Abstract
Aims
The aim of this study was to assess the performance of these main scores in predicting prognosis in patients with heart failure (HF).
Methods and results
A total of 2008 patients who were admitted to the Fourth People's Hospital of Zigong, Sichuan, from December 2016 to June 2019 and diagnosed with HF were included in the study. We compared the prognostic predictive performance of Seattle Heart Failure Model (SHFM), Meta‐Analysis Global Group in Chronic Heart Failure (MAGGIC‐HF) risk score, Get With the Guidelines‐Heart Failure programme (GWTG‐HF), Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure (ASCEND) risk scores, the Acute Decompensated Heart Failure National Registry (ADHERE) model, Barcelona Bio‐Heart Failure (BCN‐Bio‐HF) risk calculator, and Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure (GISSI‐HF) for the endpoints. The primary endpoint was 1 year all‐cause mortality and the secondary endpoint was the incidence of 28 day readmission post‐discharge. At 1 year follow‐up, 44 (2.21%) patients with HF died. Discrimination analyses showed that all risk scores performed reasonably well in predicting 1 year mortality, with areas under the receiver operating characteristic curve (AUCs) fluctuating between 0.757 and 0.822. GISSI‐HF showed the best discrimination with the AUC of 0.822 (0.768–0.876), followed by MAGGIC‐HF, BCN‐Bio‐HF, ASCEND, SHFM, GWTG‐HF, and ADHERE with AUCs of 0.819 (0.756–0.883), 0.812 (0.758–0.865), 0.802 (0.742–0.862), 0.787 (0.725–0.849), 0.762 (0.684–0.840), and 0.757 (0.681–0.833), respectively. All risk scores were similarly predictive of 28 day emergency readmissions, with AUCs fluctuating between 0.609 and 0.680. Overestimation of mortality occurred in all scores except the ASCEND. The risk scores remained with good prognostic discrimination in patients with biventricular HF and in the subgroup of patients taking angiotensin‐converting enzyme inhibitor/angiotensin II receptor blocker.
Conclusions
Currently assessed risk scores have limited clinical utility, with fair accuracy and calibration in assessing patients' 1 year risk of death and poor accuracy in assessing patients' risk of readmission. There is a need to incorporate more patient‐level information, use more advanced technologies, and develop models for different subgroups of patients to achieve more practical, innovative, and accurate risk assessment tools.
Keywords: Heart failure, Mortality, Readmission, Risk score
Introduction
Heart failure (HF) is a global public health problem 1 and is one of the leading causes of hospitalization in older people. 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 Despite advances in treatment, patients with HF remain at high risk of death. Short‐term readmission of patients with HF often proves to be a serious condition that severely affects the patient's quality of life. 5 , 6 Accurately predicting the risk of death and the occurrence of readmission in HF patients could enhance self‐monitoring, 7 while helping physicians make better decisions. 8
Numerous predictive models for HF patients based on large clinical trials have been developed, such as Seattle Heart Failure Model (SHFM), 9 Get With the Guidelines‐Heart Failure programme (GWTG‐HF), 10 and the Acute Decompensated Heart Failure National Registry (ADHERE) model. 11 Recently, Meta‐Analysis Global Group in Chronic Heart Failure (MAGGIC‐HF) 12 score and the Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure (GISSI‐HF) 13 score, two more contemporary risk scores, have been published.
However, these scores are not routinely used in clinical practice, either because of the cumbersome process of using them or because of their poor reliability at the individual patient level. The factors affecting the prognosis of patients with HF are complex. Any changes in factors such as patient's underlying status and comorbidities, the development of new medicine and improvements in medical care, patient compliance, and mobility may significantly alter the long‐term prognosis of the patients. Most current risk scores for patients with HF assess the long‐term risk of death; however, the predictive accuracy was better than longer follow‐up in all risk scores. The course of HF is uncertain and short‐term readmissions are often accompanied by acute exacerbations of HF, indicating more severe disease and a poorer prognosis. The 90 day readmission rate and 1 year readmission rate for these patients are 10–30%. 6 , 14 Short‐term readmission of patients, particularly emergency readmission, could also be used as an indicator to assess the prognosis of patients with HF.
The aim of this study was to evaluate and compare the accuracy of seven existing risk scores for predicting individual 1 year mortality and 28 day emergency readmission in contemporary HF patients and to examine the clinical utility of these risk scores.
Methods
Study setting and population
The study population was patients admitted to the Fourth People's Hospital of Zigong, Sichuan, from December 2016 to June 2019 and diagnosed with HF. The dataset is open access at PhysioNet (https://doi.org/10.13026/8a9e‐w734). 15 Data were extracted through electronic health records (EHR). The study was reviewed by the Ethics Committee (Approval Number 2020‐010), and informed consent was waived due to the retrospective nature. This study complies with the Declaration of Helsinki. All types of HF were included in this dataset, including acute HF, chronic HF, left HF, right HF, or biventricular HF. The diagnosis of HF was according to the European Society of Cardiology (ESC) guidelines 7 :
Patients presenting with symptoms and/or signs of HF. Typical symptoms include breathlessness, orthopnoea, paroxysmal nocturnal dyspnoea, reduced exercise tolerance, fatigue, tiredness, increased time to recover after exercise, and ankle swelling. Typical signs include elevated jugular venous pressure, hepatojugular reflux, third heart sound (gallop rhythm), and laterally displaced apical impulse.
Patients with elevated BNP levels [BNP > 35 pg/mL and/or N‐terminal pro‐B‐type natriuretic peptide (NT‐proBNP) > 125 pg/mL].
Objective evidence of other cardiac functional and structural alterations underlying HF.
In case of uncertainty, a stress test or invasively measured elevated left ventricular filling pressure may be needed to confirm the diagnosis.
Data preparation
The study collected demographic information, baseline characteristics, comorbidities, laboratory tests, and medications. Demographic information for first‐time patients was entered manually into the EHR by the nurse and will be automatically extracted from previous cases for non‐first‐time patients. Laboratory tests and medication were prescribed by the doctors. Demographics are obtained from the first page of the medical records.
Baseline clinical characteristics are obtained on the first day of admission. Comorbidities included the patient's previous illnesses and the Charlson Comorbidity Index (CCI) score was obtained by calculating the sum of all comorbidities. Congestive HF was not included as a comorbidity in patients admitted for the first time with congestive HF.
Laboratory tests were obtained during the patient's hospital stay including renal function, routine blood, coagulation routine, high‐sensitivity troponin, myoglobin, BNP, biochemistry, lipids, electrolytes, and arterial blood gas analysis. Treatments such as diuretics, inotropes, and vasodilators used during hospitalization were also recorded.
As the data were extracted from the EHR, there were inevitably a small number of missing values. For variables included in the calculated risk scores, the missing data were filled in using multiple interpolation. The lack of information on aortic stenosis in the GISSI‐HF was specified as ‘none’ in view of its incidence. The medication records in this study were sketchy and did not record the use of ‘statins’, ‘allopurinol’, and ‘beta‐blockers’, which were used in SHFM, MAGGIC‐HF, and Barcelona Bio‐Heart Failure (BCN‐Bio‐HF). Instead of imputing these missing data, we created a simplified version of the SHFM, MAGGIC‐HF, and BCN‐Bio‐HF scores, which did not comprise these medication variables.
Outcomes
The primary endpoint of the study was all‐cause death within 1 year of discharge. The secondary endpoint was emergency readmission within 28 days of discharge. An emergency readmission was defined as an unplanned admission from an emergency department within 28 days of discharge from hospital for any reason, with the first admission after discharge being recorded during the follow‐up period. Patients were followed up regularly after discharge. Readmission to a non‐retrieval hospital was also recorded as readmission, and follow‐up was completed by telephone for patients unable to return to the medical facility.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and categorical variables as (n)%. Continuous data between the two groups were analysed by the Student's t‐test, compared by ANOVA test between more than two groups, and categorical variables by χ 2 test. The discrimination of each score in predicting 1 year all‐cause mortality was estimated by the receiver operating characteristic (ROC) curves. The areas under the ROC curve (AUCs) with 95% confidence interval (CI) were calculated. Sensitivity analysis was performed by validating the performance of each score in different types of HF and with or without angiotensin‐converting enzyme inhibitor/angiotensin II receptor blocker (ACEI/ARB) subgroups separately. The calibration of each score for the prediction of 1 year all‐cause mortality was assessed by calibration plot. The clinical application efficacy was evaluated by the decision curve analysis (DCA). A two‐sided P < 0.05 were considered significant. Statistical analyses were completed using Stata 15.0 (StataCorp, Texas, USA).
Results
A total of 2008 patients with HF were included in the analysis, of whom 1462 (72.81%) were over 70 years old. The number of men is 845 (42.08%), nearly half of the total, and the included patients were mostly classified as New York Heart Association (NYHA) class III. Forty‐four (2.21%) patients died during the 1 year follow‐up period; the baseline characteristics of the patients with HF and the comparison between those survival and non‐survival at 1 year follow‐up are shown in Table 1 . Compared with those survival, patients who had died at the time of scheduled follow‐up had worse cardiac status, more comorbidities, and worse renal function. The serum sodium levels in non‐survival group were lower whereas BNP levels were higher and duration of hospital stay was longer. In addition, the use of ACEI/ARB in this group was significantly lower at the time of follow‐up.
Table 1.
Baseline characteristics and comparison between survivor and non‐survivor by status at 1 year follow‐up
| Characteristics | Survivor | Non‐survivor | P |
|---|---|---|---|
| N = 1964 | N = 44 | ||
| Male, n (%) | 822 (41.9) | 23 (52.3) | 0.17 |
| Age ≥ 70 years, n (%) | 0.74 | ||
| No | 535 (27.2) | 11 (25.0) | |
| Yes | 1429 (72.8) | 33 (75.0) | |
| HF type, n (%) | 0.50 | ||
| Right HF | 51 (2.6) | 0 (0.0) | |
| Left HF | 465 (23.7) | 12 (27.3) | |
| Total HF | 1448 (73.7) | 32 (72.7) | |
| NYHA class, n (%) | <0.01 | ||
| II | 349 (17.8) | 4 (9.1) | |
| III | 1028 (52.3) | 11 (25.0) | |
| IV | 587 (29.9) | 29 (65.9) | |
| Killip, n (%) | <0.01 | ||
| 1 | 524 (26.7) | 3 (6.8) | |
| 2 | 1019 (51.9) | 10 (22.7) | |
| 3 | 376 (19.1) | 16 (36.4) | |
| 4 | 45 (2.3) | 15 (34.1) | |
| MI history, n (%) | 139 (7.1) | 4 (9.1) | 0.61 |
| CHF history, n (%) | 1833 (93.3) | 39 (88.6) | 0.22 |
| COPD, n (%) | 230 (11.7) | 3 (6.8) | 0.32 |
| Diabetes, n (%) | 456 (23.2) | 10 (22.7) | 0.94 |
| HR, beats/min | 85.2 ± 21.5 | 88.9 ± 24.2 | 0.25 |
| SBP, mmHg | 131.2 ± 24.6 | 122.5 ± 31.2 | 0.02 |
| BMI, kg/m2 | 21.9 ± 13.8 | 20.6 ± 3.0 | 0.56 |
| CCI | 1.8 ± 1.0 | 2.3 ± 1.3 | <0.01 |
| LVEF, % | 48.7 ± 11.3 | 49.5 ± 11.2 | 0.63 |
| BUN, mmol/L | 9.4 ± 5.3 | 16.9 ± 10.2 | <0.01 |
| Creatinine, μmol/L | 106.8 ± 75.3 | 196.9 ± 151.4 | <0.01 |
| Uric acid, mmol/L | 479.5 ± 166.6 | 627.4 ± 223.3 | <0.01 |
| eGFR, mL/min/1.73 m2 | 69.4 ± 36.5 | 44.0 ± 32.3 | <0.01 |
| Cystatin, mg/L | 1.8 ± 0.9 | 2.8 ± 1.5 | <0.01 |
| Hb, g/dL | 11.5 ± 2.4 | 10.7 ± 2.9 | 0.03 |
| Na, mmol/L | 138.3 ± 4.9 | 136.1 ± 6.1 | <0.01 |
| Hs‐troponin, mg/L | 0.3 ± 2.0 | 0.4 ± 0.9 | 0.65 |
| BNP, pg/mL | 1268.4 ± 1344.9 | 2021.9 ± 1589.1 | <0.01 |
| TC, mmol/L | 3.7 ± 1.1 | 3.6 ± 1.0 | 0.36 |
| Furosemide, n (%) | 1871 (95.3) | 43 (97.7) | 0.44 |
| Torasemide, n (%) | 236 (12.0) | 4 (9.1) | 0.55 |
| Hydrochlorothiazide, n (%) | 265 (13.5) | 8 (18.2) | 0.37 |
| ACEI/ARB, n (%) | 760 (38.7) | 6 (13.6) | <0.01 |
| Hospitalization time, days | 10 ± 8 | 7 ± 11 | 0.1 |
ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BMI, body mass index; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; CCI, Charlson Comorbidity Index; CHF, chronic heart failure; COPD, chronic obstructive pulmonary disease; eGFR, estimated glomerular filtration rate; Hb, haemoglobin; HF, heart failure; HR, heart rate; Hs, hypersensitivity; LVEF, left ventricular ejection fraction; MI, myocardial infarction; Na, serum sodium; NYHA, New York Heart Association; SBP, systolic blood pressure; TC, total cholesterol.
