Background
Energy-based treatments include ultrasound, lasers, cryolipolysis, and radiofrequency. The most recent energy treatment for noninvasive body contouring is electromagnetic treatments—a hot topic in plastic surgery today. A systematic review to assess efficacy and safety has not been published.
Methods
An electronic search was performed using PubMed to identify the literature describing electromagnetic treatments. Measurements from imaging studies were tabulated and compared.
Results
Fourteen clinical studies were evaluated. Two studies included simultaneous radiofrequency treatments. In 11 studies, the Emsculpt device was used; in 2 studies, the Emsculpt-Neo device was used. One study included a sham group of patients. The usual protocol was 4 treatments given over a 2-week period. No complications were reported. Eight studies included abdominal measurement data obtained using magnetic resonance imaging, computed tomography, or ultrasound. Photographic results were typically modest. Photographs showing more dramatic results also showed unexplained reductions in untreated areas.
Measurement variances were high. The mean reduction in fat thickness was 5.5 mm. The mean increment in muscle thickness was 2.2 mm. The mean decrease in muscle separation was 2.9 mm (P = 0.19). Early posttreatment ultrasound images in 1 study showed an echolucent muscle layer, compared with a more echodense layer at the baseline, consistent with tissue swelling after exercise. Almost all studies were authored by medical advisors for the device manufacturer.
Discussion
Measurement data show small reductions in fat thickness, occurring almost immediately after the treatments. Adipocyte removal without tissue swelling would be unique among energy-based treatments. Similarly, muscle hypertrophy is not known to occur acutely after exercise; muscle swelling likely accounts for an early increment in muscle thickness. Any improvement in the diastasis recti is likely fictitious.
Conclusions
Electromagnetic treatments, either administered alone or in combination with radiofrequency, are safe. However, the evidence for efficacy is tenuous. Measured treatment effects are very small (<5 mm). Conflict of interest and publication bias are major factors in studies evaluating energy-based alternatives. The evidence-based physician may not be satisfied that an equivocal treatment benefit justifies the time and expense for patients.
Key Words: electromagnetic, high-intensity focused, electromagnetic muscle stimulation, radiofrequency, MRI, CT, ultrasound, systematic review, HIFEM, Emsculpt, Emsculpt-Neo, BTL
Over the last 2 decades, numerous energy-based treatments have been introduced to provide nonsurgical fat reduction. These methods include laser treatments, ultrasound, cryolipolysis, and radiofrequency. The newest energy-based modality is electromagnetic treatments. Electromagnetic muscle stimulation has been used for decades in physical therapy1 and to treat incontinence by strengthening the pelvic muscles.2 Electromagnetic fields have also been used to reduce postoperative pain and edema after plastic surgery,3,4 although the science is limited.3
The popular acronym for electromagnetic treatments applied to body contouring is HIFEM—high-intensity focused electromagnetic treatments. This method was first adapted for body contouring in 20185 and has quickly become a hot topic in plastic surgery. A 2022 publication evaluating combined HIFEM and radiofrequency6 is one of the most viewed articles in plastic surgery, with an extraordinary altmetric score of 307. This publication has been picked up by 41 news outlets. It is ranked 25th, at the 99th percentile for tracked articles of a similar age in all journals.7
Electromagnetic treatments were cleared by the US Food and Drug Administration (FDA) in 2017 for strengthening, firming, and toning the abdomen, buttocks, thighs, arms, and calves.8 In 2019, the Emsculpt device (BTL Industries, Boston, Mass) received 510(k) clearance for noninvasive lipolysis of the abdomen.9
A circular magnetic coil positioned over the body produces rapidly alternating magnetic fields that induce an electric current in the underlying tissue.10–13 Unlike radiofrequency, the energy does not cause thermal effects.8 This electric current stimulates motor neurons to cause involuntary “supramaximal” muscle contractions.5,8,11–14 Almost 20,000 pulses are delivered in a 30-minute treatment session.15–17 The rectus abdominis, internal oblique, and external oblique muscles are targeted.17 Muscle stimulation is intended to produce muscle hypertrophy without the need for exercise.5,8,14
Muscle stimulation is also believed to create a hypermetabolic state, causing local lipolysis.5,6,8,10,11,15,18–20 It is hypothesized that fat cells are overwhelmed by the metabolic reaction, becoming dysfunctional and initiating programmed death, called apoptosis.8
Publications have evaluated only 1 device in the United States, Emsculpt. This device has been modified, adding radiofrequency to the electromagnetic field treatment,6 marketed as Emsculpt-Neo.21 Radiofrequency is intended to augment both lipolysis and muscle stimulation, and deliver “less fat, more muscle.”21 Once the device is strapped on, it can be run independently, making it “an economical choice” for aesthetic practices.8 Some authors believe that the device delivers a muscle antiaging effect.12 Kilmer et al22 instruct patients to return every 1 to 3 months for electromagnetic treatments to maintain firmer, more toned results.
A systematic review of electromagnetic treatments in body contouring has not been published. This review was undertaken to evaluate the efficacy and safety of this new treatment.
METHODS
An electronic literature review was conducted to identify publications that evaluate aesthetic applications of electromagnetic treatments. The search terms “high-intensity focused electromagnetic” and “electromagnetic muscle stimulation” were entered. The search included all articles published in English starting in 2018, the year of the original publication,5 and continuing to July 2022. Only studies that included body contouring applications were included. Research conducted in animals, review articles, and studies of other applications such as physical therapy or the treatment of urinary incontinence were excluded. Publications that also included simultaneous radiofrequency were included.6,13 One study of only 2 patients was not included.23 A second retrospective study24 of the same 22 patients evaluated by computed tomography (CT) previously25 was not included. A t test was used to compare means, using published means and standard deviations where available. A P value of less than 0.05 was considered significant.
RESULTS
Fourteen studies evaluating electromagnetic treatments were identified (Table 1).5,6,10–16,19,20,22,25,26 In 11 studies, the Emsculpt device was used.5,10–12,14,15,19,20,22,25,26 In 2 studies, the Emsculpt-Neo device was used.6,13 One study used a device manufactured in Italy.16 The mean sample size was 26, with a range of 7 to 71. There were no controlled studies. One study included a sham group of 16 patients treated at very low–energy settings.6
TABLE 1.
