Abstract
Background
Molluscum contagiosum is often characterized by persistent lesions and bothersome symptomology. What patients with molluscum contagiosum and/or caregivers consider to be meaningful measures of therapeutic success is unknown.
Objective
We aimed to collect patient experience data and assess Global Impression of Change from patients and/or caregivers participating in a large phase III molluscum contagiosum interventional trial.
Methods
The Berdazimer Sodium In Molluscum Patients with LEsions (B-SIMPLE4) phase III study enrolled 891 patients with molluscum contagiosum. Patients were randomly assigned to berdazimer gel, 10.3% or vehicle gel applied once daily for 12 weeks. Assessments of participant and investigator perceptions of complete lesion clearance were collected at weeks 12 and 24 along with Global Impression of Change scores from 1 (very much improved) to 7 (very much worse). A subset of 30 B-SIMPLE4 patients participated in the patient/caregiver experience exit interview to evaluate bothersome signs and symptoms.
Results
At week 12, among participants with a ≥ 75% molluscum contagiosum lesion count reduction from baseline (as assessed by investigators), 99% (373/376) reported improvement. Perceptions of complete clearance at week 12 were nearly 40% for both participant-reported and investigator-reported Global Impression of Change in berdazimer group vs 20% in the vehicle group: 82% (322/392) of participants in the berdazimer group and 60% (237/394) in the vehicle group reported their molluscum contagiosum lesions were either very much improved or much improved at week 12. Similarly, investigators scored 80% (314/393) of berdazimer and 54% (215/396) of vehicle participants as very much improved or much improved. From the exit interview, the mean duration of participant-reported molluscum contagiosum was nearly 2 years. The most frequently reported molluscum contagiosum-related signs and symptoms were itch (n = 20), scarring (n = 18), and pain (n = 13). Visibility and contagiousness of molluscum contagiosum were the most bothersome aspects to participants. The most frequently reported psychosocial impacts were self-consciousness (n = 15) and embarrassment (n = 14). Lesion clearance was an expectation of 28/30 study participants. Overall, 26/30 reported being very satisfied (n = 18) or satisfied (n = 8) with the changes in their disease over the duration of the trial; 23/30 stated that the change in lesion count was meaningful. A mean reduction of 18 lesions (76% decrease) from the baseline lesion count was reported by participants (n = 28). Although 22 of 28 had less than complete lesion clearance, 17 of 22 reported that the reduction in the number of lesions was meaningful.
Conclusions
Molluscum contagiosum lesion reductions, with or without complete clearance, may be considered a therapeutic “success” by the patient/caregiver.
Clinical Trial Registration
NCT04535531 (registered 2 September, 2020).
Key Points
| The most bothersome aspects for patients/caregivers are molluscum contagiosum lesion visibility and contagiousness. |
| Lesion count reductions are meaningful to patients/caregivers, even when complete clearance is not achieved. |
Introduction
Molluscum contagiosum (MC), a common, highly contagious viral skin infection caused by the molluscipoxvirus [1], replicates only in human skin cells and has the unique ability to produce proteins that enable the virus to evade the host’s immune surveillance system [2, 3]. Molluscum contagiosum manifests as clusters of small raised firm bumps on infected skin and is especially common in younger children [4, 5]. Molluscum contagiosum lesions may be widespread, affecting sensitive body areas, causing pain, irritation, and redness, and if scratched, autoinoculation and heightened communicability [1]. Molluscum contagiosum infections may clear without treatment yet can persist for months or years [6]. Indeed, prolonged duration and visibility of MC lesions coupled with the potential to spread the virus can create psychosocial distress and anxiety [5] for both the patient and caregiver.
Currently, there is lack of consensus regarding treatment approaches to MC [7] and there is no US Food and Drug Administration (FDA)-approved prescription medication. Therefore, many healthcare providers take a watch-and-wait strategy with an estimated 74% of patients with MC left untreated [8]. It is unknown what impact the lack of a MC therapeutic intervention has on patient/caregiver physical and/or psychosocial well-being.
Berdazimer gel, 10.3% (SB206) is a novel, topical, nitric oxide-releasing agent under investigation as a first-in-class therapy for the treatment of MC [9–12]. The Berdazimer Sodium In Molluscum Patients with Lesions (B-SIMPLE4) pivotal phase III trial of berdazimer gel, 10.3% (ClinicalTrials.gov identifier: NCT04535531) enrolled the largest-ever cohort of patients with MC in a clinical trial (N = 891) with the results showing favorable efficacy and tolerability [9–12].
Capturing the patient experience and integrating the patient voice in dermatologic clinical trials have been a collaborative effort led by the FDA, patient advocacy groups, and the pharmaceutical industry [13]. Therefore, to better understand patients’ and caregivers’ experiences with the MC disease state and MC therapeutic strategies, patient-experience data (PED), including participant-reported and investigator-reported perception of complete clearance and participant-reported and investigator-reported Global Impression of Change (GIC), were collected in B-SIMPLE4. In addition, a qualitative exit interview was conducted with a subset of B-SIMPLE4 patients and caregivers. The objective of the exit interview was to gather input from patients and caregivers on the most bothersome signs and symptoms of MC, the psychosocial aspects of MC, expectations regarding clinical trial participation, and the meaningfulness of changes in MC lesion count and location, with special attention given to the impact of a reduced lesion count in the absence of complete clearance.
Methods
PED Assessments and Population
Briefly, B-SIMPLE4 was a multicenter, double-blind, vehicle-controlled, parallel-group (1:1) randomized clinical trial of the efficacy and safety of berdazimer gel, 10.3% applied topically once daily for 12 weeks [9]. The study methodology, eligibility criteria, patient disposition, and efficacy and safety results for B-SIMPLE4 have been published [9]. For the PED, B-SIMPLE4 included participant and investigator perceptions of MC lesion clearance at baseline and weeks 12 and 24. These assessments were based on participants’ (including patients and caregivers) and investigators’ perception of lesion clearance rather than a formal lesion count. For the GIC ratings, participants and investigators reported their overall impression of change from baseline in the patient’s overall MC condition at weeks 12 and 24 on a scale from 1 (very much improved) to 7 (very much worse) using a non-validated scale.
