Abstract
There is a public health need to understand mental health vulnerabilities to COVID-19 pandemic-related stressors and promote resilience among high-risk populations with preexisting psychiatric conditions. Recent cross-sectional studies suggest increases in mental health distress (e.g., depression and anxiety) during the pandemic. The present study expands upon these emerging findings using longitudinal latent modeling and hierarchical linear regressions. Consistent with the developmental psychopathology literature on resilience, we distinguished between promotive or risk (i.e., main effect), and protective or vulnerability (i.e., moderation) effects on mental health during the pandemic. At a large medical center, 398 veterans receiving outpatient mental health care provided pre-pandemic (Time 1) and during pandemic (Time 2) assessments of mental and physical health-related distress. Additional Time 2 questionnaires assessed pandemic-related stressors and positive behavioral adaptations in the summer of 2020. As expected, total stressor scores predicted longitudinal worsening of self-reported mental (β = −.205) and physical health (β = −.217). Positive behavioral adaptations enacted during the pandemic moderated and protected against stressor effects on mental health (β = .160). In addition, the presence of substance use disorders moderated and conferred vulnerability to stressor effects on physical health (β = −.158). Thus, higher COVID-19 pandemic stressor exposure may have exacerbated mental and physical health distress among veterans with common forms of psychopathology. Nevertheless, behavioral activation, purposeful maintenance of social connections, and focused treatment for substance misuse may be important intervention targets for reducing the longitudinal impact of pandemic stressors and enhancing resilience among people with mental illness.
Keywords: veterans, COVID-19, resilience, longitudinal, distress
The COVID-19 pandemic has brought about abrupt changes in daily life due to widespread outbreaks of disease, as well as restrictions of movement, institutional shutdowns, and social distancing. These necessary efforts to curb infections have also had significant consequences such as economic losses and interrupted access to support resources. There is growing focus on how stressors related to the pandemic may be increasing the prevalence of psychopathology and contributing to an unmet need for mental health care (Czeisler et al., 2020; Vahratian et al., 2021). People with preexisting psychiatric disorders may be at heightened risk for mental health symptoms during the pandemic (Holmes et al., 2020). Identifying which individuals with common forms of psychopathology are most vulnerable to these stressor effects is of vital public health importance for allocating resources and guiding prospective intervention efforts (Galea et al., 2020). Existing studies of mental health during the COVID-19 pandemic have been largely cross-sectional and atheoretical, but are suggestive of pandemic-related increases in psychiatric symptoms such as depression and anxiety in the general population (Aknin et al., 2022). To expand beyond these studies, a longitudinal quality improvement survey at a large United States Veterans Affairs (VA) medical center was used to assess pandemic-related changes in symptomatology, and to model the dynamic effects of individual vulnerabilities (e.g., clinical indicators) and protective resilience factors (e.g., positive behavioral adaptations to stressors). We examined a sample of active outpatients using established methods for studying resilience in the context of environmental adversity (Luthar et al., 2000).
Following exposure to pandemic-related events, there may be variability among individuals with common mental disorders in terms of resilience, or capacity to adapt, recover, and mitigate stressor effects. Rather than the presence of particular static traits, resilience is a dynamic process that only becomes apparent over time in the context of stressors (Luthar et al., 2000; Masten, 2001). Capturing longitudinal resilience requires a consideration of multiple factors: stressor dosages, symptom changes over time, and the functioning of various adaptive systems within and around the person (Masten & Narayan, 2012). In developmental studies, these adaptive systems can include personal attributes, environmental resources, patterns of thinking and behavior, or social connections (Masten et al., 2021). Environmental stressors probe the responsiveness of these adaptive systems over time, and reveal who is better or worse at counteracting stressor effects and preserving their current functioning (Abramson et al., 1989; Masten & Tellegen, 2012). However, these types of dynamic resilience models have not been tested with respect to the mental health impacts of pandemic-related stressors in high-risk populations with preexisting psychiatric conditions.
Instead, since the beginning of the pandemic, there have been many cross-sectional surveys of mental health using convenience sampling (Xiong et al., 2020). In general, most findings are consistent with established pre-pandemic associations between better current mental health and greater perceived social support (Bonsaksen et al., 2020), regular physical activity (Yang et al., 2020), use of active coping skills (Park et al., 2021), and a negative personal history of psychopathology (Alonzi et al., 2020). However, cross-sectional studies mask the process of resilience by failing to account for baseline differences in symptomatology before the pandemic onset (Bonanno et al., 2011; Polusny et al., 2017). Without modeling relative changes overtime, it is impossible to know if the observed effects on mental and physical health-related distress can be better explained by unappreciated baseline differences before the pandemic began (Bendau et al., 2021). Indeed, newer studies of the impact of COVID-19 stressors on mental health report differing effects for longitudinal versus cross-sectional analyses (Shanahan et al., 2021). Many people with baseline symptoms of psychopathology are likely capable of manifesting resilience under stressful conditions (Eisen et al., 2014). This effect will be invisible to investigators unless longitudinal changes in relative mental and physical health-related distress are considered.
Moreover, existing pandemic studies have not employed established statistical models of resilience using individual stressor scores as the key predictor of later outcomes (Garmezy et al., 1984). In developmental studies of resilience, there is a crucial distinction between stressor-independent (i.e., main) and stressor-dependent (i.e., moderation) effects (Figure 1). Typically, many types of variables are independently associated with outcomes regardless of stressor exposure (Shiner & Masten, 2012). These include risk factors, which lead to worsening outcomes, and promotive resources, which contribute to enhanced outcomes irrespective of the circumstances. In contrast to main effect predictors, only a select handful of statistical moderators increase vulnerability to stressors or confer a protective advantage against stressor effects on outcomes. The distinctions between risk versus promotive effects as well as vulnerability versus protective effects are largely made for pedagogical reasons within the developmental psychopathology literature. In practice, these terms are often considered to be reverse keyed equivalents of each other (e.g., a person scoring low on a vulnerability in the context of stressors is viewed as exhibiting protective effects, and vice versa). Stressor-dependent moderation effects – both vulnerabilities and protections – are evidence for activation of the systems within and around the person with the capacity to alter the impact of environmental challenges (Masten, 2001).
Figure 1.
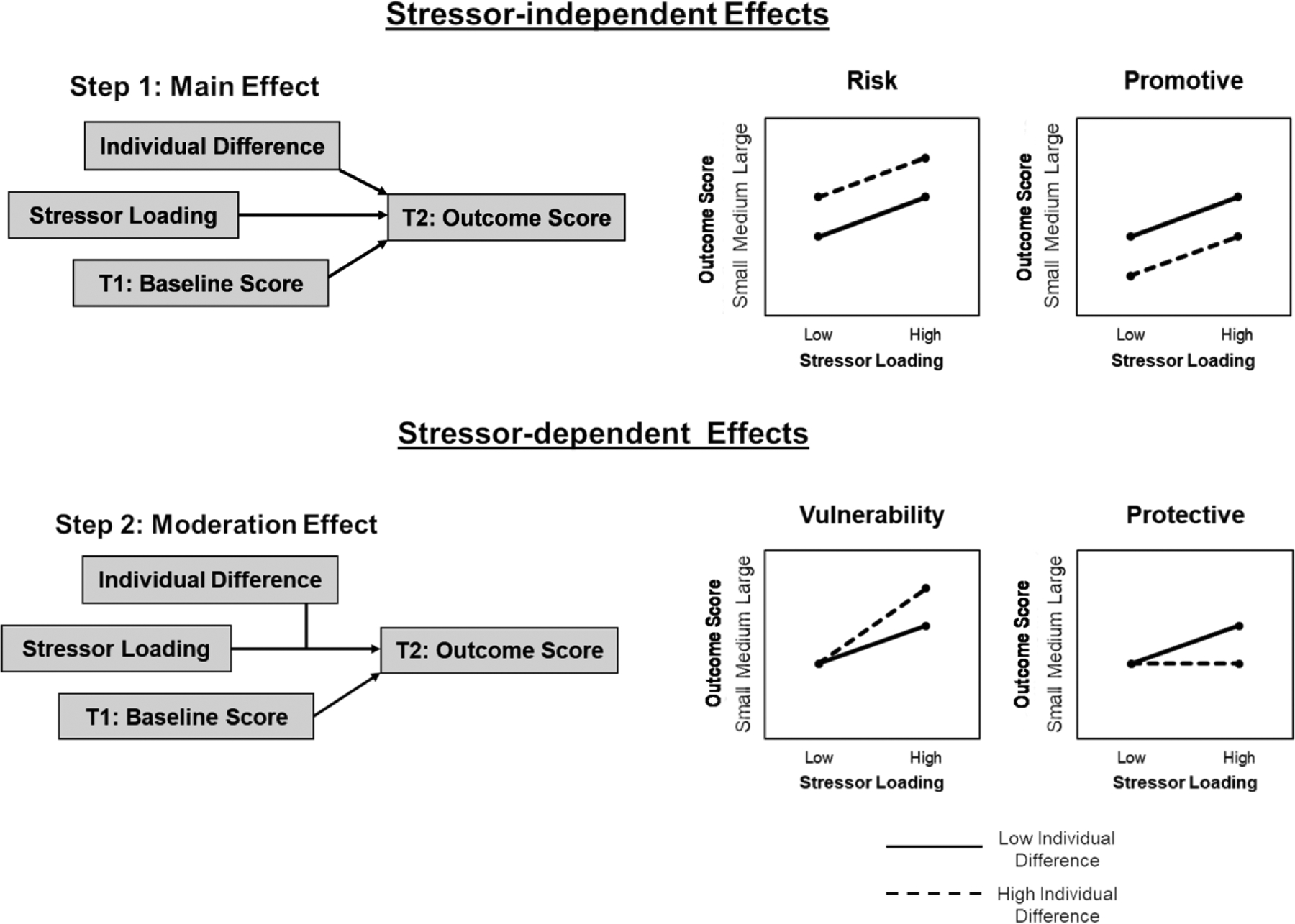
Developmental Psychopathology Framework for the Study of Resilience.