Published Studies of Electromagnetic Body Contouring Treatments
| # | Study (Year) | No. Patients | Device | No. Treatments, Times | Follow-up | Area | Complications | Measuring Device | Financial Conflict |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Jacob and Paskova (2018) | 19 | Emsculpt (BTL, Boston, Mass) | 4, 30 min | After the fourth treatment, 3 mo | Abdomen | None | Photographic evaluation, waist circumferences, Likert scale questionnaires | C.I.J. is a medical advisor for BTL. |
| 2 | Jacob et al (2018) | 71 | Emsculpt | 4, 30 min | After the fourth treatment, 1 mo | Buttocks | None | 7-point Likert scale, visual analog scale for discomfort | C.J. and B.K. are medical advisors; M.B. and S.C. are speakers for BTL. |
| 3 | Kinney and Lozanova (2019) | 22 | Emsculpt | 4, 30 min | 2 mo, 6 mo | Abdomen | None | MRI, waist circumference | B.K. is a medical advisor for BTL. |
| 4 | Katz et al (2019) | 33 | Emsculpt | 4, 30 min | 1 mo, 3 mo | Abdomen | None | Ultrasound, 5-point Likert scale, visual analog scale for discomfort | B.K. is a medical advisor for BTL. |
| 5 | Kent and Jacob (2019) | 22 | Emsculpt | 8, 30 min | 1 mo | Abdomen | None | CT, waist circumference | D.K. and C.J. are medical advisors for BTL. |
| 6 | Kinney and Kent (2020) | 21 | Emsculpt | 4–8, 30 min | 231–509 d | Abdomen | None | MRI or CT | B.M.K. and D.E.K. are medical advisors for BTL. |
| 7 | Jacob and Rank (2020) | 10 | Emsculpt | 4, 30 min | 1 mo, 3 mo, 6 mo | Abdomen | None | MRI, 7-point visual analog scale for discomfort | C.I.J. is a speaker for BTL. |
| 8 | Kilmer et al (2020) | 20 | Emsculpt | 4, 30 min | 12 wk | Abdomen | None | Photographic evaluation, patient surveys, abdominal circumference | All authors are advisory board members, consulting medical director, or employees of Allergan. |
| 9 | Jacob et al (2021) | 40 | Emsculpt-Neo | 3, 30 min | 1 mo, 3 mo, 6 mo | Abdomen | None | MRI, waist circumference, Likert scales, visual analog scale for discomfort | None reported. C.I.J. is listed as a speaker and medical advisor for BTL in other studies. |
| 10 | Palm (2021) | 7 | Emsculpt | 4, 30 min | 1 mo, 3 mo | Buttocks | None | MRI, 5-point Likert scale questionnaires | M.P. received financial support and serves on the medical board of BTL. |
| 11 | Katz and Duncan (2021) | 20 | Emsculpt | 4, 20 min | 1 mo, 3 mo, 6 mo | Arms and calves | None | Ultrasound, patient questionnaires | B.K. and D.D. are medical advisors for BTL. |
| 12 | Leone et al (2021) | 15 | Flat magnetic stimulation (Schwarzy, Italy) | 6–8, 20–45 min | 1 mo | Abdomen | None | Skinfold thickness, waist circumference, ultrasound | None reported. |
| 13 | Giesse (2021) | 14 | Emsculpt | 4, 30 min | After the fourth treatment, 2 mo | Abdomen and buttocks | None | Ultrasound, waist circumference, photographic evaluation, visual analog scale | S.G. is a speaker for BTL. |
| 14 | Samuels et al (2022) | 56 | Emsculpt-Neo | 3, 30 min | 1 mo, 3 mo, 6 mo | Abdomen | None | Ultrasound, 5-point Likert scale, visual analog scale | All authors are BTL medical advisors. |
CT, computed tomography; MRI, magnetic resonance imaging.
Most treatment sessions lasted 30 minutes.5,10,13–15,19,20,22,26 Usually, 4 treatments were given over a period of 2 weeks.5,10,14,15,19,20,22,26 (range, 3–8 treatments). Follow-up times ranged from 1 to 6 months, except for 1 study that evaluated patients almost 1 year, on average, after the treatments.11 In 11 studies, the abdomen was treated. In 1 study, the buttocks were also treated.20 One study evaluated treatment of the arms and calves,12 and 2 others evaluated the buttocks alone.14,26
Muscle fatigue and discomfort were common adverse effects that resolved within 12 to 48 hours.5,10,13,15,16,19 Erythema tended to resolve within a few hours.6 No adverse events or complications were reported in any publication. Eleven studies included measurements obtained from imaging. Four studies used magnetic resonance imaging (MRI),13,15,19,26 5 studies used ultrasound,6,10,12,16,20 1 study used CT,25 and 1 follow-up study used either MRI or CT scans.11 All of the studies weighed the patients; none reported a significant overall weight change.
The highest tolerable energy settings were applied.5,6,11,13–16,22 Intensity usually increased during treatment to 90% to 100%.5,10,15,19,20 In a study of combined electromagnetic treatment and radiofrequency,13 radiofrequency intensity was set at 100% at the beginning of the procedure and adjusted to the patients' heat tolerance.
All studies with surveys reported high patient satisfaction.5,6,10,12–14,20,22,26 Photographs typically depicted modest results (Fig. 1).5,10,11,14–16,20,22 By contrast, the sham-controlled study by Samuels et al6 showed a dramatic reduction in the abdominal profile (Fig. 2). There was also a dramatic, but puzzling, reduction in regions outside the abdominal treatment area. Samuels et al6 did not report whether any of the patients underwent other surgical or nonsurgical procedures. The authors reported no overall change in weight among subjects. The subcutaneous fat reduction in this study averaged 4.8 mm. The increase in muscle thickness averaged 2.0 mm. Combining the 2 changes, the mean reduction in overall abdominal thickness was 2.8 mm (1/9 in). The change is much less than the 48.9-mm overall reduction demonstrated in the published photographs (Fig. 2). Another study, from Italy using a different device, showed not only a reduction in the abdomen but also a reduction in the untreated thigh (Fig. 3).16
FIGURE 1.
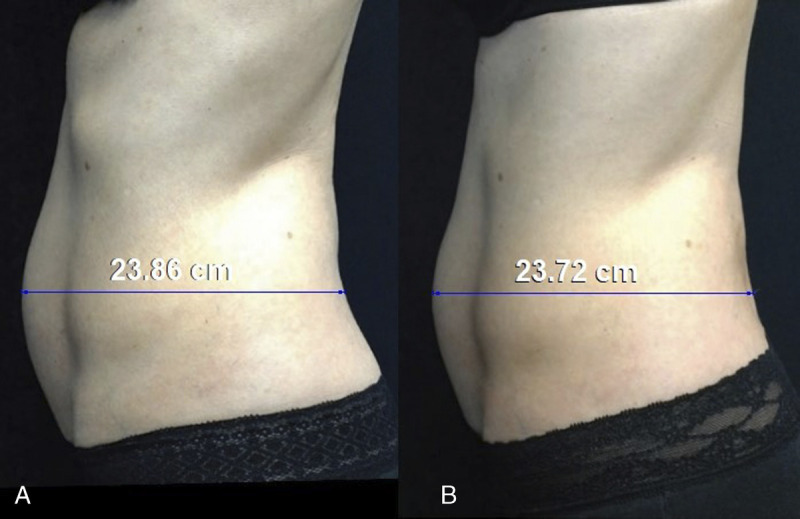
A and B, Lateral photographs of a 37-year-old woman before electromagnetic treatment and 1 year after treatment. The images have been matched for size and orientation (Canfield Scientific, Fairfield, NJ). A 45-mm torso length is used for calibration. The difference in abdominal measurements is negligible. Adapted from Kinney and Kent.1
FIGURE 2.
