Abstract
Purpose
The 4-corner arthrodesis (FCA) is a reliable, motion-sparing technique used to treat scapholunate advanced collapse and scaphoid nonunion advanced collapse arthritis, particularly in stage III wrists in which the capitolunate articulation is compromised. Surgical technique and patient-level variables may influence complications following FCA. We sought to evaluate the rate of complications in a large, combined database and manual chart review study.
Methods
Current Procedural Terminology codes were used to search the United States Veteran’s Health Administration corporate database to identify wrists treated with FCA over a 24-year period. A retrospective chart review was completed to collect data regarding scapholunate advanced collapse/scaphoid nonunion advanced collapse stage, implant used, the use of a bone graft, smoking status, and comorbidities for all patients undergoing an FCA. A multivariable cox proportional hazards regression was used to assess hazard ratios for reoperation. Incidence rates and the standard error of the mean for reoperation and conversion to total wrist fusion were calculated after grouping patients by 10-year age categories.
Results
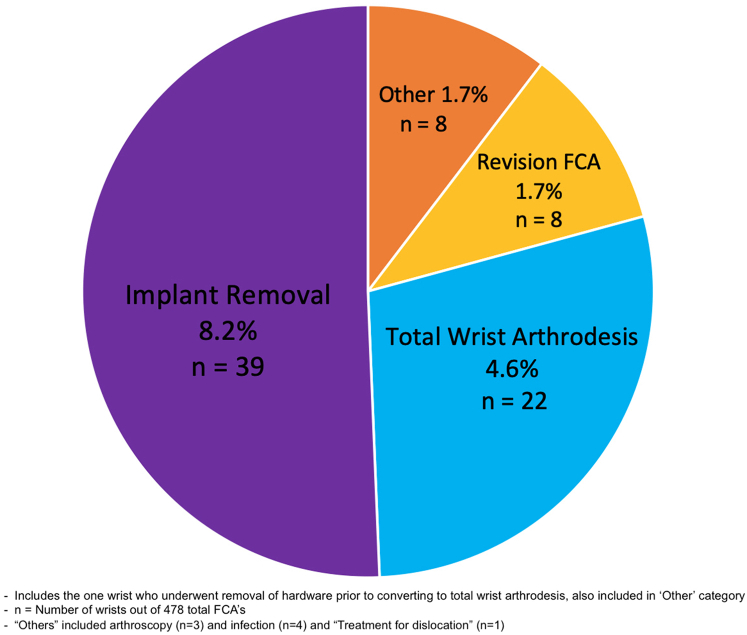
A total of 478 wrists underwent FCA during the study period, with a mean follow-up of 63 months. Seventy-three (16%) wrists required reoperation. The most frequent secondary procedures included unplanned implant removal (8.2%), total wrist arthrodesis (4.6%), and revision FCA (1.7%). Positive smoking history increased the risk of reoperation, whereas posterior interosseous nerve neurectomy, arthritis stage, and fixation type did not have a statistically significant association with reoperation. Younger age demonstrated an increased incidence of overall reoperation and wrist fusion.
Conclusions
The most common reason for reoperation after FCA was implant removal. Smoking history is associated with increased rates of reoperation and wrist arthrodesis. Knowledge of these factors may assist with accurately counseling and indicating patients for FCA.
Type of study/level of evidence
Therapeutic III.