Exit Interview Study Design and Population
For the qualitative exit interview, all English-speaking B-SIMPLE4 participants at select sites who had less than complete MC lesion clearance from baseline to their week 12 visit as determined by the investigator were eligible for qualitative exit interviews. The goal was to engage ~ 30 participants (balanced between berdazimer gel, 10.3% and placebo groups), including ~ 20 participants with lesion count reductions that ranged from 75 to < 100% and approximately three to four participants with reductions in each of the following ranges: from 50 to < 75%, 25 to < 50%, and 0 to < 25%. The 60-min qualitative interviews of participants (patients or caregivers were interviewed, depending on patient age) were conducted using an interview guide by one of two RTI Health Solutions staff members via telephone 2–4 weeks after their week 12 visit.
Analyses
PED Analyses
For the PED from B-SIMPLE4, the participant-reported and investigator-reported perceptions of complete lesion clearance and participant-reported and investigator-reported GIC were summarized descriptively.
Exit Interview Analyses
For the exit interview, each semi-structured interview began with a brief overview of the interview process and a few general questions intended to prompt participants to discuss symptoms and impacts of MC. Additionally, patients were asked specifically what their treatment expectations were before entering the clinical trial and what their experiences were during the trial. Caregivers were asked specifically what their treatment expectations were before entering the clinical trial and what their child’s experiences were during the trial. Finally, interview participants were queried about various treatment benefits and outcomes, including any improvements observed, and the importance and meaningfulness of those improvements.
Exit interview data were systematically collected from study participants as field notes captured in Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and audio files. After interviews concluded, all audio files were transcribed verbatim and prepared for qualitative analysis.
The qualitative analysis of exit interviews was facilitated by a coding software (ATLAS.ti 9; Atlas.ti Scientific Software Development GmbH, Berlin, Germany), using a coding framework that was developed and adapted as the analysis progressed and emerging themes were incorporated. Interview results were analyzed using a thematic analysis approach [14]. Using the transcripts and interviewer field notes, dominant trends in each interview were identified and compared across interviews [15] to describe themes and the relative importance of concepts described by interview participants. This analytical process generated themes or patterns in the way interview participants described their observations and experiences.
Results
B-SIMPLE4 PED
Participant-Reported and Investigator-Reported Perception of Lesion Clearance
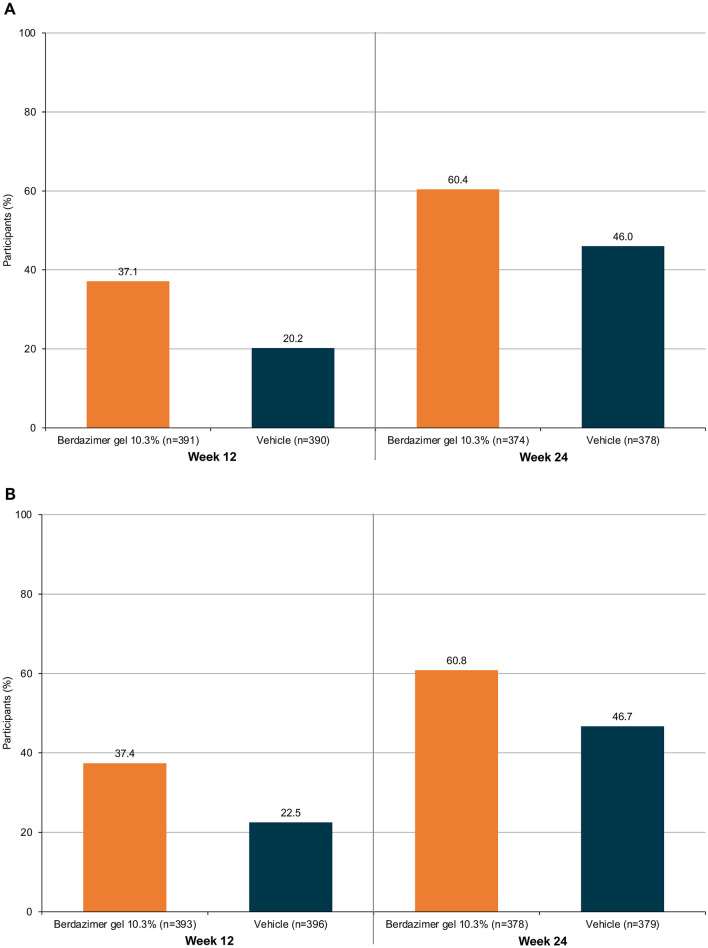
Among all B-SIMPLE4 participants who completed the participant-reported assessment of lesion clearance, complete clearance was reported by 37% (145/391) of the berdazimer group at week 12 and 60% (226/374) at week 24 compared with 20% (79/390) of the vehicle group at week 12 and 46% (174/378) at week 24 (Fig. 1A). This trend was also consistent with investigators’ perception of complete clearance, which was reported for 37% (147/393) of the berdazimer group at week 12 and 61% (230/378) at week 24 compared with 22% (89/396) of the vehicle group at week 12 and 47% (177/379) at week 24 (Fig. 1B).
Fig. 1.