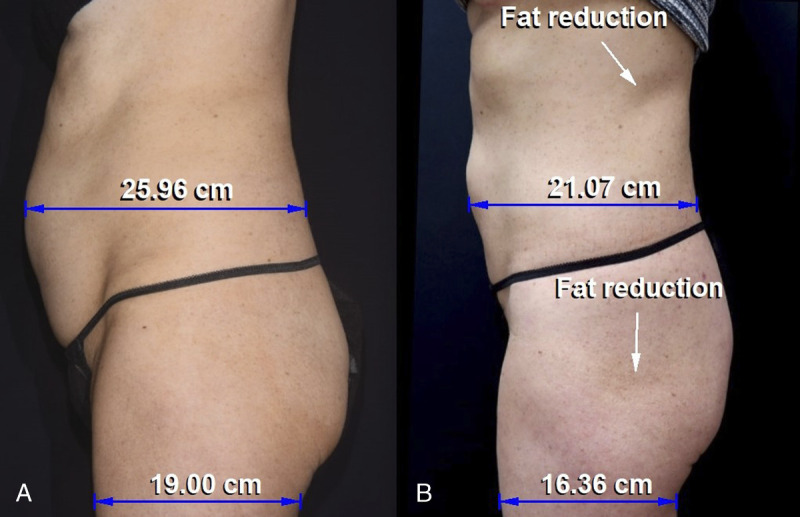
A and B, This patient's baseline image is compared with the 6-month posttreatment image. The images have been matched for size and orientation using the Canfield 7.4.1 imaging software. A mean female torso length of 45 cm is used for calibration. The posttreatment image (B) shows a dramatic reduction in the abdominal profile, extending from the upper abdomen to the pubis. The abdominal projection is reduced by 4.89 cm (18.8%). In addition, there is fatty reduction in the flank and lateral gluteal area, which are outside the abdominal treatment zone. The lateral thigh measurement is also reduced by 2.64 cm (13.9%). Adapted from Samuels et al.6
FIGURE 3.
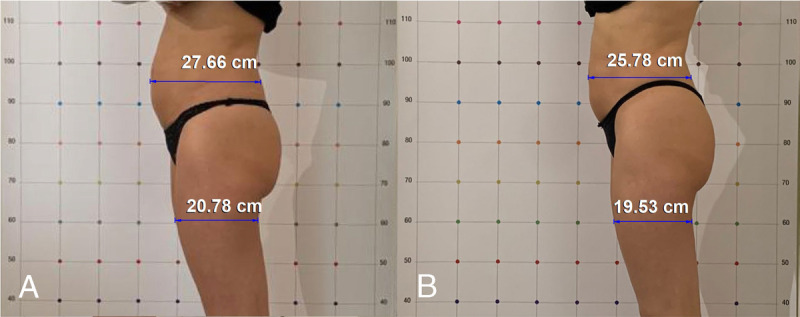
A and B, Lateral photographs of a 50-year-old woman before and 1 month after her last electromagnetic treatment. The authors have used a convenient grid to allow measurements. The abdominal profile is reduced by 1.88 cm (6.8%). The upper thigh, which is outside the treatment area, is reduced by 1.25 cm (6.0%). Adapted from Leone et al.16
Half of the studies included measurements of abdominal circumference.5,13,15,16,20,22,25 The mean reduction in waist circumference was 3.5 cm (range, 0.4–5.9 cm), with a follow-up of 1 to 3 months. The original study using this device for body shaping measured waist circumferences in 19 patients 3 months after the fourth treatment.5 The mean pretreatment waist circumference was 88.0 ± 11 cm, compared with 83.6 ± 11 cm at 3 months, representing a reduction of 4.4 cm. The error bars were wide and overlapping. This large degree of variance reduces the significance of the difference. A t test performed by the author yields a P value of 0.23. The vertical axis in the authors' graphic starts at 70 cm, enhancing the apparent magnitude of the reduction.
Although Jacob and Rank19 reported a decrease in fat thickness in postpartum patients, this reduction is not evident on their published MRI images (Fig. 4). Kinney and Kent11 showed a reduction in abdominal fat thickness in axial CT slices. However, there was a similar reduction in the untreated flanks. Table 2 tabulates measurements from 8 studies that used an imaging method. Variances in individual studies were high. In the original MRI study by Kinney and Lozanova,15 the reduction in fat thickness was 4.3 mm, the increase in muscle thickness was 1.6 mm, and the reduction in muscle separation was 1.7 mm. Although the authors reported significant changes, a t test produces nonsignificant P values for each comparison (0.07, 0.10, and 0.42, respectively). Similar values were reported in a CT study by Kent and Jacob25 (−3.1, +1.5, and −2.0 mm, respectively). Among all studies with imaging measurements, the mean reduction in fat thickness was 5.5 mm (Table 2). The mean increment in muscle thickness was 2.2 mm. The mean decrease in muscle separation was 2.9 mm (1/10 of an inch). The overall mean decrease in muscle separation among the 6 studies reporting measurements6,13,15,16,19,25 was not significant (mean P = 0.19; range, 0.002–0.465).
FIGURE 4.
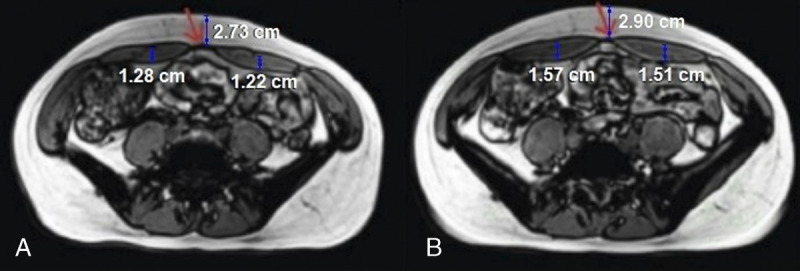
A and B, Magnetic resonance imaging images of a 38-year-old woman are compared before and 3 months after a course of 4 electromagnetic treatments. The abdominal fat thickness is 2 mm greater, and the muscle thickness is 3 mm greater in the posttreatment image (B). The images are taken at slightly different levels, as evidenced by the linea alba partially visible below the red arrow in the before image (A), but not in the after image (B). A 34-cm hip width is used for calibration. Adapted from Jacob and Rank.19
TABLE 2.
