Abstract
Introduction
Surgery of the midface for non-syndromic patients with maxillo-malar hypoplasia exclusively has had many breakthroughs lately. The surgical techniques for midface surgery are varied and must be selected according to the patient’s problem.
Purpose
The technique is a modification of the Z Osteotomy, the Modified Anterior Z Le Fort III Osteotomy (MAZLFIIIO), is used to correct posteroanterior midface deficiency of 6 mm at most. It can be combined simultaneously with a Le Fort I osteotomy if a greater maxillary advance is needed. MAZLFIIIO advances midface without grafts or distraction osteogenesis. The anterior reposition of the midface is calculated in millimetres and depends on the relation of the eye’s most inferior point, as well as the orbital’s hard and soft tissues. It is a predictable osteotomy, only for patients without vertical excess of the midface. The osteotomy planned is drawn over a stereolithographic model, and then Z-shaped surgical splints are fabricated over it. Transverse midface deficiencies of no more than 4 mm can also be corrected during the malar osteotomy. A great number of patients are operated exclusively with Le Fort I osteotomies, leaving behind an undesirable step between the upper part of the midface and the Le Fort I osteotomy.
Methods
The Modified anterior Z Le Fort III Osteotomy (MAZLFIIIO) was performed in seven patients, from 2016 to 2018.
Results
The results obtained with the proposed osteotomy notably improve the appearance of the patient and provide a better protection of the lower part of the eye, while widening the maxillary sinus.
Conclusion
We consider that maxillo-malar hypoplasias are very common; the surgeon pretends not to give importance to the deformity, exclusively using an advance Le Fort type osteotomy, with both functional and aesthetic treatment being limited. In this article, we give all the elements to perform this Le Fort III Modified Osteotomy in anterior Z, and that it is a combined and routine procedure in midface surgery.
Keywords: Modified Anterior Z Le Fort III osteotomy, 3d stereolithographic model, Midface deficiency
Introduction
Le Fort III osteotomy is a surgical procedure that represents the basic treatment for treating midface deficiency in syndromic craniosynostosis, non-syndromic midface deficiency and midface deformities. Multiple factors can influence midface development in different forms [1–4, 10–12]. Midface osteotomies were described initially by Gilles and Harrison in 1950, but it was Paul Tessier in 1957 who refined the technique and made it usable and predictable. Diverse modifications and concepts about this surgical technique have been introduced through the years to enhance aesthetic and functional results, including the combination of different osteotomies (Le Fort III and Le Fort I) in the same surgery [1–4, 6–8]. The modified Le Fort III osteotomy with interposition grafts has had multiple variations, as well as the sliding osteotomies without grafts in the zygomatic bone. The L-shaped, transverse zygomatic osteotomy was developed by Champy in 1980 [14]. The intraoral oblique sliding osteotomy without grafts was introduced in 1992 by Garcia y Sanchez (Figs. 1, 2) [15].
Fig. 1.
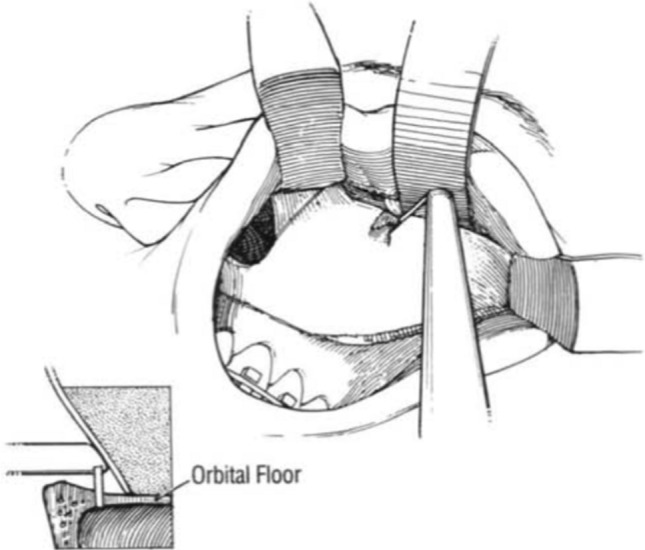
The illustration describes how the anterior orbital floor osteotomy is performed intraorally with an oscillating saw
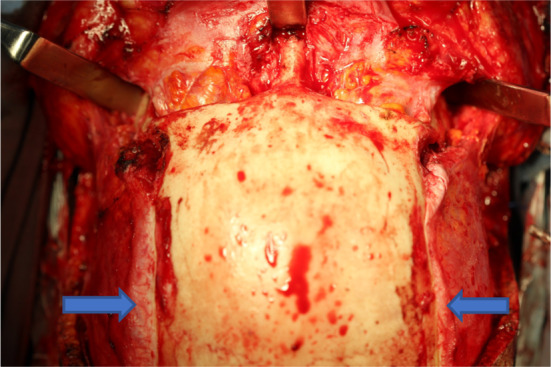
Fig. 2.

The midface disjunction with the intraoral modified oblique Le Fort III osteotomy is shown. This surgical technique was performed by suggestion of the late Dr William H. Bell (15)
The surgical technique of the modified oblique Le Fort III osteotomy with surgical guides made over 3D models was published in 2014 and 2015 [2, 5]. The Z-shaped osteotomy and the ascending osteotomy were published in 2017 [9]. The indications to these osteotomies are varied, for example, projecting the midface, lower orbital border, and the zygomatic bone, correcting lip incompetence without altering the nasal bridge [5–9]. The use of surgical guides for the modified osteotomies facilitates the surgical execution and the symmetry of the results, improving the surgeon’s confidence in manipulating the pterygomaxillary fossa, diminishing the risk of injuring the maxillary artery and shortening surgical time [2, 5, 9, 10, 13]. The modification of the Le Fort III technique allows multiple functional benefits with a positive impact in patient aesthetics as well as in the patient’s airway [5–11].
