Abstract
Flexor carpi radialis tendinitis is a condition that almost exclusively affects the distal aspect of the tendon where it lies in a tight fibro-osseous tunnel. Tendinitis of the proximal aspect of the tendon at its myotendinous junction is extremely rare. Herein, we present a single case of calcific tendinitis of the flexor carpi radialis tendon at its myotendinous junction in a throwing athlete. Diagnostic challenges and treatments are discussed.
Key words: Athlete, Calcific tendinitis, FCR, Flexor carpi radialis, Injury
Flexor carpi radialis (FCR) tendinitis is a condition that mostly affects the distal aspect of the tendon where it lies in a tight fibro-osseous tunnel and is vulnerable to primary stenosing tenosynovitis.1 However, tendinitis of the proximal aspect of the tendon at its myotendinous junction is extremely rare. Herein, we present the case of calcific tendinitis of the FCR tendon at its myotendinous junction in a throwing athlete. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Case Report
A 24-year-old right-handed dominant woman presented with chronic pain over the volar aspect of the right forearm. The patient was a former collegiate track and field athlete on scholarship for javelin, hammer, and discus throwing. Two years prior, she recalled a single javelin throw during which she felt a sudden pulling sensation in her right forearm associated with pain that radiated down the radial aspect of the volar forearm to the wrist. Her symptoms gradually improved with activity modification, nonsteroidal anti-inflammatory medications, and therapy; however, she never returned to her preinjury level. On presentation, she complained of an indentation in the proximal aspect of her volar forearm as well as pain that radiated down the forearm when attempting a grip and resisted wrist flexion.
Physical examination revealed a tender 1.5 × 1.5–cm palpable defect on the proximal aspect of the volar forearm that moved proximally and distally with wrist flexion and extension (Video 1, available online on the Journal’s website at www.jhsgo.org). Active wrist and finger range of motion was symmetric to the contralateral side. Grip strength was 42 kgf bilaterally. Forearm radiographs revealed a 4.3-cm region of calcification within the volar radial soft tissues that was approximately one-third of the length down the forearm (Fig. 1). A point-of-care ultrasound scan revealed partial disruption of the FCR at its myotendinous junction, mild tendon hyperemia, and hyperechoic lesion. Pressure over the affected area reproduced her pain during the examination. The FCR tendon and muscle belly proximal and distal to the site of interest were unremarkable (Fig. 2). Magnetic resonance imaging demonstrated a lesion consistent with calcification measuring 4.3 × 0.9 × 0.6 cm within the FCR myotendinous junction that was distending the superficial fascia and extending into the thinned subcutaneous tissues (Fig. 3). Her basic metabolic panel, complete blood cell count, and endocrine work-up were within the normal limits.
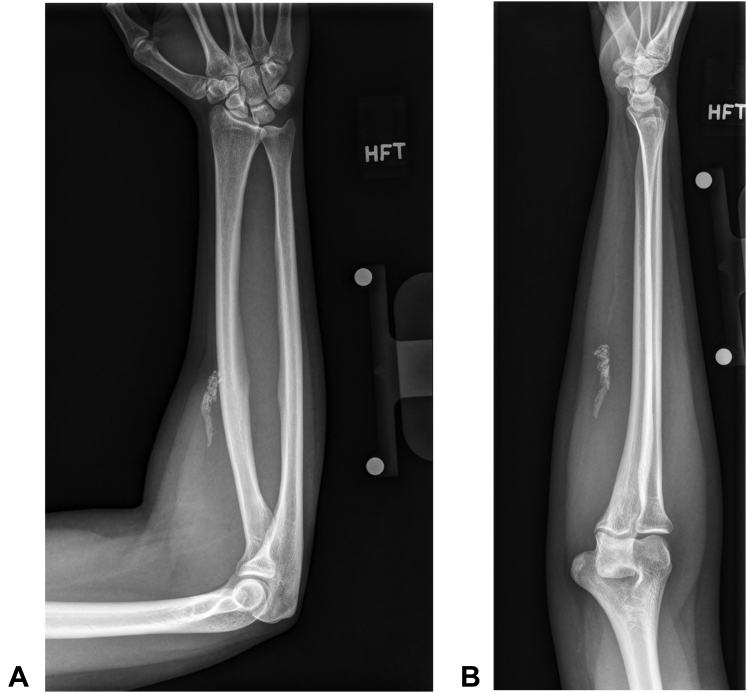
Figure 1.
A Anteroposterior and B lateral plain forearm radiographs showing the details of the calcified tendon.
Figure 2.
A Point-of-care ultrasound imaging taken in the short axis revealed intact muscle belly proximally. B and C Partial tear and calcification at the myotendinous junction. D Intact tendon distally. Dashed line outlines the FCR myotendinous junction.
Figure 3.