Measurement Data From Published Studies of Electromagnetic Treatments of the Abdomen
| # | Study (Year) | No. | Imaging | Baseline Fat Thickness, Mean (SD), mm | 1–3 mo, Mean (SD), mm | Diff., mm | Baseline Muscle Thickness, Mean (SD),* mm | 1–3 mo, Mean (SD), mm | Diff., mm | Baseline Diastasis, Mean (SD), mm | 1–3 mo, Mean (SD), mm | Diff., mm |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Kinney and Lozanova (2019) | 22 | MRI | 23.6 (8.2) |
19.3 (7.6) |
−4.3 | 11.1 (3.1) |
12.7 (3.3) |
+1.6 | 16.6 (7.2) |
14.9 (6.7) |
−1.7 |
| 2 | Katz et al (2019) | 21 | US | 23.72 (8.9) |
18.25 (N.A.) |
−5.47 | ||||||
| 22.96 (9.9) |
15.42 (N.A.) |
−7.54 | ||||||||||
| 3 | Kent and Jacob (2019) | 22 | CT | 18.3 (7.1) |
15.2 (6.5) |
−3.1 | 11.0 (2.1) |
12.5 (2.0) |
+1.5 | 20.1 (9.2) |
18.1 (8.8) |
−2.0 |
| 4 | Kinney and Kent (2020) | 21 | CT | N.A. | N.A. | −3.67 | N.A. | N.A. | +1.89 | N.A. | N.A. | −1.83 |
| 5 | Jacob and Rank (2020) | 10 | MRI | N.A. | N.A. | −2.5 | 9.3 | 11.3 | +2.0 | 22.3 (8.1) |
17.8 (7.2) |
−4.5 |
| 10.0 | 12.2 | +2.2 | 11.6 (4.6) |
8.9 (3.7) |
−2.7 | |||||||
| 6 | Jacob et al (2021) | 40 | MRI | 28.6 (11.8) |
19.9 (8.1) |
−8.7 | 9.2 (2.3) |
11.6 (3.0) |
+2.4 | 16.6 (6.3) |
12.9 (4.9) |
−3.7 |
| 24.2 (11.7) |
16.4 (8.5) |
−7.8 | 8.7 (2.3) |
11.1 (2.7) |
+2.4 | 21.4 (6.3) |
17.4 (5.2) |
−4.0 | ||||
| 7 | Leone et al (2021) | 15 | US | 12 (4) |
11 (4) |
−1.0 | 9.0 (2.0) |
11.0 (1.0) |
+2.0 | 25.0 (4.0) |
22.0 (4.0) |
−3.0 |
| 10.0 (2.0) |
13.0 (2.0) |
+3.0 | ||||||||||
| 8 | Samuels et al (2022) | 40 | US | 26.0 (12) |
19.5 (9.5) |
−6.5 | 9.4 (2.4) |
11.7 (2.5) |
+2.3 | |||
| All studies (2019–2022) | 191 | US, MRI, CT | 22.4 | 16.9 | −5.5 | 9.74 | 11.90 | +2.16 | 19.94 | 17.06 | −2.9 |
*Some studies included measurements above and below the umbilicus.
CT, computed tomography; diff., difference; MRI, magnetic resonance imaging; N.A., not available; US, ultrasound.
The ultrasound scans in 1 study showed a relatively echodense layer before treatment, compared with a more echolucent layer after treatment, possibly representing tissue swelling (Fig. 5).6
FIGURE 5.
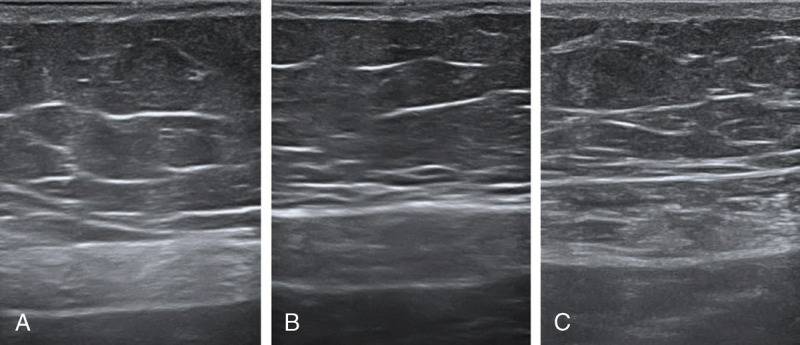
A–C, Ultrasound images before, 1 month after combined electromagnetic/radiofrequency treatments, and 6 months after treatments. The muscle appears thicker and more echolucent in the after images. Reproduced from Samuels et al.6
With 2 exceptions,14,20 the studies reported institutional review board approval, although only 4 studies specified the review board.6,11,12,22 Almost all studies had a known financial conflict, with 1 or more authors reporting that they were medical advisors or speakers for the manufacturer. The only study without a known financial conflict was the Italian study using a different device.12 Long-term results have not been investigated. Only 1 study included patients who were followed over 6 months.11
DISCUSSION
Combining Electromagnetic Treatments and Radiofrequency
Recent investigators hypothesize that a combination of electromagnetic treatments and radiofrequency produces a synergistic reduction in abdominal fat thickness and an increase in abdominal muscle thickness.6,13 Typically, electromagnetic treatment and radiofrequency (electric current) are not compatible energy sources.8 The combined treatment reportedly overcomes the interference between the 2 modalities by using proprietary synchronized radiofrequency electrodes that prevent eddy currents.6,13 Goldberg et al8 believe that the enhanced blood supply provided by radiofrequency heating prepares the muscles for exposure to electromagnetic-induced stress, similar to a warmup before a workout. Samuels et al6 believe that surface warming contributes to muscle hypertrophy under the fat layer.
Radiofrequency is a surface treatment with very limited capability to provide subcutaneous lipolysis. Adipose tissue must be heated to 60°C, well above the threshold for burning the skin (42°C) to produce subcutaneous contraction.27 This limitation prompted the development of subsurface radiofrequency treatments using heat probes, typically performed in combination with liposuction.27,28 Samuels et al6 conclude that the combination treatment exceeds what can be achieved with sequential treatments, based on comparisons with other published studies. This study did not include sequentially treated patients for comparison.
Previous studies using the Emsculpt device without radiofrequency also report fat layer reduction and muscle thickening.10,11,15,16,19,25 Imaging studies using the Emsculpt device without radiofrequency report a 1.84-mm average muscle thickening (range, 1.5–2.2 mm),11,15,19,25 almost identical to the 2.2-mm mean increase (2.0 and 2.4 mm) found in the studies of combined treatments (Table 2).6,13 The difference is minuscule (0.4 mm) and likely within the margin of error. Similarly, a 20.5% reduction in the fat layer6 is almost identical to the 19.6% reduction reported in studies using electromagnetic treatments alone.18
Although the changes expressed as percentages may seem substantial, the change in absolute measurements, measured in millimeters, was very modest. In the sham study,6 the subcutaneous fat reduction averaged 4.8 mm (1/5 of an inch); the increase in muscle thickness averaged 2.0 mm (<1/10 of an inch).5 Combining the 2 changes, the average reduction in overall abdominal thickness would be 2.8 mm (1/9 of an inch). With these small differences, any claim to enhanced results from adding radiofrequency is tenuous.
