Abstract
Background
Temporomandibular joint disc displacement disorders are a group of temporomandibular disorders beside from other inflammatory disorders and growth related disorders of joint. The purpose of this analysis was to evaluate the efficacy of arthrocentesis procedure in comparison with stabilization splints used for disc displacement disorders without reduction.
Materials and Methods
A systematic search was done in electronic databases (PubMed, Cochrane Central, Web of Science). In addition to this hand search of references and grey literatures was done. Qualities of randomized controlled clinical trials were assessed by Cochrane’s tool for Systematic Reviews of Interventions and the Newcastle–Ottawa Scale was followed to assess the prospective and retrospective studies. Outcome variables pain (VAS) and maximum mouth opening were assessed by the software review manager 5.03.
Results
A total of five studies were included in the review. Three studies showed greater improvement of symptoms in patients of arthrocentesis group in terms of maximum mouth opening, pain (VAS) value. Two other studies found no significant advantage of arthrocentesis over the other treatment protocol. The meta-analysis resulted in statistically significant difference between outcome variables favouring arthrocentesis group (VAS 1–10) (Mean Difference: 3.10; 95% CI 1.74, 4.45; P ≤ .00001, Mean difference: 2.00; 95% CI 0.29, 3.71; P = 0.02).
Conclusion
Arthrocentesis showed effective result in terms of increase in mouth opening and reduction of pain level compared to stabilization splint and other non-invasive approaches in patients with disc displacement disorders without reduction. Overall, results supported the rationale of using arthrocentesis in patients with disc displacement disorders without reduction.
Keywords: Arthrocentesis, Stabilization splint, Maximum mouth opening, Disc displacement, Meta-analysis
Introduction
Temporomandibular joint is a main component of human stomatognathic system. It is formed by mandibular condyle, glenoid fossa of temporal bone and intervening articular disc. Temporomandibular joint and its structures play a huge role in chewing, mastication, swallowing and other daily activities inside the oral cavity [1]. Functional disorders of temporomandibular joint can be classified as—derangement of the condyle–disc complex, structural incompatibility of the articular surfaces, inflammatory joint disorders [2]. Bell et al. presented a classification of temporomandibular disorders which was later modified by American Dental Association. In this classification system they categorized temporomandibular disorders into four categories- masticatory muscle disorders, temporomandibular joint disorders, chronic mandibular hypomobility, growth disorders [3]. Dawson et al. [4] similarly classified temporomandibular disorders into occluso-muscle disorders, reversible intracapsular disorders, irreversible intracapsular disorders, Non-adapted intracapsular disorders. Diagnostic criteria for temporomandibular disorders (DC/TMD) is another classification system that is more standardized and acceptable internationally which classified TMDs based on the findings obtained through history, examination and imaging modalities. Solberg et al. [5] concluded that temporomandibular disorders affect almost 25% of the population, but only a small number of affected population seek treatment. Carlsson et al. [6] stated that only 3–7% of the adult population actually need care for pain and dysfunction associated with temporomandibular joint. Various treatment procedures are recommended for treatment of temporomandibular disc displacement disorders without reduction depending on the clinical presentations ranging from arthroscopic surgery, arthrocentesis to non-invasive treatment procedures like occlusal splint therapy, anti-inflammatory drugs, mouth stretching exercise etc. Arthrocentesis of the temporomandibular joint is a procedure in which lavage of the joint combined with injection of medications like steroids or hyaluronic acid (HA) are done [7]. However, there is a debate regarding application of initial treatment approaches in this disorders. Stabilization splint is a conservative approach with long treatment duration which can cause sometimes worsening of arthropathy and making it more persistent. Various studies have shown Arthrocentesis produces relatively faster relief of pain in this disorder by eliminating inflammatory cells from the joint space which increases the mandibular mobility by removing intra-articular adhesions and the negative pressure within the joint [7–12]. Non-invasive treatment protocols for temporomandibular joint disorders can be divided into definitive and supportive therapy. Occlusal splints and occlusal equilibration procedures come under definitive group. Supportive therapy includes passive/active muscle stretching exercises, anti-inflammatory and anti-anxiolytic medications, physical therapy, etc. The purpose of this analysis was to formulate scientific evidence by comparing two treatment procedures—Arthrocentesis, Occlusal splint and non-invasive therapies in patients with disc displacement disorders without reduction.
Materials and Methods
Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines were used and the checklist was followed in this systematic review and meta-analysis [13].
Eligibility Criteria
Inclusion criteria were as follows:
Published articles on temporomandibular joint disorders (Disc displacement without reduction)
Arthrocentesis and occlusal splint/other non-invasive therapies should be used as an interventional procedure
Maximum mouth opening and Pain assessment should be included as an outcome variable in the study
Published articles in English languages
Randomized controlled clinical trials, Prospective studies, Retrospective studies
In vivo studies
Exclusion criteria were:
Animal studies, In vitro studies, Literature reviews
Case reports and case series
Non-English languages
Studies with incomplete data
Population, intervention, control, outcome, time (PICOT) strategy.
P: Patients with temporomandibular joint disc displacement disorders without reduction.
I: Arthrocentesis used as a therapeutic approach in patients suffering from temporomandibular joint disc displacement disorders without reduction.
C: Patients suffering from temporomandibular joint disc displacement disorders without reduction who underwent occlusal splint (stabilization splint) therapy and other non-invasive therapies.
O: Pain assessment (Visual Analog Scale) and Maximum mouth opening.
T: Follow-up duration of minimum 6 months after the intervention.