Note. Conceptual diagram of stressor-independent and stressor-dependent longitudinal effects modeled using a developmental psychopathology statistical and theoretical framework. T1 = Time 1, T2 = Time 2.
The COVID-19 pandemic has created a naturalistic experiment for identifying which vulnerabilities and protective systems are especially relevant for health. Within studies of children and young adults, domains such as self-regulation and perceived social support are commonly studied as predictors of resilience outcomes (Masten et al., 2021). There is value in applying similar models to predict resilience among psychiatric outpatients with heterogeneous clinical presentations. Veterans receiving outpatient care are a valuable population for studying dynamic vulnerability and protective processes because of an elevated lifetime accumulation of adverse life events (Wisco et al., 2014). Veterans often exhibit resilience following these stressors (e.g., military deployments), but there is often marked variability in the range of mental health responses (Polusny et al., 2017).
Resilience (or a lack thereof) may manifest differently depending on the individual differences of veterans with active psychiatric concerns. Certain clinical profiles may differentially predict main effect risks versus vulnerability moderations. Personal history of substance use disorders may be a longitudinal main effect risk for worsening mental health during the COVID-19 pandemic (Fein-Schaffer et al., 2022). Veterans with preexisting internalizing diagnoses (e.g., depression, fear; Conway et al., 2019) may instead have heightened vulnerability because of the close connections between life stressors and mood and anxiety symptoms (Kendler et al., 1999; Ridley et al., 2020). For example, heightened emotion dysregulation at baseline increases longitudinal vulnerability to the effects of military stressors on mental health outcomes (Cobb et al., 2017). Given this evidence, it is possible that veterans with baseline internalizing disorders as opposed to substance use disorders may be most vulnerable to experiencing a worsening of mental health-related distress in response to pandemic-related stressors. At the same time, the COVID-19 pandemic has also ushered in societal disruptions with sometimes unexpected positive effects. Many people have seen the pandemic as an opportunity to enact behavioral changes such as increasing their time spent with family, taking on new hobbies, and pursuing more physical activity (Williams et al., 2021). It is possible these types of positive behavioral adaptations can partially offset the impact of COVID-19 stressors on health, even among individuals with active psychiatric concerns.
To study resilience among veterans, we applied the above-described principles and methodologies from the field of developmental psychopathology to a survey dataset of veterans receiving mental health care at the Minneapolis Veterans Affairs Health Care System (VAHCS). At the start of the COVID-19 pandemic, in March 2020, the Minneapolis VAHCS initiated a previously unprecedented shift towards telehealth for nearly all outpatient mental health visits. Simultaneously, the general public experienced local stay-at-home orders and restrictions on non-essential businesses (Kraker & Porter, 2020). This produced sudden social isolation especially among veterans with active psychiatric needs, medical disabilities, and low resources (e.g., no personal computer access). To assess the impact of these changes, veterans with recent and upcoming outpatient mental health appointments were mailed surveys about pandemic-related events, and mental and physical health-related distress. The survey also included additional questions related to positive behavioral adaptations.
Based on the studies linking better mental health with active coping behaviors during the pandemic (Park et al., 2021; Williams et al., 2021; Yang et al., 2020), we expected (1) veterans who endorsed greater positive behavioral adaptations to experience a buffering against stressor impacts consistent with a protective resilience effect. Based on the prior research supporting links between stressors and anxiety and depression (Kendler et al., 1999; Ridley et al., 2020) as well as pre-pandemic mental health histories and pandemic outcomes (McCracken et al., 2020), we anticipated (2) a greater number of internalizing distress diagnoses (e.g., mood and anxiety disorders) would confer vulnerability to stressors. In addition, we expected (3) substance use disorders to confer a main effect risk for worsening mental health symptoms (Fein-Schaffer et al., 2022). Our analytic approach had the potential to identify clinical characteristics and behavior patterns with dynamic effects on outcomes. These analyses may immediately inform outreach efforts and clinical resource allocations targeting at-risk veterans exposed to adverse events during the COVID-19 pandemic.
Method
As part of a quality improvement project, surveys were sent to 3,361 U.S. veterans receiving mental health outpatient treatment at the Minneapolis VAHCS (i.e., attended and/or scheduled appointments between September 1, 2019 and October 31, 2020). Surveyed veterans received care in either a multidisciplinary generalist mental health clinic and/or a multidisciplinary specialty addiction clinic. In July 2020, we mailed packets with project descriptions, instructions, self-report survey measures, and pre-paid return envelopes. Completed surveys were received from 664 veterans (response rate = 19.8%) on or before September 14, 2020. Baseline pre-pandemic measures (Time 1) were available for a subset of 398 individuals (60.0%) to conduct longitudinal modeling (see Supplemental Materials for comparison of the longitudinal subsample to the remaining survey responders). This study was deemed exempt from local institutional review board (IRB) review due to the project’s program evaluation nature.
Electronic Veterans Affairs Health Record Data
The following demographic and diagnostic information was retrieved from veterans’ VA medical records on May 15, 2020, if available: demographics (age, sex, race, ethnicity), number of internalizing disorders (i.e., major depressive disorder [MDD], recurrent MDD, dysthymia, anxiety, PTSD, depression not otherwise specified [NOS], anxiety NOS, adjustment disorder), and number of substance use disorders (i.e., alcohol, drug, tobacco, and unspecified substance use disorders). The data pull was done using established internal Minneapolis VAHCS procedures for medical record quantification in the context of program evaluation. Diagnoses were extracted from actual mental health stop-coded encounters as opposed to non-psychiatric encounters, events unrelated to direct clinical care, etc. Therefore, these diagnoses reflected active treatment targets from October 1, 2019 to May 15, 2020. The count of diagnoses reflects the symptom complexity in the internalizing and substance use domains of psychopathology (cf. “internalizing-distress” and “externalizing-substance abuse” from the Hierarchical Taxonomy of Psychopathology [HiTOP]; Conway et al., 2019).
Survey Measures
National Institutes of Health Patient-Reported Outcomes Measurement Information System (PROMIS; Ader, 2007).
The PROMIS is a publicly available set of self-report measures about health. In this study, the PROMIS Global Health-10 (Hays et al., 2009) and Depression and Anxiety subscales from the PROMIS-29 Profile (Hays et al., 2018) were administered. Responses to the PROMIS Global Health were used to calculate Global Physical Health and Global Mental Health scores, each composed of four items (higher total scores indicated fewer overall symptoms). Depression (e.g., “I felt worthless,” “I felt hopeless”) and Anxiety (e.g., “I felt fearful,” “My worries overwhelmed me”) were assessed with the standard four-item scales (higher scores reflect more symptoms). All items employed a 5-point rating scheme from 1 (never) to 5 (always). Finally, we retrieved pre-pandemic responses to PROMIS items. For veterans who completed PROMIS inventories more than once prior to the pandemic as part of clinical care, the most recent responses were used (i.e., closest in time to March 1, 2020). When ≤ 2 item responses were missing for particular scales, responses were interpolated using the mean of the completed items.
