Abstract
Objectives
Pharmacists in Nova Scotia have had legislated authority to prescribe since 2011. This study aimed to describe the prescribing activities of pharmacists and the characteristics of patients who used pharmacist prescribing services.
Methods
Using provincial health administrative databases we identified all community pharmacists who prescribed during the study period (October 2016 to March 2020) and correspondingly patients who had medications prescribed by a pharmacist during this period. Differences in, and predictors of the quantity of pharmacist prescribing over three fiscal years (April 2017 to March 2020) were described. Pharmacist prescribing activity was compared across the fiscal years of the study period with One-way Analysis of Variance. Negative binomial regression examined patient factors associated with use of pharmacist prescribing services. Analysis was carried out using SAS ENTERPRISE GUIDE v.8.2 (SAS Institute Cary, NC, USA).
Key findings
A total of 1182 pharmacist prescribers were identified, who on average prescribed 24.6, 26.3, and 32.5 (p < 0.001) times per month in fiscal years 2018, 2019, 2020, respectively. The patient cohort contained 372,203 Nova Scotians over the 3-year period. For approved common and minor ailment prescribing in Nova Scotia, gastroesophageal reflux disease, vaccines (non-travel), contraceptive management, herpes zoster treatment, and allergic rhinitis had the highest number of prescriptions over the study period. Patient factors most strongly related to receiving more prescribing services by a pharmacist included receiving income assistance without copay (Incidence rate ratio (IRR) = 1.70), having >2 comorbidities (IRR = 1.51), male sex (IRR = 1.03), and greater age (IRR = 1.01). Those from an urban area (IRR = 0.92) or having a higher income (IRR = 0.95) received fewer pharmacist prescribing services (all p < 0.0001).
Conclusions
Pharmacist prescribing increased over the 3-year period. Patients who were older and those with multiple comorbidities used pharmacist prescribing services most often. Prescribing activities represent an increasingly utilized role for pharmacists in primary care.
Keywords: Pharmacists, Nova Scotia, Primary health care, Vaccines, Drug prescriptions
1. Introduction
Pharmacists' scope of practice has been increasing worldwide to facilitate the changing needs of patients and healthcare systems which has included the implementation of various prescribing activities.1,2 Some studies conducted globally report benefits of pharmacist prescribing, including: ease of patient access to healthcare services, improved patient outcomes, and reduced physician workload.3, 4, 5 Canadian studies of pharmacist prescribing note high levels of patient satisfaction and increased accessibility of health care.4,6,7 In addition, pharmacist prescribing for common and minor ailments has been shown to be cost effective.5 For example, in the Canadian province of Saskatchewan, the Pharmacists Prescribing for Minor Ailments (PPMA) program saved the province approximately $546,832 in 2014.8
Increased access to healthcare interventions including medications through prescribing services of those who have prescribing privileges is important given continued strain on the healthcare system due to the COVID-19 pandemic and the ongoing challenge of access to family physicians and nurse practitioners in many Canadian provinces.9,10 In the province of Nova Scotia, Canada, the number of people over the age of 12 who reported not having a regular healthcare provider has increased from over 47,000 as of March 2020 (the last month of the fiscal year covered in this study) to over 85,000 people as of March 2022 (over 8% of the population of Nova Scotia), and continues to grow.11,12
Revision of the prescribing standards for pharmacists in Nova Scotia has been ongoing since the original standards were approved in 2011 and has culminated in pharmacist prescribing services in 2022 that include: renewals, adaptations (alteration of a dosage form or dose of a specific medication to meet supply availability), therapeutic substitutions (substituting medications that are therapeutically equivalent), prescribing in an emergency, prescribing for conditions approved by Council (which includes common or minor ailments, preventative care, such as vaccines, and prescribing for a diagnosis supported by protocol, such as uncomplicated cystitis (bladder infections), and ordering and interpreting lab tests.13 Government funding for pharmacist assessment and prescribing for a limited number of approved conditions (uncomplicated cystitis, herpes zoster (shingles), and contraception management) was implemented in January 2020, after previously being paid for by patients as an out-of-pocket expense.14 Government funding of pharmacist prescribing services may have increased accessibility for management of approved conditions by allowing community pharmacists to meet these medication related needs.
The objective of the study is to describe pharmacist prescribing over three fiscal years (2018, 2019, and 2020) including the characteristics of pharmacist prescribers and patients who used pharmacist prescribing services in Nova Scotia, Canada.
2. Methods
This was a retrospective observational cohort study using linked administrative health data. Provincially de-identified data were accessed through Health Data Nova Scotia (HDNS).15 Data from the Drug Information System (DIS), Insured Patient Registry (MASTER), Licensed Provider Registry (DOCTORS), Medical Services Insurance (MSI) Physician Billings (MED), and the Canadian Institute for Health Information Discharge Abstract Database (CIHI-DAD) was accessed.16 DIS data were linked to MASTER data to identify sociodemographic information. Census data from Statistics Canada and the DIS and were linked to MASTER to provide rurality and aggregated relative household income by geographic area. MED and inpatient hospital data from CIHI-DAD were linked to measure continuity of primary care, via an established definition17 (described further in measures) that assessed the number of ambulatory providers seen by the patient as well as the number of visits.
The study period began on October 1, 2016, which represented inception of the province wide DIS and ended on March 31, 2020, which was the final day in the third fiscal year and the end of the period of study.
The study was approved by Dalhousie University Health Sciences Research Ethics Board on November 29, 2019, REB #2019–4961 with annual approvals.
2.1. Setting
The base of the cohort was all prescriptions written by a community pharmacist and captured in the DIS. The DIS is a province-wide system that contains a record of every prescription filled for a patient in a community pharmacy in Nova Scotia and is held by the provincial government health department. All community pharmacists, certified dispensers, and pharmacy technicians are required to disclose drug dispenses to the DIS, which is included under the regulations in the provincial Pharmacy Act. This system allows healthcare providers to access a patient's medication profile, and is part of the province's electronic health record system.18 Pharmacists were first authorized to prescribe in Nova Scotia in 2011, under specific circumstances. At the time of this study, pharmacists' scope of practice for prescribing included all drugs except for controlled drugs and substances (e.g., opioids, benzodiazepines).
