Abstract
The opioid crisis is a significant public health issue in North America that began in the 1990s with opioid-related deaths increasing each year. Although studies have been published regarding the incidence of opioid-related deaths in the general population, there is limited information regarding deaths in the prison population. To investigate the impact of the opioid epidemic in this vulnerable population, a retrospective study of all drug-related deaths that occurred in correctional facilities and penitentiaries in Ontario, Canada, between January 2009 and December 2019 was conducted. A total of 90 deaths were attributed to acute drug toxicity and the decedents ranged in age from 18 to 63 years and comprised 81 men and 9 women. The results of this study indicate the number of drug-related fatalities have increased by 375% (from 4 to 19) over the last 11 years. The detection of opioids in drug-related deaths has increased with fentanyl being the most frequently detected drug. Data also indicates the recent emergence of fentanyl-related analogues in this population. The results from this study provide valuable information about drug-related deaths in the Ontario prison system and provide insight into how the opioid crisis and the increased use of fentanyl and its analogues have affected this vulnerable population.
Keywords: Opioid, Incarceration, Forensic pathology, Toxicology, Fentanyl
Introduction/Background
The opioid crisis has been a major health care issue in North America since the 1990s and has developed into one of the leading public health crises of the current era [1]. There have been three definitive waves of the opioid crisis, each defined by a type of opioid responsible for the majority of deaths during that time period [1]. The first wave during the early 2000s was dominated by prescription opioids, fuelled by over-prescription of pain management drugs like OxyContin® (oxycodone) [1]. In 2012, Canada introduced new prescription regulations making prescription opioids harder to obtain, as well as replacing OxyContin® with a new “tamper-proof,” slow-release formulation (OxyNeo®) that curtailed access for many opioid-using individuals [2, 3]. These restrictions gave rise to a “substitution effect,” creating a booming illicit market for opioids, both prescription and non-prescription, triggering a second wave of the epidemic [2, 3]. During this second wave, North America saw a rise in illicit heroin and fentanyl use, resulting in a steep increase in overdose deaths [1, 2]. The third, most recent wave, has been dominated by synthetic opioids, such as fentanyl and fentanyl analogues, including carfentanil [1]. These powerful opioids can be up to 10,000 times more potent than morphine [4]. The increasing availability and use of extremely potent synthetic opioids has become a significant risk to public safety, resulting in 16,364 reported opioid-related deaths in Canada between January 2016 and March 2020 [5]. Furthermore, recent studies have shown an acute exacerbation of this accelerating trend of drug-related deaths throughout the COVID-19 pandemic, demonstrating an apparent compounding effect of the overlap of the opioid epidemic and COVID-19 pandemic in the drug-using population [6].
Despite the extensive security measures that can exist within correctional facilities, illicit drugs can be brought into these facilities through various means including points of entry such as with inmates, visitors, and correctional staff, or by spraying liquified drugs on incoming mail for inmates [7]. Previous research has indicated that inmates are at a particularly high risk for opioid overdoses in comparison to the general population for several reasons. First, incarceration may contribute to a decrease in drug tolerance by limiting drug availability and opportunities for use; if drug use resumes, this reduction in tolerance could result in drug toxicity or death [8]. Second, individuals who use opioids are more likely to continue drug use while incarcerated compared to those who use other types of drugs such as cocaine or methamphetamine [9]. This may be attributed to the strong reinforcing and addictive properties of opioids [10]. Finally, the possibility of unintentional exposure to potent opioids has risen substantially in recent years as drugs such as fentanyl and its analogues have made their way into illicit drug supplies, increasing the risk to individuals using these drugs with or without knowledge of their presence in the supply [11].
The purpose of this research was to examine how the correctional facility and penitentiary populations of Ontario have been impacted by the opioid crisis, how the trends in drug-related deaths have changed during this 11-year period, and whether trends in opioid-related deaths were consistent with data in the general population.
Methods
This was a retrospective study of 370 deaths occurring in custody between 2009 and 2019. In Ontario, all deaths occurring in custody require investigation by a coroner and relevant case information was obtained from the electronic databases and archives of the Office of the Chief Coroner and the Ontario Forensic Pathology Service. The cases were then further classified, as shown in Fig. 1. Inclusion criteria for the study were as follows:
Fig. 1.

