Abstract
Introduction
Paracetamol is an optimal non-opioid analgesic and holds considerable advantages over NSAIDs in managing post-operative pain. Literature to date doesn’t provide substantial documentation of it’s efficacy and safety in major oral and maxillofacial surgeries. The study is designed to compare the effectiveness of intravenous paracetamol with diclofenac sodium for controlling post-operative pain and edema in major oral and maxillofacial surgeries.
Method
The double-blind randomised prospective study includes 140 healthy patients with ASA grades I and II. Patients were divided into Group A (1gm paracetamol) and B (75 mg diclofenac sodium), 70 patients each, undergoing similar surgical procedures. VAS and VRS were assessed for pain and thread method for measuring swelling. Mouth opening in space infections was measured with calliper and scale.
Results
Independent samples t-test and chi-square test showed longer pain-free interval, more interval between first and second dose, lesser number of doses required in Group A than Group B (p-value < 0.05). Independent samples t-test and Mann–Whitney test showed faster resolution of swelling in Group A (p-value < 0.05). Independent samples t-test showed lesser time taken for resolution of trismus in space infections in Group A (p-value < 0.05).
Discussion
Paracetamol 1 g was found to be an effective analgesic with less adverse effects. It is superior non-opioid analgesic in reducing the intensity of post-operative pain and swelling, also requires less number of doses than diclofenac sodium in major surgeries. Patients treated with paracetamol had better quality of life during post-operative period.
Keywords: Acetaminophen, Diclofenac, Analgesic, Postoperative pain, Postoperative edema
Introduction
Lack of efficient management of pain is one of the main challenges an oral and maxillofacial surgeon faces after major surgeries [1]. The main focus of oral and maxillofacial surgeon is to make the patient pain-free as early as possible to help them resume normal masticatory function and daily routine.
All these years, narcotics have been used as strong analgesics in mitigating severe acute or chronic pain. However, high dose of narcotics leads to many side effects like respiratory depression, apnoea, nausea, vomiting, physical and mental dependence etc [1].Thus, other analgesics like Non-Steroidal Anti-inflammatory drugs (NSAIDs) were being increasingly used [1]. The risks associated with NSAIDs like Diclofenac, Ketorolac etc. are severe like sometimes fatal gastrointestinal bleeding, gastritis, damage to the normal protective mucus layer of GIT, reversible renal damage in elderly patients and patients with hypertension, cardiovascular diseases, or pre-existing renal disease [2]. Other NSAIDS like COX-2 inhibitors (Rofecoxib, Celecoxib etc.) have been reported to increase the risk of adverse cardiovascular events, thrombosis and might interfere with bone healing [3–8].
With the advent of intravenous paracetamol, studies in field of orthopaedic surgery, gynaecology, ophthalmology, other medical fields [1] have found results of paracetamol comparable to other analgesics in relieving mild to moderate post-operative pain. However, literature to date doesn’t provide substantial documentation of it’s efficacy and safety in major oral and maxillofacial surgeries.
Paracetamol
The mechanism of action of paracetamol is selectively inhibiting COX activities in the brain. This activity does not appear to be direct inhibition by blocking an active site, but rather by reducing COX, which must be oxidized in order to function. Paracetamol might modulate the endogenous cannabinoid system in the brain through paracetamol's metabolite, AM404 [9]. AM404 inhibits the reuptake of the endogenous cannabinoid/vanilloid and amide receptors by neurons, making it more available to reduce pain [10]. AM404 also directly activates the TRPV1, which also inhibits pain signals in the brain.
Diclofenac
The primary mechanism of action is thought to be inhibition of prostaglandin synthesis by inhibition of cyclooxygenase (COX) [2]. Several other molecular targets of diclofenac, possibly contributing to its pain-relieving actions-
Blockage of voltage-dependent sodium channels
Blockage of acid-sensing ion channels
Positive allosteric modulation of KCNQ- and BK-potassium channels.
The aim of this study is to assess and compare effectiveness of intravenous paracetamol with diclofenac sodium for controlling post-operative pain and swelling in patients undergoing major oral and maxillofacial surgical procedures.
Subjects and Methods
This present comparative randomized study was conducted at Navi Mumbai, Maharashtra in the department of oral and maxillofacial surgery, A total of 140 healthy patients with ASA grades I and II underwent various major oral and maxillofacial surgical procedures during the period of January 2018- December 2020 were recruited to participate. Before commencement of the study, ethical approval was attained from the Institutional Research and ethical board- Approval number DYPUSPD/GS-CG-OS/865-A/2016, Date of approval-15/NOV/2017). Written informed consent was obtained from all subject prior study and procedures adhere to the ethical guidelines of Declaration of Helsinki.