Participant (a) and investigator (b) perceptions of complete lesion clearance
Participant-Reported and Investigator-Reported GIC
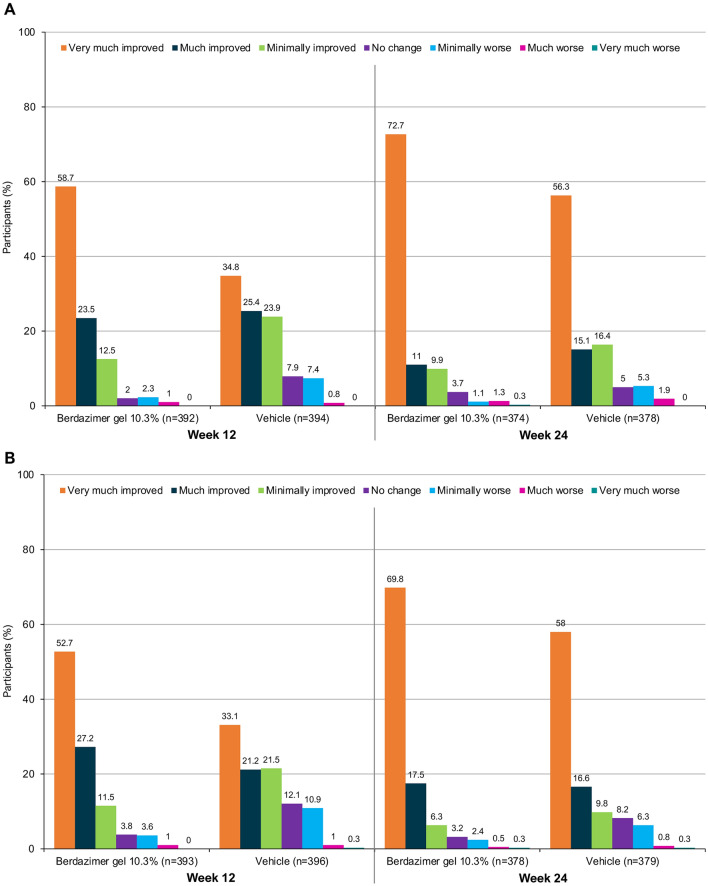
At week 12 of B-SIMPLE4, 82% (322/392) of participants in the berdazimer group and 60% (237/394) in the vehicle group reported their MC lesions were either very much improved or much improved on the GIC, for a difference between groups of 22 percentage points (Fig. 2A). The 35 and 25% of vehicle patients who reported their lesions were very much improved or much improved at week 12, respectively, may reflect the typically self-limiting nature of MC. However, at week 24, there continued to be a difference between groups (12 percentage points) with more berdazimer (84% [313/374]) than vehicle (71% [270/378]) participants reporting their lesions were either very much improved or much improved (Fig. 2A). Results for the investigator-reported GIC were similar (Fig. 2B). For participants with a ≥ 75% reduction in MC lesion count from baseline at week 12, almost all felt improvement regardless of treatment assignment (Table 1).
Fig. 2.
Global Impression of Change over time. a Participant-reported Global Impression of Change and b investigator-reported Global Impression of Change
Table 1.
Participant-reported Global Impression of Change by lesion reduction at week 12
| Efficacy | Vehicle once daily (N = 447) | Berdazimer gel, 10.3% once daily (N = 444) | Total (N = 891) | |||
|---|---|---|---|---|---|---|
| Improvement (n = 331) | No improvement (n = 63) | Improvement (n = 371) | No improvement (n = 21) | Improvement (n = 702) | No improvement (n = 84) | |
| Patients with ≥ 75% reduction from baseline in MC lesion count | 141 | 0 | 232 | 3 | 373 | 3 |
| Patients with ≥ 90% reduction from baseline in MC lesion count | 106 | 0 | 189 | 1 | 295 | 1 |
MC molluscum contagiosum
Exit Interviews
Baseline Demographic and Clinical Characteristics
Qualitative interviews were conducted with 30 English-speaking participants (two patients and 28 caregivers) from 16 US clinical trial sites. Baseline demographic and clinical characteristics are presented in Table 2. Most participants lived in the Southern region of the USA, and all participants were white.
Table 2.
Participant characteristics reported at the time of the interview
| Characteristic | Patients (n = 2) | Caregivers (n = 28) | Total (N = 30) |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 1 (50) | 2 (7.1) | 3 (10) |
| Female | 1 (50) | 26 (92.8) | 27 (90) |
| Age, years | |||
| Mean (range) | 30 (12–48) | 36.9 (27–59) | 36.4 (12–59) |
| Age of caregiver’s child, years | |||
| Mean (range) | NA | 5.6 (2–11) | 5.6 (2–11) |
| Self-reported duration of MC at study entry, months | |||
| Mean (range) | 90 (36–144) | 15.2 (1–48) | 20.2 (1–144) |
| Estimated number of lesions at study entry | |||
| Mean (range) | 14.5 (9–20) | 22.2 (5–67) | 21.7 (5–67) |
| Region, n (%) | |||
| Northeast | 0 | 1 (4) | 1 (3) |
| South | 1 (50) | 18 (64) | 19 (63) |
| Midwest | 0 | 3 (11) | 3 (10) |
| West | 1 (50) | 6 (21) | 7 (23) |
| Race, n (%) | |||
| White | 2 (100) | 28 (100) | 30 (100) |
| Education, n (%) | |||
| High school or less | 1 (50) a | 0 | 1 (3.3) |
| Some college | 1 (50) | 9 (32.1) | 10 (33.3) |
| College | 0 (0) | 11 (39.3) | 11 (36.7) |
| Post college | 0 (0) | 8 (28.6) | 7 (23) |
| Employment status, n (%) | |||
| Not applicable | 1 (50) | 0 | 1 (3.3) |
| Part time | 1 (50) | 5 (17.9) | 6 (20) |
| Full time | 0 (0) | 15 (53.6) | 15 (50) |
| Unemployed | 0 (0) | 8 (28.6) | 8 (26.7) |
MC molluscum contagiosum, NA not applicable
aParticipant was in grade school at the time of the interview
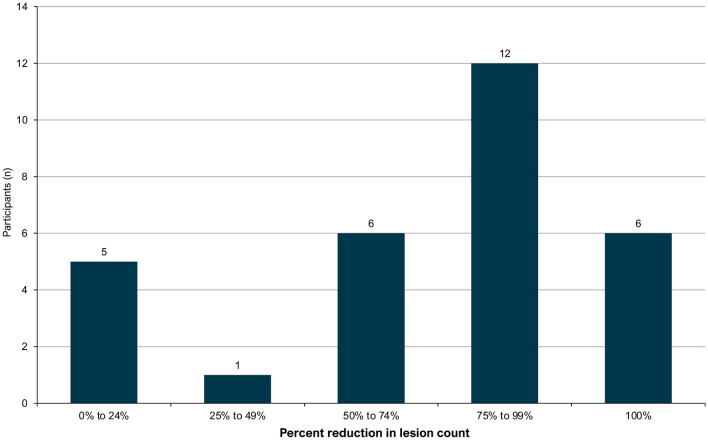
The mean duration of MC at baseline (as reported by participants) was 20.2 months. The mean number of lesions estimated by participants at the time of B-SIMPLE4 study entry was 21.7. The recruitment target for different ranges of lesion reduction at week 12 was generally met (Fig. 3). Participants were also balanced by treatment group, with 15 from the berdazimer gel, 10.3% group, and 15 from the vehicle group interviewed.
Fig. 3.
