Abstract
Background
Efforts to develop neuroimaging-based biomarkers in major depressive disorder (MDD), at the individual level, have been limited to date. As diagnostic criteria are currently symptom-based, MDD is conceptualized as a disorder rather than a disease with a known etiology; further, neural measures are often confounded by medication status and heterogeneous symptom states.
Methods
We describe a consortium to quantify neuroanatomical and neurofunctional heterogeneity via the dimensions of novel multivariate coordinate system (COORDINATE-MDD). Utilizing imaging harmonization and machine learning methods in a large cohort of medication-free, deeply phenotyped MDD participants, patterns of brain alteration are defined in replicable and neurobiologically-based dimensions and offer the potential to predict treatment response at the individual level.
International datasets are being shared from multi-ethnic community populations, first episode and recurrent MDD, which are medication-free, in a current depressive episode with prospective longitudinal treatment outcomes and in remission. Neuroimaging data consist of de-identified, individual, structural MRI and resting-state functional MRI with additional positron emission tomography (PET) data at specific sites. State-of-the-art analytic methods include automated image processing for extraction of anatomical and functional imaging variables, statistical harmonization of imaging variables to account for site and scanner variations, and semi-supervised machine learning methods that identify dominant patterns associated with MDD from neural structure and function in healthy participants.
Results
We are applying an iterative process by defining the neural dimensions that characterise deeply phenotyped samples and then testing the dimensions in novel samples to assess specificity and reliability. Crucially, we aim to use machine learning methods to identify novel predictors of treatment response based on prospective longitudinal treatment outcome data, and we can externally validate the dimensions in fully independent sites.
Conclusion
We describe the consortium, imaging protocols and analytics using preliminary results. Our findings thus far demonstrate how datasets across many sites can be harmonized and constructively pooled to enable execution of this large-scale project.
Keywords: Classification, Biomarkers, Deep learning, Neuroimaging, Depression, Harmonization, Predictors, MRI
Background
Depression has been recognized for millennia as a distinct illness, included in what Hippocrates termed ‘melancholia’ and posited to be caused by black bile. Current diagnostic criteria for major depressive disorder (MDD) are based solely on a set of symptoms and observable behaviors. MDD is characterised by a persistent low mood and/or an inability to experience usual feelings of enjoyment, associated with disturbances in sleep, appetite and psychomotor functioning, low energy, poor concentration, guilt or worthlessness, and, for some, suicidal ideation and behaviors [1, 2]. MDD is highly prevalent and has significant personal, familial and socioeconomic impacts [3, 4]. At the present time, MDD remains a syndrome without an identified etiology, rather than a disease with a demonstrable pathology. There are no neurobiological markers that can identify the diseases which comprise a clinical MDD diagnosis. We lack reproducible neurobiological markers to improve the etiological and prognostic homogeneity as well as to predict response to treatment.
Not only can heterogeneous combinations of symptoms fulfil diagnostic criteria, but current criteria do not fully capture the range of symptoms. For example, high levels of anxiety and comorbid anxiety disorders are present in 50–75% of MDD individuals, which are further linked with impaired treatment response and chronic longitudinal course [5, 6]. Heterogeneity among clinical profiles can lead to less predictable responses to a given treatment, an inability to predict the longitudinal course for individual patients, and the symptom variability in ‘gold standard’ scales designated to evaluate efficacy of therapeutic interventions. Further, treatment outcomes are frequently unsatisfactory. For 30–40% of MDD individuals in a current depressive episode, an adequate treatment response or remission is not achieved even after several trials of pharmacotherapy or psychotherapy over a year [7, 8].
It is unlikely that MDD is caused by a single etiological factor. MDD heritability estimates range from 28 to 44% [9] and are considerably lower than estimates for bipolar disorder and schizophrenia, which range from 60 to 90% [10, 11]. Genome-wide association and candidate gene studies have powerfully demonstrated polygenic heritability, consisting of hundreds of variants and genes with each having a small genetic contribution. However, genetic risk variants have not clinically useful at the individual level for diagnosis, and it is unclear how genetic risk ultimately translates into an acute depressive episode [12].
Neuroimaging-based biomarkers can help to identify the various disease components that comprise MDD. Genetic and environmental factors that lead to MDD are expressed as subtle and widespread alterations in brain structure and brain function. Research over two decades provides convincing evidence of morphometric and neural alterations in MDD, despite limitations in diagnosis and treatment selection. An overarching aim has been to delineate the neurobiological features that comprise MDD and to develop imaging markers in this disorder [13–15]. It is important to recognize though that to search for a neural signature that wholly replicates current diagnostic criteria would be circular, petitio principii, because current diagnostic criteria are based on clinical features and different mechanisms could lead to the same clinical presentation. Efforts have been further hindered by neural measures which have been confounded by a mixture of depressive states, multiple and longstanding treatments, as well as comorbid disorders.
In recent years, machine learning based methods for MRI heterogeneity analysis have been developed which detect and characterize neuroanatomical heterogeneity of disease using a data-driven approach that generates quantifiable, replicable and neurobiologically-based metrics of disease subtypes [16]. Large samples have recently been created from multi-site datasets, however the multivariate pattern analysis has been limited to either resting-state functional MRI data or structural MRI data with limited clinical phenotyping and lack of longitudinal treatment outcome data. From resting-state functional MRI data, four functional connectivity patterns were observed in frontostriatal and limbic systems which reflected different symptom profiles [17]. However, the training and cross-validation samples were confounded by medication and form of depression, namely treatment-resistant depression, which has demonstrable effects on brain structure and function [18–20], and there was no independent testing in a novel sample. Moreover, the models were not reproduced in an independent study [21], which could reflect overfitting in the clustering algorithm as well as insufficient overlap in the sample characteristics. Resting state functional MRI reflects depressive state, and these samples had distinct depressive states, multiple comorbid disorders, different forms of depression, with neurofunctional correlates that were likely underpowered for such non-overlapping samples [17–21].
In structural MRI, recent multi-site cohorts show classification accuracies ranging from 52 to 75% [22–25]. However, all the dimensions have been binary (ie. either MDD or healthy control). The highest classification accuracy was achieved in a cohort with a MDD diagnosis based on diagnostic criteria and that was in a current depressive episode, but the sample size was limited (230 MDD, 77 controls) [22]. In the largest sample to date (2288 MDD and 3077 controls), the Enhancing Neuro Imaging Genetics through Meta-Analysis (ENIGMA) consortium found a classification accuracy up to 62% [23]. However, the ENIGMA MDD sample consists of a wide range of clinical phenotypes, with multiple comorbid disorders, many forms of depression from first episode to treatment-resistant depression, but limited medication history, antidepressant dosage or duration, and no treatment outcome data [26]. Similarly, large samples from UK Biobank data have limited treatment history, no treatment outcome data, and are based on a probable diagnosis of lifetime MDD derived from self-report symptoms in a population-based sample [27].
Our consortium aims to identify imaging signatures of disease heterogeneity in MDD using structural and resting state functional MRI. This will generate a neuroanatomical-neurofunctional (NA-NF) dimensional coordinate system (COORDINATE-MDD) in which each dimension captures a distinct pattern of brain alterations. Our aim is to identify the multivariate dimensions that define disease-related phenotypes in MDD and the distinct dimensions that predict treatment response at the individual level. Importantly, this is an iterative process to: (i) define neural dimensions in deeply phenotyped participants who are medication-free and in a current depressive episode in order to delineate state and trait status; and (ii) test dimensions in novel samples to assess specificity and reproducibility. With this aim, our consortium combines extensive datasets of ‘raw’ individual-level neuroimaging and deeply phenotyped clinical data, using state-of-the-art analytic methods for big data and semi-supervised clustering. The present sample consists of richly phenotyped, individual-level data from participants with first episode or recurrent MDD, that is not treatment-resistant depression, antidepressant medication-free, with prospective longitudinal treatment outcomes, and healthy controls. The current focus is on structural and resting-state functional MRI.
We have sought to focus on first episode and recurrent MDD in the present sample. Treatment-resistant depression is currently a clinical criterion that refers to a form of depression which shows significant persistent symptoms despite a series of treatments. If treatment resistance is present at the first episode, then it might be possible to identify this dimension early in the illness. Low rates of remission associated with current treatments demonstrate their limitations [28] and could also indicate a subgroup that will progress to fulfil the clinical criterion of treatment resistance. It is possible that the pathophysiology of treatment-resistant depression might be characterized early in the course of illness [14].
Sample size directly influences the capacity of machine learning methods to reliably identify imaging signatures of disease from MRI data and machine learning-based signatures will need to be replicated in independent cohorts. Through international collaborations, we are bringing together a large and integrated sample. MRI images are processed using image processing methods that leverage robust and fully automated pipelines for extracting structural and functional imaging features. In large multi-site datasets, harmonization of imaging features from each site is a critical requirement. We will apply a statistical harmonization methodology, Combat-GAM [29], developed for pooling neuroimaging data across multiple scanners and cohorts with diverse age ranges and with the presence of nonlinear age-related differences in brain images. Combat-GAM has been shown to remove unwanted sources of variability, specifically site differences, while preserving variations due to biologically-relevant covariates in the data. Harmonized data from different scanners and sites are analyzed using machine learning and deep learning methods for imaging pattern analysis. These methods integrate small yet coordinated brain effects into signatures that may yield high sensitivity and specificity in characterizing disease effects in individuals.
The dimensional approach naturally extends to other modalities, including diffusion tensor imaging, task-based functional MRI, and to molecular brain imaging with PET. We will extend these findings to studies of at-risk individuals and to clinical trials in an iterative process [30] in which the position and trajectory of a new individual in a broader dimensional system can be interrogated along with any number of clinical phenotypes, with the potential to study such cohorts over the course of illness and with treatment.
Methods and preliminary results
To establish a NA-NF dimensional system of brain imaging biomarkers and predictors of clinical outcome, we will apply the following steps:
Inter-site harmonization and image analysis to create a methodological platform for constructive integration of structural imaging and neurofunctional connectivity data from multiple sites.
To investigate heterogeneity in neuroanatomy and functional connectivity as a collection of NA-NF patterns or dimensions, we will use semi-supervised AI methods, instead of commonly used clustering (unsupervised) approaches, in order to delineate disease-related effects, rather than variations in brain morphology and physiology that might be caused by a number of disease-irrelevant factors. Validity and relevance of identified dimensions will be verified by cross-validation and replication in independent datasets. Critically, we will derive the presence of each NA-NF signature in each participant.
To evaluate individual NA-NF signatures for their ability to predict or to moderate treatment response, two complementary approaches will be applied. The first approach is wholly data-driven and will assess the degree of expression of each signature to evaluate whether the position in the NA-NF dimensional system predicts treatment response. The second approach incorporates knowledge of treatment type and clinical response to enrich the NA-NF system by dimensions that are strong predictors in order to assess whether accuracy improves with the interaction of NA-NF dimension and clinical knowledge of treatment type and response.
Participating studies and datasets
An invitation for participation was made to research groups to share ‘raw’ neuroimaging data. The present consortium provided medication-free participants with first episode or recurrent MDD, that is not treatment-resistant depression, and healthy controls.
Collaborations have been established with centers worldwide from Canada, China, European Union, United Kingdom and USA. Each center has completed a Data Sharing Agreement to provide de-identified data in accordance with institutional policies and applicable federal, state or local laws and regulations, including ethical approvals. Summary descriptions are below (Tables 1 and 2):
Table 1.