Case classification system
Death pronounced between January 2009 and December 2019.
The decedent was considered to be in custody at the time of death.
Autopsy and toxicology testing performed.
Cause of death determined to be acute drug toxicity.
The individual’s age, sex, manner of death, and the date of death were recorded. For cases where an autopsy was ordered, the post-mortem report and toxicology report were reviewed. The pathological cause of death and drug detections were extracted. Toxicological drug detections relevant to the death were determined by the investigating pathologist and reported in the cause of death statement within the post-mortem report. The cause and manner of death were reviewed by study investigators and no reclassifications occurred for the purposes of this study.
Toxicological analyses were performed by the Centre of Forensic Sciences (CFS), a provincial forensic laboratory that performs the toxicological analyses for all medicolegal investigations in the Province of Ontario. Routine drug testing for deaths occurring in correctional facilities included immunoassay, head-space gas chromatography with flame ionization detection (GC-FID), and liquid chromatography-tandem mass spectrometry (LC-MS/MS) multi-target quantitation method. Liquid chromatography quadrupole time-of-flight MS (LC-QTOF-MS) drug screening was added to the standard screening procedures in 2017.
Data were analyzed to report the incidence of events each year and overall. Logistic modelling was used to compare the odds of events between years and to determine if certain factors played a significant role in predicting outcomes. Detected drugs were classified as opioids or non-opioid drugs of abuse and the contribution to the cause of death was determined by the pathologist and coroner. Medications that are commonly used in medical settings and were reported in the case history to have been administered in this setting—for example, resuscitation medications—were not deemed to be relevant to the cause of death.
The number of acute drug toxicity and opioid-related deaths per year was determined and further analyzed to evaluate the overall impact on the number of deaths in custody each year. Binomial logistic models were used to assess any effects of year, age, and sex to determine if any of these factors were predictors of an opioid-related death in incarcerated individuals.
Results and discussion
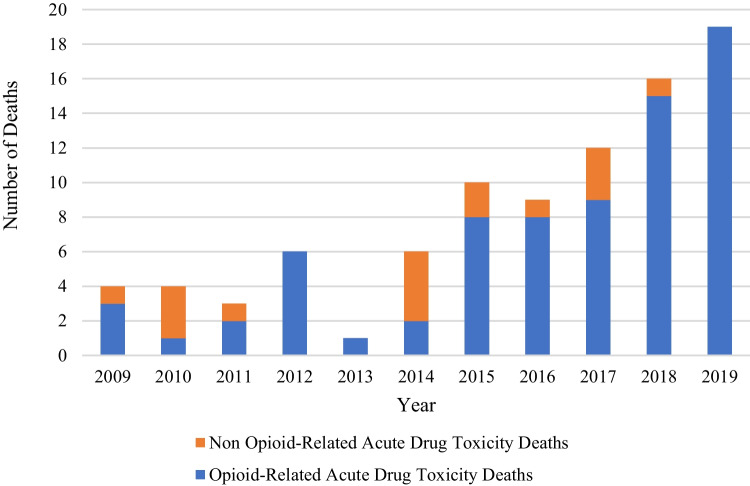
Of the 370 deaths that occurred in custody between 2009 and 2019, 90 were classified as acute drug toxicity. The number and proportion of acute drug toxicity deaths have risen substantially within recent years. Comparing 2009 to 2019 there has been a 375% increase in the number of deaths attributed to overdose per year (Fig. 2).
Fig. 2.
Number of acute drug toxicity deaths in Ontario correctional facilities and penitentiaries between 2009 and 2019, shown with the proportion of opioid and non-opioid related deaths per year
The number of opioid-related deaths has increased substantially between 2009 and 2019. The greatest increases were observed from 2015 to 2019 with the highest proportion of opioid-related deaths occurring in 2018 (44% of total deaths in custody) (Fig. 3). This data demonstrates that the number of deaths in custody attributed to opioids is not increasing simply due to an overall increase in deaths in custody; the rate of change of opioid-related deaths is independent from the changes in overall deaths in custody. Statistical modelling was performed to identify which factors may have contributed to higher odds of opioid-related death occurring. From the logistic model, it was determined that the year that the death occurred was a significant predictor of opioid overdose deaths (p-value < 0.001), with the odds of an opioid overdose 11.5 times higher in 2019 compared to 2009 (95% confidence interval of (10.5, 12.8)).