Focussed Question
“Do Arthrocentesis show greater improvement in terms of pain and maximum mouth opening in patients suffering from temporomandibular joint disc displacement disorders without reduction compared to occlusal splints?”
Search Methods and Selection Criteria
In vivo randomized controlled clinical trials, prospective studies and retrospective studies were included in this study to check and compare pain level (VAS) and maximum mouth opening in patients who underwent either arthrocentesis or splint and other non-invasive therapies for relieving temporomandibular joint disorders without reduction with a minimum 6 months follow-up period after intervention. Disc displacement without reduction were diagnosed in accordance with diagnostic criteria for temporomandibular disorders (DC/TMD). An elaborative search was done from January 2000 to March 2020 with no publication year limits by two independent reviewers (BB and RB). Following electronic databases were searched for published studies—PubMed, Cochrane central, Web of Science.
In addition to this manual search of the references mentioned in the included studies and manual search of grey literature was done.
Medical subject heading terms (MeSH) terms used during literature search were (1) temporomandibular joint disorders (2) temporomandibular disorders (3) disc displacement (4) arthrocentesis (5) occlusal splints.
Boolean operators OR and AND were used in combination with this MeSH terms to search published studies.
Following combinations of keywords were used in electronic databases during literature search-
temporomandibular joint disorders AND disc displacement AND arthrocentesis AND occlusal splints
temporomandibular joint disorders AND arthrocentesis AND occlusal splints
temporomandibular disorders AND arthrocentesis AND occlusal splints
disc displacement AND arthrocentesis AND occlusal splints
temporomandibular joint disorders OR disc displacement AND arthrocentesis AND occlusal splints
Data Collection
The data were extracted by two independent reviewers (BB and RB) from all the included studies and filled into predetermined forms. From each study, following data were obtained—study design, publication year, country, sample size, sample gender, sample age, intervention, follow-up period.
Data Analysis
Outcome variables pain (VAS) and maximum mouth opening were assessed by the software review manager 5.03 (RevMan, Nordic Cochrane Center, Copenhagen, Denmark). Bivariant differential mean statistic was applied for intergroup estimate (Arthrocentesis versus occlusal splints and other non-invasive approaches) with 95% confidence interval to measure outcome mean. Random effect model with mantel–haenszel statistics were used. I2 test statistics were applied to check heterogenicity, with a p value < 0.05 was considered significant statistically. Forest plots were formulated for the outcome variables with 95% confidence interval and overall treatment effects and subgroup effects at a significance level of 0.05.
Risk of Bias Assessment
Two reviewers (BB and RB) independently assessed the risk of bias of included randomized controlled clinical trials (RCT), prospective studies, retrospective studies. Any disagreements between the reviewers were solved by discussion. The following domains were assessed in each Randomized controlled clinical trials (RCT)-sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and other risk of bias. For each of the sections ‘no’ was used to indicate high risk of bias, ‘yes’ was used to indicate low risk of bias and ‘unclear’ was used to indicate either lack of information or uncertainty. Overall, the studies were considered ‘high’ quality if all conditions met, ‘low’ quality if ≥ 1 condition did not meet, or ‘unclear’ quality if ≥ 1 condition was partly met. The Newcastle–Ottawa Scale was followed to assess the prospective and retrospective studies [14]. The methodological quality was based on selection, comparability and outcome. The studies were classified according to the following criteria–
Good quality 3 or 4 stars in selection domain AND 1 or 2 stars in comparability domain AND 2 or 3 stars in outcome/exposure domain
Fair quality 2 stars in selection domain AND 1 or 2 stars in comparability domain AND 2 or 3 stars in outcome/exposure domain
Poor quality 0 or 1 star in selection domain OR 0 stars in comparability domain OR 0 or 1 stars in outcome/exposure domain
Results
Study Selection
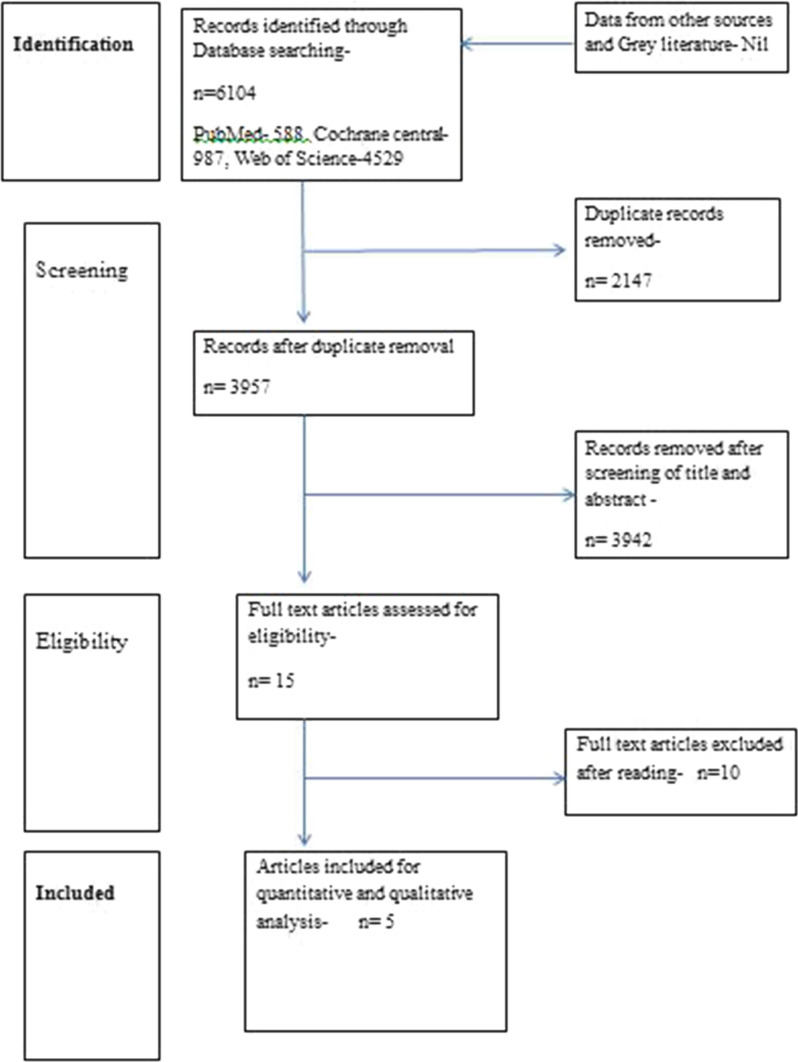
The literature search yielded total 6104 studies through search in electronic databases (PubMed-588, Cochrane central-987, Web of science-4529). Among all the studies, 2147 duplicate records were removed. 3942 studies were removed after screening title and abstracts. Total 15 studies were included for full text reading. Among fifteen studies, three randomized controlled clinical trials, one prospective and one retrospective study were included for qualitative and quantitative analysis [15–19]. Ten studies were excluded due to various reasons [12, 20–28] (Table 1). Study selection procedure was done by two independent reviewers (BB and RB) and disagreements were resolved by discussion. Study selection procedure has been shown in (Fig. 1).
