Abstract
Objectives
COVID-19 has highlighted the importance of hygiene in home and everyday life (HEDL) to build population resilience against ongoing infectious disease threats. Despite having high awareness of hygiene, people have relatively poor understanding of hygiene risk which compromises their ability to follow advice. This paper combines new insights into hygiene science and hygiene behaviour to propose a framework for achieving more effective behavior. It is aimed at supporting government initiatives to build hygiene resilience within the UK population.
Study design
Non-systematic narrative review.
Methods
The review is based on findings of recent consensus reviews, prepared by acknowledged hygiene experts. It also draws on studies of hygiene understanding, drivers for behaviour change and behaviour change models.
Results
To build hygiene resilience, HEDL hygiene requires a risk management approach where practices combine to reduce infection risk in community populations to an acceptable level. Using this we construct a framework showing when, where and how to practice hygiene. Based on visualization, it gives clear practical guidance and develops better hygiene understanding. Promoting this approach using health belief models ensures behaviours that are embedded are fit for purpose.
Conclusions
A risk management approach to hygiene, promoted through behaviour change models, provides a framework for developing effective resilient hygiene behaviour. To achieve this, however, the separate aspects of HEDL hygiene (food, healthcare, pandemic preparedness) must be combined and communicated in a user-centric manner. Leadership teams must also be established with sole responsibility for HEDL hygiene, and the power to drive change.
Keywords: Hygiene, Infection prevention, Targeted hygiene, Behaviour change, Health resilience, Antimicrobial resistance
1. Introduction
Significant trends, outlined in this review, highlight the importance of the hygiene we practice in our homes and everyday lives to reduce spread of infection, and indicate the need for re-evaluation of hygiene in public health to meet current and future needs. Hygiene behaviours in our homes and everyday lives range from routine practices whilst handling food, using the toilet, caring for domestic animals and laundering clothing, to dealing with situations where there is increased risk (e.g., flu seasons, epidemics, pandemics), or where someone more vulnerable to infection is receiving care, or caring for themselves.
In response to the pandemic, the need to strengthen hygiene resilience is recognised internationally [1]. In 2021, UK Government published its vision for a National Health Resilience Strategy, aimed at making the UK, and UK public, better able to adapt to uncertainty and address risk and adversity [2,3]. As stated in the UK 2019 action plan on antimicrobial resistance (AMR) [4] “when it comes to preventing infectious disease, government can only do so much – the public have a huge role to play”.
Since 2017, The International Scientific Forum on Home Hygiene (IFH) has been working with experts in home and everyday life hygiene to review the status of hygiene practice in community, rather than clinical settings. Consensus reports published in 2018 and 2021 [5.6] identify 3 key issues that must be addressed to develop public behaviour that meets ongoing needs:
-
1.
The separate aspects of hygiene (food safety, healthcare, AMR, pandemic preparedness etc) must be unified into an approach which recognises that they are all governed by the same microbiological principles and need to be communicated in a user-centred manner.
-
2.
Hygiene behaviour policies in home and everyday life must be based on a Microbial Risk Management approach that focuses on reducing population exposure to harmful microbes.
-
3.
The need to develop effective hygiene behaviour change strategies.
Need for action is further demonstrated by public polling studies (section 3.2) which indicate that relatively poor public understanding of hygiene practice compromised their ability to adapt their behaviour in response to advice during the COVID-19 pandemic.
The purpose of this narrative review is to evaluate current knowledge of these issues, propose an evidence-based strategy that better meets C21st needs, and identify key actions that need to be taken. The aim is to inform policy debate in developing public hygiene behaviour to meet current and future needs. Whilst focussed on the UK, the underlying principles apply globally to any community setting, with local adaptation as necessary to address factors including disease priorities, access to water and sanitation, educational status, etc.
2. Methods
This paper builds on findings and recommendations from consensus reviews prepared in 2018 and 2021 by experts in different aspects of hygiene in home and everyday life settings [5,6]. It also draws on other expert reviews pertinent to the aims of this paper [[7], [8], [9], [10], [11], [12], [13], [14]] including experts in health behaviour change [[15], [16], [17]], and new data obtained through polling to evaluate public understanding of hygiene [[18], [19], [20], [21]]. These insights are brought together to propose a policy for effective and sustainable behaviour change.
3. Results
In sections 1, 2, 3 we evaluate current understanding of the 3 key issues set out in the introduction above. In section 3.4 we propose a strategy for behaviour change.
