Abstract
Background
Prenatal mental health is a neglected public health issue that places pregnant women at a higher risk for mental disorders. The purpose of this study was to investigate the influencing factors of prenatal mental disorders and provide a scientific basis to guide and promote the mental health of pregnant women.
Methods
The study sample comprised 973 women in their first pregnancy, who were in their second trimester and third trimester, who underwent obstetric outpatient checkups at the Maternal and Child Health Hospital in Huai'an, who were recruited in the survey that was conducted from July to December 2017. The Chinese mental health scale (CMHS) was used to assess the mental health of pregnant women. The present study uses the chi-square test to compare the rates of class with different demographic variables, a latent class analysis to identify psychological symptoms, and multiple logistic regression analysis to examine whether the demographics predicted class membership.
Results
The chi-square test results showed that participants who reported feeling different in the perinatal period (χ2 = 6.35, P = 0.04), having marital satisfaction (χ2 = 15.8, P < 0.001), with an in-law relationship (χ2 = 29.43, P < 0.001), with a friend relationship (χ2 = 24.81, P < 0.001), with basic diseases (χ2 = 8.04, P = 0.02), and taking birth control pills (χ2 = 8.97, P = 0.01) have different probabilities of being classified. Three latent classes were identified: the high symptoms group (6.89%), the moderate symptoms group (20.56%), and the low symptoms group (72.56%). Pregnant women in the third trimester [odds ratio (OR) = 1.83, 95% confidence interval (CI): 1.04–3.25, P = 0.04], with a poor in-law relationship (OR = 2.82, 95% CI:1.45–5.51, P = 0.002), with a bad friend relationship (OR = 3.17, 95% CI: 1.31–7.71, P = 0.01), and who had basic diseases (OR = 1.70, 95% CI: 1.00–2.90, P = 0.04) tended to be classified under the high symptoms group than under the low symptoms group. Pregnant women with a bad friend relationship (OR = 2.15, 95% CI: 1.08–4.28, P = 0.03) and taking birth control pills (OR = 1.51, 95% CI: 1.08–2.11, P = 0.02) were more likely to be placed under the moderate symptoms group than under the low symptoms group.
Conclusions
A pregnant woman's mental health status factors include feeling different in the perinatal period, those with marital satisfaction, those with an in-law relationship, those with a friend relationship, those with basic diseases, and those taking birth control pills. To ensure a smooth progress of pregnancy and promote the physical and mental health of pregnant women, psychological screening and psychological intervention measures should be strengthened.
Keywords: pregnant women, mental health, latent class analysis, China, psychological symptoms
Introduction
People's material living standards and education level have gradually improved; however, the fertility rate does not seem to be optimistic in both developing countries and the least developed countries (1, 2). In this case, the health of pregnant women deserves more attention. However, about 9%−19% of pregnant women suffer from antenatal negative emotion (3), which affects their health.
In recent years, with the improvement in and popularization of medical treatment, the public's viewpoint on pregnant women has changed from purely physical health to more psychological health (4). Both living environment and social situations contribute to anxiety and depression during pregnancy (5). Gestation of life requires the mother to constantly adjust the internal environment for the embryo (6), including rising body weight and dramatically changing hormone and metabolic levels (7–9). Foremost among these, the perinatal status is a susceptible period with a high incidence of antenatal depression, which is related to maternal mortality, in particular suicide (10).
Unlike postnatal depression as a common cognitive in public, prenatal psychological problems seem to be ignored, which serve as an important cause of postnatal depressive symptoms (11). The harm inflicted by psychological problems is inestimable. It will not only make pregnant women lose control of their emotions, as under the influence of bad emotions, the suicidal tendency of pregnant women will increase (12); it will also affect their physical health as women experiencing depression or anxiety are more likely to suffer from gestational hypertension in pregnancy compared to their non-depressed or non-anxious counterparts (13). Recent evidence proved that, when a pregnant woman is exposed to depression, the development of the fetus can be affected (14), the offspring could suffer from infantile autism due to neurodevelopmental disorder (15, 16), and the children could experience worse socioemotional outcomes at the age of 6–7 years (17). For a family, it will undoubtedly cause huge financial losses apart from the spiritual burden.
There are many opinions about what can trigger prenatal psychological adversity, for example, whether hormone fluctuations during the perinatal periods lead to changes in inflammatory factors that increase the risk of depression (18). The state and personal behavior of pregnant women can also contribute to depression, such as the presence of anxiety and diseases (9, 19); smoking (20) and excessive consumption of alcohol (21); and the education level and work status (housewife/unemployment (2)). In addition, social support plays an important role (22), especially when the pregnant woman receives inadequate support from the husband (domestic violence (23)) or friends and lives in a disturbed family environment (24); the choice of induction of labor (25); etc.
While the factors responsible for prenatal mental disorders are complex, it is also recognized that pregnant women at risk of prenatal mental disorder are heterogeneous. Through observed and measurable behavior, the latent mental health of pregnant women can be indirectly measured in studies on their mental health. In previous studies, the standard for classifying the mental health of pregnant women was based on the sum of the scores of self-assessment scales (26, 27). The categorization standard was too straightforward to discriminate between group traits. The application of latent class analysis (28) (LCA) can solve this problem and classify the potential characteristics of a population based on the score probability of each item. Latent class analysis (28) (LCA) is an analytical method for locating homogeneous groups (classes) of people. Despite the fact that class membership is unknown, it can be inferred from response patterns to a set of categorical variables.
Due to the traditional thought of a feudal society, prenatal mental disorders have been less focused by the Chinese family. The purpose of this study was to use the LCA method to investigate the influencing factors of prenatal mental disorders to explore the variation from perinatal pregnant women in different groups and to provide a scientific basis for reducing prenatal mental disorders.
Materials and methods
Participants and procedures
In the present study, the participants were pregnant women in their first pregnancy, who were in the second trimester and third trimester, who underwent obstetric outpatient checkups at the Maternal and Child Health Hospital in Huai'an.
