Abstract
Introduction
Fractures of the zygomatic-maxillary complex (ZMC) are common facial fractures. After adequate fracture reduction, it is important to maintain stability and rigid fixation to avoid functional impairment and aesthetic sequelae. In this sense, the fixation of just one point can provide sufficient stability of the ZMC fracture when the ZMC fracture is not crushed.
Objective
To analyze the success rates of fracture stability of the ZMC, incidences of complications, and aesthetic satisfaction after 1-point fixation.
Methods
This study followed the rules of PRISMA, with publications from 2010 to 2020. The chi-square test and the Poisson probability test were performed to the occurrence of complications Low = 1, Moderate = 2, and NO = 0, adopting the α-level less than 0.05 with a statistical difference for 95% CI. The R-sq (R2) value was also analyzed among the complications variables.
Results
The results of these studies showed in a general way that the use of 1-point fixation with open reduction presented good results in the short, medium, and long term, showing fracture stability. Complication rates were low and patients' satisfaction with aesthetics was considerable.
Conclusion
The success rate of the 1-point fixation procedure for the zygomatic-maxillary complex is high, with minimal complications.
Keywords: Zygomatic-maxillary complex, 1-point fixation, Fracture stability, Complications, Aesthetics
Introduction
In the scenario of facial trauma, fractures of the zygomatic-maxillary complex (ZMC) are common facial fractures. Annually, 5.8 million people die from trauma worldwide [1]. Trauma mortality accounts for 10% of all causes of death. Thus, trauma is a worldwide public health problem. Still, trauma is the main cause of death among patients aged 1 to 44 years, and the fourth major cause considering all age groups. According to WHO data, head and face injuries can represent half of the traumatic deaths [1].
In this context, the ZMC is an important structure, serving as an important buttress of the middle third of the face. The ZMC also aesthetically projects anterolaterally to form the malar eminence and establish the width and medial-facial contour of the orbital border [2]. Attempts to treat ZMC fractures are to achieve stability and restore aesthetic appearance through three-dimensional reduction and rigid fixation. After adequate fracture reduction, it is important to maintain stability and rigid fixation to avoid functional impairment and aesthetic sequelae. Thus, open reduction and internal fixation have been used as a standard method for the treatment of these fractures [3].
Therefore, several surgical and technical procedures, including fixation of one, two, and three points, are used according to the severity and extent of ZMC fractures [4]. Among these techniques, some authors argue that fixation of just one point provides sufficient stability of the ZMC fracture when the ZMC fracture is not crushed [5, 6]. At the moment, it is not yet clear which treatment, fixation of one point, fixation of two points, or fixation of three points, is better [7]. In addition, there is a growing interest in minimally invasive procedures and concerns about scarring, further highlighting the use of fixing 1-point. Thus, fixing 1-point of the ZMC through a gingivobuccal incision has the advantage of not leaving an external scar [8, 9].
In this sense, the main indications for the use of fixation at 1-point of types of the fracture are minimal or moderate displacement of the infraorbital border in the zygoma tripod fracture, no ocular sign of diplopia or enophthalmos, and comminuted infraorbital edge fractures in which internal fixation is difficult [10]. Successful repair requires not only an accurate diagnosis but also a careful consideration of the complex three-dimensional anatomy because even minimally displaced fractures in the ZMC can result in functional and aesthetic deformities [10].
Therefore, the present study aimed to analyze, through a meta-analysis, the success rates of fracture stability of the Zygomatic-maxillary complex, incidences of complications, and aesthetic satisfaction after 1-point fixation in relation to the minimal or moderate displacement of the infraorbital border in the zygoma tripod fracture, in the ocular sign of diplopia or enophthalmos, and comminuted infraorbital edge fractures.
Methods
Study Design
This study followed the international rules of PRISMA's Systematic Review and Meta-analysis [11]. Table 1 shows the main variables of the present study that will be addressed according to the classification of the acronym PICOS (P = Patients; I = Intervention; C = Control; O = Outcomes; S = Study design).
Table 1.