3.1. Importance of hygiene in home and everyday life and the need for a unified approach
Significant trends have occurred in recent years, which re-emphasize the importance of improving hygiene in home and everyday life (HEDL) [5,6]. One of the barriers to action is that the component parts of HEDL hygiene are administered separately: food safety at home is dealt with as an extension of “farm to fork”; hygiene in home healthcare is dealt with as an extension of infection prevention in hospitals and care homes; tackling AMR in the community is dealt with as an extension of infection prevention and control in hospital and care home settings. As a result, hygiene in HEDL may be overlooked. It is only when viewed collectively that the full impact of hygiene-related disease in the community and cost-benefits of promoting behaviour change relative to other interventions, e.g., vaccines can be seen.
3.1.1. The threat of further epidemics and pandemics
In reducing the risk of emerging infections becoming epidemics and pandemics, hygiene behaviour of the public plays a vital role before measures such as vaccines can be put in place [5,6]. In March 2022, UK government and industry committed to producing effective vaccines and therapeutics within 100 days of an epidemic or pandemic threat being identified [22]. COVID-19 demonstrated this is still short of what is needed to avert a pandemic of a highly infectious strain implying that public hygiene behaviour will continue to play a key role.
3.1.2. Antimicrobial resistance (AMR)
AMR is one of the biggest threats to global health [23]. HEDL hygiene addresses AMR by preventing infections, thereby avoiding antibiotic prescribing and reducing spread of antibiotic resistant bacteria [7,24]. A consensus review of hygiene in tackling AMR [7] concluded “although WHO, EU and US action plans emphasize the need for society-wide engagement, focusing on prevention first, national plans across the world still mostly focus on healthcare facilities”.
3.1.3. Infectious intestinal diseases
The importance of everyday food hygiene in reducing the burden of foodborne infections is well accepted, with norovirus and Campylobacter being the most frequent cause [[5], [6], [7], [8], [9]]. The estimated UK burden of gastrointestinal infection is 17 million cases annually with 11 million days lost for people of working age [25].
A barrier to food hygiene behaviour change is that the public, and sometimes healthcare experts, tend to believe foodborne infection is less likely to occur in the home than in restaurants and takeaways [26,27]. Estimates from Europe, US and Canada suggest that the home is implicated in 7 up to as much as 46% of foodborne outbreaks [6].
Norovirus is readily transmitted from person-to-person via hands as well as food and is recognised as the most significant cause of infectious intestinal disease in the developed world [28]. Studies in England and Wales suggest 1 in 25 people contract norovirus each year [29].
3.1.4. Vulnerable groups
The number of people, living in the community, who must shield because they are more vulnerable to infection continues to increase, and was estimated in 2009 to account for 20% or more of the population [10]. With an ageing population who have reduced immunity to infection, often exacerbated by co-morbidities such as diabetes and cancer, this will continue to increase. It also includes the very young and discharged hospital patients being cared for at home, sometimes with invasive devices such as catheters. Also at risk are those with chronic and degenerative illnesses (e.g. HIV/AIDS) or receiving immunosuppressant therapies.
Importantly COVID-19 showed that protecting clinically vulnerable groups can drive health strategy; 2020/1 lockdowns were driven by need to sustain hospital bed and intensive care availability for vulnerable individuals who became critically ill [30].
3.1.5. Hygiene in public spaces
A key issue highlighted by COVID-19 is the importance of hygiene in shared use of public spaces. To reopen after lockdown, offices, restaurants, shops, and supermarkets had to implement strategies to make them “COVID secure”. Spraying and fogging of environmental areas and surfaces in open spaces and deep-cleaning of indoor premises in the mistaken belief this can make them “COVID secure” indicates lack of understanding of risk management [[31], [32], [33], [34]]. With safety depending upon shared responsibility, managers of public venues need to not only take responsibility for cleanliness, but also for enabling and encouraging the public to adopt good hygiene practice.
3.1.6. COVID-19 – an opportunity for change
Heightened awareness of hygiene provides an unprecedented opportunity to improve public hygiene behaviours. Online public polling in England in 2022 by the IFH and the Royal Society for Public Health [20,21] (Table 1) showed that more than 70% agreed that COVID-19 has shown why practising good hygiene is important. An earlier 2018 poll [11,18] showed that people are also aware that poor hygiene contributes to AMR, and good hygiene reduces pressure on the NHS by preventing ill health.
Table 1.