Key words: Arthrodesis, 4-corner arthrodesis, SLAC, SNAC, Wrist fusion
The 4-corner arthrodesis (FCA) is an effective, motion-preserving procedure frequently used to treat a variety of symptomatic carpal conditions, most commonly scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. In addition to motion preservation, FCA can maintain carpal height, conserve radiolunate articulation, and improve grip strength.1 As described by Watson and Ballet2, 3, 4, 5 in 1984, FCA involves scaphoidectomy followed by arthrodesis of the capitate, hamate, lunate, and triquetrum. In stage III SLAC/SNAC, FCA is the motion-preserving treatment of choice, as the degeneration of the capitolunate joint may preclude successful proximal row carpectomy. In stage II SLAC/SNAC, both proximal row carpectomy and FCA may be used to appropriately treat indicated patients, with several considerations as to when FCA may be indicated, including complication risk.1,6, 7, 8
Although FCA has proven to be an effective and dependable option for treating different carpal ailments, the current literature reports overall complication rates as high as 31% and reoperation rates from 8% to 29%.1,8, 9, 10, 11, 12, 13, 14, 15 The most commonly reported complications are symptomatic nonunion, dorsal impingement, implant-related issues, and arthritis progression.1,12,14 Reoperation performed for such complications may include the removal of hardware, revision FCA, and conversion to total wrist arthrodesis (TWA). There is a lack of peer-reviewed literature that identifies risk factors for complications and/or reoperation, with 2 of the largest studies to date including 80 and 251 patients, respectively.7,16 The second study was limited to wrists with stage II arthritis.
The current study sought to identify patient and surgical characteristics associated with an increased risk of complications leading to reoperation following FCA. We hypothesized that a greater comorbidity burden and a positive smoking history would increase the risk of reoperation following index FCA surgery.
Materials and Methods
This study was reviewed and approved by The University of Utah institutional review boards (IRB_00081183) and included approval for data used by the Veteran’s Health Administration. The United States Veterans Health Administration stores veteran medical records and demographic characteristics in a national corporate data warehouse. This database is composed of all 130 veterans’ hospitals in the United States and was accessed to retrospectively review all veterans undergoing FCA between July 1, 1992, and November 30, 2016. Current Procedural Terminology (CPT) codes for intercarpal arthrodesis with (25825) and without autograft (25820) were used to identify patients undergoing FCA, and manual chart review was used to confirm patient and procedure details. The identification of patient demographic characteristics and comorbidity data were performed using the corporate data warehouse and clinical software as outlined below.
The primary outcome of this study was the rate of unplanned secondary operations following index FCA for SLAC/SNAC wrist arthritis. This included all additional surgeries related to the index FCA and encompassed, but was not limited to, procedures such as the conversion to TWA, revision FCA for nonunion, implant removal, arthroscopic debridement, and irrigation and debridement for infection. A secondary outcome of interest was patients who underwent “planned” removal of hardware, such as Kirschner wire removal in the operating room. Outcomes of interest were identified using CPT codes as well as by chart review (Appendix 1, available on the Journal’s website at www.jhsgo.org). Finally, we used International Classification of Disease (ICD) codes to identify risk factors for reoperation, as outlined below (Appendices 2 and 3, available on the Journal’s website at www.jhsgo.org).
Chart review
The preoperative and postoperative clinical notes, immediate postoperative reports, and operative reports for each patient included in the study were reviewed by the study authors (B.N.G. and A.R.S.). This provided a careful evaluation of the arthritis stage, surgical technique details, and secondary operations/complications. A manual review provided verification of the correct association between CPT codes and procedures performed and any documented complications requiring return to the operating room that may not have been initially identified by CPT code search.
All patients aged 18 years and older with stages I–III SLAC/SNAC wrist were included. The review of operative reports provided an intraoperative description of the arthritis pattern that was used to determine staging. The intraoperative description of the arthritis stage was prioritized over documented radiology reports or clinical notes. Ultimately, each patient’s arthritis stage was based on intraoperative descriptions of wear pattern (eg, the presence or absence of arthritis noted on the head of the capitate). Only patients with operative reports available for review were included. Surgical details, including the type of fixation, use and source of bone graft (allograft vs autograft vs none), and posterior interosseous nerve (PIN) neurectomy status data were gathered. Patients with all types of fixation used for FCA were included and categorized into Kirschner wires, plates, screws, and staples. All sources and harvest sites of bone graft were included (eg, allograft vs autograft [iliac crest, distal radius, scaphoid, etc]). Only 2 patients underwent FCA for stage I disease and thus, in addition to sparing of the capitolunate joint, these patients were combined with stage II patients for statistical analysis.