Table 1.
List of excluded studies
| Study | Reason of exclusion |
|---|---|
| Bilici et al. [24] | Evaluated arthrocentesis and occlusal splint in myofascial pain disorder |
| Ghanem et al. [21] | One group treated with occlusal splint after arthrocentesis and other group treated with only arthrocentesis therapy |
| Lee et al. [20] | Evaluated result of arthrocentesis and occlusal splint therapy based on MRI findings |
| Lee et al. [23] | Both the arthrocentesis and occlusal splint therapies given in same group |
| Machon et al. [28] | Pain (VAS scale) and Maximum mouth opening not taken as outcome variable |
| Murakami et al. [27] | Used pivot splint as a splint therapy |
| Sembronio et al. [12] | Both the therapies given in same group, did not compared results in between both the groups |
| Tvrdy et al. [25] | Both the therapies given in same group, did not compared results in between both the groups |
| Vos et al. [26] | Outcome data expressed in a different way and cannot be included according to predetermined outcome variables in inclusion criteria |
| Yucel et al. [22] | One group received splint after arthrocentesis and other group undergone only splint therapy |
Fig. 1.
Study selection process
Quality of the Included Studies
Qualities of randomized controlled clinical trials were assessed by Cochrane’s tool for Systematic Reviews of Interventions [29]. Two of the three included trials mentioned about allocation concealment and adequate sequence generation procedure as a part of randomization. Blinding procedure was unclearly mentioned in all the studies. All the studies measured pre-specified outcome criteria and mentioned about attrition and exclusion of patient with proper reason. Overall, two of the included studies had low risk of bias and one had high risk of bias. Quality of the included prospective and retrospective studies was determined by Newcastle–Ottawa scale. Both the studies were of good quality as determined by scoring criteria for Newcastle–Ottawa scale. Quality assessments of the studies have been shown in Tables 2 and 3.
Table 2.
Quality assessment of randomized controlled clinical trials
| Study | Adequate sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective outcome reporting | Other risk of bias | Overall risk bias |
|---|---|---|---|---|---|---|---|
| Hosgor et al. [16] | No | No | Unclear | Yes | Yes | Yes | High |
| Malekzadeh et al. [19] | Yes | Yes | Unclear | Yes | Yes | Yes | Low |
| Tatli et al. [15] | Yes | Yes | Unclear | Yes | Yes | Yes | Low |
Table 3.
Quality assessment of included prospective and retrospective cohort studies
| Study | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis controlled for confounders | Assessment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow-up of cohorts |
|---|---|---|---|---|---|---|---|---|
| Diracoglu et al. [18] | 1 star | 1 star | 1 star | – | 1 star | 1 star | 1 star | 1 star |
| Ohnuki et al. [17] | 1 star | 1 star | 1 star | – | 1 star | 1 star | 1 star | 1 star |
Characteristics of the Included Studies
Total five studies from three different countries were included in this systematic review and meta-analysis. Various studies used different solutions during arthrocentesis—ringer lactate, sodium chloride, sodium chloride and hyaluronate solution. All the included studies used stabilization splint as an occlusal splint therapy. Characteristics of the included studies have been presented in Table 4.
Table 4.