Online polling of public opinion on the importance of hygiene.
| Polling date | Population size | Area | Question posed | % Agree | Ref |
|---|---|---|---|---|---|
| April 2022 | 2084 | England | Covid shows why practising good hygiene is important to protect against infectious diseases | 79% | [20,21] |
| I intend to continue to make greater effort to practise good hygiene | 77% | ||||
| Adopting hygiene behaviours to reduce transmission of infection is as important as changing behaviours to reduce climate change | 70% | ||||
| July 2018 | 1730 | UK | Poor hygiene contributes to antimicrobial resistance | 50% | [11,18] |
| Hygiene is important because it reduces pressure on the National Health Service by preventing ill health. | 74% |
Dramatic falls in levels of influenza, gastrointestinal infections, respiratory syncytial virus and rhinovirus, and reduced antibiotic prescribing during the pandemic demonstrate the extent to which infection can be contained through public-driven interventions that reduce exposure to pathogens [[35], [36], [37], [38]].
Although it appears that the public would be receptive to, more hygiene guidance, to capitalize on this opportunity, key issues, as outlined in 3.2 and 3.3 below need to be addressed. These reflect the view [5,6] that to change hygiene behaviour, it must be approached from the point of view of the public and their daily life actions to avoid exposure to human, food-and animal-borne pathogens, and respond to specific threats.
3.2. Behaviour change strategies must include changing public understanding of hygiene and hygiene issues
An important finding of recent polling is the extent of public misunderstanding about hygiene and how it differs from cleanliness [11,[18], [19], [20], [21]]. An IFH survey of media coverage [39] suggests we still largely see hygiene as synonymous with cleanliness aimed at eradicating dirt – inappropriately regarded as the main source of harmful microbes. An objective of the 2018 [11,18] poll was to elucidate how hygiene behaviours reflect beliefs about risks. Misperception of “what is risky” appears to be influenced by the belief that dirt and cleanliness are key indicators of infection risk prompting them to practice untargeted routine cleaning behaviours with little hygiene benefit.
These problems were also highlighted in the 2022 poll [20,21] which showed misunderstanding of how to prevent spread of COVID-19. Importantly 86–90% of respondents identified “after coughing, sneezing and nose blowing, after touching surfaces touched by others, when returning home and before eating food with fingers” as important moments to wash hands. But at the same time 90 and 84% respectively mistakenly believed that handwashing after using the toilet and before handling raw meat and poultry (actions to prevent spread of gastrointestinal pathogens) could prevent transmission of COVID-19, demonstrating lack of understanding of the route of infection of this disease. Poor understanding of the route of COVID-19 infection [20,21] was also demonstrated by the fact that 31% mistakenly believed they could be infected by virus penetrating through the skin of their hands. This may be a reason why 59% said wearing gloves was important to prevent spread of COVD-19, failing to recognise that gloved and ungloved hands can transmit infection to the eyes, nose and mouth.
During the pandemic, official advice focussed on “wash your hands frequently” but gave little guidance on when and why we need to do this, which could explain why some people thought they could be infected through their hands. Additionally, 57% said that, after someone in their home has had COVID-19, it needs to be “deep cleaned” to get rid of the virus, and 49% said they had started using an antibacterial cleaner for cleaning their home [20,21]. Inability to distinguish risk surfaces (hands and hand contact surfaces) from rarely touched, less risky environmental surfaces is unsurprising in view of media images of indiscriminate spraying surfaces in public places [[31], [32], [33], [34]]. It seems people were misled by myths and misunderstandings about cleanliness into taking inappropriate actions which would have little effect on spread of COVID-19.
3.3. The need for a user-centred approach to hygiene based on risk management
Developing HEDL hygiene behaviour that meets current and future needs requires a rethink, and acceptance that infection control guidelines formulated for clinical settings (e.g., deep cleaning, glove wearing) are not necessarily appropriate or effective in everyday life settings. Rather than focusing on zero tolerance (elimination of pathogens), as demanded in clinical settings, HEDL hygiene needs to be addressed by using a risk management approach aimed at reducing population infection risk to an acceptable level.
A core principle of risk management [40] is that a hazard (harmful microbes) may be present on hands, surfaces or in the air, but whether this poses a risk to health depends on the probability of being exposed to them. This being the case, rather than trying to eliminate harmful microbes, impossible in everyday life settings, hygiene advice should focus on reducing exposure: those not exposed to microbes cannot become infected. This allows us to identify times and places where pathogens represent a significant risk, and importantly differentiating places where removal by cleaning and/or disinfection has little impact [[5], [6], [7],12].
Progressively risk management is being accepted as a practical, evidence-based approach to developing public health measures, particularly those requiring a multibarrier approach [13]. Ever-increasing access to quantitative data on spread, exposure and infectivity rates for harmful microbes, and application of Quantitative Microbial Risk assessment, now provide tools to estimate the impact of hygiene protocols on infection rates in community settings. These data enable validation of interventions in situations where data from intervention studies are unavailable or unreliable because of difficulties in controlling such studies [[41], [42], [43]]. A case in point occurred at the outset of the pandemic, when the public were advised against wearing face coverings on the basis that clinical data supporting efficacy was “not very strong” [44]. This advice was later changed based on risk modelling data indicating significant infection risk reduction in community populations [45].