Patients were excluded if they underwent a form of intercarpal fusion other than FCA (eg, capitolunate) or if the chart review lacked sufficient detail for accurate SLAC/SNAC staging. If the operative report did not include an adequate description of the arthritis pattern to determine staging, the patient was excluded. Patients with stage IV were excluded as the clinical decision for these patients does not typically include FCA, given arthritis severity. Patients who underwent FCA for pathology other than SLAC/SNAC wrist were also excluded. The routine or planned removal of Kirschner wires after surgery was excluded from formal analysis of “unplanned reoperation” to not overinflate the rate of reoperation as a “complication.” Reoperation performed in veterans at outside institutions but paid for by the Veterans Affairs (VA) was able to be captured and included by CPT code search only. However, it could not be verified by chart review owing to access of outside hospital records. Patients without initial surgery performed at the Veterans Affairs Medical Center, that is, no operative report in the VA system, were excluded.
Patient characteristics and comorbidity
To identify patient demographic characteristics, medical comorbidities, and health care service utilization, a combination of chart review and ICD codes were used to screen patient charts. Patient characteristics such as age, gender, body mass index, and smoking status were identified by chart review and/or the VA corporate data warehouse search. Smoking history was deemed positive if the patient ever had a positive history documented. Otherwise, it was negative. We did not quantify smoking, given inconsistent documentation. Comorbidity ICD codes were simplified by grouping them into 58 categories based on the “Health Cost and Utilization Project (HCUP) single-level Clinical Classifications Software (CCS)” program.17 These categories were collapsed into 11 CCS categories. Included in these categories were diagnoses such as diabetes, a history of cancer, and a history of substance abuse (Appendix 2). Patient characteristics, including these 11 major comorbidity categories and another 11 demographic and health care utilization variables, were included in the statistical analysis for the evaluation of influence on the risk of reoperations.
Statistical analysis
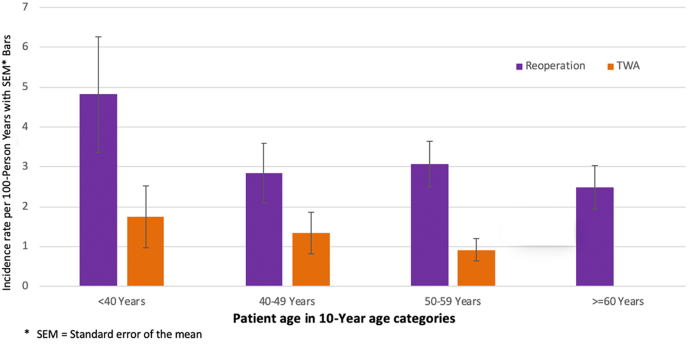
Reoperation rates were tabulated from the entire FCA population. Means, standard deviations (SDs), and interquartile ranges (IQRs) were calculated for descriptive statistics. Multivariable cox proportional hazards regression was used to assess the hazard ratios (HRs) of the factors for reoperation. These factors included age at FCA, race, smoking status, the number of distinct HCUP CCS counts, surgical technique (eg, plate, screw, pin, and staple) used, bone graft status, wrist arthritis patterns (SNAC or SLAC), and stage (I, II, and III). We used HRs to determine the influence of the clinical and surgical variables on the reoperation rates to most appropriately account for the specific follow-up time each patient contributed to the study. Incidence rates and the standard error of the mean for reoperation and the conversion to total wrist arthrodesis were calculated after grouping patients by 10-year age categories.
Results
The initial CPT code search identified 1,284 patients with operative reports who underwent intercarpal fusion. A manual chart review identified 552 potentially eligible patients that underwent FCA during the study period (732 patients underwent other forms of intercarpal fusion). Of the 552 patients identified, 23 had stage IV SLAC/SNAC arthritis and 51 had incomplete clinical documentation to determine staging and were excluded. A total of 478 primary FCAs were performed in 468 patients (10 patients had bilateral surgery) and wrists were analyzed separately.