Canada does not have universal drug coverage; however, each province provides some medication insurance coverage, typically for those over 65 years of age or within and under specific income brackets. Paying for prescription medications outside of government plans can occur through privately funded insurance, typically through the patient's employment, or for those without insurance coverage, by the patient directly. Many Canadians have out-of-pocket costs related to premiums and co-payments/co-insurance regardless of whether they have a private or publicly insured drug plan. In Canada, only 42% of prescription drug costs are covered by public programs, with 35% covered by private insurance and 23% by out-of-pocket payment.19 Private medication insurance programs were not captured in this analysis and were grouped with those who do not have any prescription medication insurance coverage (i.e., uninsured).20 Public insurance plans for those with low income are captured in this study, each with different eligibility enrollment criteria and co-payment costs, further described in methods.
Two distinct populations were analyzed in this study:
-
1.
Pharmacists registered to practice in Nova Scotia who had a record of prescribing at least once in the DIS during the study period, and
-
2.
Nova Scotia residents who had received prescribing from a pharmacist in the province at least once over the study period.
2.2. Measures
Demographic information were abstracted for pharmacists and patients from the HDNS databases. Licensed pharmacists practicing across community, hospital, and other settings (e.g., long term care, industry) who provided direct care to patients, with at least one prescribing record through community pharmacies in the DIS over the study period were included. Pharmacist's geographic location, obtained from the DOCTORS database, was classified as urban or rural based on the pharmacist's most recently self-reported county. To assess prescriptions written by pharmacists over the period of observation, a record of the first prescription written by a pharmacist (not including refills on the same prescription) was extracted from the DIS. Each prescription written by a pharmacist was categorized into one of six categories of prescribing (Table 1). For purposes of this study, it was not possible to differentiate between these types in the DIS. To identify drugs associated with common and minor ailments, drug identification numbers (DINs are Health Canada assigned numbers for drug products being marketed in Canada)21 associated with each common or minor ailment or approved condition were identified by a pharmacist (RL), first by identifying all appropriate treatment options for each condition (Table 2). All relevant DINs (i.e., for products either currently marketed or marketed during the study period) were identified using the Nova Scotia Formulary (https://novascotia.ca/dhw/pharmacare/documents/formulary.pdf)22 and Health Canada's Drug Product Database (https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/drug-product-database.html).23 For classes of medications not listed on the Nova Scotia Formulary (i.e., vaccines), Anatomical Therapeutic Chemical (ATC) codes for all relevant therapeutic classes were identified using the World Health Organization's ATC/DDD Index and then searched in the Drug Product Database to identify the corresponding DINs (see Appendix A, Supplementary Material 1). Relevant medications for each minor ailment/approved condition were identified using treatment algorithms available through several different resources including the Compendium of Pharmaceuticals and Specialties (CPS), the University of Saskatchewan's Minor Ailment and Self-Care Prescribing Guidelines, and documents from the Pharmacy Association of Nova Scotia.24., 25., 26. This led to an assumption that medications prescribed by a pharmacist were associated with the identified common or minor ailment/approved condition even though indication was not identified on the prescription nor captured directly in the administrative data.
Table 1.
Pharmacist Prescribing Categories with Definitions in Nova Scotia as of January 2022.58
| Pharmacist Prescribing Categories | Definitions |
|---|---|
| Approved Conditions | Prescribing for minor and common ailments from an approved list of conditions; when a diagnosis is provided by a primary care provider or specialist, or a diagnosis supported by a protocol. |
| Prescribing in Emergency | Prescribing when a patient has an immediate, urgent, and high-risk medical requirement for medication. |
| Prescribing Renewals | Prescribing to continue a current medication with a new prescription. The new prescription as written may include refills; but when a patient is dispensed a refill it is not counted as a prescribing service. |
| Prescribing Adaptions | Prescribing to modify the dose, formulation, regimen and/or duration of therapy when a diagnosis is known, and an intended treatment requires modification for dispensing either related to medication supply issues or specific patient factors. |
| Prescribing Therapeutic Substitutions | Prescribing to substitute with a therapeutically equivalent medication due to medication supply issues or specific patient factors. |
| Prescribing Drugs That Do Not Require a Prescription* | Prescribing any drugs that do not require a prescription as a condition of sale. This includes medications that may require pharmacist assessment prior to sale (Schedule II) or may be available for self-selection in the pharmacy (Schedule III) |
*Health Canada determines whether a drug is prescription or non-prescription; Schedule II and III refer to non-prescription designations assigned by the National Association of Pharmacy Regulatory Authorities (NAPRA).59
Table 2.
Minor and common ailments and approved conditions available for pharmacist assessment and prescribing in Nova Scotia as of January 2022.60
| Minor and Common Ailments | Allergic Rhinitis Calluses and Corns Contact Allergic Dermatitis Cough Dandruff Dysmenorrhea (menstrual cramps, not hormonal contraception) Dyspepsia Emergency Contraception Fungal Infections of the Skin Gastroesophageal Reflux Disease (GERD) Hemorrhoids Herpes Simplex (Cold Sores) Impetigo Mild Acne Mild Headache Mild to Moderate Eczema Mild Urticaria (Including Bites and Stings) Minor Joint Pain Minor Muscle Pain Minor Sleep Disorders Nasal Congestion Nausea Non-Infectious Diarrhea Oral Fungal Infection (Thrush) Oral Ulcers Pinworms Smoking Cessation Sore Throat Threadworms Vaginal Candidiasis Warts (excluding facial and genital) Xerophthalmia (Dry Eyes) |
| Preventative Medicine | Antimicrobial Prophylaxis in Special Circumstances Comprehensive Travel Health (with additional certification) Contraceptive Management⁎ Travel and Non-Travel Vaccines |
| Diagnosis Supported by a Protocol | Chemoprophylaxis for Lyme Disease⁎⁎ Herpes Zoster⁎ SARS-CoV-2⁎⁎ Uncomplicated Cystitis⁎ |
Government funding available for noted services as of January 1, 2020.
Services not available during study period.
Individuals with a valid Nova Scotia MSI identification who received prescribing services from a pharmacist in the province within the study period were included in the patient cohort. Patients were assigned to census areas based on their postal code as reported on October 1, 2016 and were classified as urban or rural using census data from Statistics Canada (urban areas were classified as those with at least 1000 people and a population density of at least 400 per square kilometre).27 Income was assigned based on Statistics Canada quintiles for the patient's local dissemination area. Based on the insured patient registry at HDNS, patient drug programs were identified, as follows:
-
1.