Data are presented as n (%) or mean ± SD.
There were 853 (42.48%) readmissions within 1 year, of which 140 (16.30%) were within 28 days of discharge. It was evident that all patients readmitted within 28 days were through the emergency department, indicating an acute adverse event. The comparison of clinical features between patients with and those without readmission within 28 days is shown in Supporting Information, Table S1 . Patients with emergency readmission within 28 days after discharge had a higher proportion of biventricular HF, a more severe NYHA classification, a higher prevalence of combined diabetes, a lower systolic blood pressure, and a higher rate of ACEI/ARB use than the non‐readmission group. Short‐term readmission patients had worse renal function, that is, higher plasma urea nitrogen, higher blood creatinine, and lower estimated glomerular filtration rate (eGFR), than the short‐term non‐readmission group.
The discrimination of the seven scores SHFM, MAGGIC‐HF, GWTG‐HF, ADHERE, Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure (ASCEND), BCN‐Bio‐HF, and GISSI‐HF in our study is shown in Table 2 . Of all scores, the AUC of risk scores for predicting the 1 year mortality fluctuates between 0.757 and 0.822. At the same time, the scores showed a decreasing trend in discrimination as follow‐up time increased. When assessing 1 year mortality, GISSI‐HF had the highest AUC at 0.822 (0.768–0.876). ASCEND, MAGGIC‐HF, and BCN‐Bio‐HF also had AUCs > 0.8. This was followed by GWTG‐HF and ADHERE, which had AUCs of 0.762 (0.684–0.840) and 0.757 (0.681–0.833), respectively.
Table 2.
Performance (AUC) of the different risk prediction tools for all‐cause mortality and readmission
| Cohort | 28 day mortality | 3 month mortality | 1 year mortality | 28 day readmission | 3 month readmission | 1 year readmission |
|---|---|---|---|---|---|---|
| ADHERE | 0.758 (0.671–0.845) | 0.768 (0.689–0.847) | 0.757 (0.681–0.833) | 0.609 (0.558–0.659) | 0.599 (0.570–0.628) | 0.568 (0.542–0.593) |
| GWTG‐HF | 0.767 (0.677–0.856) | 0.772 (0.691–0.854) | 0.762 (0.684–0.840) | 0.640 (0.594–0.696) | 0.608 (0.579–0.637) | 0.569 (0.543–0.594) |
| ASCEND | 0.833 (0.775–0.891) | 0.827 (0.771–0.884) | 0.802 (0.742–0.862) | 0.655 (0.609–0.701) | 0.614 (0.586–0.643) | 0.580 (0.555–0.605) |
| GISSI‐HF | 0.839 (0.781–0.896) | 0.831 (0.777–0.885) | 0.822 (0.768–0.876) | 0.661 (0.616–0.705) | 0.623 (0.594–0.651) | 0.598 (0.573–0.622) |
| SHFM | 0.794 (0.724–0.864) | 0.790 (0.725–0.856) | 0.787 (0.725–0.849) | 0.680 (0.637–0.723) | 0.636 (0.608–0.663) | 0.608 (0.583–0.633) |
| MAGGIC‐HF | 0.850 (0.786–0.915) | 0.836 (0.774–0.897) | 0.819 (0.756–0.883) | 0.660 (0.616–0.705) | 0.623 (0.595–0.651) | 0.602 (0.577–0.627) |
| BCN‐Bio‐HF | 0.838 (0.785–0.891) | 0.828 (0.777–0.879) | 0.812 (0.758–0.865) | 0.680 (0.636–0.724) | 0.620 (0.593–0.648) | 0.598 (0.573–0.623) |
ADHERE, the Acute Decompensated Heart Failure National Registry model; ASCEND, Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure risk scores; AUC, area under the receiver operating characteristic curve; BCN‐Bio‐HF, Barcelona Bio‐Heart Failure risk calculator; GISSI‐HF, Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure; GWTG‐HF, Get With the Guidelines‐Heart Failure programme; MAGGIC‐HF, Meta‐Analysis Global Group in Chronic Heart Failure risk score; SHFM, Seattle Heart Failure Model.
The seven scores did not perform as well in predicting patient readmission, with the AUCs not exceeding 0.7 even for predicting short‐term readmission. The AUC for 28 day emergency readmission fluctuates between 0.609 and 0.680, as shown in Table 2 . SHFM performed the best overall in predicting readmission, with AUCs of 0.680 (0.637–0.723), 0.636 (0.608–0.663), and 0.608 (0.583–0.633) for predicting 28 day, 3 month, and 1 year readmission, respectively. In contrast, ADHERE performed the worst overall in predicting the risk of readmission, with AUC of 0.609 (0.558–0.659) for predicting 28 day readmission.
Figure 1 shows the calibration for the 1 year expected and actual observed mortality calculated by each risk score. In this study, the calibration of all scores was fair (P > 0.05). The ADHERE and GWTG‐HF scores were the best calibrated followed by the ASCEND score. The BCN‐Bio‐HF, GISSI‐HF, MAGGIC‐HF, and SHFM scores were less well calibrated. The calibration plot suggested some overestimation of mortality by all scores except the ASCEND. In this population, good calibration was shown in all scores in the low‐risk population, with a large gap between predicted and actual observed outcomes in the high‐risk population.
Figure 1.
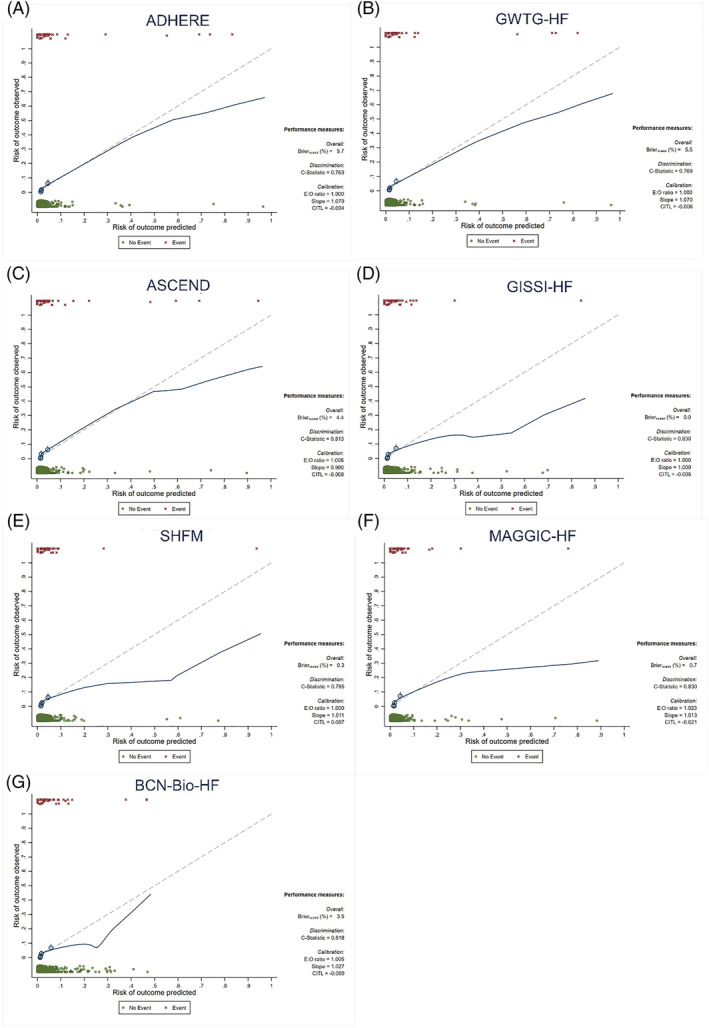
Calibration plots comparing observed vs. predicted mortality at 1 year. (A) The Acute Decompensated Heart Failure National Registry (ADHERE) model; (B) Get With the Guidelines‐Heart Failure programme (GWTG‐HF); (C) Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure (ASCEND) risk scores; (D) Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure (GISSI‐HF); (E) Seattle Heart Failure Model (SHFM); (F) Meta‐Analysis Global Group in Chronic Heart Failure (MAGGIC‐HF) risk score; (G) Barcelona Bio‐Heart Failure (BCN‐Bio‐HF) risk calculator. Y axis represents observed mortality; X axis represents expected mortality; dashed line represents best fitting curve; LOWESS smoother curve (blue line) allows assessing calibration at individual patient level; circles represent groups automatically created by the test.
The DCA in Figure 2 shows that decision making using a well‐calibrated predictive tool can benefit whenever a risk score is used, regardless of the size of the benefit. The ADHERE score and the ASCEND displayed the greatest net benefits of the scores, with the widest benefit band, and decision thresholds between 1% and 45%. SHFM has the least net benefit and the narrowest benefit band, with benefit available only in the lower risk groups, that is, a net benefit threshold between 1% and 12%.
Figure 2.
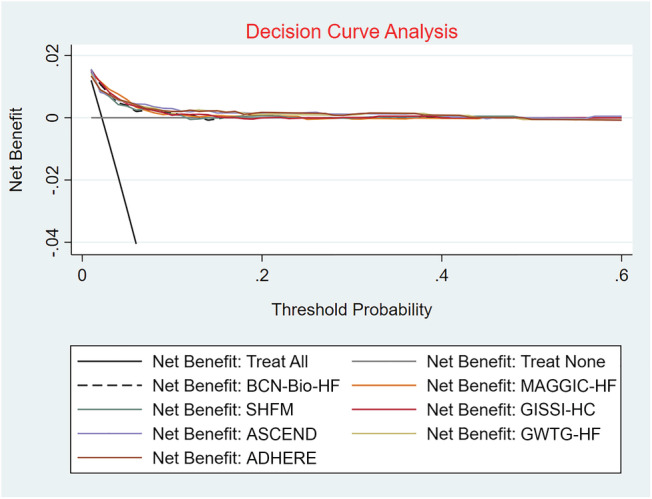
Decision curve analysis for risk scores in the validation cohort. The y‐axis measures the net benefit. The grey solid line represents the assumption that all patients are complicated with no risk. The black solid line represents the assumption that all patients are complicated with dead. The black dotted lines and other coloured lines represent the risk scores, showing that if the threshold probability of a patient is between 1% and 12%, using this prediction scores in the current study superior to the ‘intervention‐for‐none’ scheme. ADHERE, the Acute Decompensated Heart Failure National Registry model; ASCEND, Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure risk scores; BCN‐Bio‐HF, Barcelona Bio‐Heart Failure risk calculator; GISSI‐HF, Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure; GWTG‐HF, Get With the Guidelines‐Heart Failure programme; MAGGIC‐HF, Meta‐Analysis Global Group in Chronic Heart Failure risk score; SHFM, Seattle Heart Failure Model.
In this study, biventricular HF accounted for the majority of the population. The comparison of clinical features and outcomes between different types of HF is shown in Supporting Information, Table S2 . There were no significant differences in cardiac function, left ventricular ejection fraction (LVEF), CCI, and length of hospital stay among the three types of HF. However, the 3 month and 1 year readmission rates were significantly higher in patients with biventricular HF than in patients with left or right HF. Table 3 shows the performance of risk scores in patients in the biventricular, left, and right HF subgroups. Consistent with the results in the total population, the performance of the risk scores in predicting 1 year mortality was better overall than 28 day readmission, regardless of the type of patients with HF. All risk scores performed well in the biventricular HF population, with AUCs of 0.829 to 0.852. However, ADHERE and GWTG‐HF performed poorly in the left HF subgroup, with AUCs of only 0.617 and 0.650, respectively. Therein, SHFM, having the highest discrimination in patients with left HF, showed improved predictive performance over the total population. When evaluating 28 day readmission, the discrimination of the risk scores in patients with biventricular HF subgroup is comparable with that in the total HF population, but the GISSI‐HF, MAGGIC‐HF, and BCN‐Bio‐HF performed significantly better in patients with left HF subgroup than the other scores. In right HF patients, it was GWTG‐HF, ASCEND, and SHFM that performed better.
Table 3.
Performance (AUC) of the different risk prediction tools for 1 year mortality and 28 day readmission in different types of heart failure
| HF type | ADHERE | GWTG‐HF | ASCEND | GISSI‐HF | SHFM | MAGGIC‐HF | BCN‐Bio‐HF |
|---|---|---|---|---|---|---|---|
| 1 year mortality | |||||||
| Biventricular HF | 0.829 (0.761–0.897) | 0.852 (0.796–0.909) | 0.834 (0.770–0.899) | 0.827 (0.752–0.901) | 0.808 (0.741–0.875) | 0.816 (0.738–0.894) | 0.822 (0.752–0.893) |
| LHF | 0.617 (0.479–0.755) | 0.650 (0.503–0.797) | 0.811 (0.693–0.928) | 0.839 (0.702–0.975) | 0.873 (0.751–0.995) | 0.821 (0.676–0.966) | 0.859 (0.727–0.991) |
| 28 day readmission | |||||||
| Biventricular HF | 0.632 (0.576–0.686) | 0.665 (0.561–0.715) | 0.670 (0.620–0.720) | 0.666 (0.617–0.716) | 0.694 (0.647–0.742) | 0.662 (0.612–0.712) | 0.690 (0.640–0.712) |
| LHF | 0.607 (0.509–0.704) | 0.648 (0.528–0.768) | 0.609 (0.480–0.739) | 0.794 (0.727–0.862) | 0.660 (0.551–0.769) | 0.801 (0.736–0.867) | 0.774 (0.699–0.848) |
| RHF | 0.796 (0.575–1) | 0.837 (0.686–0.988) | 0.857 (0.754–0.960) | 0.663 (0.503–0.824) | 0.806 (0.635–0.977) | 0.622 (0.265–0.979) | 0.602 (0.350–0.853) |
ADHERE, the Acute Decompensated Heart Failure National Registry model; ASCEND, Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure risk scores; AUC, area under the receiver operating characteristic curve; BCN‐Bio‐HF, Barcelona Bio‐Heart Failure risk calculator; GISSI‐HF, Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure; GWTG‐HF, Get With the Guidelines‐Heart Failure programme; HF, heart failure; LHF, left heart failure; MAGGIC‐HF, Meta‐Analysis Global Group in Chronic Heart Failure risk score; RHF, right heart failure; SHFM, Seattle Heart Failure Model.