The inclusion criteria were as follows: Pregnant women who underwent antenatal checkups at our hospital and were interested in taking part in this study. The exclusion criteria were as follows: (1) women who were suffering from psychiatric and other psychotic disorders; (2) women who were experiencing serious physical diseases; (3) women who could not cooperate with the investigation owing to education level or other reasons; and (4) women who were refusing to participate.
Finally, a total of 1,000 participants were interviewed by the questionnaire from July to December 2017. After excluding individuals with missing data for key variables, 973 participants were used for analysis (response rate: 97.3%). Ethical approval for this study was obtained from the Medical Ethics Committee of Xuzhou Medical University and the Maternal and Child Health Hospital in Huai'an. The procedures used in this study adhere to the tenets of the Declaration of Helsinki. All participants gave their written informed consent before their inclusion in the present study.
Measures
The questionnaire included sociodemographic information such as age (≤ 25/26–34/≥35), education (high school or less/universities and colleges/undergraduate/postgraduate), being an only child (Yes/No), residence (urban/rural), monthly household income (< 3,000/3,000–5,000/5,001–7,000/>7,000 RMB), perinatal period (second trimester/third trimester), number of marriages (one marriage/two marriages and above), marital satisfaction (satisfied/dissatisfied), conjugal relation (good/bad), husband and wife status (equality/inequality), in-law relationship (good/bad), friend relationship (good/bad), basic diseases (Yes/No), and taking birth control pills (Yes/No).
The Chinese mental health scale (29) (CMHS) is one of the most extensively used tools for mental health screening. The CMHS consists of 10 subscales: (1) interpersonal tension; (2) poor psychological endurance; (3) poor adaptability; (4) psychological imbalance; (5) emotional disorder; (6) anxiety; (7) depression; (8) hostility; (9) stubbornly biased; and (10) somatization. Each subscale consists of eight items. On a 5-point Likert scale, the participants rate items from 1 (not at all) to 5 (nearly every day). The problem severity of each subscale is classified as none (average score of scale < 2), mild (2–2.99), moderate (3–3.99), and severe (≥4). The sum of the scores of each of the 80 items divided by 80 is the total average score of mental health. The subscale indicates whether there are problems in 10 aspects of the mental health of the subjects, and the total average score of the CMHS evaluates the overall mental health of the subjects. The total average score ranges from 1 to 5. The severity of mental health problems is categorized as no mental health problems (average score of scale < 2), mild mental health problems (2–2.99), moderate mental health problems (3–3.99), and severe mental health problems (≥4). Cronbach's alpha for CMHS was 0.97 and Cronbach's alpha for each subscale was above 0.85 in this study.
Statistical analysis
The data was collected through the Epidata 3.1 database and analyzed in SPSS 23.0 and Mplus (Mplus Version 7.4). Data analysis consisted of three parts. First, the chi-square test was performed to compare the rate of class with different demographic variables. Afterward, a latent class analysis was applied to identify psychological symptoms.
The 10 components of the CMHS were dichotomized as present or absent (values of 1 or 0 as categorical indicator variables). Latent class analysis (LCA) is a methodological approach that helps to explain population heterogeneity within observed data through the identification of underlying subgroups of individuals, thus allowing the examination of different HRBs while dealing with a diverse nature of the population (30). Six model fit indices were used to assist in determining the best model for LCA: Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), adjusted Bayesian Information Criterion (aBIC), Lo-Mendell-Rubin (LMR), Bootstrapped Likelihood Ratio Test (BLRT), and Entropy (31). LMR and BLRT are used to make a comparison between the estimated model and a model with k-1 class, or classes, with k equaling the number of classes (32). A low and significant P-value for the LMR and BLRT indicates that the estimated model outperforms the model with one fewer class (32). The AIC, BIC, and aBIC are frequently used to compare different counterpart models, with the lowest value for each indicator indicating the best-fitting model (33).
Finally, multiple logistic regression analysis was used to examine whether the demographics predicted class membership.
Results
Latent class analysis of 10 psychological symptoms
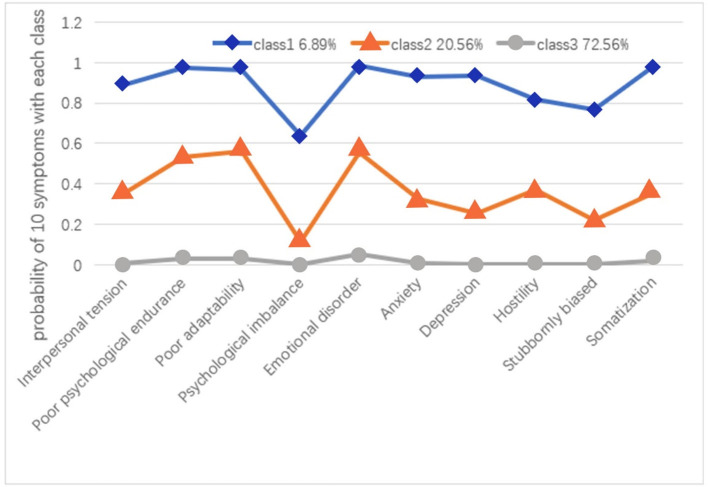
Patterns of psychological symptoms were identified by the LCA in Mplus (Mplus Version 7.4) to the five classes. The five-class and four-class models did not replicate the best LMR-LRT and BLRT values and were therefore not considered further. The three latent classes were regarded as the best model based on a series of indices (Table 1), which showed the lowest AIC, BIC, and aBIC values. Furthermore, the P-values of LMR-LRT and BLRT were statistically significant in class 3. Although, P-values of LMR-LRT and BLRT test were significant for both 2-class and 3-class models, the lower AIC, BIC, and aBIC values for the 3-class model indicated better fitness of this model in the present study. In this study, we chose the 3-class solution because it had the lowest BIC, AIC, aBIC, and LMR-LRT < 0.0001. Figure 1 shows the three identified latent classes. Latent class 1 was named as a “high symptoms group” that includes 6.89% of the subjects (n = 973). In this class, pregnant woman reported high probabilities of all 10 psychological symptoms, especially in regard to poor psychological endurance, emotional disorder, and somatization. Class 2 (moderate symptom group, 20.56% of subjects) showed high probabilities of poor psychological endurance, poor adaptability, and emotional disorder. Class 3 (72.56% of subjects) was characterized by the lowest probabilities for all 10 psychological symptoms and was therefore named the “low symptoms group.”