Select patient demographic and surgical technique details can be found in Table 1. The mean patient age at the index FCA was 56.8 years, and 99% were men. The median follow-up time from the index FCA to the first outcome, death, or the end of the study was 45 months and the IQR was 15–99 months; the mean was 62.9 months, and the SD was 57 months.
Table 1.
Patient Demographic and Surgical Characteristics of 478 Wrists Undergoing 4-Corner Arthrodesis
| Characteristics | N§ (%) |
|---|---|
| Age at exposure, y, mean (SD) | 56.8 (11.6) |
| Body mass index,∗ kg/m2, mean (SD) | 29.3 (5.2) |
| Race | |
| White | 351 (73) |
| Non-White | 127 (27) |
| Sex | |
| Male | 471 (99) |
| Female | 7 (1) |
| Positive smoking history | |
| Yes | 152 (32) |
| No | 326 (68) |
| Surgical technique | |
| Screws | 154 (32) |
| Plate | 172 (36) |
| Kirschner wires | 134 (28) |
| Staples | 18 (4) |
| Underwent PIN neurectomy | |
| Yes | 191 (40) |
| No | 287 (60) |
| Bone graft used | |
| Yes† | 400 (84) |
| No | 78 (16) |
| SLAC | 381 (80) |
| SNAC | 97 (20) |
| SLAC/SNAC stage‡ | |
| Stages I and II | 259 (54) |
| Stage III | 219 (46) |
For body mass index, 12 wrists were missing these data.
Includes both autograft and allograft.
Only 2 wrists with stage I SLAC/SNAC underwent FCA; hence, stages I and II were combined.
Unless unit otherwise specified, N = number of wrists of total 478 wrists undergoing FCA.
Reoperation
Seventy-five (16%) wrists underwent an unplanned secondary operation following index FCA. Of these, implant removal was the most common reoperation performed, with 39 (8.2%) wrists requiring unplanned removal. An additional 42 (8.8%) wrists underwent planned or routine Kirschner wire removal after surgery. A TWA was performed in 21 (4.4%) wrists, and revision FCA was performed in 8 (1.7%) wrists. Figure 1 details the frequency and type of secondary surgery performed in patients following their index FCA. One additional patient underwent TWA after first undergoing removal of the hardware, yielding a total of 4.6% of wrists converting to a TWA. The average time from the initial FCA to any secondary operation was 17.6 months (SD, 25.9 months; median, 8; IQR, 4–17 months, 95% confidence interval [CI], 11.6–23.6) in the 75 reoperations performed. The average time from FCA to TWA was 33.2 months (SD, 37.5 months; IQR, 12–33 months; 95% CI, 16.6–49.8). By 24 months, a majority (64%) of the 22 wrists had converted to TWA.
Figure 1.
Reoperation after FCA in 478 wrists represented as a percentage of total reoperation procedures.
Risk factors for reoperation
Multivariable cox regression demonstrated that a positive smoking history increased the risk of reoperation with an HR of 1.80 (95% CI, 1.13–2.87). However, no statistically significant differences in the risk of reoperation were found with respect to race, the number of comorbidities (HCUP CCS count), wrist arthritis pattern (SLAC vs SNAC), stage (I and II vs III), implant type, or performance of PIN neurectomy. Comparing various fixation methods (eg, Kirschner wires vs plate, staple vs screw), there was no increased reoperation for one method of surgical fixation over another (Table 2). The mean age of wrists not undergoing reoperation was 57.5 years (SD, 11.5 years) versus 52.6 years (SD, 11.2 years) in those undergoing reoperations. The incidence of reoperation by the 10-year age categories with the rates and standard error of the mean for unplanned reoperation and TWA are shown in Figure 2.
Table 2.