PICOS (Patients; Intervention; Control; Outcomes; Study design)
| Patients | Adults with zygomaticomaxillary complex fractures (quadripod fracture, quadramalar fracture, tripod fracture, or trimalar fracture); unilateral or bilateral factures |
| Intervention | 1-point fixation (frontozygomatic region /zygomaticomaxillary region or infraorbital region) with or without mini plates |
| Control | Different types of plates; Use of three-dimensional photogrammetric analysis; Use of ultrasound-guided technique |
| Outcomes | Patient satisfaction with function and aesthetics results; Stable fracture fixation; Pain; Quality of life; Surgical complications; Masticatory force |
| Study design | Randomized controlled trials; Prospective and retrospective studies |
Data Sources and Research Strategy
The research was carried out in June 2020 and developed at SCOPUS (Elsevier and non-Elsevier database), PubMed, OVID, Cochrane Library, life science magazines, and online books, including the National Institutes of Health RePORTER Grant database and Clinical Trial Records. The search strategies for this systematic review and meta-analysis were based on the MeSH Terms “Zygomatic maxillary complex. 1-point fixation. Single point fixation. One point fixation. Fracture stability. Complications. Aesthetics,” with publications from 2010 to 2020, to analyze the most recent scientific publications. Also, a combination of the keywords with the Booleans “OR,” AND and the operator “NOT” was used to target scientific articles of interest. The title and abstracts will be examined under all conditions. The research structure used in the databases is shown in Table 2.
Table 2.
Example of the research structure in PubMed as a model
| PubMed | Zygomatic-maxillary complex OR Fracture OR 1-point fixation OR Single-point fixation OR 1-point fixation |
| AND | |
| PubMed | Fracture stability OR Complications OR Aesthetic OR Masticatory force |
| NOT | |
| PubMed | Case report OR 2 to 4 point fixings |
Selection of Studies: Eligibility
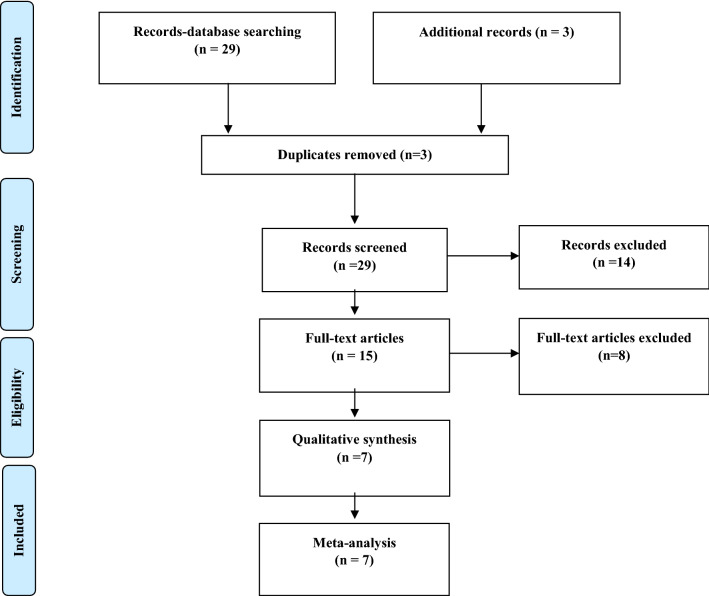
The inclusion criteria were clinical studies published from 2010 to 2020 on fractures of the ZMC and treatment with 1-point fixation, with open or closed reduction, and with the use of bioabsorbable plates or not. Exclusion criteria were case report studies, review studies, and meta-analysis or clinical studies that presented discreet results. Thirty-two scientific articles have been found at the clinical level. After applying the article selection filter, 15 articles have been found, of which only seven articles are strictly related to the analysis criteria of the present study to compose the meta-analysis (Fig. 1).
Fig. 1.
Flowchart
Risk of Bias
According to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria, the quality of the evidence was classified as high, moderate, low, or very low, according to the risk of bias, clarity of comparisons, precision, and consistency of the analyzes. The randomized controlled clinical trials (RCTs) have given the highest preference, as it provides high scientific evidence. The quality of the evidence was reduced to moderate if one of the four criteria of quality of the evidence had not been met and lower if 2 or more were not met. Low quality of evidence was attributed to case reports, editorials, and short communications. The Cochrane instrument was to be adopted to assess the risk of bias of the included studies [12].