The baseline characteristics and prognosis were different between patients taking or not taking ACEI/ARB, as shown in Supporting Information, Table S3 . Patients on ACEI/ARB had higher CCI and lower LVEF. Taking ACEI/ARB significantly affected mortality, both short and long terms, as well as 28 day readmissions. The predictive performance of risk scores in patients taking and not taking ACEI/ARB is shown in Table 4 . When evaluating 1 year mortality, all risk scores performed significantly better in the ACEI/ARB cohort than in the non‐ACEI/ARB cohort, with AUC fluctuations between 0.883 and 0.970. At the time of the 28 day readmission evaluation, the risk score performed comparably with the total population in the cohort taking ACEI/ARB or not.
Table 4.
Performance (AUC) of the risk scores for 1 year mortality and 28 day readmission in the population with or without ACEI/ARB
| HF type | ADHERE | GWTG‐HF | ASCEND | GISSI‐HF | SHFM | MAGGIC‐HF | BCN‐Bio‐HF |
|---|---|---|---|---|---|---|---|
| 1 year mortality | |||||||
| ACEI/ARB | 0.883 (0.753–1) | 0.894 (0.790–0.999) | 0.897 (0.772–1) | 0.950 (0.910–0.990) | 0.970 (0.940–1) | 0.925 (0.844–1) | 0.903 (0.769–1) |
| Non‐ACEI/ARB | 0.733 (0.650–0.817) | 0.746 (0.660–0.832) | 0.791 (0.732–0.850) | 0.774 (0.703–0.845) | 0.764 (0.694–0.833) | 0.776 (0.696–0.856) | 0.770 (0.702–0.838) |
| 28 day readmission | |||||||
| ACEI/ARB | 0.666 (0.571–0.760) | 0.671 (0.577–0.765) | 0.656 (0.568–0.744) | 0.723 (0.643–0.802) | 0.621 (0.640–0.802) | 0.696 (0.605–0.786) | 0.677 (0.588–0.766) |
| Non‐ACEI/ARB | 0.593 (0.535–0.651) | 0.643 (0.589–0.697) | 0.658 (0.604–0.711) | 0.629 (0.572–0.685) | 0.679 (0.631–0.728) | 0.631 (0.575–0.688) | 0.671 (0.619–0.724) |
ACEI, angiotensin‐converting enzyme inhibitor; ADHERE, the Acute Decompensated Heart Failure National Registry model; ARB, angiotensin II receptor blocker; ASCEND, Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure risk scores; AUC, area under the receiver operating characteristic curve; BCN‐Bio‐HF, Barcelona Bio‐Heart Failure risk calculator; GISSI‐HF, Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure; GWTG‐HF, Get With the Guidelines‐Heart Failure programme; MAGGIC‐HF, Meta‐Analysis Global Group in Chronic Heart Failure risk score; SHFM, Seattle Heart Failure Model.
Discussion
This study validated the performance and clinical efficacy of seven major risk scores in real‐world populations. The similarities and differences in the variables included in the seven risk scores were detailed in Table 5 . All scores performed reasonably well in terms of discrimination and calibration in predicting 1 year mortality but performed mediocrely in predicting 28 day emergency readmission. Patients benefited from the use of risk scores, although the net benefit intervals and magnitude of net benefit varied. Among the common risk scores, none outperformed the others. BCN‐Bio‐HF had the highest AUC for predicting mortality, although the calibration curves showed that it overestimated the risk of death. The ADHERE and GWTG‐HF scores were the best calibrated, but they were less accurate than the others in predicting the risk of death. With the exception of the ASCEND score, which slightly underestimated mortality, the other six scores tended to overestimate risk. Besides, ADHERE and ASCEND showed the greatest net benefits of the scores. For most risk scores, calibration at different risk levels remained imperfect, with all seven scores better calibrated in the low‐risk population for this study.
Table 5.
Main characteristics of the seven risk scores
| SHFM | MAGGIC‐HF | BCN‐Bio‐HF | ADHERE | GWTG‐HF | ASCEND | GISSI‐HF | |
|---|---|---|---|---|---|---|---|
| Participants | HF | HF | HF | ADHF | HF | ADHF | HF |
| Clinical variables | |||||||
| Age | * | * | * | * | * | * | * |
| Gender | * | * | * | * | |||
| Heart rate | * | * | |||||
| BMI | * | * | |||||
| NYHA class III–IV | * | * | * | * | |||
| SBP | * | * | * | * | * | * | |
| HF duration > 8 months | * | ||||||
| Dyspnoea at rest | * | ||||||
| Smoke | * | ||||||
| Black race | * | ||||||
| LVEF | * | * | * | * | |||
| Aortic stenosis | * | ||||||
| COPD | * | * | * | ||||
| DM | * | ||||||
| Laboratory parameters | |||||||
| BUN | * | * | * | ||||
| Uric acid | * | * | |||||
| Creatinine | * | ||||||
| eGFR | * | * | |||||
| Sodium | * | * | * | * | |||
| Haemoglobin | * | * | * | ||||
| Total cholesterol | * | ||||||
| Lymphocytes | * | ||||||
| Biomarkers | |||||||
| Hs‐cTnT | * | ||||||
| BNP/NT‐proBNP | * | ||||||
| ST2 | * | ||||||
| Treatments | |||||||
| ACEI/ARB | * | * | * | ||||
| Beta‐blocker | * | * | |||||
| Furosemide | * | * | |||||
| Statin | * | * | |||||
| Allopurinol | * | ||||||
| Endpoint | 1, 2, and 3 year mortality | 3 year mortality | 1, 2, and 3 year mortality | In‐hospital mortality | In‐hospital mortality | Adverse events | 2 and 4 year mortality |
ACEI, angiotensin‐converting enzyme inhibitor; ADHERE, the Acute Decompensated Heart Failure National Registry model; ADHF, acute decompensated heart failure; ARB, angiotensin II receptor blocker; ASCEND, Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure risk scores; BCN‐Bio‐HF, Barcelona Bio‐Heart Failure risk calculator; BMI, body mass index; BUN, blood urea nitrogen; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate calculated with the Modification of Diet in Renal Disease equation; GISSI‐HF, Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure; GWTG‐HF, Get With the Guidelines‐Heart Failure programme; HF, heart failure; Hs‐cTnT, high‐sensitivity circulating troponin T; LVEF, left ventricular ejection fraction; MAGGIC‐HF, Meta‐Analysis Global Group in Chronic Heart Failure risk score; NT‐proBNP, N‐terminal pro‐brain natriuretic peptide; NYHA, New York Heart Association; SBP, systolic blood pressure; SHFM, Seattle Heart Failure Model; ST2, high‐sensitivity soluble ST2.
Adverse events indicate (i) 30 day mortality/HF rehospitalization, (ii) 30 day mortality/all‐cause rehospitalization, (iii) 30 day all‐cause mortality, and (iv) 180 day all‐cause mortality.
*indicates variable included in each model.
A number of risk scores have been created for risk stratification of HF patients, but in clinical practice, these scores are not fully used. The following problems exist in studies relating to the prognostic risk assessment of patients with HF. Firstly, the extant classical risk scores were established long ago and there are differences in treatment protocols between the populations modelled and current clinical patients. 9 , 10 , 11 , 12 , 13 For example, no patients used beta‐blockers in the SHFM score and only 34% of patients used beta‐blockers in the MAGGIC‐HF score. 9 , 12 In recent years, several studies have been conducted to externally validate the performance of these scores, but patients included in most of these studies were from 10 years ago, so it is still unknown whether these validation results are consistent with that in contemporary populations. 16 , 17 , 18 Secondly, the factors that influence the prognosis of patients with HF are complex and varied. Comorbidities on admission, the variable standard of care, and the post‐discharge treatment all affect the patient's short‐ and long‐term prognosis. Factors that necessarily affect the patient's prognosis like laboratory tests and comorbidities at admission were included in most risk scores. 19 , 20
Nevertheless, with the development and application of new medicine such as recombinant human brain natriuretic peptide and levosimendan, and the interpretation and implementation of the guidelines by medical institutions at all levels, 21 the survival time and length of hospital stay for HF patients have improved significantly. 22 , 23 , 24 So the applicability of these scores to patients at different levels of medical care remains to be verified given the vast size of China and the wide variation in medical standards in different regions. Finally, for the patients themselves, any change in their personal compliance, mobility, and post‐discharge retreatment may significantly alter their prognosis. A recent retrospective cohort study showed that patient non‐adherence to recommended post‐acute care was associated with an increased risk of readmission in patients with chronic HF, and this risk was not significantly increased in the less active population. 25
Due to the diversity and unpredictability of the prognostic factors of HF, the accuracy of most risk scores in predicting patient prognosis gradually decreases with the increase of follow‐up time. Most existing studies have verified the long‐term prognosis of these risk scores, whereas previous studies have found that patients with HF have a higher risk of adverse outcomes in the early post‐discharge period, 6 so predicting short‐term adverse events may have more practical value. Furthermore, the pathophysiology and characteristics of left and right HF are different; sensitivity analyses are classified according to the type of HF for a more accurate comparison. Because ACEI/ARB significantly alleviates left ventricular remodelling and affects prognosis in patients with HF, it is necessary to compare the performance of risk scores in patients taking or not taking ACEI/ARB.
Based on the above background, this study included an updated population (December 2016 to June 2019) representative of the contemporary population to externally validate the predictive performance of seven risk scores in predicting the risk of death and short‐term emergency readmission in contemporary Chinese HF patients and to examine the clinical utility of these risk scores. This study found that the first readmission of patients within 28 days of discharge was all through emergency, indicating that patients who were readmitted within a short period of time were often accompanied by relatively severe acute adverse events, which predicted more severe illness and a worse prognosis. Therefore, short‐term emergency readmission was selected as one of the endpoint events evaluated in this study. In the subgroup analysis based on type of HF, we found that all scores performed well in biventricular HF patients. However, ADHERE and GWTG‐HF performed poorly in the left HF subgroup when evaluating 1 year mortality and SHFM had the best overall discrimination in left HF patients. When evaluating 28 day readmission, the GISSI‐HF, MAGGIC‐HF, and BCN‐Bio‐HF performed significantly better in left HF patients and GWTG‐HF, ASCEND, and SHFM performed better in right HF patients. The findings of the comparative analysis based on whether patients take ACEI/ARB or not were surprising, with high AUCs (0.883–0.970) for all scores in the cohort taking ACEI/ARB. All risk scores performed significantly better in the ACEI/ARB cohort than in the non‐ACEI/ARB cohort in 1 year mortality.
The data of this study were from SCIENTIFIC DATA and were uploaded by Zhang et al. This is an example of Chinese people using artificial intelligence to extract electronic medical records and share data, in line with the spirit of scientific research and the spirit of the Internet. The current existing risk scores for HF patients only contain laboratory tests and baseline information. Including more dimension factors like patients' physical function (strength, balance, mobility, and endurance), state of consciousness, and medically derived information such as rehabilitation interventions, especially for the elderly, may allow for a more accurate assessment of patient prognosis. 26 , 27 , 28 , 29 , 30 , 31 As data sharing continues to evolve, it will become easier to conduct clinical studies with larger populations and samples everywhere, and big data will be necessary to update and frequently calibrate online calculators to improve the accuracy of patient prognosis.
There are some limitations in this study. First, our study population consisted of general HF patients from single‐centre tertiary hospitals, the vast majority of patients originated from cardiology departments, and patients were mostly NYHA class III–IV, and the results may not be generalizable to global HF population. In the right HF subgroup analysis, validation of 1 year mortality could not be performed due to the small number of patients. Second, multiple interpolations were used for missing data and missing data in the GISSI‐HF score, SHFM, MAGGIC‐HF, and BCN‐Bio‐HF were filled in with common sense or simplified; although the final scores showed good discrimination and calibration, the possibility of bias due to missing variables cannot be ruled out. Finally, this study showed that the scores were more accurate and better calibrated for predicting patient death in the low‐risk population, possibly due to the heavier HF class in our population compared with the population for which the previous scores were established.
Conclusions
In this study, seven risk scores were externally validated. The current risk scores were moderately accurate and calibrated for predicting patients' 1 year risk of death and less accurate for assessing patients' risk of readmission. No particular score was overpowering in this population and most scores tended to overestimate risk, and each performed better in low‐risk HF patients. The risk scores remained with good prognostic discrimination in patients with biventricular HF and in the subgroup of patients taking ACEI/ARB. There is a need to incorporate more patient‐level information and to use more advanced technology to obtain a practical, innovative, and accurate risk assessment tool for different risk groups.