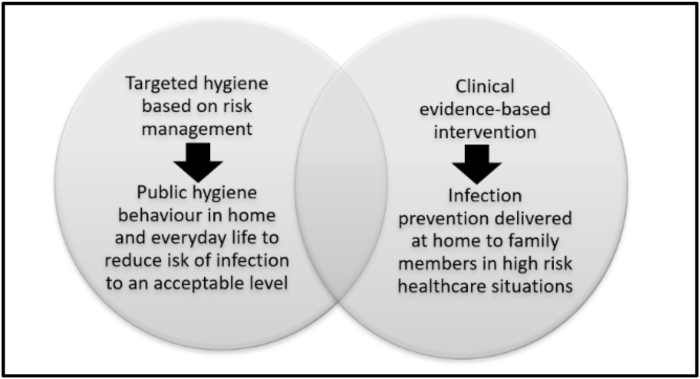
Whilst it is recognised, as shown in Fig. 1, that there is no clear distinction between routine daily hygiene carried out by the public, and clinical care delivered at home by family members or carers, e.g., care of patients recently discharge from a health-care setting, overall hygiene protocols for home settings should be based on risk management.
Fig. 1.
The interaction between everyday life hygiene and hygiene in home healthcare.
3.4. Proposal for a user-centred approach to hygiene based on risk management
Since 1997, IFH has been developing an approach to hygiene based on accepted principles of risk management, known as Targeted Hygiene [[5], [6], [7],11,12,14]. This focuses hygiene practices at the times when harmful microbes are most likely to spread, and the places through which they are spread, to break the chain of infection. It is applicable to all hygiene-related infections, including gastrointestinal, respiratory and skin infections. Targeted Hygiene focuses on hygiene as experienced by the public, as a set of interrelated, interdependent actions performed throughout daily life to reduce exposure to harmful microbes. In this way it provides a framework for communicating hygiene in a user-centric manner to be better understood.
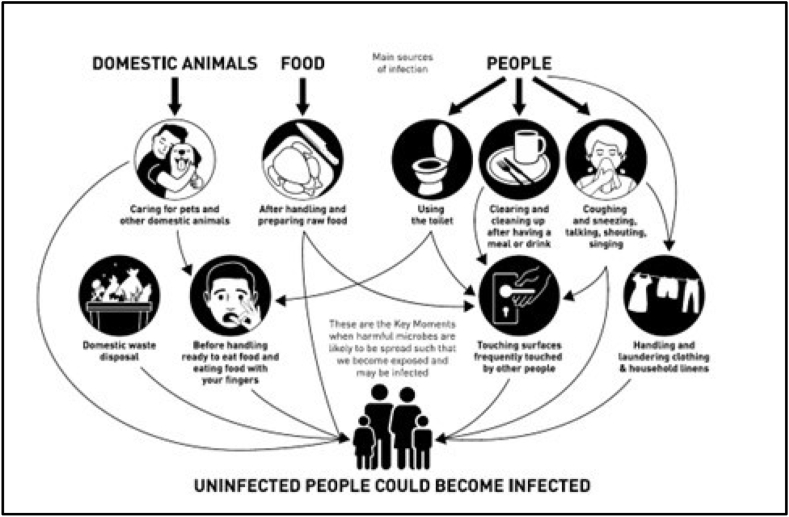
Microbiological and behavioural assessment suggests there are 9 key moments in our daily lives when harmful microbes are most likely to be spreading such that we can become exposed and infected (Fig. 2) [46]. Microbiological and epidemiological data underpinning development of Targeted Hygiene is detailed in an IFH review [14].
Fig. 2.
The key moments for hygiene in home and everyday life settings (Copyright: International Scientific Forum on Home Hygiene).
What makes this approach user-centric is that it communicates hygiene actions in the sequence in which the public need to receive it. It starts by identifying the moments in our daily lives WHEN practising hygiene is important (e.g., handling raw foods or using the toilet), and the places WHERE we need to act at that moment (hands, surfaces etc). Thirdly it identifies HOW to practise hygiene in those places (handwashing, surface cleaning, mask wearing etc) [46]. Although handwashing is central to all moments, this approach shows when it needs to be performed and the need to combine it with actions at other critical points, to maximise impact on infection risk. Although 83% of people polled in 2022 [20,21] said ‘None of the measures we take are 100% effective, so it's important to follow as many recommended measures as possible”, messaging has so far failed to convince the public to continue wearing masks voluntarily in crowded places [47].