Multivariable Cox Regression Analysis Hazards Ratios for 478 Wrists Undergoing 4-Corner Arthrodesis
| Variable | HR (95% CI) | P Value |
|---|---|---|
| Age∗ | 0.98 (0.96–1.0) | .056 |
| Race, White vs Non-White | 1.46 (0.83–2.57) | .19 |
| Smoking status, yes vs no | 1.80 (1.13–2.87) | .014 |
| Total number of distinct HCUP CCS counts† | 1.05 (0.93–1.18) | .45 |
| Surgical technique | ||
| Staple vs screw | 0.54 (0.7–4.07) | .55 |
| Plate vs screw | 0.7 (0.38–1.29) | .25 |
| Staple vs plate | 0.76 (0.10–5.76) | .79 |
| Kirschner wire vs screw | 1.21 (0.68–2.15) | .51 |
| Kirschner wire vs staple | 2.26 (0.30–17.12) | .43 |
| Kirschner wire vs plate | 1.73 (0.96–3.10) | .07 |
| Use of bone graft, yes vs no | 0.6 (0.3–1.03) | .06 |
| Underwent PIN neurectomy, yes vs no | 0.9 (0.5–1.45) | .6 |
| Wrist arthritis pattern, SNAC vs SLAC | 1.0 (0.5–1.9) | .98 |
| SLAC/SNAC stages, Stage I/II vs stage III | 1.6 (0.97–2.58) | .07 |
Compares the effect of age in patients who underwent a secondary procedure with those who did not.
CCS. Relevant comorbidities were selected using ICD codes and then grouped on the basis of HCUP single-level CCS.5
Figure 2.
Incidence of unplanned reoperation by age; TWA following FCA is represented per 100-person years.
Discussion
The national Veterans Health Affairs Corporate database was used to retrospectively review patients undergoing FCA for SLAC/SNAC arthritis over a 24-year period in the United States. This study found an unplanned reoperation rate of 16% at a mean follow-up of 63 months. The most frequently performed unplanned secondary surgeries were implant removal (8.2%) and TWA (4.6%). Positive smoking history was an independent predictor of increased risk of reoperation. Comorbidity burden, fixation method, neurectomy status, and bone graft use did not increase the risk of reoperation in our analyses; however, our study may have been underpowered.
The FCA is a classic, motion-preserving surgery used to treat ailments of the wrist. Despite good pain relief and clinical outcomes for SLAC/SNAC arthritis, FCA confers the risk of complications, given its reliance on union and implant fixation.2,14 The most notable are complications requiring an unplanned return to the operating room, typically due to pain, hardware issues, or nonunion.12 Reoperation rates and sample sizes following FCA in the literature are variable (0% to 35%), making it difficult to draw conclusions.1,9,10,12, 13, 14, 15,18,19 Several studies show complications similar to our study, with reoperation rates typically less than 20% and the risk of TWA at or approximately 5%. In a large systematic review comparing motion-preserving salvage surgery, Mulford et al1 found a rate of conversion to TWA of 2.9% in 1,175 patients, slightly lower than ours of 4.6%. Kay et al18 used a database and CPT coding for intercarpal arthrodesis and found a reoperation rate of 4.2%, with 2.7% of the 5,047 patients requiring TWA.18 Another large database study demonstrated a reoperation rate of 19% in 2,083 patients undergoing a partial wrist arthrodesis, similar to our rate (16%).20 The studies conducted by Kay et al18 and Rahgozar et al20 used CPT codes for database analysis of FCA (CPT codes 25820 and 25825). These CPT codes correspond to “intercarpal fusions” and “partial wrist fusions” and likely capture patients undergoing other forms of intercarpal arthrodesis, such as a scaphotrapeziotrapezoid arthrodesis, compromising conclusions for FCA alone. The current study was a database study combined with a manual chart review, in which 732 of the original 1,284 patients identified by a CPT search were excluded after the chart review.