Characteristics of the included studies
| Study | Year | Study design | Country | Sample description | Intervention | Follow-up |
|---|---|---|---|---|---|---|
| 1. Diracoglu et al. | 2009 | Prospective | Turkey | Arthrocentesis-54 individuals, 33.4 (15–63) years Male-3 Female-51 | Arthrocentesis Group-Lavage of superior joint space with 60 ml Ringer lactate solution | Baseline, 1st month, 3rd month, 6th month |
| Conventional-56 individuals, 34.8 (17–61)years, Male-7 Female-49 | Conventional group-Stabilization splint, 20 min hot pack daily and home exercise programme | |||||
| 2. Hosgor et al. | 2017 | Randomized clinical trial | Turkey | N = 40, Age—Not mentioned, Gender—Not mentioned | Divided into four groups | Baseline, 1st month, 3rd month, 6th month |
| Group 1—Occlusal splint therapy | ||||||
| Group 2—Arthrocentesis with 100 ml lactated Ringer’s solution | ||||||
| Group 3—NSAID (tenoxicam) 20 mg tablets | ||||||
| Group 4—Low-level laser therapy (Nd:YAG, 1064 nm) | ||||||
| 3. Malekzadeh et al. | 2019 | Randomized clinical trial | Sweden | Group 1–12 individuals, 32.5 ± 17.5 years, Female-10, Male-2 | Group 1—Non-invasive group, this group undergone self-exercise and palliative treatment, Occlusal splints given when bruxism activity diagnosed | Baseline, 3rd month, 6th month, 12th month |
| Group 2–12 individuals, 26.7 ± 7.9 years, Female-9, Male-3 | Group 2—Minimally invasive group, this group undergone arthrocentesis with 40-60 ml of sodium chloride solution | |||||
| 4. Ohnuki et al. | 2005 | Retrospective study | Japan | N = 85, 41.8 ± 17.7 years, Female-76, Male-9 | All the patients diagnosed with temporomandibular joint disorders, who were previously treated divided into four groups | Baseline, 1 year after treatment |
| Group 1—Splint therapy | ||||||
| Group 2—Pumping manipulation | ||||||
| Group 3—Arthrocentesis | ||||||
| Group 4—Arthroscopic surgery | ||||||
| 5. Tatli et al. | 2017 | Randomized clinical trial | Turkey | Group 1–40 individuals, 35.2 ± 9.4 years, Female-35, Male-5 | Group 1—Arthrocentesis with isotonic sodium chloride solution followed by sodium hyaluronate injection | Baseline, 1st month, 3rd month, 6th month |
| Group 2—40 individuals, 38.9 ± 11.3 years, Female-39, Male-1 | Group 2—Stabilization splint followed by Arthrocentesis and sodium hyaluronate injection | |||||
| Group 3—40 individuals, 34.8 ± 8.7 years, Female-33, Male-7 | Group 3—Stabilization splint only |
Results of Analysis
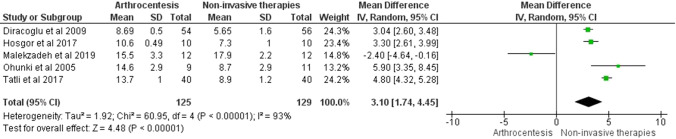
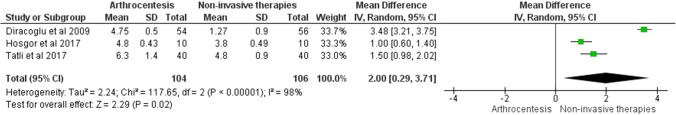
The main outcomes of this study [Maximum mouth opening, Pain (Visual analog scale)] have been presented in Table 5. There was statistically significant evidence regarding increase in maximum mouth opening in arthrocentesis group compared to stabilization splint group (Fig. 2—Mean Difference: 3.10; 95% CI 1.74, 4.45; P ≤ 0.00001). I2 value was 93%, which signified high heterogeneity in between the studies. Significant decrease in pain level was also found (Visual analog scale-1–10) after treating disorders with arthrocentesis compared to stabilization splint and non-invasive therapies (Fig. 3—Mean difference: 2.00; 95% CI 0.29, 3.71; P = 0.02). However according to analysis two studies which measured pain level by (Visual analog scale—1–100) showed difference in between both the groups but not statistically significant (Fig. 4—Mean difference: 7.49; 95% CI −0.95, 15.94; P = 0.08).
Table 5.
Outcome variables of the included studies
| Study | Sample groups | VAS scale (1–10) Mean ± SD | Maximum mouth opening (mm) Mean ± SD | ||
|---|---|---|---|---|---|
| Baseline | Outcome | Baseline | Outcome | ||
| 1. Diracoglu et al. [18] | Arthrocentesis- | 6.26 ± 2.3 | 1.51 ± 1.82 | 29.2 ± 7 | 37.89 ± 6.5 |
| Non-invasive therapies- | 5.66 ± 2.4 | 4.39 ± 2.31 | 29.89 ± 4.8 | 35.54 ± 6.41 | |
| 2. Hosgor et al. [16] | Arthrocentesis- | 7.40 ± 0.30 | 2.60 ± 0.73 | 28.40 ± 2.11 | 39.00 ± 2.60 |
| Non-invasive therapies- | 7.00 ± 0.63 | 3.20 ± 1.12 | 35.70 ± 2.75 | 43.00 ± 1.75 | |
| 3. Tatli et al. [15] | Arthrocentesis- | 6.6 ± 2.2 | 0.3 ± 0.8 | 28.5 ± 3.5 | 42.2 ± 4.5 |
| Non-invasive therapies- | 6.8 ± 1.5 | 2.0 ± 2.4 | 29.2 ± 2.9 | 38.1 ± 4.1 | |
| VAS scale (1–100) | Maximum mouth opening (mm) | ||||
| 4. Malekzadeh et al. [19] | Arthrocentesis- | 57.7 ± 17.8 | 10 ± 6.3 | 27.2 ± 2.8 | 42.7 ± 6.1 |
| Non-invasive therapies- | 49.5 ± 30 | 11 ± 17.1 | 28.4 ± 5.0 | 46.3 ± 7.2 | |
| 5. Ohnuki et al. [17] | Arthrocentesis- | 55 ± 23 | 2.2 ± 3.7 | 30.0 ± 5.9 | 44.6 ± 3.0 |
| Non-invasive therapies- | 53 ± 22 | 2.7 ± 3.4 | 35.1 ± 6.6 | 43.8 ± 3.7 | |
Fig. 2.