Table 1.
Model fit indices derived from latent class analysis on models with 1–5 classes.
| Model | k | AIC | BIC | aBIC | Entropy | LMR | BLRT | Class probability |
|---|---|---|---|---|---|---|---|---|
| 1 | 10 | 7,978.61 | 8,027.41 | 7,995.65 | ||||
| 2 | 21 | 5,513.19 | 5,615.68 | 5,548.99 | 0.95 | < 0.001 | < 0.001 | 208/765 (0.21/0.79) |
| 3 | 32 | 5,205.72 | 5,361.90 | 5,260.26 | 0.92 | < 0.001 | < 0.001 | 67/200/706 (0.07/0.20/0.73) |
| 4 | 43 | 5,186.05 | 5,395.91 | 5,259.34 | 0.89 | 0.23 | < 0.001 | 164/700/44/65 (0.17/0.72/0.05/0.07) |
| 5 | 54 | 5,173.52 | 5,437.06 | 5,265.56 | 0.90 | 0.51 | < 0.001 | 30/152/48/703/40 (0.03/0.16/0.05/0.72/0.04) |
AIC, Akaike information criterion; BIC, Bayesian information criterion; aBIC. sample size adjusted BIC; LMR, Vuong-Lo-Mendell-Rubin likelihood ratio test; BLRT, bootstrapped likelihood ratio test. The three latent classes were regarded as the best model, highlighted in bold.
Figure 1.
The three-class model and probability of 10 psychological symptoms within each class (n = 973). Class 1: the high symptoms group, Class 2: the moderate symptoms group, Class 3: the low symptoms group.
The rate of three classes with different demographic variables
The participants' demographic characteristics of the three classes are listed in Table 2, the mean age of the participants was 28.24 years. Most of them had completed at least a high school education, and 73.48% of them were not the only child to their parents. Approximately 70.00% lived in urban areas, their monthly household income was more than 7,000 RMB, accounting for 37.83%. In total, 94.35% of the sample reported one marriage and 59.20% were in the third trimester at the time of investigation. There were 790 people who were satisfied with their marriage, and most of the participants reported good relation and equal status in couples. In addition, over 80.00% of them had good in-law relationship and friend relationship, 67.63% had no basic diseases, and 64.75% of the participants did not take birth control pills.
Table 2.
Classification and comparison of three latent phenotypes of pregnant women with different demographic characteristics.
| Demographics | Total | High | Moderate | Low | χ2 | P-value |
|---|---|---|---|---|---|---|
| (n = 973) | (n = 67) | (n = 200) | (n = 706) | |||
| Age, M (SD) | 28.24 (4.88) | 28.1 (4.09) | 28.18 (4.44) | 28.3 (5.06) | 0.52 | 0.97 |
| ≤ 25 | 285 (29.29%) | 18 (26.87%) | 59 (29.50%) | 208 (29.46%) | ||
| 26–34 | 572 (58.79%) | 42 (62.69%) | 116 (58.00%) | 414 (58.64%) | ||
| ≥35 | 116 (11.92%) | 7 (10.44%) | 25 (12.50%) | 84 (11.90%) | ||
| Education | ||||||
| High school or less | 336 (34.53%) | 25 (37.31%) | 72 (36.00%) | 239 (33.85%) | 1.57 | 0.95 |
| Universities and colleges | 266 (27.34%) | 17 (25.37%) | 53 (26.50%) | 196 (27.76%) | ||
| Undergraduate | 341 (35.05%) | 24 (35.82%) | 70 (35.00%) | 247 (35.00%) | ||
| Postgraduate | 30 (3.08%) | 1 (1.50%) | 5 (2.50%) | 24 (3.39%) | ||
| Only child | ||||||
| Yes | 258 (26.52%) | 15 (22.39%) | 50 (25.00%) | 193 (27.34%) | 1.07 | 0.59 |
| No | 715 (73.48%) | 52 (77.61%) | 150 (75.00%) | 513 (72.66%) | ||
| Residence | ||||||
| Urban | 689 (70.82%) | 48 (71.64%) | 130 (65.00%) | 511 (72.38%) | 4.13 | 0.13 |
| Rural | 284 (29.18%) | 19 (28.36%) | 70 (35.00%) | 195 (27.62%) | ||
| Monthly household income (RMB) | ||||||
| < 3,000 | 80 (8.22%) | 3 (4.48%) | 22 (11.00%) | 55 (7.79%) | 8.52 | 0.20 |
| 3,000–5,000 | 282 (28.98%) | 27 (40.30%) | 52 (26.00%) | 203 (28.75%) | ||
| 5,001–7,000 | 243 (24.97%) | 15 (22.39%) | 45 (22.50%) | 183 (25.92%) | ||
| >7,000 | 368 (37.83%) | 22 (32.83%) | 81 (40.50%) | 265 (37.54%) | ||
| Number of marriages | ||||||
| One marriage | 918 (94.35%) | 65 (97.01%) | 191 (95.50%) | 662 (93.77%) | 1.84 | 0.40 |