Income Assistance copay15: Includes income assistance clients, disability support program clients, children in the care of child welfare through either a district office of the Department of Community Services or a Children's Aid Society/Family and Children's Services agency, and Low-Income Pharmacare for Children (LIPC) clients who pay a copayment equivalent to 20% of the prescription price up to an annual maximum based on family size and income.
-
2.
Income Assistance no copay: The same as above without a copayment required.
-
3.
Seniors' (Pharmacare) non-GIS: Voluntary prescription medication services insurance program for adults 65 years of age and older who do not receive a guaranteed income supplement (GIS). An annual premium is paid to participate in the Pharmacare program, the cost of which varies by household income. Additionally, an annual copayment is charged, typically 30% of the total cost of each prescription up to an annual maximum.
-
4.
Seniors' (Pharmacare) GIS: Voluntary prescription medication services insurance program for adults 65 years of age and older who receive a guaranteed income supplement, also receive Old Age Security (OAS) pension, and qualify as low income (less than $22,986 per year if single/widowed/divorced or a combined income less than $26,817). The Pharmacare annual premium is not required if an individual is receiving a GIS.
-
5.
Seniors' (Pharmacare) no copay: This is an artifact of older programs that provides the same supports as Seniors' Pharmacare above but without requiring a copay and includes adults living in long-term care settings for a long time.
Enrollment in any of the programs was recorded for each patient. Patients may have enrolled in more than one program over the study period and our data collection allowed individuals to be captured in all programs they were enrolled in over the study period. The insurance programs were not mutually exclusive categories but instead reflected enrollment over the three-year period of observation. Thus, participation in each program was coded dichotomously (yes/no) for each participant.
Continuity of care was assessed using the Modified, Modified Continuity Index (MMCI),28 using physician billings and inpatient hospital discharge abstract data. The MMCI was used to assess dispersion between providers based on the number of providers seen and the number of visits to those providers (as shown in the formula below). The index values range from 0 (each visit made to a different physician) to 1 (all visits made to one physician). This is a widely used and validated measure to assess continuity of care, and was used in our study to better understand how consistently a patient had access to a usual provider.29,30
Patient comorbidities were defined as per the Canadian Chronic Disease Surveillance System (CCDSS) case definitions (see Appendix A, Supplementary Material 2), which relied on use of data from physician billings and inpatient hospital discharge abstract data. We used 21 of the CDSS case definitions to code for 19 comorbidities (the definitions for stroke and epilepsy were each collapsed across two definitions), and patients were classified into categorical groups to facilitate data analysis by the number of unique comorbidities for which they met case definitions within the study period (0,1,2,>2 comorbid conditions).
2.3. Data analysis
Descriptive data were reported as means and frequencies. Prescribing activity was compared across the fiscal years of the study period with One-way Analysis of Variance (ANOVA) in order to best compare the average rates of prescribing across all community pharmacists who prescribed in each year of the study. Changes in prescribing by pharmacists were analyzed by fiscal year (as previously defined). Differences in prescribing frequency between pharmacists in rural versus urban areas were compared via an independent samples t-test. To assess the patient cohort, prescribing activity was compared across demographic characteristics of patients receiving pharmacist prescribing using One-way ANOVAs when there were more than two groups (e.g., age) or independent samples t-tests (e.g., sex), as appropriate. The Type 1 experiment wise error rate (i.e., multiple comparisons) were corrected in the ANOVA procedure via Bonferroni (Dunn) t-tests for post-hoc comparisons.
To further understand the relationship between patient demographic factors and frequency of receiving prescribing services by a pharmacist, a negative binomial regression model was run. The outcome was number of prescriptions received from a pharmacist, with predictors including age, sex, geography, MMCI value, income quintile, co-morbidity count, and drug plan. All data analysis was carried out using SAS ENTERPRISE GUIDE v.8.2 (SAS Institute, Cary, NC, USA).
3. Results
There were a total of 1182 unique pharmacists identified as prescribers over the study period. The number of prescribers was lower in the first year with 987 pharmacist prescribers in 2018, 984 in 2019, and 1000 in 2020. Prescribing frequency, defined as the number of prescribing activities carried out by each pharmacist per month, was lower in 2018 (x = 24.6) compared to 2020 (x = 32.5) (p < 0.05) (see Table 3).
Table 3.
Pharmacist Prescribing Activity Frequency, 2017–2020.
| Number of Unique Pharmacist Prescribers Per Year | Mean Number of Prescriptions/Month | 95% CI | p-value | |
|---|---|---|---|---|
| Fiscal Year | <0.001 | |||
| 2018 | 987 | 24.6 | [23.4, 25.7] | |
| 2019 | 984 | 26.3 | [25.1, 27.5] | |
| 2020 | 1000 | 32.5 | [31.0, 34.0] | |
| Geography | <0.001 | |||
| Rural | 663 | 25.8 | [24.3, 27.4] | |
| Urban | 519 | 18.0 | [16.6, 19.5] |
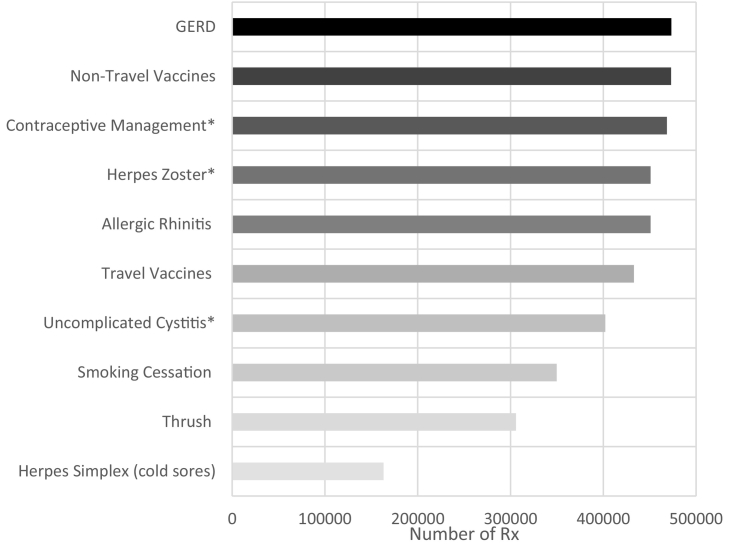
The frequency of approved conditions (including common and minor ailments) prescribed by pharmacists during the study period was estimated (Fig. 1). The number of pharmacists prescribing for each approved condition varied significantly (n = 273 for herpes simplex treatment compared to n = 1098 for gastroesophageal reflux disease (GERD). The highest number of prescriptions dispensed were for GERD medications during the study period (frequency = 473,327), followed by non-travel vaccines and contraceptive management (frequency = 473,021, and 468,520 respectively). Almost all pharmacists identified in the sample prescribed for the following: 1098 (93%) prescribed at least once for GERD, 1044 (88%) for non-travel vaccines and 1066 (90%) for contraceptive management. The fewest number of pharmacists prescribed for herpes simplex over the study period (23%), which was also the condition for which the fewest prescriptions were written (frequency = 163,185).