Participant-reported reduction in lesion count at the time of the interview. One participant in the 0–24% category reported an overall increase in lesion count. Participants were selected for interviews based on the investigator-determined reduction in lesion count, these numbers represent the participant-reported reduction in lesion count
Signs and Symptoms of MC
Participants described their MC lesions as bumps, spots, rashes, and warts. Caregivers frequently reported use of the term “bumps” by their child to describe lesions. Participants also reported various attributes of MC lesions including location, size, number, contagiousness, and visibility.
The most frequently reported MC-related signs and symptoms were itch, scarring, and pain (Table 3). Additionally, some participants spontaneously reported the terms pustules or inflammation, sores or blisters, and bleeding when describing their MC lesions. Participants could distinguish between MC-related signs and symptoms and adverse events associated with study medication.
Table 3.
Signs, symptoms, and characteristics of molluscum contagiosum reported by participants
| Reported sign, symptom, or characteristic | Patients (n = 2) n |
Caregivers (n = 28) n |
Total (N = 30) n (%) |
|---|---|---|---|
| Raised skin (bump, spot, wart) | 2 | 28 | 30 (100.0) |
| Location | 2 | 28 | 30 (100.0) |
| Number | 2 | 27 | 29 (96.7) |
| Size | 1 | 27 | 28 (93.3) |
| Contagiousness | 1 | 20 | 21 (70.0) |
| Itch | 1 | 19 | 20 (66.7) |
| Visibility | 1 | 19 | 20 (66.7) |
| Scarring | 1 | 17 | 18 (60.0) |
| Pain | 1 | 12 | 13 (43.3) |
| Pustules or inflamed a | 1 | 12 | 13 (43.3) |
| Sore or blister a | 1 | 6 | 7 (23.3) |
| Bleeding a | 0 | 1 | 1 (3.3) |
| Looks infected a | 0 | 2 | 2 (6.7) |
aSymptom not probed during interview but spontaneously reported by participants
The two patient participants indicated visibility and contagiousness as the most bothersome aspects of MC (Table 3). Similarly, caregivers most frequently reported visibility and contagiousness as the most bothersome aspect of their child’s MC. Of note, two caregivers reported that nothing about their child’s MC bothered them.
Impacts of MC
The most frequently reported impacts of MC were psychosocial, including self-consciousness, embarrassment, and worrying about others noticing or commenting on lesions (Table 4). Other impacts reported by ≥ 20% of participants included having to avoid certain clothing and physical activity limitations. One participant each reported impact on mood (annoying), social relationships, work, interpersonal relationships, and sleep. Caregiver impacts of MC focused on the time required to apply the study medicine and the time and effort needed to clean household surfaces to prevent viral spread.
Table 4.
Impacts of molluscum contagiosum reported by participants
| Impact | Patients (n = 2) n |
Caregivers (n = 28) n |
Total (N = 30) n (%) |
|---|---|---|---|
| Self-consciousness | 1 | 14 | 15 (50.0) |
| Embarrassment | 2 | 12 | 14 (46.7) |
| Worry about others noticing or commenting | 2 | 8 | 10 (33.3) |
| Avoiding certain clothing (e.g., shorts or bathing suits) | 2 | 6 | 8 (26.7) |
| Physical activities | 1 | 5 | 6 (20.0) |
| Worry about contagiousness | 1 | 1 | 2 (6.7) |
| Teased or treated meanly | 1 | 2 | 3 (10.0) |
| Bath time | 1 | 1 | 2 (6.7) |
| Daily activities | – | 2 | 2 (6.7) |
| Sleep a | – | 1 | 1 (3.3) |
| Interpersonal or social relationships a | 1 | 1 | 2 (6.7) |
| Work a | 1 | – | 1 (3.3) |
aImpact not probed during the interview but spontaneously reported by participants
Clinical Trial Participation Expectations
The two patients and 26 of 28 caregivers reported that lesion clearance was an expectation of study participation before enrolling in B-SIMPLE4. Additionally, two caregivers reported an expectation of preventing MC recurrence. Other reasons caregivers provided for deciding to enroll their children in B-SIMPLE4 were trying something new in hopes of treating their child’s MC and the possibility of a quicker resolution of their child’s MC.
Improvements During the Course of the Clinical Trial
The most frequently reported improvement was a reduction in lesion number, reported by 28 of 30 participants (two patients and 26 caregivers [93%]). Although participants were selected based on less than complete lesion clearance as assessed by the investigator, six (20%) participants reported complete clearance at the time of the interview. The two caregivers who did not report lesion count improvement reported no change in lesion count (n = 1; 3%) or an increase in lesion count (n = 1; 3%). Other reported improvements were a shorter duration of healing (n = 4; 13%), a reduction in lesion size (n = 4; 13%), and less inflammation (n = 2; 7%). Improvements in spreading, redness, itch, and swelling were each reported by one caregiver.
Improvement in Most Bothersome Symptom and Impact
Of the 24 participants who reported a most bothersome sign or symptom, 21 (88%) stated that the sign or symptom had improved during the study. Of the 22 participants who reported a most bothersome impact, 19 (86%) reported that the impact had improved during the study.
Change in Lesion Number
For the 28 participants who reported a reduction in lesions, the average was 18 fewer lesions, which represented a 76% decrease from the baseline lesion count (Table 5). Of these 28 participants, 22 (79%) reported that the decrease represented “many less” lesions and 6 (21%) reported “less” lesions at study end, compared with the baseline lesion count.
Table 5.
Participant-reported change in lesion count since study initiation
| Lesions | Increased (n = 1) | No change (n = 1) | Decreased (n = 28) |
|---|---|---|---|
| Count | |||
| Mean (range) | 30 a (NA) | 0 (NA) | 18 (1-67) |
| Percentage | |||
| Mean (range) | 150% (NA) | 0% (NA) | 76% (11–100%) |
NA not applicable
aParticipant reported 30 additional lesions
Meaningfulness of Change in Lesion Count and Lesion Location
Of 30 participants, 23 (77%) reported a meaningful change in lesion count since study initiation, and 25 (83%) reported a change in lesion location during the study. Of these 25 participants, 14 (56%) reported the change in lesion location had not been as important or as meaningful as the reduction in lesion number, whereas 11 (44%) reported the change in lesion location had been meaningful because of reduced visibility and less irritation or discomfort.