Establishing a “when, where, how” framework works to build resilience to change; because it is common to all hygiene-related infectious diseases it enables the public to easily understand, adapt and respond to “enhanced” or intensified hygiene advice when necessary.
3.5. Targeted hygiene - a tool for developing behaviour change strategies
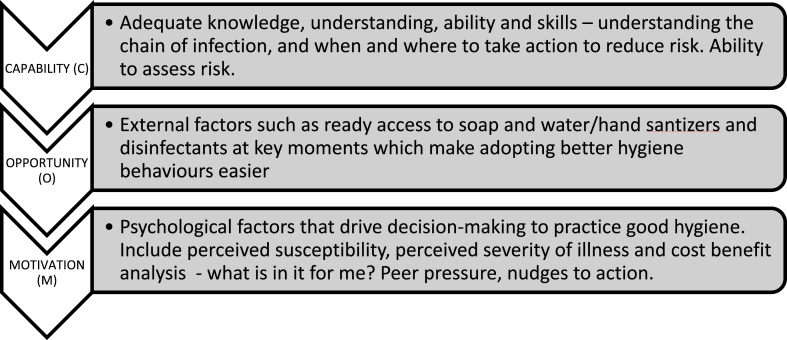
In the last few years, we have seen development of the Health Belief Model [15,16] and COM-B [17] (Fig. 3) for changing hygiene behaviours. Targeted Hygiene provides a hygiene practice policy which, when combined with these models not only promotes behaviour change, but also ensures that hygiene behaviours and messages are effective in protecting against exposure to infection.
Fig. 3.
Targeted Hygiene Behaviour Change based on Health Belief Models.
Fig. 3 shows that Targeted Hygiene works not only to communicate knowledge (i.e., effective practice communicated in a way that builds cognitive understanding), but also to develop positive, constructive messaging (motivation) which build on “opportunities” such as provision of hand hygiene facilities. Rather than giving prescriptive guidance, Targeted Hygiene can be communicated through visual images, graphics and YouTube videos that work to dispel myths and misunderstandings and engage and empower the public to practice effective hygiene (as opposed to visible cleanliness) at key moments [46].
Targeted Hygiene, applied with behaviour change models was used to control transmission of COVID-19 and other infections, in public areas at the 2021 COP26 Glasgow summit [48,49]. Public messaging and strategically placed hand santizer stations were deployed to promote targeted hand hygiene.
4. Discussion
From the 1970s when experts were predicting the end of the era of infectious diseases [50], 2020 brought a pandemic with 6 million reported deaths, long-term health problems, and global disruption of public and economic life. The evidence given in the above narrative indicates that to build public hygiene understanding and resilience that meets current and future needs, the following actions are needed:
4.1. Action 1. establish effective leadership
The separate aspects of HEDL hygiene (food safety, healthcare, AMR, pandemic preparedness) need to be brought together under a dedicated leadership team with power and investment to drive change. Developing a consistent approach to public messaging that recognises that all aspects of hygiene are based on the same underlying principles requires a strategy that is user-centric. With separate aspects of HEDL hygiene being dealt with by different agencies or different departments within agencies, vital data on the overall health, economic and societal costs of hygiene-preventable diseases are lacking and need to be generated.
The leadership team must be supported by advisory groups from a wide range of disciplines, departments, agencies and NGOs (environmental health, food safety, pandemic preparedness, healthcare and AMR).
4.2. Action 2. adopt a risk management approach to HEDL hygiene
HEDL Hygiene requires a risk management approach, focussed on reducing infection exposure risk to an acceptable level. Targeted Hygiene provides a framework to address all types of infection risks (respiratory, skin, intestinal, etc) by communicating when, where and how to practise hygiene, but also provides a tool for building hygiene understanding and resilience. Further work is needed to develop Quantitative Microbial Risk Assessment models that utilise the database of quantitative information about how pathogens spread in occupied settings, to produce quantitative estimates of the impact of public hygiene behaviours in reducing infection rates.