Conflict of interest
There were no conflicts of interest.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81770231 and No. 81270203), the Natural Science Foundation of Jiangsu Province (No. BK20161436), Jiangsu Province Key Medical Research Project (No. K2019006), Jiangsu Provincial Key Medical Discipline (No. ZDXKA2016023), and Jiangsu Provincial Key Research and Development Program (No. BE2016785).
Supporting information
Table S1. Baseline characteristics and comparison between 28‐day non‐readmission and readmission patients.
Table S2. Baseline characteristics and comparison between different types of HF.
Table S3. Baseline characteristics and comparison between the taking and non‐taking ACEI/ARB population.
Acknowledgements
We would like to thank Medical Big Data and Artificial Intelligence Laboratory of Zigong Fourth People's Hospital. We would also like to thank Professor Zhongheng Zhang for providing clinical data for this study.
Bo, X. , Zhang, Y. , Liu, Y. , Kharbuja, N. , and Chen, L. (2023) Performance of the heart failure risk scores in predicting 1 year mortality and short‐term readmission of patients. ESC Heart Failure, 10: 502–517. 10.1002/ehf2.14208.
Xiangwei Bo and Yahao Zhang contributed equally.
References
- 1. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner L, Wang NY, Tsao CW, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021; 143: e254–e743. [DOI] [PubMed] [Google Scholar]
- 2. Lombardi C, Peveri G, Cani D, Latta F, Bonelli A, Tomasoni D, Sbolli M, Ravera A, Carubelli V, Saccani N, Specchia C, Metra M. In‐hospital and long‐term mortality for acute heart failure: analysis at the time of admission to the emergency department. ESC Heart Fail. 2020; 7: 2650–2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ye SD, Wang SJ, Wang GG, Li L, huang ZW, Qin J, Li CS, Yu XZ, Shen H, Yang LP, Fu Y, Zheng YA, Zhao B, Yu DM, Qin FJ, Zhou DG, Li Y, Liu FJ. Association between anemia and outcome in patients hospitalized for acute heart failure syndromes: findings from Beijing Acute Heart Failure Registry (Beijing AHF Registry). Intern Emerg Med. 2021; 16: 183–192. [DOI] [PubMed] [Google Scholar]
- 4. Al‐Jarallah M, Rajan R, Al‐Zakwani I, Dashti R, Bulbanat B, Sulaiman K, Alsheikh‐Ali AA, Panduranga P, AlHabib KF, Al Suwaidi J, Al‐Mahmeed W, Al Faleh H, Elasfar A, Al‐Motarreb A, Ridha M, Bazargani N, Asaad N, Amin H. Incidence and impact of cardiorenal anaemia syndrome on all‐cause mortality in acute heart failure patients stratified by left ventricular ejection fraction in the Middle East. ESC Heart Fail. 2019; 6: 103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Straube BM, McGann PE, Rapp MT. Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009; 361: 311 author reply 2. [PubMed] [Google Scholar]
- 6. Greene SJ, Fonarow GC, Vaduganathan M, Khan SS, Butler J, Gheorghiade M. The vulnerable phase after hospitalization for heart failure. Nat Rev Cardiol. 2015; 12: 220–229. [DOI] [PubMed] [Google Scholar]
- 7. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group . 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 8. Seferovic PM, Ponikowski P, Anker SD, Bauersachs J, Chioncel O, Cleland JGF, Boer RA, Drexel H, Ben Gal T, Hill L, Jaarsma T, Jankowska EA, Anker MS, Lainscak M, Lewis BS, McDonagh T, Metra M, Milicic D, Mullens W, Piepoli MF, Rosano G, Ruschitzka F, Volterrani M, Voors AA, Filippatos G, Coats AJS. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019; 21: 1169–1186. [DOI] [PubMed] [Google Scholar]
- 9. Levy WC, Mozaffarian D, Linker DT, Sutradhar SC, Anker SD, Cropp AB, Anand I, Maggioni A, Burton P, Sullivan MD, Pitt B, Poole‐Wilson PA, Mann DL, Packer M. The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation. 2006; 113: 1424–1433. [DOI] [PubMed] [Google Scholar]
- 10. Peterson PN, Rumsfeld JS, Liang L, Albert NM, Hernandez AF, Peterson ED, Fonarow GC, Masoudi FA, American Heart Association Get With the Guidelines‐Heart Failure Program . A validated risk score for in‐hospital mortality in patients with heart failure from the American Heart Association get with the guidelines program. Circ Cardiovasc Qual Outcomes. 2010; 3: 25–32. [DOI] [PubMed] [Google Scholar]
- 11. Fonarow GC, Adams KF Jr, Abraham WT, Yancy CW, Boscardin WJ, ADHERE Scientific Advisory Committee, Study Group, and Investigator . Risk stratification for in‐hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005; 293: 572–580. [DOI] [PubMed] [Google Scholar]
- 12. Pocock SJ, Ariti CA, McMurray JJ, Maggioni A, Køber L, Squire IB, Swedberg K, Dobson J, Poppe KK, Whalley GA, Doughty RN, Meta‐Analysis Global Group in Chronic Heart Failure . Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Eur Heart J. 2013; 34: 1404–1413. [DOI] [PubMed] [Google Scholar]
- 13. Barlera S, Tavazzi L, Franzosi MG, Marchioli R, Raimondi E, Masson S, Urso R, Lucci D, Nicolosi GL, Maggioni AP, Tognoni G, GISSI‐HF Investigators . Predictors of mortality in 6975 patients with chronic heart failure in the Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico‐Heart Failure trial: proposal for a nomogram. Circ Heart Fail. 2013; 6: 31–39. [DOI] [PubMed] [Google Scholar]
- 14. Bateman RM, Sharpe MD, Jagger JE, Ellis CG, Solé‐Violán J, López‐Rodríguez M, Herrera‐Ramos E, Ruíz‐Hernández J, Borderías L, Horcajada J, González‐Quevedo N, Rajas O, Briones M, Rodríguez de Castro F, Rodríguez Gallego C, Esen F, Orhun G, Ergin Ozcan P, Senturk E, Ugur Yilmaz C, Orhan N, Arican N, Kaya M, Kucukerden M, Giris M, Akcan U, Bilgic Gazioglu S, Tuzun E, Riff R, Naamani O, Douvdevani A, Takegawa R, Yoshida H, Hirose T, Yamamoto N, Hagiya H, Ojima M, Akeda Y, Tasaki O, Tomono K, Shimazu T, Ono S, Kubo T, Suda S, Ueno T, Ikeda T, Hirose T, Ogura H, Takahashi H, Ojima M, Kang J, Nakamura Y, Kojima T, Shimazu T, Ikeda T, Suda S, Izutani Y, Ueno T, Ono S, Taniguchi T, Dinter C, Lotz J, Eilers B, Wissmann C, Lott R, Meili MM, Schuetz PS, Hawa H, Sharshir M, Aburageila M, Salahuddin N, Chantziara V, Georgiou S, Tsimogianni A, Alexandropoulos P, Vassi A, Lagiou F, Valta M, Micha G, Chinou E, Michaloudis G, Kodaira A, Ikeda T, Ono S, Ueno T, Suda S, Izutani Y, Imaizumi H, De la Torre‐Prados MV, Garcia‐De la Torre A, Enguix‐Armada A, Puerto‐Morlan A, Perez‐Valero V, Garcia‐Alcantara A, Bolton N, Dudziak J, Bonney S, Tridente A, Nee P, Nicolaes G, Wiewel M, Schultz M, Wildhagen K, Horn J, Schrijver R, Van der Poll T, Reutelingsperger C, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Gayat EG, Struck J, Cariou A, Deye N, Guidet B, Jabert S, Launay J, Legrand M, Léone M, Resche‐Rigon M, Vicaut E, Vieillard‐Baron A, Mebazaa A, Arnold R, Capan M, Linder A, Akesson P, Popescu M, Tomescu D, Sprung CL, Calderon Morales R, Munteanu G, Orenbuch‐Harroch E, Levin P, Kasdan H, Reiter A, Volker T, Himmel Y, Cohen Y, Meissonnier J, Girard L, Rebeaud F, Herrmann I, Delwarde B, Peronnet E, Cerrato E, Venet F, Lepape A, Rimmelé T, Monneret G, Textoris J, Beloborodova N, Moroz V, Osipov A, Bedova A, Sarshor Y, Pautova A, Sergeev A, Chernevskaya E, Odermatt J, Bolliger R, Hersberger L, Ottiger M, Christ‐Crain M, Mueller B, Schuetz P, Sharma NK, Tashima AK, Brunialti MK, Machado FR, Assuncao M, Rigato O, Salomao R, Cajander SC, Rasmussen G, Tina E, Söderquist B, Källman J, Strålin K, Lange AL, Sundén‐Cullberg JS, Magnuson AM, Hultgren OH, Davies G, Pillai S, Mills G, Aubrey R, Morris K, Williams P, Evans P, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Pillai S, Davies G, Mills G, Aubrey R, Morris K, Williams P, Evans P, Van der Geest P, Mohseni M, Linssen J, De Jonge R, Duran S, Groeneveld J, Miller R III, Lopansri BK, McHugh LC, Seldon A, Burke JP, Johnston J, Reece‐Anthony R, Bond A, Molokhia A, Mcgrath C, Nsutebu E, Bank Pedersen P, Pilsgaard Henriksen D, Mikkelsen S, Touborg Lassen A, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Wiewel MA, Harmon MB, Van Vught LA, Scicluna BP, Hoogendijk AJ, Horn J, Zwinderman AH, Cremer OL, Bonten MJ, Schultz MJ, Van der Poll T, Juffermans NP, Wiersinga WJ, Eren G, Tekdos Y, Dogan M, Acicbe O, Kaya E, Hergunsel O, Alsolamy S, Ghamdi G, Alswaidan L, Alharbi S, Alenezi F, Arabi Y, Heaton J, Boyce A, Nolan L, Johnston J, Dukoff‐Gordon A, Dean A, Molokhia A, Mann Ben Yehudah T, Fleischmann C, Thomas‐Rueddel D, Haas C, Dennler U, Reinhart K, Suntornlohanakul O, Khwannimit B, Breckenridge F, Puxty A, Szturz P, Folwarzcny P, Svancara J, Kula R, Sevcik P, Caneva L, Casazza A, Bellazzi E, Marra S, Pagani L, Vetere M, Vanzino R, Ciprandi D, Preda R, Boschi R, Carnevale L, Lopez V, Aguilar Arzapalo M, Barradas L, Escalante A, Gongora J, Cetina M, Adamik B, Jakubczyk D, Kübler A, Radford A, Lee T, Singer J, Boyd J, Fineberg D, Williams M, Russell J, Scarlatescu E, Tomescu D, Droc G, Arama S, Müller M, Straat M, Zeerleder SS, Juffermans NP, Fuchs CF, Scheer CS, Wauschkuhn SW, Vollmer MV, Meissner KM, Kuhn SK, Hahnenkamp KH, Rehberg SR, Gründling MG, Yamamoto N, Ojima M, Hamaguchi S, Hirose T, Akeda Y, Takegawa R, Tasaki O, Shimazu T, Tomono K, Gómez‐Sánchez E, Heredia‐Rodríguez M, Álvarez‐Fuente E, Lorenzo‐López M, Gómez‐Pesquera E, Aragón‐Camino M, Liu‐Zhu P, Sánchez‐López A, Hernández‐Lozano A, Peláez‐Jareño MT, Tamayo E, Thomas‐Rüddel DO, Fleischmann C, Haas C, Dennler U, Reinhart K, Adora V, Kar A, Chakraborty A, Roy S, Bandyopadhyay A, Das M, Mann Ben Yehudah T, BenYehudah G, Salim M, Kumar N, Arabi L, Burger T, Lephart P, Toth‐martin E, Valencia C, Hammami N, Blot S, Vincent JL, Lambert ML, Brunke J, Riemann T, Roschke I, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Nimitvilai S, Jintanapramote K, Jarupongprapa S, Adukauskiene D, Valanciene D, Bose G, Lostarakos V, Carr B, Khedher S, Maaoui