Graphics and Measurements
Some studies feature graphics with a vertical axis that starts at a measurement greater than zero,5,6 which makes small changes appear larger. In the study by Samuels et al,6 the bottom halves of the wide error bars are missing. If they were included, the error bars at 1 month and baseline for the treatment group would extend to the bottom of the graph. Consequently, there is considerable overlap in the regions contained within the error bars, revealing high measurement variability.
Such variability in measurements is expected. Ultrasound measurements are affected by the amount of pressure applied to the transducer.10 Variability is expected between operators and at different times. Interoperator variability and test-retest reliability are relevant to such comparisons but are not quantitated. Compared with CT and MRI, the tissue layers are less well defined on ultrasound scans (Fig. 5). It is also a challenge to exactly match the measurement sites before and after treatment. Samuels et al6 report that ultrasound measurements were made 2 inches on either side of the umbilicus but do not report right- and left-sided data.
Duplicating the measurement site is a challenge, regardless of the imaging method. Computed tomography and MRI slices are typically spaced 5 mm apart.11 Aligning the level exactly is essential when measuring the thickness and diastasis of the rectus muscles, which vary depending on the vertical level. Small differences in level can be apparent on the published images (Fig. 4). For example, a pretreatment image contains a slice through the vertebral body; the posttreatment slice is through the disk space.13 Differences related to the measurement level may be of greater magnitude than a small treatment effect (ie, a few millimeters). Selection bias must be considered when less than half of enrolled patients return for their postoperative imaging.11 Inclusion rates of 80% or more are needed to ensure that results are representative of the group as a whole.29
Although ultrasound devices are now common in plastic surgery offices, CT and MRI are not. These modalities have their own disadvantages. One is cost. None of the authors report the funding source for these examinations, which is presumably the manufacturer. It is not clear whether patients are reimbursed for their time and inconvenience. Only 1 study commented on financial incentives; patients were not financially incentivized for participating in the MRI study.15 Remarkably, all 22 patients completed the study. Repeated radiation exposure from CT scans might be expected to be a problem for institutional review board approval, especially when alternatives that do not include ionizing radiation (ultrasound and MRI) are available.
Study Design
A sham study would seem to be ideal for evaluating this treatment. In their recent publication, Samuels et al6 describe a single-blind study design but do not specify whether the investigators or participants were masked, although the clinical trial registry suggests that the investigator was masked.30 Typically, in a single-blind study design, the researchers know which patients received the sham treatments and whether measurements are pretreatment or posttreatment. The authors do not report whether the radiologist reading the scans was masked. Lack of masking undermines the value of a sham procedure by allowing confirmation bias.31
Samuels et al6 report that their patients were randomized but do not describe the randomization method, which assigned patients in a 2:1 ratio. Practical difficulties are encountered when attempting to randomize elective cosmetic patients.31 Few patients presenting for body contouring treatments are likely to be willing to submit to randomization,31 knowing that they may be wasting their time and not accomplishing their goal if they are allotted to the sham group, especially without a financial incentive. Sham patients, and operators, are likely to suspect that they received low-intensity (5%)6,30 treatments simply by observing the low magnitude and discomfort of their muscle contractions.
Samuels et al6 do not report their energy settings but do state that the treatment intensities, both heat and electromagnetic stimulation, were adjusted to the maximum tolerable level.6,30 Maximally tolerable energies would presumably cause considerable discomfort for patients while their abdominal muscles are electrically stimulated to contract, yet the discomfort scores averaged only 2.9 on a 0-to-10 visual analog scale.6 Other studies report even lower mean pain scores (1.05–2.3).10,13,14 Patient surveys are known to be subjective.11 Interestingly, 40% of the sham patients reported that they were satisfied, and 31.6% reported an improvement in both the fat layer and muscle,6 attesting to the subjectivity of patient surveys.
Proposed Mechanism
The scientific basis for efficacy is controversial.17 The mechanism for electromagnetically induced fat reduction is speculative and extrapolated from a 2007 Danish exercise physiology study.32 The theory is that vigorous muscle contractions lead to hypertrophy, plus a reduction of local fat by increased metabolism.18 These Danish subjects were not treated with an energy-based device. The abdominal muscles and adipose layer were not measured. Not surprisingly, volunteer men exercising their lower extremities experienced increased blood flow and a 1°C temperature increase in the exercising thigh muscles.32 This increased blood flow is believed to overlap to the adjacent adipose tissue, exposing this fatty tissue to higher levels of circulating epinephrine.32 Stallknecht et al32 speculate that paracrine factors, such as interleukin 6, may be released from the contracting muscles, diffuse into local tissues, and produce “spot lipolysis.” A problem with this theory is that circulating catecholamines influence all adipose tissue deposits in the body, not just adipose tissue adjacent to contracting muscles.32 Direct norepinephrine-mediated sympathetic innervation may also stimulate lipolysis.32 However, it is not clear that increased lipolysis leads to local apoptosis or lipocyte death. Changes in the subcutaneous fat thickness were not evaluated in the referenced 2007 study.32 If local adipose tissue loss occurred secondary to intense adjacent muscle activity, permanent fat atrophy might be expected in the limbs and torsos of athletes. Such a phenomenon (fortunately) has not been observed. A mechanism for reduction of visceral fat24 is unclear.
A porcine model suggests that fat cell apoptosis occurs after electromagnetic muscle stimulation.33 Until recently, no studies had evaluated this possibility in humans. In 2021, Zachary et al34 reported a unique study in human subjects undergoing abdominoplasty 3 to 17 days after their energy-based treatments.
Hematoxylin and eosin staining can reveal an inflammatory response but does not distinguish living and dead adipocytes. Inflammatory cells are recruited for digestion and clearance of expired adipocytes. Perilipin staining is a standard method of assessing adipocyte viability. In the study by Zachary et al,34 6 patients were treated with Emsculpt and 3 patients were treated with cryolipolysis. One control tissue sample and 1 treated tissue sample were obtained from each subject. Subcutaneous fat harvested from the treated areas was subdivided into superficial and deep specimens, to assess fat viability immediately adjacent to the muscle. None of the electromagnetic muscle stimulation samples, from both superficial and deep fat layers, and at all time points (3, 11, and 17 days post treatment), showed signs of an inflammatory response or loss of perilipin staining, similar to controls. By contrast, the patients who were treated with cryolipolysis demonstrated an inflammatory response in the fat layer and loss of perilipin, indicating irreversible fat cell injury. Despite replicating the sophisticated study methods for the porcine study,33 the authors were unable to reproduce results showing apoptosis after electromagnetic treatments. The authors recommend more basic science research. Goldberg35 reported that adipocytes were flattened and reduced in size after electromagnetic treatment combined with radiofrequency. However, the study did not report evidence of apoptosis or inflammation associated with lipolysis.