Summary of Literary Findings
The present study had some limitations as few clinical studies in the last 10 years on 1-point fixation in the ZMC (n = 7), with three studies being retrospective and three were prospective, and only one study was randomized.
Statistical Analysis
For data analysis, a database has built on the Microsoft Excel spreadsheet which has exported to the Minitab 18® statistical program (version 18, Minitab, LLC, State College, Pennsylvania, USA) (Minitab®) and also to the OriginPro® 9 (DPR Group, Inc., Northampton, Massachusetts, USA). A common descriptive statistical analysis was performed, obtaining the values of total n, mean and standard deviation, confidence interval (CI), and percentage for all the variables. The chi-square and the Poisson probability test were performed to the occurrence of complications Low = 1, Moderate = 2, and NO = 0, adopting the α-level less than 0.05 with a statistical difference for 95% CI. The R-sq (R2) value was also analyzed among the complications variables, with the codes being adopted, low association = < 25%, medium association 25% < X < 50% and high association = > 50%.
Results of Meta-analysis
After the application of the descriptors (MeSH Terms) in the databases presented in the item data sources and research strategy, 32 scientific articles were found at the clinical level. After applying the article selection filter for the last 10 years, 15 articles have been found, of which only seven articles are strictly related to the objective of the present study and entered the meta-analysis.
Table 3 presents the general data of each study analyzed, such as type of study, some patients in each study, the types of fixation points used, highlighting the priority for the analysis of 1-point fixation, the main results of each study, and the follow-up or period of analysis of each study. It also presents, in a manner described below, in Table 3, which were the main complications presented in some of the studies. Two of the studies used biodegradable plates to compare fracture stability with other plates. Also, fixing 1-point on the ZMC can prevent unpleasant scarring and provide high satisfaction in patients with tripod fractures, with this location and modality of use with 1-point fixation being the most favorable found in the literature.
Table 3.
General data of the selected studies to compose the meta-analysis
| Authors (n = 7) /Major points and results | Type of Study | N patients | Procedures (Fixings-Points) | Major Results | Follow-up or Analysis period |
|---|---|---|---|---|---|
| Shokri et al. [6] | Prospective | 162 | 1 | The ZMC fracture responded well with the 1-point fixation | 3.4 months |
| Panchanathan et al. [8] | Controlled prospective | 40 (n = 20 control) |
1 (n = 4) 2 (n = 12) 3 (n = 4) |
Increased bite strength and muscle activity | 6 months |
| Kim et al. [9] | Retrospective | 30 |
1 (n = 14) 2 (n = 16) |
There was no statistical difference between the three types of fixation | Evaluation of 5-year medical records |
| Hwang [10] | Retrospective | 14 | 1 | Fixing 1-point on the ZMC can prevent unpleasant scarring and provide high satisfaction in patients with tripod fractures | Evaluation of 1.5-year medical records |
| Kim et al. [14] | Retrospective | 34 | 1* | The deformities of the steps of the infraorbital edges were improved | Evaluation of medical records of 9 months |
| Sato et al. [15] | Prospective | 24 | 1** | All patients were satisfied with the postoperative appearance | 6 months |
| Tripathi et al. [16] | Randomized | 20 | 1*** | All patients achieved satisfactory bone stability and a symmetrical malar appearance | 6 months |
*7 experienced intraoral plate exposure, with 2 subsequently in exchange for plate complications, 8 infections
**Group I: Titanium. Swelling was observed in all patients on the first postoperative day. Diplopia was observed in 5% of patients for 3 months in subgroup A. Palpability was also observed in 5% of cases in subgroup B for 6 months. On the contrary, enophthalmos, paraesthesia, screw breakage, plate exposure, infection at the site, malocclusion, and thermal sensitivity were not observed in the postoperative period and the bite efficiency of all patients was normal in the postoperative period
**Group II: Biomaterial. As the postoperative complication found in group II, swelling was observed in all patients on the first postoperative day. Diplopia was observed in 10% of patients, screw loosening was observed in 10% of the patient at the time of surgery, plate exposure and infection at the site was observed in 10% of cases in the 6-month review. On the contrary, enophthalmos, paresthesia, palpability, thermal sensitivity, and malocclusion were not observed in any patient in the postoperative period. Bite efficiency was considered normal in all patients
***n = 10 with titanium plates and n = 10 with biodegradable plates
Table 4 shows in quantitative terms the main complications in each study, using the numeric codes Low = 1, Moderate = 2, and NO = 0, as well as showing the success rates related to each study technique, highlighting that in one study the technique was used by three-dimensional photogrammetric analysis and in another study the ultrasound-guided technique was used and titanium and biodegradable plates were used.