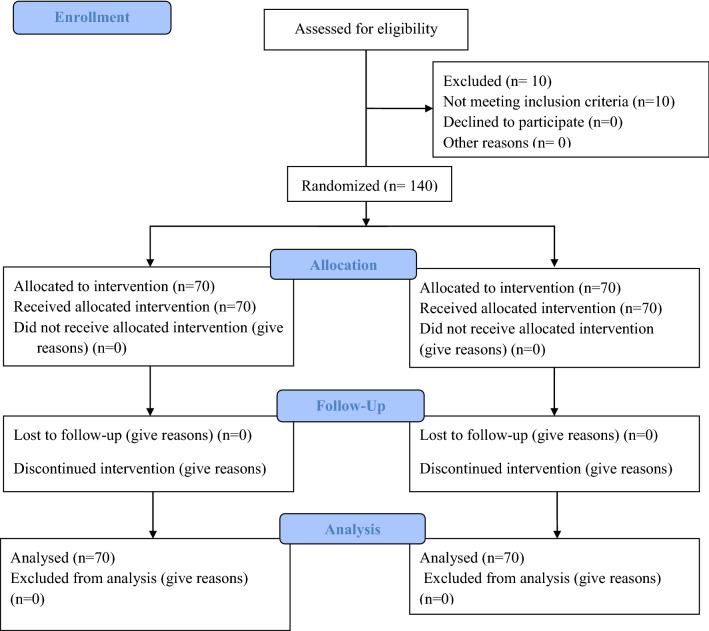
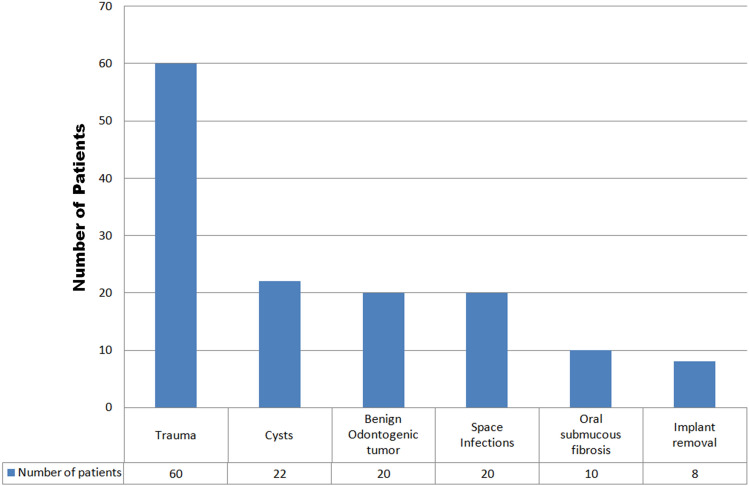
This study is conducted and reported in accordance with Consolidated Standards of Reporting Trials (CONSORT) guidelines (Fig. 1). Sample size was calculated using software Open Epi Open Source Epidemiologic Statistics for Public Health, with a statistical formula having 5% α value, 80% power, and 95% confidence interval. A sample size of 140 participants was determined to maintain the power of the study at 80%. A detailed case history of all patients was recorded prior to the admission (Fig. 1). Randomization of the 140 patients was done in two groups (A and B), which included 70 patients each, who underwent similar major oral and maxillofacial surgical procedures. Group A received paracetamol and Group B received diclofenac sodium for post-operative analgesia. The surgical procedures were categorised into duration of 2 h and 3 to 4 h respectively. The surgeries including trauma (60), cysts (22), benign odontogenic tumors (20), removal of plates (8), oral submucous fibrosis (10) and space infections (20) (Fig. 2) were uniformly divided into two groups on the basis of type and duration of surgery. Surgeries were performed by Professors, who were blinded to the drugs administered.
Fig. 1.
Consort flowchart diagram
Fig. 2.
Types of surgeries and number of patients
Inclusion Criteria
140 patients with ASA status I and II, age group of 18–60 years and weight ranging between 50 and 120 kgs were included in the study. All the patients were able to use the pain scales. Patients were hospitalised and all routine haematological including liver function test, radiographic investigations and pre-anesthetic evaluation were carried out prior to the surgery.
Exclusion Criteria
Patients with history of sensitivity to paracetamol and/or diclofenac sodium, medically compromised patients particularly impaired liver function, peptic ulcers and renal dysfunction, neurological diseases, endocrinal diseases, asthma, alcoholics were excluded from study. Patients with history of other painful conditions, psychological disturbance which might affect patient’s perception of pain were also excluded. Patients with history of bleeding and/or clotting disorders and patients on other medications like anticoagulant therapy, patient who has been administered any NSAID within last 8 h, Paracetamol within last 24 h, any analgesic within last 12 h and corticosteroids within last 7 days before administration of study drug were also excluded from the study. Patients were hospitalised and routine haematological investigations including liver function test, radiographs and pre-anesthetic evaluation were carried out prior to the surgery.