| Two marriages and above | 55 (5.65%) | 2 (2.99%) | 9 (4.50%) | 44 (6.23%) | ||
| Perinatal period | ||||||
| Second trimester | 397 (40.80%) | 20 (29.85%) | 73 (36.50%) | 304 (43.10%) | 6.35 | 0.04 |
| Third trimester | 576 (59.20%) | 47 (70.15%) | 127 (63.50%) | 402 (56.90%) | ||
| Marriage satisfaction | ||||||
| Satisfied | 790 (81.19%) | 45 (67.16%) | 152 (76.00%) | 593 (84.00%) | 15.8 | < 0.001 |
| Dissatisfied | 183 (18.81%) | 22 (32.84%) | 48 (24.00%) | 113 (16.00%) | ||
| Conjugal relation | ||||||
| Good | 902 (92.70%) | 59 (88.10%) | 180 (90.00%) | 663 (93.91%) | 5.81 | 0.06 |
| Bad | 71 (7.30%) | 8 (11.90%) | 20 (10.00%) | 43 (6.09%) | ||
| Husband and wife status | ||||||
| Equality | 863 (88.69%) | 58 (86.57%) | 172 (86.00%) | 633 (89.66%) | 2.41 | 0.30 |
| Inequality | 110 (11.31%) | 9 (13.43%) | 28 (14.00%) | 73 (10.34%) | ||
| In-law relationship | ||||||
| Good | 816 (83.86%) | 43 (64.18%) | 157 (78.50%) | 616 (87.25%) | 29.43 | < 0.001 |
| Bad | 157 (16.14%) | 24 (35.82%) | 43 (21.50%) | 90 (12.75%) | ||
| Friend relationship | ||||||
| Good | 917 (94.24%) | 56 (83.58%) | 181 (90.50%) | 680 (96.32%) | 24.81 | < 0.001 |
| Bad | 56 (5.76%) | 11 (16.42%) | 19 (9.50%) | 26 (3.68%) | ||
| Basic diseases | ||||||
| Yes | 315 (32.37%) | 29 (43.28%) | 75 (37.50%) | 211 (29.90%) | 8.04 | 0.02 |
| No | 658 (67.63%) | 38 (56.72%) | 125 (62.50%) | 495 (70.10%) | ||
| Take birth control pills | ||||||
| Yes | 343 (35.25%) | 28 (41.79%) | 86 (43.00%) | 229 (32.44%) | 8.97 | 0.01 |
| No | 630 (64.75%) | 39 (58.21%) | 114 (57.00%) | 477 (67.56%) | ||
Bold values indicate P < 0.05.
The chi-square test results showed that participants reported differently in perinatal period, marriage satisfaction, in-law relationship, friend relationship, basic diseases, and taking birth control pills have different probabilities of being classified (all P < 0.05). No statistically significant differences of psychological symptoms were found in other variables.
Multiple logistic regression analysis
Furthermore, focusing on the different profiles of the high symptoms group, the moderate symptoms group, and the low symptoms group, we used multiple logistic regression analysis to examine whether demographics predicted class membership, after adjusting for sociodemographic characteristic (age, education, only child, residence, and monthly household income).
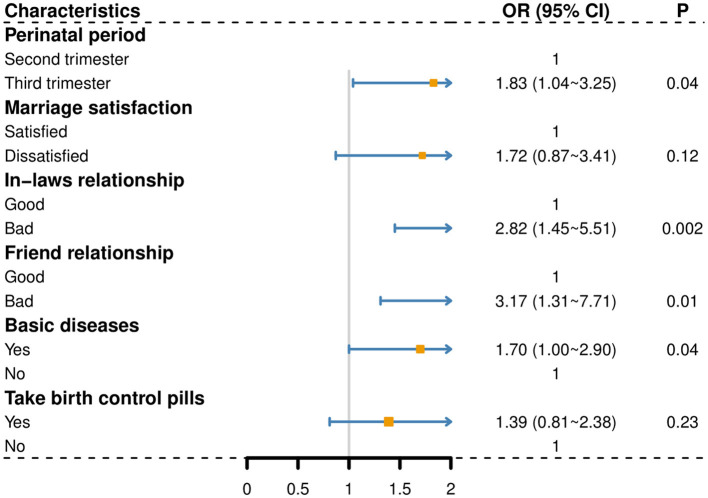
First, the high symptoms group was compared with the low symptoms group (as a reference; Figure 2). Compared with the second trimester, the third trimester was more likely to be categorized into the high symptoms group (OR = 1.83, 95% CI: 1.04–3.25, P = 0.04). Compared with good in-law relationship, pregnant women with lousy in-law relationship exhibited higher odds of belonging to the high symptoms group (OR = 2.82, 95% CI: 1.45–5.51, P = 0.002). Compared with good friend relationship, those who had bad friend relationship were more likely to be categorized into the high symptoms group (OR = 3.17, 95% CI: 1.31–7.71, P = 0.01). Compared with no basic diseases, those who had basic diseases were easier to be divided into the high symptoms group (OR = 1.70, 95% CI: 1.00–2.90, P = 0.04).
Figure 2.
The high symptoms group compared to the low symptoms group (as a reference); A P-value of < 0.05 was considered significant.
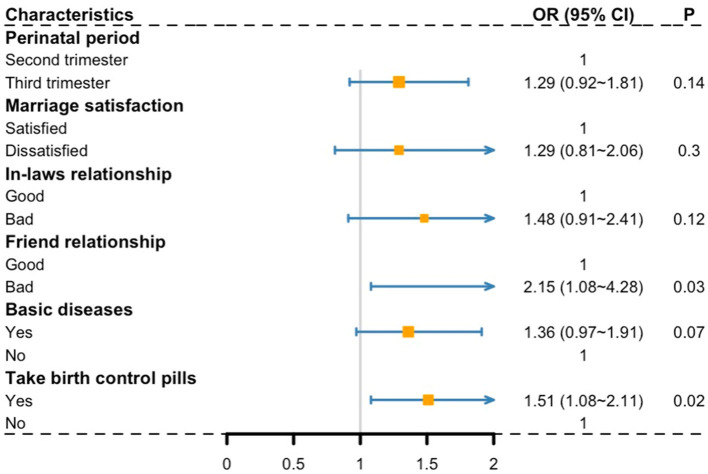
Second, the moderate symptoms group was compared with the low symptoms group (as a reference) (Figure 3), those who have a bad friend relationship (OR = 2.15, 95% CI: 1.08–4.28, P = 0.03) and take birth control pills (OR = 1.51, 95% CI: 1.08–2.11, P = 0.02) were more likely divided into the moderate symptoms group.