Demographic, clinical and neuroimaging data
| Clinical assessments | |
| Demographic data (age, sex, ethnicity, handedness, IQ, years of education) | |
| Standardised diagnostic criteria (DSM or ICD) | |
| Psychiatric history (including comorbid disorders) | |
| Form of depression (first episode, recurrent, treatment resistant) | |
| Treatment (current, history) | |
| Depression rating scales (HRSD, MADRS, QIDS) | |
| Depressive severity (mild, moderate, severe) | |
| Treatment outcome (baseline and post-treatment rating scale scores, remission, response) | |
| Neuroimaging | |
| Structural MRI | |
| Resting-state fMRI | |
| Diffusion tensor imaging | |
| PET | |
| EEG | |
| Neuropsychological assessments |
Table 2.
Preliminary study demographics, MRI field strength and MRI scanner model
| Study | Number | Mean age | Age range | MRI | MRI scanner model |
|---|---|---|---|---|---|
| CAN-BIND | 309 | 34 | 18–61 | 3 T | GE Discovery MR750 |
| 3 T | GE Signa HDx | ||||
| 3 T | Philips Intera | ||||
| 3 T | Siemens TrioTim | ||||
| EMBARC | 336 | 37 | 18–65 | 3 T | GE Discovery MR750 |
| 3 T | GE Signa HDx | ||||
| 3 T | Philips Achieva | ||||
| 3 T | Philips Ingenia | ||||
| 3 T | Siemens TrioTim | ||||
| KCL | 40 | 30 | 18–45 | 3 T | GE Discovery MR750 |
| LIBR | 296 | 32 | 18–59 | 3 T | GE Discovery MR750 |
| Manchester | 70 | 35 | 20–56 | 1.5 T | Philips Intera |
| NeuroPharm1 | 207 | 28 | 18–59 | 3 T | Siemens Prisma |
| Oxford | 70 | 30 | 19–61 | 3 T | Siemens TrioTim |
| PReDICT | 344 | 40 | 18–64 | 3 T | Siemens TrioTim |
| HMRRC | 269 | 31 | 18–60 | 3 T | GE Excite |
| 3 T | Siemens TrioTim | ||||
| Stanford | 110 | 33 | 19–58 | 3 T | GE Signa-Excite |
| STRADL | 1189 | 60 | 26–84 | 3 T | Philips Achieva-TX |
| 3 T | Philips Prisma-FIT |
Canadian Biomarker Integration Network in Depression (CAN-BIND) is a national depression program with recruitment from 7 centers [31, 32]. The CAN-BIND-1 treatment protocol is an 8-week trial with a selective serotonin reuptake inhibitor (SSRI) antidepressant, escitalopram, followed by an 8-week augmentation with aripiprazole if there was poor treatment response (i.e., less than 50% improvement in depressive symptoms). MRI scans were acquired at baseline, weeks 2 and 8 in both MDD and healthy participants.
Copenhagen University (NeuroPharm1) cohort consists of data from the Center for Integrated Molecular Brain Imaging (Cimbi) and Center for Experimental Medicine Neuropharmacology prospective longitudinal treatment study with an SSRI, escitalopram. The protocol is a 12-week trial with a SSRI, escitalopram, which could be switched to a serotonin norepinephrine reuptake inhibitor, duloxetine at week 4 if there were unacceptable side effects or poor treatment response (i.e., less than 25% improvement in depressive symptoms). MRI scans were acquired at baseline in healthy participants and at baseline and week 8 in MDD [33–39].
Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care (EMBARC) is a multisite, randomized, placebo-controlled clinical trial with recruitment from 4 centers [40]. Treatment protocol consists of two stages. Stage 1 is an 8-week, double-blind, randomized allocation to placebo medication or to an SSRI, sertraline, followed by Stage 2, an 8-week, double-blind, cross over treatment design. At Stage 2, participants continue treatment for 8 weeks (either placebo or sertraline) if the Clinical Global Improvement scale (CGI) rating is at least “much improved”. If the CGI rating is less than “much improved”, then treatment is switched under double-blind conditions. From the initial placebo treatment arm, treatment is switched to the SSRI, sertraline, and from the initial SSRI, sertraline, treatment arm, the treatment is switched to the non-serotonergic antidepressant, bupropion. MRI scans were acquired in medication-free MDD and healthy participants at baseline.
Huaxi MR Research Center (HMRRC) cohort consists of medication-naïve first episode MDD and matched healthy participants with single session MRI scans [41–43].
King’s College London cohort consists of 4 studies [44–50]. Treatment protocol was an 8-week trial of serotonin-norepinephrine reuptake inhibitor (SNRI), duloxetine. MRI scans were acquired at baseline, weeks 2 and 8 in both MDD and healthy participants [47].
Laureate Institute for Brain Research (LIBR) cohort consists of 2 studies with MRI data in first episode and recurrent MDD and matched healthy controls [51–53].
University of Manchester cohort consists of 3 studies [54–56]. Treatment protocol was an 8-week trial of SSRI, citalopram, with MRI scans acquired at baseline and week 8 in both MDD and healthy participants [54].
University of Oxford cohort consists of an 6-week trial of SSRI, escitalopram, with MRI scans acquired at baseline and week 6 [57, 58].
Predictors of Remission in Depression to Individual and Combined Treatments (PReDICT) study is a 12-week randomized clinical trial of treatment-naïve MDD with 3 treatment arms: an SSRI, escitalopram; an SNRI, duloxetine; or CBT, and a 12-week second phase if remission was not achieved with monotherapy, with the addition of CBT to the medication treatment arms or augmentation with escitalopram to the CBT treatment arm. MRI scans were acquired at baseline and week 12 [59, 60].
REST-meta-MDD study consists of resting state fMRI data in medication-naïve first episode and recurrent MDD from 17 sites in China [61, 62].
Southwest University (SWU) cohort consists of a community-based recruitment which includes first episode and recurrent MDD and healthy control participants [63–65].
Stanford University cohort consists of MRI data in first episode and recurrent MDD and healthy control participants [66–68].
STratifying Resilience and Depression Longitudinally (STRADL) is a community-based cohort from the Generation Scotland Scottish Family Health Study with detailed clinical, cognitive and neuroimaging assessments. Single session MRI scans were acquired [24, 69].
University of California at San Francisco (UCSF) cohort consists of first episode and recurrent MDD and healthy control participants [70, 71].
Assessments
MDD diagnosis is based on standardised diagnostic criteria, DSM or ICD: DSM-IV (HMRRC, Manchester, Oxford, PReDICT, SWU), DSM-IV-TR (CAN-BIND, EMBARC, KCL, LIBR, Stanford, STRADL) and DSM-5 (Neuropharm1). Structured clinical interview assessments were performed: Structured Clinical Interview for DSM (SCID) (EMBARC, HMMRC, KCL, LIBR, Manchester, Oxford, PReDICT, Stanford, SWU, STRADL) or Mini International Neuropsychiatric Interview (MINI) (CAN-BIND, KCL, Neuropharm1).
Symptom severity has been measured using standardised clinician-rated symptom scales: 17-item Hamilton Rating Scale for Depression (HRSD) [72] (EMBARC, HMRRC, KCL, LIBR, Neuropharm1, Oxford, Stanford, SWU), 24-item HRSD (PReDICT), Montgomery-Åsberg Depression Rating Scale (MADRS) [73] (CAN-BIND, LIBR, Manchester; PReDICT), and Quick Inventory for Depressive Symptomatology (QIDS-SR) [74, 75] (EMBARC, PReDICT, STRADL).
Clinical measures include illness history (e.g., age onset, number of previous episodes) and medication records. Demographic information (e.g., years of education) and neuropsychological assessments, including memory and executive function, where available are included (CAN-BIND, EMBARC, KCL, LIBR, Manchester, Neuropharm1, PReDICT, STRADL).
Prospective longitudinal treatment studies have provided clinical outcome data (CAN-BIND, EMBARC, KCL, Manchester, Neuropharm1, Oxford, PReDICT). We have additional information in MDD participants taking antidepressant medication (CAN-BIND, KCL, Manchester, Neuropharm1, Oxford, PReDICT, Stanford, STRADL, SWU).
Clinical data harmonization
High reliability, internal consistency and correspondence have been demonstrated for HRSD [76], between HRSD and QIDS [77, 78], HRSD and MADRS [79], and QIDS and MADRS [80] in outpatient non-psychotic MDD. Standardized conversions will be applied to generate comparable scores [77, 78, 81]. Clinical remission is defined as 17-item HRSD score of less than or equal to 7 and the equivalent in MADRS and QIDS, and treatment response is defined as having an improvement of at least 50% relative to baseline depressive severity [8].
It is possible that derived NA-NF dimensions could be transdiagnostic. We will also incorporate clinical knowledge using a Research Domain Criteria (RDoC)-informed approach to specify transdiagnostic dimensions, using individual items as well as symptom clusters scores from rating scales [82–85]. For example, within the Arousal and Regulatory System domain, we can specify fine-grained disturbances in sleep (i.e., initial, middle and late insomnia, as well as hypersomnia) and vegetative disturbances (i.e., appetite increase or decrease, weight increase or decrease), and in the Negative Valence Systems domain, a dimension based on items assessing anxiety reflecting sensitivity to potential threat.
While all patients have a diagnosis based on standardised criteria, we cannot rule out the possibility of site differences reflecting true cultural or ethnic differences in MDD phenomenology. Potential systemic differences in symptom profiles across sites due to different socio-cultural contexts will be examined. Common factor structures have been demonstrated across cultures [86, 87]. Principal component analyses will be performed to examine factor structures that characterize symptom profiles by site. We will control for any site differences in the magnitude of symptoms by deriving within-center standardized scores using the residuals. If necessary, we will apply factorization methods to the standardized scores to obtain illness dimensions, which we will validate by analyzing their associations with demographic, diagnostic, neurocognitive and other clinical data. We will empirically test the brain-to-symptom mappings by altering the balance between inter-site pooling and within-site normalization.
MRI imaging characteristics
MRI data include structural MPRAGE or equivalent structural MRI scans and resting state functional MRI scans acquired on 1.5 Tesla (T) or 3 T MRI systems. Different models of scanner have been used, including Discovery MR750 3 T (GE Healthcare, Little Chalfont, Buckinghamshire, UK), Signa HDxt 3 T (GE Healthcare, Little Chalfont, Buckinghamshire, UK), MAGNETOM TrioTim or MAGNETOM Prisma Fit (Siemens Healthcare, Erlangen, Germany), and Achieva 3 T (Philips Healthcare, Best, Netherlands) (Table 2).
MRI data integration and harmonization
Harmonization is a critical process as it enables the constructive pooling and integration of all datasets within the consortium. Although imaging protocols among all included studies are comparable, scanner and minor acquisition protocol variations nonetheless introduce inter-study differences in imaging characteristics which render direct pooling of the data very difficult. In the present consortium, we have harmonized image processing pipelines, statistical harmonization of derived measures, and deep learning based harmonization of raw images [88].
Image-level extraction of structural anatomy and functional connective measures
Imaging variables are extracted from the MRI scans to provide a multi-scale representation of structural and connectomic characteristics. Some features are defined a priori (e.g., multi atlas-based parcellations) and some are data-driven (e.g., structural covariance and functional connectivity networks).