Epidemic-Pandemic Impacts Inventory (EPII; Grasso et al., 2020, 2021).
The EPII (Version 04/03/2020) is an experimental 84-item measure of pandemic-related experiences regarding Work and Employment (11 items), Education and Training (2 items), Home Life (13 items), Social Activities (10 items), Economic (5 items), Emotional Health and Well-Being (8 items), Physical Health Problems (8 items), Physical Distancing and Quarantine (8 items), and Positive Change (19 items; Tables 1, S1, and S2). With the exception of Positive Change, each of the EPII domains indexed negative or adverse life changes experienced since the start of the pandemic. In contrast, Positive Change indexed a range of positive behavioral and attitudinal adaptations in response to the pandemic. Examples included increased quality time and social connections with family and friends, increased physical exercise, spending more time doing enjoyable activities, experiencing greater appreciativeness, paying greater attention to personal health, helping other people, and finding greater purpose and productivity during life pursuits. Although these items query perceptions of behavioral increases during the pandemic, the scale is retrospective without a true baseline comparison. Veterans responded “Yes,” “No” or “N/A” to each item.
Table 1.
Participant Demographics and Clinical Characteristics.
| n | M | SD | Cronbach’s α | |
|---|---|---|---|---|
| Totala | 398 | |||
| Female | 59 | |||
| Non-white | 24 | |||
| Hispanic | 50 | |||
| Married | 193 | |||
| Age, years | 59.9 | 13.2 | ||
| VA Service Connection level | 59.9 | 34.4 | ||
| EPIIb | ||||
| Work and Employment, % | 10.8 | 15.1 | .70 | |
| Education and Training, % | 9.8 | 23.6 | .44 | |
| Home Life, % | 6.0 | 11.3 | .74 | |
| Social Activities, % | 43.1 | 25.8 | .76 | |
| Economic, % | 8.4 | 17.1 | .61 | |
| Emotional Health and Well-being, % | 30.6 | 22.0 | .68 | |
| Physical Health Problems, % | 37.8 | 24.1 | .70 | |
| Physical Distancing and Quarantine, % | 16.6 | 17.8 | .60 | |
| Total stressors, % | 20.0 | 12.1 | .89 | |
| Positive Change, % | 31.0 | 21.4 | .82 | |
| PROMISc | ||||
| Global Physical Health (T1) | 13.1 | 2.8 | .71 | |
| Global Physical Health (T2) | 12.9 | 3.0 | .76 | |
| Global Mental Health (T1) | 10.8 | 3.3 | .84 | |
| Global Mental Health (T2) | 10.7 | 3.3 | .83 | |
| Depression (T1) | 9.6 | 4.1 | .92 | |
| Depression (T2) | 9.8 | 4.3 | .93 | |
| Anxiety (T1) | 9.9 | 3.7 | .88 | |
| Anxiety (T2) | 10.4 | 4.1 | .90 | |
| Internalizing diagnoses, count | 2.2 | 1.3 | ||
| Externalizing diagnoses, count | 1.4 | 1.2 |
Note.
Veterans with PROMIS scores at both Time 1 and Time 2 (longitudinal analyses sample) presented in this table; see Table S1 for data from the full Time 2 sample.
For EPII, percent scores are displayed, which are linear transformations of EPII total count scores for ease of interpretation.
T-score equivalents of the mean PROMIS scores based on general population normative data are as follows: Global physical health (T1) = 42.9, Global physical health (T2) = 42.5, Global mental health (T1) = 40.6, Global mental health (T2) = 40.2, Depression (T1) = 57.2, Depression (T2) = 57.5, Anxiety (T1) = 58.5, Anxiety (T2) = 59.5. M = mean, SD = standard deviation, T1 = Time 1, T2 = Time 2, VA = United States Veterans Affairs, EPII = Epidemic-Pandemic Impacts Inventory, PROMIS = Patient-Reported Outcomes Measurement Information System.
Given that the EPII is a newly developed measure, optimal scoring procedures have yet to be established. For our analyses, “No,” “N/A,” and missing responses were collapsed together and interpreted as denials. A total EPII stressor score was derived using the sum total of “Yes” endorsement counts across the adverse life event domains (Haydon & Salvatore, 2021). However, for ease of interpretation of the EPII scores, we also provide percent counts in Table 1 (% of “Yes” endorsements). EPII Emotional Health and Well-being items with content overlapping with the PROMIS mental health measures were excluded (items 44, 45, and 46) to avoid circularity between the model predictors and outcomes. Secondly, a total EPII Positive Change percent “Yes” endorsement count score was computed, and used as a predictor of health (Bleil et al., 2021).
Characteristics of Survey Responders versus Non-Responders
Survey responders compared to non-responders tended to be older (M = 60.5 years, SD = 12.8 and M = 50.8 years, SD = 14.5, respectively; t(3357) = 15.61, p < .001, Cohen’s d = .70. The majority of responders served within the Vietnam War era (63.7%), while veterans from the Operations Enduring and Iraqi Freedom (OEF/OIF) and Persian Gulf War eras were underrepresented among responders (33.7%). Responders were more likely to be married, χ2(1, n = 3359) = 32.98, p < .001, Cramer’s V = .10, and to racially identify as white, χ2(1, n = 3359) = 18.84, p < .001, Cramer’s V = .08. Based on the VA medical record, responders also had fewer internalizing disorders than non-responders (M = 2.0, SD = 1.3 and M = 2.2, SD = 1.4, respectively; t(3343) = 2.44, p = . 015, Cohen’s d = .11), and fewer substance use disorders than non-responders (M = 1.4, SD = 1.3 and M = 1.7, SD = 1.3, respectively; t(3343) = 6.17, p < .001, Cohen’s d = .27); however, these group difference effect sizes were small. Responders and non-responders did not significantly differ based on gender identity, ethnicity, and VA Service Connection disability status level, ps ≥ .078.
Statistical Approach
Using the whole sample of 664 responders, we evaluated EPII psychometric properties and overall rates of EPII endorsement. Specifically, Cronbach’s alpha was calculated to describe the internal consistency of the EPII. To support our creation of the EPII total stressor index, we performed exploratory factor analysis (maximum likelihood) using the nine EPII subscale scores (SPSS 25). The remaining analyses relied on a subset of 398 responders with pre-pandemic/baseline measures. Longitudinal changes in PROMIS Global Mental Health, Anxiety, and Depression total scores were estimated using maximum likelihood structural equation modeling (three indicators for a single factor, two time points; Mplus 8). We evaluated the measurement invariance of this single factor using a one-sample approach with correlated indicator errors and increasingly restrictive measurement parameters (Brown, 2015). The baseline comparison model consisted of an identical configural structure at both time points (equal form). For the PROMIS Global Mental Health indicator, factor loadings were fixed to 1 (i.e., high latent score = less mental health distress) and intercepts were fixed to zero. Model fit was then compared using equal factor loadings (weak invariance). Then, the model was further constrained using equal indicator intercepts (strong invariance). Finally, indicator error variances were constrained across both time points (strict invariance). Relative changes in model fit were assessed with nested X2 difference tests and Bayesian information criterion (BIC). Overall model fit was assessed using root mean square error of approximation (RMSEA) with 90% confidence intervals and test of close fit (CFIT), standardized root mean square residual (SRMR), comparative fit index (CFI), and Tucker-Lewis index (TLI). We planned to extract factor estimates using the most restrictive measurement parameters supported by the fit indices. For PROMIS Global Physical Health, overall functioning was estimated using the raw total score.
To evaluate longitudinal changes using developmental psychopathology principles, hierarchical linear regressions were performed (SPSS 25). We generated separate models for the latent factor estimate of mental health distress and for PROMIS Global Physical Health. During Step 1, the survey interval (M = 461 days, SD = 271 days) between the pre-pandemic and during pandemic assessments was entered. For Step 2, the relevant baseline PROMIS measures scores were added as statistical covariates so that Steps 3 – 5 predictor effects would represent associations with relative changes in PROMIS scores over time. The total stressor score from the EPII was entered at Step 3. EPII Positive Change, or internalizing and substance use diagnostic counts were entered as main effect predictors at Step 4. Significant effects at Step 4 would be consistent with risk or promotive associations independent of total stressor scores. Step 5 included interaction terms between the individual difference measures (i.e., EPII Positive Change, psychiatric disorder counts) and total stressor scores to model vulnerability or protective effects. Supplemental Materials present additional analyses using an individual difference measure of overall medical risk/complexity for comparison (Ruiz et al., 2018; Osborne et al., 2020).