Table 4.
Data on the findings of complications and success rate of the studies addressed
| Authors | Complications (Low = 1, Moderate = 2, and NO = 0) | Technique success Rate (%) |
|---|---|---|
| Shokri et al. [6] | 2 | 90.0 |
| Panchanathan et al. [8] | 0 | 74.2 |
| Kim et al. [9] | 0 | 100 |
| Hwang [10] | 0 | 100 |
| Kim et al. [14]* | 0 | 100 |
| Sato et al. [15] | 0 | 100 |
| Tripathi et al. [16]** | 1 | 70 |
*Used non-sintered hydroxyapatite (u-HA) / poly-L-lactide (PLLA) plates and three-dimensional photogrammetric analysis
**Guided by ultrasound and used titanium and biodegradable plates
After the statistical analysis to find out what the associations were between the complications of the studies by the chi-square test, the results showed that there was no statistical difference between them, with p = 0.305 > 0.05 and R2 = 55.2% (high association). In addition, using the Poisson probability test, it was found that the probability of complications Low = 1, Moderate = 2 and NO = 0 was 0.65, 0.28 and 0.07, respectively (Table 5). This same table shows that the frequency of occurrence of NO-Complication was 5 (71.43%), Low-Complication was 1 (14.29%), and Moderate-Complication was 1 (14.29%).
Table 5.
Statistical results of the chi-square analysis, Poisson probability, frequency and percentage of occurrence of the levels of complications, with p < 0.05 with statistical difference, CI95%
| Complications (Low = 1, Moderate = 2 and NO = 0) | Poisson | ||
|---|---|---|---|
| Probability | Frequency | Percent(%) | |
| 0 | 0.65 | 5 | 71.43 |
| 1 | 0.28 | 1 | 14.29 |
| 2 | 0.07 | 1 | 14.29 |
Chi-square test
p value = 0.305 > 0.05
R2 = 55.2%
Figure 2 shows the graph with data on frequency, probability, and percentage of occurrence of complications.
Fig. 2.
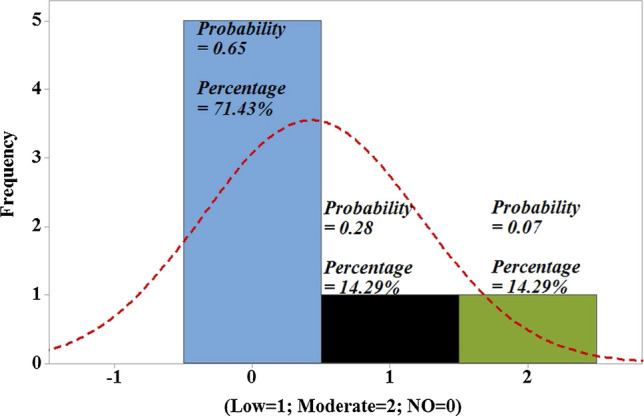
Graph showing the comparisons between the levels of complications, being Low = 1, Moderate = 2 and NO = 0
Discussion
The present study presented the state-of-the-art with the presentation of a meta-analysis of the last 10 years of publications of clinical studies on the use of 1-point fixation for fractures of the ZMC, both with the use of non-absorbable plates and bioabsorbable. The results of these studies showed in general that the use of 1-point fixation showed good results in the short, medium, and long term, showing fracture stability, with open or closed reduction. Complication rates were low and patient satisfaction with aesthetics was considerable.
The studies of the present work also showed that the use of three-dimensional photogrammetric analysis and the ultrasound-guided technique can significantly favor the procedure and, in addition, they also showed that the use of biodegradable plates can offer good advantages since they showed equal fracture stability when compared to conventional plates. In this sense, achieving satisfactory results in the treatment of complex fractures of the ZMC involves a series of decisions, including the approach of the zygomatic arch as the main point of treatment.