Level of Satisfaction with Any Changes Since Study Initiation
Overall, 26 of 30 participants reported being very satisfied (n = 18; 60%) or satisfied (n = 8; 27%) with any MC lesion changes since study initiation (range of percent improvement in lesion count from baseline as reported by participants at the time of the interview: 23–100%). Of the remaining four participants, three (10%) reported being neither satisfied nor dissatisfied, and one (3%) reported being dissatisfied. Twenty-one caregivers provided a satisfaction rating from their child’s perspective: 17 (57%) said their child was “very satisfied” (n = 12; 40%) or “satisfied” (n = 5; 17%), and four said their child was “neither satisfied nor dissatisfied” (n = 2; 7%) or “dissatisfied” (n = 2; 7%).
Changes in Lesion Count and Location in Participants with Less Than Complete Clearance
Of the 28 participants who reported a lesion count reduction, 22 (79%) reported less than complete clearance. For these 22 participants, the mean lesion count reduction was 14, representing a mean percentage decrease from baseline of 70%. When probed, these participants described the change as “many less” (n = 16; 73%) or “less” (n = 6; 27%) lesions compared with baseline. Of these 22 participants, 17 (77%) reported that the reduction in lesion number was meaningful and 11 (50%) reported that the change in lesion location was meaningful. Consistent with GIC results captured in the full B-SIMPLE4 sample, most of these participants (n = 19; 86%) reported being “very satisfied” (n = 13; 68%) or “satisfied” (n = 6; 32%) with MC lesion changes during the clinical trial. Patient and caregiver quotes grouped by interview topics are shown in Table 6.
Table 6.
Select quotes grouped by interview topic
| Description of molluscum contagiosum |
| “He’d just say that he has little bumps that are his boo-boos, on his leg or on his arm. I would say it’s like little warts all over your skin, and some areas have more than others, but then they also turn into big sores and pustules.” |
| “He just calls them his bumps. It’s kind of warts.” |
| Signs, symptoms, and characteristics |
| Itch |
| “They’re itchy and quite bothersome.” |
| Pain |
| “They also turn into big sores and pustules, and they’re very painful when they get to that point.” |
| Scarring |
| “Yes, we have scarring. They pretty much look like chickenpox scars, which are like a lighter-skin, circular scar.” |
| Location |
| “Before the study he had some all over his eyebrows and around his eyes, and he had them on…a couple near his hands in the study, and then on his legs. He had a lot on his legs, lower extremities.” |
| Size |
| “Most of them were little. Some of them were medium and then some of them were big and huge.” |
| Number |
| “There was probably at least 10 on his face, probably at least 10 more on his legs. I mean, I’d say a good 20 lesions on his body at least.” |
| “Yes. I think on our first visit I counted 67 bumps.” |
| Contagiousness |
| “I personally feel like the contagiousness of it is the most alarming part of it for me. Realizing how contagious they are and I’m giving my kid a hug, consoling my kid. It’s frustrating because you can’t really do much about that.” |
| “It was primarily because he has a sister. They are 20 months apart and they used to bathe together all the time. That was a big thing because they had to stop taking a bath together. And they really enjoyed bathing together and playing in the tub.” |
| “It definitely spread. It was spread through contact. Her largest molluscum were on her left shoulder and upper arms. And they continued to spread to up her arm and started to form on her chin and jaw line on that side.” |
| Visibility and contagiousness as bothersome aspects of MC |
| “The fact that they turn into these sores, and they leave scars. That’s the most bothersome, because every time a molluscum, I guess, bump turned into a sore or turned into a pustule it would leave somewhat of a scar, and it wouldn’t go away quickly.” |
| “I didn’t like it being on her face, because she is in school, and I’m a schoolteacher, and I know how mean kids are. And so, I didn’t want people making fun of her either. And I didn’t want it to keep spreading and not … the spreading them, the contagiousness.” |
| “I feel bad because there was nothing we could do and I know it was bothersome to her, so it always bothered me that it felt like we were doing nothing to make it better. And then just the added complication of trying to remember to not have the kids together, make sure her towels go in the wash after use, and nobody else is using the towels that come from her and trying to stop it from spreading. It took a lot of effort. And then in the end it happened anyway.” |
| “Yes, we avoided going to the lake right before the clinical study, because we were worried they would get infected from the water.” |
| “I wasn’t worried about them being contagious, but my younger brother got molluscum from me. So I would say they were contagious, because he got them.” |
| “The one on the chin I didn’t like because others could see them but the rest of them I didn’t like them because I didn’t like them on my skin.” |
| “The visibility, the location. Just she didn’t like people talking about it.” |
| Self-consciousness/embarrassment/worry |
| “It definitely made her more self-conscious.” |
| “She would tell me that kids would point it out at school and point at it and laugh and say that they didn’t want to play with her: |
| “He would just make comments like, ‘I hate them so bad; they look so gross, I don’t want people to see them, I wish they would just go away,” things like that. And then when we’d go swimming, he’d be like, ‘I don’t want to take off my shirt.’ Just things like that.” |
| “But other than the looks and where it was, and her self-esteem; thinking people are looking at her or talking about her.” |
| “Only the one on my chin [I was embarrassed]. Every time we went out into public.” |
| Clothing choices |
| “Yeah, I’ve had to put him in pants before when his sores were bad instead of shorts.” |
| “We did avoid wearing certain … any clothes that had direct contact, like hard pressure on there because it was rough and they’d become uncomfortable to her because she’d rub them raw if she didn’t have a band-aid.” |
| “Probably would be having to dress differently. That’s unfortunate … well, I mentioned living in [name deleted] and being in the heat of humidity, this is uncomfortable and then you get hot and sweaty and then things start to itch and then guess what? Now you have more itching and you’re trying to keep them covered you’re trying not to expose anyone else but you’re also sweating and dying and it’s not comfortable. It’s not fun. People are looking at you, like you’re weird too because it’s 110 degrees outside and you’re wearing a long sleeve shirt.” |
| Physical activities |
| “There was one time where he didn’t get to go kind of swim with friends because of the sores, because I didn’t want them to spread.” |
| “She plays softball. Running sometimes would … the way that her pants would rub against them because they are up on the top of her thighs. That would be bothersome so it would make her not want to run because that hurt.” |
| Being teased/treated meanly |
| “I think there was a little bit of bullying at school around it.” |
| Clinical trial expectations |
| “I really wanted to see if there was something that would work on it, and his molluscum bumps, because we had gotten a bunch of different ointments and I just didn’t feel like they were … I felt like they were hurting him, because he didn’t like them, he noticed them. I felt like they didn’t work very well, so I just was open to try something else.” |
| “I was thrilled that they had some kind of way to treat her because I’ve never been given an option before.” |
| “She had very large molluscum compared to the size that our son had and they seemed to be spreading at that point. So, I was very much hoping to find a resolution because had tried many of the home remedy types of solutions with my son and my daughter and they were not working so I was extremely excited to find a study to hopefully help her stop the spread. Especially since they were on her face at that point.” |