Figure 3.
The moderate symptoms group compared to the low symptoms group (as a reference); A P-value of < 0.05 was considered significant.
Discussion
In this study, we used the LCA to detect any causes that may result in significant heterogeneity of adverse psychological status among pregnant women. The LCA was selected over other exploratory approaches because it is model based, allows model comparisons to be statistically tested, and is appropriate for questionnaire-derived data, yet permitting differing variable measurement scales and variances (29, 34).
The findings of previous studies (35, 36) reported three or four latent classes, with one class having a low probability of psychological symptoms and the other having a high probability of psychological symptoms. The main findings of our study were as follows: (1) We identified three distinct subgroups, namely “low symptoms group,” “moderate symptoms group,” and “high symptoms group”; (2) different distributions during pregnancy were essential factors, and compared with the second trimester, participants in the third trimester were more likely to be categorized into the high symptoms group; (3) basic diseases or bad social relationships (including in-laws and friends) can also lead pregnant women to have an adverse psychological impact that leads them to be assigned to the high symptoms group; (4) the moderate symptoms group was more likely to have a bad friend relationship and take birth control pills than the low symptoms group.
Effects of different stages of pregnancy
When compared to earlier findings (37, 38), heavier psychological symptoms are likely to occur in the third trimester than in the second trimester, which are consistent with the findings of this study. The reason for this development is attributed to the possibility that pregnant women are not satisfied with their body during pregnancy (39). From the second trimester to the third trimester, body dissatisfaction of pregnant women is positively correlated with psychological symptoms (40). Pregnant women with body dissatisfaction might fear negative evaluations by others and worry about their own ability to return to their pre-pregnancy body shape, which may predispose mental disorders (41). Moreover, according to a Korean study (42), psychological problems follow a growing pattern from the first to the third trimester. A systematic review (43) showed that second- and third-trimester cortisol assessments reported a connection, and elevated cortisol concentrations were observed in expected recovery periods. The higher the estradiol level in the third trimester, the greater the possibility of mental disorders. Therefore, medical institutions should take the screening of maternal mental health problems as a part of routine prenatal care (44). During each prenatal examination, they should ask about the emotional status of pregnant women and understand their psychosocial risk factors. It is important to provide standardized prenatal emotional management training for pregnant women (45). Noteworthy is that pregnant women in the third trimester are the potential population of postpartum depression (46). The mother, child, and family all have different challenges as a result of postpartum depression, which may also have an impact on the mother's ability to learn about baby care (47). Nursing staff have essential duties to carry out, including subjecting patients to efficient depression screenings and carrying out different approaches of psychological care according to the characteristics of different parturients, informing them about the possible postpartum emotional changes, giving appropriate encouragement or comfort, and guiding or helping them to improve their breathing patterns so as to eliminate the fear of the parturient.
Underlying basic diseases or bad social environment
Our findings also revealed that pregnant women with basic diseases are apt to experience severer psychological symptoms. Psychological symptoms in the third trimester are related to the presence of pregnancy-related complications. Other authors (48, 49) have also found this relationship. Complications are difficult life experiences as well as a psychological burden for women. Moreover, pregnant women worry that their afflication of basic diseases will affect the health of their unborn child/children. In addition, bad social relationships (including in-laws and friends) are prone to worsen psychological symptoms. First of all, bad social relationships implies dangerous interpersonal relations, and by their nature, they may reduce social resources such as social support, and reduction in such social resources is a risk factor for mental health problems (50). Moreover, resource conservation theory (51) indicates that resource loss is the primary factor in the stress process as well as the cause of the emergence of psychological symptoms. Previous research (52) proved that the need for equal status as the husband in family relationships is one of the most influential factors causing mental disorders in pregnant women. Several lines of evidence (53–55) suggest that pregnant women may not be prepared to cope with the changes in social environments. Pregnant women are more likely to live in unstable social environments, lack security and support from their partners, and experience more marital conflict. Family members should give pregnant women full understanding and support and establish a good family support system. We should encourage tripartite talks among pregnant women, family members, and medical staffs during pregnancy to discuss how families should deal with common problems during pregnancy.
The use of birth control pills
Some studies conducted in Western communities revealed a protective effect of birth control pills against mental health problems (56, 57). However, this study showed that taking birth control pills is a risk factor for psychological symptoms. A questionnaire study (58) of 101 birth control pill users and 90 pregnant controls revealed the presence of depression in 34%, irritability in 29%, adverse effects in 64%, etc. Having had a negative reaction to the confirmation of pregnancy was related to both probable depression and major depression in all three trimesters. A prospective cohort study (59) of 2,072 women was conducted in Sabah during 2009–2010, which suggested that pregnant women who were taking birth control pills appeared to have an increased risk of depression. As described earlier, birth control pills are likely to increase emotional lability, indicating that taking birth control pills will lead to heavier psychological symptoms.
As such, all these circumstances increase the risk of pregnant women's psychological symptoms.
Strengths and limitations
Due to the complexity of the living environment and the differences between pregnant women (60), it is not convenient to simply classify individuals into whether they are in an adverse mood or not for researching pathogenesis. Thus, we explore the heterogeneity of perinatal adverse mood based on potential category variables from the pregnant respondents. The Chinese mental health scale was used to assess the adverse emotions of pregnant women, and patterns of psychological symptoms were identified to three classes by LCA, namely “high symptoms group,” “moderate symptoms group,” and “low symptoms group.” There were significant differences in 10 psychological items among different classes, which provide the convenience of implementation for investigating the relationship between the different demographic features and three latent phenotypes among Chinese pregnant women. Then, by analyzing the differences between different groups, we can find out the influencing factors that may lead to the bad mood of pregnant women.