MUSE region of interest segmentation
Volumetric MRI features are extracted via established and validated methods using a fully automated processing pipeline. Raw 3D T1-weighted MRIs are first quality checked for motion, image artifacts, or restricted field-of-view. Each participant’s quality-controlled T1-weighted MRI scan is preprocessed with a containerized processing pipeline. Preprocessing steps consist of magnetic field intensity inhomogeneity correction [89] and multi-atlas skull-stripping for the removal of extra-cranial material [90].
The images are segmented using a state-of-the-art, multi-atlas, multi-warp label-fusion method, MUSE [91]. In this framework, multiple atlases with semi-automatically extracted ground-truth region of interest (ROI) labels are first warped individually to the target image using two different non-linear registration methods. A spatially adaptive weighted voting strategy is then applied to fuse the ensemble into a final segmentation. This procedure is used to segment each image into 145 anatomical regions of interest (ROIs) spanning the entire brain. We calculate the volumes of the 145 ROIs, as well as the volumes of 113 composite ROIs that are obtained by combining individual ROIs into larger anatomical regions following a predefined ROI hierarchy whereby brain anatomy can be quantified at multiple levels of resolutions [91].
MUSE has obtained top accuracy in comparison with multiple benchmark methods in independent evaluations [92]. MUSE utilizes state-of-the-art multi-atlas, multi-warp algorithms, with a very rich set of atlases spanning several protocols from 1.5 T SPGR images to 3 T MPRAGE images. The ensemble of atlases used to segment each scan contains sufficient diversity which renders it robust to scanner variations [91]. Critically, we have leveraged several studies which have scanned the same individuals in multiple scanners and hence have built procedures that render the multi-scanner atlases mutually consistent [91].
Voxel-based, tissue-specific (grey matter, white matter, cerebrospinal fluid) regional volumetric maps are obtained using MUSE segmentation and inverse atlas warping is applied for voxel-based analyses. Voxel-wise regional volumetric maps (RAVENS) are generated for each tissue [93] by spatially aligning the skull-stripped images to a template in MNI-space [94]. Quality control (QC) on derived maps and imaging variables is performed using a semi-automated approach. An automated procedure automatically ranks scans based on outlying values of quantified metrics (i.e., ROI values) and flags those that show deviation from estimated population distributions. Flagged images are examined by visual inspection using a visualization and annotation tool for evaluating for pipeline failures (e.g., poor brain extraction, tissue segmentation, and registration errors).
Structural covariance networks
Our prior work has highlighted the potential of structural covariance networks as a flexible and biologically interpretable way of reducing complex anatomical images down to a relatively small set of measurements [95, 96]. This approach uses orthogonally-projective non-negative matrix factorizations to parcellate the brain into regions that show consistent trends across individuals, potentially because they are influenced by common underlying neurobiological factors. For example, we found that patterns of structural covariance were highly reproducible, aligned well with functional networks, displayed differential developmental trajectories during adolescence, and correlated with maps of evolutionary cortical expansion [96]. We have recently developed a novel method that computes multi-scale non-negative matrix factorization (NMF) components [97]. This allows us to characterize heterogeneous presentation of neuropsychiatric and neurodegenerative diseases in multiple scales. These networks will be part of our imaging feature panel and might be well-suited for capturing the neurodevelopmental underpinnings of MDD.
Deep learning generative adversarial networks (GAN)
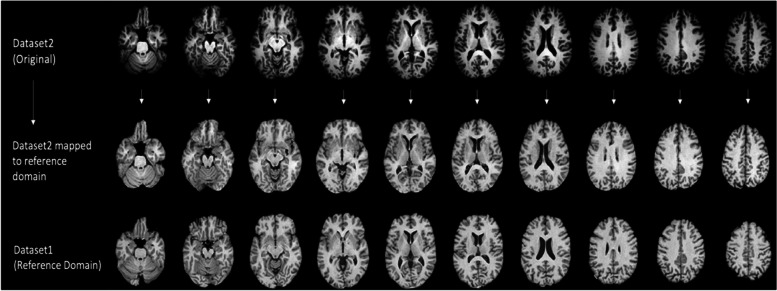
A second approach utilizes deep learning CycleGAN and STAR-GAN methods [88], which synthesize images drawn from certain distributions. This method has been used extensively in numerous applications seeking to transform images from one style to another. We have used data from numerous scanners to learn the mapping of brain MRI scans to a canonical reference domain, in which inter-scanner variations are minimized [88] (Fig. 1). By making the characteristics of images very similar, while preserving important information, subsequent image analysis steps, including segmentation and parcellation, become significantly more consistent across studies. We will further refine and adapt this method to this project, including some of the current directions that involve nonlinear modelling co-variates in order to better restrict these mappings to differences related to MRI scanners and protocols, while preserving anatomical characteristics.
Fig. 1.
Example of image harmonization via deep learning based canonical mapping to a reference domain presented in bottom row
Personalized functional networks
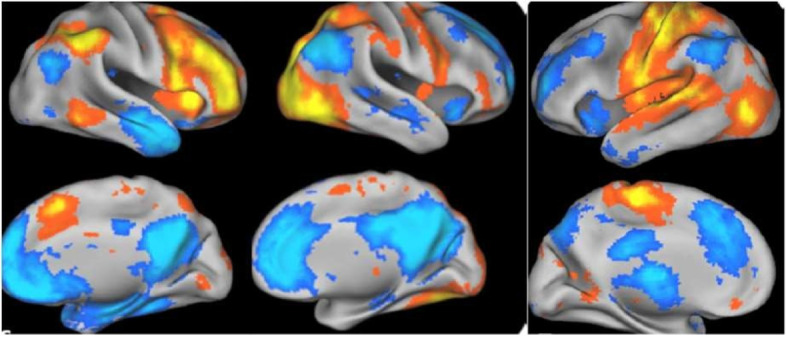
For resting state fMRI, personalized functional networks using a spatially-regularized NMF method align well with functional activation patterns and have improved functional homogeneity [98] (Fig. 2). Functional homogeneity quantifies the degree to which a functional network represents one signal, rather than mixing multiple neurophysiological signals. Measures of functional connectivity, derived from brain parcellations and functional networks show promise in predicting brain maturity and distinguishing disease from healthy brain states [99–102]. Furthermore, there are significant correlations between elements of the connectivity matrices, which may lead to unreliable classification [103]. Using our NMF method, we found increased homogeneity compared to standard network definitions using a group atlas, as well as a null distribution created using a conservative spin-based spatial permutation procedure [104]. The personalized functional networks delineated from our NMF method showed that the networks with the greatest variability in functional topography in youth are the very higher-order association networks impacted by psychopathology, these association networks are refined with age in development, and individual differences in association network topography predicted executive function [104] (Fig. 3).
Fig. 2.
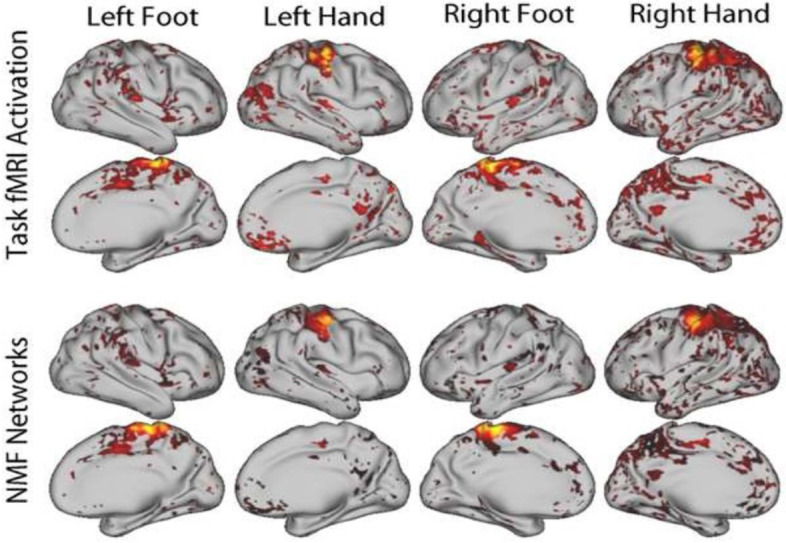
Personalized functional networks defined using NMF with resting state fMRI data aligned with activation during a motor task, adapted from Li et al. [98]
Fig. 3.
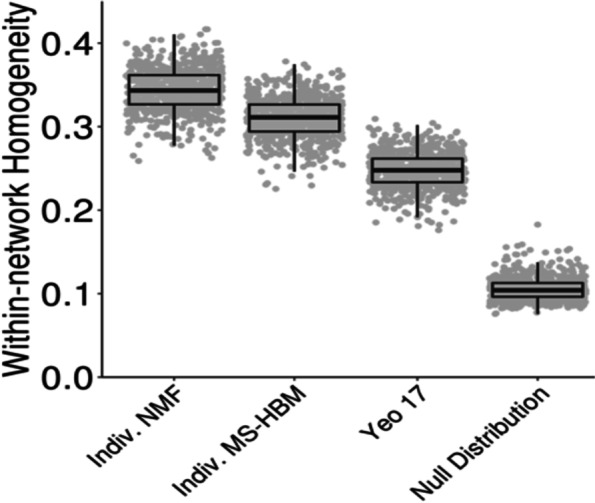
Personalized functional networks improve functional homogeneity. Functional homogeneity is higher within personalized functional networks (from either non-negative matrix factorization (NMF) or multi-session hierarchical Bayesian model (MS-HBM)) than standard group-level networks (Yeo 17-network group atlas (Yeo 17)) or a null model that preserves spatial covariance structure, adapted from Cui et al. [105]
We are also employing a complementary method based on sparse connectivity pattern (SCP) learning, leveraging the effective non-linearity of sparse dictionary learning [104, 106–108] as a means for describing the functional connectivity patterns of brain networks [109]. SCPs also minimize the negative impact of correlated features on the robustness of prediction models [103] (Fig. 4). A hierarchical extension of this approach extracts these functional networks at multiple scales [110]. Adopting these complementary techniques will provide a rich set of imaging features to characterize the functional brain connectome.
Fig. 4.