4.3. Action 3. develop effective behaviour change strategies
Despite high awareness of the importance of hygiene, people are at risk because of their poor understanding of the nature of infection routes and risks they encounter. Hygiene behaviour change models together with the Targeted Hygiene framework need to be further developed and tested as a means to develop more effective and resilient hygiene behaviour.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.WHO’s 7 policy recommendations on building resilient health systems 2021. https://www.who.int/news/item/19-10-2021-who-s-7-policy-recommendations-on-building-resilient-health-systems [PMC free article] [PubMed]
- 2.UK Biological Security Strategy. UK Government Cabinet Office; 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1055196/biological-security-strategy-cfe.pdf [Google Scholar]
- 3.The National Resilience Strategy – a Call for Evidence. UK Government Cabinet Office; 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1001404/Resilience_Strategy_-_Call_for_Evidence.pdf [Google Scholar]
- 4.UK 5-year Action Plan for Antimicrobial Resistance 2019 to 2024. Department of Health and Social Care; 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/784894/UK_AMR_5_year_national_action_plan.pdf [Google Scholar]
- 5.Developing and promoting hygiene in home and everyday life to meet 21st Century needs; what can we learn from the COVID-19 pandemic? International Scientific Forum on Home Hygiene. 2021 https://www.ifh-homehygiene.org/review/developing-and-promoting-home-and-everyday-life-hygiene-meet-21st-century-needs-what-can-we [Google Scholar]
- 6.Containing the Burden of Infectious Diseases Is Everyone's Responsibility: a Call for an Integrated Strategy for Developing and Promoting Hygiene Behaviour Change in Home and Everyday Life”. International Scientific Forum on Home Hygiene; 2018. https://www.ifh-homehygiene.org/review/containing-burden-infectious-diseases-everyones-responsibility-call-integrated-strategy [Google Scholar]
- 7.Maillard J.-Y., Bloomfield S.F., Courvalin P., Essack Y.S., Gandra S., Gerba P., et al. Reducing antibiotic prescribing and addressing the global problem of antibiotic resistance by targeted hygiene in the home and everyday life settings. Am. J. Infect. Control. 2020;48:1090–1099. doi: 10.1016/j.ajic.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO estimates of the global burden of foodborne diseases. https://apps.who.int/iris/handle/10665/199350 Foodborne diseases burden epidemiology reference group 2007-2015.
- 9.Redmond E.C., Curnin A., Eves A., Raats M., Day C., Morris J. Systematic review of the relative proportion of foodborne disease associated with food preparation or handling practices in the home. FSA Research project report. 2018 https://www.food.gov.uk/research/foodborne-diseases/systematic-review-of-the-relative-proportion-of-foodborne-disease-caused-by-food-preparation-or-handling-within-the-home [Google Scholar]
- 10.The Global Burden of Hygiene-Related Diseases in Relation to the Home and Community. International Scientific Forum on Home Hygiene; 2009. https://www.ifh-homehygiene.org/review/global-burden-hygiene-related-diseases-relation-home-and-community [Google Scholar]
- 11.Too Clean or Not Too Clean? the Case for Targeted Hygiene in Home and Everyday Life. Royal Society for Public Health; 2018. https://www.rsph.org.uk/static/uploaded/06b37f30-2241-4e98-aba93fc15346e7a5.pdf [Google Scholar]
- 12.Bloomfield S.F., Rook G.A., Scott E.A., Shanahan F., Stanwell-Smith R., Turner P. Time to abandon the hygiene hypothesis: new perspectives on allergic disease, the human microbiome, infectious disease prevention and the role of targeted hygiene. Perspec Public Heal. 2016;136:213–224. doi: 10.1177/1757913916650225. https://doi:10.1177/1757913916650225 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grading Evidence and Recommendations for Public Health Interventions: Developing and Piloting a Framework. UK Health Development Agency; London: 2005. https://orca.cardiff.ac.uk/id/eprint/69810/1/grading_evidence.pdf [Google Scholar]
- 14.The Chain of Infection Transmission in the Home and Everyday Life Settings, and the Role of Hygiene in Reducing the Risk of Infection. International Scientific Forum on Home Hygiene; 2012. https://www.ifh-homehygiene.org/review/chain-infection-transmission-home-and-everyday-life-settings-and-role-hygiene-reducing-risk [Google Scholar]
- 15.Jones C.L., Jensen J.D., Scherr C.L., Brown N.R., Christy K., Weaver J. The Health Belief Model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. 2015;30:566–576. doi: 10.1080/10410236.2013.873363. https://doi:10.1080/10410236.2013.873363 Epub 2014 Jul 10. PMID: 25010519; PMCID: PMC4530978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ackerley L. Consumer awareness of food hygiene and food poisoning. Environ. Health. 1994;102:69–74. [Google Scholar]