Fig. 1.
Total number of pharmacist prescriptions per approved condition over the period from fiscal years 2018 through 2020.
*Services with government funding that began January 1, 2020.
A total of 372,203 unique patients were identified who had at least one record of receiving pharmacist prescribing services (see Table 4). The mean number of prescriptions per patient was higher per person for older (x = 4.32 for those 80+ years) compared to younger patients (x = 1.78 for those younger than 18 years) (p < 0.0001). More females used pharmacist prescribing than males (213, 247 versus 158, 213), but males received more prescriptions from pharmacists on average compared to females (2.97 versus 2.88 p < 0.0001). There were fewer prescriptions per patient for patients from higher income quintiles compared to lower quintiles (p < 0.05), and those in rural areas received more prescriptions per person than those in urban areas (3.17 versus 2.79, p < 0.0001). The median MMCI value for the full patient cohort was 0.80 (IQR = 0.31). The average number of prescriptions received was lower for those with fewer comorbidities, 2.21 for people with no comorbidities, 3.13 to those with 1 comorbidity, and 3.22 for those with 2 or more comorbidities (p < 0.05) (Table 4).
Table 4.
Patient sociodemographic characteristics and volume of medications prescribed by a pharmacist in the categories described.
| Number of Medications Prescribed |
|||
|---|---|---|---|
| N | mean ± SD | p+ | |
| Age (years) | |||
| <18 | 31,908 | 1.78 ± 1.18 | All groups significantly different at p < 0.05* |
| 18–34 | 53,781 | 2.02 ± 1.99 | |
| 35–49 | 64,673 | 2.56 ± 2.84 | |
| 50–59 | 72,042 | 3.00 ± 3.49 | |
| 60–69 | 75,099 | 3.25 ± 3.58 | |
| 70–79 | 48,399 | 3.79 ± 4.41 | |
| ≥80 | 25,558 | 4.32 ± 1.19 | |
| Sex | |||
| Female | 213,247 | 2.88 ± 3.41 | <0.0001 |
| Male | 158,213 | 2.97 ± 3.51 | |
| Income quintile* | |||
| Q1 | 68,677 | 3.13 ± 3.92 | All groups significantly different at p < 0.05* |
| Q2 | 76,323 | 3.07 ± 3.65 | |
| Q3 | 73,152 | 2.94 ± 3.37 | |
| Q4 | 76,240 | 2.81 ± 3.24 | |
| Q5 | 77,068 | 2.66 ± 3.06 | |
| Geography | |||
| Rural Residence | 126,525 | 3.17 ± 3.73 | <0.0001 |
| Urban Residence | 244,935 | 2.79 ± 3.30 | |
| Drug Plan vs. No Drug Plan (includes private plans) | |||
| Income Assistance Copay | 13,393 | 2.65 ± 3.40 | <0.0001 |
| Income Assistance No Copay | 13,387 | 4.59 ± 6.07 | <0.0001 |
| Seniors' (Pharmacare) Non-GIS | 72,268 | 3.45 ± 3.82 | <0.0001 |
| Seniors' (Pharmacare) GIS | 45,988 | 4.16 ± 4.90 | <0.0001 |
| Seniors' (Pharmacare) No Copay | 239 | 5.19 ± 6.23 | <0.0001 |
| No Plan Captured in DIS | 244,301 | 2.52 ± 2.76 | |
| Number of Comorbidities | |||
| 0 | 153,546 | 2.21 ± 2.18 | All groups significantly different at p < 0.05* |
| 1 | 92,535 | 3.13 ± 3.45 | |
| 2 | 79,737 | 3.22 ± 3.75 | |
| >2 | 46,385 | 4.33 ± 5.35 | |
p values shown represent the results from an independent samples t-test, or one-way ANOVA post-hoc tests if >2 groups *Bonferroni correction applied.
Individuals with no history of accessing a public medication insurance program during the study period had the lowest pharmacist prescribing rates, with 2.52 prescriptions per person. For people on income assistance, those with no co-pay had a significantly higher average number of prescriptions per person compared to those with a co-pay (2.65 versus 4.590 (p < 0.0001). For Seniors' Pharmacare beneficiaries, those with no co-pay had the highest mean number of prescriptions during the study period (5.19), which was significantly higher than Seniors' Pharmacare beneficiaries with the guaranteed income supplement (GIS) (4.16), and those with no GIS (3.45) (p < 0.0001).
Patient demographic factors were entered into a negative binomial regression model to understand the relationship between these factors and the frequency of receiving prescription services by a pharmacist (see Table 5). Having received income assistance without copay (IRR = 1.70, p < 0.0001), having >2 comorbidities (IRR = 1.51, p < 0.0001) were the factors most associated with increased prescribing. Conversely, those with higher income (IRR = 0.95, p < 0.0001 for Q5), receiving income assistance with copay (IRR = 0.89, p < 0.0001), and living in an urban area (IRR = 0.91, p < 0.0001) were associated with decreased pharmacist prescribing.
Table 5.