Three representative SCPs identified. Left column: Default mode anti-correlated with fronto-parietal network; Middle column: visual and default mode anti-correlated regions; Right column: sensorimotor regions anti-correlated with fronto-parietal network; blue and orange colours represent anti-correlated regions, adapted from Eavani et al. [109]
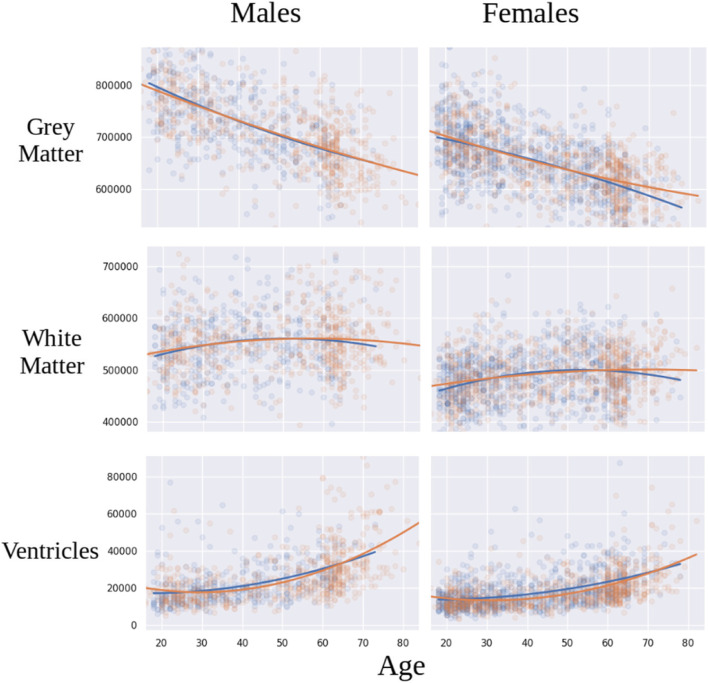
Harmonization of derived measures
We have developed a statistical harmonization approach [29], building upon the COMBAT method that has been successfully used for over a decade to remove batch effects in genomic studies and recently adapted in neuroimaging research [111–114]. This approach is fully multivariate, utilizing hyper-parameters to define over-arching statistical priors, and has been successfully adopted in imaging. In order to model nonlinear effects of covariates (e.g., age), we have combined COMBAT with generalized additive models (GAMs) using spline functions. The resultant COMBAT-GAM general tool for harmonization can be applied to various forms of data, including ROIs and coefficients of structural covariance and functional connectivity networks. Preliminary results of statistical harmonization from the present consortium are shown in Fig. 5.
Fig. 5.
Preliminary results from the COORDINATE MDD datasets (EMBARC, Oxford, HMRRC, Stanford, STRADL) showing age trajectories in grey matter, white matter and ventricular volumes in MDD patients (colored blue) as compared to healthy controls (colored red)
Harmonization of resting state fMRI data is typically performed at the correlation matrix level. In particular, we have developed a functional connectivity covariance batch effect correction (FC-CovBAT) [115] that models second order moments of the upper-triangular elements of individual correlation matrices derived from the fMRI data. FC-CovBAT is an extension of COMBAT and CovBat methods [116] for structural imaging data. These methods statistically model the site/scanner differences not only in the means and variances of the multivariate correlation values, but also in the covariance structures between the multivariate correlation values from the FC data (Fig. 6).
Fig. 6.
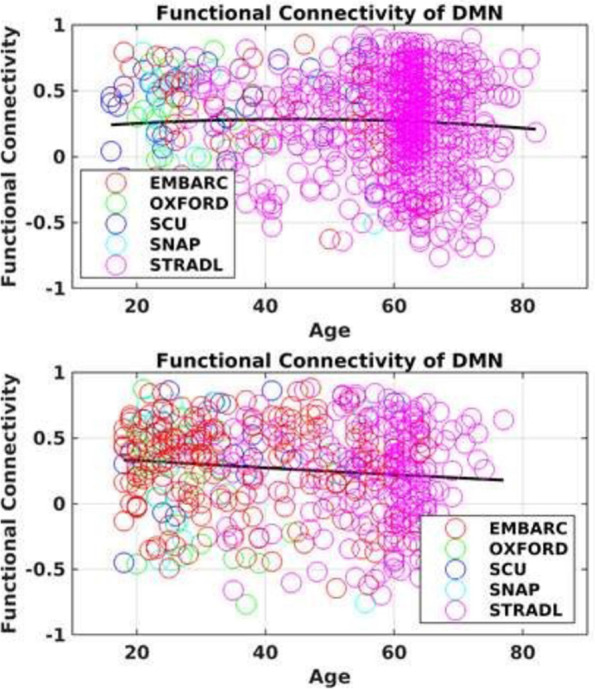
Preliminary results showing functional connectivity of DMN (between anterior cingulate cortex and posterior cingulate cortex) in healthy controls (top panel) and MDD participants (bottom panel) from the COORDINATE MDD datasets (EMBARC, Oxford, SCU (HMRRC), SNAP (Stanford), STRADL)
NA-NF dimensional neurobiological representation of MDD
Direct clustering of patient data, especially high-dimensional images, is challenged by effects of confounding variations in the data, namely variations in healthy individuals that are not related to disease effects. We have developed semi-supervised clustering methods to account for these effects, effectively clustering differences between patients and healthy controls, rather than directly clustering patient data. The methods assume that patient data have been derived from healthy control data via one of several, to be estimated, transformations that reflect disease effects (Fig. 7). Whatever variations are present in the healthy control data and are unrelated to disease effects will follow the disease-specific transformations. Within this approach, we acknowledge that some control samples might reflect a “super-healthy” control group without any chronic diseases that may represent resilience [117], though healthy control participants have also been recruited from the general community in the present consortium.
Fig. 7.

Healthy controls (green) are separated from patients via a number of maximum-margin hyperplanes that define disease subtypes. Iterative classification and clustering determine subtype membership and classification hyperplanes
Two semi-supervised methods will be used: 1) HYDRA, a conventional machine learning approach that is largely a discriminative method [16], with its multi-scale extension [118]; and 2) Generative Adversarial Networks (GANs), a complementary method which leverages the power of a class of generative deep learning methods [119]. These methods have complementary strengths, which will be combined in seeking robust and reproducible MDD dimensions.
HYDRA
HYDRA uses the concept of a convex polytope, in conjunction with support vector machine principles (maximum margin cost function), to simultaneously classify patients from healthy controls and to determine a number of hyperplanes that represent disease dimensions. An iterative process determines the disease dimensions, as well as memberships in them. HYDRA has recently helped discover two distinct neuroanatomical dimensions in schizophrenia with evidence of differences in cognitive and clinical profiles between dimensions, in polygenic risk scores for schizophrenia and autism, as well as in brain development and aging studies [120]. We will apply this method to the imaging feature panels (ROI volumes, structural covariance network coefficients derived from voxel-based maps, and functional connectivity network coefficients), in order to identify MDD dimensions and to obtain positions of each patient within each dimension. It is likely that some patients will express multiple NA-NF signatures concurrently.
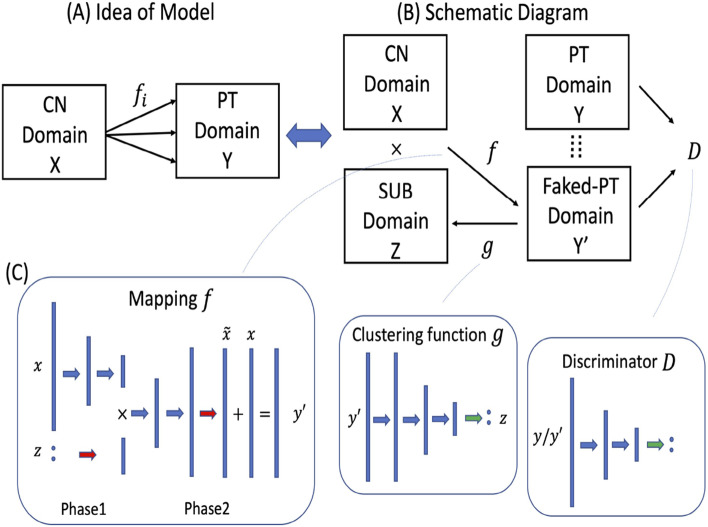
Deep learning and generative adversarial networks (GANs)
The second approach relies on a generative methodology for semi-supervised clustering, termed Smile-GAN, which utilizes state-of-the-art deep learning CycleGAN architectures, with latent variables representing neurobiological dimensions [119]. The model simultaneously learns the mapping and clustering functions using the discriminator function and the data from the patient domain. Representations of the patient clustering structure and the depression-related NA-NF dimensions are stored respectively in the network weights of functions after learning, which are the main outcomes of the model training (Fig. 8).
Fig. 8.
Our deep learning-based approach to subtyping. A General idea behind Smile-GANs (B) Schematic diagram of Smile-GANs. CN: healthy control, PT: patient, SUB: subtype (C) Network architectures of the three main functions (f, g, D): blue arrow represents one linear transformation followed by one leaky relu function, green arrow represents one linear transformation followed by one softmax function, red arrow represents only one linear transformation. The GAN network learns to synthesize MDD patient scans from scans of normal controls, contingent upon subtype, SUB, which is learned in the training process. The discriminator, D, of this GAN ensures that these synthesized scans are indistinguishable from real MDD patients scans. The mappings, f, estimated in this process capture features of the neuropathologic processes that transform imaging data of controls to those of MDD patients, adapted from Yang et al. [119]
While these approaches can be very powerful, they require large training datasets. The availability of a sufficiently large and well-harmonized dataset in the present consortium will allow us to harness the power of these deep learning methods. We will seek experimental confirmation via split sample and sensitivity analyses.
We use cross-validation, split-sample, and random permutation experiments to determine the optimal number of reproducible and statistically significant clusters corresponding to NA-NF dimensions of MDD, by measuring the adjusted rand index (ARI) [120]. The most reproducible clusters, according to two main criteria, both high and statistically significant ARI, will be used to derive the NA-NF dimensions. As part of the method, cluster memberships of each individual will be readily calculated [16, 119]. These memberships will effectively be the coordinates of an individual in the NA-NF coordinate system, reflecting the dominant NA-NF MDD patterns.
Incorporating clinical knowledge
We will augment this approach with the use of clinical measures, namely symptom profile as well as depressive state and medication status. The main idea is that NA-NF dimensions might not necessarily be easily interpretable clinically. By incorporating clinical phenotypic measures in parts of the clustering procedure, we will favor imaging patterns that simultaneously have relatively distinct clinical phenotypes. Methodological extensions will include, for example, introducing a discriminant term, which encodes the dimensions. This term will encourage NA-NF dimensions that have relatively distinct clinical phenotypes. We will also modify the latent space formulation to allow for continuous latent variables, in order to better model anatomy and function in individuals who might present mixed patterns.
Multidimensional predictors of treatment responses
A main goal is to investigate whether position in the NA-NF dimensional system captures disease effect in predicting treatment response at the individual level based on semi-supervised approaches. Treatment response will be defined as the harmonized change in clinician-rated depressive severity scales. Changes of scores after the treatment period will be modelled both as continuous values and binary variables. We recognise that these measures are often insufficient for capturing treatment efficacy and might not reflect patient experience. We will further investigate whether NA-NF dimensions might map onto subfacets of the scales with greater clinimetric properties [121].
We will further enrich NA-NF dimensions by directly and specifically looking for patterns that predict treatment response via supervised classification. Such imaging signatures might or might not capture broad and treatment-oblivious NA-NF variations, however they capture NA-NF measures that are tailored to prediction of treatment response in which baseline clinical variables will be part of these treatment-specific predictive models.
In particular, specificity to particular categories of treatment will be investigated. Prediction of differential response between placebo and antidepressant medication is highly important, yet difficult to assess. Prediction of placebo response is uniquely accessible in the present sample, in which treatment outcome data are available for both active antidepressant and placebo arms of randomized controlled trials.
To identify pre-treatment moderators of differential treatment response, the specificity of NA-NF predictors to different categories of antidepressant medication will be investigated. Treatment outcome data are available for SSRI and SNRI medication classes. Specificity of NA-NF predictors of response to psychotherapy or to antidepressant medication will also be investigated.
A key weakness of multivariate pattern analysis studies has been the frequent lack of generalizability and validation on new datasets. Given the size of the consortium, we will test the NA-NF dimensional system in wholly independent prospective longitudinal treatment cohorts, namely Copenhagen University. We emphasize that cross-validation methods are engrained in all our analyses to reduce overfitting and improve generalizability.