- 17.Michie S., Van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:1–2. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bloomfield S.F. RSPH and IFH call for a clean-up of public understanding and attitudes to hygiene. 2019;139:285–288. doi: 10.1177/1757913919878367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.International Association for Soaps, Detergents and Maintenance Products. 2021. Developing household hygiene to meet 21st century needs: a collaborative industry/academia report on cleaning and disinfection in homes & analysis of European consumers' hygiene beliefs and behaviour in 2020.https://www.ifh-homehygiene.org/review/developing-household-hygiene-meet-21st-century-needs-collaborative-industryacademia-report [Google Scholar]
- 20.It's Time to Clean up Our Act on Home Hygiene: Embedding Targeted Hygiene for Health Resilience. Royal Society for Public Health; 2022. www.rsph.org.uk/TargetedHygiene I January 2023. [Google Scholar]
- 21.Bloomfield S.F., Ackerley L. Perspectives in Public Health, in press; 2023. Developing Better Understanding of Hygiene Is Key to Developing Hygiene Behaviour Change in Home and Everyday Life Settings. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joint Statement from the UK Government, CEPI, IFPMA, BIA, BIO and DCVMN on Delivering the 100 Days Mission. UK Department of Health and Social Care; 2022. https://www.gov.uk/government/publications/joint-statement-on-delivering-the-100-days-mission/joint-statement-from-the-uk-government-cepi-ifpma-abpi-bia-bio-and-dcvmn-on-delivering-the-100-days-mission [Google Scholar]
- 23.Antibiotic Resistance. World Health Organisation; 2020. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance [Google Scholar]
- 24.Collignon P., Beggs J.J., Walsh T.R., Gandra S., Laxminarayan R. Anthropological and socioeconomic factors contributing to global antimicrobial resistance: a univariate and multivariable analysis. Lancet Planet. Health. 2018 Sep;2(9):e398–e405. doi: 10.1016/S2542-5196(18)30186-4. https://doi:10.1016/S2542-5196(18)30186-4 [DOI] [PubMed] [Google Scholar]
- 25.The Second Study of Infectious Intestinal Diseases in the Community (IID2 Study) 2016. https://www.food.gov.uk/research/foodborne-disease/the-second-study-of-infectious-intestinal-disease-in-the-community-iid2-study [Google Scholar]
- 26.Food Standards Agency and Government Statistical Service . February 2020. Public Attitudes Tracker, Wave 19.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/919329/public_attitudes_tracker_wave_19_final_report.pdf Accessed August 2022 [Google Scholar]
- 27.Fighting the Germ of Our Near Obsessive Cleanliness. 2015. https://mumbaimirror.indiatimes.com/others/health-lifestyle/Fighting-the-germ-of-our-near-obsessive-cleanliness/articleshow/50085504.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst [Google Scholar]
- 28.Lopman B.A., Steele D., Kirkwood C.D., Parashar U.D. The vast and varied global burden of norovirus: prospects for prevention and control. PLoS Med. 2016;13(4) doi: 10.1371/journal.pmed.1001999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tam C.C., Rodrigues L.C., Viviani L., Dodds J.P., Evans M.R., Hunter P.R., et al. Longitudinal study of infectious intestinal disease in the UK (IID2 study): incidence in the community and presenting to general practice. Gut. 2011;61:69–77. doi: 10.1136/gut.2011.238386. https://doi:10.1136/gut.2011.23838618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.New TV Advert Urges Public to Stay at Home to Protect the NHS and Save Lives. 2021. https://www.gov.uk/government/news/new-tv-advert-urges-public-to-stay-at-home-to-protect-the-nhs-and-save-lives [Google Scholar]
- 31.Thompson D. 2020. The Atlantic.https://www.theatlantic.com/ideas/archive/2020/07/scourge-hygiene-theater/614599/ Hygiene Theater Is a Huge Waste of Time. [Google Scholar]
- 32.Palmer M. 2020. Spray that Costs Pennies and Kills Viruses Instantly Could Be a Simple, Cheap Solution to Britain's Covid Nightmare - as Scientists Ask Why We're Not Already Using it.https://www.dailymail.co.uk/news/article-8558121/Spray-costs-pennies-kills-viruses-instantly-simple-solution-Covid-nightmare.html?ito=email_share_article-bottom%22%20%5Ct%20%22_blank [Google Scholar]
- 33.Coronavirus Editorial. Is in the air — there's too much focus on surfaces. Nature. 2021;590:7. doi: 10.1038/d41586-021-00277-8. [DOI] [PubMed] [Google Scholar]
- 34.Safety Precautions when Using Electrostatic Sprayers, Foggers, Misters, or Vaporizers for Surface Disinfection during the COVID-19 Pandemic. Centers for Disease Control and Prevention; 2021. https://www.cdc.gov/coronavirus/2019-ncov/php/eh-practitioners/sprayers.html [Google Scholar]