Fig. 3.
Opioid-related deaths and non-opioid related acute drug toxicity deaths as a proportion of total deaths occurring in custody per year between 2009 and 2019
In Ontario, manner of death is categorized into 1 of 5 categories: natural, accident, suicide, homicide, or undetermined. An undetermined manner is assigned in cases where there is insufficient or contradictory information on whether the death can be categorized into one of the other four manners of death. The majority of the deaths in this study were classified as accident (94.4%), with three classified as suicide (3.3%), two as undetermined (2.2%), none as natural, and none as homicide (Table 1). All of the cases where the manner of death was determined to be suicide had been subject to a coroner’s inquest (a public hearing reviewing the available evidence in the death investigation before a 5 member jury panel of eligible community jurors) and the reported manner of death reflected the jury’s conclusion on manner of death to the evidentiary standard of the balance of probabilities based on the available evidence in the case. Evidence to support such a conclusion ranged from toxic concentrations of therapeutic drugs with availability of sufficient quantities of the same medication(s) through to notes discovered at the scene with suggestive writing. Both of the cases classified as undetermined represented cases where the evidentiary base was considered insufficient to differentiate between accident and suicide or homicide. All of the non-accidental manner of death cases were reviewed by the forensic pathologist involved in this study and none was reclassified for the purposes of this study. The observation that the majority of overdose deaths were accidental is consistent with observations made for drug-related deaths in the general population of North America [12–14].
Table 1.
Age, sex, and manner of death of decedents, presented by year. Homicide and natural have been excluded from manner of death classification in this table, as none of the 90 acute drug toxicity deaths was homicide or natural deaths
| Year | Average age | Males | Females | Accident | Suicide | Undetermined |
|---|---|---|---|---|---|---|
| 2009 | 32 | 4 | 0 | 4 | 0 | 0 |
| 2010 | 45 | 4 | 0 | 3 | 1 | 0 |
| 2011 | 25 | 3 | 0 | 3 | 0 | 0 |
| 2012 | 38 | 5 | 1 | 5 | 1 | 0 |
| 2013 | 62 | 1 | 0 | 1 | 0 | 0 |
| 2014 | 38 | 5 | 1 | 6 | 0 | 0 |
| 2015 | 38 | 10 | 0 | 8 | 1 | 1 |
| 2016 | 39 | 8 | 1 | 9 | 0 | 0 |
| 2017 | 34 | 9 | 3 | 11 | 0 | 1 |
| 2018 | 36 | 16 | 0 | 16 | 0 | 0 |
| 2019 | 35 | 16 | 3 | 19 | 0 | 0 |
The age range of the decedents in this sample was 18 years of age to 63 years of age. The mean age of the decedents at their time of death was 36 years of age, with a median of 35 years of age and a standard deviation of 9.4 years. Previous drug toxicity studies involving the general Ontario population have reported that the highest proportion of deaths are in the age range of 25–44 [12] suggesting that this age range is particularly susceptible to drug-related deaths regardless of incarceration status [13]. Ninety percent of the decedents in this sample were male, with females only making up 10% of the acute drug toxicity deaths during this time period. This is a greater difference between males and females than in the general population [13], which may be attributed to differences in sex distribution between the incarcerated compared to the general population [15].
Of the non-opioid acute drug toxicity deaths, the most commonly detected drugs were cocaine (n = 14) and methamphetamine (n = 13). Other drugs frequently detected in these deaths were prescription benzodiazepines, amitriptyline and nortriptyline, tetrahydrocannabinol and its metabolites, and naloxone. Except for one amitriptyline toxicity death (accidental), the prescription benzodiazepines, amitriptyline, and nortriptyline were detected at concentrations within their respective therapeutic ranges.