Material and Methods
The Modified anterior Z Le Fort III Osteotomy (MAZLFIIIO) was performed in 7 patients, from 2016 to 2018, at Hospital de Especialidades Dr. Bernardo Sepulveda in the Centro Medico Nacional Siglo XXI of the Instituto Mexicano del Seguro Social. A 23 mm reciprocating saw and a 7 mm oscillating saw were used in each surgery. Lindemann burs sized 702L and 703L were also employed. An ultrasonic micro-tip cutter and 3D models of each patient were also used.
Planification of the Surgical Technique over the 3D Model
Planning midface surgery combined with lower facial third surgery is more complex than the usual Le Fort I maxillary osteotomy combined with sagittal mandibular surgery. The patient’s profile needs to be fully analysed. The inferior pole of the eye must be identified to adequately locate it compared to the lower orbital rim. A steep and flat lower orbital portion denotes the midface deficiency. In the frontal view, a generalized depression of the lower orbital rim is noted. Also, dystopia is appreciated, noting the right orbit lies lower than the left one. In the lateral image, a deficiency of 6 mm is noted between the upper eyelid and the malar depression in the midface. This is the amount of surgical advancement needed (Fig. 3).
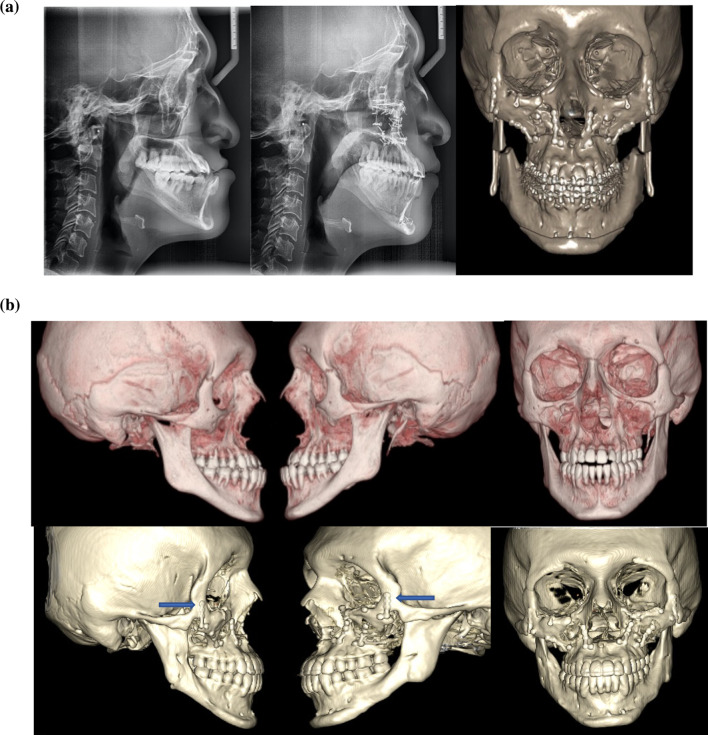
Fig. 3.
Frontal and lateral photographs that demonstrate midface deficiency. In the patient’s profile, the adequate method of measuring midface deficiency is shown, observing a 6 mm posterior position of the zygomatic bone compared to the eyelids, making the patient an ideal candidate for the MAZLFIIIO
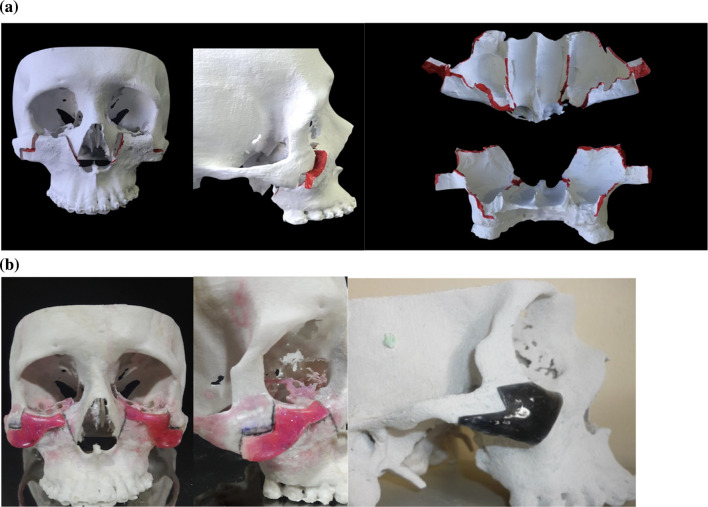
The MAZLFIIIO surgical technique was performed over the 3D model. The red border demonstrates the osteotomy edges, which consist of almost the complete midface, except the nasal bridge. The length and depth of the osteotomy are registered in every part of the model. The walls of the maxillary sinus will augment 6 mm. The surgical guides are fabricated over the MAZLFIIIO, designed with a 6 mm advancement over the zygomatic bone. A comparison between the MAZLFIIIO guides and the modified Z Le Fort III osteotomy (MZLFIIIO) is demonstrated in (Fig. 4a, b).