Worth noting are the 42 (8.8%) wrists that had “planned” Kirschner wire removal, 19 of which were performed in the operating room and were not included in the analysis as unplanned reoperations. When combined with the non–Kirschner wire wrists, the hardware removal rate doubled (17%). Inevitably, these patients may experience anxiety and discomfort with Kirschner wire removal.
Surgeons may augment the surgical technique with various forms of bone graft or configurations of Kirschner wires, screws, or staples. Studies have evaluated the differences in the complication rates for fixation methods investigating plates versus traditional techniques (Kirschner wires, staples, screws), finding mixed complication profiles.10,21, 22, 23, 24 Comparing fixation methods, our study found no significant difference in reoperation. The comparative data in this arena are limited by small sample sizes. In light of no apparent differences in reoperation, the costs between fixation methods should be considered by surgeons.25
Considering the performance of neurectomy, a retrospective review of 266 patients undergoing motion-preserving procedures demonstrated significantly decreased rates of TWA with the performance of PIN and/or anterior interosseous nerve neurectomy, whereas a different study of 51 young patients undergoing FCA found no difference at long-term follow-up.8,16 Our study demonstrated no change in the rates of conversion to TWA based on PIN neurectomy status. However, our study may have been underpowered to evaluate that specific question in our models.
We found a significantly increased risk of reoperation in patients with a positive smoking history. This finding is consistent with previous literature demonstrating that smoking increases the likelihood of delayed union and nonunion.26 Van Hernen et al16 demonstrated an increased risk of conversion to TWA in patients who were smokers (odds ratio, 4.9; 95% CI, 1.8–13.5). In a different study with 11-year follow-up, positive smoking history also increased the risk of complications, particularly nonunion.8 With respect to age, the current study shows that the incidence of overall unplanned reoperation remains higher among younger patients aged less than 40 years (incidence ratio of 2.2 per 100-person years) than among patients aged more than 60 years (incidence ratio of 0 per 100-person years). This was true for conversion to wrist arthrodesis as well. This trend is similar to that in another large study in which higher rates of TWA were noted in younger patients (aged 45–54 years).20 It is worth noting that the current study did not possess sufficient clinical documentation to quantify the extent of smoking, which could have changed our results.
Finally, our study found that comorbidities and wrist arthritis patterns had no significant effect on reoperation. Recent large database studies have not evaluated comorbidities or the stage of arthritis as a risk factor for reoperation.18,20 One smaller study found that a history of diabetes mellitus did not increase the risk of reoperation.16 In terms of the arthritis stage, large studies evaluating the effect of the preoperative SLAC/SNAC arthritis stage on the rate of reoperation are lacking. The current study found no significant increased risk of reoperation in early stage (I and II) compared with later stage (III) arthritis.
The current study has several limitations. First, it is retrospective and associated with limitations inherent in the design. With respect to follow-up, we were able to capture operations at outside hospitals that were paid for by the VA but not those paid for by other insurance. Operative reports for revision surgery and/or complications completed outside the VA were unable to be reviewed. This could have affected rates of unplanned reoperation, given veteran use of other forms of insurance and health systems.27 In addition, a majority of the patients in this study were men, potentially limiting broader application. Our follow-up was shorter than that noted in some studies, although many studies have previously shown that a majority of reoperations tend to occur within the first 2–3 years after the initial FCA.9,14,19 Ultimately, given the size of this study and the number of events, our study may be underpowered to detect the true significance (statistical and/or clinical) of some demographic and surgical variables as risk factors for failure.
Despite these limitations, this study has important strengths. The greatest strength is the large cohort of patients analyzed from a national database with an accompanying manual chart review. The FCA is a dependable procedure with good functional and clinical outcomes.9,12,14 We demonstrated a 16% unplanned reoperation rate and that positive smoking history significantly increased the risk of reoperation. These data assist surgeons with preoperative patient counseling.
Acknowledgments
The authors acknowledge Salt Lake City VA COIN and VERITAS for partially funding the statistical analysis for this work.