Drugs and Intubation
All patients were kept nil by mouth for 8 h before the procedure. All patients were premedicated with an antibiotic (inj.Augmentin or inj.Taxim), antacid (inj.Pan40), antiemetic (inj.Emeset) before the surgery. In a fully equipped operating room, anaesthesia was induced with Propofol 20 ml, Midazolam 1 mg, Vecuronium 6 mg given for muscle relaxation. Other drugs used intra-operatively are Glycopyrrolate 0.2 mg, Emeset 4 mg, and Rantac 150 mg. After endotracheal intubation, lungs were mechanically ventilated with pressure-controlled ventilation and end-tidal carbon dioxide (ETCO2) tension was maintained at 30-35 mmHg. Intravenous fluid management included administration of lactated Ringer’s solution. Adrenaline was injected locally for vasoconstriction.
No additional opioids were given intraoperatively. After induction of anaesthesia, Group A patients were administered with 1000 mg paracetamol IV preparation in 100 ml intraoperatively and continued with same in postoperative period while Group B patients were administered with 75 mg diclofenac sodium diluted in 100 ml normal saline solution intraoperatively and continued with same in postoperative period and shifted tablet form. All drugs were administered by an anaesthesiologist who was blinded to the details of the study. Both the analgesics were administered just before the incision was taken as a slow infusion over 15 min through a different IV cannula placed in the other arm.
All vitals were monitored continuously during the procedure. At the end of the operation, reversal was achieved with Neostigmine. After extubation when respiration was regular and adequate in rate and depth, patients were transferred to post-anaesthesia care unit. Once awake and oriented, patients were transferred to the surgical ward where they were observed and assessed for the next 5–7 days postoperatively. On the first post-operative day, vitals, haematological examination including liver function tests were repeated to observe any abnormal variations from baseline values.
Assessment of Parameters
The comparison of various parameters was done in both the groups for similar procedures (type and duration). Primary variables were pain, swelling and secondary variables included trismus and adverse effects.
Postoperative assessment of analgesia was done by determining the following parameters:
Pain intensity using Visual Analogue Scale (VAS) and Verbal Response Scale (VRS) –
VAS (0 = no pain►10 = worst imaginable pain).
VRS a four-point VRS was recorded as follows: 0- none, 1- mild, 2- moderate, and 3- severe. Pain intensity was measured post-extubation at intervals of 1, 2, 4 h and every 4 h in the postoperative period. VAS and VRS were evaluated for both drug groups.
Peak of pain relief The primary efficacy variable, PR, was rated on 5-point verbal scale as follows: 0- none, 1 -a little, 2- moderate, 3- a lot, and 4- complete. Pain-free interval was also assessed.
Rescue drug Attentive to proposed form and based on moral considerations, patients with severe pain (VAS > 7), inj. Tramadol 50 mg was recommended as the rescue drug.
Assessment of swelling was done using thread method till it resolved completely.
Assessment of Trismus in 20 cases of space infections was done by measuring mouth opening of patients using calliper and scale.
Safety variables comprised adverse events (AEs), vital signs (Confounders variables) (arterial blood pressure and heart rate) and laboratory variables (haematology and plasma biochemistry). AEs were assessed before surgery, on 1st post-operative day and till the patient was admitted. Vital signs were measured just before medication and at 1 h and 6 h post medication. Blood samples for laboratory variables were drawn between Day 6 and Day 1 and at 48 h post medication.
Statistical Analysis
The data were entered in Microsoft Excel and SPSS 15.0 package was used for the data analyses. Statistical analysis included descriptive statistics of numerical variables, including arithmetic mean, standard deviation, minimum and maximum (range) was done for all the parameters. Independent samples t-test, Chi-square test, Cramer’s V test were done to assess the difference in parameters between the groups. All statistical analysis was done at 95% Confidence interval and p < 0.05 was considered statistically significant.
Results
Analysis for the pain-free interval was assessed through the VAS and VRS assessment scores. For 2 h surgery, VAS showed that 93.0% patients on paracetamol treatment did not experience pain by 2 h in contrast to 18.0% patients on diclofenac sodium. VRS showed 98.0% of the patients taking paracetamol didn’t experience pain at 2 h compared to 28.0% of the patients taking diclofenac sodium. The average pain setting time through VAS scores for paracetamol 4.73 h and 2.83 h for diclofenac sodium (Table 1). On VRS scale, the average pain setting time for paracetamol 5.28 h and 3.03 h for diclofenac sodium (Table 2). The results of equality test for VAS & VRS were statistically significant (p-value < 0.0005) (Table 3).
Table 1.