In this context, the ZMC plays a fundamental role in the structure, function, and aesthetic appearance of the facial skeleton, influencing approximately 40% of fractures of the middle face, constituting the second most common facial bone fracture, after the nasal bones [3]. The fracture complex results from a direct impact on the malar eminence and results in three distinct fracture components that interrupt the anchorage of the zygoma, also resulting in temporal muscle shock, trismus, and compromising the foramen/infraorbital nerve [13].
In this sense, a study carried out a 4-year retrospective review of 245 patients treated for fractures in the ZMC. Closed or open reduction methods were performed with the aim of treating the preservation of the normal facial structure, sensory function, globe position, and chewing functionality. As a result, postoperative infection rates were extremely low and the long-term prognosis after repair of ZMC fractures was very good [5].
In this regard, no clinical consensus has been established regarding the number of fixation points required together with open or closed reduction. A retrospective study of 211 patients over a 20-year period looked at the usefulness of single-point fixation in the treatment of ZMC fractures. The average follow-up time was 3.4 months. Of the 211 patients, 162 with ZMC fractures were treated with single-point fixation. During the follow-up period, one patient suffered tooth loss due to a root present in the fracture line, 7 experienced intraoral exposure of the plate, with 2 subsequently in exchange for the plate, and 8 developed wound infection. No patient required surgery or other procedures for malar asymmetry. No patient developed hypoglobus or enophthalmos, and none required a review of the internal fracture fixation [6]. Despite this, there are still biases regarding exposure to reduction and anatomical fixation required during open reduction and internal fixation of ZMC fractures [7].
Also, a prospective controlled study evaluated the functionality of the masseter and temporal muscles after fractures of the ZMC, evaluating the strength of the bite, the electromyography (EMG), and the mandibular movements for a period of 6 months. Group I consisted of 20 patients with unilateral fractures of the ZMC who were treated surgically with fixations of one, two, or three points. The control group (group II) included 20 normal patients. The evaluation consisted of measuring the bite force, EMG analysis of the masseter and temporal muscles, and measures of the mandibular movements. There was an increase in bite strength and electromyographic activity throughout the evaluated postoperative period, with a slight reduction in relation to the control groups. The maximum mouth opening increased considerably after surgery. According to the bite force and EMG, the masticatory muscles returned to almost normal levels in the third month after surgery, mainly with 1-point fixation [8].
Fracture of the zygomatic tripod is common and usually requires open fixation with internal reduction. However, lateral incisions of the eyebrow sometimes leave scars and, therefore, 1-point fixation in the ZMC can be used through a mucogingival incision to improve aesthetics. Thus, a 5-year retrospective study with 30 patients compared the fixation of 1 point in the ZMC with the fixation of 2 points in the ZMC and frontozygomatic (FZ) areas in tripod fractures. Thus, 14 patients received fixation of 1 point in the ZMC (group 1), 1 of whom had bilateral tripod fractures, and 16 patients with fixation of 2 points in the ZM and FZ area (group 2). Of the 16 patients in group 2, 10 (63%) complained of ugly scars at the site of the lateral incision of the eyebrow, while none of the patients in group 1 complained of external scars. In both groups, none of the patients complained of bone movement and pain in the FZ area. In group 2, 25% of the patients complained of palpability in the FZ area, however, in group 1 no one complained. The satisfaction score for the surgery was 9.4 ± 1.6 in group 1 and 7.7 ± 2.6 in group 2 (p < 0.05). In addition, two patients underwent surgery to remove plate in group 2 [9].
One study analyzed the cases of lateral incision of the forehead and fixation of 1 point in 70 patients with tripod fractures. Of these, 14 patients (20%) underwent the 1-point fixation technique. Seven cases (50%) were type III, six cases (43%) type IV, and one (7%) type V, according to the North Classification (Knight). A simple fracture of the infraorbital border was observed in ten patients (71%) and the crushed fracture was observed in four patients (29%). In 11 patients, the front zygomatic sutures were fixed with square microplates with 4 holes and 0.5 mm thick, and straight mini plates with 4 holes and 1.0 mm thick were used in three patients. Of the 14 tripod fractures, six (43%) were associated with floor fractures. Seven had a displacement of the infraorbital border, and the other seven had no displacement of the infraorbital border. After surgery, the deformities of the steps at the infraorbital edges were improved. Still, all patients were satisfied with the aesthetic [10].