Predictors were evaluated using percentile bootstrap methodology with 95% confidence intervals (Wood, 2005) and repeated resampling (2,000 times per model; consistent random seed number across all models). This created non-parametric effect distributions representative of the observed data. When significant interactions were observed for the diagnostic count models, non-significant moderators were pruned and the effects were re-estimated. Significant interaction terms were probed by centering the relevant individual difference terms at the 7th, 16th, 33rd, 50th, 66th, and 84th, and 93rd percentiles. Given the three sets of individual difference measures across the main text and Supplemental Materials, we also used a Bonferroni-corrected threshold of α = .01667 to further evaluate the model effects. Effects not surviving this threshold are highlighted in the Results.
Finally, hierarchical linear regressions for both mental health distress and Physical Health outcomes were repeated using age (years), white racial identification (binary), and gender (binary) as covariates in Step 1. This yielded qualitatively identical resilience-related effects as those presented in the Results below (see Supplemental Materials).
Transparency and Openness
We report study sample determination, all data exclusions/manipulations (if any), and all measures. Study data/materials and statistical analyses syntax (SPSS 25, Mplus 8) are available by emailing the corresponding author. This study was not preregistered.
Results
EPII Pandemic-related Experiences
Table 1 shows internal consistencies for the EPII using the full n = 664 survey sample. As expected, internal consistency was closely associated with subscale length: all subscales with 10 items or more displayed acceptable or better internal consistency. EPII total stressors exhibited good-to-excellent internal consistency when including all adverse event items and when excluding items 44, 45, and 46 related to emotional well-being. Internal consistency of Positive Change was good. Furthermore, all EPII subscales except Positive Change were positively correlated with all other subscales (Table S3). Eigenvalues from an exploratory factor analysis of the nine EPII subscales pointed towards a one-factor solution with a scree plot elbow at two factors (Figure S1). For the one-factor solution, all EPII subscale factor loadings were ≥ .423 with the exception of EPII Positive Change (−.004).
At Time 2, veterans (n = 664) most frequently endorsed items on the EPII Social Activities subscale (Table S1). This was followed by endorsements of adverse pandemic-related experiences in the EPII domains of Physical Health Problems, Emotional Health and Well-being, and Physical Distance and Quarantine. Average endorsement for the remaining adverse EPII domains was below 11%. The five most commonly endorsed items in the total stressor score included increased physical sedentariness (67.9%), interrupted family celebrations (67.0%), increased screen time (63.6%), less physical exercise (61.4%), and cancelation of travel plans (58.7%). Veterans endorsed 30.0% of the 19 EPII Positive Change items on average. The five most commonly endorsed individual items included feeling more appreciative (64.8%), paying more attention to physical health (55.6%) and injury prevention (47.9%), spending more time outdoors (40.2%), and doing more enjoyable activities (40.0%).
Change in PROMIS Mental Health Distress
Latent models of mental health distress using the PROMIS Global Mental Health, Depression, and Anxiety indicator scale scores exhibited strict measurement invariance (Table S5; Figures 2 and S2). The addition of model constraints did not result in a significant change in X2, 90% confidence intervals for RMSEA included zero for all models, SRMR for all models was ≤ .024, and BIC model fit continued to improve as model restrictions were added. Strict measurement invariance of this sort suggests similar factor loadings, similar scale biases, and similar scale residual variances for the PROMIS measures before and during the pandemic. Therefore, changes in latent mental health distress are most likely due to true longitudinal changes rather than changes in the structure or measurement of the construct over time. Latent factor estimates of mental health distress (reversed; lower scores = greater distress) were extracted using the strict measurement model constraints (n = 398).
Figure 2.
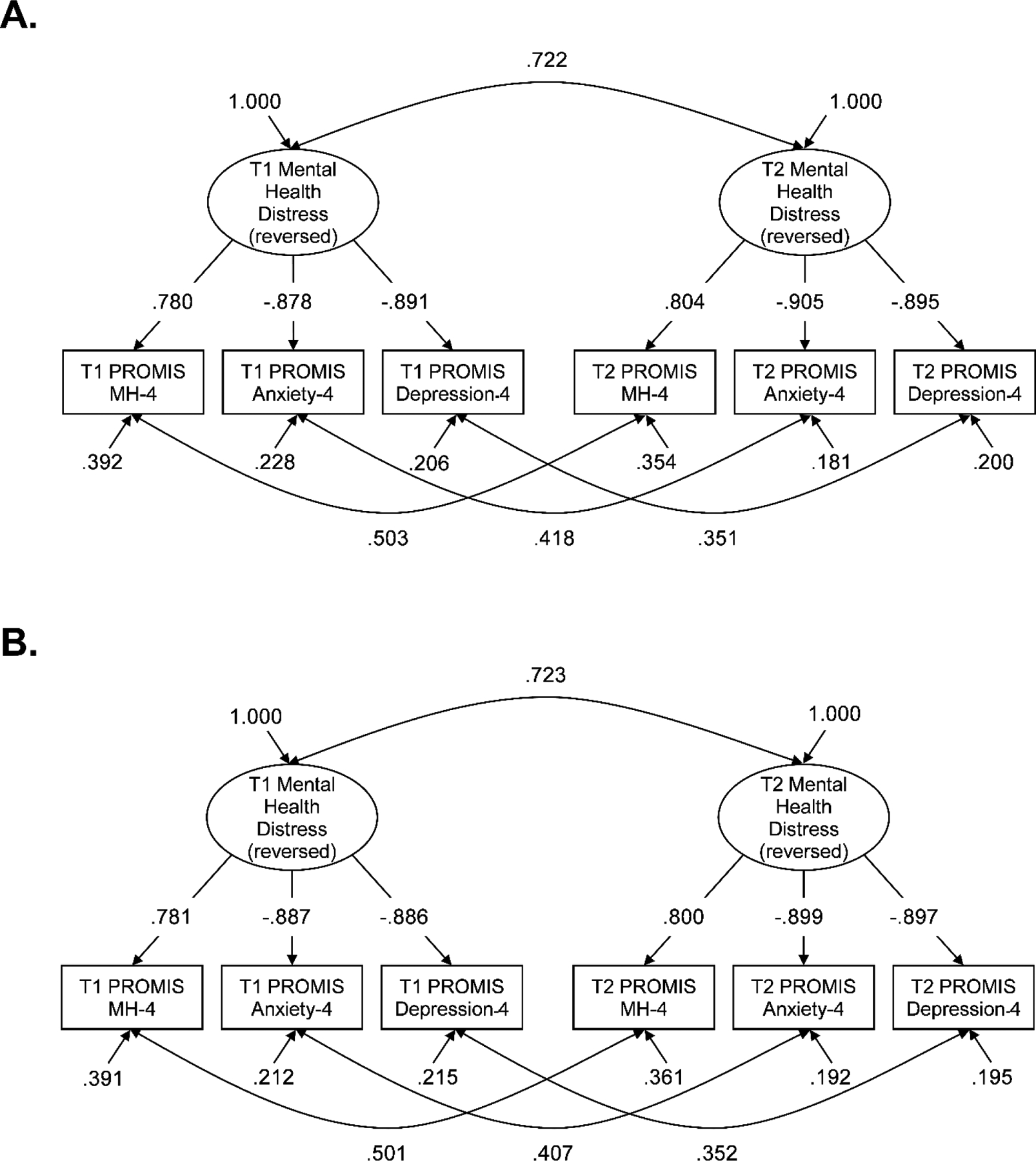
Longitudinal Latent Modeling of Mental Health Distress.
Note. Standardized coefficients depicted: (A) configural model with equal form, and (B) strict model with equal form, factor loadings, indicator intercepts, and indicator error variances. T1 = time 1, T2 = time 2, PROMIS = Patient-Reported Outcomes Measurement Information System, MH = Global Mental Health.