However, the survey also has the following deficiencies and limitations. First, the sample distribution of the survey is not perfect, and the proportion of pregnant women in the high symptoms group is relatively small. Second, as a cross-sectional study, there was no follow-up survey on the production outcome and postpartum psychological status. Future research should involve larger well-designed studies, including different childbearing populations and postpartum follow-up surveys, to explore better the influencing factors of adverse emotions during pregnancy.
Conclusions
The factors of pregnant women's mental health status include difficulty in the perinatal period, marital satisfaction, in-law relationship, friend relationship, basic diseases, and taking birth control pills. To ensure the smooth progress of pregnancy and promote the physical and mental health of pregnant women, psychological screening and psychological intervention measures should be strengthened.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Xuzhou Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
WW and XZ were involved in conceptualization and methodology. YP, QC, and YZ participated in data curation and writing—original draft preparation. JW, JT, HH, and ZZ supervised and validated the study. WW participated in writing—reviewing and editing. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank all the participants involved in the survey and the medical staff at the Maternal and Child Health Hospital in Huai'an.
Funding Statement
This work was supported by the National Natural Science Foundation of China (82003484 to WW), Natural Science Fund for Colleges and Universities in Jiangsu Province (20KJB330005 to WW), and Xuzhou Science and Technology Program (KC21270 to ZZ).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Haque R, Alam K, Rahman SM, Keramat SA, Al-Hanawi MK. Women's empowerment and fertility decision-making in 53 low and middle resource countries: a pooled analysis of demographic and health surveys. BMJ Open. (2021) 11:e045952. 10.1136/bmjopen-2020-045952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Innocenti N, Vignoli D, Lazzeretti L. Economic complexity and fertility: insights from a low fertility country. Reg Stud. (2021) 55:1388–402. 10.1080/00343404.2021.1896695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henriksson HE, Malavaki C, Bränn E, Drainas V, Lager S, Iliadis SI, et al. Blood plasma metabolic profiling of pregnant women with antenatal depressive symptoms. Transl Psychiatry. (2019) 9:204. 10.1038/s41398-019-0546-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kingston DE, McDonald S, Austin MP, Hegadoren K, Lasiuk G, Tough S. The Public's views of mental health in pregnant and postpartum women: a population-based study. BMC Pregnancy Childbirth. (2014) 14:84. 10.1186/1471-2393-14-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bedaso A, Adams J, Peng W, Sibbritt D. The association between social support and antenatal depressive and anxiety symptoms among Australian women. BMC Pregnancy Childbirth. (2021) 21:708. 10.1186/s12884-021-04188-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuhler GM. The immune system and microbiome in pregnancy. Best Pract Res Clin Gastroenterol. (2020) 44–45:101671. 10.1016/j.bpg.2020.101671 [DOI] [PubMed] [Google Scholar]
- 7.Tinius RA, Yoho K, Blankenship MM, Maples JM. Postpartum metabolism: how does it change from pregnancy and what are the potential implications? Int J Womens Health. (2021) 13:591–9. 10.2147/IJWH.S314469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang X, Yang T, Miao J, Liu H, Wu K, Guo J, et al. Correlation between maternal and fetal insulin resistance in pregnant women with gestational diabetes mellitus. Clin Lab. (2018) 64:945–53. 10.7754/Clin.Lab.2018.171214 [DOI] [PubMed] [Google Scholar]
- 9.Tinius RA, Blankenship MM, Furgal KE, Cade WT, Pearson KJ, Rowland NS, et al. Metabolic flexibility is impaired in women who are pregnant and overweight/obese and related to insulin resistance and inflammation. Metabolism. (2020) 104:154142. 10.1016/j.metabol.2020.154142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Putnam KT, Wilcox M, Robertson-Blackmore E, Sharkey K, Bergink V, Munk-Olsen T, et al. Clinical phenotypes of perinatal depression and time of symptom onset: analysis of data from an international consortium. Lancet Psychiatry. (2017) 4:477–85. 10.1016/S2215-0366(17)30136-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pampaka D, Papatheodorou SI, AlSeaidan M, Wotayan RA, Wright RJ, Buring JE, et al. Postnatal depressive symptoms in women with and without antenatal depressive symptoms: results from a prospective cohort study. Arch Womens Ment Health. (2019) 22:93–103. 10.1007/s00737-018-0880-8 [DOI] [PubMed] [Google Scholar]
- 12.Kalmbach DA, Cheng P, Ong JC, Ciesla JA, Kingsberg SA, Sangha R, et al. Depression and suicidal ideation in pregnancy: exploring relationships with insomnia, short sleep, and nocturnal rumination. Sleep Med. (2020) 65:62–73. 10.1016/j.sleep.2019.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shay M, MacKinnon AL, Metcalfe A, Giesbrecht G, Campbell T, Nerenberg K, et al. Depressed mood and anxiety as risk factors for hypertensive disorders of pregnancy: a systematic review and meta-analysis. Psychol Med. (2020) 50:2128–40. 10.1017/S0033291720003062 [DOI] [PubMed] [Google Scholar]