Mean for pain free time on VAS scale for paracetamol and diclofenac sodium
| Treatment | Mean (a) | ||||
|---|---|---|---|---|---|
| Duration of surgery | Estimate | Std. error | 95% Confidence interval | ||
| Lower bound | Upper bound | ||||
| Paracetamol | 2 h | 4.73 | 0.15 | 4.43 | 5.02 |
| Diclofenac sodium | 2.83 | 0.12 | 2.58 | 3.07 | |
| Overall | 3.78 | 0.14 | 3.49 | 4.06 | |
| Paracetamol | 3 to 4 h | 4.40 | 0.23 | 3.94 | 4.86 |
| Diclofenac sodium | 2.15 | 0.13 | 1.89 | 2.41 | |
| Overall | 3.28 | 0.22 | 2.84 | 3.71 | |
Table 2.
Means for pain free time on VRS scale for paracetamol and diclofenac sodium
| Treatment | Mean (a) | ||||
|---|---|---|---|---|---|
| Duration of surgery | Estimate | Std. error | 95% Confidence interval | ||
| Lower bound | Upper bound | ||||
| Paracetamol | 2 h | 5.28 | 0.13 | 5.01 | 5.54 |
| Diclofenac sodium | 3.03 | 0.17 | 2.70 | 3.35 | |
| Overall | 4.15 | 0.17 | 3.83 | 4.47 | |
| Paracetamol | 3 to 4 h | 5.20 | 0.25 | 4.72 | 5.68 |
| Diclofenac sodium | 1.95 | 0.05 | 1.85 | 2.05 | |
| Overall | 3.58 | 0.29 | 3.01 | 4.14 | |
Table 3.
Test of equality of pain free time distributions for treated with paracetamol and diclofenac sodium
| Name of the test | Duration of surgery | Chi-square | df | p-value |
|---|---|---|---|---|
| ON VAS scale | ||||
| Log rank (Mantel-Cox) | 2 h | 50.85 | 1 | < .05 |
| Breslow (Generalized Wilcoxon) | 50.50 | 1 | < .05 | |
| Tarone-ware | 51.35 | 1 | < .05 | |
| Log rank (Mantel-Cox) | 3–4 h | 30.37 | 1 | < .05 |
| Breslow (generalized wilcoxon) | 29.37 | 1 | < .05 | |
| Tarone-ware | 30.14 | 1 | < .05 | |
| ON VRS scale | ||||
| Log rank (Mantel-Cox) | 2 h | 51.72 | 1 | < .05 |
| Breslow (Generalized Wilcoxon) | 51.35 | 1 | < .05 | |
| Tarone-ware | 52.28 | 1 | < .05 | |
| Log rank (Mantel-Cox) | 3–4 h | 38.18 | 1 | < .05 |
| Breslow (Generalized Wilcoxon) | 38.10 | 1 | < .05 | |
| Tarone-Ware | 38.14 | 1 | < .05 | |
For 3–4 h surgeries, VAS scale showed 80.0% patients treated with paracetamol were pain-free at 2 h compared to 5.0% patients treated with diclofenac sodium. On VRS scale, the pain-free time period for 95.0% of the patients on diclofenac sodium was 30 min whereas for 90.0% of the paracetamol patients it was of 2 h. On VAS, the mean pain-free time for paracetamol was 4.4 h than that for the diclofenac sodium 2.15 h (Table 1). On VRS, the mean pain-free time for paracetamol was 5.2 h and 1.95 h for diclofenac sodium (Table 2). The results of equality test were statistically significant (Table 3). Irrespective of duration of surgery and the type of scale used to identify pain, patients treated with paracetamol experienced longer pain-free period compared to the patients treated with diclofenac sodium.
Descriptive statistics for time interval between first and second dose showed positive skewness for both the groups in surgeries with duration of 2 h. The mean interval between the first two doses was 7 h for paracetamol and 5.18 h for diclofenac sodium in 2 h surgery (Table 4).
Table 4.
Descriptive statistics for Time interval between first and second dose for Two Treatments
| Duration of surgery | Treatment | N | Minimum | Maximum | Mean | Standard deviation | Skewness ratio |
|---|---|---|---|---|---|---|---|
| 2 h | Paracetamol | 11 | 6 | 9 | 7.00 | 1 | 1.11 |
| Diclofenac sodium | 11 | 4 | 7 | 5.18 | 1.17 | 0.75 | |
| 3–4 h | Paracetamol | 6 | 5 | 7 | 6.33 | 0.82 | − 1.01 |
| Diclofenac sodium | 6 | 4 | 5 | 4.33 | 0.52 | 1.15 |
| Results of t-test for equality of Means | |||||||
|---|---|---|---|---|---|---|---|
| Mean difference | Std. error difference | t | df | Sig. (p- value) (2-tailed) | 95% Confidence interval of the difference | ||
| Lower | Upper | ||||||
| 2 h | 1.82 | 0.46 | 3.92* | 20 | 0.001 | 0.85 | 2.79 |
| 3 to 4 h | 2.00 | 0.39 | 5.07* | 10 | < .05 | 1.12 | 2.88 |
*t-value is statistically significant at .05 level
Descriptive statistics for time interval between first and second dose for two treatments showed negative skewness for paracetamol and positive skewness for diclofenac sodium in surgeries that lasted for 3-4 h. The mean time interval between first two doses for paracetamol was 6.33 h significantly higher than that for the diclofenac sodium was 4.33 h (Table 4). Result of t-value associated with the difference in the mean time interval between first two doses for 2 h and 3-4 h surgeries was statistically significant (Table 4).