For the regression-based longitudinal developmental psychopathology models, the number of days between assessments was not associated with Time 2 latent PROMIS mental health distress scores (Tables 2 and S6). As expected, Time 1 mental health distress predicted Time 2 mental health distress. With Time 1 scores included as a covariate (i.e., modeling change), total EPII stressor score predicted a relative worsening of self-reported mental health distress over time. EPII Positive Change predicted main effects on mental health distress changes independent of stressor scores (b = 1.513, 95% CIboot [.657, 2.320], β = .128). In addition, there was a moderation effect between EPII Positive Change and stressor scores (b = 6.156, 95% CIboot [.562, 11.399], β = .160). More frequent endorsement of positive changes during the pandemic was associated with a lessening of pandemic-related effects on changes in mental health distress (Figure 3A). This was most evident for veterans who reported the highest amounts of positive behavioral adaptations during the pandemic– the bootstrap-estimated confidence interval for the total stressor score predictor included zero for veterans who endorsed the highest number of EPII Positive Change items. In other words, veterans with the highest endorsement of positive behavioral adaptations reported no effect of the pandemic-related stressors on their self-reported mental health (i.e., protection).
Table 2.
Longitudinal Prediction of Latent PROMIS Mental Health Distress using EPII Positive Change.
| Bootstrap Results | ||||||
|---|---|---|---|---|---|---|
| 95% CI | ||||||
| Predictor | b | β | SE | p | LL | UL |
| Step 1 | ||||||
| Survey Interval | .000 | −.028 | .000 | .551 | −.001 | .001 |
| Step 2 | ||||||
| PROMIS Mental Health Distress Time 1 | .812 | .758 | .033 | < .001 | .743 | .875 |
| Step 3 | ||||||
| EPII Stressor Loading | −4.295 | −.205 | .655 | < .001 | −5.645 | −3.025 |
| Step 4 (Risk/Promotive) | ||||||
| EPII Positive Change | 1.513 | .128 | .421 | < .001 | .657 | 2.320 |
| Step 5 (Vulnerability/Protective) | ||||||
| EPII Stressor Loading * EPII Positive Change | 6.156 | .160 | 2.723 | .020 | .562 | 11.399 |
Note. b = unstandardized predictor coefficient, SE = standard error, CI = confidence interval, LL = lower limit, UL = upper limit, PROMIS = Patient-Reported Outcomes Measurement Information System, EPII = Epidemic-Pandemic Impacts Inventory. Boldface type indicates significant associations. Mental Health Distress is reverse scored.
Figure 3.
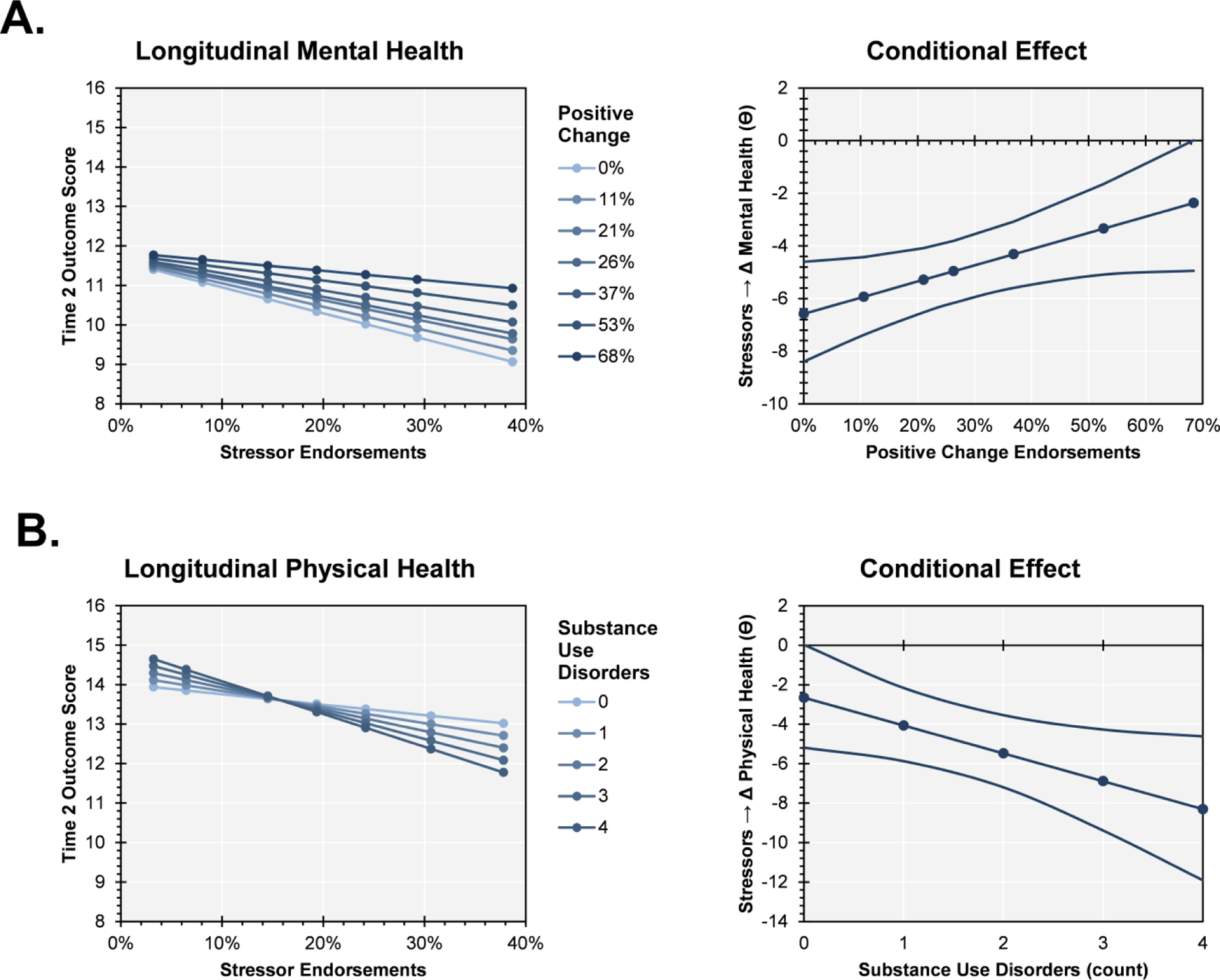
Stressor-dependent Moderation Effects using Longitudinal Models.
Note. Model output is displayed for moderations between total stressor endorsements and individual differences measures while covarying for baseline symptoms: (A) latent Patient-Reported Outcomes Measurement Information System (PROMIS) mental health distress, and (B) PROMIS Physical Health. Sub-figures on the left depict outcome scores at 7th, 16th, 33rd, 50th, 66th, and 84th, and 93rd percentiles. Sub-figures on the right depict the conditional effects of total stressor scores on changes in PROMIS scores using Johnson-Neyman-style plots. Bootstrap-estimated 95% confidence intervals are depicted.
Finally, neither the total number of internalizing disorders (main effect b = −.111, 95% CIboot [−.235, .022], β = −.058; moderation b = −.177, 95% CIboot [−1.097, .725], β = −.038) nor the total number of substance use disorders (main effect b = .097, 95% CIboot [−.042, .232], β =.047; moderation b = −.184, 95% CIboot [−1.289, .996], β = −.026) predicted longitudinal changes in PROMIS mental health distress.
Change in PROMIS Physical Health Distress
Number of days between Times 1 and 2 assessments was not associated with Time 2 PROMIS Global Physical Health scores (Tables 3 and S8). As expected, Time 1 physical health predicted Time 2 physical health. With Time 1 scores included as a covariate, EPII total stressor scores predicted a relative worsening of self-reported physical health over time. Independent of stressor scores, more frequent endorsements of Positive Change items (b = 1.400, 95% CIboot [.371, 2.430], β = .099) and fewer number of internalizing diagnoses (b = −.203, 95% CIboot [−.390, −.013], β = −.088) were associated with less perceived decline in physical health. Thus, these individual differences are consistent with longitudinal promotive and risk main effects, respectively, which occurred irrespective of pandemic-related stressor exposures.
Table 3.