Some studies reported a reduction in the fat layer immediately after a 2-week course of 4 treatments.5,20 All of the studies using imaging modalities reported a fat layer reduction and muscle thickening 1 month after treatment (Table 2).6,10,13,16,19,20,25 The mechanism for such a quick reduction in the fat layer is unclear. Other energy-based treatments such as radiofrequency, cryolipolysis, and ultrasound are followed by a protracted period of swelling, often lasting several months, caused by inflammation.28,36,37
Proponents of electromagnetic treatments suggest that muscle hypertrophy accounts for an early increase in muscle thickness.6,11,13,15,16,19,25 However, such a mechanism is not supported by the exercise physiology literature.38–41 In untrained subjects, muscle hypertrophy is virtually nonexistent during the initial stages of resistance training, with most of strength gains resulting from neural adaptations.38–40 Increases in muscle cross-sectional area of approximately 10% to 15% require at least 10 to 14 weeks of dynamic heavy resistance training.40,41 Muscle contractions are believed to cause muscle fiber microinjury, the stimulus for muscle hypertrophy.8,18,38,40 Muscle hypertrophy is not known to occur after only 2 weeks of vigorous muscle activity. Early increase in muscle thickness after a workout, “the muscle pump,” is caused by cellular edema, not muscle hypertrophy.38 It is more likely that the acute reaction to supramaximal muscle contractions is temporary swelling. The 1-month and 3-month ultrasound images show an echolucent muscle layer, compared with a more echodense layer at the baseline (Fig. 5).6 This change is consistent with tissue edema.
Even if early muscle hypertrophy occurs, the clinical usefulness of a 2.2-mm (<1/10 of an inch) thicker muscle in the abdomen is questionable, particularly if the muscles remain hidden under a layer of fat.11 A slight increase in muscle thickness is not synonymous with improved muscle definition. Some investigators recommend limiting the treatment to patients with less than 2.5 cm of pinchable subcutaneous fat.11,15,17,42
Results of this energy treatment are generally considered inferior to liposuction.11,16,42 Some authors conclude that patients with body mass indices < 25 kg/m2 are ideal candidates for this energy treatments,20,42 but not liposuction.5,20 On the contrary, nonobese patients make excellent candidates for liposuction. Magnetic resonance images show a 45% mean reduction in the fat layer after liposuction (Fig. 6).37 Liposuction allows 3-dimensional body contouring, treating confluent areas of the lower body (eg, the flanks along with the abdomen). One sponsored position paper concludes that adding radiofrequency can widen the patient base to include obese patients with body mass indices up to 35 kg/m2. Unlike liposuction, noninvasive energy-based treatments such as cryolipolysis and electromagnetic treatments are limited to spot treatments.
FIGURE 6.
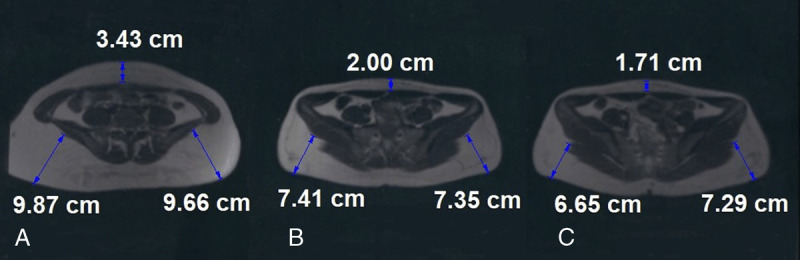
A–C, Axial magnetic resonance imaging images of a 24-year-old woman before, 3 months, and 6 months after liposuction of the lower body. The subcutaneous fat appears white in these T1-weighted images. The abdominal fat thickness is reduced by 50%.
Muscle hyperplasia has been proposed, based on preliminary porcine studies.43,44 However, the change in the number of muscle fibers per slice in treated animals was not statistically significant.43 Evidence that hyperplasia occurs in human subjects is lacking.38 No explanation has been offered for a nonsurgical correction of a rectus diastasis. Not surprisingly, the overall measurement difference among the studies was not significant (P = 0.19). Kent and Jacob,25 in comparing their results with other studies,10,15 concluded that no additional benefit in fat reduction or muscle thickening was obtained from extra treatments, beyond the usual course of 4 treatments. The lack of a dose response (ie, more treatments do not produce greater changes)11,25 is inconsistent with treatment efficacy.
Absence of complications is unique among energy treatments. None of the studies report temporary swelling or nodularity, which contrasts with other energy-based treatments such as ultrasound, cryolipolysis, and radiofrequency treatments.28,36,37 Swelling would be expected from lipolysis, especially without liposuction.
510(k) Clearance
The BTL-899 device received FDA 510(k) clearance for lipolysis and reduction of the fat layer9 based on clinical trials45,46 conducted by a Bulgarian dermatologist and sponsored by BTL. Evidence of lipolysis was based on histological signs of fat cell disruption in biopsies of abdominal tissue.45 Although the histological and clinical studies are listed as completed, no findings are reported on the clinical trial website.45,46 The studies cannot be found among publications listed on the PubMed website.
Terminology
Terminology merits comment. This technology has received FDA clearance for muscle toning.8 The device is marketed to improve muscle tone.8,12–14,16,22,23 Muscle tone is defined as the internal state of muscle-fiber tension within individual muscles and muscle groups or the degree of muscle tension or resistance during rest or in response to stretching.47 There is no evidence that electromagnetic treatments affect these muscle properties.
The acronym “HIFEM” includes the words “high intensity.” All energy treatments have a range of intensities, from low to high, and this treatment is no different. One could just as easily speak of high-intensity radiofrequency or high-intensity ultrasound. The word “focused” suggests that the energy is directed at a specific site, like a camera lens, or stereotactic surgery. However, none of the studies identify a specific subcutaneous level that receives the directed energy. The electromagnetic field is believed to penetrate to a depth of 7 cm,10,15 although no study confirming this tissue penetration is referenced. An alternative label is electromagnetic muscle stimulation.22,34
A recent review and position paper, published by authors who were compensated by BTL for their contributions, referenced experienced physicians and the number of recent publications as evidence supporting the value of this new treatment.8 These are not evidence-based considerations.29 Evidence-based medicine (refreshingly) puts little value on first principles, expert opinion, consensus statements, or the number of publications supporting a treatment. It is concerned solely with the factual basis for efficacy.29
Photographic Integrity
The recent study by Samuels et al6 is designated a hot topic and is accompanied by a highly favorable press release. The photographs show an extraordinary result (Fig. 2).
Plastic surgeons rely on photographs when evaluating plastic surgery innovations. Therefore, their integrity is essential. The Code of Ethics of the American Society of Plastic Surgeons prohibits plastic surgeons from publicly promoting photographs that show results that are not typical of the results obtained by the average patient, are likely to create false or unjustified expectations, or are intended to attract patients by exaggerated claims.48 Clearly, the ethical standards for advertising should not exceed the quality requirements for scientific publications.