Forest plot showing difference in maximum mouth opening
Fig. 3.
Forest plot showing difference in pain level (VAS 1–10)
Fig. 4.
Forest plot showing difference in pain level (VAS 1–100)
Discussion
The aim of this review and meta-analysis was to assess the therapeutical advantage of arthrocentesis over stabilization splints, other non-invasive approaches in treatment of temporomandibular disc displacement disorders without reduction. All the studies included in the study evaluated patients who had temporomandibular joint disc displacement disorders without reduction according to diagnostic criteria for temporomandibular disorders (DC/TMD). Only one study assessed patients with osteoarthritis in temporomandibular joint in addition to internal derangement disorders of temporomandibular joint. Temporomandibular disc displacement without reduction can occur due to functional imbalance in the joint either due to microtrauma (overloading of joint due to para-functional activities) or macrotrauma (sudden force affecting temporomandibular joint) [30, 31]. Increased laxity of joint, elongation of ligaments, changes in position and morphology of condyle are also one of the predisposing factors for disc displacement [32, 33]. Incidence rate of this disorder is around 2–8% among the TMD patients [34, 35]. There are various treatment options are available for this disorder but there is lacking amount of evidence on application of specific treatment procedure for this disorder [36]. Al-baghdadi et al. found no significant differences between non-invasive conservative interventions and minimally invasive or invasive surgical interventions in the treatment of disc displacement without reduction. It has been also stated that disc displacement without reduction should be treated first with minimal and less invasive intervention and more invasive treatment approach should only be taken in the requirement of any objective clinical needs [37].
Many techniques of arthrocentesis have been mentioned till now in literature. Murakami et al. [38] first described a unique technique of TMJ arthrocentesis by using pumping irrigation and hydraulic pressure to the upper joint cavity followed by manipulation of the jaw. Later on, Nitzan et al. [7] described a different technique utilizing the insertion of two needles into the upper joint compartment which permitted more effective lavage of the joint. For two-needle technique, access is performed by taking Holmlund–Hellsing line (canthotragal line joining medial portion of tragus and outer canthus of ipsilateral eye) as a reference plane [39]. Ideal range of volume for irrigation solution has been mentioned in literature as 50–500 ml [40]. Ringer's lactate or physiological saline are mostly has been used as an irrigating solution [41]. Ringers lactate showed more effective result than normal saline due to its chemically similar nature to human serum [42–44].
Different types of non-invasive therapies have been mentioned in literature regarding temporomandibular joint disorders ranging from pharmacological approach (analgesics, anti-inflammatory drugs, anxiolytic agents, antidepressants) to various physiotherapy procedures [2]. Physical self-regulation protocol proposed by Bertrand and Carlson also became one of the effective approaches in treatment of temporomandibular joint disorders [45]. Occlusal splints have been used for a long time in dentistry for treatment of temporomandibular joint disorders. There are almost eight factors that can modulate treatment outcome after occlusal splint therapy. Stabilization splint is a type of occlusal splint made up off acrylic or polycarbonate which stabilizes maxilla and mandible, provides occlusal stability and decrease muscles tension [46, 47]. Stabilization splints are fabricated in musculoskeletally stable position by giving even and simultaneous contact on all the teeth. Canine guided occlusion also provided in eccentric movements [2].
Pficer et al. [48] showed stabilization splint improved symptoms in short term but in follow-up periods no statistically significant improved effect found compared with other therapeutic modalities. Although previously many systematic reviews have been done to evaluate the effect of stabilization splint but conclusive evidence still not generated [49–55].
Hosgor et al. [16] conducted a study, in which 40 individuals were selected and all of them had group II temporomandibular disorders according to the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD): disc displacement (DD) with reduction/DD without reduction with limited opening/DD without reduction without limited opening. 19 cases were diagnosed as disc displacement with reduction and 21 cases were diagnosed as disc displacement without reduction. First group of patients underwent occlusal splint therapy and arthrocentesis was done in second group of patients. NSAIDs and low-level laser therapy were applied in other two groups. Maximal mouth opening increased and pain level decreased in all the groups (P < 0.05;). However, statistically significant changes were not found in between the groups (P > 0.05). After 6 months Arthrocentesis group showed more increased mouth opening compared to mouth opening after pre-op and 1-month period. Outcome data of only Arthrocentesis group and occlusal splint groups were included as determined by predetermined inclusion criteria.
Tatli et al. [15] included 120 patients who were diagnosed as unilateral TMJ disc displacement without reduction both clinically and through magnetic resonance imaging. All the patients had persistent pain despite of taking non-steroidal anti-inflammatory drugs (NSAID) and muscle relaxants, soft diet for 2 weeks. Patients were divided into three groups—group 1 (Arthrocentesis only), group 2 (Arthrocentesis and stabilization splint), group 3 (stabilization splint only). Groups 1 and 2 showed similar pain values at the 1-, 3-, and 6-month follow-up visits (P = 1.000, P = 0.951, and P = 1.000, respectively). However, group 3 showed significantly higher pain level than in groups 1 and 2 at all follow-up visits (P < 0.01). The differences in maximum mouth opening values between groups 1 and 2 were not significant in follow-up periods (1 month, P = 0.577; 3 months, P = 1.000; 6 months, P = 0.685). However patients in group 1 and group 2 showed significantly greater degree of mouth opening than those of group 3 at all follow-up visits (all P < 0.001).