Another 2019 retrospective study evaluated the results of stability and aesthetic appearance of fixing 1-point using a three-dimensional photogrammetric analysis (three-dimensional camera (Morphius®)). In 9 months of medical record analysis, 34 patients with ZMC fractures were treated by fixing 1-point on the ZMC using non-sintered hydroxyapatite (u-HA)/poly-L-lactide (PLLA) plates. Differences in soft tissue inter-malar height between the fractured and non-fractured sides were assessed by photogrammetric analysis preoperatively and 1 week, 1 and 3 months after surgery. All patients achieved satisfactory bone stability and asymmetrical malar appearance. There was no statistically significant difference between 1 and 3 months, only between before and 6 months after surgery [14].
Besides, a prospective study with 24 patients analyzed the precision and postoperative stability of 1-point ultrasound-guided fixation in the ZMC for the treatment of fractures. The authors used titanium plates in the first 6 cases and biodegradable plates in the remaining 18 cases. The results suggested that the fixation of 1 point guided by ultrasound in the ZMC can provide an accurate reduction of the fractures of the ZMC without the separation of the frontal process of the fracture of the zygomatic bone. Also, fracture stability has been established, even with the use of biodegradable plates [15].
Also, a randomized study with 20 patients compared the fracture stability of the ZMC using biodegradable plates and titanium mini plates with fixation at one point. Group I patients were treated with a titanium miniplate in the ZMC and group II was treated with bioresorbable plates. The fixation of 1-point was performed in the ZMC or in the frontozygomatic suture and it was observed that the site has been the most preferred for rigid internal fixation in terms of stability, aesthetics, and prevention of rotation of the fracture segment, vertical or horizontal axis. There was no significant difference in postoperative results between the two groups, but the system still bioresorbable has some advantage over the titanium system, as these plates reabsorb for a period of time and do not interfere with growth and postoperative radiotherapy [16].
The reduction and fixation of the zygomatic arch is a key point in the treatment of complex fractures of the ZMC. The fixation of the miniplate and screw of this fracture requires a great detachment of soft tissues, being technically more difficult for an adequate fixation, and increasing the risk of damage to soft tissues. Therefore, a study described an operative approach to fix this type of fracture using an adaptation of the delay screw technique. After the initial reduction of the zygomatic bone, the proximal segment of the zygomatic arch containing the sagittal fracture is anatomically reduced and a 2.0 mm titanium screw is placed with a lower inclination of 10° to 15° in the mastoid cells of the temporal bone, thus avoiding the placement of intracranial screws. Thus, excellent results were presented in reduction and long-term stability and with fixation of 1-point, facilitating the surgical procedure, reducing the risk of damage to soft tissues, and reducing costs in comparison with the conventional miniplate and fixation by screws [17].
Conclusion
The present study showed that the success rate of the 1-point fixation procedures for the zygomatic-maxillary complex is high, with minimal complications.
Limitations
Despite the satisfactory results presented on the 1-point fixation technique of the zygomatic-maxillary complex, the present study had some limitations as few studies on the 1-point fixation, a limited number of studied patients, and presented three retrospective studies, three prospective and only one randomized study.
Acknowledgement
We appreciate all the financial support and research support from Prevent Senior, Health plan, São Paulo/SP, Brazil.