Total number of pharmacist prescribed prescriptions per approved condition over the period from fiscal years 2018 through 2020.
| Variable | IRR | CI |
|---|---|---|
| Age (continuous) | 1.009 | [1.0088, 1.0092] |
| MMCI | 1.0256 | [1.0133, 1.0381] |
| Sex | ||
| Female | 1 | |
| Male | 1.0253 | [1.0196, 1.031] |
| Geography | ||
| Rural | 1 | |
| Urban | 0.9148 | [0.9096, 0.9202] |
| Income | ||
| Q1 | 1 | |
| Q2 | 0.987 | [0.9785, 0.9955] |
| Q3 | 0.9754 | [0.967, 0.984] |
| Q4 | 0.9508 | [0.9425, 0.9592] |
| Q5 | 0.9496 | [0.9413, 0.9581] |
| Comorbidities | ||
| 0 Comorbidities | 1 | |
| 1 Comorbidity | 1.1959 | [1.1871, 1.2048] |
| 2 Comorbidities | 1.2523 | [1.2428, 1.2619] |
| >2 Comorbidities | 1.5135 | [1.4999, 1.5271] |
| Drug Plan | ||
| No Listed Drug Plan | 1 | |
| Income Assistance Copay | 0.8907 | [0.8764, 0.9053] |
| Income Assistance No Copay | 1.7001 | [1.6765, 1.7241] |
| Seniors (Pharmacare) non-GIS | 0.9831 | [0.976, 0.9903] |
| Seniors (Pharmacare) GIS | 1.1072 | [1.0979, 1.1166] |
| Seniors (Pharmacare) No Copay | 0.8974 | [0.8176, 0.9852] |
Note: Negative binomial regression model examining patient factors associated with use of pharmacist prescribing services.
4. Discussion
This study examined pharmacist prescribing activities over three fiscal years (2018, 2019, 2020). The mean number of prescriptions by pharmacists increased from the first to last fiscal year of the study. Patients who used pharmacist prescribing more frequently, were more likely to be older, male, living with multiple chronic medical conditions, have a higher MMCI value, participating in a government-funded prescription medication insurance program, or living in a rural location. The frequency of prescribing for common and minor ailments was also examined. Prescribing for GERD was the most common, as identified by prescriptions for medications indicated for GERD, followed by prescribing for non-travel vaccines, and contraceptive management.
Medications that treat GERD (such as proton pump inhibitors and H2 receptor antagonists, See Appendix A, Supplementary Material 1 for full list, both of which have some availability as prescription and non-prescription products) were the most frequently prescribed by pharmacists. Given that GERD is a common condition affecting an estimated 15% of the population, this is not surprising.31 Research has indicated that pharmacists may take a cautious approach in prescribing, due to a fear of making errors.32 Given the relative safety of medications used to treat this condition, pharmacists' likely had greater confidence in prescribing for this. Prior to pharmacist prescribing services being available for common and minor ailments, pharmacists would have regularly assessed patients and recommended non-prescription GERD therapies.
Other commonly prescribed medications in Nova Scotia included contraceptive management, herpes zoster, allergic rhinitis, uncomplicated cystitis, smoking cessation, thrush, and herpes simplex. Compared to other published research from the United Kingdom and parts of Europe, these medications differ from what was most commonly reported as prescribed by pharmacists, which included cardiovascular, nervous system, respiratory system, and infectious diseases medications.33,34 Given differences across countries in when independent prescribing for pharmacists began, and related differences in approved conditions for prescribing, this is not unexpected. Many research studies have demonstrated the efficacy and safety of pharmacist prescribing35,36 for conditions such as uncomplicated cystitis, with demonstrated patient satisfaction with this practice.37,38
Vaccines, both those recommended or required for travel and non-travel use, were present in the top 10 prescribing services accessed. Travel vaccines were dominated by prescriptions for the combined hepatitis A and B vaccine (Twinrix®) and the oral, inactivated cholera and LT-producing ETEC diarrhea vaccine (Dukoral®) where flu vaccines made up most of the prescriptions in the non-travel category. This likely reflects the convenience for patients based on the hours of operation of a pharmacy and the walk-in services available compared to a family medicine practice. Based on international evidence, other research has confirmed that pharmacists and physicians identified convenience as a significant factor for those seeking vaccination39 which makes the community pharmacy an ideal location for this service. Herpes Zoster (shingles), contraception, and uncomplicated cystitis were also on the list of the top 10 prescribed conditions by pharmacists in this study.
Some of these pharmacist assessment and prescribing services became government funded for all Nova Scotians with MSI in January of 2020, which likely impacted the frequency for which they were prescribed by pharmacists, as patients did not have to pay the assessment fee. This expanded financial coverage for patients needing this service is likely to have increased the affordability of the previously uninsured service provided by pharmacists and thus accessibility of this service. Given the shortage of family physicians in the province it may be difficult to seek timely access to care from a physician, thus the ability to seek timely identification and treatment is important in optimizing patient outcomes. Previous research in Poland has found the most common reason patients access a prescription directly from a pharmacist, is when they are unable to contact their physician for a prescription renewal.40 During the final two weeks of the period studied41 (March 19, 2020 to March 31, 2020), funding was expanded to include publicly-funded prescription renewals for all Nova Scotians with MSI. It is anticipated that pharmacist prescribing has increased even further than seen in the study given this expansion of funded services, as well as the increased role pharmacists in Nova Scotia have been playing since the COVID-19 pandemic.42, 43, 44
Identifying factors related to increased likelihood of using pharmacist prescribing services revealed several interesting trends. Despite there being fewer people in certain demographic groups (e.g., older age groups, being from a rural area), the average number of prescriptions per person was higher in older age groups, for individuals in a rural area, for males, in those with a lower income and with a higher number of comorbidities. Older age cohorts likely used pharmacist prescribing services more often as older adults generally use more medications than younger people.45 In contrast, females tended to have greater medication needs then males, yet males in the study used prescribing services more often on average. Although the study data only provided sex, differences in prescribing for males and females may reflect gender differences in health-seeking behaviour, with research showing that men are less likely than women to visit their primary care provider,46, 47, 48 or to seek out preventative care (e.g., blood pressure checks, influenza vaccinations).49 This delay in seeking care or planning for care in advance may have resulted in an increased need for pharmacist prescribing services for males. Increased pharmacist prescribing in rural areas may also be explained by a reduced use of family physicians based on limited access, as patterns of family physician shortages generally demonstrate reduced access in rural areas.50,51 This may also be related to the geographic accessibility of pharmacies, where seeking out primary care either through a regular provider, a walk-in, or emergency care may be more difficult to access in rural areas, especially during the winter months.52 We also found that patients from lower income quintiles used pharmacist prescribing services more often, which may reflect disparities in access to primary care with research demonstrating that lower income groups face more barriers before reaching primary care practices,53 thus increasing demand on pharmacist care. Measures of comorbidity consistently identified that those with more comorbidities were more likely to use pharmacist prescribing services, again likely related to their higher medication needs.