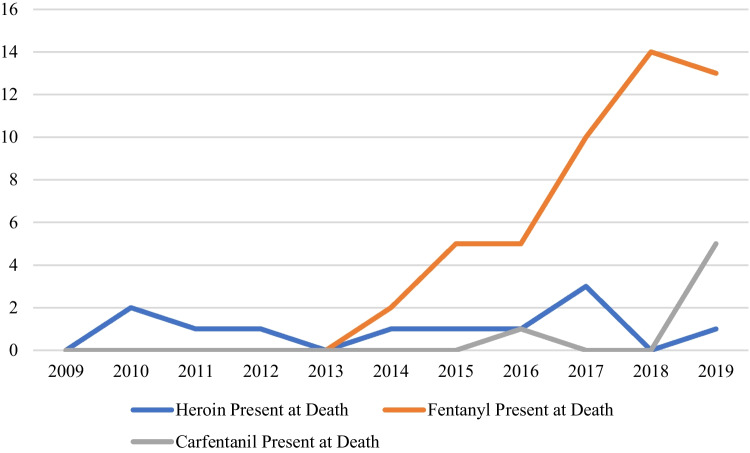
In the 90 cases in this study, fentanyl was the most frequently detected drug (n = 49) (Fig. 4). The only other opioid that was frequently detected was morphine, which was identified in 21 cases. The majority of these morphine detections were in combination with codeine or 6-monoacetylmorphine (6-MAM). Morphine can be detected as a result of heroin (diacetylmorphine) administration, morphine administration, and/or arise as a metabolite, with the presence of the heroin-specific metabolite 6-monoacetylmorphine considered indicative of heroin administration [16].
Fig. 4.
Opioids detected in toxicological tests for the 90 acute drug toxicity deaths. Inclusion, as detected, does not consider significance to cause of death. Multiple opioids may have been detected for one decedent
In Fig. 5, the major contributing drug in each of the opioid-related deaths every year is shown. A drug was considered to be a major contributing factor if it was listed in the cause of death statement by the forensic pathologist. The three most frequently detected opioids were heroin, fentanyl, and carfentanil. Eight opioid deaths are not accounted for in this graph because they were attributed to mixed drug toxicity with no dominant contributor. Heroin was the most frequently detected drug in deaths occurring between 2009 and 2013 which was expected when comparing to trends seen in the general North American population [1]. The rates of heroin detection remained fairly stable throughout the time period, demonstrating that the large increase in opioid deaths can be attributed to the rise of fentanyl and fentanyl analogues. Fentanyl contributed to 49 deaths in this study, more than any other drug detected and has been the most frequently detected drug since 2013. Logistic modelling methods showed that the year of death was important to the risk of death due to drug toxicity involving fentanyl (p-value < 0.001).
Fig. 5.
Number of acute drug toxicity deaths categorized by year and by type of opioid present at death
Analytical capabilities are an important consideration when conducting toxicology analyses in death investigation cases. During the timeframe of this study, the CFS implemented a routine LC-QTOF-MS screening method capable of detecting > 300 drugs and improved the capabilities of targeted LC-MS/MS analyses for emergent drugs. In response to the appearance of carfentanil in the illicit drug supply in 2016, the CFS developed and implemented a quantitative method in 2017. Due to the potency of carfentanil, the sensitivity of the method was further improved in 2019 and may have contributed to the increase in carfentanil detection.
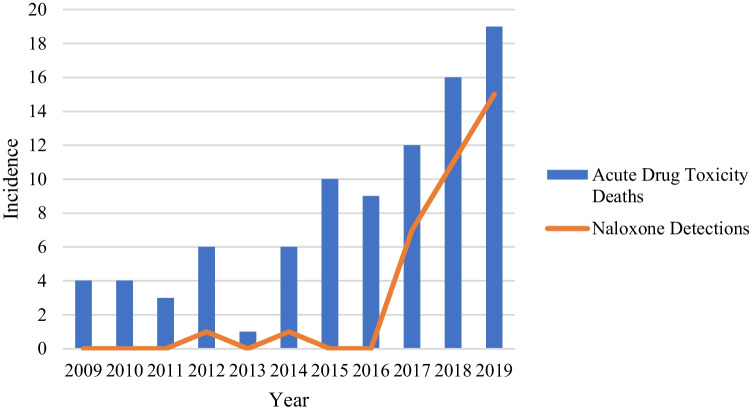
In the latter part of our study, in addition to observing an increase in opioid deaths, we also saw an increase in the detection of the opioid antagonist naloxone, with naloxone being detected in the majority of cases beginning in 2017 (Fig. 6). This could be due to the implementation of routine QTOF screening methods in 2017, which enabled reliable detection of naloxone. In addition, inquests into the deaths of a number of individuals who died in correctional facilities have recommended the availability of naloxone, which may account for the increased detection rates in later years of the study [17]. The use of naloxone can be an important tool in reducing opioid toxicity; however, in the face of increased use of synthetic opioids such as fentanyl and carfentanil, naloxone’s effectiveness may be reduced. It has been proposed that, due to the increased potency of some synthetic opioids, higher doses of naloxone should be administered than are currently recommended [18]. Furthermore, although not reported in any cases in the current study, other potent central nervous system depressants have been detected in acute drug toxicity cases in Ontario, including various designer benzodiazepines and several nitazenes, the appearance of which could very well have an adverse impact on the efficacy of standard dose naloxone reversal strategies [19].