Declarations
Conflicts of interest
The authors declare nothing and all authors are aware of the article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.PAHO/WHO-Pan American Health Organization/World Health Organization. Available in: https://www.paho.org/bra/index.php?option=com_content&view=article&id=2989:traumas-matam-mais-que-as-tres-grandes-endemias-malaria-tuberculose-e-aids&Itemid=839. Accessed in 29 May 2020
- 2.Sharma R, Muralidharan CG, Roy ID, Jain NK, Patrikar S. Radiological evaluation of sphenozygomatic suture fixation for restoration of orbital volume: a retrospective study. J Craniomaxillofac Surg. 2016;44(12):1903–1908. doi: 10.1016/j.jcms.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Abbas A, Syed IB, Abbas H, Abbas I. Paradigm in aetiology and management of zygomatic complex fractures in Pakistan. J Ayub Med Coll Abbottabad. 2012;24(3–4):193–196. [PubMed] [Google Scholar]
- 4.Olate S, Lima SM, Jr, Sawazaki R, Moreira RW, de Moraes M. Surgical approaches and fixation patterns in zygomatic complex fractures. J Craniofac Surg. 2010;21(4):1213–1217. doi: 10.1097/SCS.0b013e3181e1b2b7. [DOI] [PubMed] [Google Scholar]
- 5.Balakrishnan K, Ebenezer V, Dakir A, Kumar S, Prakash D. Management of tripod fractures (zygomaticomaxillary complex) 1 point and 2 point fixations: a 5-year review. J Pharm Bioallied Sci. 2015;7(Suppl 1):S242–S247. doi: 10.4103/0975-7406.155937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shokri T, Sokoya M, Cohn JE, Bahrami A, Inman J, Ducic Y. Single-point fixation for noncomminuted zygomaticomaxillary complex fractures-A 20-year experience. J Oral Maxillofac Surg. 2020;78(5):778–781. doi: 10.1016/j.joms.2019.12.030. [DOI] [PubMed] [Google Scholar]
- 7.Jazayeri HE, Khavanin N, Yu JW, Lopez J, Shamliyan T, Peacock ZS, Dorafshar AH. Fixation points in the treatment of traumatic zygomaticomaxillary complex fractures: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2019;77(10):2064–2073. doi: 10.1016/j.joms.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 8.Panchanathan S, Saranathan M, Kamalakaran AK, Duraisamy K. Functional evaluation of the behavior of masticatory muscles in zygomaticomaxillary complex fracture: a prospective study. J Contemp Dent Pract. 2016;17(6):463–469. doi: 10.5005/jp-journals-10024-1873. [DOI] [PubMed] [Google Scholar]
- 9.Kim ST, Go DH, Jung JH, Cha HE, Woo JH, Kang IG. Comparison of 1-point fixation with 2-point fixation in treating tripod fractures of the zygoma. J Oral Maxillofac Surg. 2011;69(11):2848–2852. doi: 10.1016/j.joms.2011.02.073. [DOI] [PubMed] [Google Scholar]
- 10.Hwang K. One-point fixation of tripod fractures of zygoma through a lateral brow incision. J Craniofac Surg. 2010;21(4):1042–1044. doi: 10.1097/SCS.0b013e3181e48607. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins J, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration
- 13.Ji SY, Kim SS, Kim MH, Yang WS. Surgical methods of zygomaticomaxillary complex fracture. Arch Craniofac Surg. 2016;17(4):206–210. doi: 10.7181/acfs.2016.17.4.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim SY, Nam SM, Park ES, Kim YB. Evaluation of one-point fixation for zygomaticomaxillary complex fractures using a three-dimensional photogrammetric analysis. J Otolaryngol Head Neck Surg. 2019;48(1):36. doi: 10.1186/s40463-019-0359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sato A, Imai Y, Muraki K, Tachi M. Reliability of ultrasound-guided one-point fixation for zygomaticomaxillary complex fractures. J Craniofac Surg. 2019;30(1):218–222. doi: 10.1097/SCS.0000000000005133. [DOI] [PubMed] [Google Scholar]
- 16.Tripathi N, Goyal M, Mishra B, Dhasmana S. Zygomatic complex fracture: a comparative evaluation of stability using titanium and bio-resorbable plates as one point fixation. Natl J Maxillofac Surg. 2013;4(2):181–187. doi: 10.4103/0975-5950.127648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ribeiro Ribeiro AL, Rodrigues TM, Alves-Junior Sde M, Pinheiro JJ. Interfragmentary screw fixation of the zygomatic arch in complex midface and zygomaticomaxillary fractures. J Oral Maxillofac Surg. 2015;73(3):494–498. doi: 10.1016/j.joms.2014.09.028. [DOI] [PubMed] [Google Scholar]