In Canada, pharmacists have taken on an increasing prescribing role. In a 2017 study in Alberta, almost all pharmacists (93%) reported that they had prescribed, with most for continuity of therapy (92%), followed by substituting a medication due to shortage (80%), and then altering doses (74%).1 Pharmacists with additional prescribing authority were more likely to prescribe to adjust (64%) versus initiate a new medication (18%). This study also found that pharmacists in rural areas were prescribing more frequently. These findings are consistent with our findings in Nova Scotia and explain much of the successes experienced with pharmacist supported services, such as prescribing and vaccination, during the COVID-19 pandemic.42, 43, 44 Pharmacist prescribing increased over the period of this study, which ended right as the COVID-19 pandemic began (World Health Organization declaration was March 11, 2020),54 with few changes in staffing models or supplementary support to facilitate pharmacist prescribing activities. This serves as a baseline to compare changes in pharmacist prescribing during and after the acute pandemic period, alterations in the funding model, or changes in context. Given this increase, there is concern around the sustainability of the current model of pharmacist prescribing services, and future research should seek to understand barriers to prescribing as the healthcare system continues to change to better meet patient needs.
4.1. Limitations
There are several limitations that must be considered with respect to this study, mainly related to the data available. Within the DIS, there was incomplete differentiation between the different types of prescribing services offered. Additionally, when assigning a medication prescription to an associated common and minor ailment this was dependent upon the drug alone and assigned without knowing the indication, as indication was not captured in the DIS. Thus, within the data, the assumption was that medications prescribed by a pharmacist were associated with the most likely identified common and minor ailment/approved condition. In addition, products which have not undergone consideration for interchangeability may have been excluded from the Formulary and may not have been captured when compiling the list of DINs for common and minor ailments. As well, drugs were only identified in the dataset by DIN, so natural health products or other non-prescription medications assigned Natural Product Numbers (NPNs) through the Licensed Natural Health Products Database were not captured.55
There were also limitations with respect to how certain variables were defined within the data available and the associated interpretation of results. With insurance plan, there was limitations due to crossover between plans, where some patients may have been a beneficiary of different insurance plans at various points in the study period. Additionally, there is a large degree of variability in private drug insurance plans and medication coverage across private drug insurance programs. Due to the use of administrative data, we were only able to access data on biological sex of the patient (associated with a patient's MSI data, which to date, only identifies patient sex recorded at birth). Given this, we interpreted sex differences based on data available on gender differences in health service access. However, we were not able to assess patient gender, gender roles or health seeking behaviour directly, which would better facilitate interpretation of data around sex differences as measured in this study.56,57 There were also limitations with respect to the identification of provider demography. The definition of rural and urban for pharmacists was based on the pharmacist's most recently reported license county or city, which may identify a pharmacist's personal address rather than the specific pharmacy where the prescription was dispensed and may not coincide with the time the prescribing took place if prior to their most recently reported address.
5. Conclusions
Pharmacist prescribing services were found to have increased in each subsequent year for each of the three years studied. Patients' who used pharmacist prescribing more frequently were more likely to be older, male, living with multiple chronic medical conditions, have a higher MMCI value, participate in a government funded prescription medication insurance program, or live in a rural location. We believe that pharmacists have a role in improving accessibility to routine medical care and the increasing patient use of pharmacist prescribing services over the study period indicates that the public is interested in accessing these services. Despite increased prescribing over time, there remain opportunities to better understand the optimal level of pharmacist prescribing services to ensure patient needs are met and that pharmacists can sustainably offer these services within their model of practice. Future research could assess the quality of pharmacist prescribing, the supports needed to sustain and expand these services, the impact of the COVID-19 pandemic, and recently increased public funding for pharmacist prescribing services (of which only two weeks of data were captured within the study dates) on patient access, satisfaction, and outcomes.
Funding statement
This work was supported by the Maritime SPOR Support Unit (MSSU), which receives financial support from the Canadian Institutes of Health Research (CIHR), the Nova Scotia Department of Health and Wellness, the New Brunswick Department of Health, the Nova Scotia Health Research Foundation (NSHRF), and the New Brunswick Health Research Foundation (NBHRF). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by the MSSU or the named funding partners is intended or should be inferred.
Declaration of Competing Interest
The data used in this report were made available by Health Data Nova Scotia of Dalhousie University. Although this research analysis is based on data obtained from the Nova Scotia Department of Health and Wellness, the observations and opinions expressed are those of the authors and do not represent those of either Health Data Nova Scotia or the Department of Health and Wellness.
Acknowledgements
The team would like to gratefully acknowledge the support of Dr. David Stock, Ashley Crawford, Katelyn Frizzell, Juanna Ricketts, and Amy Mireault.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rcsop.2023.100221.
Contributor Information
Amy Grant, Email: amyk.grant@nshealth.ca.
Shanna Trenaman, Email: shanna.trenaman@dal.ca.
Samuel Stewart, Email: sam.stewart@dal.ca.
Lihui Liu, Email: Lihui.liu@nshealth.ca.
Elizabeth Jeffers, Email: Elizabeth.jeffers@nshealth.ca.
Rebecca Lawrence, Email: rebecca.lawrence@dal.ca.
Andrea Murphy, Email: andrea.murphy@dal.ca.
Ingrid Sketris, Email: ingrid.sketris@dal.ca.
Lisa Woodill, Email: lisa@pans.ns.ca.
Jennifer E. Isenor, Email: jennifer.isenor@dal.ca.