Summary
COORDINATE-MDD brings together deeply phenotyped clinical data, multi-site ‘raw’ individual-level structural and functional neuroimaging data, and state-of-the-art AI-based methods in order to identify the multimodal dimensions that comprise MDD and which inform treatment response. Our consortium data are derived from adults with first episode or recurrent MDD, medication-free, in a current major depressive episode, that is not treatment-resistant depression, and healthy controls. We leverage statistical harmonization, machine learning and deep learning methods and large integrated and harmonized sample of highly-phenotyped, individual-level patient data with prospective longitudinal treatment outcomes. Our objectives are to delineate the robust and reproducible neurobiological NA-NF signatures which comprise MDD and which predict or moderate treatment response. We will follow an iterative process by first defining the multivariate neural dimensions that characterise deeply phenotyped samples and then testing the utility of these dimensions in novel samples.
Acknowledgements
MT, CCF, CHYF and all authors wish to thank the participants, families, staff, and colleagues who made this project possible. BWD acknowledges W. Edward Craighead, PhD. The views expressed are those of the author(s) and not necessarily those of the funding agencies.
Abbreviations
- MDD
Major depressive disorder
- NA-NF
Neuroanatomical-neurofunctional
- SSRI
Selective serotonin reuptake inhibitor
- CAN-BIND
Canadian Biomarker Integration Network in Depression
- Cimbi
Center for Integrated Molecular Brain Imaging
- EMBARC
Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care
- CGI
Clinical Global Improvement scale
- HMRRC
Huaxi MR Research Center
- SNRI
Serotonin-norepinephrine reuptake inhibitor
- LIBR
Laureate Institute for Brain Research
- PReDICT
Predictors of Remission in Depression to Individual and Combined Treatments
- SWU
Southwest University
- STRADL
STratifying Resilience and Depression Longitudinally
- UCSF
University of California at San Francisco
- MINI
Mini International Neuropsychiatric Interview
- HRSD
Hamilton Rating Scale for Depression
- MADRS
Montgomery-Åsberg Depression Rating Scale
- QIDS-SR
Quick Inventory for Depressive Symptomatology
- RDoC
Research Domain Criteria
- T
Tesla
- ROIs
Regions of interest
- GAN
Generative adversarial networks
- NMF
Non-negative matrix factorization
- SCP
Sparse connectivity pattern
- GAMs
Generalized additive models
- FC-CovBAT
Functional connectivity covariance batch effect correction
- GANs
Generative Adversarial Networks
- ARI
Adjusted rand index
Authors’ contributions
Authors made substantial contributions to the conception of the work (CHYF, CD), design (all authors), data acquisition (all authors), analysis (CD, CHYF, GE, YF, MA, JG, HS). All authors have contributed to drafting and revising the work. All authors have approved the submitted version. All authors agree both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Funding
IMA received funding from the Medical Research Council (MRC) (G0601526). DA received funding from the Academy of Medical Science (AMS-SGCL8) and National Institute for Health and Care Research (NIHR) PhD studentship.
BNF, SHK, SH, SCS, SRA, and SR received funding from Ontario Brain Institute and Canadian Institutes of Health Research (CIHR) (for CANBIND01 data).
CD received funding from the National Institute of Health (R01 MH112070), HC (RF1-AG054409, R01-MH123550, U01-AG068057), IHG (R37MH101495) and YF (R01 AG066650 and R01EB022573).
EMBARC study (NCT01407094) was supported by the National Institute of Mental Health of the National Institutes of Health under award numbers U01MH092221 (Trivedi, M.H.) and U01MH092250 (McGrath, P.J., Parsey, R.V., Weissman, M.M.), and in part by the Hersh Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Valeant Pharmaceuticals donated the Wellbutrin XL used in the study. This work was supported by the EMBARC National Coordinating Center at UT Southwestern Medical Center, Madhukar H. Trivedi, M.D., Coordinating PI, and the Data Center at Columbia and Stony Brook Universities. In addition, this work was funded in part by the Center for Depression Research and Clinical Care (PI: Madhukar Trivedi).
RE received funding from the National Institute for Health and Care Research (NIHR), and the Medical Research Council (MRC).
CHYF received funding from the Medical Research Council (MRC) (G0802594) and Brain and Behaviour NARSAD Young Investigators Award.
QG received funding from the National Natural Science Foundation of China (81820108018; 81621003).
CJH received support from the Medical Research Council (G0701421) and is supported by the Oxford Health NIHR Biomedical Research Centre.
GMK, MG & VGF received funding from the Lundbeck Foundation (R279–2018-1145 (BrainDrugs)).
HSM & BWD received funding from the National Institute of Mental Health (P50MH077083, 1RO1MH080880).
MPP received funding from The William K. Warren Foundation, National Institute on Drug Abuse (U01 DA041089), and National Institute of General Medical Sciences Center Grant Award Number (1P20GM121312).
MDS received funding from the National Institute of Mental Health (R01MH125850).
JS received funding from the National Institute of Mental Health (K01MH096077; R01MH098099).
STRADL study was supported and funded by the Wellcome Trust Strategic Award, Stratifying Resilience and Depression Longitudinally (ref. 104036/Z/14/Z), and the Medical Research Council (MRC-MC/PC/17209). AMM received funding from the Wellcome Trust (220857/Z/20/Z, 216767/Z/19/Z). AS was funded as part of the STRADL study and indirectly through the Lister Institute of Preventive Medicine award ref. 173096. Data processing used the resources provided by the Edinburgh Compute and Data Facility (ECDF) (http://www.ecdf.ed.ac.uk/).
SWU dataset was supported by the following: National Natural Science Foundation of China (31571137; 31500885), the National Outstanding young people plan, the Program for the Top Young Talents by Chongqing, the Fundamental Research Funds for the Central Universities (SWU1509383; SWU1509451; SWU1609177), Natural Science Foundation of Chongqing (cstc2015jcyjA10106), the Fok Ying Tung Education Foundation (151023) to JQ and DTW.
DT received funding from the National Institute of Mental Health (5R01MH101472).
TW received funding from the Anthony and Elizabeth Mellows Charitable Foundation.
CGY was supported by the National Natural Science Foundation of China (82122035) and Beijing Nova Program of Science and Technology (Z191100001119104).
AHY independent research is funded by the National Institute for Health and Care Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London.
RZ received funding from the Medical Research Council (MRC) (MR/T017538/1).
Availability of data and materials
Original data can be requested from each consortium member. Derived data in the present consortium can be made available from the corresponding author on reasonable request and with permission of each consortium member.
Declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. All participating sites had obtained permission from their local Institutional Review Boards or Ethics Committees, and all participants had provided written informed consent. Research analyses specific to this study only used de-identified data. Data Sharing Agreements were reviewed and approved by the Grants Department and Contracts Offices for each of the following research centers: Ontario Brain Institute (OBI) on behalf of the Canadian Biomarker Integration Network in Depression (CAN-BIND); University of East London (UEL); University of Texas Southwestern Medical Center on behalf of the Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care study (EMBARC); Emory University on behalf of the Predictors of Remission in Depression to Individual and Combined Treatments study (PReDICT); Huaxi MR Research Center (HMRRC), Sichuan University; King’s College London (KCL); Laureate Institute for Brain Research (LIBR); University of Manchester; University of Oxford; University of Pennsylvania; REST-meta-MDD consortium and the International Big-Data Center for Depression Research, Institute of Psychology, Chinese Academy of Sciences; Southwest University (SWU); Stanford University; and University of Edinburgh on behalf of STratifying Resilience and Depression Longitudinally study (STRADL).
Consent for publication
Not applicable.
Competing interests
SRA has consulted for Indoc Research Canada.
AMM has received research support from Eli Lilly, Janssen, and The Sackler Trust. AMM has also received speaker fees from Illumina and Janssen. CHYF has received grant funding from MRC, Wellcome Trust, Brain and Behaviour NARSAD, Eli Lilly, Flow Neuroscience, Baszucki Brain Research Fund Milken Institute, Rosetrees Trust.
HS has received grant funding from NIH.
SCS received research support from Brain Canada, CIHR (Canadian Institutes of Health Research), Ontario Brain Institute and CFI (canadian Foundation for Innovation). SCS is a founder and share holder of ADMdx, Inc.
DT has received grant funding from NIH.
RZ is a private psychiatrist service provider at The London Depression Institute and co-investigator on a Livanova-funded observational study of Vagus Nerve Stimulation for Depression. RZ has received honoraria for talks at medical symposia sponsored by Lundbeck as well as Janssen. He has collaborated with EMIS PLC and advises Depsee Ltd. He is affiliated with the D’Or Institute of Research and Education, Rio de Janeiro and advises the Scients Institute, USA.
BWD has received research support from Boehringer-Ingelheim, Compass, Pathways, NIMH, Otsuka, Usona. Honoraria for Consulting: Aya Biosciences, Myriad Neuroscience, Otsuka, Sophren Therapeutics, Cerebral Therapeutics, Sage.
CJH serves as a consultant for P1vital, Lundbeck, Servier and Compass Pathways. She holds grant income from Zogenix and J&J.
SHK has received funding for Consulting or Speaking engagements from Abbvie, Boehringer-Ingelheim, Janssen, Lundbeck, Lundbeck Institute, Merck, Otsuka Pfizer, Sunovion and Servier. He has received Research Support from Abbott, Brain Canada, CIHR (Canadian Institutes of Health Research), Janssen, Lundbeck, Ontario Brain Institute, Otsuka, Pfizer, SPOR (Canada’s Strategy for Patient-Oriented Research). He has stock/stock options in Field Trip Health.
GMK has received honoraria as a speaker for Sage Biogen and as a consultant for Sanos.
HSM has received grant funding from NIH; Consulting and IP Licenses Fees from Abbott Labs.
MHT received Research Support from: NIH, PCORI, AFSP; Consultant: Alkermes Inc., Alto Neuroscience Inc., Axsome Therapeutics, Boegringer Ingelheim, GH Research, GreenLight VitalSign6 Inc., Heading Health, inc., Janssen Pharmaceutical, Legion Health, Merck Sharp & Dohme Corp., Mind Medicine Inc., Navitor, Neurocrine Biosciences Inc., Noema Pharma AG, Orexo US Inc., Otsuka Canada Pharmaceutical Inc., Otsuka Pharmaceutical Development & Commercialization, Inc. (MDD Section Advisor), SAGE Therapeutics, Signant Health, Takeda Pharmaceuticals Inc.; Editorial compensation from Oxford University Press.
AHY reports declaration of interests: Paid lectures and advisory boards for the following companies: Astrazenaca, Eli Lilly, Lundbeck, Sunovion, Servier, Livanova, Janssen, Allegan, Bionomics, Sumitomo Dainippon Pharma, COMPASS, Sage, Novartis. Consultant to Johnson & Johnson and to Livanova. Received honoraria for attending advisory boards and presenting talks at meetings organised by LivaNova. Principal Investigator in the Restore-Life VNS registry study funded by LivaNova. UK Chief Investigator for Novartis MDD study MIJ821A12201. Principal Investigator on ESKETINTRD3004: “An Open-label, Long-term, Safety and Efficacy Study of Intranasal Esketamine in Treatment-resistant Depression”. Principal Investigator on “The Effects of Psilocybin on Cognitive Function in Healthy Participants”. Principal Investigator on “The Safety and Efficacy of Psilocybin in Participants with Treatment-Resistant Depression (P-TRD)”. No shareholdings in pharmaceutical companies. Deputy Editor of BJPsych Open. Grant funding (past and present): NIMH (USA); CIHR (Canada); NARSAD (USA); Stanley Medical Research Institute (USA); MRC (UK); Wellcome Trust (UK); Royal College of Physicians (Edin); BMA (UK); UBC-VGH Foundation (Canada); WEDC (Canada); CCS Depression Research Fund (Canada); MSFHR (Canada); NIHR (UK). Janssen (UK).