- 14.Glover V. Prenatal mental health and the effects of stress on the foetus and the child. Should psychiatrists look beyond mental disorders? World Psychiatry. (2020) 19:331–2. 10.1002/wps.20777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beversdorf DQ, Stevens HE, Jones KL. Prenatal stress, maternal immune dysregulation, and their association with autism spectrum disorders. Curr Psychiatry Rep. (2018) 20:76. 10.1007/s11920-018-0945-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiegersma AM, Dalman C, Lee BK, Karlsson H, Gardner RM. Association of prenatal maternal anemia with neurodevelopmental disorders. JAMA Psychiatry. (2019) 76:1294–304. 10.1001/jamapsychiatry.2019.2309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maselko J, Sikander S, Bhalotra S, Bangash O, Ganga N, Mukherjee S, et al. Effect of an early perinatal depression intervention on long-term child development outcomes: follow-up of the Thinking Healthy Programme randomised controlled trial. Lancet Psychiatry. (2015) 2:609–17. 10.1016/S2215-0366(15)00109-1 [DOI] [PubMed] [Google Scholar]
- 18.Mattina GF, Van Lieshout RJ, Steiner M. Inflammation, depression and cardiovascular disease in women: the role of the immune system across critical reproductive events. Ther Adv Cardiovasc Dis. (2019) 13:1753944719851950. 10.1177/1753944719851950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bjelica A, Cetkovic N, Trninic-Pjevic A, Mladenovic-Segedi L. The phenomenon of pregnancy - a psychological view. Ginekol Pol. (2018) 89:102–6. 10.5603/GP.a2018.0017 [DOI] [PubMed] [Google Scholar]
- 20.Patten CA, Lando HA, Desnoyers CA, Klejka J, Decker PA, Bock MJ, et al. Association of tobacco use during pregnancy, perceived stress, and depression among alaska native women participants in the healthy pregnancies project. Nicotine Tob Res. (2020) 22:2104–8. 10.1093/ntr/ntz189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maschke J, Roetner J, Bösl S, Plank A-C, Rohleder N, Goecke TW, et al. Association of prenatal alcohol exposure and prenatal maternal depression with offspring low-grade inflammation in early adolescence. Int J Environ Res Public Health. (2021) 18:7920. 10.3390/ijerph18157920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Popo E, Kenyon S, Dann SA, MacArthur C, Blissett J. Effects of lay support for pregnant women with social risk factors on infant development and maternal psychological health at 12 months postpartum. PLoS ONE. (2017) 12:e0182544. 10.1371/journal.pone.0182544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheeba B, Nath A, Metgud CS, Krishna M, Venkatesh S, Vindhya J, et al. Prenatal depression and its associated risk factors among pregnant women in bangalore: a hospital based prevalence study. Front Public Health. (2019) 7:108. 10.3389/fpubh.2019.00108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joshi D, Shrestha S, Shrestha N. Understanding the antepartum depressive symptoms and its risk factors among the pregnant women visiting public health facilities of Nepal. PLoS ONE. (2019) 14:e0214992. 10.1371/journal.pone.0214992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koelewijn JM, Sluijs AM, Vrijkotte TGM. Possible relationship between general and pregnancy-related anxiety during the first half of pregnancy and the birth process: a prospective cohort study. BMJ Open. (2017) 7:e013413. 10.1136/bmjopen-2016-013413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ayaz R, Hocaoglu M, Günay T, Yardimci OD, Turgut A, Karateke A. Anxiety and depression symptoms in the same pregnant women before and during the COVID-19 pandemic. J Perinat Med. (2020) 48:965–70. 10.1515/jpm-2020-0380 [DOI] [PubMed] [Google Scholar]
- 27.Dong H, Hu R, Lu C, Huang D, Cui D, Huang G, et al. Investigation on the mental health status of pregnant women in China during the pandemic of COVID-19. Arch Gynecol Obstet. (2021) 303:463–9. 10.1007/s00404-020-05805-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lanza ST, Rhoades BL. Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prev Sci. (2013) 14:157–68. 10.1007/s11121-011-0201-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jisheng W. Compilation and standardization of Chinese adults' mental health scale. Chin J Public Health. (2006) 22:137–8. 10.3321/j.issn:1001-0580.2006.02.006 [DOI] [Google Scholar]
- 30.Laska MN, Pasch KE, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev Sci. (2009) 10:376–86. 10.1007/s11121-009-0140-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nylund K, Bellmore A, Nishina A, Graham S. Subtypes, severity, and structural stability of peer victimization: what does latent class analysis say? Child Dev. (2007) 78:1706–22. 10.1111/j.1467-8624.2007.01097.x [DOI] [PubMed] [Google Scholar]
- 32.Sun J-W, Cao D-F, Li J-H, Zhang X, Wang Y, Bai H-Y, et al. Profiles and characteristics of clinical subtypes of perinatal depressive symptoms: a latent class analysis. J Adv Nurs. (2019) 75:2753–65. 10.1111/jan.14136 [DOI] [PubMed] [Google Scholar]
- 33.Carragher N, Adamson G, Bunting B, McCann S. Treatment-seeking behaviours for depression in the general population: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Affect Disord. (2010) 121:59–67. 10.1016/j.jad.2009.05.009 [DOI] [PubMed] [Google Scholar]
- 34.Haltigan JD, Vaillancourt T. The influence of static and dynamic intrapersonal factors on longitudinal patterns of peer victimization through mid-adolescence: a latent transition analysis. J Abnorm Child Psychol. (2018) 46:11–26. 10.1007/s10802-017-0342-1 [DOI] [PubMed] [Google Scholar]
- 35.Grunwell JR, Gillespie S, Morris CR, Fitzpatrick AM. Latent class analysis of school-age children at risk for asthma exacerbation. J Allergy Clin Immunol Pract. (2020) 8:2275–84.e2272. 10.1016/j.jaip.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haviland MJ, Nillni YI, Cabral HJ, Fox MP, Wise LA, Burris HH, et al. Adverse psychosocial factors in pregnancy and preterm delivery. Paediatr Perinat Epidemiol. (2021) 35:519–29. 10.1111/ppe.12756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Míguez MC, Vázquez MB. Prevalence of depression during pregnancy in spanish women: trajectory and risk factors in each trimester. Int J Environ Res Public Health. (2021) 18:6789. 10.3390/ijerph18136789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marchesi C, Bertoni S, Maggini C. Major and minor depression in pregnancy. Obstet Gynecol. (2009) 113:1292–8. 10.1097/AOG.0b013e3181a45e90 [DOI] [PubMed] [Google Scholar]