Longitudinal Prediction of PROMIS Global Physical Health using Psychiatric Diagnoses.
| Bootstrap Results | ||||||
|---|---|---|---|---|---|---|
| 95% CI | ||||||
| Predictor | b | β | SE | p | LL | UL |
| Step 1 | ||||||
| Survey Interval | .000 | −.026 | .001 | .627 | −.001 | .001 |
| Step 2 | ||||||
| PROMIS Physical Health Time 1 | .730 | .679 | .034 | < .001 | .664 | .795 |
| Step 3 | ||||||
| EPII Stressor Loading | −5.464 | −.217 | .857 | < .001 | −7.103 | −3.730 |
| Step 4 (Risk/Promotive) | ||||||
| Internalizing Dx(s) | −.203 | −.088 | .094 | .035 | −.390 | −.013 |
| Substance Use Dx(s) | −.061 | −.025 | .091 | .502 | −.239 | .126 |
| Step 5 (Vulnerability/Protective) | ||||||
| EPII Stressor Loading * Internalizing Dx(s) | .677 | .093 | .760 | .375 | −.756 | 2.233 |
| EPII Stressor Loading * Substance Use Dx(s) | −1.560 | −.171 | .679 | .019 | −2.924 | −.225 |
| Step 5 Pruned | ||||||
| EPII Stressor Loading * Substance Use Dx(s) | −1.412 | −.158 | .656 | .031 | −2.741 | −.152 |
Note. b = unstandardized predictor coefficient, SE = standard error, CI = confidence interval, LL = lower limit, UL = upper limit, PROMIS = Patient-Reported Outcomes Measurement Information System, EPII = Epidemic-Pandemic Impacts Inventory, Dx = diagnosis. Boldface type indicates significant associations.
There was no main effect of the number of substance use disorders. However, the number of substance use disorders moderated stressor effects on physical health (b = −1.412, 95% CIboot [−2.741, −.152], β = −.165). Veterans without a diagnosis of a substance use disorder did not report changes in physical health as a function of stressor exposure (Figure 3B). In contrast, veterans with one or more substance use disorder diagnoses reported a stressor-related worsening of physical health. This indicates that pre-existing substance use disorders were a vulnerability factor for physical health outcomes associated with pandemic-related stressor experiences. No other moderator effects were observed for EPII Positive Change (b = 1.749, 95% CIboot [−4.860, 8.197], β = .038) or number of internalizing diagnoses (b = .677, 95% CIboot [−.756, 2.233], β = .108).
All model effects survived multiple comparison correction minus the following: main effect of internalizing diagnoses on physical health, moderation effect of Positive Change on mental health, and moderation effect of externalizing diagnoses on physical health.
Discussion
The present study identified novel resilience-related effects in the context of COVID-19 pandemic stressors among veterans with common mental disorders using developmental psychopathology methodology. As expected, greater exposure to recent pandemic stressors was associated with increases in both mental and physical health-related distress compared with pre-pandemic levels. These longitudinal findings match prior cross-sectional reports of pandemic-related mental health risks, which had been commonly attributed to an assortment of stressors (Alonzi et al., 2020; Czeisler et al., 2020). We extended these findings beyond convenience samples in the general population to treatment-seeking veterans with pre-existing psychopathology. Positive behavioral adaptations and number of internalizing diagnoses had stressor-independent promotive and risk main effects on changes in physical health distress. Critically, within these developmental psychopathology-informed resilience models, more endorsements of positive adaptations in attitudes and behaviors during the pandemic (EPII Positive Change) were protective against stressor effects on mental health distress (i.e., moderation). Also, substance use diagnoses increased vulnerability for stressor effects on self-reported physical health (i.e., moderation). Thus, it was positive behavioral adaptations and an absence of substance use diagnoses that best explained veterans’ stressor-dependent capacity for resilience during the COVID-19 pandemic in terms of mental and physical health distress, respectively.
This study underscores the clinical utility of identifying protective factors relevant to environmental stressors during the COVID-19 pandemic, especially with regard to personal behaviors that could be proactively encouraged (Aknin et al., 2022; Williams et al., 2021). For this cohort with preexisting psychiatric conditions, increasing endorsements of positive behavioral adaptations during the pandemic attenuated – or even eliminated for some veterans – pandemic-related stressor effects on mental health distress (see Figure 3A). Given our study’s naturalistic design, we cannot know if endorsements on this scale are causal or merely an epiphenomenon of some other process (e.g., greater ease of recalling positive behaviors). Still, it is important to note the face validity of some EPII Positive Change subscale items, which appear similar to evidence-based psychotherapeutic interventions such as behavioral activation (Dimidjian et al., 2011). Furthermore, the EPII Positive Change items assess individual willingness to pursue social interactions to increase a sense of interpersonal belonging. These positive behavioral adaptations may then lead to indirect effects on perceived social support, which is frequently associated with resilience in the developmental literature (Masten et al., 2021). When disruptions to clinical and community social support were experienced by veterans during the local shutdowns, purposeful maintenance of social connections and active cultivations of meaningful life experiences may have played an important role in reducing the impact of these negative life events on mental health.
In addition, we examined measurement invariance using the PROMIS Global Mental Health, Anxiety, and Depression scales; the longitudinal effects of COVID-19 stressor endorsement likely reflect true changes in the latent construct of mental health distress rather than measurement artifact. Our psychometric findings also supported the use of the EPII Positive Change scale and demonstrated how the item pool assesses a coherent domain of experiences. This increases interpretive weight for the study findings and highlights EPII Positive Change as an important domain for future study and targeted intervention. Positive coping behaviors, rather than being merely a main effect predictor of longitudinal changes (e.g., Shanahan et al., 2021), may be dynamically involved with buffering the impact of COVID-19 stressors on mental health. The study’s findings suggest that two individuals can experience the same relative amount of stressors and yet report different changes in mental health outcomes as a function of their active use of proactive behaviors. There is a need for research on how existing public health interventions could foster positive behavioral adaptations, as measured by EPII Positive Change, among people facing immediate stressors during the current COVID-19 pandemic. This measurement domain may point toward generalizable behavioral processes that mitigate the impact of many types of adverse life events (e.g., chronic physical illness, personal loss, local environmental catastrophes).
The number of substance use disorders conferred a specific vulnerability to a stressor-related worsening of physical health distress during the COVID-19 pandemic. The connection between psychological stressors and later physical health concerns is well-established (Friedman & Schnurr, 1995; Pizarro et al., 2006). Veterans with increasingly complex maladaptive substance use presentations may be particularly susceptible to the deleterious effects of COVID-19-related disruptions, which manifest through worsening perceptions of physical health. This substance use disorder finding addresses a need for specific markers of physical health vulnerabilities using a developmental psychopathology framework, albeit with older adults (Doom, 2021). Physical health should be a heightened assessment priority for veterans with addiction psychopathology. Increased substance use interventions and prevention outreach efforts may also be warranted when exposure to recent environmental stressors is anticipated among veterans. This could include additional emphasis on adaptive coping for stress and health issues beyond a sole focus on harm reduction. Future studies should probe the mechanisms through which increases in actual substance use during the pandemic are associated with changes in physical health (Ornell et al., 2020).
Pre-existing internalizing psychopathology diagnoses were associated with worsening of self-reported physical health independent of COVID-19 stressor scores, but we did not observe similar main effects for mental health distress. Accounting for pre-pandemic mental health distress while modeling longitudinal change likely eliminated stressor-independent associations between internalizing diagnoses and mental health outcomes. Many existing studies of pandemic effects do not include pre-pandemic measures of mental health to assess relative change. PROMIS measures are highly sensitive to internalizing psychopathology symptoms, which increases the confidence in the observed findings. Therefore, COVID-19 era cross-sectional studies of risks and vulnerabilities with respect to preexisting psychopathology have likely overestimated the effects by failing to model longitudinal change. Comprehensive characterizations of diagnostic subgroupings (e.g., HiTOP subfactors; Conway et al., 2019), or trait defensive responding (e.g., negative emotionality; Masten et al., 1999) may be necessary to fully appreciate potential moderation effects related to internalizing psychopathology.
We observed qualitatively similar main and moderation effect sizes for the various individual difference predictors in this study. Nevertheless, the p-values for the moderation effects did not survive multiple comparisons correction. This likely reflects the reality of survey research and the reduction in statistical power involved with trait-by-trait and trait-by-non-trait interactions (Vize et al., 2022). Despite including nearly four hundred participants, the study sample size may have been on the lower end for identifying moderation resilience effects in naturalistic experiments like the COVID-19 pandemic. More longitudinal studies of resilience with larger scale recruitment efforts are needed to capture a wide range of stressor exposures and individual differences necessary for moderation.