Diraçoğlu et al. [18] similarly selected one hundred twenty consecutive patients diagnosed of disc displacement without reduction. Two different treatment approaches arthrocentesis or a combination of splint, hot pack, and home exercise programme were given to two groups. Baseline pain (Visual analog score) values of the arthrocentesis and conventional treatment groups were 6.26 ± 2.3 cm and 5.66 ± 2.4 cm, and baseline maximum mouth opening values were 31.2 ± 7.0 mm and 29.89 ± 4.8 mm, respectively. Pain score was decreased in both the groups after 1, 3, 6 months compared to baseline values. Arthrocentesis group showed greater decrease in pain value compared to other group. Regarding maximal mouth opening, no statistically significant differences were found between the baseline values and values in follow-up periods.
In another study twenty-four patients with clinically diagnosed symptomatic closed lock (disc displacement without reduction) underwent either non-invasive (information, self-exercise, occlusal splints) therapy and minimally invasive (information, arthrocentesis with lavage, manipulation, postoperative self-exercise) therapy. Although there were no statistically significant improvements found regarding pain value (VAS) and maximum mouth opening in between both the groups, however condition improved in both the groups after treatment compared to baseline values. After 1 year there was 63% improvement for the non-invasive group and 57% improvement for the minimally invasive treatment group. VAS scores improved 77.8% for the non-invasive group and 82.7% for the minimally invasive treatment group [19].
Ohnuki et al. [17] compared four different treatment therapies splint therapy, pumping manipulation, arthrocentesis, and arthroscopic surgery. Total eighty-five patients with unilateral internal derangement (disc displacement without reduction) or osteoarthritis that were treated with success were included in this retrospective study. In all groups, there was significant improvement in mouth opening and pain value after treatment (P < 0.01). However, no significant difference was found among the groups. Outcome data from only splint group and arthrocentesis group were included in this review.
Limitations of this review include selection of articles published in English languages only, less number of studies available according to predetermined inclusion criteria, high heterogeneity in between studies. Within limitations of this study results of meta-analysis showing statistically significant improvement in maximum mouth opening among the included studies in favour of arthrocentesis (Mean Difference: 3.10; 95% CI 1.74, 4.45; P ≤ 0.00001). Pain value (VAS 1–10) in three studies also improved in arthrocentesis when intergroup data were estimated (Mean difference: 2.00; 95% CI 0.29, 3.71; P = 0.02).
Conclusion
Arthrocentesis showed effective result in terms of increase in mouth opening and reduction of pain level compared to stabilization splint and other non-invasive approaches in patients with disc displacement disorders without reduction. Overall, results supported the rationale of using arthrocentesis in patients with disc displacement disorders without reduction.
Acknowledgements
Nil.
Funding
Nil.
Declarations
Conflict of interest
The authors have no actual or potential conflicts of interest.
Human and Animals Rights
Review article, not involving any human participants/or animals.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bappaditya Bhattacharjee, Email: bappadityabhattacharjee1@gmail.com.
Rathindra Nath Bera, Email: rathin12111991@gmail.com.
Arju Verma, Email: arju6000@gmail.com.
Romesh Soni, Email: rsoni80@gmail.com.
Atul Bhatnagar, Email: atuldent@hotmail.com.
References
- 1.Meghan K, Murphy BE, Regina F, MacBarb BS, Wong ME, Athanasiou KA. Temporomandibular joint disorders: a review of etiology, clinical management, and tissue engineering strategies. Int J Oral Maxillofac Implants. 2013;28:e393–e414. doi: 10.11607/jomi.te20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okeson JP. Management of temporomandibular disorders and occlusion. St. Louis: CV Mosby; 2008. [Google Scholar]
- 3.Bell WE. Temporomandibular disorders: classification, diagnosis, management. Chicago: Year Book Medical; 1986. [Google Scholar]
- 4.Dawson PE. Functional occlusion from TMJ to smile design. St. Louis Missouri: Elsevier Mosby; 2007. [Google Scholar]
- 5.Solberg WK, Woo MW, Houston JB. Prevalence of mandibular dysfunction in young adults. J Am Dent Assoc. 1979;98:5–34. doi: 10.14219/jada.archive.1979.0008. [DOI] [PubMed] [Google Scholar]
- 6.Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain. 1999;13:232–237. [PubMed] [Google Scholar]
- 7.Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49:1163–1167. doi: 10.1016/0278-2391(91)90409-F. [DOI] [PubMed] [Google Scholar]
- 8.Nishimura M, Segami N, Kaneyama K, Sato J, Fujimura K. Comparison of cytokine level in synovial fluid between successful and unsuccessful cases in arthrocentesis of the temporomandibular joint. J Oral Maxillofac Surg. 2004;62:284–287. doi: 10.1016/j.joms.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 9.Dimitroulis G, Dolwick MF, Martinez A. Temporomandibular joint arthrocentesis and lavage for the treatment of closed lock: a follow-up study. Br J Oral Maxillofac Surg. 1995;33:23–26. doi: 10.1016/0266-4356(95)90081-0. [DOI] [PubMed] [Google Scholar]
