Positive pressure ventilation gained widespread clinical acceptance during the Danish polio epidemic of 1952,1 when it dramatically reduced the mortality of respiratory failure, and it has saved countless lives in ensuing years by enabling modern critical care and the safe practice of surgery under general anesthesia. Nonetheless, evidence emerged in the 1970s that positive pressure ventilation can itself cause lung injury.2 Since then, two fundamental facts have been established. First, large tidal lung excursions are detrimental if they lead to end-inspiratory overdistension and/or cyclical alveolar or bronchiolar derecruitment–recruitment between breaths. Second, the lungs of patients during general anesthesia or with acute respiratory distress syndrome are functionally smaller: functional residual capacity is reduced because some of the airspaces become atelectatic, consolidated, or flooded with edema. A corollary of these facts has been the quest to restore the relationship between tidal volume and functional residual capacity either by decreasing the former or increasing the latter. This concept represents the physiologic underpinning of all “protective” ventilation strategies.
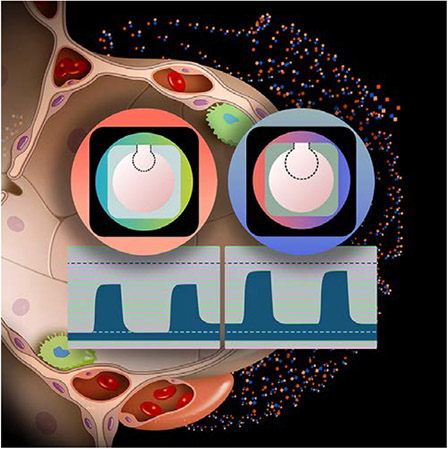
Such framework is helpful to analyze the study by Turan and colleagues3 in this issue of Anesthesiology. In this large factorial crossover cluster trial, adults undergoing orthopedic surgery during general anesthesia (approximately 50% also with regional block and slightly more than 50% undergoing arthroplasty) were allocated to two levels of tidal volume (6 and 10 ml/kg of predicted body weight) and of positive end-expiratory pressure (PEEP, 5 and 8 cm H2O). Presumably, ventilation with lower tidal volume and higher PEEP could lead to better postoperative oxygenation and lower incidence of respiratory complications, because such a strategy would limit both end-inspiratory overdistension and end-expiratory derecruitment, the two biophysical triggers of ventilator-induced lung injury. The results instead show no meaningful clinical or statistical difference among the four studied groups in oxygenation within the first postoperative hour, oxygenation later on the ward, frequency of postoperative pulmonary complications, or duration of hospitalization.
“When is protective intraoperative ventilation most beneficial?”
It is important to note that the authors did not use excessively high or low tidal volumes4,5 and PEEP, but instead values considered acceptable in current clinical practice.4-6 Accordingly, two main inferences can be drawn. First, in a cohort of patients with a low prevalence of lung disease and borderline obesity undergoing nonabdominal surgery of moderate duration (about 3.5 h) and without major physiologic impact (e.g., blood loss), low tidal volumes as well as higher acceptable tidal volumes (10 ml/kg)4,5 with higher PEEP were well tolerated. It is interesting that a tidal volume of 6 ml/kg did not result in lower oxygenation even at the lower PEEP, given that atelectasis is usually considered the main downside of low tidal volume. These results suggest that relatively healthy lungs in the studied conditions can withstand a few hours of low tidal volume ventilation during nonabdominal surgery without developing significant atelectasis even at low PEEP. Higher PEEP and tidal volume did not seem to compromise postoperative lung function either. Second, these results release the cognitive anchor to a single optimal PEEP or tidal volume, at least in this patient population, and instead portray a range of equally acceptable values, consistent with a range—not merely a point—of maximal compliance in the pressure–volume curve of a healthy lung. This message is important because it argues against the transposition without qualification of inferences and values derived from critical care studies to the operating room.