| “I was hopeful that she would be one of the kids in the study that receives the medication and that it actually helped to clear up the molluscum after we’d been going through it for a year.” |
| “I was hopeful that they would put something on her bumps and that they would magically go away. That they would disappear and that we would be molluscum free.” |
| “Because he wanted them to go away, and we’d already tried something and didn’t work completely. It left him with some scarring, so we thought we could find something else that would maybe work better without the scarring.” |
| “Because it was bothering her quite a bit, it was pretty itchy, it would burn, and she complained about it a lot.” |
| Improvements during the clinical trial |
| “It seemed like it improved when I say that the bumps decreased and disappeared quicker than our previous medicine we were using. There was less of an inflamed time for each bump. Well, I guess the pustule inflammation time was smaller.” |
| “It has lessened because the size of the molluscums shrank pretty quickly, so the smaller that they became, the less areas she had that were irritated, so the less itching she did.” |
| “They’re almost all gone. Visually you can’t really see them, you can still feel where they were but for the most part it’s not noticeable at all.” |
| “I have noticed some like where he’s cleared up in some places like in his neck area, a lot of those have went away. It’s just mostly now confined to just, like I said, his upper torso and his belly area. He has had some that popped up on his arms and those have went away. Some on his knees and went away.” |
| “The ones on her face went away, so I’m happy.” |
| “Yes, since most of his bumps are gone, or pretty much all are gone that we don’t really have a concern of it spreading more on him since there’s none on there.” |
| “They actually did clear up. I think she only has one small area left, one small lesion left. So they almost completely cleared up.” |
| “I want to say yes, that they went away faster, because they would go away within 4 weeks of treatment as opposed to months of them, letting them go away on their own. So, yes, they got treated faster.” |
| “Yeah, she doesn’t itch as much, at least not in those areas anymore. She’s not complaining about the bumps, the itching, the burning and so, yeah, that’s pretty much it.” |
| Improvement in most bothersome sign or symptom |
| “She doesn’t complain of itching at all anymore.” |
| Improvement in most bothersome impact |
| “I felt much better just finding that there was something that we could do and that it worked for him. As a parent you kind of want to be able to fix things.” |
| “I teach Pilates. I’m in fitness. So I want to wear a tank top, I want people to see that Pilates does wonderful things for my triceps but if I’ve got a low hanging armhole in my tank top, that could be an area where I’m going to have some spots. Well, I can wear that cute little tank top now because I’m not worried about having all those spots.” |
| “I feel like that the bumps went away and I didn’t notice the scars. I didn’t even notice where they were as much as I did before with the other ones. So there was less scarring, there was less noticeable marks when they went away.” |
| “I mean, like I said, we didn’t have too many before. We just had a few because of the facial ones, and like I said, the swimming thing. I feel like there were less impacts while we were on the study because of the medicine we were taking. I felt like it was helping.” |
| “Yeah. She’s pretty much back to her normal self, so I don’t really have to worry about anything [worrying about the contagiousness of it, about it spreading, dressing her a certain way] anymore.” |
| Change in number of lesions |
| “I would say many less than at the beginning of the study. Sheer numbers. She had so many the first time we went that we were flipping her from back to belly counting all of them on her legs. And the last visit we went, we were having a hard time figuring out if there were even any that were actually still active. So, it just, like you’re saying, from 10 to 1 small one left.” |
| Meaningfulness of change |
| “The most important improvement is the resolution of the spots with a lack of scarring.” |
| “If I had 1 small one left yeah that’d be fine. Two small ones. Yeah, that’d be fine too.” |
| “It’s been the same location since the beginning. I’ve always had them in that area so I would say the location doesn’t matter to me as much as the number of them.” |
| “Yes. That’s exactly what I wanted. I just wanted to be done with the bumps all over her. They just kept getting worse and worse and immediately it just started clearing up and she’s happy they’re gone and I’m happy because I don’t have to worry about them spreading to everybody else. And that’s it.” |
| “Yeah, extremely important. That way we’re not having to watch our daughter suffering through pain, and just constant itching, and we don’t have to worry about her spreading it to other people either.” |
| “I think the change in the number would be more significant to me. If they … if we treated some and then some others popped up, I wouldn’t see the study drug being a failure.” |
| “At least half. Just because it would, I guess, an overall improvement, I think. Any improvement I guess is good, but that would be a great improvement.” |
| Level of satisfaction |
| “Very satisfied. Because we did see so much improvement with her not just in the physical aspect of it, but the emotional aspect of it too, I guess you could say. And just being able to see her go back to the way she was before everything.” |
| “I’m very satisfied because the visibility and potential scarring was my number one concern, and that concern is now eliminated because the molluscum are gone.” |
| “Very satisfied. Because I went into this just thinking that they would … it would take a while to do anything, any kind of changes and within that first month, so they started disappearing real fast. I didn’t expect it to happen this fast.” |
| “Very satisfied. Because we went from 25 to 30 molluscum bumps, down to practically zero. And so her legs look better, it’s something she won’t be self-conscious about, and it’s an irritant that we don’t have to deal with, at least for the time being.” |
| “I was very satisfied after I saw a change after taking the medication. After starting the medication, it was nice to see that change of them going away, even though sometimes she’d wake up and have more, and then other times wake up and have less. But the fact that they’ve gone down so many, going from so many to so little, I’m very satisfied.” |
|
“I would say satisfied. I think that learning a lot about what this was and kind of how these processes work. I’m hopeful that this is the beginning of the end for them because everyone has said about a year. It’s been about a year.” “I would say neither satisfied nor dissatisfied. I’m just kind of indifferent to the results. I didn’t like…I mean I knew it was a study, it may or may not … there may or may not be results and I’m not sure that they’re less significant results, so it doesn’t bother me and I’m not thrilled with it either.” “Probably neither one [satisfied or dissatisfied]. Just because he’s got so much more and didn’t get rid of many.” |
| “I would probably say dissatisfied. Like I said, it became an ethical quandary for me of just being like, have I done something wrong in … what’s the bigger picture here and trying to outweigh the balance [of treatment and discomfort].” |
Discussion
Patient experiences are becoming increasingly important in the understanding of skin disease burden and unmet therapeutic needs [13]. Indeed, patients’ views of their symptoms and how symptoms may affect their daily lives are instrumental in treatment decisions in dermatology [13]. Although healthcare providers may be aware of the bothersome symptomology of dermatologic diseases, the impact on patient and/or caregiver quality of life is not well understood. Patient-centric assessments can measure what is important to patients and generate information on patient perceptions regarding the clinical benefit of an experimental medication that goes beyond overt physical changes in severity or lesion count as evaluated by a clinical investigator [13].