Authors AS, AS, BRG, BNF, CCF, C-GY, CD, DA, DTW, GE, HCW, IHG, IMA, IS, JFWD, JQ, JS, JG, KH, KSC, KQ, MPP, MA, MDS, MG, QG, RDW, RE, SH, SR, TAV, TC, TW, VGF and YF declare that they have no competing interests to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.American Psychiatric Association . Diagnostic and statistical manual of mental disorders, (DSM-5-TR®). Fifth Edition, Text Revision. Arlington: American Psychiatric Pub; 2022. [Google Scholar]
- 2.World Health Organization . International Statistical Classification of Diseases and Related Health Problems. 11 2021. [Google Scholar]
- 3.Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34(1):119–138. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 5.Fava M, Alpert JE, Carmin CN, Wisniewski SR, Trivedi MH, Biggs MM, et al. Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D. Psychol Med. 2004;34(7):1299–1308. doi: 10.1017/S0033291704002612. [DOI] [PubMed] [Google Scholar]
- 6.Hofmeijer-Sevink MK, Batelaan NM, van Megen HJGM, Penninx BW, Cath DC, van den Hout MA, et al. Clinical relevance of comorbidity in anxiety disorders: a report from the Netherlands study of depression and anxiety (NESDA) J Affect Disord. 2012;137(1–3):106–112. doi: 10.1016/j.jad.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. AJP. 2006;163(11):1905–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- 8.Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. AJP. 2006;163(1):28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 9.Fernandez-Pujals AM, Adams MJ, Thomson P, McKechanie AG, Blackwood DHR, Smith BH, et al. Epidemiology and heritability of major depressive disorder, stratified by age of onset, sex, and illness course in Generation Scotland: Scottish Family Health Study (GS:SFHS) PLoS One. 2015;10(11):e0142197. doi: 10.1371/journal.pone.0142197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geschwind DH, Flint J. Genetics and genomics of psychiatric disease. Science. 2015;349(6255):1489–1494. doi: 10.1126/science.aaa8954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johansson V, Kuja-Halkola R, Cannon TD, Hultman CM, Hedman AM. A population-based heritability estimate of bipolar disorder – in a Swedish twin sample. Psychiatry Res. 2019;278:180–187. doi: 10.1016/j.psychres.2019.06.010. [DOI] [PubMed] [Google Scholar]
- 12.McIntosh AM, Sullivan PF, Lewis CM. Uncovering the genetic architecture of major depression. Neuron. 2019;102(1):91–103. doi: 10.1016/j.neuron.2019.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arnone D, Job D, Selvaraj S, Abe O, Amico F, Cheng Y, et al. Computational meta-analysis of statistical parametric maps in major depression. Hum Brain Mapp. 2016;37(4):1393-404. [DOI] [PMC free article] [PubMed]
- 14.Fu CHY, Fan Y, Davatzikos C. Widespread morphometric abnormalities in major depression: neuroplasticity and potential for biomarker development. Neuroimaging Clin N Am. 2020;30(1):85–95. doi: 10.1016/j.nic.2019.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fu CHY, Costafreda SG. Neuroimaging-based biomarkers in psychiatry: clinical opportunities of a paradigm shift. Can J Psychiatr. 2013;58(9):499–508. doi: 10.1177/070674371305800904. [DOI] [PubMed] [Google Scholar]
- 16.Varol E, Sotiras A, Davatzikos C. HYDRA: revealing heterogeneity of imaging and genetic patterns through a multiple max-margin discriminative analysis framework. NeuroImage. 2017;145:346–364. doi: 10.1016/j.neuroimage.2016.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drysdale AT, Grosenick L, Downar J, Dunlop K, Mansouri F, Meng Y, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23(1):28–38. doi: 10.1038/nm.4246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shah PJ, Glabus MF, Goodwin GM, Ebmeier KP. Chronic, treatment-resistant depression and right fronto-striatal atrophy. Br J Psychiatry. 2002;180(5):434–440. doi: 10.1192/bjp.180.5.434. [DOI] [PubMed] [Google Scholar]
- 19.Guo W, Liu F, Xue Z, Gao K, Liu Z, Xiao C, et al. Abnormal resting-state cerebellar–cerebral functional connectivity in treatment-resistant depression and treatment sensitive depression. Prog Neuro-Psychopharmacol Biol Psychiatry. 2013;44:51–57. doi: 10.1016/j.pnpbp.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 20.de Kwaasteniet BP, Rive MM, Ruhé HG, Schene AH, Veltman DJ, Fellinger L, et al. Decreased resting-state connectivity between neurocognitive networks in treatment resistant depression. Front Psychiatry. 2015;6:28. [DOI] [PMC free article] [PubMed]
- 21.Dinga R, Schmaal L, Penninx BWJH, van Tol MJ, Veltman DJ, van Velzen L, et al. Evaluating the evidence for biotypes of depression: Methodological replication and extension of Drysdale et al. (2017) NeuroImage. 2019;22:101796. doi: 10.1016/j.nicl.2019.101796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang J, Zhang M, Ahn H, Zhang Q, Jin TB, Li I, et al. Development and evaluation of a multimodal marker of major depressive disorder. Hum Brain Mapp. 2018;39(11):4420–4439. doi: 10.1002/hbm.24282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Belov V, Erwin-Grabner T, Gonul AS, Amod AR, Ojha A, Aleman A, et al. Multi-site benchmark classification of major depressive disorder using machine learning on cortical and subcortical measures. arXiv. 2022; Available from: http://arxiv.org/abs/2206.08122. Cited 2022 Sep 28. [DOI] [PMC free article] [PubMed]
- 24.Stolicyn A, Harris MA, Shen X, Barbu MC, Adams MJ, Hawkins EL, et al. Automated classification of depression from structural brain measures across two independent community-based cohorts. Hum Brain Mapp. 2020;41(14):3922–3937. doi: 10.1002/hbm.25095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Winter NR, Leenings R, Ernsting J, Sarink K, Fisch L, Emden D, et al. Quantifying deviations of brain structure and function in major depressive disorder across neuroimaging modalities. JAMA Psychiatry. 2022;79(9):879–888. doi: 10.1001/jamapsychiatry.2022.1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schmaal L, Pozzi EC, C Ho T, van Velzen LS, Veer IM, Opel N, et al. ENIGMA MDD: seven years of global neuroimaging studies of major depression through worldwide data sharing. Transl Psychiatry. 2020;10(1):172. doi: 10.1038/s41398-020-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shen X, Reus LM, Cox SR, Adams MJ, Liewald DC, Bastin ME, et al. Subcortical volume and white matter integrity abnormalities in major depressive disorder: findings from UK biobank imaging data. Sci Rep. 2017;7(1):5547. doi: 10.1038/s41598-017-05507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gartlehner G, Wagner G, Matyas N, Titscher V, Greimel J, Lux L, et al. Pharmacological and non-pharmacological treatments for major depressive disorder: review of systematic reviews. BMJ Open. 2017;7(6):e014912. doi: 10.1136/bmjopen-2016-014912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pomponio R, Erus G, Habes M, Doshi J, Srinivasan D, Mamourian E, et al. Harmonization of large MRI datasets for the analysis of brain imaging patterns throughout the lifespan. NeuroImage. 2020;208:116450. doi: 10.1016/j.neuroimage.2019.116450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wen J, Fu CHY, Tosun D, Veturi Y, Yang Z, Abdulkadir A, et al. Characterizing heterogeneity in neuroimaging, cognition, clinical symptoms, and genetics among patients with late-life depression. JAMA Psychiatry. 2022;79(5):464–474. doi: 10.1001/jamapsychiatry.2022.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kennedy SH, Downar J, Evans KR, Feilotter H, W. Lam RW, GM MQ, et al. The Canadian biomarker integration network in depression (CAN-BIND): advances in response prediction. CPD. 2012;18(36):5976–5989. doi: 10.2174/138161212803523635. [DOI] [PubMed] [Google Scholar]
- 32.Lam RW, Milev R, Rotzinger S, Andreazza AC, Blier P, Brenner C, et al. Discovering biomarkers for antidepressant response: protocol from the Canadian biomarker integration network in depression (CAN-BIND) and clinical characteristics of the first patient cohort. BMC Psychiatry. 2016;16(1):105. doi: 10.1186/s12888-016-0785-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brandt IM, Köhler-Forsberg K, Ganz M, Ozenne B, Jorgensen MB, Poulsen A, et al. Reward processing in major depressive disorder and prediction of treatment response – Neuropharm study. Eur Neuropsychopharmacol. 2021;44:23–33. doi: 10.1016/j.euroneuro.2020.12.010. [DOI] [PubMed] [Google Scholar]
- 34.Dam VH, Stenbæk DS, Köhler-Forsberg K, Ip C, Ozenne B, Sahakian BJ, et al. Hot and cold cognitive disturbances in antidepressant-free patients with major depressive disorder: a NeuroPharm study. Psychol Med. 2021;51(14):2347–2356. doi: 10.1017/S0033291720000938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fisher P, Ozenne B, Ganz M, Frokajer V, Dam V, Penninx B, et al. Emotional faces processing in major depressive disorder and prediction of antidepressant treatment response – a NeuroPharm study. J Psychopharmacol. In Press. [DOI] [PubMed]
- 36.Ip CT, Ganz M, Dam VH, Ozenne B, Rüesch A, Köhler-Forsberg K, et al. NeuroPharm study: EEG wakefulness regulation as a biomarker in MDD. J Psychiatr Res. 2021;141:57–65. doi: 10.1016/j.jpsychires.2021.06.021. [DOI] [PubMed] [Google Scholar]
- 37.Ip CT, Olbrich S, Ganz M, Ozenne B, Köhler-Forsberg K, Dam VH, et al. Pretreatment qEEG biomarkers for predicting pharmacological treatment outcome in major depressive disorder: independent validation from the NeuroPharm study. Eur Neuropsychopharmacol. 2021;49:101–112. doi: 10.1016/j.euroneuro.2021.03.024. [DOI] [PubMed] [Google Scholar]
- 38.Köhler-Forsberg K, Jorgensen A, Dam VH, Stenbæk DS, Fisher PM, Ip CT, et al. Predicting treatment outcome in major depressive disorder using serotonin 4 receptor PET brain imaging, functional MRI, cognitive-, EEG-based, and peripheral biomarkers: a NeuroPharm open label clinical trial protocol. Front Psychiatry. 2020;11:641. doi: 10.3389/fpsyt.2020.00641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Larsen SV, Ozenne B, Köhler-Forsberg K, Poulsen AS, Dam VH, Svarer C, et al. The impact of hormonal contraceptive use on serotonergic neurotransmission and antidepressant treatment response: results from the NeuroPharm 1 study. Front Endocrinol (Lausanne) 2022;13:799675. doi: 10.3389/fendo.2022.799675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trivedi MH, McGrath PJ, Fava M, Parsey RV, Kurian BT, Phillips ML, et al. Establishing moderators and biosignatures of antidepressant response in clinical care (EMBARC): rationale and design. J Psychiatr Res. 2016;78:11–23. doi: 10.1016/j.jpsychires.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qiu L, Xia M, Cheng B, Yuan L, Kuang W, Bi F, et al. Abnormal dynamic functional connectivity of amygdalar subregions in untreated patients with first-episode major depressive disorder. JPN. 2018;43(4):262–272. doi: 10.1503/jpn.170112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao Y, Niu R, Lei D, Shah C, Xiao Y, Zhang W, et al. Aberrant gray matter networks in non-comorbid medication-naive patients with major depressive disorder and those with social anxiety disorder. Front Hum Neurosci. 2020;14:172. doi: 10.3389/fnhum.2020.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhao Y, Zhang F, Zhang W, Chen L, Chen Z, Lui S, et al. Decoupling of gray and white matter functional networks in medication-naïve patients with major depressive disorder. J Magn Reson Imaging. 2021;53(3):742–752. doi: 10.1002/jmri.27392. [DOI] [PubMed] [Google Scholar]