So, is intraoperative protective ventilation all fiction? Substantive observational evidence has identified tidal volume as a risk factor for postoperative pulmonary complications after general anesthesia.7,8 These studies indicated that “protective” ventilation (generally defined as lower tidal volume plus PEEP and/or recruitment maneuvers) may reduce such complications4,8 that are associated with increased mortality, intensive care unit admission, and length of stay.7 The Intraoperative Protective Ventilation (IMPROVE) trial confirmed a marked beneficial effect of protective ventilation on major abdominal surgery.6
Yet, as with Turan’s trial, several trials on protective ventilation did not demonstrate a difference between groups.5,9,10 What could explain these inconsistencies, and when is protective intraoperative ventilation most beneficial? It has been increasingly recognized that the ratio of tidal volume to end-expiratory lung volume, proportional to the driving pressure and a surrogate for lung strain, is the biophysical mediator of the effects of tidal volume and PEEP on ventilator-induced lung injury.4 In fact, the potential of different tidal volumes to reduce postoperative pulmonary complications depends on the patient’s respiratory compliance.11 This physiologic individuality may be a reason for discrepancies. Patient population is another factor. The IMPROVE trial targeted a high-risk population for pulmonary complications6 (major open abdominal surgery, pre-existent respiratory risk factors), whereas Turan and colleagues studied a population at lower risk3 based on the Assess Respiratory Risk in Surgical Patients in Catalonia risk score.12 There is evidence that pulmonary outcomes are less likely to depend on PEEP in nonabdominal/noncardiothoracic surgery, e.g., neurologic versus abdominal surgery.13 This also implies that Turan’s results should not be extrapolated to abdominal or cardiothoracic surgery, when additional injury mechanisms are present and, consequently, the effects of different ventilatory settings could be more evident.13 Time may also be an important variable. Normal lungs show only limited inflammation after 2 h of ventilation even at high driving pressures.14 Sixteen to 24 h were necessary for a significant pulmonary inflammatory response and mechanical deterioration to develop in experiments applying clinical tidal volumes (6 to 8 ml/kg) in initially uninjured lungs.15-17 Finally, the separation between ventilator settings is relevant. The IMPROVE trial acted on multiple variables (tidal volume, PEEP, recruitment maneuvers) setting them apart enough (tidal volumes of 6 to 8 ml/kg with PEEP = 6 to 8 cm H2O versus 10 to 12 ml/kg with PEEP = 0 cm H20) that, presumably, the effect could be detected in contrast to current practice used by Turan and colleagues.3
If there is a range of equally acceptable values for ventilatory settings, it may be hard to show an effect, especially when clinical practice has already converged toward such a range. Turan and colleagues studied a large population and observed a smaller SD for the primary outcome than that initially presumed, which ultimately yielded a high power to detect the predefined mean effect. The 97.5% CIs for the effect estimates were a time-weighted average Spo2/Fio2 of −0.4 to 7.3% for tidal volume and −4.0 to 3.6% for PEEP, numbers that convincingly demonstrate comparable postoperative oxygenation in the studied groups. These results also imply that, although previous clinical studies documented the presence of an effect, they did not necessarily provide the best or single setting of the variable of interest to achieve that effect.
The hemodynamic impact of mechanical ventilation is frequently a concern. A clinically meaningful finding by Turan and colleagues3 in this regard was the similar intraoperative use of vasopressors and incidence of hypotension in all combinations of PEEP and tidal volume. This finding reinforces the concept that the mild-to-moderate range of ventilatory settings explored does not usually result in major hemodynamic effects.
The study opens several questions. Many patients were excluded by anesthesiologists, or due to comorbidities, instability, or other reasons. Such subset of potentially higher-risk patients could represent those patients who would most benefit from specific ventilatory interventions. Although the primary outcome of Spo2/Fio2 in the first hour is a sensitive marker of oxygenation impairment, it could be affected predominantly by factors other than ventilatory settings. The absence of differences in the ward reinforces that any influence of intraoperative settings on postoperative oxygenation was unlikely. Also, even if there was an intraoperative effect of the interventions, this could be lost at extubation, without subsequent benefit. Finally, the reported rate of pulmonary complications was quite low, implying a low-risk group and the potential risk for false negatives, given that the occurrence of those complications derived from registry and billing data not from prospective collection.
Such limitations will deserve future exploration to advance this relevant area. For now, Turan and colleagues provide evidence that mild-to-moderate differences in key ventilator settings—tidal volume and PEEP—within currently accepted ranges do not result in substantial differential effects on postoperative oxygenation and other pulmonary outcomes during orthopedic surgery. Mechanical ventilation in the operating room requires its own specific set of knowledge, with ranges different from those of patients with acute respiratory distress syndrome in intensive care units. Protective ventilation is not defined by single arbitrary numbers, but by ranges of ventilatory settings that likely differ in distinct conditions and in relation to patient-specific physiopathologic features.
Research Support
Dr. Vidal Melo was supported by National Institutes of Health-National Heart, Lung, and Blood Institute (Bethesda, Maryland) grants UH3HL140177 and R01HL121228.
Footnotes
Competing Interests
The authors declare no competing interests.
Contributor Information
Guido Musch, Department of Anesthesiology and Perioperative Medicine, UMass Chan Medical School, Worcester, Massachusetts.
Marcos F. Vidal Melo, Department of Anesthesiology, Columbia University Irving Medical Center, New York, New York.