A, Ezzamouri A, Salem M, Chen J, Cranendonk DR, Van Vught LA, Wiewel MA, Cremer OL, Horn J, Bonten MJ, Schultz MJ, Van der Poll T, Wiersinga WJ, Day M, Penrice G, Roy K, Robertson P, Godbole G, Jones B, Booth M, Donaldson L, Kawano Y, Ishikura H, Al‐Dorzi H, Almutairi M, Alhamadi B, Crizaldo Toledo A, Khan R, Al Raiy B, Arabi Y, Talaie H, Van Oers JA, Harts A, Nieuwkoop E, Vos P, Boussarsar Y, Boutouta F, Kamoun S, Mezghani I, Koubaji S, Ben Souissi A, Riahi A, Mebazaa MS, Giamarellos‐Bourboulis E, Tziolos N, Routsi C, Katsenos C, Tsangaris I, Pneumatikos I, Vlachogiannis G, Theodorou V, Prekates A, Antypa E, Koulouras V, Kapravelos N, Gogos C, Antoniadou E, Mandragos K, Armaganidis A, Robles Caballero AR, Civantos B, Figueira JC, López J, Silva‐Pinto A, Ceia F, Sarmento A, Santos L, Almekhlafi G, Sakr Y, Al‐Dorzi H, Khan R, Baharoon S, Aldawood A, Matroud A, Alchin J, Al Johani S, Balkhy H, Arabi Y, Alsolamy S, Yousif SY, Alotabi BO, Alsaawi AS, Ang J, Curran MD, Enoch D, Navapurkar V, Morris A, Sharvill R, Astin J, Heredia‐Rodríguez M, Gómez‐Sánchez E, Peláez‐Jareño MT, Gómez‐Pesquera E, Lorenzo‐López M, Liu‐Zhu P, Aragón‐Camino M, Hernández‐Lozano A, Sánchez‐López A, Álvarez‐Fuente E, Tamayo E, Patel J, Kruger C, O'Neal J, Rhodes H, Jancik J, François B, Laterre PF, Eggimann P, Torres A, Sánchez M, Dequin PF, Bassi GL, Chastre J, Jafri HS, Ben Romdhane M, Douira Z, Kamoun S, Bousselmi M, Ben Souissi A, Boussarsar Y, Riahi A, Mebazaa MS, Vakalos A, Avramidis V, Craven TH, Wojcik G, Kefala K, Mccoubrey J, Reilly J, Paterson R, Inverarity D, Laurenson I, Walsh TS, Mongodi S, Bouhemad B, Orlando A, Stella A, Via G, Iotti G, Braschi A, Mojoli F, Haliloglu M, Bilgili B, Kasapoglu U, Sayan I, Süzer Aslan M, Yalcın A, Cinel I, Vakalos A, Avramidis V, Ellis HE, Bauchmuller K, Miller D, Temple A, Chastre J, François B, Torres A, Luyt CE, Sánchez M, Singer M, Jafri HS, Nassar Y, Ayad MS, Trifi A, Abdellatif S, Daly F, Nasri R, Ben Lakhal S, Bilgili B, Haliloglu M, Gul F, Cinel I, Kuzovlev A, Shabanov A, Polovnikov S, Moroz V, Kadrichu N, Dang T, Corkery K, Challoner P, Bassi GL, Aguilera E, Chiurazzi C, Travierso C, Motos A, Fernandez L, Amaro R, Senussi T, Idone F, Bobi J, Rigol M, Torres A, Hodiamont CJ, Juffermans NP, Janssen JM, Bouman CS, Mathôt RA, De Jong MD, Van Hest RM, Payne L, Fraser GL, Tudor B, Lahner M, Roth G, Krenn C, Talaie H, Jault P, Gabard J, Leclerc T, Jennes S, Que Y, Rousseau A, Ravat F, Al‐Dorzi H, Eissa A, Al‐Harbi S, Aldabbagh T, Khan R, Arabi Y, Trifi A, Abdellatif S, Daly F, Nasri R, Ben Lakhal S, Paramba F, Purayil N, Naushad V, Mohammad O, Negi V, Chandra P, Kleinsasser A, Witrz MR, Buchner‐Doeven JF, Tuip‐de Boer AM, Goslings JC, Juffermans NP, Van Hezel M, Straat M, Boing A, Van Bruggen R, Juffermans N, Markopoulou D, Venetsanou K, Kaldis V, Koutete D, Chroni D, Alamanos I, Koch L, Jancik J, Rhodes H, Walter E, Maekawa K, Hayakawa M, Kushimoto S, Shiraishi A, Kato H, Sasaki J, Ogura H, Matauoka T, Uejima T, Morimura N, Ishikura H, Hagiwara A, Takeda M, Tarabrin O, Shcherbakow S, Gavrychenko D, Mazurenko G, Ivanova V, Chystikov O, Plourde C, Lessard J, Chauny J, Daoust R, Shcherbakow S, Tarabrin O, Gavrychenko D, Mazurenko G, Chystikov O, Vakalos A, Avramidis V, Kropman L, In het Panhuis L, Konings J, Huskens D, Schurgers E, Roest M, De Laat B, Lance M, Durila M, Lukas P, Astraverkhava M, Jonas J, Budnik I, Shenkman B, Hayami H, Koide Y, Goto T, Iqbal R, Alhamdi Y, Venugopal N, Abrams S, Downey C, Toh CH, Welters ID, Bombay VB, Chauny JM, Daoust RD, Lessard JL, Marquis MM, Paquet JP, Siemens K, Sangaran D, Hunt BJ, Durward A, Nyman A, Murdoch IA, Tibby SM, Ampatzidou F, Moisidou D, Dalampini E, Nastou M, Vasilarou E, Kalaizi V, Chatzikostenoglou H, Drossos G, Spadaro S, Fogagnolo A, Fiore T, Schiavi A, Fontana V, Taccone F, Volta C, Chochliourou E, Volakli E, Violaki A, Samkinidou E, Evlavis G, Panagiotidou V, Sdougka M, Mothukuri R, Battle C, Guy K, Mills G, Evans P, Wijesuriya J, Keogh S, Docherty A, O'Donnell R, Brunskill S, Trivella M, Doree C, Holst L, Parker M, Gregersen M, Almeida J, Walsh T, Stanworth S, Moravcova S, Mansell J, Rogers A, Smith RA, Hamilton‐Davies C, Omar A, Allam M, Bilala O, Kindawi A, Ewila H, Ampatzidou F, Moisidou D, Nastou M, Dalampini E, Malamas A, Vasilarou E, Drossos G, Ferreira G, Caldas J, Fukushima J, Osawa EA, Arita E, Camara L, Zeferino S, Jardim J, Gaioto F, Dallan L, Jatene FB, Kalil Filho R, Galas F, Hajjar LA, Mitaka C, Ohnuma T, Murayama T, Kunimoto F, Nagashima M, Takei T, Tomita M, Omar A, Mahmoud K, Hanoura S, Sudarsanan S, Sivadasan P, Othamn H, Shouman Y, Singh R, Al Khulaifi A, Mandel I, Mikheev S, Suhodolo I, Kiselev V, Svirko Y, Podoksenov Y, Jenkins SA, Griffin R, Tovar Doncel MS, Lima A, Aldecoa C, Ince C, Taha A, Shafie A, Mostafa M, Syed N, Hon H, Righetti F, Colombaroli E, Castellano G, Righetti F, Colombaroli E, Hravnak M, Chen LC, Dubrawski AD, Clermont GC, Pinsky MR, Gonzalez S, Macias D, Acosta J, Jimenez P, Loza A, Lesmes A, Lucena F, Leon C, Tovar Doncel MS, Ince C, Aldecoa C, Lima A, Bastide M, Richecoeur J, Frenoy E, Lemaire C, Sauneuf B, Tamion F, Nseir S, Du Cheyron D, Dupont H, Maizel J, Shaban M, Kolko R, Salahuddin N, Sharshir M, AbuRageila M, AlHussain A, Mercado P, Maizel J, Kontar L, Titeca D, Brazier F, Riviere A, Joris M, Soupison T, De Cagny B, Slama M, Wagner J, Körner A, Kubik M, Kluge S, Reuter D, Saugel B, Colombaroli E, Righetti F, Castellano G, Tran T, De Bels D, Cudia A, Strachinaru M, Ghottignies P, Devriendt J, Pierrakos C, Martínez González Ó, Blancas R, Luján J, Ballesteros D, Martínez Díaz C, Núñez A, Martín Parra C, López Matamala B, Alonso Fernández M, Chana M, Huber W, Eckmann M, Elkmann F, Gruber A, Klein I, Schmid RM, Lahmer T, Moller PW, Sondergaard S, Jakob SM, Takala J, Berger D, Bastoni D, Aya H, Toscani L, Pigozzi L, Rhodes A, Cecconi M, Ostrowska C, Aya H, Abbas A, Mellinghoff J, Ryan C, Dawson D, Rhodes A, Cecconi M, Cronhjort M, Wall O, Nyberg E, Zeng R, Svensen C, Mårtensson J, Joelsson‐Alm E, Aguilar Arzapalo M, Barradas L, Lopez V, Cetina M, Parenti N, Palazzi C, Amidei LA, Borrelli FB, Campanale SC, Tagliazucchi FT, Sedoni GS, Lucchesi DL, Carella EC, Luciani AL, Mackovic M, Maric N, Bakula M, Aya H, Rhodes A, Grounds RM, Fletcher N, Cecconi M, Avard B, Zhang P, Mezidi M, Charbit J, Ould‐Chikh M, Deras P, Maury C, Martinez O, Capdevila X, Hou P, Linde‐Zwirble WZ, Douglas ID, Shapiro NS, Ben Souissi A, Mezghani I, Ben Aicha Y, Kamoun S, Laribi B, Jeribi B, Riahi A, Mebazaa MS, Pereira C, Marinho R, Antunes R, Marinho A, Crivits M, Raes M, Decruyenaere J, Hoste E, Bagin V, Rudnov V, Savitsky A, Astafyeva M, Korobko I, Vein V, Kampmeier T, Arnemann P, Hessler M, Wald A, Bockbreder K, Morelli A, Van Aken H, Rehberg S, Ertmer C, Arnemann P, Hessler M, Kampmeier T, Rehberg S, Van Aken H, Ince C, Ertmer C, Reddy S, Bailey M, Beasley R, Bellomo R, Mackle D, Psirides A, Young P, Reddy S, Bailey M, Beasley R, Bellomo R, Mackle D, Young P, Venkatesh H, Ramachandran S, Basu A, Nair H, Egan S, Bates J, Oliveira S, Rangel Neto NR, Reis FQ, Lee CP, Lin XL, Choong C, Eu KM, Sim WY, Tee KS, Pau J, Abisheganaden J, Maas K, De Geus H, Lafuente E, Marinho R, Moura J, Antunes R, Marinho A, Doris TE, Monkhouse D, Shipley T, Kardasz S, Gonzalez I, Stads S, Groeneveld AJ, Elsayed I, Ward N, Tridente A, Raithatha A, Steuber A, Pelletier C, Schroeder S, Michael E, Slowinski T, Kindgen‐Milles D, Ghabina S, Turani F, Belli A, Busatti S, Barettin G, Candidi F, Gargano F, Barchetta R, Falco M, Demirkiran O, Kosuk M, Bozbay S, Weber V, Hartmann J, Harm S, Linsberger I, Eichhorn T, Valicek G, Miestinger G, Hoermann C, Faenza S, Ricci D, Mancini E, Gemelli C, Cuoghi A, Magnani S, Atti M, Laddomada T, Doronzio A, Balicco B, Gruda MC, O'Sullivan P, Dan VP, Guliashvili T, Scheirer A, Golobish TD, Capponi VJ, Chan PP, Kogelmann K, Drüner M, Jarczak D, Turani F, Belli AB, Martni SM, Cotticelli VC, Mounajergi F, Barchetta R, Morimoto S, Ishikura H, Hussain I, Salahuddin N, Nadeem A, Ghorab K, Maghrabi K, Kloesel SK, Goldfuss C, Stieglitz A, Stieglitz AS, Krstevska L, Albuszies G, Aguilar Arzapalo M, Barradas L, Lopez V, Escalante A, Jimmy G, Cetina M, Izawa J, Iwami T, Uchino S, Takinami M, Kitamura T, Kawamura T, Powell‐Tuck JG, Crichton S, Raimundo M, Camporota L, Wyncoll D, Ostermann M, Hana A, De Geus HR, De Geus HR, Hana A, Aydogdu M, Boyaci N, Yuksel S, Gursel G, Cayci Sivri AB, Meza‐Márquez J, Nava‐López J, Carrillo‐Esper R, Dardashti A, Grubb A, Maizel J, Wetzstein M, Titeca D, Kontar L, Brazier F, De Cagny B, Riviere A, Soupison T, Joris M, Slama M, Peters E, Njimi H, Pickkers P, Vincent JL, Waraich M, Doyle J, Samuels T, Forni L, Desai N, Baumber R, Gunning P, Sell A, Lin S, Torrence H, O'Dwyer M, Kirwan C, Prowle J, Kim T, O'Connor ME, Hewson RW, Kirwan CJ, Pearse RM, Prowle J, Hanoura S, Omar A, Othamn H, Sudarsanan S, Allam M, Maksoud M, Singh R, Al Khulaifi A, O'Connor ME, Hewson RW, Kirwan CJ, Pearse RM, Prowle J, Uzundere O, Memis D, Ýnal M, Gultekin A, Turan N, Aydin MA, Basar H, Sencan I, Kapuagasi A, Ozturk M, Uzundurukan Z, Gokmen D, Ozcan A, Kaymak C, Artemenko VA, Budnyuk A, Pugh R, Bhandari S, Mauri T, Turrini C, Langer T, Taccone P, Volta CA, Marenghi C, Gattinoni L, Pesenti A, Sweeney L, O'Sullivan A, Kelly P, Mukeria E, MacLoughlin R, Pfeffer M, Thomas JT, Bregman GB, Karp GK, Kishinevsky EK, Stavi DS, Adi NA, Poropat T, Knafelj R, Llopart E, Batlle M, De Haro C, Mesquida J, Artigas A, Pavlovic D, Lewerentz L, Spassov A, Schneider R, De Smet S, De Raedt S, Derom E, Depuydt P, Oeyen S, Benoit D, Decruyenaere J, Gobatto A, Besen B, Tierno P, Melro L, Mendes P, Cadamuro F, Park M, Malbouisson