Apart from assessing the pain-free time interval, number of doses was also calculated. In case of paracetamol, 29 and 14 patients got relief from pain with just a single dose compared to 7 and 3 patients taking diclofenac sodium in 2 h and 3-4 h surgeries (Table 4).
Cramer’s V value was statistically significant and suggests a strong relationship between Treatment and number of dose/s, for the patients with 2 h and 3-4 h surgeries (Table 5).
Table 5.
Cramer’s V test for number of patients and dose/s for 2 h and 3-4 h surgeries
| Treatment | Duration of surgery | Number of patients dose/s given | Total | Cramer’s V | P value | |||
|---|---|---|---|---|---|---|---|---|
| Single | Two | Three | Four | |||||
| Paracetamol | 2 h | 29 | 11 | 0 | 40 | .61 | p < .05 | |
| Diclofenac sodium | 7 | 18 | 15 | 40 | ||||
| Total | 36 | 29 | 15 | 80 | ||||
| Paracetamol | 3–4 h | 14 | 4 | 2 | 1 | 21 | .60 | p = .001 |
| Diclofenac sodium | 3 | 4 | 13 | 2 | 22 | |||
| Total | 17 | 8 | 15 | 3 | 43 | |||
The t-test of equality was statistically significant (Table 6) which was confirmed with Mann- Whitney test (U = 924.00, z-value = − 4.73, p < 0.0005).
Table 6.
Results of independent samples t-test for time for swelling resolution (days) by paracetamol and diclofenac sodium
| Results of t-test for equality of Means | ||||||
|---|---|---|---|---|---|---|
| Mean Difference | Std. Error Difference | t | df | Sig. (2-tailed) | 95% Confidence interval of the difference | |
| Lower | Upper | |||||
| − 1.17 | 0.23 | − 5.16* | 118 | < .05 | − 1.61 | − 0.72 |
*t-value is statistically significant at .05 level
The mean number of days required to achieve adequate mouth opening in cases of space infections was lesser in paracetamol group (4.4) than those treated with diclofenac sodium (5.9) showing positive skewness (Table 7). The t-value associated with the difference of 1.5 days is statistically significant (Table 7).
Table 7.
Descriptive statistics for average no of days taken to achieve adequate mouth opening for two treatments and results of t-test
| Diagnosis | Treatment | N | Minimum | Maximum | Mean | Standard deviation | Skewness ratio |
|---|---|---|---|---|---|---|---|
| Space infection | Paracetamol | 10 | 3 | 6 | 4.4 | 0.84 | 0.57 |
| Diclofenac sodium | 10 | 4 | 8 | 5.9 | 1.20 | 0.34 |
| Results of t-test for equality of means | |||||||
|---|---|---|---|---|---|---|---|
| Mean difference | Std. error difference | t | df | Sig. (2-tailed) | 95% confidence interval of the difference | ||
| Lower | Upper | ||||||
| − 1.5 | 0.46 | − 3.24* | 18 | 0.005 | − 2.47 | − 0.53 | |
*t-value is statistically significant at .05 level
Discussion
Our present study focussed on comparing the efficacy of paracetamol with diclofenac sodium in reducing post-operative pain and swelling after major surgeries.
Assessment of Pain
Irrespective of duration, type of surgery and type of pain assessment scale used, the patients treated with paracetamol experienced longer pain-free time compared to diclofenac sodium.
Based on observations of VAS and VRS scores, the patients on paracetamol were completely pain-free for almost 5 h compared to 3 h in case of diclofenac sodium. The average pain setting time however was earlier for 3–4 h surgeries in both the groups.
The mean time interval between first two doses of paracetamol was 7 h for 2 h surgeries compared to 5 h for diclofenac sodium and 6 h for 3–4 h surgeries compared to 4 h. This difference could be due to higher grade of surgery.
Various studies have been undertaken in other medical fields to assess the effectiveness of paracetamol in the last few years but have shown variable results. Studies have observed pain relief scores ranging between 15 min and 6 h, and median time to peak pain relief was 30 min [11]. Furthermore, a study showed that a combination of 1 g paracetamol and 40 mg parecoxib showed positive changes in the VAS at rest and at movement at 8 h interval [12]. On the contrary, the overall mean index measurement of pain in the period from 30 min to 4 h after surgery showed insignificant difference between acetaminophen and diclofenac [1].