Fig. 6.
Number of acute drug toxicity deaths per year compared to the number of cases where naloxone was detected in acute drug toxicity death cases
This study has several limitations. The interpretation of post-mortem blood concentrations can be complicated by factors including post-mortem redistribution, drug stability, and overlap between incidental and fatal concentrations. As the overlap between incidental and fatal concentrations can be substantial for opioids due to the development of tolerance, the significance of an opioid finding cannot be determined solely from a detected blood concentration. In addition to the toxicology results, information including available prescribed medications, drug and/or case history, and autopsy findings can assist with interpretation and may be considered in the cause of death determination; however, if this information is unavailable or inconsistently reported in post-mortem reports, it could contribute to an overestimation of opioid toxicity. In addition, the small number of opioid-related fatalities and the inclusion of only correctional facilities and penitentiaries in Ontario provides insight into the opioid crisis on the local incarcerated population but further research into other Canadian jurisdictions is required to evaluate the full impact and regional trends.
Conclusion
This study demonstrated that opioid-related deaths in correctional facilities and penitentiaries have substantially increased over the 10-year time period between 2009 and 2019. The odds of a death occurring due to acute opioid toxicity in 2019 was estimated to be 11.5× higher than in 2009. Incarcerated men have died more frequently as a result of an opioid overdose as compared to incarcerated women, which is consistent with the findings in the general population. The vast majority of acute drug toxicity deaths that occurred during this period were accidents, with only 3 deaths classified as suicides. This study also highlights the serious risk of fentanyl and carfentanil exposure for incarcerated individuals, evidenced by the increasing number of opioid-related deaths involving fentanyl and its analogs. Continued monitoring of the specific drugs detected in correctional facility and penitentiary deaths is necessary in order to best inform preventative measures or interventions, such as the availability of naloxone. Understanding trends in the drugs and toxins involved in acute drug toxicity-related deaths in Ontario’s incarcerated population is an essential step to inform the evaluation of various preventative health measures and provide the best available interventions to individuals at risk of death due to substance use while incarcerated. Ongoing studies surveilling various aspects of acute drug toxicity deaths in the incarcerated population, including studying the emergence of novel psychoactive substances (NPS) and the use of opioid antagonists such as naloxone, are needed to gain a deeper understanding of how the evolving opioid crisis continues to impact this vulnerable population and to inform the best strategies for harm reduction.
Key points
This 11-year retrospective study into drug-related deaths in Ontario’s incarcerated population demonstrated a 375% increase in drug-related deaths during the study period.
Opioid-related deaths have substantially increased and now account for about 40% of all deaths in custody.
Specific opioids of concern have evolved from heroin and oxycodone to more potent synthetic opioids including fentanyl and carfentanil.
Acknowledgements
We would like to thank Adele Lauzon from the Univeristy of Toronto Department of Statistical Sciences and Dr Ramya Thinniyam from the University of Toronto Mississauga Mathematical and Computational Sciences for their contributions to the statistical analyses.