LM, Civantos BC, Lopez JL, Robles A, Figueira J, Yus S, Garcia A, Oglinda A, Ciobanu G, Oglinda C, Schirca L, Sertinean T, Lupu V, Kelly P, O'Sullivan A, Sweeney L, MacLoughlin R, O'Sullivan A, Kelly P, Sweeney L, Mukeria E, Wolny M, MacLoughlin R, Pagano A, Numis F, Visone G, Saldamarco L, Russo T, Porta G, Paladino F, Bell C, Liu J, Debacker J, Lee C, Tamberg E, Campbell V, Mehta S, Silva‐Pinto A, Sarmento A, Santos L, Kara Ý, Yýldýrým F, Zerman A, Güllü Z, Boyacý N, Basarýk Aydogan B, Gaygýsýz Ü, Gönderen K, Arýk G, Turkoglu M, Aydogdu M, Aygencel G, Ülger Z, Gursel G, Boyacý N, Isýkdogan Z, Özdedeoglu Ö, Güllü Z, Badoglu M, Gaygýsýz U, Aydogdu M, Gursel G, Kongpolprom N, Sittipunt C, Eden A, Kokhanovsky Y, Bursztein – De Myttenaere S, Pizov R, Neilans L, MacIntyre N, Radosevich M, Wanta B, Weber V, Meyer T, Smischney N, Brown D, Diedrich D, Fuller A, McLindon P, Sim K, Shoaeir M, Noeam K, Mahrous A, Matsa R, Ali A, Dridi C, Koubaji S, Kamoun S, Haddad F, Ben Souissi A, Laribi B, Riahi A, Mebazaa MS, Pérez‐Calatayud A, Carrillo‐Esper R, Zepeda‐Mendoza A, Diaz‐Carrillo M, Arch‐Tirado E, Carbognin S, Pelacani L, Zannoni F, Agnoli A, Gagliardi G, Cho R, Adams A, Lunos S, Ambur S, Shapiro R, Prekker M, Thijssen M, Janssen L, Foudraine N, Voscopoulos CJ, Freeman J, Voscopoulos CJ, Freeman J, George E, Voscopoulos CJ, Eversole D, Freeman J, George E, Muttini S, Bigi R, Villani G, Patroniti N, Williams G, Voscopoulos CJ, Freeman J, George E, Waldmann A, Böhm S, Windisch W, Strassmann S, Karagiannidis C, Waldmann A, Böhm S, Windisch W, Strassmann S, Karagiannidis C, Karagiannidis CK, Waldmann AW, Böhm SB, Strassmann S, Windisch WW, Persson P, Lundin S, Stenqvist O, Porta G, Numis F, Serra CS, Pagano AP, Masarone MM, Rinaldi LR, Amelia AA, Fascione MF, Adinolfi LA, Ruggiero ER, Asota F, O'Rourke K, Ranjan S, Morgan P, DeBacker JW, Tamberg E, O'Neill L, Munshi L, Burry L, Fan E, Mehta S, Poo S, Mahendran K, Fowles J, Gerrard C, Vuylsteke A, Loveridge R, Chaddock C, Patel S, Kakar V, Willars C, Hurst T, Park C, Best T, Vercueil A, Auzinger G, Borgman A, Proudfoot AG, Grins E, Emiley KE, Schuitema J, Fitch SJ, Marco G, Sturgill J, Dickinson MG, Strueber M, Khaghani A, Wilton P, Jovinge SM, Sampson C, Harris‐Fox S, Cove ME, Vu LH, Sen A, Federspiel WJ, Kellum JA, Mazo Torre C, Riera J, Ramirez S, Borgatta B, Lagunes L, Rello J, Kuzovlev AK, Moroz V, Goloubev A, Polovnikov S, Nenchuk S, Karavana V, Glynos C, Asimakos A, Pappas K, Vrettou C, Magkou M, Ischaki E, Stathopoulos G, Zakynthinos S, Spadaro S, Kozhevnikova I, Dalla Corte F, Grasso S, Casolari P, Caramori G, Volta C, Andrianjafiarinoa T, Randriamandrato T, Rajaonera T, El‐Dash S, Costa ELV, Tucci MR, Leleu F, Kontar L, De Cagny B, Brazier F, Titeca D, Bacari‐Risal G, Maizel J, Amato M, Slama M, Mercado P, Maizel J, Kontar L, Titeca D, Brazier F, Riviere A, Joris M, Soupison T, De Cagny B, El Dash S, Slama M, Remmington FA, Squire S, Boichat M, Honzawa H, Yasuda H, Adati T, Suzaki S, Horibe M, Sasaki M, Sanui M, Marinho R, Daniel J, Miranda H, Marinho A, Milinis K, Cooper M, Williams GR, McCarron E, Simants S, Patanwala I, Welters I, Su Y, Fernández Villanueva J, Fernández Garda R, López Lago A, Rodríguez Ruíz E, Hernández Vaquero R, Tomé Martínez de Rituerto S, Varo Pérez E, Lefel N, Schaap F, Bergmans D, Olde Damink S, Van de Poll M, Tizard K, Lister C, Poole L, Ringaitiene D, Gineityte D, Vicka V, Norkiene I, Sipylaite J, O'Loughlin A, Maraj V, Dowling J, Velasco MB, Dalcomune DM, Dias EB, Fernandes SL, Oshima T, Graf S, Heidegger C, Genton L, Karsegard V, Dupertuis Y, Pichard C, Friedli N, Stanga Z, Mueller B, Schuetz P, Vandersteen L, Stessel B, Evers S, Van Assche A, Jamaer L, Dubois J, Marinho R, Castro H, Moura J, Valente J, Martins P, Casteloes P, Magalhaes C, Cabral S, Santos M, Oliveira B, Salgueiro A, Marinho A, Marinho R, Santos M, Lafuente E, Castro H, Cabral S, Moura J, Martins P, Oliveira B, Salgueiro A, Duarte S, Castro S, Melo M, Casteloes P, Marinho A, Gray S, Maipang K, Bhurayanontachai R, Grädel LG, Schütz P, Langlois P, Manzanares W, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Manzanares W, Langlois P, Lemieux M, Elke G, Bloos F, Reinhart K, Heyland D, Langlois P, Lemieux M, Aramendi I, Heyland D, Manzanares W, Su Y, Marinho R, Babo N, Marinho A, Hoshino M, Haraguchi Y, Kajiwara S, Mitsuhashi T, Tsubata T, Aida M, Rattanapraphat T, Bhurayanontachai R, Kongkamol C, Khwannimit B, Marinho R, Santos M, Castro H, Lafuente E, Salgueiro A, Cabral S, Martins P, Moura J, Oliveira B, Melo M, Xavier B, Valente J, Magalhaes C, Casteloes P, Marinho A, Moisidou D, Ampatzidou F, Koutsogiannidis C, Moschopoulou M, Drossos G, Taskin G, Çakir M, Güler AK, Taskin A, Öcal N, Özer S, Yamanel L, Wong JM, Fitton C, Anwar S, Stacey S, Aggou M, Fyntanidou B, Patsatzakis S, Oloktsidou E, Lolakos K, Papapostolou E, Grosomanidis V, Suda S, Ikeda T, Ono S, Ueno T, Izutani Y, Gaudry S, Desailly V, Pasquier P, Brun PB, Tesnieres AT, Ricard JD, Dreyfuss D, Mignon A, White JC, Molokhia A, Dean A, Stilwell A, Friedlaender G, Peters M, Stipulante S, Delfosse A, Donneau AF, Ghuysen A, Feldmann C, Freitag D, Dersch W, Irqsusi M, Eschbach D, Steinfeldt T, Wulf H, Wiesmann T, Kongpolprom N, Cholkraisuwat J, Beitland S, Nakstad E, Stær‐Jensen H, Drægni T, Andersen G, Jacobsen D, Brunborg C, Waldum‐Grevbo B, Sunde K, Hoyland K, Pandit D, Hayakawa K, Oloktsidou E, Kotzampassi K, Fyntanidou B, Patsatzakis S, Loukipoudi L, Doumaki E, Grosomanidis V, Yasuda H, Admiraal MM, Van Assen M, Van Putten MJ, Tjepkema‐Cloostermans M, Van Rootselaar AF, Horn J, Ragusa F, Marudi A, Baroni S, Gaspari A, Bertellini E, Taha A, Abdullah T, Abdel Monem S, Alcorn S, McNeill S, Russell S, Eertmans W, Genbrugge C, Meex I, Dens J, Jans F, De Deyne C, Cholkraisuwat J, Kongpolprom N, Avard B, Burns R, Patarchi A, Spina T, Tanaka H, Otani N, Ode S, Ishimatsu S, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Won MH, Dakova S, Ramsheva Z, Ramshev K, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Cho J, Moon JB, Park CW, Ohk TG, Shin MC, Marudi A, Baroni S, Gaspari A, Bertellini E, Orhun G, Senturk E, Ozcan PE, Sencer S, Ulusoy C, Tuzun E, Esen F, Tincu R, Cobilinschi C, Tomescu D, Ghiorghiu Z, Macovei R, Van Assen M, Admiraal MM, Van Putten MJ, Tjepkema‐Cloostermans M, Van Rootselaar AF, Horn J, Fallenius M, Skrifvars MB, Reinikainen M, Bendel S, Raj R, Abu‐Habsa M, Hymers C, Borowska A, Sivadhas H, Sahiba S, Perkins S, Rubio J, Rubio JA, Sierra R, English S, Chasse M, Turgeon A, Lauzier F, Griesdale D, Garland A, Fergusson D, Zarychanski R, Tinmouth A, Van Walraven C, Montroy K, Ziegler J, Dupont Chouinard R, Carignan R, Dhaliwal A, Lum C, Sinclair J, Pagliarello G, McIntyre L, English S, Chasse M, Turgeon A, Lauzier F, Griesdale D, Garland A, Fergusson D, Zarychanski R, Tinmouth A, Van Walraven C, Montroy K, Ziegler J, Dupont Chouinard R, Carignan R, Dhaliwal A, Lum C, Sinclair J, Pagliarello G, McIntyre L, Groza T, Moreau N, Castanares‐Zapatero D, Hantson P, Carbonara M, Ortolano F, Zoerle T, Magnoni S, Pifferi S, Conte V, Stocchetti N, Carteron L, Suys T, Patet C, Quintard H, Oddo M, Rubio JA, Rubio J, Sierra R, Spatenkova V, Pokorna E, Suchomel P, Ebert N, Jancik J, Rhodes H, Bylinski T, Hawthorne C, Shaw M, Piper I, Kinsella J, Kink AK, Rätsep IR, Boutin A, Moore L, Chasse M, Zarychanski R, Lauzier F, English S, McIntyre L, Lacroix J, Griesdale D, Lessard‐Bonaventure P, Turgeon AF, Boutin A, Moore L, Green R, Lessard‐Bonaventure P, Erdogan M, Butler M, Lauzier F, Chasse M, English S, McIntyre L, Zarychanski R, Lacroix J, Griesdale D, Desjardins P, Fergusson DA, Turgeon AF, Goncalves B, Vidal B, Valdez C, Rodrigues AC, Miguez L, Moralez G, Hong T, Kutz A, Hausfater P, Amin D, Struja T, Haubitz S, Huber A, Mueller B, Schuetz P, Brown T, Collinson J, Pritchett C, Slade T, Le Guen M, Hellings S, Ramsaran R, Alsheikhly A, Abe T, Kanapeckaite L, Abu‐Habsa M, Bahl R, Russell MQ, Real KJ, Abu‐Habsa M, Lyon RM, Oveland NP, Penketh J, Mcdonald M, Kelly F, Alfafi M, Alsolamy S, Almutairi W, Alotaibi B, Van den Berg AE, Schriel Y, Dawson L, Meynaar IA, Talaie H, Silva D, Fernandes S, Gouveia J, Santos Silva J, Foley J, Kaskovagheorgescu A, Evoy D, Cronin J, Ryan J, Huck M, Hoffmann C, Renner J, Laitselart P, Donat N, Cirodde A, Schaal JV, Masson Y, Nau A, Leclerc T, Howarth O, Davenport K, Jeanrenaud P, Raftery S, MacTavish P, Devine H, McPeake J, Daniel M, Kinsella J, Quasim T, Alrabiee S, Alrashid A, Alsolamy S, Gundogan O, Bor C, Akýn Korhan E, Demirag K, Uyar M, Frame F, Ashton C, Bergstrom Niska L, Dilokpattanamongkol P, Suansanae T, Suthisisang C, Morakul S, Karnjanarachata C, Tangsujaritvijit V, Mahmood S, Al Thani H, Almenyar A, Vakalos A, Avramidis V, Sharvill R, Penketh J, Morton SE, Chiew YS, Pretty C, Chase JG, Shaw GM, Knafelj R, Kordis P, Patel S, Grover V, Kuchyn I, Bielka K, Aidoni Z, Grosomanidis V, Kotzampassi K, Stavrou G, Fyntanidou B, Patsatzakis S, Skourtis C, Lee SD, Williams K, Weltes ID, Berhane S, Arrowsmith C, Peters C, Robert S, Caldas J, Panerai RB, Robinson TG, Camara L, Ferreira G, Borg‐Seng‐Shu E, De Lima Oliveira M, Mian NC, Santos L, Nogueira R, Zeferino SP, Jacobsen Teixeira M, Galas F, Hajjar LA, Killeen P, McPhail M, Bernal W, Maggs J, Wendon J, Hughes T, Taniguchi LU, Siqueira EM, Vieira JM Jr, Azevedo LC, Ahmad AN, Abu‐Habsa M, Bahl R, Helme E, Hadfield S, Loveridge R, Shak J, Senver C, Howard‐Griffin R, Wacharasint P, Fuengfoo P, Sukcharoen N, Rangsin R, Sbiti‐Rohr D, Schuetz P, Na H, Song S, Lee S, Jeong E, Lee K, Cooper M, Milinis K, Williams G, McCarron E, Simants S, Patanwala I, Welters ID, Zoumpelouli E, Volakli EA, Chrysohoidou V, Georgiou