Assessment of Number of Doses
The number of doses of paracetamol required by the patient was lesser than diclofenac sodium irrespective of duration of surgery. Single dose of paracetamol in contrast to 3 doses of diclofenac sodium was required for most surgeries of 2 h & 3-4 h duration. Also, maximum two doses of paracetamol were required in 2 h surgeries and very few surgeries of 3–4 h duration required 3 doses.
A review article reported that the use of paracetamol at standard doses reduced at least 50% of pain over 4–6 h following a single dose of paracetamol [13].
Rescue Drug
Tramadol was used as a rescue drug in 3 cases in diclofenac sodium group in surgeries of 3 to 4 h duration which was statistically insignificant.
A study in orthopaedic surgeries reported that the single dose of intravenous acetaminophen and propacetamol reduced the need for rescue doses over the entire 24 h study interval.The period between median time to first rescue medication was found to be 4 h for intravenous acetaminophen and 1.6 h for placebo group [11].
The number of morphine doses were reduced post-operatively when a combination of paracetamol and parecoxib was used [13]. Propacetamol or i.v paracetamol was found to reduce the amount of morphine consumption in 16–46% patients undergoing major orthopaedic [1, 2, 14, 15], spinal [16] and tonsillectomy surgeries [17].
Studies have reported meperidine as an effective post-operative analgesic after orthopaedic and caesarean surgery [18, 19]. Another study reported a larger dose (35 mg/kg) of acetaminophen as effective as ketorolac in reducing pain after tonsillectomy [20].
Rectal acetaminophen has also been found to serve as an adjuvant to NSAIDS and local anaesthetics as a multimodal fast tracking surgery recovery protocol [21]. A study reported that in myringotomy surgery in children, acetaminophen and diclofenac had similar efficacy in reducing the post—surgical pain [22]. A combination of acetaminophen with NSAIDS showed good pain relief treatment plan because of less side effects of acetaminophen when compared to NSAIDS [23].
Very few studies have been conducted on efficacy of paracetamol in major oral and maxillofacial procedures. A study was conducted to compare the post operative pain relief by paracetamol 1gm i.v with diclofenac sodium 75 mg i.m in bimaxillary osteotomies. Higher VAS scores were observed in case of paracetamol till 6 h, however they concluded that both drugs were comparable as a single dose to effectively decrease post operative pain in 12hrs [24].
Few studies are documented in minor oral surgeries where paracetamol is compared with other NSAIDS administered through oral route.
A study compared paracetamol (250 mg/5 ml) with Ibuprofen (100 mg/5 ml) in post operative pain relief after primary tooth extractions. Ibuprofen exhibited lower pain scores [25].
Paracetamol (1gm), ibuprofen (400 mg) and diclofenac potassium (50 mg) were compared in extractions and cavity preparations. Diclofenac was most effective and rescue analgesia was needed in maximum cases of paracetamol [26]. A study comparing paracetamol (500 mg) and ketorolac (10 mg) concluded requirement of rescue drug after 5 h in paracetamol group compared to 4 h in ketorolac group [27].
Another study compared paracetamol (1000 mg) with celecoxib (400 mg) and diclofenac sodium (50 mg) in patients undergoing impacted third molar surgeries and removal of plates and screws. The duration of post operative analgesia was 3 to 4 h for all the drugs [28].
Paracetamol (500 mg) was compared with diclofenac (100 mg) as preemptive analgesic agent given 30 min before extractions.Rescue analgesic was required after 3 h of administration of paracetamol and after 6 h in case of diclofenac [29].
A study comparing preoperative and postoperative administration of paracetamol (500 mg), ibuprofen (400 mg) and mefenamic acid (500 mg) for post extraction pain control concluded no significant difference in the efficacy of analgesia of the drugs but ibuprofen and mefenamic acid showed better antiinflammatory properties [30].
Assessment of Post Operative Swelling
The duration required for swelling resolution was lesser for paracetamol than diclofenac sodium.
Assessment of Trismus in Space Infections
The number of days required for adequate mouth opening was lesser for patients in paracetamol group compared to diclofenac sodium. No major adverse effects reported in context to any of the two drugs. However, 5 patients in diclofenac sodium group had episode of gastritis which was statistically insignificant.
To the best of our knowledge, this study has larger sample size and elaborately discusses various parameters in comparing the two drugs in different major oral and maxillofacial surgeries.
Intravenous Paracetamol (1 g) is a superior analgesic to diclofenac in relieving post operative pain and swelling in major oral and maxillofacial surgeries.
The study had the limitation of small sample size of space infections to conclude on resolution of trismus.
Further research in the field of surgical oncology and reconstruction would be helpful in adding significance to the current study.
Conclusion
Paracetamol turned out to be a superior non opioid analgesic in reducing the intensity of post-operative pain and swelling, also requiring lesser number of doses than diclofenac sodium in major surgeries. Patients treated with paracetamol had better quality of life in post- operative period and sooner recovery to daily routine.