- 44.Green S, Lambon Ralph MA, Moll J, Deakin JFW, Zahn R. Guilt-selective functional disconnection of anterior temporal and subgenual cortices in major depressive disorder. Arch Gen Psychiatry. 2012;69(10):1014–1021. doi: 10.1001/archgenpsychiatry.2012.135. [DOI] [PubMed] [Google Scholar]
- 45.Lythe KE, Gethin JA, Workman CI, Lambon Ralph MA, Deakin JFW, Moll J, et al. Subgenual activation and the finger of blame: individual differences and depression vulnerability. Psychol Med. 2022;52(8):1560–8. [DOI] [PubMed]
- 46.Nouretdinov I, Costafreda SG, Gammerman A, Chervonenkis A, Vovk V, Vapnik V, et al. Machine learning classification with confidence: application of transductive conformal predictors to MRI-based diagnostic and prognostic markers in depression. NeuroImage. 2011;56(2):809–813. doi: 10.1016/j.neuroimage.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 47.Sankar A, Zhang T, Gaonkar B, Doshi J, Erus G, Costafreda SG, et al. Diagnostic potential of structural neuroimaging for depression from a multi-ethnic community sample. BJPsych Open. 2016;2(4):247–254. doi: 10.1192/bjpo.bp.115.002493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wise T, Marwood L, Perkins AM, Herane-Vives A, Joules R, Lythgoe DJ, et al. Instability of default mode network connectivity in major depression: a two-sample confirmation study. Transl Psychiatry. 2017;7(4):e1105. doi: 10.1038/tp.2017.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wise T, Marwood L, Perkins AM, Herane-Vives A, Williams SCR, Young AH, et al. A morphometric signature of depressive symptoms in unmedicated patients with mood disorders. Acta Psychiatr Scand. 2018;138(1):73–82. doi: 10.1111/acps.12887. [DOI] [PubMed] [Google Scholar]
- 50.Workman CI, Lythe KE, McKie S, Moll J, Gethin JA, Deakin JF, et al. Subgenual cingulate-amygdala functional disconnection and vulnerability to melancholic depression. Neuropsychopharmacology. 2016;41(8):2082–2090. doi: 10.1038/npp.2016.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ford BN, Yolken RH, Aupperle RL, Teague TK, Irwin MR, Paulus MP, et al. Association of early-life stress with cytomegalovirus infection in adults with major depressive disorder. JAMA Psychiatry. 2019;76(5):545–547. doi: 10.1001/jamapsychiatry.2018.4543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Misaki M, Suzuki H, Savitz J, Drevets WC, Bodurka J. Individual variations in nucleus accumbens responses associated with major depressive disorder symptoms. Sci Rep. 2016;6(1):21227. doi: 10.1038/srep21227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zheng H, Ford BN, Bergamino M, Kuplicki R, Hunt PW, Bodurka J, et al. A hidden menace? Cytomegalovirus infection is associated with reduced cortical gray matter volume in major depressive disorder. Mol Psychiatry. 2021;26(8):4234–4244. doi: 10.1038/s41380-020-00932-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arnone D, McKie S, Elliott R, Thomas EJ, Downey D, Juhasz G, et al. Increased amygdala responses to sad but not fearful faces in major depression: relation to mood state and pharmacological treatment. AJP. 2012;169(8):841–850. doi: 10.1176/appi.ajp.2012.11121774. [DOI] [PubMed] [Google Scholar]
- 55.Arnone D, McKie S, Elliott R, Juhasz G, Thomas EJ, Downey D, et al. State-dependent changes in hippocampal grey matter in depression. Mol Psychiatry. 2013;18(12):1265–1272. doi: 10.1038/mp.2012.150. [DOI] [PubMed] [Google Scholar]
- 56.Dutta A, McKie S, Downey D, Thomas E, Juhasz G, Arnone D, et al. Regional default mode network connectivity in major depressive disorder: modulation by acute intravenous citalopram. Transl Psychiatry. 2019;9(1):116. doi: 10.1038/s41398-019-0447-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Godlewska BR, Browning M, Norbury R, Cowen PJ, Harmer CJ. Early changes in emotional processing as a marker of clinical response to SSRI treatment in depression. Transl Psychiatry. 2016;6(11):e957. doi: 10.1038/tp.2016.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Godlewska BR, Browning M, Norbury R, Igoumenou A, Cowen PJ, Harmer CJ. Predicting treatment response in depression: the role of anterior cingulate cortex. Int J Neuropsychopharmacol. 2018;21(11):988–996. doi: 10.1093/ijnp/pyy069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dunlop BW, Binder EB, Cubells JF, Goodman MM, Kelley ME, Kinkead B, et al. Predictors of remission in depression to individual and combined treatments (PReDICT): study protocol for a randomized controlled trial. Trials. 2012;13(1):106. doi: 10.1186/1745-6215-13-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dunlop BW, Rajendra JK, Craighead WE, Kelley ME, McGrath CL, Choi KS, et al. Functional connectivity of the subcallosal cingulate cortex and differential outcomes to treatment with cognitive-behavioral therapy or antidepressant medication for major depressive disorder. Am J Psychiatry. 2017;174(6):533–545. doi: 10.1176/appi.ajp.2016.16050518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shi Y, Zhang L, Wang Z, Lu X, Wang T, Zhou D, et al. Multivariate machine learning analyses in identification of major depressive disorder using resting-state functional connectivity: a multicentral study. ACS Chem Neurosci. 2021;12(15):2878–2886. doi: 10.1021/acschemneuro.1c00256. [DOI] [PubMed] [Google Scholar]
- 62.Yan CG, Chen X, Li L, Castellanos FX, Bai TJ, Bo QJ, et al. Reduced default mode network functional connectivity in patients with recurrent major depressive disorder. Proc Natl Acad Sci U S A. 2019;116(18):9078–9083. doi: 10.1073/pnas.1900390116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hu J, Liu J, Liu Y, Wu X, Zhuang K, Chen Q, et al. Dysfunction of the anterior and intermediate hippocampal functional network in major depressive disorders across the adult lifespan. Biol Psychol. 2021;165:108192. doi: 10.1016/j.biopsycho.2021.108192. [DOI] [PubMed] [Google Scholar]
- 64.Liu W, Wei D, Chen Q, Yang W, Meng J, Wu G, et al. Longitudinal test-retest neuroimaging data from healthy young adults in Southwest China. Sci Data. 2017;4(1):170017. doi: 10.1038/sdata.2017.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu Y, Meng J, Wang K, Zhuang K, Chen Q, Yang W, et al. Morphometry of the hippocampus across the adult life-span in patients with depressive disorders: association with neuroticism. Brain Topogr. 2021;34(5):587–597. doi: 10.1007/s10548-021-00846-0. [DOI] [PubMed] [Google Scholar]
- 66.Sacchet MD, Livermore EE, Iglesias JE, Glover GH, Gotlib IH. Subcortical volumes differentiate major depressive disorder, bipolar disorder, and remitted major depressive disorder. J Psychiatr Res. 2015;68:91–98. doi: 10.1016/j.jpsychires.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sacchet MD, Gotlib IH. Myelination of the brain in major depressive disorder: an in vivo quantitative magnetic resonance imaging study. Sci Rep. 2017;7(1):2200. doi: 10.1038/s41598-017-02062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schwartz J, Ordaz SJ, Kircanski K, Ho TC, Davis EG, Camacho MC, et al. Resting-state functional connectivity and inflexibility of daily emotions in major depression. J Affect Disord. 2019;249:26–34. doi: 10.1016/j.jad.2019.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Navrady LB, Wolters MK, MacIntyre DJ, Clarke TK, Campbell AI, Murray AD, et al. Cohort profile: Stratifying resilience and depression longitudinally (STRADL): a questionnaire follow-up of generation Scotland: Scottish family health study (GS:SFHS) Int J Epidemiol. 2018;47(1):13–14g. doi: 10.1093/ije/dyx115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bomyea J, Choi SH, Sweet A, Stein M, Paulus M, Taylor C. Neural changes in reward processing following approach avoidance training for depression. Soc Cogn Affect Neurosci. 2022;17(3):336–49. [DOI] [PMC free article] [PubMed]
- 71.Kryza-Lacombe M, Pearson N, Lyubomirsky S, Stein MB, Wiggins JL, Taylor CT. Changes in neural reward processing following amplification of positivity treatment for depression and anxiety: preliminary findings from a randomized waitlist controlled trial. Behav Res Ther. 2021;142:103860. doi: 10.1016/j.brat.2021.103860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 74.Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 75.Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, et al. The inventory of depressive symptomatology, clinician rating (IDS-C) and self-report (IDS-SR), and the quick inventory of depressive symptomatology, clinician rating (QIDS-C) and self-report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med. 2004;34(1):73–82. doi: 10.1017/S0033291703001107. [DOI] [PubMed] [Google Scholar]
- 76.Trajković G, Starčević V, Latas M, Leštarević M, Ille T, Bukumirić Z, et al. Reliability of the Hamilton rating scale for depression: a meta-analysis over a period of 49 years. Psychiatry Res. 2011;189(1):1–9. doi: 10.1016/j.psychres.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 77.Leucht S, Fennema H, Engel RR, Kaspers-Janssen M, Szegedi A. Translating the HAM-D into the MADRS and vice versa with equipercentile linking. J Affect Disord. 2018;226:326–331. doi: 10.1016/j.jad.2017.09.042. [DOI] [PubMed] [Google Scholar]
- 78.Rush AJ, Trivedi MH, Carmody TJ, Ibrahim HM, Markowitz JC, Keitner GI, et al. Self-reported depressive symptom measures: sensitivity to detecting change in a randomized, controlled trial of chronically depressed, nonpsychotic outpatients. Neuropsychopharmacol. 2005;30(2):405–416. doi: 10.1038/sj.npp.1300614. [DOI] [PubMed] [Google Scholar]
- 79.Uher R, Farmer A, Maier W, Rietschel M, Hauser J, Marusic A, et al. Measuring depression: comparison and integration of three scales in the GENDEP study. Psychol Med. 2008;38(2):289–300. doi: 10.1017/S0033291707001730. [DOI] [PubMed] [Google Scholar]
- 80.Bernstein IH, Rush AJ, Stegman D, Macleod L, Witte B, Trivedi MH. A comparison of the QIDS-C 16 , QIDS-SR 16 , and the MADRS in an adult outpatient clinical sample. CNS Spectr. 2010;15(7):458–468. doi: 10.1017/S1092852900000389. [DOI] [PubMed] [Google Scholar]