Fig. 4.
a osteotomy over the 3D model in frontal and lateral views. The distal segment is shown, the red colour demonstrates the sites of the osteotomy. b the surgical guides on the frontal and lateral view. The right image demonstrates the MZLFIIIO guide in onyx colour
Surgical Technique
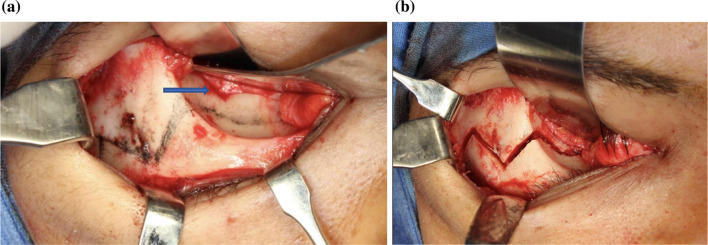
The MAZLFIIIO can be achieved through different surgical approaches, such as coronal, transconjunctival with Mustarde’s canthotomy or subcilliary with Mustarde’s canthotomy, also, intraorally through an extended vestibular incision. The ideal approach to avoid skin scars is the combination of the coronal approach with the transconjunctival approach. For the coronal approach, the dissection must have two fundamental principles, the first, the temporal’s dissection depth must be over the temporal fascia to avoid injuries to the frontal branch of the facial nerve. This cleavage plane is demonstrated by the blue arrows. The second principle consists in having a wide zygomatic dissection in order to be able to perform the osteotomies, such as the ones in (Fig. 5).
Fig. 5.
The coronal flap is extended up to the zygomatic bone and the temporal fasciae remain intact
In order to have adequate access to the orbital floor, a transconjunctival approach is used. This approach has the benefit of leaving no facial scars. For a faster access and diminishing surgical time, a transconjunctival approach with a 15 mm. Mustarde canthotomy is another option but transconjunctival approach with extension through the union of the edges increases the risk of leaving a noticeable scar at the level of the outer edge of the eyelid. The osteotomy goes through the orbital floor in its anterior portion. It is initiated over the zygomatic bone, 5 mm anterior to the inferior orbital fissure as shown by the blue arrow in (Fig. 6). The surgical guide is placed over the zygomatic bone, and the osteotomy is completed (Fig. 6a, b).
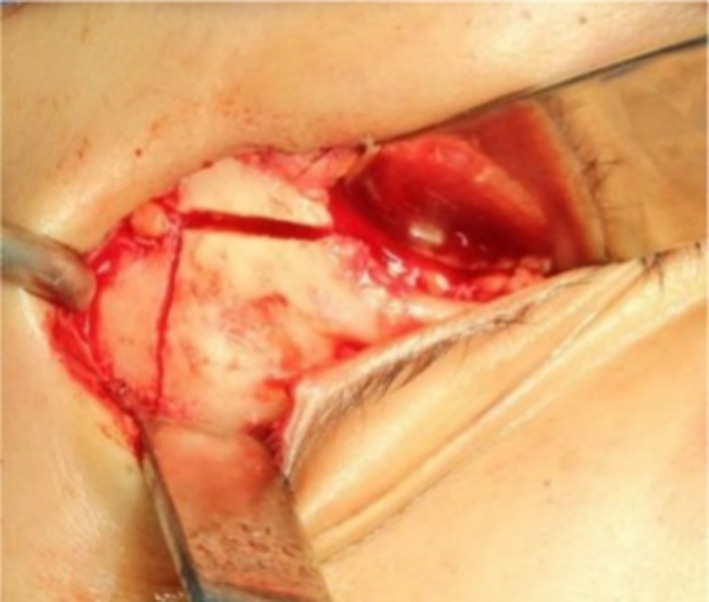
Fig. 6.
a The osteotomy is drawn with a pencil. b The osteotomy is performed after placing the surgical guide
After the orbital and zygomatic osteotomy is finished, the intraoral osteotomies are performed. The approach is through an extended vestibular incision, from the second molar of one side to the opposite second molar. The osteotomy is performed from the pterygoid processes to the orbital floor, 5 mm anterior to the inferior orbital fissure. For this, the surgical guide is needed to perform symmetric osteotomies with the oscillating saw. Note that the green surgical guide is used in this area and it also possess a metal hook located in its most superior portion to protect the inferior orbital contents (Figs. 7, 8) [2, 9]. The objective is to make the craniofacial disjunction symmetrical and in accordance with the surgical planification. The millimetres advanced in the zygomatic bone correspond to the same amount of advancement in the pterygoid region.
Fig. 7.

The surgical guide is positioned over the pterygomaxillary buttress in an anterior view
Fig. 8.

Posterior view of the pterygomaxillary guide with a security hook to stop the oscillating saw from entering the pterygomaxillary fossa and the inferior orbital content. The pink triangle corresponds to the danger zone in which the maxillary artery could be injured
We will explain the above in detail, the osteotomy of the pterygomaxillary fossa. The disjunction of the pterygoid processes is exactly the same as in the Le Fort I Type Osteotomy; however, an ascending oblique linear osteotomy with a length of 4 to 4.5 cm in its entirety is required. The osteotomy is performed in two sections with an oscillating saw (7 mm saw for women and 12 mm for men). The first section goes from the pterygoid junction until it reaches below the posterior buttress, sinking the saw blade completely, to have a better view it is recommended to remove the fat bag of bichat. The second section will be performed following the direction marked by a surgical guide (green) designed on a stereolithographic model. The osteotomy is performed at this level with the 7 mm oscillating blade regardless of whether it is a female or male patient, this step is performed by exclusively sinking half of the saw into the bone until reaching the orbital floor, specifically the osteotomy is finished at 5 mm ahead of the inferior orbital fissure. All of this osteotomy takes place within the pterygomaxillary fossa.