S, Charisopoulou K, Kotzapanagiotou E, Panagiotidou V, Manavidou K, Stathi Z, Sdougka M, Salahuddin NS, AlGhamdi B, Marashly Q, Zaza K, Sharshir M, Khurshid M, Ali Z, Malgapo M, Jamil M, Shafquat A, Shoukri M, Hijazi M, Abe T, Uchino S, Takinami M, Rangel Neto NR, Oliveira S, Reis FQ, Rocha FA, Moralez G, Ebecken K, Rabello LS, Lima MF, Hatum R, De Marco FV, Alves A, Pinto JE, Godoy M, Brasil PE, Bozza FA, Salluh JI, Soares M, Krinsley J, Kang G, Perry J, Hines H, Wilkinson KM, Tordoff C, Sloan B, Bellamy MC, Moreira E, Verga F, Barbato M, Burghi G, Soares M, Silva UV, Azevedo LC, Torelly AP, Kahn JM, Angus DC, Knibel MF, Brasil PE, Bozza FA, Salluh JI, Velasco MB, Dalcomune DM, Marshall R, Gilpin T, Tridente A, Raithatha A, Mota D, Loureiro B, Dias J, Afonso O, Coelho F, Martins A, Faria F, Al‐Dorzi H, Al Orainni H, AlEid F, Tlaygeh H, Itani A, Hejazi A, Arabi Y, Gaudry S, Messika J, Ricard JD, Guillo S, Pasquet B, Dubief E, Dreyfuss D, Tubach F, Battle C, James K, Temblett P, Davies L, Battle C, Lynch C, Pereira S, Cavaco S, Fernandes J, Moreira I, Almeida E, Seabra Pereira F, Malheiro M, Cardoso F, Aragão I, Cardoso T, Fister M, Knafelj R, Muraray Govind P, Brahmananda Reddy N, Pratheema R, Arul ED, Devachandran J, Velasco MB, Dalcomune DM, Knafelj R, Fister M, Chin‐Yee N, D'Egidio G, Thavorn K, Heyland D, Kyeremanteng K, Murchison AG, Swalwell K, Mandeville J, Stott D, Guerreiro I, Devine H, MacTavish P, McPeake J, Quasim T, Kinsella J, Daniel M, Goossens C, Marques MB, Derde S, Vander Perre S, Dufour T, Thiessen SE, Güiza F, Janssens T, Hermans G, Vanhorebeek I, De Bock K, Van den Berghe G, Langouche L, Devine H, MacTavish P, Quasim T, Kinsella J, Daniel M, McPeake J, Miles B, Madden S, Devine H, Weiler M, Marques P, Rodrigues C, Boeira M, Brenner K, Leães C, Machado A, Townsend R, Andrade J, MacTavish P, McPeake J, Devine H, Kinsella J, Daniel M, Kishore R, Fenlon C, Quasim T, Fiks T, Ruijter A, Te Raa M, Spronk P, Chiew YS, Docherty P, Dickson J, Moltchanova E, Scarrot C, Pretty C, Shaw GM, Chase JG, Hall T, Ngu WC, Jack JM, Morgan P, Avard B, Pavli A, Gee X, Bor C, Akin Korhan E, Demirag K, Uyar M, Shirazy M, Fayed A, Gupta S, Kaushal A, Dewan S, Varma A, Ghosh E, Yang L, Eshelman L, Lord B, Carlson E, Helme E, Broderick R, Hadfield S, Loveridge R, Ramos J, Forte D, Yang F, Hou P, Dudziak J, Feeney J, Wilkinson K, Bauchmuller K, Shuker K, Faulds M, Raithatha A, Bryden D, England L, Bolton N, Tridente A, Bauchmuller K, Shuker K, Tridente A, Faulds M, Matheson A, Gaynor J, Bryden D, S South Yorkshire Hospitals Research Collaboration , Ramos J, Peroni B, Daglius‐Dias R, Miranda L, Cohen C, Carvalho C, Velasco I, Forte D, Kelly JM, Neill A, Rubenfeld G, Masson N, Min A, Boezeman E, Hofhuis J, Hovingh A, De Vries R, Spronk P, Cabral‐Campello G, Aragão I, Cardoso T, Van Mol M, Nijkamp M, Kompanje E, Ostrowski P, Omar A, Kiss K, Köves B, Csernus V, Molnár Z, Hoydonckx Y, Vanwing S, Stessel B, Van Assche A, Jamaer L, Dubois J, Medo V, Galvez R, Miranda JP, Stone C, Wigmore T, Arunan Y, Wheeler A, Bauchmuller K, Bryden D, Wong Y, Poi C, Gu C, Molmy P, Van Grunderbeeck N, Nigeon O, Lemyze M, Thevenin D, Mallat J, Ramos J, Correa M, Carvalho RT, Forte D, Fernandez A, McBride C, Koonthalloor E, Walsh C, Webber A, Ashe M, Smith K, Jeanrenaud P, Marudi A, Baroni S, Ragusa F, Bertellini E, Volakli EA, Chochliourou E, Dimitriadou M, Violaki A, Mantzafleri P, Samkinidou E, Vrani O, Arbouti A, Varsami T, Sdougka M, Bollen JA, Van Smaalen TC, De Jongh WC, Ten Hoopen MM, Ysebaert D, Van Heurn LW, Van Mook WN, Sim K, Fuller A, Roze des Ordons A, Couillard P, Doig C, Van Keer RV, Deschepper RD, Francke AF, Huyghens LH, Bilsen JB, Nyamaizi B, Dalrymple C, Molokhia A, Dobru A, Marrinan E, Ankuli A, Molokhia A, McPeake J, Struthers R, Crawford R, Devine H, Mactavish P, Quasim T, Morelli P, Degiovanangelo M, Lemos F, Martinez V, Verga F, Cabrera J, Burghi G, Rutten A, Van Ieperen S, De Geer S, Van Vugt M, Der Kinderen E, Giannini A, Miccinesi G, Marchesi T, Prandi E. 36th International Symposium on Intensive Care and Emergency Medicine: Brussels, Belgium. 15–18 March 2016. Crit Care. 2016; 20: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhang Z, Cao L, Chen R, Zhao Y, Lv L, Xu Z, Xu P. Electronic healthcare records and external outcome data for hospitalized patients with heart failure. Sci Data. 2021; 8: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Canepa M, Fonseca C, Chioncel O, Laroche C, Crespo‐Leiro MG, Coats AJS, Mebazaa A, Piepoli MF, Tavazzi L, Maggioni AP, Crespo‐Leiro M, Anker S, Mebazaa A, Coats A, Filippatos G, Ferrari R, Maggioni AP, Piepoli MF, Amir O, Chioncel O, Dahlström U, Delgado Jimenez JF, Drozdz J, Erglis A, Fazlibegovic E, Fonseca C, Fruhwald F, Gatzov P, Goncalvesova E, Hassanein M, Hradec J, Kavoliuniene A, Lainscak M, Logeart D, Merkely B, Metra M, Otljanska M, Seferovic PM, Srbinovska Kostovska E, Temizhan A, Tousoulis D, Ferreira T, Andarala M, Fiorucci E, Folkesson Lefrancq E, Glémot M, Gracia G, Konte M, Laroche C, McNeill PA, Missiamenou V, Taylor C, Auer J, Ablasser K, Fruhwald F, Dolze T, Brandner K, Gstrein S, Poelzl G, Moertl D, Reiter S, Podczeck‐Schweighofer A, Muslibegovic A, Vasilj M, Fazlibegovic E, Cesko M, Zelenika D, Palic B, Pravdic D, Cuk D, Vitlianova K, Katova T, Velikov T, Kurteva T, Gatzov P, Kamenova D, Antova M, Sirakova V, Krejci J, Mikolaskova M, Spinar J, Krupicka J, Malek F, Hegarova M, Lazarova M, Monhart Z, Hassanein M, Sobhy M, el Messiry F, el Shazly AH, Elrakshy Y, Youssef A, Moneim AA, Noamany M, Reda A, Abdel Dayem TK, Farag N, Ibrahim Halawa S, Abdel Hamid M, Said K, Saleh A, Ebeid H, Hanna R, Aziz R, Louis O, Enen MA, Ibrahim BS, Nasr G, Elbahry A, Sobhy H, Ashmawy M, Gouda M, Aboleineen W, Bernard Y, Luporsi P, Meneveau N, Pillot M, Morel M, Seronde MF, Schiele F, Briand F, Delahaye F, Damy T, Eicher JC, de Groote P, Fertin M, Lamblin N, Isnard R, Lefol C, Thevenin S, Hagege A, Jondeau G, Logeart D, le Marcis V, Ly JF, Coisne D, Lequeux B, le Moal V, Mascle S, Lotton P, Behar N, Donal E, Thebault C, Ridard C, Reynaud A, Basquin A, Bauer F, Codjia R, Galinier M, Tourikis P, Stavroula M, Tousoulis D, Stefanadis C, Chrysohoou C, Kotrogiannis I, Matzaraki V, Dimitroula T, Karavidas A, Tsitsinakis G, Kapelios C, Nanas J, Kampouri H, Nana E, Kaldara E, Eugenidou A, Vardas P, Saloustros I, Patrianakos A, Tsaknakis T, Evangelou S, Nikoloulis N, Tziourganou H, Tsaroucha A, Papadopoulou A, Douras A, Polgar L, Merkely B, Kosztin A, Nyolczas N, Csaba Nagy A, Halmosi R, Elber J, Alony I, Shotan A, Vazan Fuhrmann A, Amir O, Romano S, Marcon S, Penco M, di Mauro M, Lemme E, Carubelli V, Rovetta R, Metra M, Bulgari M, Quinzani F, Lombardi C, Bosi S, Schiavina G, Squeri A, Barbieri A, di Tano G, Pirelli S, Ferrari R, Fucili A, Passero T, Musio S, di Biase M, Correale M, Salvemini G, Brognoli S, Zanelli E, Giordano A, Agostoni P, Italiano G, Salvioni E, Copelli S, Modena MG, Reggianini L, Valenti C, Olaru A, Bandino S, Deidda M, Mercuro G, Cadeddu Dessalvi C, Marino PN, di Ruocco MV, Sartori C, Piccinino C, Parrinello G, Licata G, Torres D, Giambanco S, Busalacchi S, Arrotti S, Novo S, Inciardi RM, Pieri P, Chirco PR, Ausilia Galifi M, Teresi G, Buccheri D, Minacapelli A, Veniani M, Frisinghelli A, Priori SG, Cattaneo S, Opasich C, Gualco A, Pagliaro M, Mancone M, Fedele F, Cinque A, Vellini M, Scarfo I, Romeo F, Ferraiuolo F, Sergi D, Anselmi M, Melandri F, Leci E, Iori E, Bovolo V, Pidello S, Frea S, Bergerone S, Botta M, Canavosio FG, Gaita F, Merlo M, Cinquetti M, Sinagra G, Ramani F, Fabris E, Stolfo D, Artico J, Miani D, Fresco C, Daneluzzi C, Proclemer A, Cicoira M, Zanolla L, Marchese G, Torelli F, Vassanelli C, Voronina N, Erglis A, Tamakauskas V, Smalinskas V, Karaliute R, Petraskiene I, Kazakauskaite E, Rumbinaite E, Kavoliuniene A, Vysniauskas V, Brazyte‐Ramanauskiene R, Petraskiene D, Stankala S, Switala P, Juszczyk Z, Sinkiewicz W, Gilewski W, Pietrzak J, Orzel T, Kasztelowicz P, Kardaszewicz P, Lazorko‐Piega M, Gabryel J, Mosakowska K, Bellwon J, Rynkiewicz A, Raczak G, Lewicka E, Dabrowska‐Kugacka A, Bartkowiak R, Sosnowska‐Pasiarska B, Wozakowska‐Kaplon B, Krzeminski A, Zabojszcz M, Mirek‐Bryniarska E, Grzegorzko A, Bury K, Nessler J, Zalewski J, Furman A, Broncel M, Poliwczak A, Bala A, Zycinski P, Rudzinska M, Jankowski L, Kasprzak JD, Michalak L, Wojtczak Soska K, Drozdz J, Huziuk I, Retwinski A, Flis P, Weglarz J, Bodys A, Grajek S, Kaluzna‐Oleksy M, Straburzynska‐Migaj E, Dankowski R, Szymanowska K, Grabia J, Szyszka A, Nowicka A, Samcik M, Wolniewicz L, Baczynska K, Komorowska K, Poprawa I, Komorowska E, Sajnaga D, Zolbach A, Dudzik‐Plocica A, Abdulkarim AF, Lauko‐Rachocka A, Kaminski L, Kostka A, Cichy A, Ruszkowski P, Splawski M, Fitas G, Szymczyk A, Serwicka A, Fiega A, Zysko D, Krysiak W, Szabowski S, Skorek E, Pruszczyk P, Bienias P, Ciurzynski M, Welnicki M, Mamcarz A, Folga A, Zielinski T, Rywik T, Leszek P, Sobieszczanska‐Malek M, Piotrowska M, Kozar‐Kaminska K, Komuda K, Wisniewska J, Tarnowska A, Balsam P, Marchel M, Opolski G, Kaplon‐Cieslicka A, Gil RJ, Mozenska O, Byczkowska K, Gil K, Pawlak A, Michalek A, Krzesinski P, Piotrowicz K, Uzieblo‐Zyczkowska B, Stanczyk A, Skrobowski A, Ponikowski P, Jankowska E, Rozentryt P, Polonski L, Gadula‐Gacek E, Nowalany‐Kozielska E, Kuczaj A, Kalarus Z, Szulik M, Przybylska K, Klys J, Prokop‐Lewicka G, Kleinrok A, Tavares Aguiar C, Ventosa A, Pereira S, Faria R, Chin J, de Jesus I, Santos R, Silva P, Moreno N, Queirós C, Lourenço C, Pereira A, Castro A, Andrade A, Oliveira Guimaraes T, Martins S, Placido R, Lima G, Brito D, Francisco AR, Cardiga R, Proenca M, Araujo I, Marques