Author contributions
Lourdes Button: methodology, formal analysis, investigation, writing—original draft. Karen Woodall: conceptualization, supervision, methodology, investigation, writing—review and editing. Andrew Williams: supervision, methodology, investigation, writing—review and editing. Christina Lamparter: conceptualization, writing—review and editing
Declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Review Committee (ERC) at the University of Toronto Mississauga (Reference #: 2020-016).
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019;71:183–8. doi: 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fischer B, Pang M, Tyndall M. The opioid death crisis in Canada: crucial lessons for public health. Lancet Public Heal. 2019;4(2):e81–2. doi: 10.1016/S2468-2667(18)30232-9. [DOI] [PubMed] [Google Scholar]
- 3.Fischer B, Keates A. “Opioid Drought”, Canadian-style? Potential implications of the “natural experiment” of delisting oxycontin in Canada. Int J Drug Policy. 2012;23(6):495–7. doi: 10.1016/j.drugpo.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Rab E, Flanagan RJ, Hudson S. Detection of fentanyl and fentanyl analogues in biological samples using liquid chromatography–high resolution mass spectrometry. Forensic Sci Int. 2019;300:13–8. doi: 10.1016/j.forsciint.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Public Health Agency of Canada. Apparent opioid-related deaths surveillance of opioid- related harms in Canada. Ottawa. 2020.
- 6.Dmetrichuk JM, Rosenthal JS, Man J, Cullip M, Wells RA. Retrospective study of non-natural manners of death in Ontario: effects of the COVID-19 pandemic and related public health measures. Lancet Reg Heal - Am. 2022;7:100130. doi: 10.1016/j.lana.2021.100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shukla R, Peterson BE, Kim K. Contraband and interdiction strategies in correctional facilities. 2021.
- 8.McIntyre JL. Combatting the opioid crisis from prison: initiating opioid agonist therapy. J Forensic Nurs. 2018 doi: 10.1097/JFN.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 9.Strang J, Gossop M, Heuston J, Green J, Whiteley C, Maden A. Persistence of drug use during imprisonment: relationship of drug type, recency of use and severity of dependence to use of heroin, cocaine and amphetamine in prison. Addiction. 2006 doi: 10.1111/j.1360-0443.2006.01475.x. [DOI] [PubMed] [Google Scholar]
- 10.Kelly TH. Conditioning history and the reinforcing effects of drugs: comment on Alessi, Roll, Reilly, and Johanson (2002) Exp Clin Psychopharmacol. 2002;10(2):92–5. doi: 10.1037/1064-1297.10.2.92. [DOI] [PubMed] [Google Scholar]
- 11.Bucerius SM, Haggerty KD. Fentanyl behind bars: the implications of synthetic opiates on prisoners and correctional officers. Int J Drug Policy. 2019 doi: 10.1016/j.drugpo.2019.05.018. [DOI] [PubMed] [Google Scholar]
- 12.Gomes T, Greaves S, Martins D, et al. Latest trends in opioid-related deaths in Ontario: 1991 to 2015. Ontario Drug Policy Res Netw. 2017;(April):1–2.
- 13.Public Health Ontario. Opioid mortality surveillance report: analysis of opioid-related deaths in Ontario July 2017 – June 2018. 2019.
- 14.Jalal H, Buchanich JM, Sinclair DR, Roberts MS, Burke DS. Age and generational patterns of overdose death risk from opioids and other drugs. Nat Med. 2020;26(5):699–704. doi: 10.1038/s41591-020-0855-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malakieh J. Adult and youth correctional statistics in Canada, 2018/2019. Juristat. 2018;(85):2–21.
- 16.Keary CJ, Wang Y, Moran JR, Zayas LV, Stern TA. Toxicologic testing for opiates: understanding false-positive and false-negative test results. Prim Care Companion J Clin Psychiatry. 2012;14(4):23251863. doi: 10.4088/PCC.12f01371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jhirad R. Verdict of Coroner ’s Jury Office of the Chief Coroner -Hamilton Wentworth Detention Centre. 2018;1–15.
- 18.Moss RB, Carlo DJ. Higher doses of naloxone are needed in the synthetic opiod era. Subst Abus Treat Prev Policy. 2019;14(1):1–6. doi: 10.1186/s13011-019-0195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Public Health Ontario. Novel non-fentanyl synthetic opioids: risk assessment and implications for practice. 2021;1–14.