Next, an osteotomy is done from the orbital floor, approximately 5 mm lateral to the nasolacrimal duct, descending to the pyriform rim below the inferior turbinate. The nasal wall is dissected as in conventional Le Fort I osteotomy and the osteotomy are continued along the lateral nasal wall, stopping anterior to the descending palatine artery. This osteotomy is connected to the descending osteotomy that comes from the inferior orbital rim as shown in (Figs. 9, 10) [15]. Next, the septum disjunction is performed conventionally from the anterior nasal spine to the posterior nasal spine. Contralateral osteotomies are performed as described previously. Before the craniofacial disjunction is performed, the osteotomies are visualized and probed to make sure they have been adequately executed to avoid bad splits. If a simultaneous Le Fort I osteotomy is needed, the MAZLFIIIO is fixed first with osteosynthesis and then the Le Fort I osteotomy is performed and subsequently fixed.
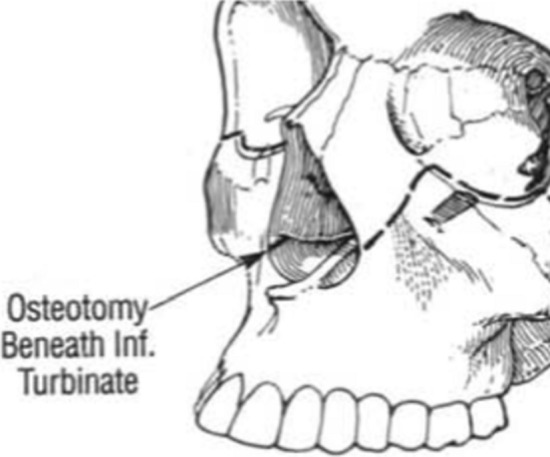
Fig. 9.

Marking of the orbital osteotomy with the oblique descent to the pyriform rim below the inferior turbinate
Fig. 10.
The osteotomy is anterior to the descending palatine artery along the medial nasal wall
Analysis of the Le Fort III Osteotomy Developed by Champy
The Champy’s Modified Le Fort III osteotomy (CMLFIIIO) is an extraordinary technique for correcting midface deficiencies no greater than 5 mm in a posteroanterior view. The osteotomy is shown in (Fig. 11) [9]. The 3D model is shown in lateral and frontal views in Figs. 12, 13.
Fig. 11.
The osteotomy engulfs the zygomatic base
Fig. 12.
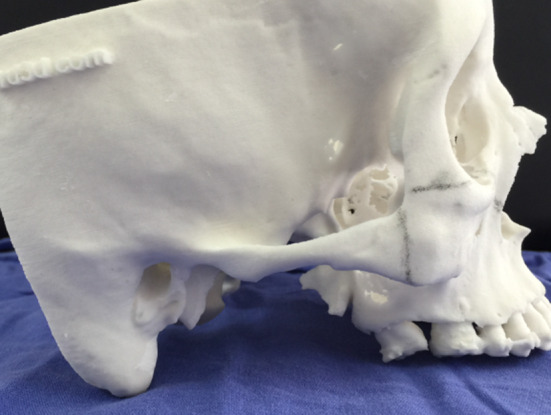
Lateral view of the 3d model
Fig. 13.
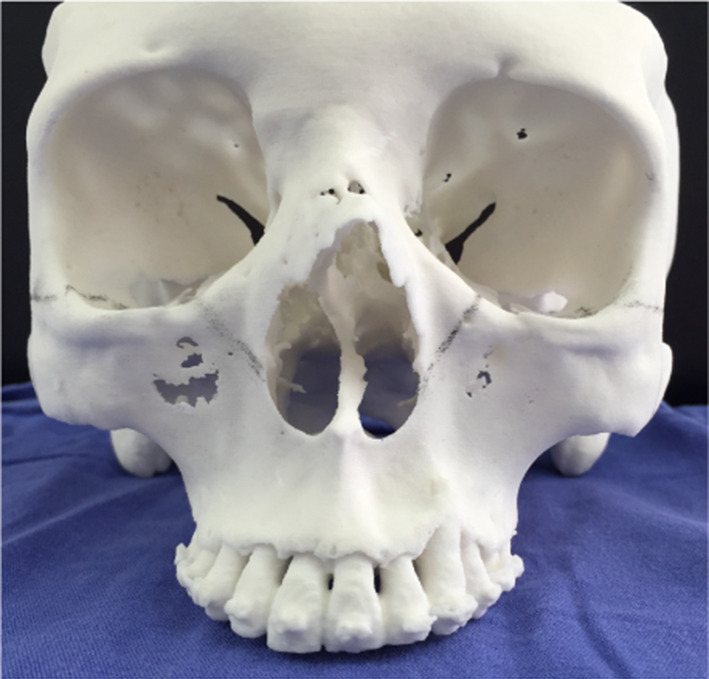
Frontal view of the 3d model
With our currently described technique, which was inspired by diverse modifications of the Champy osteotomy, no grafts are required as it is a sliding osteotomy.
The CMLFIIIO was performed in a 35-year-old patient. The zygomatic osteotomy is symmetrically and easily performed in the 3d model as well as in the patient with the help of surgical guides (Fig. 14). If there is a vertical discrepancy between the left and right side of the face, it can be corrected without an additional Le Fort I osteotomy by ascending or descending the affected side.