- 35.Love N.K., Elliot A.J., Chalmers R.M., Douglas A., Gharbia S., McCormick J., et al. Impact of the COVID-19 pandemic on gastrointestinal infection trends in England. February– July 2020. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-050469. https://doi:10.1136/bmjopen-2021-050469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sullivan S.G., Carlson S., Cheng A.C., Chilver M.B., Dwyer D.E., Irwin M., et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.47.2001847. https://doi:10.2807/1560-7917.ES.2020.25.47 2001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lepak A.J., Taylor L.N., Stone C.A., Schulz L.T., Anderson M.C., Fox B.C., et al. Association of changes in seasonal respiratory virus activity and ambulatory antibiotic prescriptions with the COVID-19 pandemic. JAMA Intern. Med. 2021;181:1399–1402. doi: 10.1001/jamainternmed.2021.2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Armitage R., Nellums L.B. Antibiotic prescribing in general practice during COVID-19. Lancet Infect. Dis. 2021;21(6):e144. doi: 10.1016/S1473-3099(20)30917-8. https://10.1016/S1473-3009(20)30917-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perceptions of Cleanliness, Hygiene and Hygiene Issues: a Survey of UK and US Media Coverage 1989 to 2017. International Scientific Forum on Home Hygiene; 2017. https://www.ifh-homehygiene.org/review/perceptions-cleanliness-hygiene-and-hygiene-issues-%E2%80%93-survey-uk-and-us-media-coverage-1989 [Google Scholar]
- 40.Notermans S., Barendsz A.W. In: Microbiological Risk Assessment in Food Processing. Brown M., Stringer M., editors. Woodhead Publishing Series in Food Science, Technology and Nutrition; 2002. Rombouts F the evolution of microbiological risk assessment; pp. 5–43. [Google Scholar]
- 41.Haas C.N., Marie J.R., Rose J.B., Gerba C.P. Assessment of benefits from use of antimicrobial hand products: reduction in risk from handling ground beef. Int. J. Hyg Environ. Health. 2005;208:461–466. doi: 10.1016/j.ijheh.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 42.Ryan M.O., Haas C.N., Gurian N.L., Gerba C.P., Panzl B.M., Rose J.B. Application of quantitative microbial risk assessment for selection of microbial reduction targets for hard surface disinfectants. Am. J. Infect. Control. 2014;42:1165–1172. doi: 10.1016/j.ajic.2014.07.024. [DOI] [PubMed] [Google Scholar]
- 43.Wilson A.M., Weir M.H., Bloomfield S.F., Scott E.A., Reynolds K.A. Modeling COVID-19 infection risks for a single hand-to-fomite scenario and potential risk reductions offered by surface disinfection. Am. J. Infect. Control. 2021;49:846–848. doi: 10.1016/j.ajic.2020.11.013. https://doi:10.1016/j.ajic.2020.11.013 Epub 2020 Nov 15. PMID: 33207258; PMCID: PMC7666808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Now Deputy Chief Medical Officer Jenny Harries Says the Evidence that Masks Stop the Spread of Coronavirus Is 'not Very Strong in Either Direction. 2020. https://www.dailymail.co.uk/news/article-8676535/Jenny-Harries-says-face-coverings-evidence-not-strong.html Accessed 5th September 2020. [Google Scholar]
- 45.Edelstein P., Ramakrishnan L. DELVE Addendum MAS-TD1; July 2020. Report on Face Masks for the General Public - an Update.https://rs-delve.github.io/addenda/2020/07/07/masks-update.html [Google Scholar]
- 46.Breaking the Chain of Infection in Our Homes and Everyday Lives: a Practical Approach to Encourage Effective Targeted Hygiene. International Scientific Forum on Home Hygiene; 2022. https://www.ifh-homehygiene.org/online-learning/breaking-chain-infection-our-homes-and-everyday-lives-practical-approach-encourage [Google Scholar]
- 47.The Psychology of Masks: Why Have So Many People Stopped Covering Their Faces? Oct 2021. https://www.theguardian.com/world/2021/oct/26/the-great-cover-up-why-the-uk-stopped-wearing-face-masks [Google Scholar]
- 48.Ackerley L., Buckley C., Paskey A., Cooper S., Slater K., Bainbridge S. American Society for Microbiology Microbe Conference, June 10 2022, Washington D.C. 2022. Targeted Hygiene: a risk-based approach to applying policies and hygiene interventions. [Google Scholar]
- 49.How the development of Targeted Hygiene protocols is helping to create a more hygienic, time-saving and cost-saving Birmingham. Commonwealth Games. 2022 https://fmuk-online.co.uk/features/3157-how-the-development-of-targeted-hygiene-protocols-is-helping-to-create-a-more-hygienic-time-saving-and-cost-saving-birmingham-2022-commonwealth-games [Google Scholar]
- 50.Fauci A.S. Infectious diseases: considerations for the 21st century. Clin. Infect. Dis. 2001;32:675. doi: 10.1086/319235. [DOI] [PubMed] [Google Scholar]