- 10.Kaneyama K, Segami N, Nishimura M, Sato J, Fujimura K, Yoshimura H, et al. The ideal lavage volume for removing bradykinin, interleukin-6, and protein from the temporomandibular joint by arthrocentesis. J Oral Maxillofac Surg. 2004;62:657–661. doi: 10.1016/j.joms.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 11.Moses JJ, Sartoris D, Glass R, Tanaka T, Poker I. The effect of arthroscopic surgical lysis and lavage of the superior joint space on TMJ disc position and mobility. J Oral Maxillofac Surg. 1989;47:674–678. doi: 10.1016/S0278-2391(89)80004-7. [DOI] [PubMed] [Google Scholar]
- 12.Sembronio S, Albiero AM, Toro C, Robiony M, Politi M. Is there a role for arthrocentesis in recapturing the displaced disc in patients with closed lock of the temporomandibular joint? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:274–280. doi: 10.1016/j.tripleo.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lo CK, Mertz D, Loeb M. Newcastle-Ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tatli U, Benlidayi ME, Ekren O, Salimov F. Comparison of the effectiveness of three different treatment methods for temporomandibular joint disc displacement without reduction. Int J Oral Maxillofac Surg. 2017;46:603–609. doi: 10.1016/j.ijom.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 16.Hosgor H, Bas B, Celenk C. A comparison of the outcomes of four minimally invasive treatment methods for anterior disc displacement of the temporomandibular joint. Int J Oral Maxillofac Surg. 2017;46:1403–1410. doi: 10.1016/j.ijom.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 17.Ohnuki T, Fukuda M, Nakata A, Nagai H, Takahashi T, Sasano T, Miyamoto Y. Evaluation of the position, mobility, and morphology of the disc by MRI before and after four different treatments for temporomandibular joint disorders. Dentomaxillofac Radiol. 2006;35:103–109. doi: 10.1259/dmfr/25020275. [DOI] [PubMed] [Google Scholar]
- 18.Diraçoğlu D, Saral IB, Keklik B, Kurt H, Emekli U, Ozçakar L, et al. Arthrocentesis versus nonsurgical methods in the treatment of temporomandibular disc displacement without reduction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:3–8. doi: 10.1016/j.tripleo.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 19.Malekzadeh BO, Cahlin BJ, Widmark G. Conservative therapy versus arthrocentesis for the treatment of symptomatic disk displacement without reduction: a prospective randomized controlled study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:18–24. doi: 10.1016/j.oooo.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Lee SH, Yoon HJ. MRI findings of patients with temporomandibular joint internal derangement: before and after performance of arthrocentesis and stabilization splint. J Oral Maxillofac Surg. 2009;67:314–317. doi: 10.1016/j.joms.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 21.Ghanem WA. Arthrocentesis and stabilizing splint are the treatment of choice for acute intermittent closed lock in patients with bruxism. J Craniomaxillofac Surg. 2011;39:256–260. doi: 10.1016/j.jcms.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Yucel MA, Gozneli R, Alkumru HN, Kulak-Ozkan Y. Evaluating the additional effects of arthrocentesis on the condylar pathways of temporomandibular joint in patients with internal derangement treated with stabilizing splint. J Craniomaxillofac Surg. 2014;42:e86–90. doi: 10.1016/j.jcms.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Lee HS, Baek HS, Song DS, Kim HC, Kim HG, Kim BJ. Effect of simultaneous therapy of arthrocentesis and occlusal splints on temporomandibular disorders: anterior disc displacement without reduction. J Korean Assoc Oral Maxillofac Surg. 2013;39:14–20. doi: 10.5125/jkaoms.2013.39.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bilici IS, Emes Y, Aybar B, Yalçın S. Evaluation of the effects of occlusal splint, trigger point injection and arthrocentesis in the treatment of internal derangement patients with myofascial pain disorders. J Craniomaxillofac Surg. 2018;46:916–922. doi: 10.1016/j.jcms.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 25.Tvrdy P, Heinz P, Zapletalova J, Pink R, Michl P. Effect of combination therapy of arthrocentesis and occlusal splint on non-reducing temporomandibular joint disk displacement. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015;159:677–680. doi: 10.5507/bp.2014.044. [DOI] [PubMed] [Google Scholar]
- 26.Vos LM, Slater JJRH, Stegenga B. Arthrocentesis as initial treatment for temporomandibular joint arthropathy: a randomized controlled trial. J Craniomaxillofac Surg. 2014;42:134–139. doi: 10.1016/j.jcms.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 27.Murakami K, Hosaka H, Moriya Y, Segami N, Iizuka T. Short-term treatment outcome study for the management of temporomandibular joint closed lock. A comparison of arthrocentesis to nonsurgical therapy and arthroscopic lysis and lavage. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:253–257. doi: 10.1016/S1079-2104(05)80379-8. [DOI] [PubMed] [Google Scholar]
- 28.Machon V, Hirjak D, Lukas J. Therapy of the osteoarthritis of the temporomandibular joint. J Craniomaxillofac Surg. 2011;39:127–130. doi: 10.1016/j.jcms.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 29.Higgins JPT, Altman GD, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huddleston Slater JJ, Lobbezoo F, Onland-Moret NC, Naeije M. Anterior disc displacement with reduction and symptomatic hypermobility in the human temporomandibular joint: prevalence rates and risk factors in children and teenagers. J Orofac Pain. 2007;21:55–62. [PubMed] [Google Scholar]