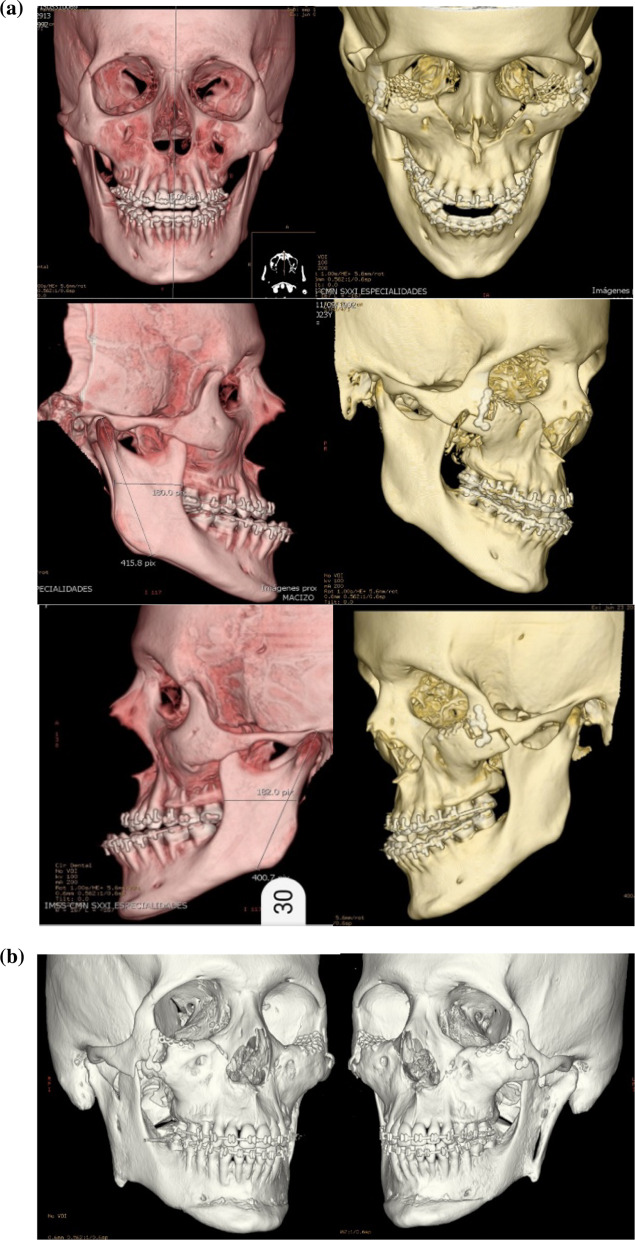
Fig. 14.
Lateral views of the CT scan as well as frontal view. This is then printed, and then surgical splints are fabricated over the 3D model
In the 3d reconstruction of the patient’s CT scan at 4 years postop, it can be appreciated that the midface can have rigid fixation only at the zygomatic bone with one L-shaped plate on each side. The patient underwent a mandibular setback of 3 mm, genioplasty advancement of 7 mm and CMLFIIIO with a 4 mm advancement. In Fig. 15, the blue arrows show the bone gap. This is the reason why CMLFIIIO cannot have more than 5 mm in advancement. Also, a complete consolidation can be observed at the piriform rim (Fig. 15).
Fig. 15.
Postop lateral and frontal views of the CT scan. CMLFIIIO with symmetric osteotomies, adequate consolidation and bone modelling. Gaps remain at the zygomatic bone
Preop and postop photographs of the patient demonstrate an adequate aesthetic result, correcting scleral exposition below the limbus and good zygomatic bone projection. A slight deepening of the skin is noted over the zygomatic bone, shown with the blue arrow. Labial incompetence was also corrected (Fig. 16).
Fig. 16.
Preop and postop photographs. Adequate aesthetic outcome with a slight skin depression over the zygomatic bone shown in the blue arrow
Case 1
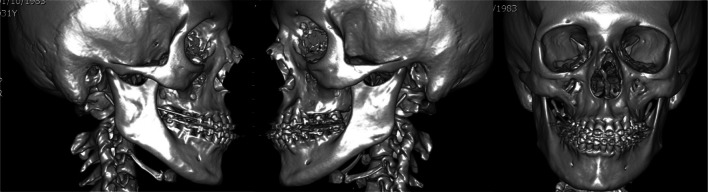
32-year-old male who underwent 2 surgeries. The first was a MAZLFIIIO with a 6 mm advancement through a coronal and transconjunctival approach. The second surgery was a Le Fort I osteotomy with a 5 mm advancement and a 6 mm advancement genioplasty. The midface deficiency is shown in the CT scan (Fig. 17). After the MAZLFIIIO, a CT scan was made, where the symmetric osteotomies have an advancement of 6 mm and an upward movement of the right side, of 3 mm. Only 2 L-shaped plates were placed over the zygomatic bones, and orbital meshes were also used to cover the 6 mm gap at the floor of the orbit (Fig. 18).
Fig. 17.
Preop CT scans
Fig. 18.
CT scan after the first surgery, where the symmetry of the osteotomies is demonstrated as well as the L-shaped plates on both zygomatic bones with 2 orbital meshes covering the orbital floor gap. On the frontal view, symmetry is observed in osteotomies and in the plates. The orbital meshes are used to cover the 6 mm gap at the floor of the orbit and firmly adapted to the inner orbit
The patient showed dystopia (shown with a line that traverses both corneas. This dystopia was corrected significantly with the MAZLFIIIO, by ascending the right side of the midface 3 mm more than the left side, without the need of craniofacial surgery. On the frontal view of the 3D scan, the symmetry of the MAZLFIIIO on the inferior orbital rim can be observed through the lower lid thus, correcting the orbital dystopia. The photographs in Fig. 19 can be used to demonstrate how the midface and orbital dystopia can be corrected through the MAZLFIIIO with only one surgical procedure. Lateral photographs demonstrate how the MAZLFIIIO differs from the MZLFIIIO by maintaining a bony bridge superior and medially and leaving a gap medially and inferior (Fig. 19).
Fig. 19.
