sexual and substance-use risk behaviours among female sex workers in Kenya’s coast province: Findings from a behavioural monitoring survey. SAHARA J : Journal of Social Aspects of HIV/AIDS Research Alliance 7 (4):10–16. doi: 10.1080/17290376.2010.9724972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanessa H, and Crano WD. 2009. Family structure and adolescent drug use: An exploration of single-parent families. Substance Use and Misuse 44 (14):2099–113. doi: 10.3109/10826080902858375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO ASSIST Working Group. 2002. The alcohol, smoking and substance involvement screening test (ASSIST): Development, reliability and feasibility. Addiction (Abingdon, England) 97 (9):1183–94. http://www.ncbi.nlm.nih.gov/pubmed/12199834. [DOI] [PubMed] [Google Scholar]
- Yadav D, Ramanathan S, Goswami P, Ramakrishnan L, Sen S, George B, Paranjape R, Subramanian T, and Rachakulla H. 2013. P6.016 factors associated with frequent alcohol use among female sex workers in three high prevalence States of India: Findings from a bio-behavioural survey. Sexually Transmitted Infections 89 (Suppl 1):A374.2–A374. doi: 10.1136/sextrans-2013-051184.1170. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