Abbreviations
- VAS
Visual analogue scale
- VRS
Verbal response scale
Declarations
Conflict of interest
We have no conflicts of interest.
Ethical Approval
Ethics approval or patients’ consent was required for this paper, though the patients gave written consent for the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Charu Girotra, Email: charugirotra@yahoo.com.
Mukul Padhye, Email: mukul.padhye@gmail.com.
Pratibha Mahajan, Email: drpratibha@gmail.com.
Siddhi Savla, Email: tuk97226@temple.edu.
Aishwarya Nair, Email: draishwarya.gnair@gmail.com.
Pranay Pardeshi, Email: pranay391989@gmail.com.
Gaurav Tomar, Email: dr.gauravtom@gmail.com.
Yogesh Kini, Email: yogesh.kini@dypatil.edu.
References
- 1.Khoshraftar E, Anvari HM, Assadi HK, Abdulamir AS, Abu Bakar F. Comparative study on the effectiveness of acetaminophen and diclofenac pretreatment in the relief of acute pain after out-patient surgery. Eur J Dent Med. 2011;3:23–27. doi: 10.3923/ejdm.2011.23.27. [DOI] [Google Scholar]
- 2.White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg. 2005;101(5 Suppl):S5–S22. doi: 10.1213/01.ANE.0000177099.28914.A7. [DOI] [PubMed] [Google Scholar]
- 3.Li X, Zhou M, Xia Q, Li J. Parecoxib sodium reduces the need for opioids after tonsillectomy in children: a double-blind placebo-controlled randomized clinical trial. Can J Anaesth. 2016;63(3):268–274. doi: 10.1007/s12630-015-0560-3. [DOI] [PubMed] [Google Scholar]
- 4.Marquez-Lara A, Hutchinson ID, Nuñez F, Jr, Smith TL, Miller AN. Nonsteroidal anti-inflammatory drugs and bone-healing: a systematic review of research quality. JBJS reviews. 2016;4(3):e4. doi: 10.2106/JBJS.RVW.O.00055. [DOI] [PubMed] [Google Scholar]
- 5.Seidenberg AB, An YH. Is there any inhibitory effect of COX-2 inhibitors on bone healing? Pharm Res. 2004;50:151–156. doi: 10.1016/j.phrs.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 6.Harder AT, An YH. The mechanism of the inhibitory effects of non-steroidal anti-inflammatory drugs on bone healing: a concise review. J Clin Pharm. 2004;43:807–815. doi: 10.1177/0091270003256061. [DOI] [PubMed] [Google Scholar]
- 7.Khan JS, Margarido C, Devereaux PJ, Clarke H, McLellan A, Choi S. Preoperative celecoxib in noncardiac surgery: a systematic review and meta-analysis of randomised controlled trials. Eur J Anaesthesiol (EJA) 2016;33(3):204–214. doi: 10.1097/EJA.0000000000000346. [DOI] [PubMed] [Google Scholar]
- 8.Issioui T, Klein KW, White PF, et al. cost-efficacy of rofecoxib versus acetaminophen for preventing pain after ambulatory surgery. Anesthesiology. 2002;97:931–937. doi: 10.1097/00000542-200210000-00027. [DOI] [PubMed] [Google Scholar]
- 9.Soraya WS, Ariel RM, Ellen F, et al. AM404, paracetamol metabolite prevents prostaglandin synthesis in activated microglia by inhibiting COX activity. J Neuroinflammation. 2018;15:34. doi: 10.1186/s12974-018-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ross RA. Anandamide and vanilloid TRPV1 receptors. Brit J Pharmacol. 2003;140:790–801. doi: 10.1038/sj.bjp.0705467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McNicol ED, Ferguson MC, Haroutounian S, Carr DB, Schumann R (2016) Single dose intravenous paracetamol or intravenous propacetamol for postoperative pain. Cochrane Datab Syst Rev (5) [DOI] [PMC free article] [PubMed]
- 12.Zeinab AE, Salwa OK, Ahmed MK, Eman MA, Layal FA. Combined parecoxib and IV paracetamol provides additional analgesic effect with better postoperative satisfaction in patients undergoing anterior cruciate ligament reconstruction. Saudi J Anaesth. 2011;5:45–49. doi: 10.4103/1658-354X.76510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toms L, McQuay HJ, Derry S, Moore RA. Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. Cochrane Datab Syst Rev. 2008;2008(4):CD004602. doi: 10.1002/14651858.CD004602.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McNicol ED, Tzortzpoulou A, Cepeda MS, Francia MB, Farhat T, Schumann R. single dose intravenous paracetamol or propacetamol for prevention of treatment of post-operative pain: a systematic review and meta-analysis. Br J Anaesth. 2011;106(6):764–775. doi: 10.1093/bja/aer107. [DOI] [PubMed] [Google Scholar]