In frontal view and in the CT scan, midface deficiency and its surgical outcome can be appreciated, as well as the transverse orbital dystopia. Lateral views demonstrate the midface projection after the surgery, correcting the midface deficiency with the MAZLFIIIO. The 3D reconstruction of the soft tissues has a blue arrow that signals the gap produced by the MAZLFIIIO and the red arrow signals the bony bridge between the zygomatic bone’s body and the zygomatic arch
Sagittal CT scan demonstrate an increase in the airway’s volume produced by the MAZLFIIIO, taking as a reference point, the distance between the posterior nasal spine and the anterior part of the odontoid process (Fig. 20). The advancement remains the same at the level of the zygoma and the superior part of the airway. The preop distance was of 36.7 mm and the postop distance of 42.1, having an increase of 5.4 mm. The Le Fort III advancement surgery in any form will always increase the upper airway’s measurements and volume.
Fig. 20.
Sagittal view demonstrating that a 6 mm advancement at the zygomatic orbital rim, achieved a 5.4 mm advancement at the upper airway
The result after orthognathic surgery can be seen in the lateral preop and postop photographs with structural bony and soft tissue changes. Facial balance is acceptable, and the 6 mm labial incompetence was corrected (Fig. 21). Dental occlusion went from a class III to I on the right side and from III to II in the left side due to de absence of the superior second premolar (Fig. 22).
Fig. 21.
The preop and postop photographs after the MAZLFIIIO and a delayed 6 mm Le Fort I advancement and genioplasty. The orbital rim structure improved aesthetically by protecting the globe with the inferior orbital border advancement, which also improved the zygomatic bone projection. The frontal photographs demonstrate an aesthetic improvement, correcting midface deficiency, orbital dystopia and lip incompetence
Fig. 22.
Pre-operatory and post-operatory dental occlusion. The patient was treated at the Centro de Estudios Superiores de Ortodoncia (CESO by Dr. Maria Angelica Sanchez Contreras)
Case 2
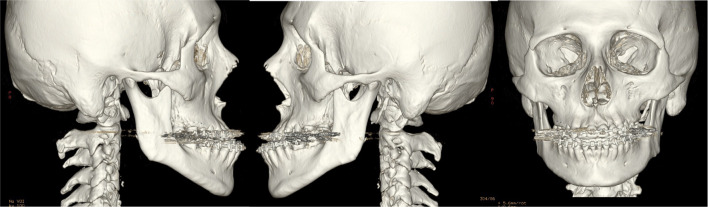
24-year-old male patient with severe midface deficiency. The first surgery was a MAZLFIIIO with a 6 mm advancement through a coronal and transconjunctival approach. He had a posteroanterior discrepancy of 11 mm as shown in the preop lateral radiograph. On the second surgery, a 4 mm advancement Le Fort I osteotomy was performed along with an intraoral inverted L oblique modified osteotomy (IILOMO) with a 3 mm mandibular setback. A basal extended mentoplasty [16] (BEM) of 8 mm was also performed on the patient. The preop and postop lateral radiograph are shown. The 1-day postop CT scan with osteotomies and rigid internal fixation is also shown in Fig. 23a. The preop CT scan and the 2-year postop CT scan of the same patient are shown in Fig. 23b. A symmetric midface advancement with adequate bone consolidation is shown. The IILOMO is shown with adequate bone consolidation and the BEM adds harmony to the basal portion of the mandible without steps, appreciated in Fig. 23b.
Fig. 23.
a Pre- and post-operative lateral radiograph. Significant changes in the midface and lower third of the face can be seen. CT reconstruction immediately following the second surgery. A symmetric MAZLFIIIO can be appreciated along with a simultaneous repositioning of the maxilla, mandible and chin. b CT reconstruction in frontal and lateral views. 3D reconstruction at 2 years postop
Result after orthognathic surgery can be seen in lateral and frontal views. An acceptable facial balance was achieved, changing the patient’s physiognomy for better (Fig. 24). The dental occlusion went from a class III to a class I (Fig. 25).
Fig. 24.
Significant facial changes can be observed
Fig. 25.
Preop and postop dental occlusion
Case 3
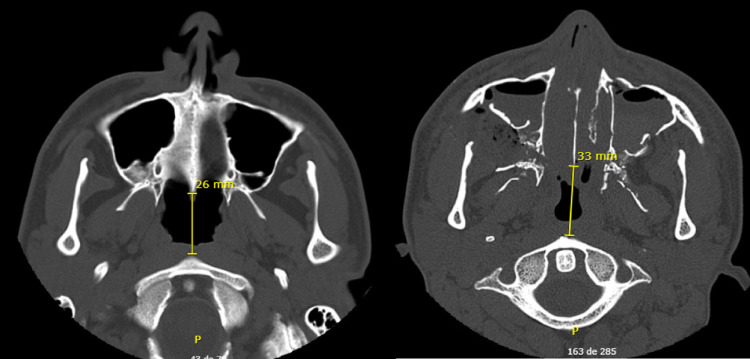
21-year-old male patient with severe midface deficiency. The first surgery was a 6 mm in advancement MAZLFIIIO through a transconjunctival with lateral canthotomy approach. The patient had a -10 mm overjet. After surgery, orthodontic treatment was indicated, and a second surgery was performed. The patient underwent an intraoral vertical subsigmoid osteotomy (IVSO) with a 6 mm setback and a BEM with an 8 mm advancement. The preop and postop CT scan demonstrates the MAZLFIIIO. Symmetry can be appreciated at the osteotomy sites, achieved through surgical guides (Fig. 26a).
Fig. 26.
a CT scan with 3D reconstruction preop and postop. Note the symmetry of the osteotomies. b 1-year postop 3D reconstruction. Adequate bone consolidation of the midface can be seen, achieving stability and symmetry of the MAZLFIIIO. The IVSO is adequately adapted. The BEM is also adequately consolidated to the mandibular body
A CT scan 1 year postop demonstrates a stable and symmetric midface advancement. The blue arrows indicate the zygomatic arch as one piece without any gaps. The IVSO is shown with adequate bone consolidation; however, the left proximal segment was displaced 3 mm lateral of the articular cavity. Nevertheless, the patient is asymptomatic. The BEM allows for an adequate facial harmony at the inferior border of the mandible without any steps, seen in Fig. 26b.