Conflict of Interest
Twelve of the 14 studies are authored by BTL medical editors or speakers. The heavy costs of the MRI images and CT scans are likely borne by the manufacturer. None of the authors have reported that these expenses were absorbed by the investigators. Industry financial support is not mandatory. Other investigators (including this author) have paid for ultrasound and MRI studies, without corporate funding, to avoid conflict of interest.37,49 As the cost borne by the manufacturer goes up, so does the pressure to find a positive result, creating publication bias.31 Two studies that did not received funding from BTL found little or no treatment effect.22,34
Conflict of interest is a common problem affecting evaluation of energy-based treatments.28,36 Investigators may receive their devices discounted or at no charge.28 Although Samuels et al6 disclose no financial assistance for the study, the clinical trial website indicates that the trial was sponsored by BTL Industries and BTL was the responsible party. BTL also provides histological slides, CT images, and clinical photographs to authors.18
The literature on this method, and other energy-based devices, merits renewed scrutiny.28,36,50 It is not coincidental that the 2 studies finding little or no benefit for HIFEM treatments22,34 were also the only studies that were not funded by BTL. Recommended changes to reduce bias include eliminating reliance on corporate funding for plastic surgeons, professional societies, and scientific journals.50,51 Manufacturers fund plastic surgeons to build loyalty and become our “corporate partners.” However, our duty is to our patients.
CONCLUSIONS
Electromagnetic treatment effects are very small, often just a few millimeters, and may lie within the margin of error. A scientific foundation for early changes is lacking. Images often show concomitant fat reductions in untreated areas. Conflict of interest creates bias. Publication in a scientific journal is advertised as a marker of scientific legitimacy on manufacturer websites.28 Our scientific publications serve an important gatekeeping function. Plastic surgeons need to be vigilant to be sure that such publications are adequately vetted so as not to simply represent marketing tools.28,36 In evaluating a new method, 2 basic criteria must be met—a sound physical basis and reliable evidence of efficacy.28 Whether electromagnetic treatments, with or without simultaneous radiofrequency, meet this standard remains open to question.
Footnotes
Dr Swanson receives royalties from Springer Nature (Cham, Switzerland).
Conflicts of interest and sources of funding: none declared.
REFERENCES
- 1.Abulhasan JF Rumble YLD Morgan ER, et al. Peripheral electrical and magnetic stimulation to augment resistance training. J Funct Morphol Kinesiol. 2016;1:328–342. [Google Scholar]
- 2.Galloway NTM El-Galley RES Sand PK, et al. Extracorporeal magnetic innervation therapy for stress urinary incontinence. Urology. 1999;53:1108–1111. [DOI] [PubMed] [Google Scholar]
- 3.Kinney BM. Pulsed electromagnetic field therapy in plastic surgery. Aesthet Surg J. 2005;25:87–91. [DOI] [PubMed] [Google Scholar]
- 4.Strauch B Herman C Dabb R, et al. Evidence-based use of pulsed electromagnetic field therapy in clinical plastic surgery. Aesthet Surg J. 2009;29:135–143. [DOI] [PubMed] [Google Scholar]
- 5.Jacob CI, Paskova K. Safety and efficacy of a novel high-intensity focused electromagnetic technology device for noninvasive abdominal body shaping. J Cosmet Dermatol. 2018;17:783–787. [DOI] [PubMed] [Google Scholar]
- 6.Samuels JB, Katz B, Weiss RA. Radiofrequency heating and high-intensity focused electromagnetic treatment delivered simultaneously: the first sham-controlled randomized trial. Plast Reconstr Surg. 2022;149:893e–900e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Metrics . Available at: https://journals.lww.com/plasreconsurg/Fulltext/2022/05000/Radiofrequency Heating_and_High_Intensity_Focused.14.aspx. Accessed June 30, 2022.
- 8.Goldberg DJ Enright KM Goldfarb R, et al. The role and clinical benefits of high-intensity focused electromagnetic devices for non-invasive lipolysis and beyond: a narrative review and position paper. J Cosmet Dermatol. 2021;20:2096–2101. [DOI] [PubMed] [Google Scholar]
- 9.FDA 510(k) approval letter. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf19/K192224.pdf. Accessed June 30, 2022.
- 10.Katz B Bard R Goldfarb R, et al. Ultrasound assessment of subcutaneous abdominal fat thickness after treatments with a high-intensity focused electromagnetic field device: a multicenter study. Dermatol Surg. 2019;45:1542–1548. [DOI] [PubMed] [Google Scholar]
- 11.Kinney BM, Kent DE. MRI and CT assessment of abdominal tissue composition in patients after high-intensity focused electromagnetic therapy treatments: one-year follow-up. Aesthet Surg J. 2020;40:NP686–NP693. [DOI] [PubMed] [Google Scholar]
- 12.Katz B, Duncan D. Lifting and toning of arms and calves using high-intensity focused electromagnetic field (HIFEM) procedure documented by ultrasound assessment. J Drugs Dermatol. 2021;20:755–759. [DOI] [PubMed] [Google Scholar]
- 13.Jacob C, Kent D, Ibrahim O. Efficacy and safety of simultaneous application of HIFEM and synchronized radiofrequency for abdominal fat reduction and muscle toning: a multicenter magnetic resonance imaging evaluation study. Dermatol Surg. 2021;47:969–973. [DOI] [PubMed] [Google Scholar]
- 14.Jacob C Kinney B Busso M, et al. High intensity focused electro-magnetic technology (HIFEM) for non-invasive buttock lifting and toning of gluteal muscles: a multi-center efficacy and safety study. J Drugs Dermatol. 2018;17:1229–1232. [PubMed] [Google Scholar]
- 15.Kinney BM, Lozanova P. High intensity focused electromagnetic therapy evaluated by magnetic resonance imaging: safety and efficacy study of a dual tissue effect based non-invasive abdominal body shaping. Lasers Surg Med. 2019;51:40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leone A Piccolo D Conforti C, et al. Evaluation of safety and efficacy of a new device for muscle toning and body shaping. J Cosmet Dermatol. 2021;20:3863–3870. [DOI] [PubMed] [Google Scholar]
- 17.Murgia RD Noell C Weiss M, et al. Body contouring for fat and muscle in aesthetics: review and debate. Clin Dermatol. 2022;40:29–34. [DOI] [PubMed] [Google Scholar]
- 18.Hoffmann K Soemantri S Hoffmann K, et al. Body shaping with high-intensity focused electromagnetic technology. J Ästhet Chir. 2020;13:64–69. [Google Scholar]
- 19.Jacob CI, Rank B. Abdominal remodeling in postpartum women by using a high-intensity focused electromagnetic (HIFEM) procedure: an investigational magnetic resonance imaging (MRI) pilot study. J Clin Aesthet Dermatol. 2020;13(9, suppl 1):S16–S20. [PMC free article] [PubMed] [Google Scholar]
- 20.Giesse S. A German prospective study of the safety and efficacy of a non-invasive, high-intensity, electromagnetic abdomen and buttock contouring device. J Clin Aesthet Dermatol. 2021;14:30–33. [PMC free article] [PubMed] [Google Scholar]
- 21.BTL Website . Available at: https://bodybybtl.com. Accessed July 5, 2022.