Molluscum contagiosum, although one of the most common skin diseases affecting children, has not been widely investigated in clinical trials or through qualitative research. The B-SIMPLE4 trial provided the opportunity to query study patients and/or their caregivers on the impact of MC and a topical clinical intervention. Findings from the exit interviews revealed that lesion location, number, and size, as well as pain, scarring, itching, visibility, and contagiousness, were of concern to patients and caregivers, with visibility and contagiousness being the most bothersome. The most common psychosocial concerns were self-consciousness, embarrassment, and worry about others noticing or commenting on MC lesions.
In the absence of either FDA-approved medications or standard-of-care guidelines for MC, many clinicians adopt a watch-and-wait strategy. Many of the exit interview participants reported being motivated to participate in B-SIMPLE4 because of a desire to try an investigational topical treatment that might result in partial or complete lesion clearance. Availability of new treatment options will likely be welcomed by clinicians and patients [16, 17].
Indeed, participants who experienced partial or complete MC lesion clearance were satisfied with their clinical trial participation. Additionally, participants with less than complete clearance reported that the change in lesion count since study initiation was meaningful. These results highlight the importance of lesion count reductions to patients with MC and caregivers, even when complete clearance is not achieved. The PED indicated that nearly 40% of B-SIMPLE4 participants who received berdazimer gel, 10.3% perceived complete clearance by week 12, indicating that some may have perceived lesion resolution at week 12 as complete clearance even when the complete clearance rate was 34% based on investigator lesion counts in the primary study [9]. In addition, some patients who participated in the exit interview may have achieved complete clearance at the time of the interview, which occurred 2–4 weeks after the week 12 visit. Despite actual lesion counts, most participants reported their MC was much or very much improved by week 12. The nearly identical scores between participant-reported GIC and investigator-reported GIC were notable.
Limitations
Because the B-SIMPLE4 study was designed to fulfill regulatory requirements for marketing authorization, the exit interviews conducted as a substudy may not be an optimal setting to fully capture experiences of a wide range of patients with MC. All exit interview patients were white as the majority of B-SIMPLE4 patients were white [9]; therefore, results may not be generalizable to the general population of patients with MC. In addition, most exit interview participants were caregivers, and therefore the patient experience was primarily reported by caregivers. In addition, the sample size was small (n = 30), though reasonable for a qualitative design. Despite these limitations, the study provided valuable qualitative data on both patient and caregiver experiences with MC treatment. The research methodology and analysis were guided by established qualitative research practices and followed FDA guidance [18–20]. To expand upon study findings and further confirm these results, additional qualitative research is needed in a more diverse group of patients with MC and their caregivers. Additionally, qualitative interviews should be conducted in patients less than 11 years of age who are able to self-report on their experiences with MC so that information can be gathered directly from the patient perspective. Finally, although B-SIMPLE4 included two PED assessments, development of a fit-for-purpose patient-reported outcome measure for patients with MC may be a worthy endeavor that would allow for the comparison of patient-reported outcomes between treatment groups in future, randomized controlled intervention trials.
Conclusions
The PED and exit interviews revealed important factors motivating MC patients/caregivers to participate in clinical trials that might result in complete, partial, or accelerated MC lesion clearance. The underlying drivers appear to be related to the desire to mitigate both physical and psychosocial MC symptomology. Although statistical success of a clinical trial in patients with MC is typically measured by complete lesion clearance, patients/caregivers may be satisfied with partial clearance. Indeed, the PED results and interviews reveal the importance of a reduction in MC lesion count, with or without complete clearance, which highlights the need to involve patients/caregivers in defining therapeutic “success.”
Acknowledgements
The authors are grateful to the patients and caregivers who gave the gift of clinical research participation. In addition, we thank the following B-SIMPLE4 investigators for recruiting patients for the exit interview: Michael P. Husseman, MD, Wee Care Pediatrics—Layton, Layton, UT, USA; Jane C. Gibson, MD, Qualmedica Research, LLC, Bowling Green, KY, USA; Cindy E. Owen, MD, DC Research, Louisville, KY, USA; David Brougher, MD, Qualmedica Research, LLC, Evansville, IN, USA; Joseph A. Ley, MD, Holston Medical Group, Kingsport, TN, USA; Jennifer Martin, MD, Qualmedica Research, LLC, Owensboro, KY, USA, Navid Ezra, MD, Clinical Trials Research Institute, Thousand Oaks, CA, USA; Edward Primka, Dermatology Associates of Knoxville, Knoxville, TN, USA; Richard Ohnmacht, MD, Omega Medical Research, Warwick, RI, USA; Mary Christian-Reed, MD, DelRicht Research, Tulsa, OK, USA; Sarah Jackson, MD, DelRicht Research, New Orleans, LA, USA; Matthew Miller, MD, Palmetto Clinical Trial Services, LLC, Greenville, SC, USA; Douglass Forsha, MD, Jordan Valley Dermatology Center, West Jordan, UT, USA; and Joel Cohen, MD, AboutSkin Research, LLC, Greenwood Village, CO, USA.
Declarations
Funding
Novan, Inc. funded B-SIMPLE4, the qualitative analyses of the exit interviews, and manuscript development.