Axial images demonstrate the increase in the distance between the anterior nasal spine and the body of the axis (Fig. 27). The preop distance was of 26 mm and the postop of 33 mm.
Fig. 27.
Axial views of the CT scan demonstrating midface advancement
The result after the orthognathic surgery can be seen in the frontal and lateral views. The facial physiognomy was improved, as well as the dental occlusion which went from a class III to class I (Figs. 28, 29).
Fig. 28.
Preop and postop photographs side by side, demonstrating surgical outcome
Fig. 29.
Preop and postop photographs of dental occlusion, side by side
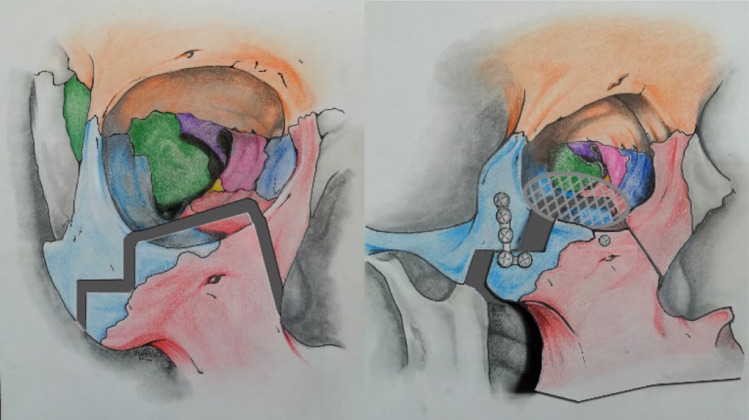
Results
The aesthetic improvement obtained with upper airway amplification through an MAZLFIIIO makes this technique an option for advancing the zygomatic and maxillary bones in midface deficiency. Adequate stability is obtained through the demonstrated rigid internal fixation. Also, an additional Le Fort I osteotomy can be performed if needed. Patients with maxillo-malar hypoplasia present short faces, when advancing the middle third, facial height is increased in Le Fort III Ostectomies Modified in Z and in anterior Z, facial height is also significantly increased by BEM Osteotomy.
The left image describes the osteotomy line, from the zygomatic bone, through the orbital floor and to the pyriform rim. The right image describes the adequate plate positioning through an L-shaped plate pertaining to a 1.5 plating system. Additionally, an orbital mesh can be placed over the orbital floor (Fig. 30).
Fig. 30.
MAZLFIIIMO images
Advantages
Midface deficiency correction, which is relatively common in patients with concave profile. A maximum midface advancement of 6 mm can be successfully achieved to protect the inferior portion of the eye.
Harmonic facial balance and aesthetics between the midface and the lower face.
Significant increase in upper airway.
Le Fort I osteotomy can be performed if needed.
Midface asymmetry can be addressed if it’s less than 4 mm in a vertical direction.
Only two L-shaped plates are needed.
Disadvantages
Midface deficiencies greater than 6 mm cannot be achieved due to a possible Z-shaped asymmetry in the zygomatic bone and a gap could be produced, along with skin depression.
This surgical technique is not for vertical midface excess.
Should not be used in severe syndromic midface deficiencies because usually, more than 6 mm in advancement are needed for those patients.
Complications
- 1.
Neurosensory defects: The only anatomical region that could be affected neurosensoryly is the infraorbital branch due to the osteotomy of the orbital floor and the elongation of the infraorbital nerve when the midface moves forward. This infraorbital branch is extremely elastic. When a neurectomy is performed before breaking the nerve, it supports an elongation of approximately 8-10mm [5] (Fig. 31); Let us remember that the anterior Z osteotomy is only indicated in a maximum advance of 6mm, therefore the elongation suffered by the advance does not cause a rupture of the infraorbital neurovascular bundle.
- 2.
Hemorrhage: The guides were devised for the ascending cut towards the inferior orbital fissure in the pterygomaxillary fossa (see Fig. 8), thus reducing the possibility of damage to the maxillary artery. The hemorrhage, as in a Le Fort I osteotomy, can come from the descending palatal artery, and which can be avoided in the following way: since in the 3D printing model or the stereolithographic, the distance from the piriformis opening to In the greater palatine foramens, the average distance that we have found between these two anatomical structures is approximately 32 to 36mm. With this exact position of the palatine foramen, we performed the osteotomy 5mm before reaching this point. The superoposterior alveolar arterial branches can bleed as in the Le Fort I Osteotomy, as an element of hemostasis we routinely use the bipolar coagulator.
- 3.
Deviation of the nasal septum: When impacting the middle third, an importation and fracture of the nasal septum would occur, to avoid this situation once the craniofacial disjunction is made, the separated middle third of the skull is lowered and as in a Le Fort I Osteotomy A groove is made from the posterior nasal spine to 3mm before the nasopalatine foramen, this is to avoid septal deviation and the nasal septum will have a new resting position.
- 4.
Unfavorable skull base fractures or pterygoid processes: Fortunately we have not had skull base fractures but there are chances of it happening, so we suggest that this type of osteotomy be performed first in the 3D or stereolithographic model, the surgeon It will observe in detail the position of the pterygoid processes with the maxillary tuberosity and will perform the osteotomy on the model, providing it with precise knowledge of the depth of the osteotomies of both the pterygomaxillary fossa and the pterygoid processes.
Fig. 31.