- 15.Delbos A, Boccard E. The morphine sparing effect of propacetamol in orthopaedic post-operative pain. J Pain Symptom Manage. 1995;10:279–286. doi: 10.1016/0885-3924(95)00004-I. [DOI] [PubMed] [Google Scholar]
- 16.Hernandez-Palazon J, Tortosa JA, Martinez-Lage JF, Perez FD. Intravenous administration of propacetamol reduces morphine consumption after spinal fusion surgery. AnaesthAnalg. 2001;92:1473–1476. doi: 10.1097/00000539-200106000-00024. [DOI] [PubMed] [Google Scholar]
- 17.Hiller A, Silvanto M, Savolainen S, Tarkkila P. Propacetamol and diclofenac alone and in combination for analgesia after elective tonsillectomy. Acta Anaesthesiol Scand. 2004;48:1185–1189. doi: 10.1111/j.1399-6576.2004.00473.x. [DOI] [PubMed] [Google Scholar]
- 18.Fidkowski CW, Shah S, Kataria S, Alsaden MR. A randomized controlled trial of intravenous and intramuscular ketorolac for post-cesarean analgesia. J Anesth Clin Res. 2018;9(861):2. [Google Scholar]
- 19.Shrestha L, Joshi B, Palikhey A, Bhattarai K. Comparative study on efficacy of ketorolac and pethidine for postoperative pain management. J Univ Coll Med Sci. 2019;7(1):27–32. doi: 10.3126/jucms.v7i1.24682. [DOI] [Google Scholar]
- 20.Rusy LM, Houck CS, Sullivan LJ, et al. a double blinded evaluation of ketorolac tromethamine versus acetaminophen in pediatric tonsillectomy : analgesia and bleeding. Anesth Analg. 1995;80:226–229. doi: 10.1097/00000539-199502000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Gelineau AM, King MR, Ladha KS, Burns SM, Houle T, Anderson TA. Intraoperative esmolol as an adjunct for perioperative opioid and postoperative pain reduction: a systematic review, meta-analysis, and meta-regression. Anesth Analg. 2018;126(3):1035–1049. doi: 10.1213/ANE.0000000000002469. [DOI] [PubMed] [Google Scholar]
- 22.Rømsing J, Ostergaard D, Drozdziewicz D, Schultz P, Ravn G. Diclofenac or acetaminophen for analgesia in paediatric tonsillectomy outpatients. Acta Anaesthesiol Scand. 2000;44(3):291–295. doi: 10.1034/j.1399-6576.2000.440312.x. [DOI] [PubMed] [Google Scholar]
- 23.Camu F, Borgeat A, Heylen RJ, Viel EJ, Boye ME, Cheung RY. Parecoxib, propacetamol, and their combination for analgesia after total hip arthroplasty: a randomized non-inferiority trial. Acta Anaesthesiol Scand. 2017;61(1):99–110. doi: 10.1111/aas.12841. [DOI] [PubMed] [Google Scholar]
- 24.Mobini A, Mehra P, Chigurupati R. Postoperative pain and opioid analgesic requirements after orthognathic surgery. J Oral Maxillofac Surg. 2018;76(11):2285–2295. doi: 10.1016/j.joms.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 25.Kharouba J, Hawash N, Peretz B, Blumer S, Srour Y, Nassar M, Somri M. Effect of intravenous paracetamol as pre-emptive compared to preventive analgesia in a pediatric dental setting: a prospective randomized study. Int J Pediatr Dent. 2018;28(1):83–91. doi: 10.1111/ipd.12311. [DOI] [PubMed] [Google Scholar]
- 26.Gazal G, Al-Samadani KH. Comparison of paracetamol, ibuprofen, and diclofenac potassium for pain relief following dental extractions and deep cavity preparations. Saudi Med J. 2017;38(3):284–291. doi: 10.15537/smj.2017.3.16023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rao TD, Santhoshkumar MP. Analgesic efficacy of paracetamolvs ketorolac after dental extractions. Res J Pharm Tech. 2018;11(8):3375–3379. doi: 10.5958/0974-360X.2018.00621.2. [DOI] [Google Scholar]
- 28.Hanzawa A, et al. A comparative study of oral analgesics for postoperative pain after minor oral surgery. Anesth Prog. 2018;65(1):24–29. doi: 10.2344/anpr-65-01-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thenarasu V, Gurunathan D, Kumar MP. Comparison of efficacy of diclofenac and paracetamol as preemptive analgesic agent. Biomed Pharmacol J. 2018;11:1699–1706. doi: 10.13005/bpj/1539. [DOI] [Google Scholar]
- 30.Kumar G, Shu-Lyn C, Win G, Sie L, Lakman NF, Haque N. Comparison between preoperative and post-operative administration of paracetamol, ibuprofen and mefenamic acid for post-extraction pain control. Biomed Res Therapy. 2020;7(5):3794–3798. doi: 10.15419/bmrat.v7i5.606. [DOI] [Google Scholar]