Noncontrast T2 weighted magnetic resonance imaging showing calcification about the proximal aspect of the FCR tendon (arrows). A Axial view, B Sagittal view, C Coronal view.
Owing to patient’s strong desire to reduce pain and improve function in the context of failed conservative management, the patient was indicated for partial or complete excision of the calcified FCR tendon. However, we recommended against primary repair of the tendon.
Surgical excision was performed under regional anesthesia with the use of an arm tourniquet. A longitudinal incision was made that was centered over the defect (Fig. 4). Exploration of the proximal FCR revealed a portion of the tendon that was still in continuity. This remnant was preserved during meticulous dissection of the calcific mass off the underlying scar bed (Figure 5, Figure 6). Histology confirmed the presence of chronic inflammation and heterotopic calcification within the tendinous tissue. After surgery, the wrist was placed in an orthosis in the neutral position for 2 weeks, at which point the patient was transitioned to a removable orthosis for an additional 3 weeks. Range of motion exercises and gradual return to activity was started 5 weeks after surgery. At 6 months from surgery, the patient reported complete resolution of her painful symptoms. Active wrist and hand range of motion and grip strength also remained comparable to the contralateral side.
Figure 4.
Longitudinal incision of the mass revealed calcified tendon at the FCR myotendinous junction.
Figure 5.
Dissected tendon from the FCR myotendinous junction. Remaining slip of the tendon is visible in the wound bed.
Figure 6.
Macroscopic picture of the excised calcified tendon. The units of the reference scale are in centimeters.
Discussion
Calcific tendinitis is usually a self-limited, inflammatory condition characterized by the deposition of amorphous calcium phosphate and calcium hydroxyapatite crystals. It usually progresses through the following 4 distinct stages: (1) formative, (2) resting, (3) resorptive, and (4) postcalcific.2 Although the precise etiology remains unclear, it has been suggested that deposits may form secondary to decreased oxygen tension, fibrocartilaginous metaplasia, and secondary mineralization.3 Rotator cuff tendons are most commonly affected; however, involvement of the gluteus maximus, rectus femoris, flexor carpi ulnaris, and pronator quadratus has also been described. Furthermore, disease severity has been associated with endocrinopathies.3
The anatomy of the distal FCR tendon predisposes it to stenosing tenosynovitis. However, the superficial location and bed of loose areolar tissue enveloping the proximal tendon at its myotendinous junction make the pathology in this region extremely rare. Tendinitis of the proximal FCR, with or without calcification, has not been reported in literature.
The throwing athlete is susceptible to a variety of pathologies that are unique to their craft, such as internal impingement of the shoulder, superior labra tears, glenohumeral internal rotation deficit, scapular dyskinesis, nerve or vascular entrapments, spiral fractures of the humerus, elbow ulnar collateral ligament injuries, flexor pronator mass injuries, medial epicondylitis or apophysitis, olecranon stress fractures, and ulnar neuritis.4 Although FCR injuries in athletes are rare, they have been previously described.5 However, even with direct trauma to the muscle or myotendinous junction, tendinitis or rupture still manifests distally within the fibro-osseous tunnel.5 We hypothesize that our patient had an acute partial tear of the proximal FCR tendon during the single symptomatic javelin throw that she recalled. Over time, continued throwing likely resulted in chronic tendinitis, calcification, and scarring to the overlying skin at the myotendinous junction. Another possible explanation for her pathology is chronic overuse. Although the patient recalled a traumatic event that triggered her symptoms and sought evaluation, no imaging was pursued at that time. Finally, an injury to the overlying fascia rather than to the FCR tendon may have potentially triggered chronic inflammation. However, this seems less likely, given the imaging findings of a partial tear, hyperemia, and deposition were limited to the myotendinous junction.
The diagnosis of proximal FCR tendinitis at the myotendinous junction may be challenging given its rarity. Our patient presented with a tender mass that was adherent to the overlying skin causing indentation. The lesion moved with wrist flexion and extension and was more painful with resisted wrist flexion. We were confident in the quality of the imaging study and the interpretation by an experienced musculoskeletal radiologist in differentiating calcific tendinitis from heterotopic ossification, dystrophic calcification, malignancies, and other pathologies. Laboratory studies were not required to make a diagnosis. However, patients with endocrine diseases are less likely to improve with conservative treatment and such studies may be of some prognostic value.6 In our patient, they were all within normal limits.
The imaging characteristics of calcific tendinitis are quite distinct. Plain radiographs may show a region of homogenous calcifications. As described by Gärtner and Heyer,7 dense calcifications with well-defined borders can be seen in the formative phase. In the resting phase, these borders become indefinite. Finally, in the resorptive phase, calcifications become translucent and borders become indistinct.
Ultrasonography may also prove helpful, and in experienced hands is more sensitive than plain radiographs.8 In the resting phase, deposits appear hyperechoic and arc shaped, although they appear more fragmented, cystic, and nodular in the resolving phase. Increased vascularity around deposits can also be seen in the resolving phase.