Despite the strengths of the present study, such as the relatively large sampling of veterans with preexisting psychiatric concerns, longitudinal design, well-validated symptom measures, and theory-driven analyses, there are important limitations. First, this study includes a limited scope of psychopathology dimensions, which precludes generalization of findings to people with other primary clinical symptoms (e.g., thought disorder, acute suicidal behavior). There is a need to examine whether the same resilience domains are relevant for other mental health outcomes, such as exacerbation of psychosis following environmental stressors (Mayo et al., 2017). Second, the present sample predominantly identifies as male, which is typical for veteran populations, but limits our ability to examine gender differences of resilience effects. In addition, responders were older, more likely to be married, and disproportionately served during the Vietnam War era relative to Operations Enduring and Iraqi Freedom (OEF/OIF) and Persian Gulf War eras. Given disproportionate COVID-19 infection and medical complication rates among people of color (Rozenfeld et al., 2020; Wortham, 2020), future studies should examine differences in resilience factors between people from diverse racial and ethnic backgrounds, as well as in other civilian populations. Third, data about pre-existing mental disorders were retrieved from the VA electronic medical records rather than independent, structured clinical interview assessments, which would have provided more fine-grained assessments of all active pre-existing psychopathology. Fourth, this study relied on self-report for assessing pandemic-related stressors, positive adaptations, and current mental health at Time 2, which may have led to assessment biases across the measures and limits causal interpretations. Corroboration using outside sources of information about real-world behaviors, symptomatology, and substance use could provide confirmation of the study’s effects. Finally, this survey was completed during summer of 2020. The relative effects of COVID-19-related stressor may have changed during later years of the pandemic.
In summary, veterans actively receiving outpatient mental health services at a large U.S. VA medical center responded to a comprehensive longitudinal survey during the early phases of the COVID-19 pandemic. By utilizing pre-pandemic quality improvement data, this study identified risk and protective factors relevant to changes in self-reported health in the context of environmental stressors. Positive behavioral adaptations and coping styles (e.g., increased physical activity, maintaining social connections) conferred a protective advantage against pandemic-related stressor effects on mental health. Similarly, the absence of substance use disorders was protective against the pandemic-related stressor effects on physical health. Thus, our use of a developmental psychopathology research framework revealed several individual difference domains that contribute to resilience outcomes. Future longitudinal research could examine whether specific types of environmental stressors (e.g., trauma, interpersonal or economic loss) pose greater risk effects on long-term mental and physical health trajectories, especially for veterans with common forms of internalizing psychopathology. Moreover, future investigations should assess the feasibility of enhancing resilience capacity by fostering positive behavioral coping styles in real-world settings during the COVID-19 pandemic era and beyond.
Supplementary Material
General Impact Statement:
Veterans from psychiatric outpatient clinics were assessed before and during the COVID-19 pandemic on measures of mental and physical health. Pandemic stressor exposures were associated with increased mental and physical health distress, but positive behavioral adaptations and a lack of preexisting substance use disorders conferred a protective buffering against stressor effects. Behavior activation and meaningful social connections may be important targets for enhancing resilience among veterans with preexisting psychopathology.
Acknowledgments
This quality improvement project was supported with resources and the use of facilities at the Minneapolis VA Health Care System. The content is solely the responsibility of the authors and does not necessarily represent the official views or policy of the U.S. Department of Veterans Affairs or the United States Government. The authors thank Amna Dogar for assistance with the literature review and Dr. Paul Thuras for assistance with the medical records data. Jessica Hill was supported by a Research Supplement to Promote Diversity in Health-Related Research through the National Center for Complementary & Integrative Health under award number UH3AT009651.
Footnotes
The authors have no known conflicts of interest to disclose.
References
- Abramson LY, Metalsky GI, & Alloy LB (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96(2), 358–372. 10.1037/0033-295X.96.2.358 [DOI] [Google Scholar]
- Ader D (2007). Developing the Patient-Reported Outcomes Measurement Information System (PROMIS). Medical Care, 45(5), S1–S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aknin LB, De Neve JE, Dunn EW, Fancourt DE, Goldberg E, Helliwell JF, … & Ben Amor Y (2022). Mental health during the first year of the COVID-19 pandemic: A review and recommendations for moving forward. Perspectives on Psychological Science, 17(4), 915–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonzi S, La Torre A, & Silverstein MW (2020). The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S236–S238. 10.1037/tra0000840 [DOI] [PubMed] [Google Scholar]
- Bendau A, Kunas SL, Wyka S, Petzold MB, Plag J, Asselmann E, & Ströhle A (2021). Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: The role of pre-existing anxiety, depressive, and other mental disorders. Journal of Anxiety Disorders, 79, 102377. 10.1016/j.janxdis.2021.102377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleil ME, Appelhans BM, Thomas AS, Gregorich SE, Marquez N, Roisman GI, Booth-LaForce C, & Crowder K (2021). Early life predictors of positive change during the coronavirus disease pandemic. BMC Psychology, 9(1), 83. 10.1186/s40359-021-00586-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA, Westphal M, & Mancini AD (2011). Resilience to Loss and Potential Trauma. Annual Review of Clinical Psychology, 7(1), 511–535. 10.1146/annurev-clinpsy-032210-104526 [DOI] [PubMed] [Google Scholar]
- Bonsaksen T, Heir T, Schou-Bredal I, Ekeberg Ø, Skogstad L, & Grimholt TK (2020). Post-Traumatic Stress Disorder and Associated Factors during the Early Stage of the COVID-19 Pandemic in Norway. International Journal of Environmental Research and Public Health, 17(24), 9210. 10.3390/ijerph17249210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA (2015). Confirmatory factor analysis for applied research. Guilford publications. [Google Scholar]
- Cobb AR, Lancaster CL, Meyer EC, Lee HJ, & Telch MJ (2017). Pre-deployment trait anxiety, anxiety sensitivity and experiential avoidance predict war-zone stress-evoked psychopathology. Journal of contextual behavioral science, 6(3), 276–287. 10.1016/j.jcbs.2017.05.002 [DOI] [Google Scholar]
- Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R, Mullins-Sweatt SN, Shackman AJ, Skodol AE, South SC, Sunderland M, Waszczuk MA, Zald DH, Afzali MH, Bornovalova MA, Carragher N, Docherty AR, Jonas KG, Krueger RF, … Eaton NR (2019). A Hierarchical Taxonomy of Psychopathology Can Transform Mental Health Research. Perspectives on Psychological Science, 14(3), 419–436. 10.1177/1745691618810696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA, Howard ME, & Rajaratnam SMW (2020). Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049–1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Barrera M, Martell C, Muñoz RF, & Lewinsohn PM (2011). The Origins and Current Status of Behavioral Activation Treatments for Depression. Annual Review of Clinical Psychology, 7(1), 1–38. 10.1146/annurev-clinpsy-032210-104535 [DOI] [PubMed] [Google Scholar]
- Doom J (2021). Advantages of a Developmental Psychopathology Approach to Studying the Antecedents of Physical Health. OSF Preprints. 10.31219/osf.io/egkbx [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen SV, Schultz MR, Glickman ME, Vogt D, Martin JA, Osei-Bonsu PE, Drainoni M-L, & Elwy AR (2014). Postdeployment Resilience as a Predictor of Mental Health in Operation Enduring Freedom/Operation Iraqi Freedom Returnees. American Journal of Preventive Medicine, 47(6), 754–761. 10.1016/j.amepre.2014.07.049 [DOI] [PubMed] [Google Scholar]
- Fein-Schaffer D, Hawn SE, Annunziata AJ, Ryabchenko K, Miller MW, & Wolf EJ (2022). Premorbid traumatic stress and veteran responses to the COVID-19 pandemic. Journal of traumatic stress, 35(2), 559–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MJ, & Schnurr PP (1995). The relationship between trauma, post-traumatic stress disorder, and physical health. In Neurobiological and clinical consequences of stress: From normal adaptation to post-traumatic stress disorder (pp. 507–524). Lippincott Williams & Wilkins Publishers. [Google Scholar]