Appendix A. Supplementary data
Supplementary material 1
Supplementary material 2
References
- 1.Taylor S., Cairns A., Glass B. Expanded practice in rural community pharmacy: a macro-, meso and micro-level perspective. Rural Remote Health. 2021;21:6158. doi: 10.22605/RRH6158. [DOI] [PubMed] [Google Scholar]
- 2.Mizranita V., Sim T.F., Sunderland B., Parsons R., Hughes J.D. Pharmacists’ and pharmacy technicians’ scopes of practice in the management of minor ailments at community pharmacies in Indonesia: a cross-sectional study. Pharm Pract. 2021;19:2295. doi: 10.18549/PharmPract.2021.2.2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jebara T., et al. Stakeholders’ views and experiences of pharmacist prescribing: a systematic review. Br J Clin Pharmacol. 2018;84:1883–1905. doi: 10.1111/bcp.13624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beahm N.P., Smyth D.J., Tsuyuki R.T. Outcomes of urinary tract infection management by pharmacists (RxOUTMAP): a study of pharmacist prescribing and care in patients with uncomplicated urinary tract infections in the community. Can Pharm J CPJ Rev Pharm Can RPC. 2018;151:305–314. doi: 10.1177/1715163518781175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dineen-Griffin S., Vargas C., Williams K.A., Benrimoj S.I., Garcia-Cardenas V. Cost utility of a pharmacist-led minor ailment service compared with usual pharmacist care. Cost Eff Resour Alloc CE. 2020;18:24. doi: 10.1186/s12962-020-00220-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Famiyeh I.-M., MacKeigan L., Thompson A., Kuluski K., McCarthy L.M. Exploring pharmacy service users’ support for and willingness to use community pharmacist prescribing services. Res Soc Adm Pharm RSAP. 2019;15:575–583. doi: 10.1016/j.sapharm.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 7.Bishop A.C., et al. Public perceptions of pharmacist expanded scope of practice services in Nova Scotia. Can Pharm J CPJ Rev Pharm Can RPC. 2015;148:274–283. doi: 10.1177/1715163515596757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rafferty E., Yaghoubi M., Taylor J., Farag M. Costs and savings associated with a pharmacists prescribing for minor ailments program in Saskatchewan. Cost Eff Resour Alloc CE. 2017;15:3. doi: 10.1186/s12962-017-0066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murphy A.L., Simon K., Pelletier E., Miller L., Gardner D.M. Bloom program pharmacy teams’ experiences providing mental health services during the COVID-19 pandemic. Can Pharm J Rev Pharm Can. 2022;155:93–100. doi: 10.1177/17151635211065426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adams J.L., et al. Report of the 2020-2021 strategic engagement standing committee. Am J Pharm Educ. 2021;8715 doi: 10.5688/ajpe8715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nova Scotia Health Authority Finding a primary care provider in Nova Scotia - March 2020. 2020. https://www.nshealth.ca/sites/nshealth.ca/files/finding_a_primary_care_provider_in_nova_scotia_report_march_2020.pdf
- 12.Nova Scotia Health Authority Finding a primary care provider in Nova Scotia - March 2022. 2022. https://www.nshealth.ca/sites/nshealth.ca/files/finding_a_primary_care_provider_in_nova_scotia_report_mar_2022.pdf
- 13.Standards of Practice: Prescribing Drugs. Vol. 23. 2019. [Google Scholar]
- 14.Scotia C.N. New government funding provides expanded pharmacy services. 2018. https://novascotia.ca/news/release/?id=20191209001 News Releases.
- 15.Dalhousie University . Dalhousie University; 2022. Health Data Nova Scotia: Department of Community Health and Epidemiology.https://medicine.dal.ca/departments/department-sites/community-health/research/hdns.html [Google Scholar]
- 16.Data Holdings. Dalhousie University https://medicine.dal.ca/departments/department-sites/community-health/research/hdns/health-databases.html.
- 17.Magill M.K., Senf J. A new method for measuring continuity of care in family practice residencies. J Fam Pract. 1987;24:165–168. [PubMed] [Google Scholar]
- 18.Nova Scotia Department of Health and Wellness E-Health: Drug Information System. 2021. https://novascotia.ca/dhw/ehealth/dis/
- 19.Canadian Institute for Health Information . 2017. National Health Expenditure Trends, 1975 to 2017; p. 45. [Google Scholar]
- 20.The Commonwealth Fund. International Health Care System Profiles: Canada 2020. https://www.commonwealthfund.org/international-health-policy-center/countries/canada
- 21.Health Canada Drug Identification Number (DIN) 2001. https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/fact-sheets/drug-identification-number.html
- 22.Nova Scotia Department of Health and Wellness Nova Scotia Pharmacare: Formulary. 2021. https://novascotia.ca/dhw/pharmacare/formulary.asp
- 23.Canada H. Drug Product Database: Access the database. 2010. https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/drug-product-database.html
- 24.Pharmacy Association of Nova Scotia Resources For Pharmacy Professionals. 2021. https://pans.ns.ca/pharmacy-professionals
- 25.University of Saskatchewan-MedSak Guidelines for Prescribing for Minor Ailments and Patient Self-Care. Minor Ailment and Self-Care Guidelines. 2021. https://medsask.usask.ca/professional-practice/minor-ailment-guidelines.php
- 26.Canadian Pharmacists Association CPS 2020: Compendium of pharmaceuticals and specialities: Canada's trusted drug reference. 2020. https://myrxtx.ca
- 27.Statistics Canada Population Centre and Rural Area Classification 2016. Population Centre and Rural Area Classification 2016. 2016. https://www.statcan.gc.ca/en/subjects/standard/pcrac/2016/introduction
- 28.Magill M.K., Senf J. A new method for measuring continuity of care in family practice residencies. J Fam Pract. 1987;24:165–168. [PubMed] [Google Scholar]
- 29.Reid R.J., Haggerty J., McKendry R. 2002. Defusing the Confusion: Concepts and Measures of Continuity of Healthcare. [Google Scholar]
- 30.Cabana M.D., Jee S.H. Does continuity of care improve patient outcomes. J Fam Pr. 2004;53:974–980. [PubMed] [Google Scholar]
- 31.Eusebi L.H., et al. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–440. doi: 10.1136/gutjnl-2016-313589. [DOI] [PubMed] [Google Scholar]
- 32.Mills T., Patel N., Ryan K. Pharmacist non-medical prescribing in primary care. A systematic review of views, opinions, and attitudes. Int J Clin Pract. 2021;75 doi: 10.1111/ijcp.13827. [DOI] [PubMed] [Google Scholar]