Infraorbitary nerve is preserved, the figure is shown in an anatomical model of the cadaver [5]
Discussion
The MAZLFIIIO is based on the Modified Le Fort III Osteotomy in Z (this technique designed for maxillo-malar deficiencies of more than 6 mm), the difference between the two will be the millimetres required by the patient to move the middle facial third forward. The MAZLFIIIO will be used more frequently because most maxillo-malar hypoplasias are 6 to 4 mm. The two techniques can only be used in patients who do not have a vertical excess of the maxilla.
Conclusions
We consider the MAZLFIIIO to be an alternative for patients with midface deficiency in which a conventional Le Fort I osteotomy would be insufficient for improving midface aesthetics. These patients have an exposed sclera inferior to the limbus without adequate lower lid coverage. Upper airway widening and zygomatic repositioning give functional and aesthetic improvements, compared with alloplastic implants which do not modify upper airway and tend to produce pits over the bone in which they are placed.
Due to the osteotomy’s characteristics, surgical guides should be designed to safely approach the pterygomaxillary fossa so that the surgeon can safely cut through this area. Surgical guides make the surgery safe and accurate.
Funding
No funding was needed.
Declarations
Conflict of interest
There are no conflicts of interest within the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Garcia y Sánchez Jose Manuel, Email: maxilofacialcirugiasuperlativa@gmail.com.
D.A. Valdes Martínez, Email: cmfvaldes@hotmail.com.
Lopez Bonilla Salvador, Email: maxilofacialbonilla@hotmail.com.
Rosales Díaz Mirón Dayel Gerardo, Email: cmfdayel@gmail.com.
Estrada Orozco Juan José, Email: juanjosestrada16@gmail.com.
Elizalde Monroy Martin, Email: elizaldecmf@live.com.mx.
Reyes Huerta Pablo, Email: pabloseyer@gmail.com.
References
- 1.Cheung L, Ow A, Chua H. Simultaneous modified oblique Le Fort III and segmentalized Le Fort I osteotomies. J Oral Maxillofac Surg. 2010;68:915–923. doi: 10.1016/j.joms.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Garcia y Sanchez JM, Gomez C, Romero J. Surgical guides for modified oblique Le Fort III osteotomy. J Maxillofac Oral Surg. 2014;2:487–496. doi: 10.1007/s12663-014-0620-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown M, Okada H, Valiathan M, Lakin G. 45 years of simultaneous Le Fort III and Le Fort I osteotomies: a systematic literature review. Cleft Palate Craniofac J. 2015;52:1–9. doi: 10.1597/14-005R. [DOI] [PubMed] [Google Scholar]
- 4.Vu D, Tiwana P (2015) Le Fort III and Le Fort II osteotomies. Atlas Oral AND Maxillofac Surg Clin N Am 1–10 [DOI] [PubMed]
- 5.Garcia y Sanchez JM, Romero J, Gomez C. Modified oblique Le Fort III osteotomy new concepts. J Maxillofac Oral Surg. 2016;1:22–42. doi: 10.1007/s12663-016-0893-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sebastiani A, Rebelatto N, Kluppel L. Le Fort III osteotomy for severe dentofacial deformity correction associated with hypoplasia of the midface. Rev Gaúch Odontol Porto Alegre. 2016;64:453–459. doi: 10.1590/1981-8637201600030000143129. [DOI] [Google Scholar]
- 7.Magraw C, Garaas R, Shaw A, Phillips C, Turvey T. Changes in scleral exposure following modified Le Fort III osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;04:1–22. doi: 10.1016/j.oooo.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Boos Lima F, Hochuli E, Juergens P (2017) Is sub cranial Le Fort III plus Le Fort I osteotomy stable? J Cranio-Maxillo-Facial Surg 1–7 [DOI] [PubMed]
- 9.Garcia y Sanchez JM, Gomez C, Pacheco G. Modified Le Fort III osteotomy: different applications. J Maxillofac Oral Surg. 2017;1:1–10. doi: 10.1007/s12663-017-1021-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Orra S, Tierney W, Capone A, Gharb B (2017) Relevant surgical anatomy of pterygomaxillary disjunction in Le Fort III Osteotomy. Plast Reconstr Surg 701–709 [DOI] [PubMed]
- 11.Boos Lima F, Dutra C, Pereira-Filho V, Hochuli-Vieira E, Lima S. Three-dimensional airway changes after sub cranial Le Fort III osteotomy combined with Le Fort I osteotomy. Int J Oral Maxillofac Surg. 2017;46:320. [Google Scholar]
- 12.Fariña R, Valladares S, Raposo A, Silva F. Modified Le Fort III osteotomy: A simple solution to severe midfacial hypoplasia. J Cranio-Maxillo-Facial Surg. 2018;3:1–36. doi: 10.1016/j.jcms.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Choi W, Yang W, Leung M, Su Y. Application of three-dimensional printed plates in Le Fort III osteotomy. J Oral Maxillofac Surg. 2019;48:113. doi: 10.1016/j.ijom.2019.03.346. [DOI] [Google Scholar]
- 14.Maxime C. Surgical treatment of midface deformities. Head Neck Surg. 1980;2(6):451–65. doi: 10.1002/hed.2890020603. [DOI] [PubMed] [Google Scholar]
- 15.Garcia Sanchez JM (1992) Oblique modified Le Fort III osteotomy chapter 50: modern practice in orthognathic and reconstructive surgery, vol 3. William Bell. Saunders, Philadelphia
- 16.Garcia Sanchez JM, Cols A. Basal extended mentoplasty. J Maxillofac Oral Surg. 2020;1:1–14. doi: 10.1007/s12663-020-01474-0. [DOI] [PMC free article] [PubMed] [Google Scholar]