- 39.Fuller-Tyszkiewicz M, Skouteris H, Watson BE, Hill B. Body dissatisfaction during pregnancy: a systematic review of cross-sectional and prospective correlates. J Health Psychol. (2013) 18:1411–21. 10.1177/1359105312462437 [DOI] [PubMed] [Google Scholar]
- 40.Chan CY, Lee AM, Koh YW, Lam SK, Lee CP, Leung KY, et al. Associations of body dissatisfaction with anxiety and depression in the pregnancy and postpartum periods: a longitudinal study. J Affect Disord. (2020) 263:582–92. 10.1016/j.jad.2019.11.032 [DOI] [PubMed] [Google Scholar]
- 41.Fuller-Tyszkiewicz M, Broadbent J, Richardson B, Watson B, Klas A, Skouteris H, et al. network analysis comparison of central determinants of body dissatisfaction among pregnant and non-pregnant women. Body Image. (2020) 32:111–20. 10.1016/j.bodyim.2019.12.001 [DOI] [PubMed] [Google Scholar]
- 42.Park JH, Karmaus W, Zhang H. Prevalence of and risk factors for depressive symptoms in korean women throughout pregnancy and in postpartum period. Asian Nurs Res. (2015) 9:219–25. 10.1016/j.anr.2015.03.004 [DOI] [PubMed] [Google Scholar]
- 43.Nishi D, Su K-P, Usuda K, Chang JP-C, Hamazaki K, Ishima T, et al. Plasma estradiol levels and antidepressant effects of omega-3 fatty acids in pregnant women. Brain Behav Immun. (2020) 85:29–34. 10.1016/j.bbi.2019.02.014 [DOI] [PubMed] [Google Scholar]
- 44.Barkin JL, Van Cleve S. Screening for maternal mental health in the pediatric setting: situational stressors and supports. J Pediatr Health Care. (2020) 34:405–6. 10.1016/j.pedhc.2020.04.001 [DOI] [PubMed] [Google Scholar]
- 45.Tschudin S, Huang D, Mor-Gültekin H, Alder J, Bitzer J, Tercanli S. Prenatal counseling–implications of the cultural background of pregnant women on information processing, emotional response and acceptance. Ultraschall Med. (2011) 32(Suppl 2):E100–7. 10.1055/s-0031-1281665 [DOI] [PubMed] [Google Scholar]
- 46.Mikšić Š, Miškulin M, Juranić B, Rakošec Ž, Včev A, Degmečić D. Depression and suicidality during pregnancy. Psychiatr Danub. (2018) 30:85–90. 10.24869/psyd.2018.85 [DOI] [PubMed] [Google Scholar]
- 47.Oztora S, Arslan A, Caylan A, Dagdeviren HN. Postpartum depression and affecting factors in primary care. Niger J Clin Pract. (2019) 22:85–91. 10.4103/njcp.njcp_193_17 [DOI] [PubMed] [Google Scholar]
- 48.Ajinkya S, Jadhav PR, Srivastava NN. Depression during pregnancy: prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind Psychiatry J. (2013) 22:37–40. 10.4103/0972-6748.123615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thompson O, Ajayi I. Prevalence of antenatal depression and associated risk factors among pregnant women attending antenatal clinics in Abeokuta North Local Government Area, Nigeria. Depress Res Treat. (2016) 2016:4518979. 10.1155/2016/4518979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hobfoll SE. 127 Conservation of resources theory: its implication for stress, health, and resilience. In:Folkman S, editor. The Oxford Handbook of Stress, Health, and Coping. Oxford: Oxford University Press; (2010), 127–47. 10.1093/oxfordhb/9780195375343.013.0007 [DOI] [Google Scholar]
- 52.Wang J, Pei Y, Tang J, Chen Q, He C, Zhang Y, et al. The association between family relationships and depressive symptoms among pregnant women: a network analysis. Front Psychiatry. (2022) 13:919508. 10.3389/fpsyt.2022.919508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sedgh G, Bankole A, Oye-Adeniran B, Adewole IF, Singh S, Hussain R. Unwanted pregnancy and associated factors among Nigerian women. Int Fam Plan Perspect. (2006) 32:175–84. 10.1363/3217506 [DOI] [PubMed] [Google Scholar]
- 54.Gariepy A, Lundsberg LS, Vilardo N, Stanwood N, Yonkers K, Schwarz EB. Pregnancy context and women's health-related quality of life. Contraception. (2017) 95:491–9. 10.1016/j.contraception.2017.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shandley LM, Kipling LM, Spencer JB, Morof D, Mertens AC, Howards PP. Factors associated with unplanned pregnancy among cancer survivors. J Womens Health. (2002) 31:665–74. 10.1089/jwh.2021.0176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cheslack-Postava K, Keyes KM, Lowe SR, Koenen KC. Oral contraceptive use and psychiatric disorders in a nationally representative sample of women. Arch Womens Mental Health. (2015) 18:103–11. 10.1007/s00737-014-0453-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Keyes KM, Cheslack-Postava K, Westhoff C, Heim CM, Haloossim M, Walsh K, et al. Association of hormonal contraceptive use with reduced levels of depressive symptoms: a national study of sexually active women in the United States. Am J Epidemiol. (2013) 178:1378–88. 10.1093/aje/kwt188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kane FJ Jr. Psychiatric reactions to oral contraceptives. Am J Obstet Gynecol. (1968) 102:1053–63. 10.1016/0002-9378(68)90471-7 [DOI] [PubMed] [Google Scholar]
- 59.Mohamad Yusuff AS, Tang L, Binns CW, Lee AH. Prevalence of antenatal depressive symptoms among women in Sabah, Malaysia. J Matern Fetal Neonatal Med. (2016) 29:1170–4. 10.3109/14767058.2015.1039506 [DOI] [PubMed] [Google Scholar]
- 60.Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. (2014) 384:1775–88. 10.1016/S0140-6736(14)61276-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.