- 31.Greene CS. Concepts of TMD etiology: effects on diagnosis and treatment. Chicago: Quintessence; 2006. [Google Scholar]
- 32.Kaplan A, Assel LA. Temporomandibular disorders: diagnosis and treatment. Philadelphia: W.B. Saunders Company; 1991. [Google Scholar]
- 33.Vichaichalermvong S, Nilner M, Panmekiate S, Petersson A. Clinical follow-up of patients with different disc positions. J Orofac Pain. 1993;7:61–67. [PubMed] [Google Scholar]
- 34.Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:453–462. doi: 10.1016/j.tripleo.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 35.Poveda-Roda R, Bagan JV, Sanchis JM, Carbonell E. Temporomandibular disorders. A case-control study. Med Oral Patol Oral Cir Bucal. 2012;17:e794–e800. doi: 10.4317/medoral.18040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Durham J, Exley C, Wassell R, Steele JG. Management is a black art—professional ideologies with respect to temporomandibular disorders. Br Dent J. 2007;202:682–683. doi: 10.1038/bdj.2007.369. [DOI] [PubMed] [Google Scholar]
- 37.Al-Baghdadi M, Durham J, Araujo-Soares V, Robalino S, Errington L, Steele J. TMJ disc displacement without reduction management: a systematic review. J Dent Res. 2014;93:37–51. doi: 10.1177/0022034514528333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murakami KI, Iizuka T, Matsuki M, Ono T. Recapturing the persistent anteriorly displaced disk by mandibular manipulation after pumping and hydraulic pressure to the upper joint cavity of the temporomandibular joint. Cranio. 1987;5:17–24. doi: 10.1080/08869634.1987.11678169. [DOI] [PubMed] [Google Scholar]
- 39.Guarda-Nardini L, Manfredini D, Ferronato G. Arthrocentesis of the temporomandibular joint: a proposal for a single-needle technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:483–486. doi: 10.1016/j.tripleo.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 40.Al-Belasy FA, Dolwick MF. Arthrocentesis for the treatment of temporomandibular joint closed lock: a review article. Int J Oral Maxillofac Surg. 2007;36:773–782. doi: 10.1016/j.ijom.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 41.Sanromán JF. Closed lock (MRI fixed disc): a comparison of arthrocentesis and arthroscopy. Int J Oral Maxillofac Surg. 2004;33:344–348. doi: 10.1016/j.ijom.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 42.Tozoglu S, Al-Belasy FA, Dolwick MF. A review of techniques of lysis and lavage of the TMJ. Br J Oral Maxillofac Surg. 2011;49:302–309. doi: 10.1016/j.bjoms.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 43.Shinjo H, Nakata K, Shino K, Hamada M, Nakamura N, Mae T, et al. Effect of irrigation solutions for arthroscopic surgery on intraarticular tissue: comparison in human meniscus-derived primary cell culture between lactate ringer's solution and saline solution. J Orthop Res. 2002;20:1305–1310. doi: 10.1016/S0736-0266(02)00062-1. [DOI] [PubMed] [Google Scholar]
- 44.Ebenezer V, Balakrishnan R, Vivek M, Elumalai M. Usage of Ringer's lactate treatment in temporomandibular joint disorder. Biomed Pharmacol J. 2012;5:345–349. doi: 10.13005/bpj/364. [DOI] [Google Scholar]
- 45.Carlson CR, Bertrand P. Self-regulation training manual. Lexington: University Press; 1995. [Google Scholar]
- 46.Ramfjord SP, Ash MM. Reflections on the Michigan occlusal splint. J Oral Rehabil. 1994;21:491–500. doi: 10.1111/j.1365-2842.1994.tb01164.x. [DOI] [PubMed] [Google Scholar]
- 47.Glaros AG, Owais Z, Lausten L. Reduction in parafunctional activity: a potential mechanism for the effectiveness of splint therapy. J Oral Rehabil. 2007;34:97–104. doi: 10.1111/j.1365-2842.2006.01660.x. [DOI] [PubMed] [Google Scholar]
- 48.Pficer JK, Dodic S, Lazic V, Trajkovic G, Milic N, Milicic B. Occlusal stabilization splint for patients with temporomandibular disorders: meta-analysis of short and long term effects. PLoS ONE. 2017;12:e0171296. doi: 10.1371/journal.pone.0171296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Forssell H, Kalso E. Application of principles of evidence-based medicine to occlusal treatment for temporomandibular disorders: are there lessons to be learned? J Orofac Pain. 2004;18:9–22. [PubMed] [Google Scholar]
- 50.Ebrahim S, Montoya L, Busse JW, Carrasco-Labra A, Guyatt GH. The effectiveness of splint therapy in patients with temporomandibular disorders: a systematic review and meta-analysis. J Am Dent Assoc. 2012;143:847–857. doi: 10.14219/jada.archive.2012.0289. [DOI] [PubMed] [Google Scholar]
- 51.Turp JC, Komine F, Hugger A. Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Investig. 2004;8:179–195. doi: 10.1007/s00784-004-0265-4. [DOI] [PubMed] [Google Scholar]
- 52.Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances—evidence of their efficacy. J Am Dent Assoc. 2001;132:770–777. doi: 10.14219/jada.archive.2001.0274. [DOI] [PubMed] [Google Scholar]
- 53.Fricton J, Look JO, Wright E, Alencar FGP, Hong C, Lang M, et al. Systematic review and metaanalysis of randomized controlled trials evaluating intraoral orthopedic appliances for temporomandibular disorders. J Orofac Pain. 2010;24:237–254. [PubMed] [Google Scholar]
- 54.Al-Ani MZ, Davies SJ, Gray RJ, Sloan P, Glenny AM. Stabilisation splint therapy for temporomandibular pain dysfunction syndrome. Cochrane Database Syst Rev. 2004;1:Cd002778. doi: 10.1002/14651858.CD002778.pub2. [DOI] [PubMed] [Google Scholar]
- 55.Aggarwal VR, Lovell K, Peters S, Javidi H, Joughin A, Goldthorpe J. Psychosocial interventions for the management of chronic orofacial pain. Cochrane Database Syst Rev. 2011;11:Cd008456. doi: 10.1002/14651858.CD008456.pub2. [DOI] [PubMed] [Google Scholar]