Conflict of interest
John Caleb Browning and Ira Thorla Jr were study investigators and are compensated (i.e., honoraria, personal fees) advisors to Novan, Inc. Martina Cartwright and Tomoko Maeda-Chubachi are employees of and stockholders in Novan, Inc. Oyebimpe Olayinka-Amao and Susan A. Martin are employees of RTI Health Solutions, which received funding to conduct the qualitative research and manuscript development. Martina Cartwright was employed by Cassiopea Inc. at the time the study was conducted.
Ethics approval
The interviews were included as part of the B-SIMPLE4 clinical trial. Study approval was obtained from relevant ethics committees and institutional review boards for all 55 B-SIMPLE4 US clinical trial sites that participated in B-SIMPLE4, and the protocol was reviewed by the FDA. The study was conducted in accordance with the Declaration of Helsinki.
Consent to participate/publish
Study approval was obtained from relevant ethics committees and institutional review boards for all 55 B-SIMPLE4 US clinical trial sites that participated in B-SIMPLE4, and the protocol was reviewed by the FDA. The study was conducted in accordance with the Declaration of Helsinki. Patients/caregivers voluntarily provided written informed consent/assent before screening procedures for B-SIMPLE4 were initiated. Verbal consent/assent for the interviews were confirmed before each telephone interview.
Availability of data and material
Data will not be shared.
Code availability
Not applicable.
Author contributions
TMC, SAM, and OO-A contributed to the exit interview study conception and design. Data collection and analysis were performed by SAM and OO-A. The first draft of the manuscript was written by OO-A, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- 1.Meza-Romero R, Navarrete-Dechent C, Downey C. Molluscum contagiosum: an update and review of new perspectives in etiology, diagnosis, and treatment. Clin Cosmet Investig Dermatol. 2019;12:373–381. doi: 10.2147/ccid.S187224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen X, Anstey AV, Bugert JJ. Molluscum contagiosum virus infection. Lancet Infect Dis. 2013;13(10):877–888. doi: 10.1016/s1473-3099(13)70109-9. [DOI] [PubMed] [Google Scholar]
- 3.Shisler JL. Immune evasion strategies of molluscum contagiosum virus. Adv Virus Res. 2015;92:201–252. doi: 10.1016/bs.aivir.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Coyner T. Molluscum contagiosum: a review for healthcare providers. Dermatol Nurses Assoc. 2020;12(3):115–120. doi: 10.1097/JDN.0000000000000534. [DOI] [Google Scholar]
- 5.Olsen JR, Gallacher J, Finlay AY, Piguet V, Francis NA. Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study. Lancet Infect Dis. 2015;15(2):190–195. doi: 10.1016/s1473-3099(14)71053-9. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Molluscum contagiosum. Available from: https://www.cdc.gov/poxvirus/molluscum-contagiosum/index.html. Accessed 15 June 2022.
- 7.Nguyen HP, Tyring SK. An update on the clinical management of cutaneous molluscum contagiosum. Skin Therapy Lett. 2014;19(2):5–8. [PubMed] [Google Scholar]
- 8.Basdag H, Rainer BM, Cohen BA. Molluscum contagiosum: to treat or not to treat? Experience with 170 children in an outpatient clinic setting in the northeastern United States. Pediatr Dermatol. 2015;32(3):353–357. doi: 10.1111/pde.12504. [DOI] [PubMed] [Google Scholar]
- 9.Browning JC, Enloe C, Cartwright M, Hebert A, Paller AS, Hebert D, et al. Efficacy and safety of topical nitric oxide-releasing berdazimer gel in patients with molluscum contagiosum: a phase III randomized clinical trial. JAMA Dermatol. 2022 doi: 10.1001/jamadermatol.2022.2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cartwright M, Enloe C, Stripling S, Maeda-Chubachi T. Pharmacokinetic profile, safety, and tolerability of topical berdazimer gel, 10.3% in patients with molluscum contagiosum. J Drugs Dermatol. 2022. (In Press). [DOI] [PubMed]
- 11.Hebert AA, Siegfried EC, Durham T, de León EN, Reams T, Messersmith E, et al. Efficacy and tolerability of an investigational nitric oxide-releasing topical gel in patients with molluscum contagiosum: a randomized clinical trial. J Am Acad Dermatol. 2020;82(4):887–894. doi: 10.1016/j.jaad.2019.09.064. [DOI] [PubMed] [Google Scholar]
- 12.Maeda-Chubachi T, Hebert D, Messersmith E, Siegfried EC. SB206, a nitric oxide-releasing topical medication, induces the beginning of the end sign and molluscum clearance. JID Innov. 2021;1(3):100019. doi: 10.1016/j.xjidi.2021.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daniels SR, Marcus KA, Bent R, Papadopoulos E. Measuring what matters to patients in dermatology drug development: a regulatory perspective. Dermatol Clin. 2022;40(3):333–337. doi: 10.1016/j.det.2022.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 15.Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant. 2002;36(4):391–409. doi: 10.1023/A:1020909529486. [DOI] [Google Scholar]
- 16.Eichenfield LF, McFalda W, Brabec B, Siegfried E, Kwong P, McBride M, et al. Safety and efficacy of VP-102, a proprietary, drug-device combination product containing cantharidin, 0.7% (w/v), in children and adults with molluscum contagiosum: two phase 3 randomized clinical trials. JAMA Dermatol. 2020;156(12):1315–1323. doi: 10.1001/jamadermatol.2020.3238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oza VS. Molluscum contagiosum therapeutics: new options may be around the corner. JAMA Dermatol. 2022 doi: 10.1001/jamadermatol.2022.2719. [DOI] [PubMed] [Google Scholar]
- 18.Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, et al. Content validity: establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation. ISPOR PRO Good Research Practices Task Force report: part 1: eliciting concepts for a new PRO instrument. Value Health. 2011;14(8):967–977. doi: 10.1016/j.jval.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 19.US Food and Drug Administration. Patient-focused drug development: methods to identify what is important to patients. Draft guidance. Feb 2022. Available from: https://www.fda.gov/media/131230/download. Accessed 4 Mar 2022.
- 20.US Food and Drug Administration. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims. Dec 2009. Available from: https://www.fda.gov/downloads/drugs/guidances/UCM193282.pdf. Accessed 4 Mar 2022. [DOI] [PMC free article] [PubMed]