F, Fonseca C, Moura B, Leite S, Campelo M, Silva‐Cardoso J, Rodrigues J, Rangel I, Martins E, Sofia Correia A, Peres M, Marta L, Ferreira da Silva G, Severino D, Durao D, Leao S, Magalhaes P, Moreira I, Filipa Cordeiro A, Ferreira C, Araujo C, Ferreira A, Baptista A, Radoi M, Bicescu G, Vinereanu D, Sinescu CJ, Macarie C, Popescu R, Daha I, Dan GA, Stanescu C, Dan A, Craiu E, Nechita E, Aursulesei V, Christodorescu R, Otasevic P, Seferovic PM, Simeunovic D, Ristic AD, Celic V, Pavlovic‐Kleut M, Suzic Lazic J, Stojcevski B, Pencic B, Stevanovic A, Andric A, Iric‐Cupic V, Jovic M, Davidovic G, Milanov S, Mitic V, Atanaskovic V, Antic S, Pavlovic M, Stanojevic D, Stoickov V, Ilic S, Deljanin Ilic M, Petrovic D, Stojsic S, Kecojevic S, Dodic S, Cemerlic Adic N, Cankovic M, Stojiljkovic J, Mihajlovic B, Radin A, Radovanovic S, Krotin M, Klabnik A, Goncalvesova E, Pernicky M, Murin J, Kovar F, Kmec J, Semjanova H, Strasek M, Savnik Iskra M, Ravnikar T, Cernic Suligoj N, Komel J, Fras Z, Jug B, Glavic T, Losic R, Bombek M, Krajnc I, Krunic B, Horvat S, Kovac D, Rajtman D, Cencic V, Letonja M, Winkler R, Valentincic M, Melihen‐Bartolic C, Bartolic A, Pusnik Vrckovnik M, Kladnik M, Slemenik Pusnik C, Marolt A, Klen J, Drnovsek B, Leskovar B, Fernandez Anguita MJ, Gallego Page JC, Salmeron Martinez FM, Andres J, Genis AB, Mirabet S, Mendez A, Garcia‐Cosio L, Roig E, Leon V, Gonzalez‐Costello J, Muntane G, Garay A, Alcade‐Martinez V, Lopez Fernandez S, Rivera‐Lopez R, Puga‐Martinez M, Fernandez‐Alvarez M, Serrano‐Martinez JL, Crespo‐Leiro M, Grille‐Cancela Z, Marzoa‐Rivas R, Blanco‐Canosa P, Paniagua‐Martin MJ, Barge‐Caballero E, Laynez Cerdena I, Famara Hernandez Baldomero I, Lara Padron A, Ofelia Rosillo S, Dalmau Gonzalez‐Gallarza R, Salvador Montanes O, Iniesta Manjavacas AM, Castro Conde A, Araujo A, Soria T, Garcia‐Pavia P, Gomez‐Bueno M, Cobo‐Marcos M, Alonso‐Pulpon L, Segovia Cubero J, Sayago I, Gonzalez‐Segovia A, Briceno A, Escribano Subias P, Vicente Hernandez M, Ruiz Cano MJ, Gomez Sanchez MA, Delgado Jimenez JF, Barrios Garrido‐Lestache E, Garcia Pinilla JM, Garcia de la Villa B, Sahuquillo A, Bravo Marques R, Torres Calvo F, Perez‐Martinez MT, Gracia‐Rodenas MR, Garrido‐Bravo IP, Pastor‐Perez F, Pascual‐Figal DA, Diaz Molina B, Orus J, Epelde Gonzalo F, Bertomeu V, Valero R, Martinez‐Abellan R, Quiles J, Rodrigez‐Ortega JA, Mateo I, ElAmrani A, Fernandez‐Vivancos C, Bierge Valero D, Almenar‐Bonet L, Sanchez‐Lazaro IJ, Marques‐Sule E, Facila‐Rubio L, Perez‐Silvestre J, Garcia‐Gonzalez P, Ridocci‐Soriano F, Garcia‐Escriva D, Pellicer‐Cabo A, de la Fuente Galan L, Lopez Diaz J, Recio Platero A, Arias JC, Blasco‐Peiro T, Sanz Julve M, Sanchez‐Insa E, Aured‐Guallar C, Portoles‐Ocampo A, Melin M, Hägglund E, Stenberg A, Lindahl IM, Asserlund B, Olsson L, Dahlström U, Afzelius M, Karlström P, Tengvall L, Wiklund PA, Olsson B, Kalayci S, Temizhan A, Cavusoglu Y, Gencer E, Yilmaz MB, Gunes H. Performance of prognostic risk scores in chronic heart failure patients enrolled in the European Society of Cardiology Heart Failure Long‐Term Registry. JACC Heart Fail. 2018; 6: 452–462. [DOI] [PubMed] [Google Scholar]
- 17. Win S, Hussain I, Hebl VB, Dunlay SM, Redfield MM. Inpatient mortality risk scores and postdischarge events in hospitalized heart failure patients: a community‐based study. Circ Heart Fail. 2017; 10: e003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Agostoni P, Paolillo S, Mapelli M, Gentile P, Salvioni E, Veglia F, Bonomi A, Corrà U, Lagioia R, Limongelli G, Sinagra G, Cattadori G, Scardovi AB, Metra M, Carubelli V, Scrutinio D, Raimondo R, Emdin M, Piepoli M, Magrì D, Parati G, Caravita S, Re F, Cicoira M, Minà C, Correale M, Frigerio M, Bussotti M, Oliva F, Battaia E, Belardinelli R, Mezzani A, Pastormerlo L, Guazzi M, Badagliacca R, di Lenarda A, Passino C, Sciomer S, Zambon E, Pacileo G, Ricci R, Apostolo A, Palermo P, Contini M, Clemenza F, Marchese G, Gargiulo P, Binno S, Lombardi C, Passantino A, Filardi PP. Multiparametric prognostic scores in chronic heart failure with reduced ejection fraction: a long‐term comparison. Eur J Heart Fail. 2018; 20: 700–710. [DOI] [PubMed] [Google Scholar]
- 19. Bergsten TM, Nicholson A, Donnino R, Wang B, Fang Y, Natarajan S. Predicting adults likely to develop heart failure using readily available clinical information: an analysis of heart failure incidence using the NHEFS. Prev Med. 2020; 130: 105878. [DOI] [PubMed] [Google Scholar]
- 20. Thibodeau JT, Drazner MH. The role of the clinical examination in patients with heart failure. JACC Heart Fail. 2018; 6: 543–551. [DOI] [PubMed] [Google Scholar]
- 21. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo‐Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A, ESC Scientific Document Group , de Boer RA, Christian Schulze P, Abdelhamid M, Aboyans V, Adamopoulos S, Anker SD, Arbelo E, Asteggiano R, Bauersachs J, Bayes‐Genis A, Borger MA, Budts W, Cikes M, Damman K, Delgado V, Dendale P, Dilaveris P, Drexel H, Ezekowitz J, Falk V, Fauchier L, Filippatos G, Fraser A, Frey N, Gale CP, Gustafsson F, Harris J, Iung B, Janssens S, Jessup M, Konradi A, Kotecha D, Lambrinou E, Lancellotti P, Landmesser U, Leclercq C, Lewis BS, Leyva F, Linhart A, Løchen ML, Lund LH, Mancini D, Masip J, Milicic D, Mueller C, Nef H, Nielsen JC, Neubeck L, Noutsias M, Petersen SE, Sonia Petronio A, Ponikowski P, Prescott E, Rakisheva A, Richter DJ, Schlyakhto E, Seferovic P, Senni M, Sitges M, Sousa‐Uva M, Tocchetti CG, Touyz RM, Tschoepe C, Waltenberger J, Adamo M, Baumbach A, Böhm M, Burri H, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo‐Leiro MG, Farmakis D, Gardner RS, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Piepoli MF, Price S, Rosano GMC, Ruschitzka F, Skibelund AK. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 42: 3599–3726. [DOI] [PubMed] [Google Scholar]
- 22. Richards AM, Lainchbury JG, Troughton RW, Espiner EA, Nicholls MG. Clinical applications of B‐type natriuretic peptides. Trends Endocrinol Metab. 2004; 15: 170–174. [DOI] [PubMed] [Google Scholar]
- 23. Comín‐Colet J, Manito N, Segovia‐Cubero J, Delgado J, García Pinilla JM, Almenar L, Crespo‐Leiro MG, Sionis A, Blasco T, Pascual‐Figal D, Gonzalez‐Vilchez F, Lambert‐Rodríguez JL, Grau M, Bruguera J, on behalf of the LION‐HEART Study Investigators . Efficacy and safety of intermittent intravenous outpatient administration of levosimendan in patients with advanced heart failure: the LION‐HEART multicentre randomised trial. Eur J Heart Fail. 2018; 20: 1128–1136. [DOI] [PubMed] [Google Scholar]
- 24. Papp Z, Agostoni P, Alvarez J, Bettex D, Bouchez S, Brito D, Černý V, Comin‐Colet J, Crespo‐Leiro MG, Delgado JF, Édes I, Eremenko AA, Farmakis D, Fedele F, Fonseca C, Fruhwald S, Girardis M, Guarracino F, Harjola VP, Heringlake M, Herpain A, Heunks LMA, Husebye T, Ivancan V, Karason K, Kaul S, Kivikko M, Kubica J, Masip J, Matskeplishvili S, Mebazaa A, Nieminen MS, Oliva F, Papp JG, Parissis J, Parkhomenko A, Põder P, Pölzl G, Reinecke A, Ricksten SE, Riha H, Rudiger A, Sarapohja T, Schwinger RHG, Toller W, Tritapepe L, Tschöpe C, Wikström G, Lewinski DV, Vrtovec B, Pollesello P. Levosimendan efficacy and safety: 20 years of SIMDAX in clinical use. J Cardiovasc Pharmacol. 2020; 76: 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chou A, Euloth T, Matcho B, Pastva AM, Bilderback A, Freburger JK. Is discordance between recommended and actual postacute discharge setting a risk factor for readmission in patients with congestive heart failure? J Am Heart Assoc. 2021; 10: e020425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lee DS, Stitt A, Austin PC, Stukel TA, Schull MJ, Chong A, Newton GE, Lee JS, Tu JV. Prediction of heart failure mortality in emergent care: a cohort study. Ann Intern Med. 2012; 156: 767–775 w‐261, w‐2. [DOI] [PubMed] [Google Scholar]
- 27. Fleming LM, Gavin M, Piatkowski G, Chang JD, Mukamal KJ. Derivation and validation of a 30‐day heart failure readmission model. Am J Cardiol. 2014; 114: 1379–1382. [DOI] [PubMed] [Google Scholar]
- 28. Dodson JA, Hajduk AM, Murphy TE, Geda M, Krumholz HM, Tsang S, Nanna MG, Tinetti ME, Goldstein D, Forman DE, Alexander KP, Gill TM, Chaudhry SI. Thirty‐day readmission risk model for older adults hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2019; 12: e005320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Voors AA, Ouwerkerk W, Zannad F, van Veldhuisen DJ, Samani NJ, Ponikowski P, Ng LL, Metra M, ter Maaten JM, Lang CC, Hillege HL, van der Harst P, Filippatos G, Dickstein K, Cleland JG, Anker SD, Zwinderman AH. Development and validation of multivariable models to predict mortality and hospitalization in patients with heart failure. Eur J Heart Fail. 2017; 19: 627–634. [DOI] [PubMed] [Google Scholar]
- 30. Yang M, Tao L, An H, Liu G, Tu Q, Zhang H, Qin L, Xiao Z, Wang Y, Fan J, Feng D, Liang Y, Ren J. A novel nomogram to predict all‐cause readmission or death risk in Chinese elderly patients with heart failure. ESC Heart Fail. 2020; 7: 1015–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kitzman DW, Whellan DJ, Duncan P, Pastva AM, Mentz RJ, Reeves GR, Nelson MB, Chen H, Upadhya B, Reed SD, Espeland MA, Hewston LA, O'Connor CM. Physical rehabilitation for older patients hospitalized for heart failure. N Engl J Med. 2021; 385: 203–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Baseline characteristics and comparison between 28‐day non‐readmission and readmission patients.
Table S2. Baseline characteristics and comparison between different types of HF.
Table S3. Baseline characteristics and comparison between the taking and non‐taking ACEI/ARB population.