- Galea S, Merchant RM, & Lurie N (2020). The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Internal Medicine, 180(6), 817–818. 10.1001/jamainternmed.2020.1562 [DOI] [PubMed] [Google Scholar]
- Garmezy N, Masten AS, & Tellegen A (1984). The Study of Stress and Competence in Children: A Building Block for Developmental Psychopathology. Child Development, 55(1), 97–111. 10.2307/1129837 [DOI] [PubMed] [Google Scholar]
- Grasso DJ, Briggs-Gowan MJ, Carter AS, Goldstein BL, & Ford JD (2021). Profiling COVID-related experiences in the United States with the Epidemic-Pandemic Impacts Inventory: Linkages to psychosocial functioning. Brain and Behavior. 10.1002/brb3.2197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasso DJ, Briggs-Gowan MJ, Ford JD, & Carter AS (2020). The Epidemic— Pandemic Impacts Inventory (EPII) [Https://www.phenxtoolkit.org/toolkit_content/PDF/Grasso_EPII.pdf]. U.S. National Library of Medicine. https://www.nlm.nih.gov/dimrc/disasterinfo.html [Google Scholar]
- Haydon KC, & Salvatore JE (2021). A Prospective Study of Mental Health, Well-Being, and Substance Use During the Initial COVID-19 Pandemic Surge. Clinical Psychological Science. 10.1177/21677026211013499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Bjorner JB, Revicki DA, Spritzer KL, & Cella D (2009). Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Quality of Life Research, 18(7), 873–880. 10.1007/s11136-009-9496-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Spritzer KL, Schalet BD, & Cella D (2018). PROMIS®−29 v2.0 profile physical and mental health summary scores. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 27(7), 1885–1891. 10.1007/s11136-018-1842-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, … Bullmore E (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, & Prescott CA (1999). Causal Relationship Between Stressful Life Events and the Onset of Major Depression. American Journal of Psychiatry, 156(6), 837–841. 10.1176/ajp.156.6.837 [DOI] [PubMed] [Google Scholar]
- Kraker D, & Porter S (2020). MN’s stay-at-home order: What you need to know. MPR News. https://www.mprnews.org/story/2020/03/25/minnesotas-covid19-stayathome-order-what-you-need-to-know [Google Scholar]
- Luthar S, Cicchetti D, & Becker B (2000). The Construct of Resilience: A Critical Evaluation and Guidelines for Future Work. Child Development, 71(3), 543–562. 10.1111/1467-8624.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken LM, Badinlou F, Buhrman M, & Brocki KC (2020). Psychological impact of COVID-19 in the Swedish population: Depression, anxiety, and insomnia and their associations to risk and vulnerability factors. European Psychiatry, 63(1). doi: 10.1192/j.eurpsy.2020.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS (2001). Ordinary magic: Resilience processes in development. American Psychologist, 56(3), 227. 10.1037/0003-066X.56.3.227 [DOI] [PubMed] [Google Scholar]
- Masten AS, Hubbard J, Gest S, Tellegen A, Garmezy N, & Ramirez M (1999). Competence in the context of adversity: Pathways to resilience and maladaptation from childhood to late adolescence. Development and Psychopathology. 10.1017/S0954579499001996 [DOI] [PubMed] [Google Scholar]
- Masten AS, Lucke CM, Nelson KM, & Stallworthy IC (2021). Resilience in development and psychopathology: Multisystem perspectives. Annual Review of Clinical Psychology, 17, 521–549. [DOI] [PubMed] [Google Scholar]
- Masten AS, & Narayan AJ (2012). Child Development in the Context of Disaster, War, and Terrorism: Pathways of Risk and Resilience. Annual Review of Psychology, 63(1), 227–257. 10.1146/annurev-psych-120710-100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, & Tellegen A (2012). Resilience in developmental psychopathology: Contributions of the Project Competence Longitudinal Study. Development and Psychopathology, 24(2), 345–361. 10.1017/S095457941200003X [DOI] [PubMed] [Google Scholar]
- Mayo D, Corey S, Kelly LH, Yohannes S, Youngquist AL, Stuart BK, Niendam TA, & Loewy RL (2017). The Role of Trauma and Stressful Life Events among Individuals at Clinical High Risk for Psychosis: A Review. Frontiers in Psychiatry, 8. 10.3389/fpsyt.2017.00055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell F, Moura HF, Scherer JN, Pechansky F, Kessler FHP, & von Diemen L (2020). The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Research, 289, 113096. 10.1016/j.psychres.2020.113096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne TF, Veigulis ZP, Arreola DM, Röösli E, & Curtin CM (2020). Automated EHR score to predict COVID-19 outcomes at US Department of Veterans Affairs. PLOS ONE, 15(7), e0236554. 10.1371/journal.pone.0236554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL, Finkelstein-Fox L, Russell BS, Fendrich M, Hutchison M, & Becker J (2021). Americans’ distress early in the COVID-19 pandemic: Protective resources and coping strategies. Psychological Trauma: Theory, Research, Practice, and Policy, 13(4), 422–431. 10.1037/tra0000931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizarro J, Silver RC, & Prause J (2006). Physical and Mental Health Costs of Traumatic War Experiences Among Civil War Veterans. Archives of General Psychiatry, 63(2), 193–200. 10.1001/archpsyc.63.2.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polusny M, Erbes C, Kramer M, Thuras P, DeGarmo D, Koffel E, Litz B, & Arbisi P (2017). Resilience and Posttraumatic Stress Disorder Symptoms in National Guard Soldiers Deployed to Iraq: A Prospective Study of Latent Class Trajectories and Their Predictors. Journal of Traumatic Stress, 30(4), 351–361. 10.1002/jts.22199 [DOI] [PubMed] [Google Scholar]
- Ridley M, Rao G, Schilbach F, & Patel V (2020). Poverty, depression, and anxiety: Causal evidence and mechanisms. Science. 10.1126/science.aay0214 [DOI] [PubMed] [Google Scholar]
- Rozenfeld Y, Beam J, Maier H, Haggerson W, Boudreau K, Carlson J, & Medows R (2020). A model of disparities: Risk factors associated with COVID-19 infection. International Journal for Equity in Health, 19(1), 126. 10.1186/s12939-020-01242-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz JG, Priyadarshni S, Rahaman Z, Cabrera K, Dang S, Valencia WM, & Mintzer MJ (2018). Validation of an automatically generated screening score for frailty: The care assessment need (CAN) score. BMC Geriatrics, 18(1), 106. 10.1186/s12877-018-0802-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L, Steinhoff A, Bechtiger L, Murray AL, Nivette A, Hepp U, Ribeaud D, & Eisner M (2021). Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine, 1–10. 10.1017/S003329172000241X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiner RL, & Masten AS (2012). Childhood personality as a harbinger of competence and resilience in adulthood. Development and Psychopathology, 24(2), 507–528. 10.1017/S0954579412000120 [DOI] [PubMed] [Google Scholar]
- Vahratian A, Blumberg SJ, Terlizzi EP, & Schiller JS (2021). Symptoms of Anxiety or Depressive Disorder and Use of Mental Health Care Among Adults During the COVID-19 Pandemic. Morbidity and Mortality Weekly Report, 70(13), 490–494. 10.15585/mmwr.mm7013e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vize CE, Sharpe BM, Miller JD, Lynam DR, & Soto CJ (2022). Do the Big Five personality traits interact to predict life outcomes? Systematically testing the prevalence, nature, and effect size of trait-by-trait moderation. European Journal of Personality. 10.1177/08902070221111857. [DOI] [Google Scholar]
- Wang L, Porter B, Maynard C, Evans G, Bryson C, Sun H, Gupta I, Lowy E, McDonell M, Frisbee K, Nielson C, Kirkland F, & Fihn SD (2013). Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Medical Care, 51(4), 368–373. 10.1097/MLR.0b013e31827da95a [DOI] [PubMed] [Google Scholar]
- Williams L, Rollins L, Young D, Fleming L, Grealy M, Janssen X, Kirk A, MacDonald B, & Flowers P (2021). What have we learned about positive changes experienced during COVID-19 lockdown? Evidence of the social patterning of change. PLOS ONE, 16(1). 10.1371/journal.pone.0244873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood M (2005). Bootstrapped Confidence Intervals as an Approach to Statistical Inference. Organizational Research Methods, 8(4), 454–470. 10.1177/1094428105280059 [DOI] [Google Scholar]
- Wortham JM (2020). Characteristics of Persons Who Died with COVID-19. MMWR. Morbidity and Mortality Weekly Report, 69. 10.15585/mmwr.mm6928e1 [DOI] [PubMed] [Google Scholar]
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, & McIntyre RS (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X-H, Yu H-J, Liu M-W, Zhang J, Tang B-W, Yuan S, Gasevic D, Paul K, Wang P-G, & He Q-Q (2020). The impact of a health education intervention on health behaviors and mental health among Chinese college students. Journal of American College Health, 68(6), 587–592. 10.1080/07448481.2019.1583659 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