Finally, magnetic resonance imaging studies may be diagnostic.8 Calcifications typically appear as low signal focal areas on all pulse sequences within the tendon. They lack the well-defined shape and hyperintense core (on T1 weighted images) of heterotopic ossification. If edema is present, as seen in the resorptive phase of calcific tendinitis, increased signal intensity around the deposits may be present on T2-weighted sequences.
Most published studies focus on calcific tendinitis of the rotator cuff. Nonsurgical management is the first line of treatment and includes analgesics, nonsteroidal anti-inflammatory drugs, corticosteroid injections, physical therapy, ultrasound-guided percutaneous irrigation, and extracorporeal shock wave therapy.8 However, a prospective study involving 420 patients with chronic calcific tendinitis of the shoulder found that 27% had persistent symptoms after conservative treatment.6 When conservative measures fail to relieve symptoms, surgical excision should be considered.
Prior to presentation, our patient had trialed an orthosis, activity modification, therapy, and oral nonsteroidal anti-inflammatory drugs. We did not attempt a corticosteroid injection as the patient had dense calcifications adherent to the overlying skin and thin subcutaneous tissues. Therefore, we felt that she had exhausted the conservative measures. Partial tendon excision was performed with complete resolution of symptoms. Prior to surgery, complete tendon excision was also discussed as a surgical alternative. Although complete loss of FCR function has not been shown to lead to substantial wrist motion deficits in the general population, we were hesitant to remove the tendon in its entirety in a high performing athlete.9 Finally, calcifications can recur. Wittenberg et al10 reported recurrence rate of 18% after surgical excision of rotator cuff calcific deposits. This risk was discussed with the patient prior to surgery.
In summary, FCR tendinitis is a condition that almost exclusively affects the distal aspect of the tendon where it lies in a tight fibro-osseous tunnel. Tendinitis of the proximal aspect of the tendon at its myotendinous junction is extremely rare. This case report presents the case of calcific tendinitis of the FCR tendon at its myotendinous junction in a throwing athlete who failed conservative therapy and was successfully treated with partial excision of the tendon.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
Supplementary Data
Preoperative evaluation of the patient.
References
- 1.Bishop A.T., Gabel G., Carmichael S.W. Flexor carpi radialis tendinitis. Part I: operative anatomy. J Bone Joint Surg Am. 1994;76(7):1009–1014. doi: 10.2106/00004623-199407000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Uhthoff H.K., Loehr J.W. Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis, and management. J Am Acad Orthop Surg. 1997;5(4):183–191. doi: 10.5435/00124635-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Iyengar K.P., Yusta-Zato J.A., Botchu R. Calcific tendinopathy of the pronator quadratus muscle: a rare site and cause of ulnar sided wrist pain. J Clin Orthop Trauma. 2022;32 doi: 10.1016/j.jcot.2022.101968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wo S., Mulcahy H., Richardson M.L., et al. Pathologies of the shoulder and elbow affecting the overhead throwing athlete. Skeletal Radiol. 2017;46(7):873–888. doi: 10.1007/s00256-017-2627-4. [DOI] [PubMed] [Google Scholar]
- 5.Kanevsky J., Zammit D., Brutus J.P. Rupture of the flexor carpi radialis tendon secondary to trauma: case report and literature review. Plast Aesthet Res. 2015;2:138–139. [Google Scholar]
- 6.Ogon P., Suedkamp N.P., Jaeger M., Izadpanah K., Koestler W., Maier D. Prognostic factors in nonoperative therapy for chronic symptomatic calcific tendinitis of the shoulder. Arthritis Rheum. 2009;60(10):2978–2984. doi: 10.1002/art.24845. [DOI] [PubMed] [Google Scholar]
- 7.Gärtner J., Heyer A. Calcific tendinitis of the shoulder. Orthopade. 1995;24(3):284–302. [PubMed] [Google Scholar]
- 8.Merolla G., Singh S., Paladini P., Porcellini G. Calcific tendinitis of the rotator cuff: state of the art in diagnosis and treatment. J Orthop Traumatol. 2016;17(1):7–14. doi: 10.1007/s10195-015-0367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tomaino M.M., Coleman K. Use of the entire width of the flexor carpi radialis tendon for the ligament reconstruction tendon interposition arthroplasty does not impair wrist function. Am J Orthop (Belle Mead NJ) 2000;29(4):283–284. [PubMed] [Google Scholar]
- 10.Wittenberg R.H., Rubenthaler F., Wölk T., Ludwig J., Willburger R.E., Steffen R. Surgical or conservative treatment for chronic rotator cuff calcifying tendinitis–a matched-pair analysis of 100 patients. Arch Orthop Trauma Surg. 2001;121(1–2):56–59. doi: 10.1007/s004020000195. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preoperative evaluation of the patient.