Footnotes
Declaration of interests: B.N.G. received a fellowship education grant during her fellowship year from Arthrex. No medical device companies were specifically mentioned in this manuscript. No benefits in any form have been received or will be received by the other authors related directly or indirectly to the subject of this article.
Supplementary Data
References
- 1.Mulford J.S., Ceulemans L.J., Nam D., Axelrod T.S. Proximal row carpectomy vs four corner fusion for scapholunate (Slac) or scaphoid nonunion advanced collapse (Snac) wrists: a systematic review of outcomes. J Hand Surg Eur Vol. 2009;34(2):256–263. doi: 10.1177/1753193408100954. [DOI] [PubMed] [Google Scholar]
- 2.Ashmead D., Watson H.K., Damon C., Herber S., Paly W. Scapholunate advanced collapse wrist salvage. J Hand Surg Am. 1994;19(5):741–750. doi: 10.1016/0363-5023(94)90177-5. [DOI] [PubMed] [Google Scholar]
- 3.Shin A.Y. Four-corner arthrodesis. J Am Soc Surg Hand. 2001;1(2):93–111. [Google Scholar]
- 4.Watson H.K. Limited wrist arthrodesis. Clin Orthop Relat Res. 1980;149:126–136. [PubMed] [Google Scholar]
- 5.Watson H.K., Ballet F.L. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9(3):358–365. doi: 10.1016/s0363-5023(84)80223-3. [DOI] [PubMed] [Google Scholar]
- 6.Dacho A.K., Baumeister S., Germann G., Sauerbier M. Comparison of proximal row carpectomy and midcarpal arthrodesis for the treatment of scaphoid nonunion advanced collapse (SNAC-wrist) and scapholunate advanced collapse (SLAC-wrist) in stage II. J Plast Reconstr Aesthet Surg. 2008;61(10):1210–1218. doi: 10.1016/j.bjps.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Garcia B.N., Lu C.C., Stephens A.R., et al. Risk of total wrist arthrodesis or reoperation following 4-corner arthrodesis or proximal row carpectomy for stage-II SLAC/SNAC arthritis: a propensity score analysis of 502 wrists. J Bone Joint Surg Am. 2020;102(12):1050–1058. doi: 10.2106/JBJS.19.00965. [DOI] [PubMed] [Google Scholar]
- 8.Wagner E.R., Werthel J.D., Elhassan B.T., Moran S.L. Proximal row carpectomy and 4-corner arthrodesis in patients younger than age 45 years. J Hand Surg Am. 2017;42(6):428–435. doi: 10.1016/j.jhsa.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 9.Bain G.I., Watts A.C. The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg Am. 2010;35(5):719–725. doi: 10.1016/j.jhsa.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 10.Chung K.C., Watt A.J., Kotsis S.V. A prospective outcomes study of four-corner wrist arthrodesis using a circular limited wrist fusion plate for stage II scapholunate advanced collapse wrist deformity. Plast Reconstr Surg. 2006;118(2):433–442. doi: 10.1097/01.prs.0000227737.90007.5d. [DOI] [PubMed] [Google Scholar]
- 11.Mavrogenis A.F., Flevas D.A., Raptis K., et al. Four-corner fusion of the wrist: clinical and radiographic outcome of 31 patients. Eur J Orthop Surg Traumatol. 2016;26(8):859–866. doi: 10.1007/s00590-016-1824-5. [DOI] [PubMed] [Google Scholar]
- 12.Saltzman B.M., Frank J.M., Slikker W., Fernandez J.J., Cohen M.S., Wysocki R.W. Clinical outcomes of proximal row carpectomy versus four-corner arthrodesis for post-traumatic wrist arthropathy: a systematic review. J Hand Surg Eur Vol. 2015;40(5):450–457. doi: 10.1177/1753193414554359. [DOI] [PubMed] [Google Scholar]
- 13.Tomaino M.M., Miller R.J., Cole I., Burton R.I. Scapholunate advanced collapse wrist: proximal row carpectomy or limited wrist arthrodesis with scaphoid excision? J Hand Surg Am. 1994;19(1):134–142. doi: 10.1016/0363-5023(94)90237-2. [DOI] [PubMed] [Google Scholar]