- 33.Zimmermann A., Płaczek J., Wrzosek N., Owczarek A. Assessment of pharmacists prescribing practices in Poland—a descriptive study. Healthcare. 2021;9:1505. doi: 10.3390/healthcare9111505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deslandes P., Blowers H., Haines K., Hodson K., Deslandes R. Medicines prescribed by non-medical independent prescribers in primary care in Wales: a 10-year longitudinal study April 2011–March 2021. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-059204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weeks G., George J., Maclure K., Stewart D. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst Rev. 2016;11 doi: 10.1002/14651858.CD011227.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu J.H.-C., et al. Community pharmacist prescribing of antimicrobials: a systematic review from an antimicrobial stewardship perspective. Can Pharm J CPJ Rev Pharm Can RPC. 2021;154:179–192. doi: 10.1177/1715163521999417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Spann N., et al. Independent pharmacist prescribing of statins for patients with type 2 diabetes: an analysis of enhanced pharmacist prescriptive authority in Idaho. J Am Pharm Assoc JAPhA. 2020;60 doi: 10.1016/j.japh.2019.12.015. S108-S114.e1. [DOI] [PubMed] [Google Scholar]
- 38.Speirits I.A., et al. Patient experiences of pharmacist independent prescriber-led post-myocardial infarction left ventricular systolic dysfunction clinics. Int J Pharm Pract. 2021;29:55–60. doi: 10.1111/ijpp.12662. [DOI] [PubMed] [Google Scholar]
- 39.Jusufoska M., Abreu de Azevedo M., Tolic J., Deml M.J., Tarr P.E. ‘Vaccination needs to be easy for the people, right ?’: A qualitative study of the roles of physicians and pharmacists regarding vaccination in Switzerland. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-053163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zimmermann A., Płaczek J., Wrzosek N., Owczarek A. Assessment of pharmacists prescribing practices in Poland—a descriptive study. Healthcare. 2021;9:1505. doi: 10.3390/healthcare9111505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nova Scotia Pharmacare . 2020. Nova Scotia Formulary Updates: MARCH 2020. https://novascotia.ca/dhw/pharmacare/pharmacare-news-bulletins.asp https://novascotia.ca/dhw/pharmacare/pharmacists_bulletins/Pharmacists_Bulletin_March_20-03.pdf. [Google Scholar]
- 42.Mohamed Ibrahim O., Ibrahim R.M., Ibrahim Y.A., Madawi E.A., Al Deri M.Y. Shedding the light on Pharmacists’ roles during COVID-19 global pandemic. Saudi Pharm J SPJ Off Publ Saudi Pharm Soc. 2022;30:14–27. doi: 10.1016/j.jsps.2021.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lin Y.W., Lin C.H., Lin M.H. Vaccination distribution by community pharmacists under the COVID-19 vaccine appointment system in Taiwan. Cost Eff Resour Alloc CE. 2021;19:76. doi: 10.1186/s12962-021-00331-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stämpfli D., et al. Community pharmacist-administered COVID-19 vaccinations: a pilot customer survey on satisfaction and motivation to get vaccinated. Vaccines. 2021;9:1320. doi: 10.3390/vaccines9111320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Canada Institute of Health Information Drug Use Among Seniors in Canada, 2016. 69. 2016. https://secure.cihi.ca/free_products/drug-use-among-seniors-2016-en-web.pdf
- 46.Thompson A.E., et al. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. 2016;17:38. doi: 10.1186/s12875-016-0440-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schlichthorst M., Sanci L.A., Pirkis J., Spittal M.J., Hocking J.S. Why do men go to the doctor? Socio-demographic and lifestyle factors associated with healthcare utilisation among a cohort of Australian men. BMC Public Health. 2016;16:1028. doi: 10.1186/s12889-016-3706-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu K.T., Borders T.F. Gender, health, and physician visits among adults in the United States. Am J Public Health. 2003;93:1076–1079. doi: 10.2105/ajph.93.7.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vaidya V., Partha G., Karmakar M. Gender differences in utilization of preventive care services in the United States. J Women’s Health. 2012;21:140–145. doi: 10.1089/jwh.2011.2876. [DOI] [PubMed] [Google Scholar]
- 50.Marchildon G.P., Allin S., Merkur S. Canada: health system review. Health Syst Transit. 2020;22:1–194. [PubMed] [Google Scholar]
- 51.Charter L., Scully R., Laidlaw A. ‘The word that comes to mind is polymath’: medical students’ perceptions of rural postgraduate careers. Rural Remote Health. 2021;21:6750. doi: 10.22605/RRH6750. [DOI] [PubMed] [Google Scholar]
- 52.Wong S., Regan S. Patient perspectives on primary health care in rural communities: effects of geography on access, continuity and efficiency. Rural Remote Health. 2009;9:1–12. [PubMed] [Google Scholar]
- 53.Corscadden L., et al. Factors associated with multiple barriers to access to primary care: an international analysis. Int J Equity Health. 2018;17:1–10. doi: 10.1186/s12939-018-0740-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ghebreyesus T. 2020. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19-25 May 2020. https://www.who.int/ https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---25-may-2020. [Google Scholar]
- 55.Health Canada Licensed natural health products database (LNHPD) 2007. https://www.canada.ca/en/health-canada/services/drugs-health-products/natural-non-prescription/applications-submissions/product-licensing/licensed-natural-health-products-database.html
- 56.Morgan T., Ness D., Robinson M. Vol. 16. 2003. Students’ help-seeking behaviours by gender, racial background, and student status. [Google Scholar]
- 57.Ang R.P., Lim K.M., Tan A.-G., Yau T.Y. Effects of gender and sex role orientation on help-seeking attitudes. Curr Psychol. 2004;23:203–214. [Google Scholar]
- 58.Nova Scotia College of Pharmacists . Vol. 24. 2019. Standards of practice: prescribing drugs. [Google Scholar]
- 59.National Association of Pharmacy Regulatory Authorities NAPRA: National Association of Pharmacy Regulatory Authorities. 2022. https://www.napra.ca/
- 60.Nova Scotia College of Pharmacists Standards of practice: general. Pharm Pract. 2014;31 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1
Supplementary material 2