- 22.Kilmer SL Cox SE Zelickson BD, et al. Feasibility study of electromagnetic muscle stimulation and cryolipolysis for abdominal contouring. Dermatol Surg. 2020;46:S14–S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katz B. MRI assessment of arm and calf muscle toning with high-intensity focused electromagnetic technology: case study. J Drugs Dermatol. 2020;19:556–558. [PubMed] [Google Scholar]
- 24.Kent DE, Kinney BM. The effect of high-intensity focused electromagnetic procedure on visceral adipose tissue: retrospective assessment of computed tomography scans. J Cosmet Dermatol. 2021;20:757–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kent DE, Jacob CI. Simultaneous changes in abdominal adipose and muscle tissues following treatments by high-intensity focused electromagnetic (HIFEM) technology-based device: computed tomography evaluation. J Drugs Dermatol. 2019;18:1098–1102. [PubMed] [Google Scholar]
- 26.Palm M. Magnetic resonance imaging evaluation of changes in gluteal muscles after treatments with the high-intensity focused electromagnetic procedure. Dermatol Surg. 2021;47:386–391. [DOI] [PubMed] [Google Scholar]
- 27.Paul M, Mulholland RS. A new approach for adipose tissue treatment and body contouring using radiofrequency-assisted liposuction. Aesthetic Plast Surg. 2009;33:687–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swanson E. A systematic review of subsurface radiofrequency treatments in plastic surgery. Ann Plast Surg. 2022;89:274–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sackett DL Straus SE Richardson WS, et al. Therapy. In: Evidence-Based Medicine. 2nd ed. Toronto, ON: Churchill Livingstone; 2000:105–153. [Google Scholar]
- 30.ClinicalTrials.gov . rPMS and radiofrequency for abdominal toning and reduction of subcutaneous fat. Available at: https://clinicaltrials.gov/ct2/show/NCT04587986. Accessed July 5, 2022.
- 31.Swanson E. Levels of evidence in cosmetic surgery: analysis and recommendations using a new CLEAR classification. Plast Reconstr Surg Glob Open. 2013;1:e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stallknecht B, Dela F, Helge JW. Are blood flow and lipolysis in subcutaneous adipose tissue influenced by contractions in adjacent muscles in humans? Am J Physiol Endocrinol Metab. 2007;292:E394–E399. [DOI] [PubMed] [Google Scholar]
- 33.Weiss RA, Bernardy J. Induction of fat apoptosis by a non-thermal device: mechanism of action of non-invasive high-intensity electromagnetic technology in a porcine model. Lasers Surg Med. 2019;51:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zachary CB Burns AJ Pham LD, et al. Clinical study demonstrates that electromagnetic muscle stimulation does not cause injury to fat cells. Lasers Surg Med. 2021;53:70–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goldberg DJ. Deletion of adipocytes induced by a novel device simultaneously delivering synchronized radiofrequency and hifem: human histological study. J Cosmet Dermatol. 2021;20:1104–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Swanson E. Cryolipolysis: the importance of scientific evaluation of a new technique. Aesthet Surg J. 2015;35:NP116–NP119. [DOI] [PubMed] [Google Scholar]
- 37.Swanson E. Assessment of reduction in subcutaneous fat thickness after liposuction using magnetic resonance imaging. J Plast Reconstr Aesthet Surg. 2012;65:128–130. [DOI] [PubMed] [Google Scholar]
- 38.Schoenfeld BJ. The mechanisms of muscle hypertrophy and their application to resistance training. J Strength Cond Res. 2010;24:2857–2872. [DOI] [PubMed] [Google Scholar]
- 39.Mulligan SE Fleck SJ Gordon SE, et al. Influence of resistance exercise volume on serum growth hormone and cortisol concentrations in women. J Strength Cond Res. 1996;10:256–262. [Google Scholar]
- 40.Schoenfeld B. The use of specialized training techniques to maximize muscle hypertrophy. Strength Cond J. 2011;33:60–65. [Google Scholar]
- 41.McCall GE Byrnes WC Dickinson A, et al. Muscle fiber hypertrophy, hyperplasia, and capillary density in college men after resistance training. J Appl Physiol (1985). 1996;81:2004–2012. [DOI] [PubMed] [Google Scholar]
- 42.Mazzoni D Lin MJ Dubin DP, et al. Review of non-invasive body contouring devices for fat reduction, skin tightening and muscle definition. Australas J Dermatol. 2019;60:278–283. [DOI] [PubMed] [Google Scholar]
- 43.Duncan D, Dinev I. Noninvasive induction of muscle fiber hypertrophy and hyperplasia: effects of high-intensity focused electromagnetic field evaluated in an in-vivo porcine model: a pilot study. Aesthet Surg J. 2020;40:568–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Halaas Y Duncan D Bernardy J, et al. Activation of skeletal muscle satellite cells by a device simultaneously applying high-intensity focused electromagnetic technology and novel RF technology: fluorescent microscopy facilitated detection of NCAM/CD56. Aesthet Surg J. 2021;41:NP939–NP947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.ClinicalTrials.gov . Clinical evaluation of the BTL-899 device for non-invasive lipolysis on human fat tissue. Available at: https://clinicaltrials.gov/ct2/show/NCT03923855?term=Denkova&draw=2&rank=4. Accessed July 5, 2022.
- 46.ClinicalTrials.gov . Effect of the BTL-899 therapy for non-invasive lipolysis and circumference reduction of abdomen. Available at: https://clinicaltrials.gov/ct2/show/NCT03270150?term=BTL&draw=2&rank=1. Accessed July 5, 2022.
- 47.The Free Dictionary . Muscle tone definition. Available at: https://medical-dictionary.thefreedictionary.com/muscle+tone. Accessed July 5, 2022.
- 48.Code of ethics of the American Society of Plastic Surgeons. Available at: https://www.plasticsurgery.org/documents/Governance/asps-code-of-ethics.pdf. Accessed October 27, 2022.
- 49.Swanson E. Prospective controlled study of buttock fat transfer using ultrasound and photographic measurements. Plast Reconstr Surg Glob Open. 2016;4:e697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Swanson E, Brown T. A discussion of conflicts of interest in plastic surgery and possible remedies. Plast Reconstr Surg Glob Open. 2018;6:e2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Swanson E, Bloom RJ. It is time for plastic surgeons to start picking up the tab. Ann Plast Surg. 2020;85:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]