- 14.Trail I.A., Murali R., Stanley J.K., et al. The long-term outcome of four-corner fusion. J Wrist Surg. 2015;4(2):128–133. doi: 10.1055/s-0035-1549277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wyrick J.D. Proximal row carpectomy and intercarpal arthrodesis for the management of wrist arthritis. J Am Acad Orthop Surg. 2003;11(4):277–281. doi: 10.5435/00124635-200307000-00007. [DOI] [PubMed] [Google Scholar]
- 16.van Hernen J.J., Lans J., Garg R., Eberlin K.R., Chen N.C. Factors associated with reoperation and conversion to wrist fusion after proximal row carpectomy or 4-corner arthrodesis. J Hand Surg Am. 2020;45(2):85–94.e2. doi: 10.1016/j.jhsa.2019.10.023. [DOI] [PubMed] [Google Scholar]
- 17.Healthcare Cost and Utilization Project. Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality. HCUP Clinical Classifications Software (CCS) https://www.hcup-us.ahrq.gov/tools_software.jsp [PubMed]
- 18.Kay H.F., Kang H.P., Alluri R., Azad A., Ghiassi A. Proximal row carpectomy versus 4-corner fusion: incidence, conversion to fusion, and cost. J Hand Surg Am. 2020;45(5):427–432. doi: 10.1016/j.jhsa.2019.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Williams J.B., Weiner H., Tyser A.R. Long-term outcome and secondary operations after proximal row carpectomy or four-corner arthrodesis. J Wrist Surg. 2018;7(1):51–56. doi: 10.1055/s-0037-1604395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rahgozar P., Zhong L., Chung K.C. A comparative analysis of resource utilization between proximal row carpectomy and partial wrist fusion: a population study. J Hand Surg Am. 2017;42(10):773–780. doi: 10.1016/j.jhsa.2017.07.032. [DOI] [PubMed] [Google Scholar]
- 21.Kiefhaber T.R. Management of scapholunate advanced collapse pattern of degenerative arthritis of the wrist. J Hand Surg Am. 2009;34(8):1527–1530. doi: 10.1016/j.jhsa.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 22.Merrell G.A., McDermott E.M., Weiss A.P.C. Four-corner arthrodesis using a circular plate and distal radius bone grafting: a consecutive case series. J Hand Surg Am. 2008;33(5):635–642. doi: 10.1016/j.jhsa.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 23.Skie M.C., Gove N., Ciocanel D.E., Smith H. Management of non-united four-corner fusions. Hand (N Y) 2007;2(1):34–38. doi: 10.1007/s11552-007-9021-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vance M.C., Hernandez J.D., DiDonna M.L., Stern P.J. Complications and outcome of four-corner arthrodesis: circular plate fixation versus traditional techniques. J Hand Surg Am. 2005;30(6):1122–1127. doi: 10.1016/j.jhsa.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Kazmers N.H., Stephens A.R., Presson A.P., Xu Y., Feller R.J., Tyser A.R. Comparison of direct surgical costs for proximal row carpectomy and four-corner arthrodesis. J Wrist Surg. 2019;8(1):66–71. doi: 10.1055/s-0038-1675791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pearson R.G., Clement R.G.E., Edwards K.L., Scammell B.E. Do smokers have greater risk of delayed and non-union after fracture, osteotomy and arthrodesis? A systematic review with meta-analysis. BMJ Open. 2016;6(11) doi: 10.1136/bmjopen-2015-010303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hynes D.M., Koelling K., Stroupe K., et al. Veterans’ access to and use of Medicare and Veterans Affairs health care. Med Care. 2007;45(3):214–223. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.