References
- 1.Ibsen B: The anaesthetist’s viewpoint on the treatment of respiratory complications in poliomyelitis during the epidemic in Copenhagen, 1952. Proc R Soc Med 1954; 47:72–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Webb HH, Tierney DF: Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 1974; 110:556–65 [DOI] [PubMed] [Google Scholar]
- 3.Turan A, Esa WAS, Rivas E, Wang J, Bakal O, Stamper S, Farag E, Maheswari K, Mao G, Ruetzler K, Sessler DI; Ventilation-PEEP Trial Group: Tidal volume and positive end-expiratory pressure and postoperative hypoxemia during general anesthesia: A single-center multiple crossover factorial cluster trial. Anesthesiology 2022; 137:406–17 [DOI] [PubMed] [Google Scholar]
- 4.Ladha K, Vidal Melo MF, McLean DJ, Wanderer JP, Grabitz SD, Kurth T, Eikermann M: Intraoperative protective mechanical ventilation and risk of postoperative respiratory complications: hospital based registry study. BMJ 2015; 351:h3646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karalapillai D, Weinberg L, Peyton P, Ellard L, Hu R, Pearce B, Tan CO, Story D, O’Donnell M, Hamilton P, Oughton C, Galtieri J, Wilson A, Serpa Neto A, Eastwood G, Bellomo R, Jones DA: Effect of intraoperative low tidal volume vs conventional tidal volume on postoperative pulmonary complications in patients undergoing major surgery: A randomized clinical trial. JAMA 2020; 324:848–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, LefTant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S; IMPROVE Study Group: A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013; 369:428–37 [DOI] [PubMed] [Google Scholar]
- 7.Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Martinez Ruiz R, Lee JW, Henderson WG, Moss A, Mehdiratta N, Colwell MM, Bartels K, Kolodzie K, Giquel J, Vidal Melo MF: Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery: A multicenter study by the Perioperative Research Network Investigators. JAMA Surg 2017; 152:157–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Serpa Neto A, Hemmes SN, Barbas CS, Beiderlinden M, Biehl M, Binnekade JM, Canet J, Fernandez-Bustamante A, Futier E, Gajic O, Hedenstierna G, Hollmann MW, Jaber S, Kozian A, Licker M, Lin WQ, Maslow AD, Memtsoudis SG, Reis Miranda D, Moine P, Ng T, Paparella D, Putensen C, Ranieri M, Scavonetto F, Schilling T, Schmid W, Selmo G, Severgnini P, Sprung J, Sundar S, Talmor D, Treschan T, Unzueta C, Weingarten TN, Wolthuis EK, Wrigge H, Gama de Abreu M, Pelosi P, Schultz MJ; PROVE Network Investigators: Protective versus conventional ventilation for surgery: A systematic review and individual patient data meta-analysis. Anesthesiology 2015; 123:66–78 [DOI] [PubMed] [Google Scholar]
- 9.PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology, Hemmes SN, Gama de Abreu M, Pelosi P, Schultz MJ: High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet 2014; 384:495–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lagier D, Fischer F, Fornier W, Huynh TM, Cholley B, Guinard B, Heger B, Quintana G, Villacorta J, Gaillat F, Gomert R, Degirmenci S, Colson P, Lalande M, Benkouiten S, Minh TH, Pozzi M, Collart F, Latremouille C, Vidal Melo MF, Velly LJ, Jaber S, Fellahi JL, Baumstarck K, Guidon C; PROVECS Study Group: Effect of open-lung vs conventional perioperative ventilation strategies on postoperative pulmonary complications after on-pump cardiac surgery: the PROVECS randomized clinical trial. Intensive Care Med 2019; 45:1401–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suleiman A, Costa E, Santer P, Tartler TM, Wachtendorf LJ, Teja B, Chen G, Baedorf-Kassis E, Nagrebetsky A, Vidal Melo MF, Eikermann M, Schaefer MS: Association between intraoperative tidal volume and postoperative respiratory complications is dependent on respiratory elastance: A retrospective, multicentre cohort study. Br J Anaesth 2022; 129:263–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, Sabaté S, Mazo V, Briones Z, Sanchis J; ARISCAT Group: Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 2010; 113:1338–50 [DOI] [PubMed] [Google Scholar]
- 13.de Jong MAC, Ladha KS, Vidal Melo MF, Staehr-Rye AK, Bittner EA, Kurth T, Eikermann M: Differential effects of intraoperative positive end-expiratory pressure (PEEP) on respiratory outcome in major abdominal surgery versus craniotomy. Ann Surg 2016; 264:362–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costa EL, Musch G, Winkler T, Schroeder T, Harris RS, Jones HA, Venegas JG, Vidal Melo MF: Mild endotoxemia during mechanical ventilation produces spatially heterogeneous pulmonary neutrophilic inflammation in sheep. Anesthesiology 2010; 112:658–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tucci MR, Costa EL, Wellman TJ, Musch G, Winkler T, Harris RS, Venegas JG, Amato MB, Melo MF: Regional lung derecruitment and inflammation during 16 hours of mechanical ventilation in supine healthy sheep. Anesthesiology 2013; 119:156–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szabari MV, Takahashi K, Feng Y, Locascio JJ, Chao W, Carter EA, Vidal Melo MF, Musch G: Relation between respiratory mechanics, inflammation, and survival in experimental mechanical ventilation. Am J Respir Cell Mol Biol 2019; 60:179–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Motta-Ribeiro GC, Hashimoto S, Winkler T, Baron RM, Grogg K, Paula LFSC, Santos A, Zeng C, Hibbert K, Harris RS, Bajwa E, Melo MFV: Deterioration of regional lung strain and inflammation during early lung injury. Am J Respir Crit Care Med 2018; 198:891–902. 10.1164/rccm.201710-2038OC [DOI] [PMC free article] [PubMed] [Google Scholar]