- 81.Liu J, Xiang YT, Lei H, Wang Q, Wang G, Ungvari GS, et al. Guidance on the conversion of the Chinese versions of the Quick Inventory of Depressive Symptomatology-Self-Report (C-QIDS-SR) and the Montgomery–Asberg Scale (C-MADRS) in Chinese patients with major depression. J Affect Disord. 2014;152–154:530–533. doi: 10.1016/j.jad.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 82.Citrome L, Abi-Dargham A, Bilder RM, Duffy RA, Dunlop BW, Harvey PD, et al. Making sense of the matrix: a qualitative assessment and commentary on connecting psychiatric symptom scale items to the research domain criteria (RDoC) Innov Clin Neurosci. 2022;19(1–3):26–32. [PMC free article] [PubMed] [Google Scholar]
- 83.Cuthbert BN. Research domain criteria: toward future psychiatric nosologies. Dialogues Clin Neurosci. 2015;17(1):89–97. doi: 10.31887/DCNS.2015.17.1/bcuthbert. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. AJP. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 85.Uher R, Frey BN, Quilty LC, Rotzinger S, Blier P, Foster JA, et al. Symptom dimension of interest-activity indicates need for aripiprazole augmentation of escitalopram in major depressive disorder: a CAN-BIND-1 report. J Clin Psychiatry. 2020;81(4):9256. doi: 10.4088/JCP.20m13229. [DOI] [PubMed] [Google Scholar]
- 86.Furukawa TA, Streiner DL, Azuma H, Higuchi T, Kamijima K, Kanba S, et al. Cross-cultural equivalence in depression assessment: Japan-Europe-north American study. Acta Psychiatr Scand. 2005;112(4):279–285. doi: 10.1111/j.1600-0447.2005.00587.x. [DOI] [PubMed] [Google Scholar]
- 87.Vindbjerg E, Makransky G, Mortensen EL, Carlsson J. Cross-cultural psychometric properties of the Hamilton depression rating scale. Can J Psychiatr. 2019;64(1):39–46. doi: 10.1177/0706743718772516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bashyam VM, Doshi J, Erus G, Srinivasan D, Abdulkadir A, Singh A, et al. Deep generative medical image harmonization for improving cross-site generalization in deep learning predictors. J Magn Reson Imaging. 2021;55(3):908–916. doi: 10.1002/jmri.27908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tustison NJ, Avants BB, Cook PA, Zheng Y, Egan A, Yushkevich PA, et al. N4ITK: improved N3 bias correction. IEEE Trans Med Imaging. 2010;29(6):1310–1320. doi: 10.1109/TMI.2010.2046908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Doshi J, Erus G, Ou Y, Gaonkar B, Davatzikos C. Multi-atlas skull-stripping. Acad Radiol. 2013;20(12):1566–1576. doi: 10.1016/j.acra.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Doshi J, Erus G, Ou Y, Resnick SM, Gur RC, Gur RE, et al. MUSE: MUlti-atlas region segmentation utilizing ensembles of registration algorithms and parameters, and locally optimal atlas selection. NeuroImage. 2016;127:186–195. doi: 10.1016/j.neuroimage.2015.11.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Asman AJ, Chambless LB, Thompson RC, Landman BA. Out-of-atlas likelihood estimation using multi-atlas segmentation. Med Phys. 2013;40(4):043702. doi: 10.1118/1.4794478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Davatzikos C, Genc A, Xu D, Resnick SM. Voxel-based morphometry using the RAVENS maps: methods and validation using simulated longitudinal atrophy. Neuroimage. 2001;14(6):1361–1369. doi: 10.1006/nimg.2001.0937. [DOI] [PubMed] [Google Scholar]
- 94.Ou Y, Sotiras A, Paragios N, Davatzikos C. DRAMMS: deformable registration via attribute matching and mutual-saliency weighting. Med Image Anal. 2011;15(4):622–639. doi: 10.1016/j.media.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sotiras A, Resnick SM, Davatzikos C. Finding imaging patterns of structural covariance via non-negative matrix factorization. NeuroImage. 2015;108:1–16. doi: 10.1016/j.neuroimage.2014.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sotiras A, Toledo JB, Gur RE, Gur RC, Satterthwaite TD, Davatzikos C. Patterns of coordinated cortical remodeling during adolescence and their associations with functional specialization and evolutionary expansion. Proc Natl Acad Sci U S A. 2017;114(13):3527–3532. doi: 10.1073/pnas.1620928114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wen J, Varol E, Chand G, Sotiras A, Davatzikos C, et al. MAGIC: Multi-scale heterogeneity analysis and clustering for brain diseases. In: Martel AL, Abolmaesumi P, Stoyanov D, Mateus D, Zuluaga MA, Zhou SK, et al., editors. Medical image computing and computer assisted intervention – MICCAI 2020. Cham: Springer International Publishing; 2020. pp. 678–687. [Google Scholar]
- 98.Li H, Satterthwaite TD, Fan Y. Large-scale sparse functional networks from resting state fMRI. NeuroImage. 2017;156:1–13. doi: 10.1016/j.neuroimage.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dosenbach NUF, Nardos B, Cohen AL, Fair DA, Power JD, Church JA, et al. Prediction of individual brain maturity using fMRI. Science. 2010;329(5997):1358–1361. doi: 10.1126/science.1194144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jafri MJ, Pearlson GD, Stevens M, Calhoun VD. A method for functional network connectivity among spatially independent resting-state components in schizophrenia. NeuroImage. 2008;39(4):1666–1681. doi: 10.1016/j.neuroimage.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Savadjiev P, Kindlmann GL, Bouix S, Shenton ME, Westin CF. Local white matter geometry from diffusion tensor gradients. NeuroImage. 2010;49(4):3175–3186. doi: 10.1016/j.neuroimage.2009.10.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zeng LL, Shen H, Liu L, Wang L, Li B, Fang P, et al. Identifying major depression using whole-brain functional connectivity: a multivariate pattern analysis. Brain. 2012;135(5):1498–1507. doi: 10.1093/brain/aws059. [DOI] [PubMed] [Google Scholar]
- 103.Toloşi L, Lengauer T. Classification with correlated features: unreliability of feature ranking and solutions. Bioinformatics. 2011;27(14):1986–1994. doi: 10.1093/bioinformatics/btr300. [DOI] [PubMed] [Google Scholar]
- 104.Elad M. Sparse and redundant representations: from theory to applications in signal and image processing. New York: Springer; 2010. p. 376. [Google Scholar]
- 105.Cui Z, Li H, Xia CH, Larsen B, Adebimpe A, Baum GL, et al. Individual variation in functional topography of association networks in youth. Neuron. 2020;106(2):340–353.e8. doi: 10.1016/j.neuron.2020.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kreutz-Delgado K, Murray JF, Rao BD, Engan K, Lee TW, Sejnowski TJ. Dictionary learning algorithms for sparse representation. Neural Comput. 2003;15(2):349–396. doi: 10.1162/089976603762552951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Olshausen BA, Field DJ. Sparse coding with an overcomplete basis set: a strategy employed by V1? Vis Res. 1997;37(23):3311–3325. doi: 10.1016/S0042-6989(97)00169-7. [DOI] [PubMed] [Google Scholar]
- 108.Vinje WE, Gallant JL. Sparse coding and decorrelation in primary visual cortex during natural vision. Science. 2000;287(5456):1273–1276. doi: 10.1126/science.287.5456.1273. [DOI] [PubMed] [Google Scholar]
- 109.Eavani H, Satterthwaite TD, Filipovych R, Gur RE, Gur RC, Davatzikos C. Identifying sparse connectivity patterns in the brain using resting-state fMRI. NeuroImage. 2015;105:286–299. doi: 10.1016/j.neuroimage.2014.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sahoo D, Satterthwaite TD, Davatzikos C. Hierarchical extraction of functional connectivity components in human brain using resting-state fMRI. IEEE Trans Med Imaging. 2021;40(3):940–950. doi: 10.1109/TMI.2020.3042873. [DOI] [PubMed] [Google Scholar]
- 111.Beer JC, Tustison NJ, Cook PA, Davatzikos C, Sheline YI, Shinohara RT, et al. Longitudinal ComBat: a method for harmonizing longitudinal multi-scanner imaging data. NeuroImage. 2020;220:117129. doi: 10.1016/j.neuroimage.2020.117129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fortin JP, Sweeney EM, Muschelli J, Crainiceanu CM, Shinohara RT. Alzheimer’s Disease Neuroimaging Initiative. Removing inter-subject technical variability in magnetic resonance imaging studies. Neuroimage. 2016;132:198–212. doi: 10.1016/j.neuroimage.2016.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fortin JP, Cullen N, Sheline YI, Taylor WD, Aselcioglu I, Cook PA, et al. Harmonization of cortical thickness measurements across scanners and sites. Neuroimage. 2018;167:104–120. doi: 10.1016/j.neuroimage.2017.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Johnson WE, Li C, Rabinovic A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics. 2007;8(1):118–127. doi: 10.1093/biostatistics/kxj037. [DOI] [PubMed] [Google Scholar]
- 115.Chen AA, Srinivasan D, Pomponio R, Fan Y, Nasrallah IM, Resnick SM, et al. Harmonizing functional connectivity reduces scanner effects in community detection. NeuroImage. 2022;256:119198. doi: 10.1016/j.neuroimage.2022.119198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chen AA, Beer JC, Tustison NJ, Cook PA, Shinohara RT, Shou H, et al. Mitigating site effects in covariance for machine learning in neuroimaging data. Hum Brain Mapp. 2022;43(4):1179–1195. doi: 10.1002/hbm.25688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.McDaid AF, Joshi PK, Porcu E, Komljenovic A, Li H, Sorrentino V, et al. Bayesian association scan reveals loci associated with human lifespan and linked biomarkers. Nat Commun. 2017;8:15842. doi: 10.1038/ncomms15842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wen J, Varol E, Sotiras A, Yang Z, Chand GB, Erus G, et al. Multi-scale semi-supervised clustering of brain images: deriving disease subtypes. Med Image Anal. 2022;1(75):102304. doi: 10.1016/j.media.2021.102304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yang Z, Wen J, Davatzikos C. Smile-GANs: Semi-supervised clustering via GANs for dissecting brain disease heterogeneity from medical images. arXiv:200615255 [cs, eess, q-bio, stat]. 2020; Cited 2022 Apr 29. Available from: http://arxiv.org/abs/2006.15255.
- 120.Chand GB, Dwyer DB, Erus G, Sotiras A, Varol E, Srinivasan D, et al. Two distinct neuroanatomical subtypes of schizophrenia revealed using machine learning. Brain. 2020;143(3):1027–1038. doi: 10.1093/brain/awaa025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Timmerby N, Andersen JH, Søndergaard S, Østergaard SD, Bech P. A systematic review of the clinimetric properties of the 6-item version of the Hamilton depression rating scale (HAM-D6) Psychother Psychosom. 2017;86(3):141–149. doi: 10.1159/000457131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Original data can be requested from each consortium member. Derived data in the present consortium can be made available from the corresponding author on reasonable request and with permission of each consortium member.